1. Introduction
The rapid advancement of wireless telecommunication technologies has resulted in significant exposure of the general public to electromagnetic fields (EMFs). Nowadays, people are constantly exposed to various sources of EMFs, including mobile phones, mobile base stations, cordless phones, Wi-Fi routers, and power lines. Consequently, global concerns about the potential adverse health effects of EMF exposure have prompted researchers to investigate the extent to which low-intensity EMFs may affect human health and other organisms.
Several studies have investigated the potential health effects of exposures to microwave radiation, EMFs, radiofrequency (RF), and radiofrequency electromagnetic radiations [
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15]. A cross-sectional study found that individuals living within <300 meters of mobile base stations reported more frequent symptoms of nausea, headache, dizziness, irritability, discomfort, nervousness, depression, sleep disturbance, memory loss, and diminished libido compared to those living further away (>300 meters) [
16]. In a review published in 2010, 8 out of 10 studies through PubMed reported an increased prevalence of adverse neurobehavioral symptoms in populations living within <500 meters of base stations, as well as other effects such as headache, fatigue, sleep disturbance, and poor concentration [
5].
The potential adverse health effects of human exposure to radiofrequency electromagnetic fields, including long-term effects such as an increased risk of cancer, are well-documented. Jooyan and Mortazavi addressed the challenging issue of the carcinogenesis of radiofrequency radiation in their commentary published in JAMA Oncology and also highlighted the shortcomings of studies that do not support a potential link between exposure to radiofrequency radiation and increased cancer risk[
17].
The exposure from broadcasting sites and base stations affects the entire body from a distance, while smartphones and smart gadgets only affect the head and hands in close proximity[
18]. Recent studies show that mobile phone base stations are the primary source of the radiofrequency radiation spectrum[
19]. A review conducted on the effects of base station antennas on human health in 2022 revealed three types of impacts: radiofrequency sickness, cancer, and changes in biochemical parameters. Out of the 38 studies reviewed globally, 28 showed some form of effect, with radiofrequency sickness being the most common at 73.9% [
20]. A case study conducted in Stockholm, Sweden investigated the effects of electromagnetic hypersensitivity (EHS) near mobile phone base stations[
21]. Epidemiology studies are the primary focus of RF research concerning human exposure, even though it is challenging to separate distance from a tower as an independent variable and determine actual exposure levels due to the prevalence of ELF and RF fields in daily life through personal wireless devices. This poses a potential weakness in such studies as it becomes difficult to find unexposed controls[
22].
Given the exponential growth of wireless technology, developing a model to predict potential adverse health effects in advance could help minimize health hazards and symptoms for those living or planning to settle in close proximity to mobile phone base stations. Such models could also be used as a precautionary measure when siting mobile base stations to minimize potential health hazards.
While the adverse health effects of living in proximity to MPBS are well-documented, reports on using artificial intelligence-based models to predict subjective health symptoms in people living or working near these stations are scarce. In a previous study, we proposed multilayer perceptron neural network (MLPNN)-based models to predict subjective health symptoms among individuals living near cellular phone base stations[
23]. The system provided promising results, but its sensitivity in predicting symptoms such as fatigue was low. Therefore, there is a need for a more accurate model for early detection of health symptoms among individuals living near mobile stations.
In this work, we explored the possibility of developing a reliable and applicable model using the Support Vector Machines (SVM) algorithm, which hasbeen shown to be a robust method for classification and pattern recognition[
24] , particulary effective in analyzing medical data[
24,
25,
26]. The rest of this paper includes a brief discussion of the classifiers used, a description of the methodology, and the results and discussion sections.
To the best of our knowledge, despite some limitations such as subjective symptom reporting, this is the first study to use Support Vector Machines to predict subjective health symptoms among individuals living near cellular phone base stations. The key advantage of the SVM-based model developed in our study is its excellent performance in terms of accuracy and AUC.
2. Materials and Methods
The objective of this study was to develop a model for predicting the subjective health symptoms of individuals living near mobile base stations, with a focus on the five common complaints of headache, sleep disturbance, dizziness, vertigo, and fatigue. The desired model should determine whether an individual might have one or more of these symptoms. The development process included three main steps: data collection, data preprocessing, and model development. A detailed description of these steps is provided below.
2.1. Data collection
Data collection was performed through a cross-sectional study of 699 adults, including 363 men (32 ±13 years) and 336 women (32 ±12 years), all living in the close vicinity of cellular phone base stations in 11 different districts of Shiraz, Iran. The inhabitants were selected randomly, with 20% of the stations in each district selected randomly. Buildings located up to 1km from the selected stations were grouped into four categories based on their distance from the nearest station (D); Group 1 for D < 100m, Group 2 for 100m < D < 300m, Group 3 for 300m < D < 600m, and Group 4 for 600m < D < 1000m. These ranges were used since a previous study revealed that individuals living at D < 300m from the base station might experience subjective symptoms such as tiredness, headache, sleep disturbance, discomfort, irritability, depression, loss of memory, dizziness, and diminished libido[
16].
