1. Introduction
Carotid intima media thickness (cIMT) as a surrogate of atherosclerosis on cardiovascular risk prediction and treatment evaluation has been extensively studied [
1]. Evidence suggests that cIMT modestly improves cardiovascular risk assessment in addition to traditional cardiovascular risk factors [
2], and it may be a useful indicator for monitoring cardiovascular disease (CVD) risk progress in clinical practice [
3]. Weight changes over a short time period, either loss or gain, among community-dwelling older adults are common and most of them are unintentional [
4]. Results from the Korean Longitudinal Study of Ageing suggest that a weight loss of 5 kg or more within two-years will significantly increase risk for all-cause mortality [
5]. On the other hand, obesity, defined as an excess of body fat mass, is extensively associated with many chronic diseases, in particular CVD [
6]; as its prevalence is constantly increase globally it becomes a serious public health concern [
7]. Longitudinal studies reveal that childhood body mass index (BMI) is positively related to cIMT in young or middle-aged adults [
8,
9]. Studies conducted among older adults or menopaused women also showed that high BMI is associated with elevated levels of cIMT [
10,
11].
Weight loss for people suffering from obesity is considered an effective approach of lowering CVD risk. For example, a meta-analysis conducted with small studies having examined weight loss through surgical, diet/exercise, or pharmacological interventions among obese individuals found that weight loss was associated with reduction in cIMT [
12]. However, a generous size randomized clinical trial conducted among overweight or obese adults with type 2 diabetes did not show that medical weight loss could lead to a reduction in incidence of coronary artery disease [
13]. Therefore, there are still debates on how to apply cIMT in prediction of CVD, particularly among older adults as they often have chronic conditions such as high blood pressure, glucose, and/or dyslipidemia [
2,
14,
15]. In addition, there are no studies that have examined the relationship between cIMT and weight change among the middle-age and older adults. Thus, using the first follow-up of the Canadian Longitudinal Study on Aging (CLSA), we aim to assess the relationship between weight change and atherosclerosis measured by cIMT.
2. Materials and Methods
2.1. Participants from the Canadian Longitudinal Study on Aging (CLSA)
Approximately 51,000 men and women aged 45 – 85 years across Canada (mean age 60 years) were enrolled in the baseline (2011 – 2015) of two sub-cohorts of the CLSA, i.e., Tracking and Comprehensive. Participants from the Comprehensive cohort were randomly selected from within a 25 – 50 km radius of one of the eleven Data Collection Sites (DCS) in seven Canadian Provinces and completed in-person home interviews and underwent physical assessments at a DCS. The participants from the Tracking cohort were excluded because they had no measurements on cIMT and weight for the analysis. There were 30,097 participants from the Comprehensive cohort at the baseline, 27,765 of them were followed at the first wave of the follow-up (2015 – 2018), and a total of 20,700 men and women who had complete measurements of weight and cIMT were included in this study. Detailed information of the CLSA regarding study design and data collection at baseline and first wave of follow-up can be found elsewhere [
16,
17].
2.2. Measurement of cIMT
The cIMT measurement was conducted at baseline as well as first wave follow-up at the DCS following the standard operating procedure [
18]. All participants from the Comprehensive cohort who were able to stand without the assistance of another person were eligible for the measurement. The participant was required to lie on the exam bed for at least five minutes prior to measurement. Carotid artery images were obtained using a 12-MHz linear array probe attached to a high-resolution ultrasound system (GE VIVIDi) with concurrent electrocardiogram gating at all testing sites. Average IMT, maximum IMT and minimum IMT from both right and left carotid arteries were determined during diastole. The average cIMT value is the most common measurement used in cardiovascular risk prediction studies [
3], thus, in this study we focused on the relationship between weight change and average IMT from both the right- and left- carotid artery at the first wave of follow-up. Based on whether the cIMT values were larger than 1.0 mm, which is suggestive of plaque, a sign for high-risk of atherosclerosis [
2], participants were also grouped into two categories, those with either the right or the left cIMT average > 1.0 mm, or those with cIMT ≤ 1.0 mm.
