Submitted:
15 September 2023
Posted:
18 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
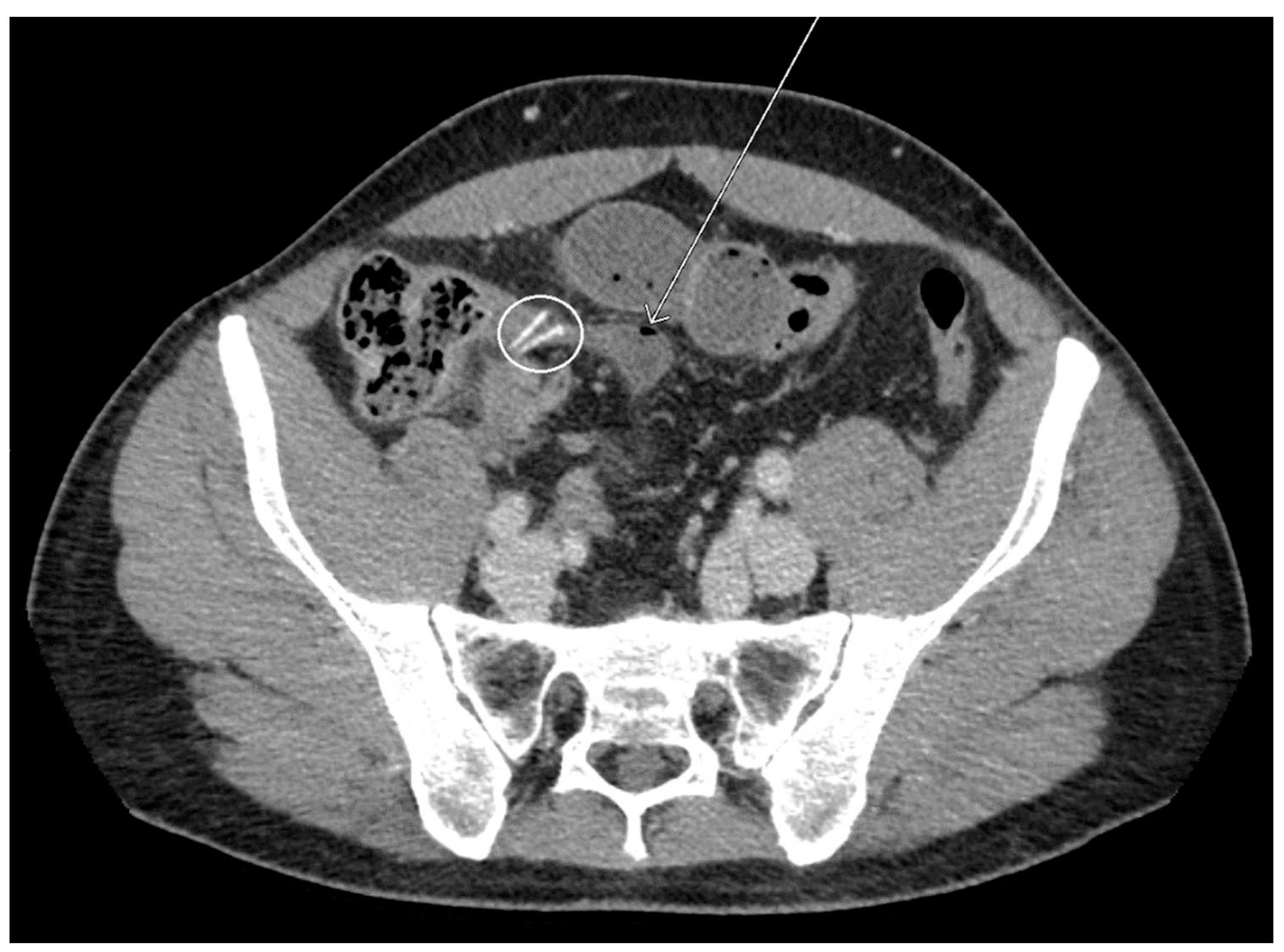
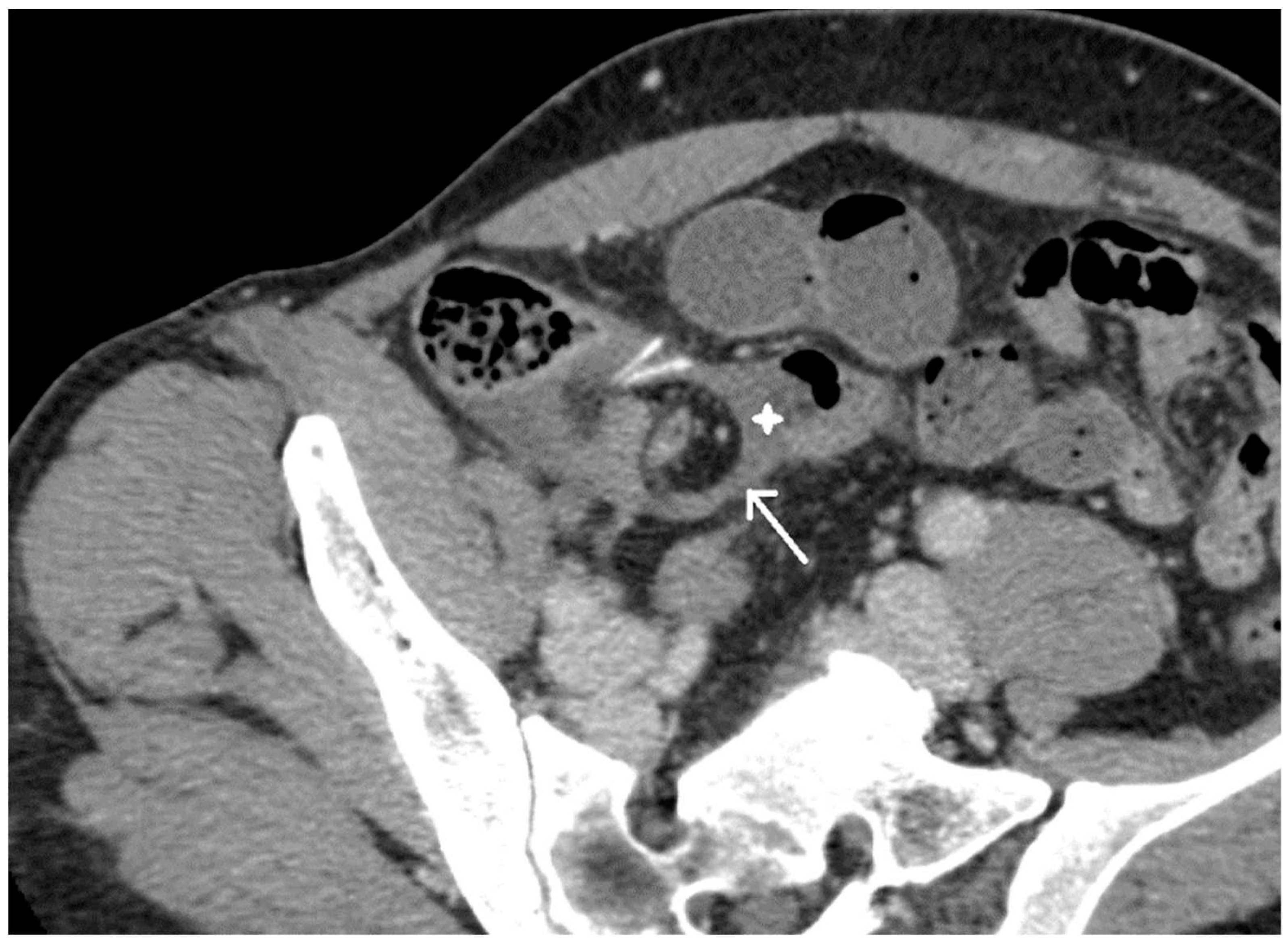
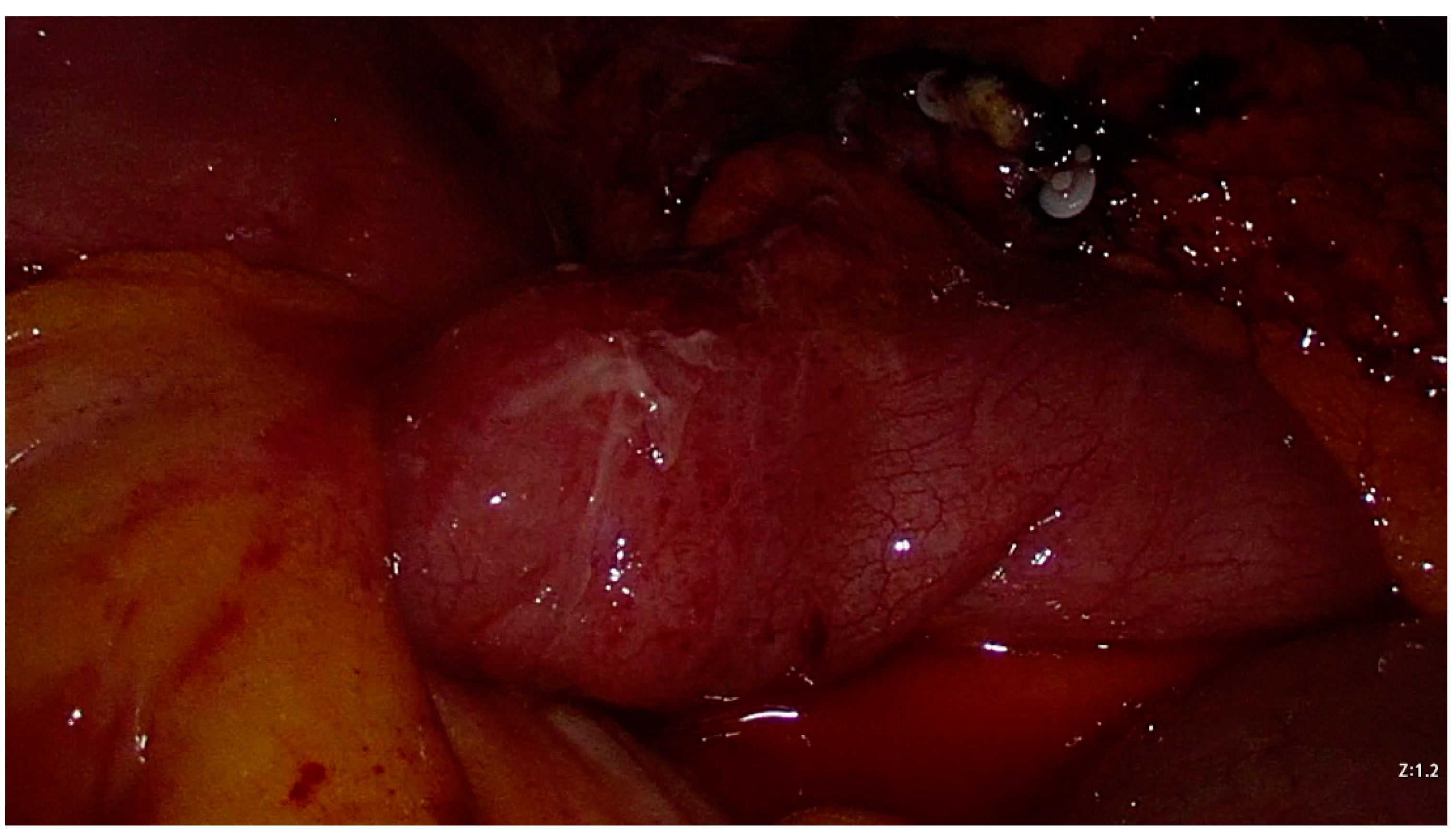
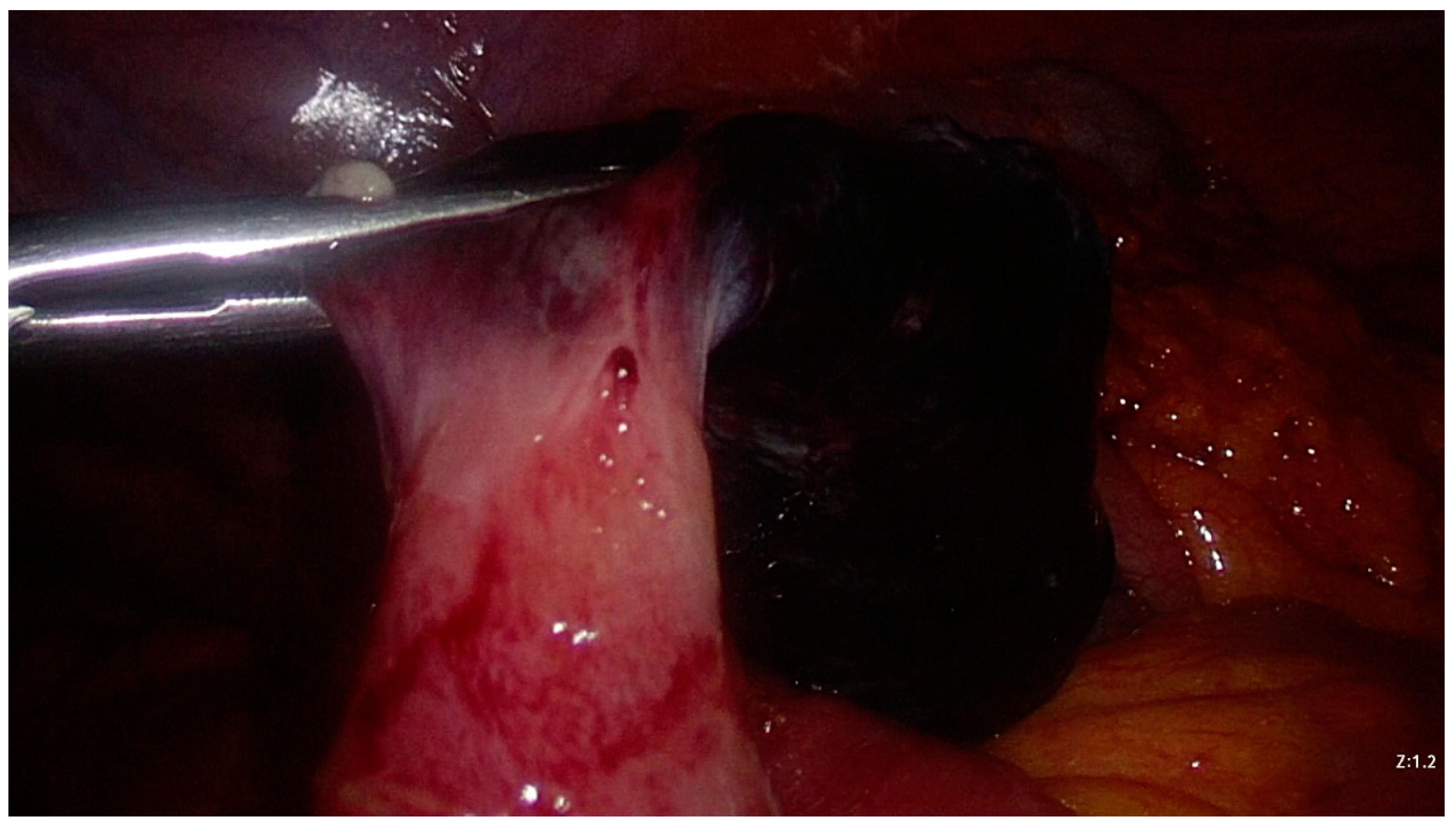
2. Case presentation
3. Materials and Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine (Baltimore). 