A questionnaire was administered, containing questions on demographic data, subjective complaints, and occupational and environmental exposure to different sources of electromagnetic fields. The average electric and magnetic field strengths were measured in each household using a recently calibrated EMF meter. Personal information, along with comprehensive details of the participants’ lifestyles, was collected by trained interviewers. For each participant, age, gender, education level, mobile phone usage during day/week/month, and the distance of the living/working place to the base station tower were recorded. Ultimately, 11 parameters related to the living status of each participant were recorded, and subjective complaints including nausea, headache, dizziness, irritability, discomfort, nervousness, depression, sleep disturbance, memory loss, and diminished libido were recorded. Written informed consent was obtained from each participant before they participated in the study. Data collection was conducted through door-to-door measurements and face-to-face interviews.
2.2. Statistical analysis and data preprocessing
This step aimed to identify and remove outliers or unusual observations and select the variables to be used in the model Graphical display methods like scatterplots and box plots were used, along with quantitative methods such as the Interquartile Range (IQR). Inconsistent data, such as daily cellphone usage exceeding 24 hours, were considered unacceptable parameters. Each feature variable was normalized using the min-max scaling method (Equation 1), which scales the variables to a range of 0 to 1.
where
x is an original value of a given variable and
is the normalized value.
2.3. Model Development
The model development process consisted of two main steps: feature selection and classification. In the feature selection step, we aimed to identify relevant predictors and eliminate irrelevant ones. We utilized a neighborhood component analysis method, a non-parametric technique that estimates the relative weight of each variable by maximizing the expected classification accuracy. Additional details on the algorithms can be found in reference [
27]. Ultimately, after the selection process, we identified 11 parameters related to the individuals' living status that proved effective for the model. The list of these parameters and a description of each one is provided in
Table 1.
Table 1.
The list of variables included in subjective health symptoms prediction model.
Table 1.
The list of variables included in subjective health symptoms prediction model.
| Variable |
Description |
| Age |
Age (year), at the time of interview |
| Gender |
Gender (male/female/not declared) |
| Mobile phone call time |
Average daily call time (min) |
| History of mobile phone usage |
Number of months of mobile phone usage |
| Cordless phone use |
Average daily call time using cordless phones (min) |
| VDU use |
Average daily use of Video Display Units (VDUs) (min) |
| Distance from base station |
Distance from the nearest mobile base station (m) |
| Duration of residence |
Duration of residence in the present house (month) |
| Exposure time |
Average daily exposure time to mobile base stations (h) |
| Exposure to power lines |
Living in the vicinity of a power line (yes/no) |
| Other wireless devices |
Exposure to other sources of electromagnetic fields (yes/no) |
The objective of the model was to predict subjective health symptoms in individuals living near mobile base stations using the 11 living status parameters outlined in
Table 1. Specifically, the model aimed to determine whether a participant experienced one or more health symptoms, such as headache, sleep disturbance, dizziness, vertigo, and fatigue. This task falls under the classification category in machine learning, where the class of a new sample is determined based on known class labels in a given dataset. In our study, we employed Support Vector Machines (SVM) and Random Forest (RF) algorithms to develop the desired prediction models. The models were developed using Matlab's Statistics and Machine Learning Toolbox (Mathworks, Natick MA, USA).
Support Vector Machines (SVM) is a statistical supervised learning model that minimizes structural risk theory, effectively addressing common machine learning challenges like overfitting and local minimum [
28]. It achieves this by minimizing an upper bound on the generalization error, a crucial objective in statistical pattern recognition and automated estimation systems. We trained the SVM using the Sequential Minimal Optimization (SMO) method, as described in reference[
29].
Random Forest (RF) algorithm generates multiple decision trees, with each tree incorporating random features. The trees are constructed by selecting the most informative features to separate classes, and the process continues recursively based on the dataset. Training in the random forest occurs through bagging and replacement, where random subsets are chosen from the dataset, and a tree is fitted to each subset. To classify a test sample, it is classified by each tree, and the outputs of the trees are combined to make the final decision. The RF model employed 100 decision trees to create a forest, and the Gini impurity metric was used to measure attribute importance. Aggregating the outputs of the classifiers through majority voting is a common practice in the RF algorithm.
2.4. Model Evaluation
The performance of the developed model was evaluated quantitatively using sensitivity, specificity, and accuracy indices. These indices help measure the accuracy and effectiveness of the classification process in correctly identifying individuals with or without symptoms.These three indices are given by:
where the parameters TP,TN, FP, and FN are defined as follows:
TP: The number of subjects correctly classified as having a symptom.
TN: The number of subjects correctly classified as not having a symptom.