2.3. Weight change
Weight values at both the baseline and the follow-up were measured in the DCS by trained research assistants using the 140-10 Healthweight Digital Physician Scale and recorded to the nearest 0.1 kg according to the standard arthrometric operating procedure [
19]. The weight change was defined as the difference of the weight values measured at the follow-up and baseline. All participants were further categorized into four groups based on the distribution of weight change quartile cutoffs, i.e., Q1: < -2.25, Q2: -2.25 ~ 0.10, Q3: 0.10 ~ 2.35, Q4: ≥ 2.35 (kg).
2.4. Measurements of demographic variables and other cardiovascular risk factors at baseline
2.4.1. Demographic variables
Age (years), sex (male vs. female), education (bachelor’s degree or above vs. other), marital status (married or living with a partner vs. other), and birth of country (Canada vs. other).
2.4.2. Cardiovascular risk factors
a) Variables derived from the in-person home interview: current smoking (yes vs. no), alcohol (ever drinking alcohol during the past 12 months: yes vs. no), general health (good or excellent vs. other), CESD10 (Center for Epidemiological Studies Depression Scale 10 questions version, a score to detect current depressive symptomatology), and cardiovascular events (including historical heart disease, stroke, diabetes, and/or hypertension: yes vs. no).
b) Variables derived from laboratory and physical examination: total cholesterol (mol/L), high-density lipoprotein (HDL) cholesterol (mol/L), non-HDL cholesterol (mol/L), systolic blood pressure (SBP mmHg), diastolic blood pressure (DBP mmHg), body mass index (BMI kg/m2), waist circumference (cm), weight (kg) and height (m).
The demographic variables, as well as related to lifestyle and general health variables were collected through questionnaire survey conducted during in-person home interviews. Blood pressure measurements and physical examination were done in the DCS by trained research assistants. Non-fasting venipuncture blood samples were collected for lipid profiles in the DCS.
2.5. Statistical analysis
All analyses were conducted using RStudio (R version 4.2.2). Statistical significance was set at two-sided α < 0.05. Mean [SE (Standard Error)] were used to present central tendency and variability for continuous variables and percentage proportions were used for categorical variables. For the univariate analysis, one-way ANOVA (analysis of variance) was used for continuous variables and Chi-square test for categorical variables.
There were significant differences in age and sex among participants in weight change quartiles, therefore, general linear models were used to obtain the age and sex adjusted mean levels of cIMT and logistic regression was used to obtain the age and sex adjusted prevalence of cIMT > 1.0 mm at the follow-up.
Four logistic regression models were created to examine the risk association of cIMT > 1.0 mm at follow-up for weight change and weight change values in the second quartile (Q2) served as the reference group. Covariates included in the models were those statistically significant or borderline significant in the univariate analysis. Odds ratios (OR 95% confidence interval [CI]) were used as the evaluation indicator for the risk association. In model one, variables of age, sex, marital status, education, and birth country were adjusted. In model two, we further adjusted for health and lifestyle related variables, which included self-reported general health, current smoking, and alcohol intake. In model three, we further adjusted for CVD related risk factors, including SBP, HDL cholesterol, standing height and right cIMT at baseline (since more participants had right cIMT value at baseline). Finally, in model four, we further adjusted for BMI and cardiovascular events reported at baseline.