2018 Aug;97(35):e12154. [CrossRef] [PubMed Central]
- Sagar J, Kumar V, Shah DK. Meckel’s diverticulum: a systematic review. J. R. Soc. Med. 2006; 99: 501–5.
- Sancar S, Demirci H, Sayan A, Arıkan A, Candar A. Meckel’s diverticulum: Ten years’ experience. Ulus Cerrahi Derg. 2015 Jun 1;31(2):65-7. [CrossRef] [PubMed] [PubMed Central]
- Srisajjakul S, Prapaisilp P, Bangchokdee S. Many faces of Meckel’s diverticulum and its complications. Jpn J Radiol. 2016 May;34(5):313-20. Epub 2016 Mar 1. [CrossRef] [PubMed]
- Kuru S, Kismet K. Meckel’s diverticulum: clinical features, diagnosis, and management. Rev Esp Enferm Dig. 2018 Nov;110(11):726-732. [CrossRef] [PubMed]
- Turgeon DK, Barnett JL. Meckel’s diverticulum. Am J Gastroenterol. 1990 Jul;85(7):777-81. [PubMed]
- Schaedlich DS, Borges PC, Lacombe A, Moron RA. Intestinal intussusception of Meckel’s diverticulum, a case report and literature review of the last five years. einstein (São Paulo). 2023;21:eRC0173.