FP: The number of individuals without a symptom that are incorrectly identified as having a symptom.
FN: The number of individuals with a symptom that are incorrectly identified as not having a symptom.
To estimate these indices, the subjective complaints recorded during data collection were considered as the "gold standard" for training and testing the model. To ensure unbiased estimation and ultimately an unbiased evaluation of the model, the data were randomly divided into three parts: a training set comprising 75% of the data, a validation set with 5% of the data, and a test set containing 20% of the data.
The training set was used to find the support vectors and determine the parameters of the decision function [
28]. The validation dataset was utilized to select the best parameters for the model and optimize it by finding the optimal values for regularization parameters, the kernel function, and its parameters.
The RF model was trained using the bagging method, which involves randomly sampling subsets of the training data, fitting a decision tree to each subset, and aggregating the predictions. This RF model utilizes the Gini impurity metric to measure the quality of nodes and branches, aiming to achieve the best results.
Finally, the test dataset was employed to evaluate the final model fitted to the training dataset. This evaluation involved comparing the predicted values for these examples with the actual values, providing a measure of the model's performance.
3. Results
Once the models were developed, we evaluated their performance using data collected from 140 samples (test data) and four performance indices: sensitivity, specificity, accuracy, and area under the receiver operating characteristic curve (AUC). The performance of the developed models, as measured by the three indices mentioned above, is summarized in
Table 2. For comparison, we also included the results of a previously developed model (MLPNN-based model) described in reference [
23].
The SVM-based model demonstrated excellent performance in predicting health symptoms such as headache, sleep disturbance, dizziness, vertigo, and fatigue. For example, it achieved accuracies of 85.3%, 82%, 84%, 82.4%, and 65.1% respectively. The corresponding AUCs were 0.99, 0.98, 0.92, 0.89, and 0.81 respectively. Compared to the RF model and the previously developed model, the SVM-based model showed higher sensitivity (83.4%, 85.3%, 73%, 69%, and 70% for headache, sleep disturbance, dizziness, vertigo, and fatigue respectively). Notably, it significantly improved sensitivity and AUC for predicting fatigue, with values of 70% and 0.81 respectively, compared to 8% and 0.62 for MLPNN, and 11.1% and 0.64 for RF.