Since weight loss is an important risk factor of all-causes mortality for older people and they are also more likely to lose weight [
20], we further evaluated the risk association of cIMT > 1.0 mm with weight change by age group; participants were categorized into less than 65 years or 65 years and above. In addition, we also examined the impact of baseline BMI or reported cardiovascular events on the observed risk association. Based on the obesity criteria participants were categorized into a) normal weight BMI < 25 kg/m
2, b) overweight BMI 25 ~ 29.9 kg/m
2, and obese BMI> 30 kg/m
2. With weight change quartiles, we created 12 groups (3 x 4). In the risk association analysis, participants who were normal weight (BMI < 25 kg/m
2) and weight change in the second quartile (Q2) were served as the reference group. Based on the cardiovascular events reported at baseline (yes vs. no) and weight change quartiles, we created eight groups (2 x 4) and participants who did not have cardiovascular events reported at baseline and weight change in the second quartile (Q2) were used as the reference in the risk association analysis. All covariates included in these models were like that in model 4 with some necessary modification, e.g., variable cardiovascular events would be dropped off when analyzing its interaction effect with weight change quartiles. To ensure generalizability, the trimmed inflation weight was used for calculation means (SEs) and proportions and analytic weight was used to count the impact of sampling strategy when examining relationships between variables [
21].
3. Results
At the follow-up, participants’ weight, on average, increased 0.118 kg (Q1: -5.79 kg, Q2: -0.95 kg, Q3: 1.18 kg, Q4: 5.29 kg); if cIMT >1.0 mm was used to define the elevated risk for atherosclerosis, 16.4% of participants were fallen into this category at follow-up. Summaries of the statistics for the selected demographics and other cardiovascular risk factors by weight change quartiles were presented in
Table 1. Participants in the Q1 differed statistically from people in the other weight change quartiles (Q2 – Q4) in certain demographic and lifestyle variables including having the highest proportions of males (51.2%) and current smokers (12.3%), but the lowest proportions of married or living with a partner (72.7%), bachelor’s degree education (40.6%), self-reported good or excellent general health (89.2%), and alcohol during the past year (84.8%). The proportion of birth country was comparable with other quartiles. They had a poor cardiovascular profile, their total cholesterol mean level was comparable to other weight change quartiles, but they had the lowest mean level of HDL, highest mean levels of blood pressures, non-HDL cholesterol (though not significant), and measurements related to body compositions (i.e., BMI, waist circumference, weight, but not height), in addition, over half of them reported cardiovascular events at baseline. Interestingly, people in the Q4 of weight change group were much younger than other groups and they had a comparable CVD risk profile as those in the Q1 (
Table 1).
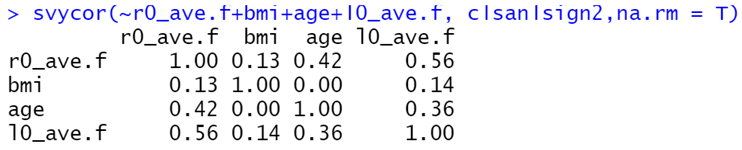
The mean levels of cIMT measured at the follow-up were comparable between people from different weight change quartiles (Q1 – Q4) for either right or left carotid arteries (
Figure 1) or age and sex as male adjusted values (
Figure 2). In general, the mean levels of the left cIMT were slightly higher than that of the right cIMT, but there was no statistical difference among weight change quartiles in either right or left cIMT mean levels. The overall prevalence of cIMT > 1.0 mm was 17.2% after adjusting for age and sex, which was a little higher than that of unadjusted (16.4%). The unadjusted prevalence rates of cIMT > 1.0 mm for people in the Q1 to Q4 were 18.7%, 16.6%, 14.1% and 15.9% respectively (
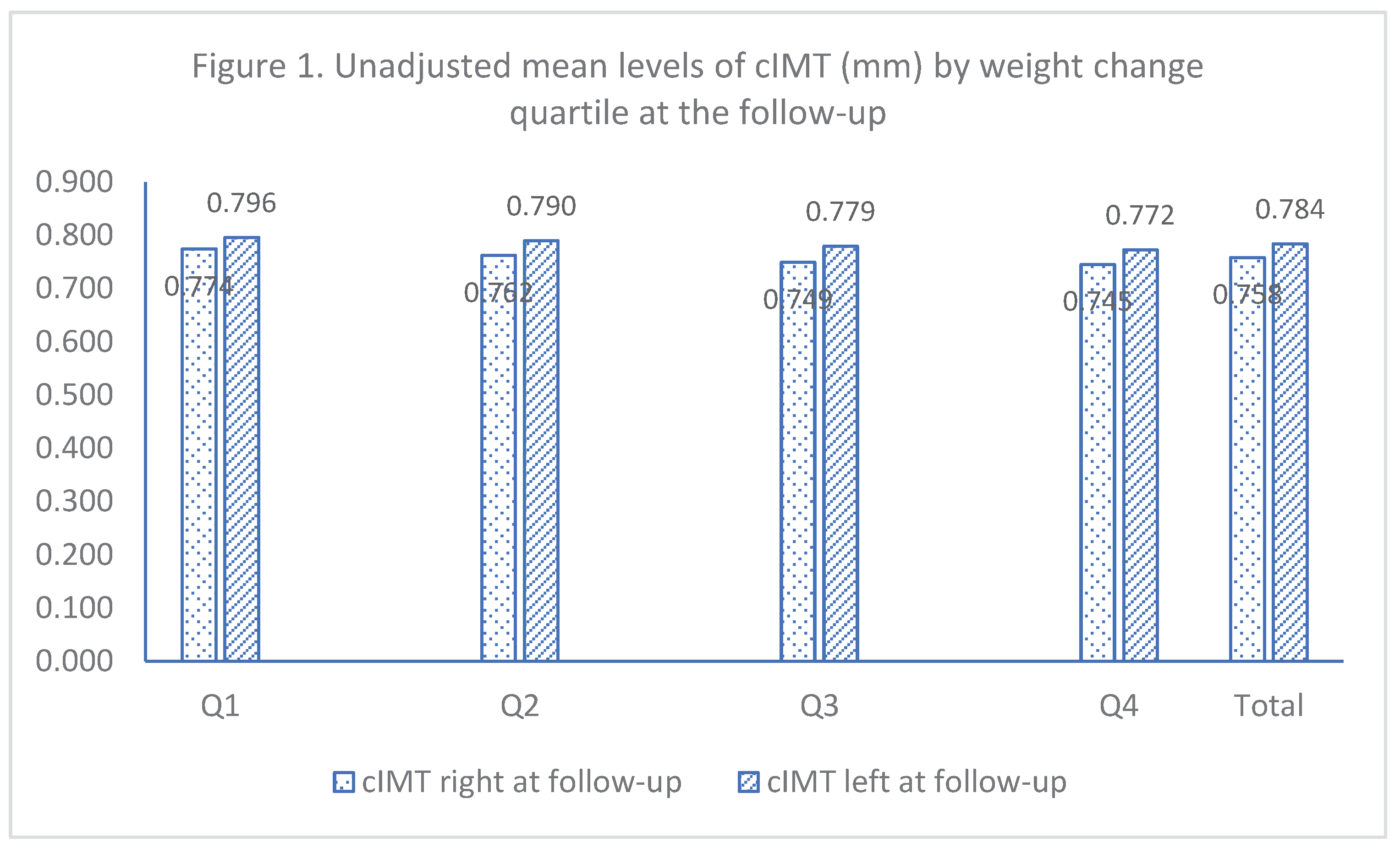
Figure 3), however, after adjusting for age and sex as male, the highest prevalence rate was found among individuals in the Q4 (19.1%), participants in the Q1 had the second highest (17.8%), and people in Q2 had the lowest adjusted prevalence (15.4%).
Table 2 shows the adjusted ORs of cIMT > 1.0 mm for weight change in quartiles at the follow-up. After adjusting for age, sex, marital status, education, and birth country (model one), the ORs (95% CIs) were 1.14 (1.01, 129), 1.09 (0.96, 1.23), and 1.29 (1.14, 1.46) for those in the Q1, Q3, and Q4, respectively. Further adjusted for variables related to general health and lifestyle (model two), variables related to cardiovascular risk factors (model three), and BMI and CVD events reported at baseline (model four), the OR (95% CI) for Q4 did not change much (1.25 [1.08, 1.45]), however, the OR for Q1 (1.00 [0.86, 1.15]) and Q3 (1.19 [1.03, 1.38]) did change.