- Kovacs M, Botstein J, Braverman S. Angiographic diagnosis of Meckel’s diverticulum in an adult patient with negative scintigraphy. J Radiol Case Rep. 2017 Mar 31;11(3):22-29. [CrossRef] [PubMed] [PubMed Central]
- Uppal K, Tubbs RS, Matusz P, Shaffer K, Loukas M. Meckel’s diverticulum: a review. Clin Anat. 2011 May;24(4):416-22.
- Chen JJ, Lee HC, Yeung CY, Chan WT, Jiang CB, Sheu JC, Wang NL. Meckel’s Diverticulum: Factors Associated with Clinical Manifestations. ISRN Gastroenterol. 2014 Apr 1;2014:390869. [CrossRef] [PubMed] [PubMed Central]
- Chen, Q.; Gao, Z.; Zhang, L.; Zhang, Y.; Pan, T.; Cai, D.; Xiong, Q.; Shu, Q.; Qian, Y. Multifaceted behavior of Meckel’s diverticulum in children. J. Pediatr. Surg. 2018, 53, 676–681.
- Leijonmarck CE, Bonman-Sandelin K, Frisell J, Räf L. Meckel’s diverticulum in the adult. Br J Surg. 1986 Feb;73(2):146-9. [CrossRef] [PubMed]
- Fa-Si-Oen PR, Roumen RM, Croiset van Uchelen FA. Complications and management of Meckel’s diverticulum--a review. Eur J Surg. 1999 Jul;165(7):674-8. [CrossRef] [PubMed]
- Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg. 2005 Mar;241(3):529-33. [CrossRef] [PubMed] [PubMed Central]
- Alemayehu H, Hall M, Desai AA, St Peter SD, Snyder CL. Demographic disparities of children presenting with symptomatic Meckel’s diverticulum in children’s hospitals. Pediatr Surg Int. 2014 Jun;30(6):649-53. Epub 2014 May 9. [CrossRef] [PubMed]
- Kabir SA, Raza SA, Kabir SI. Malignant neoplasms of Meckel’s diverticulum; an evidence based review. Ann Med Surg (Lond). 2019 Jun 4;43:75-81. [CrossRef] [PubMed] [PubMed Central]
- Kloss, B.T., Broton, C.E. & Sullivan, A.M. Perforated Meckel diverticulum. Int J Emerg Med 3, 455–457 (2010). [CrossRef]
- Zani A, Eaton S, Rees CM, Pierro A. Incidentally detected Meckel diverticulum: to resect or not to resect? Ann Surg. 2008 Feb;247(2):276-81. [CrossRef] [PubMed]
- Ruscher KA, Fisher JN, Hughes CD, Neff S, Lerer TJ, Hight DW, Bourque MD, Campbell BT. National trends in the surgical management of Meckel’s diverticulum. J Pediatr Surg. 2011 May;46(5):893-6.
- Sharma RK, Jain VK. Emergency surgery for Meckel’s diverticulum. World J Emerg Surg. 2008 Aug 13;3:27. [CrossRef] [PubMed] [PubMed Central]
- Mukai M, Takamatsu H, Noguchi H, Fukushige T, Tahara H, Kaji T. Does the external appearance of a Meckel’s diverticulum assist in choice of the laparoscopic procedure? Pediatr Surg Int. 2002 May;18(4):231-3. [CrossRef] [PubMed]
- Ding Y, Zhou Y, Ji Z, Zhang J, Wang Q. Laparoscopic Management of Perforated Meckel’s diverticulum in adults. Int. J. Med. Sci. 2012; 9: 243–7.
- Piñero A, Martínez-Barba E, Canteras M, Rodriguez JM, Castellanos G, Parrilla P. Surgical management and complications of Meckel’s diverticulum in 90 patients. Eur J Surg. 2002;168(1):8-12. [CrossRef] [PubMed]
- Tree K, Kotecha K, Reeves J, Aitchison L, Noeline Chui J, Gill AJ, Mittal A, Samra JS. Meckel’s diverticulectomy: a multi-centre 19-year retrospective study. ANZ J Surg. 2023 Feb 23. Epub ahead of print. [CrossRef] [PubMed]
- Lequet J, et al. Meckel’s diverticulum in the adult. Journal of Visceral Surgery (2017). [CrossRef]
- Meckel’s: A National Surgical Quality Improvement Program Survey in Adults Comparing Diverticulectomy and Small Bowel Resection Joseph G. Brungardt, MD1, Brian R. Cummiskey, MD1, and Kurt P. Schropp, MD1.
- Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV, Kavalakat AJ. Laparoscopic management of symptomatic Meckel’s diverticula: a simple tangential stapler excision. JSLS. 2008 Jan-Mar;12(1):66-70. [PubMed] [PubMed Central]
- Ezekian B, et al., Outcomes of laparoscopic resection of Meckel’s diverticulum are equivalent to open laparotomy, J Pediatr Surg (2018). [CrossRef]
- Rahmat S, Sangle P, Sandhu O, Aftab Z, Khan S. Does an Incidental Meckel’s Diverticulum Warrant Resection? Cureus. 2020 Sep 8;12(9):e10307. [CrossRef] [PubMed] [PubMed Central]
- WEINSTEIN EC, CAIN JC, REMINE WH. Meckel’s diverticulum: 55 years of clinical and surgical experience. JAMA. 1962 Oct 20;182:251-3. [CrossRef] [PubMed]
- Soltero MJ, Bill AH. The natural history of Meckel’s Diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel’s Diverticulum found in King County, Washington, over a fifteen year period. Am J Surg. 1976 Aug;132(2):168-73. [CrossRef] [PubMed]
- DiGiacomo JC, Cottone FJ. Surgical treatment of Meckel’s diverticulum. South Med J. 1993 Jun;86(6):671-5. [CrossRef] [PubMed]
- Peoples JB, Lichtenberger EJ, Dunn MM. Incidental Meckel’s diverticulectomy in adults. Surgery 1995;118:649-52.
- Cullen JJ, Kelly KA, Moir CR, Hodge DO, Zinsmeister AR, Melton LJ 3rd. Surgical management of Meckel’s diverticulum. An epidemiologic, population-based study. Ann Surg. 1994 Oct;220(4):564-8; discussion 568-9. [CrossRef] [PubMed] [PubMed Central]
- Matsagas MI, Fatouros M, Koulouras B, Giannoukas AD. Incidence, complications, and management of Meckel’s diverticulum. Arch Surg. 1995 Feb;130(2):143-6. [CrossRef] [PubMed]
- Bani-Hani KE, Shatnawi NJ. Meckel’s diverticulum: comparison of incidental and symptomatic cases. World J Surg. 2004Sep;28(9):917-20. [CrossRef] [PubMed]
- Chiu EJ, Shyr YM, Su CH, Wu CW, Lui WY. Diverticular disease of the small bowel. Hepatogastroenterology. 2000 Jan-Feb;47(31):181-4. [PubMed]
- Zulfikaroglu B, Ozalp N, Zulfikaroglu E, Ozmen MM, Tez M, Koc M. Is incidental Meckel’s diverticulum resected safely? N Z Med J. 2008 Sep 22;121(1282):39-44. [PubMed]
- Thirunavukarasu P, Sathaiah M, Sukumar S, Bartels CJ, Zeh H 3rd, Lee KK, Bartlett DL. Meckel’s diverticulum--a high-risk region for malignancy in the ileum. Insights from a population-based epidemiological study and implications in surgical management. Ann Surg. 2011 Feb;253(2):223-30. [CrossRef] [PubMed] [PubMed Central]
- Caracappa D, Gullà N, Lombardo F, Burini G, Castellani E, Boselli C, Gemini A, Burattini MF, Covarelli P, Noya G. Incidental finding of carcinoid tumor on Meckel’s diverticulum: case report and literature review, should prophylactic resection be recommended? World J Surg Oncol. 2014 May 8;12:144. [CrossRef] [PubMed] [PubMed Central]
- Kilius, A., Samalavicius, N.E., Danys, D. et al. Asymptomatic heterotopic pancreas in Meckel’s diverticulum: a case report and review of the literature. J Med Case Reports 9, 108 (2015). [CrossRef]
- Jadlowiec CC, Bayron J, Marshall WT 3rd. Is an Incidental Meckel’s Diverticulum Truly Benign? Case Rep Surg. 2015;2015:679097. Epub 2015 Feb 9. [CrossRef] [PubMed] [PubMed Central]