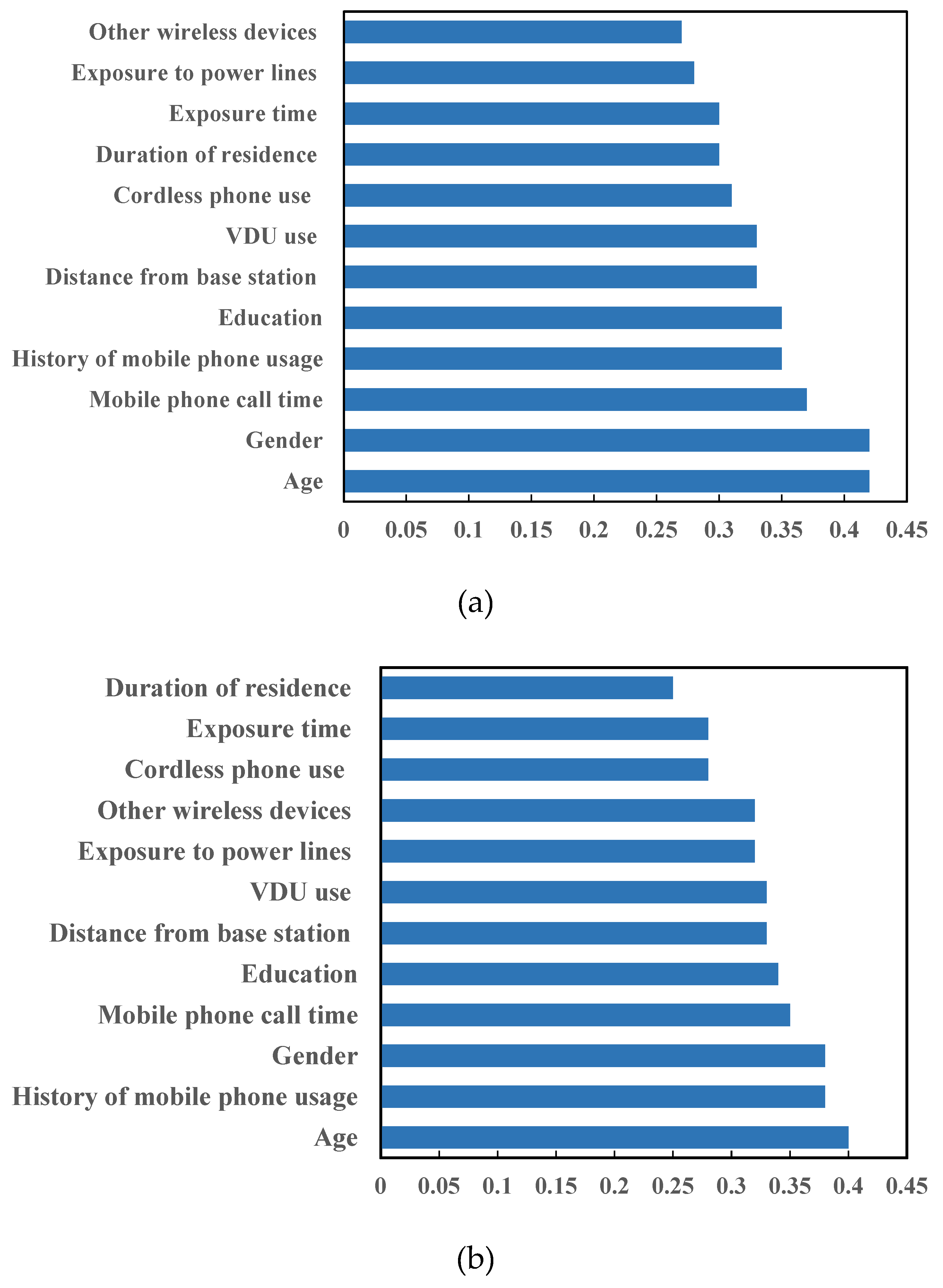
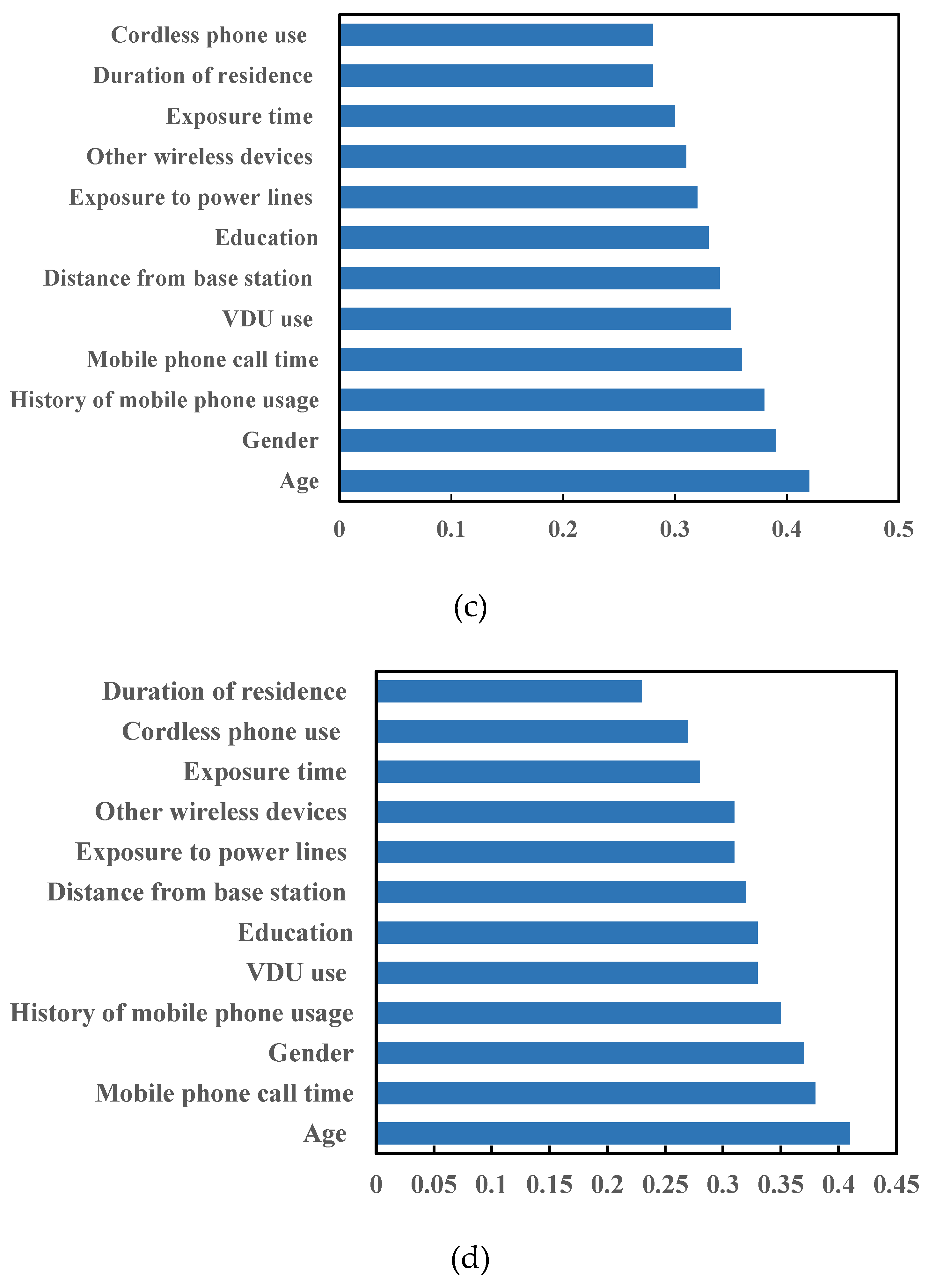
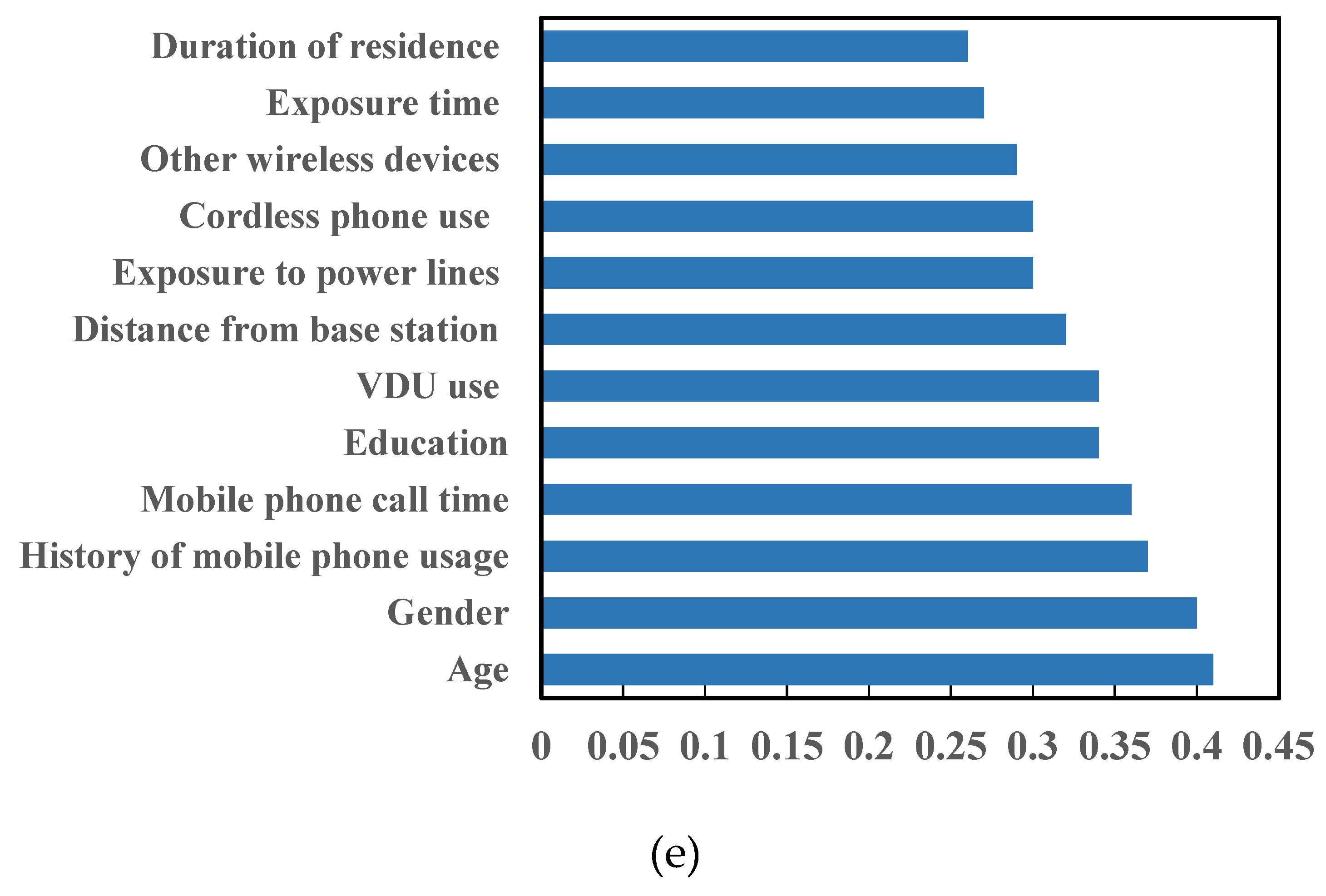
Figure 1 presents the relative attribute importance for the variables included in the model. These numbers were estimated based on the average impurity for each class in the random forest algorithm. The figure highlights three variables as the most important predictors of health symptoms: the distance from the mobile base station, the age of the participant, and the duration of residence in the area.
4. Discussion
The aim of this study was to explore the potential of AI in predicting the health risks associated with exposure to EMF. The results presented in
Table 2 demonstrate that the SVM-based system outperforms other systems in predicting subjective health symptoms for most cases, as indicated by higher sensitivity and AUC values. This finding is consistent with previous studies highlighting the effectiveness of SVM in classification problems [
26,
30]. However, the accuracy in predicting fatigue symptoms using the SVM-based model is slightly lower than that of other symptoms. This discrepancy can be attributed to the multifactorial nature of fatigue, which can stem from various factors other than EMF exposure.