Table 3 presented the unadjusted cIMT mean, prevalence of cIMT > 1.0 mm, and adjusted ORs (95% CIs) for weight change quartiles by age group. The overall cIMT mean in each age group were similar to what was observed, left cIMT slightly higher than right cIMT, but the mean levels for participants aged 65 or above were significantly higher than that for those aged less that 65 years, i.e., age < 65 vs. 65+, right cIMT (mm): 0.720 vs. 0.853, left cIMT (mm): 0.749 vs. 0.874. Interestingly, there was an approximately 0.13 mm difference between those aged < 65 and 65+ years in cIMT means, but the unadjusted prevalence of cIMT > 1.0 mm for people aged 65 years or above was almost three times higher than for those aged less than 65 (30.0% vs. 11.0%). Using the same covariates as in model 4 and reference group (Q2), the ORs (95% CIs) were 1.20 (0.98, 1.48), 1.36 (1.11, 1.66), and 1.41 (1.17, 1.72) for weight change quartiles, Q1, Q3 and Q4, among those aged less than 65 years, respectively, and 0.98 (0.81,1.15), 1.09 (0.91, 1.30), and 1.21 (1.00, 1.48) for weight change quartiles, Q1, Q3 and Q4, among those aged 65 years or above, respectively.
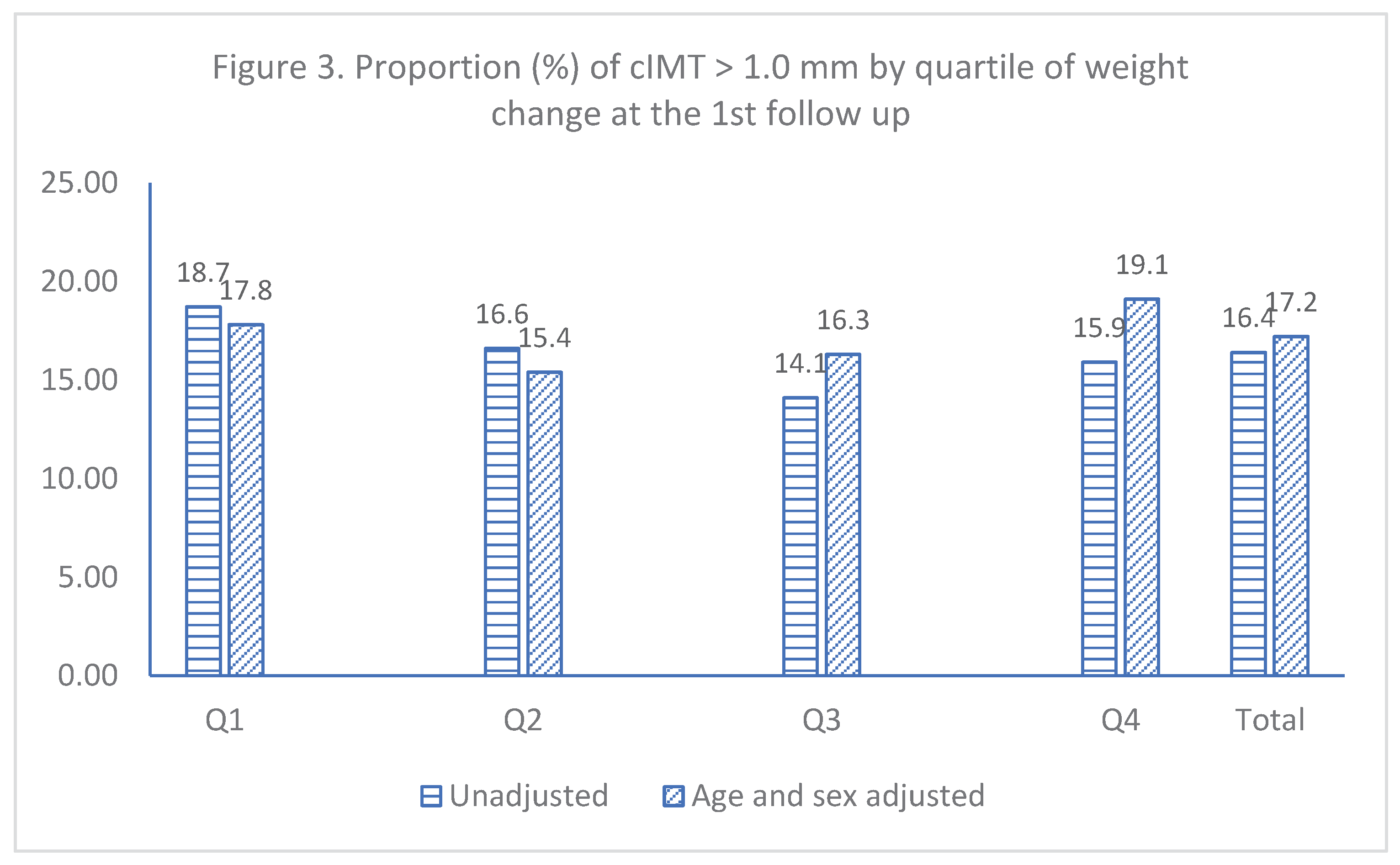
The adjusted ORs for weight change quartiles at follow-up and obesity status at baseline are shown in