- Gezer HÖ, Temiz A, İnce E, Ezer SS, Hasbay B, Hiçsönmez A. Meckel diverticulum in children: Evaluation of macroscopic appearance for guidance in subsequent surgery. J Pediatr Surg. 2016 Jul;51(7):1177-80. Epub 2015 Sep 15. [CrossRef] [PubMed]
- Mora-Guzmán I, Muñoz de Nova JL, Martín-Pérez E. Neuroendocrine tumours within a Meckel’s diverticulum. Ann R Coll Surg Engl. 2018 Jan;100(1):e10-e11. Epub 2017 Oct 19. [CrossRef] [PubMed] [PubMed Central]
- Ismael Mora-Guzmán, José Luis Muñoz de Nova & Elena Martín-Pérez (2018): Meckel’s diverticulum in the adult: surgical treatment, Acta Chirurgica Belgica. [CrossRef]
- Demirel B. D. , Hancıoglu S. , Bicakci U. , Bernay F. , Ariturk E. Complications of Meckel’s diverticulum in children: A 10-years experience. J. Exp. Clin. Med.. 2020; 36(3): 67-71.
- Stone PA, Hofeldt MJ, Campbell JE, Vedula G, DeLuca JA, Flaherty SK. Meckel diverticulum: ten-year experience in adults. South Med J. 2004 Nov;97(11):1038-41. [CrossRef] [PubMed]
- Mackey WC, Dineen P. A fifty year experience with Meckel’s diverticulum. Surg Gynecol Obstet. 1983 Jan;156(1):56-64. [PubMed]
- Ueberrueck T, Meyer L, Koch A, Hinkel M, Kube R, Gastinger I. The significance of Meckel’s diverticulum in appendicitis--a retrospective analysis of 233 cases. World J Surg. 2005 Apr;29(4):455-8. [CrossRef] [PubMed]
- Robijn J, Sebrechts E, Miserez M. Management of incidentally found Meckel’s diverticulum a new approach: resection based on a Risk Score. Acta Chir Belg. 2006 Jul-Aug;106(4):467-70. [CrossRef] [PubMed]
- Vane DW, West KW, Grosfeld JL. Vitelline duct anomalies. Experience with 217 childhood cases. Arch Surg. 1987 May;122(5):542-7. [CrossRef] [PubMed]
- St-Vil D, Brandt ML, Panic S, Bensoussan AL, Blanchard H. Meckel’s diverticulum in children: a 20-year review. J Pediatr Surg. 1991 Nov;26(11):1289-92. [CrossRef] [PubMed]
- Onen A, Ciğdem MK, Oztürk H, Otçu S, Dokucu AI. When to resect and when not to resect an asymptomatic Meckel’s diverticulum: an ongoing challenge. Pediatr Surg Int. 2003 Apr;19(1-2):57-61. Epub 2003 Jan 17. [CrossRef] [PubMed]
- Groebli Y, Bertin D, Morel P. Meckel’s diverticulum in adults: retrospective analysis of 119 cases and historical review. Eur J Surg. 2001 Jul;167(7):518-24. [CrossRef] [PubMed]
- Dumper J., Mackenzie S., Mitchell P., Sutherland F., Quan M.L., Mew D. Complications of Meckel’s diverticula in adults. Can. J. Surg. 2006;49:353–357.
- McKay R. High incidence of symptomatic Meckel’s diverticulum in patients less than fifty years of age: an indication for resection. Am Surg. 2007 Mar;73(3):271-5. Erratum in: Am Surg. 2007 Dec;73(12):1293. [PubMed]
- Blouhos K, Boulas KA, Tsalis K, et al. Meckel’s diverticulum in adults: surgical concerns [J]. Front Surg 2018; 5: 55.
- Chen Y, Liu Y, Jiang L, Jiang F, Zhu T. Axially torsional b Meckel’s diverticulum accompanied by small bowel volvulus: a case report. J Int Med Res. 2021 Oct;49(10):3000605211053554. [CrossRef] [PubMed] [PubMed Central]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