A comparison between the SVM-based model and the previously developed MLPNN-based model (23) revealed that SVM's superior performance can be attributed to its focus on minimizing generalization error during training. In contrast, MLPNNs tend to overfit the training data, resulting in lower performance on unseen data. These results align with previous research highlighting SVM's capability in classification problems [
26,
30].
There is one exception observed in
Table 2, where the accuracy of the SVM in predicting fatigue symptoms is lower than both the MLPNN-based model (23) and RF-based model. However, the sensitivity of the SVM-based model for fatigue symptoms is significantly higher than that of the other models. This trade-off between sensitivity and accuracy indicates that improving one metric may come at the cost of the other. In this study, we addressed this trade-off by incorporating class weights in training the classifier, assigning higher costs to false negative errors compared to false positive errors (FN=2FP). Consequently, the AUC value of the SVM for predicting fatigue symptoms is higher than that of the other models.
The relative attribute importance results for the variables (Fig. 1) indicate that "age" and "gender" have the most significant influence on health symptoms. Additionally, both "mobile usage factors (history and call time)" are among the top four influential parameters. However, the effect of other attributes on cognitive symptoms is also comparable to that of the most important one. These findings are consistent with previously published works that reported "mobile phone usage" and "age" as among the top four influential features for each cognitive symptom [
23].
From a broader perspective, our findings align with studies that have reported that while there are increasing concerns about the detrimental health effects of RF-EMF exposures from mobile phone base stations, health complaints of people living near base stations cannot be fully explained by these concerns [
31]. Notably, previous large population-based studies have shown that residents who were concerned about or attributed detrimental biological effects of RF-EMF generated by mobile phone base stations, as well as those living closer to the base station (e.g., <500 m), had more health complaints compared to others [
31]. Furthermore, our results support reports showing the presence of sleep disturbances, headaches, dizziness, irritability, concentration difficulties, and hypertension in the majority of people residing near mobile phone base stations [
32]. Additionally, our results align with reports indicating a higher risk of developing neuropsychiatric problems in people living in the vicinity of mobile phone base stations (9). Headache, memory changes, dizziness, tremors, depressive symptoms, and sleep disturbance have been reported to be significantly higher in people living around mobile phone base stations [
33].
Regarding the co-existence of proximity to power lines and mobile phone base stations, our results are in line with studies that associate perceived proximity to both with non-specific physical symptoms (NSPS) (29). However, our findings contradict a limited number of studies that reported no significant association between measured RF-EMFs emitted from mobile phone base stations and adverse health effects [
34].
The practical application of our study lies in utilizing AI to predict health risks associated with EMF exposure. By employing relatively simple and easily measurable variables as inputs, our model can predict the health status of individuals residing near cellular phone base stations. This predictive capability can aid in assessing potential health risks for those currently living near these stations or individuals considering moving to such areas. Consequently, the model can contribute to the reduction of EMF-related health risks and inform decision-making processes related to the management and establishment of mobile base stations.
While this study presents promising results, it is essential to acknowledge its limitations. All variables used, including both input and output variables, rely on self-reports, which introduce a degree of uncertainty in the values. Achieving accurate estimates for these parameters would require individual monitoring using specialized instruments, which may pose logistical challenges. However, the focus of this study was to develop a practical model using easily accessible variables. Furthermore, the findings should be considered preliminary, and further evaluation of the model's predictability and reliability is necessary using a more extensive dataset with long-term follow-up, such as a five-year study. Future research should also explore the inclusion of additional variables, such as weight, hours of sleep per night, general health, and socio-economic factors. Deep statistical analysis, such as multidimensional analysis, can provide deeper insights, and the model's performance should be assessed over an extended follow-up period.
5. Conclusions
Our study demonstrates that mitigating the impact of microwave radiation on the human nervous system and cognitive functions requires consideration of various factors, including environmental exposure to mobile phone base stations and individual health conditions. By harnessing the power of AI, healthcare providers can better understand and predict the health risks associated with EMF exposure, enabling them to deliver targeted interventions and support to affected individuals. In this study, we successfully implemented an SVM classifier to predict five subjective health symptoms, surpassing the performance of a previously developed MLPNN-based model. The findings of this research underscore the potential of AI-based models in assisting healthcare professionals, including physicians, in effectively managing symptoms associated with EMF exposure in individuals living near mobile phone base stations. Future work should include additional variables, statistical analyses, and longer follow-up periods.
Acknowledgments
This study was funded by Shiraz University of Medical Sciences (grant number 97-01-106-19326). The authors wish to thank H. Argasi at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for his invaluable assistance in editing this manuscript.
References
- Calvente, I.; Pérez-Lobato, R.; Nuñez, M.; Ramos, R.; Guxens, M.; Villalba, J.; Olea, N.; Fernández, M. Does exposure to environmental radiofrequency electromagnetic fields cause cognitive and behavioral effects in 10-year-old boys? Bioelectromagnetics 2016, 37, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Woelders, H.; Wit, A.; Lourens, S.; Stockhofe, N.; Engel, B.; Hulsegge, I.; Schokker, D.; van Heijningen, P.; Vossen, S.; Bekers, D.; et al. Study of potential health effects of electromagnetic fields of telephony and Wi-Fi, using chicken embryo development as animal model: Health Effects of Electromagnetic Fields. Bioelectromagnetics 2017, 38. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, A.R.; Mortazavi, G.; Mortazavi, S.M.J. Comments on Meo et al. Association of Exposure to Radio-Frequency Electromagnetic Field Radiation (RF-EMFR) Generated by Mobile Phone Base Stations with Glycated Hemoglobin (HbA1c) and Risk of Type 2 Diabetes Mellitus. International Journal of Environmental Research and Public Health 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, S.M.J.; Mahbudi, A.; Atefi, M.; Bagheri, s.; Bahaedini, N.; Besharati, A. An old issue and a new look: Electromagnetic hypersensitivity caused by radiations emitted by GSM mobile phones. Technology and health care : official journal of the European Society for Engineering and Medicine 2011, 19, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Khurana, V.; Hardell, L.; Everaert, J.; Bortkiewicz, A.; Carlberg, M.; Ahonen, M. Epidemiological Evidence for a Health Risk from Mobile Phone Base Stations. International journal of occupational and environmental health 2010, 16, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Mortavazi, S.; Habib, A.; Ganj-Karami, A.; Samimi-Doost, R.; PourAabedi, A.; Babaee, A. Alterations in TSH and Thyroid Hormones Following Mobile Phone Use. Oman medical journal 2009, 24, 274–278. [Google Scholar] [CrossRef]
- Gaafar Abdel-Rassoul, A.; El-Fateh, O.; Abou Salem, M.; Michael, A.; Farahat, F.; Al-Batanony, M.; Salem, E. Neurobehavioral effects among inhabitants around mobile phone base stations. Neurotoxicology 2007, 28, 434–440. [Google Scholar] [CrossRef]
- Hutter, H.P.; Moshammer, H.; Wallner, P.; Kundi, M. Subjective symptoms, sleeping problems, and cognitive performance in subjects living near mobile phone base stations. Occupational and environmental medicine 2006, 63, 307–313. [Google Scholar] [CrossRef]
- Habash, R.; Brodsky, L.; Leiss, W.; Krewski, D.; Repacholi, M. Health Risks of Electromagnetic Fields. Part I: Evaluation and Assessment of Electric and Magnetic Fields. Critical reviews in biomedical engineering 2003, 31, 141–195. [Google Scholar] [CrossRef]
- Habash, R.; Brodsky, L.; Leiss, W.; Krewski, D.; Repacholi, M. Health Risks of Electromagnetic Fields. Part II: Evaluation and Assessment of Radio Frequency Radiation. Critical reviews in biomedical engineering 2003, 31, 197–254. [Google Scholar] [CrossRef]
- Santini, R.; Santini, P.; Ruz, P.; Danze, J.; Seigne, M. Survey Study of People Living in the Vicinity of Cellular Phone Base Stations. Electromagnetic Biology and Medicine 2003, 22, 41–49. [Google Scholar] [CrossRef]
- Medicine, N.L.o. Index Medicus; U.S. Department of Health, Education, and Welfare, Public Health Service, National Institutes of Health, National Library of Medicine: 2002.
- Repacholi, M.H. Low-level exposure to radiofrequency electromagnetic fields: health effects and research needs. Bioelectromagnetics 1998, 18, 1–19. [Google Scholar] [CrossRef]
- Bortkiewicz, A.; Gadzicka, E.; Szyjkowska, A.; Politanski, P.; Mamrot, P.; Szymczak, W.; Zmyslony, M. Subjective complaints of people living near mobile phone base stations in Poland. International journal of occupational medicine and environmental health 2012, 25, 31–40. [Google Scholar] [CrossRef]
- Eskander, E.; Estefan, S.; Abd-Rabou, A. How does long term exposure to base stations and mobile phones affect human hormone profiles? Clinical biochemistry 2011, 45, 157–161. [Google Scholar] [CrossRef] [PubMed]
- SA., A. Mobile Phone Base Stations Health Effects. . Diyala J Med 2011., 1:44,.
- Jooyan, N.; Mortazavi, S.M. Evidence Base on the Potential Carcinogenicity of Radiofrequency Radiation. JAMA Oncology 2022, 8, 948. [Google Scholar] [CrossRef] [PubMed]
- Hansson Mild, K.; Mattsson, M.O.; Jeschke, P.; Israel, M.; Ivanova, M.; Shalamanova, T. Occupational Exposure to Electromagnetic Fields-Different from General Public Exposure and Laboratory Studies. Int J Environ Res Public Health 2023, 20. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Han, M.; Chen, Y.; Yue, Y. Public exposure to broadband electromagnetic fields and its association with population density and building density: The case study of Beijing. Heliyon 2023, 9, e17153. [Google Scholar] [CrossRef]
- Balmori, A. Evidence for a health risk by RF on humans living around mobile phone base stations: From radiofrequency sickness to cancer. Environ Res 2022, 214, 113851. [Google Scholar] [CrossRef]
- Hardell, L.; Koppel, T. Electromagnetic hypersensitivity close to mobile phone base stations - a case study in Stockholm, Sweden. Rev Environ Health 2023, 38, 219–228. [Google Scholar] [CrossRef]
- McCredden, J.E.; Cook, N.; Weller, S.; Leach, V. Wireless technology is an environmental stressor requiring new understanding and approaches in health care. Front Public Health 2022, 10, 986315. [Google Scholar] [CrossRef]
- Parsaei, H.; Faraz, M.; Mortazavi, S.M.J. A Multilayer Perceptron Neural Network–Based Model for Predicting Subjective Health Symptoms in People Living in the Vicinity of Mobile Phone Base Stations. Ecopsychology 2017, 9. [Google Scholar] [CrossRef]
- Huang, S.; Cai, N.; Pacheco, P.; Narrandes, S.; Wang, Y.; Xu, W. Applications of Support Vector Machine (SVM) Learning in Cancer Genomics. Cancer genomics & proteomics 2018, 15, 41–51. [Google Scholar] [CrossRef]
- Taherisadr, M.; Dehzangi, O.; Parsaei, H. Single Channel EEG Artifact Identification Using Two-Dimensional Multi-Resolution Analysis. Sensors 2017, 17, 2895. [Google Scholar] [CrossRef]
- Shabaniyan, T.; Parsaei, H.; Aminsharifi, A.; Movahedi, M.; Torabi Jahromi, A.; Pouyesh, S.; Parvin, H. An artificial intelligence-based clinical decision support system for large kidney stone treatment. Australasian physical & engineering sciences in medicine / supported by the Australasian College of Physical Scientists in Medicine and the Australasian Association of Physical Sciences in Medicine 2019, 42, 771–779. [Google Scholar] [CrossRef]
- Yang, W.; Wang, K.; Zuo, W. Neighborhood Component Feature Selection for High-Dimensional Data. JCP 2012, 7, 161–168. [Google Scholar] [CrossRef]
- Vapnik, V.N. The Nature of Statistical Learning Theory; Springer: 1999; Volume %6, p. %&.
- Platt, J. Fast Training of Support Vector Machines Using Sequential Minimal Optimization. Advances in Kernel Methods: Support Vector Learning 1999, 185-208.
- Parsaei, H.; Jahanmiri-Nezhad, F.; Stashuk, D.; Hamilton-Wright, A. Validation of Motor Unit Potential Trains Using Motor Unit Firing Pattern Information. Conference proceedings :... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference 2009, 2009, 974–977. [Google Scholar] [CrossRef]
- Blettner, M.; Schlehofer, B.; Breckenkamp, J.; Kowall, B.; Schmiedel, S.; Reis, U.; Potthoff, P.; Schüz, J.; Berg-Beckhoff, G. Mobile phone base stations and adverse health effects: Phase 1 of a population-based, cross-sectional study in Germany. Occupational and environmental medicine 2008, 66, 118–123. [Google Scholar] [CrossRef]
- Singh, K.; Anup, N.; Yousuf, A.; Ganta, S.; Pareek, S.; Vishnani, P. Effect of electromagnetic radiations from mobile phone base stations on general health and salivary function. Journal of International Society of Preventive and Community Dentistry 2016, 6, 54. [Google Scholar] [CrossRef]
- Baliatsas, C.; van Kamp, I.; Kelfkens, G.; Schipper, M.; Bolte, J.; Yzermans, J.; Lebret, E. Non-specific physical symptoms in relation to actual and perceived proximity to mobile phone base stations and powerlines. BMC public health 2011, 11, 421. [Google Scholar] [CrossRef]
- Berg-Beckhoff, G.; Blettner, M.; Kowall, B.; Breckenkamp, J.; Schlehofer, B.; Schmiedel, S.; Bornkessel, C.; Reis, U.; Potthoff, P.; Schüz, J. Mobile phone base stations and adverse health effects: Phase 2 of a cross-sectional study with measured radio frequency electromagnetic fields. Occupational and environmental medicine 2009, 66, 124–130. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).