Figure 4. Compared to people who were normal weight at baseline but with a moderate weight change (Q2) at follow-up, participants with normal weight at baseline but with either weight loss (Q1) or gain (Q3 and Q4) at follow-up had a similar risk association, and this was true as well for people who were overweight at baseline but with weight loss (Q1) or moderate weight change (Q2) at follow-up; while for those who were overweight at baseline but with weight gain (Q3 and Q4) at follow-up, there was over a 30% increase in OR for cIMT > 1.0 mm. While for people who were obese at baseline regardless of either weight loss (Q1), or moderate weight change (Q2), or weight gain (Q3 and Q4) at follow-up, they all had an increased OR of cIMT > 1.0 mm, i.e., 1.35 for Q1, 1.26 for Q2, 1.52 for Q3, and 1.70 for Q4, respectively, and all ORs except for those with a moderate weight change (Q2) were statistically significant (P < 0.05).
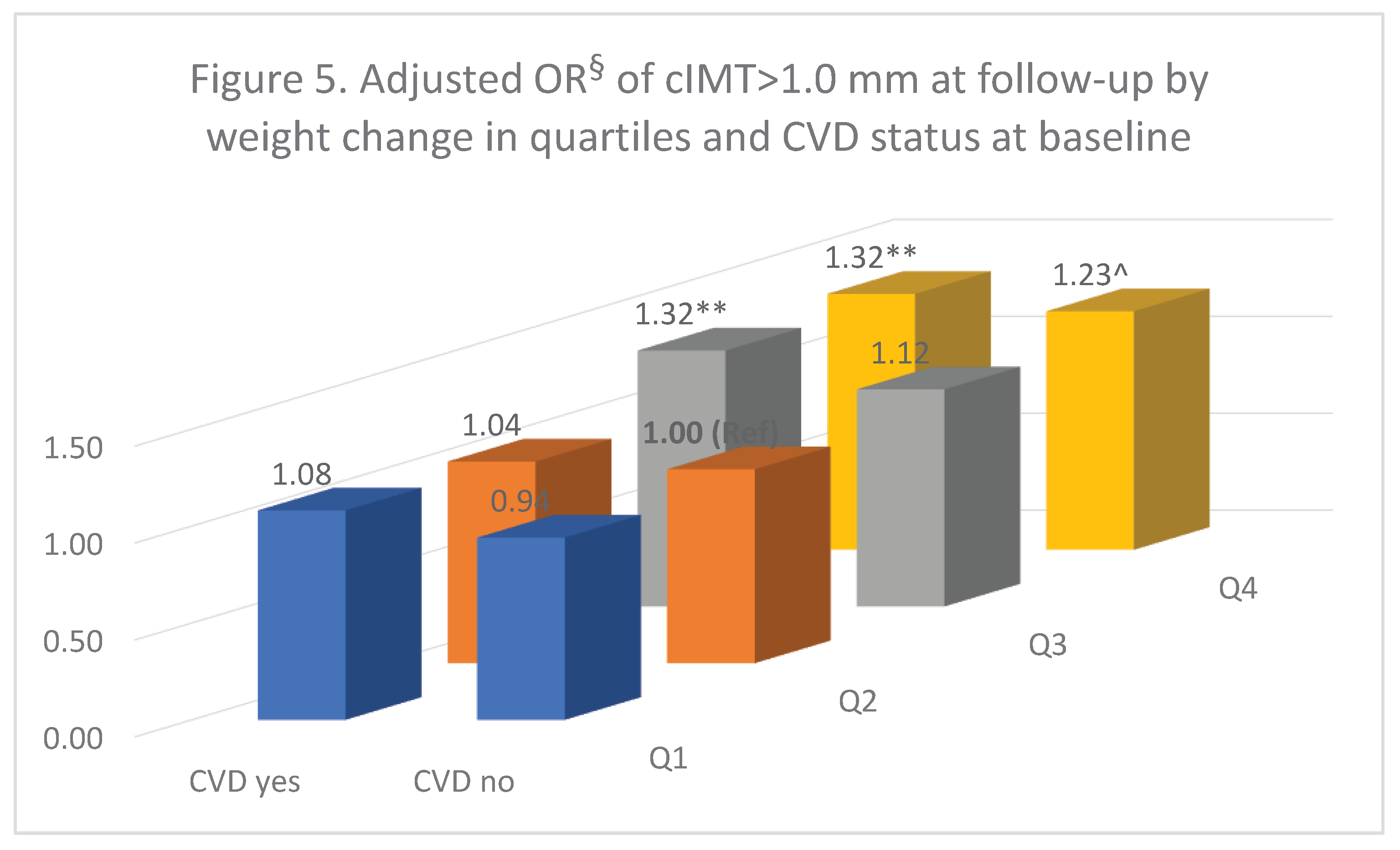
The adjusted ORs for weight change in quartiles at follow-up and reported CVD events at baseline are shown in
Figure 5. Compared to people with a moderate weight change (Q2) at follow-up but without cardiovascular events at baseline, those who were weight loss (Q1) regardless of their CVD status had a similar OR for cIMT > 1.0 mm. This similar result was also observed for participants with a moderate weight change at follow-up (Q2) but with CVD events at baseline. Compared to the reference group, people with weight gain (Q3 and Q4) all had an increased OR for cIMT > 1.0 mm, however, only for people who were with reported CVD events at baseline was statistically significant (OR = 1.32, P <0.01); while for people without cardiovascular events, the ORs were 1.12 for the Q3 and 1.23 for the Q4 but was only Q4 borderline significant (P = 0.052).
4. Discussion
Using the data of the CLSA first follow-up we examined the relationship between cIMT and weight change in middle-age and older Canadian adults. From this study we observed that people with weight loss did not improve either their mean cIMT or the odds of cIMT > 1.0 mm; moreover, those who were obese at baseline but did lose weight at follow-up had an increased risk for atherosclerosis. For those who gained weight, their cIMT mean at follow-up was comparable to those who lost weight, but they had a significant increased risk for atherosclerosis; this was more apparent among people aged less than 65 year or having CVD event at baseline.
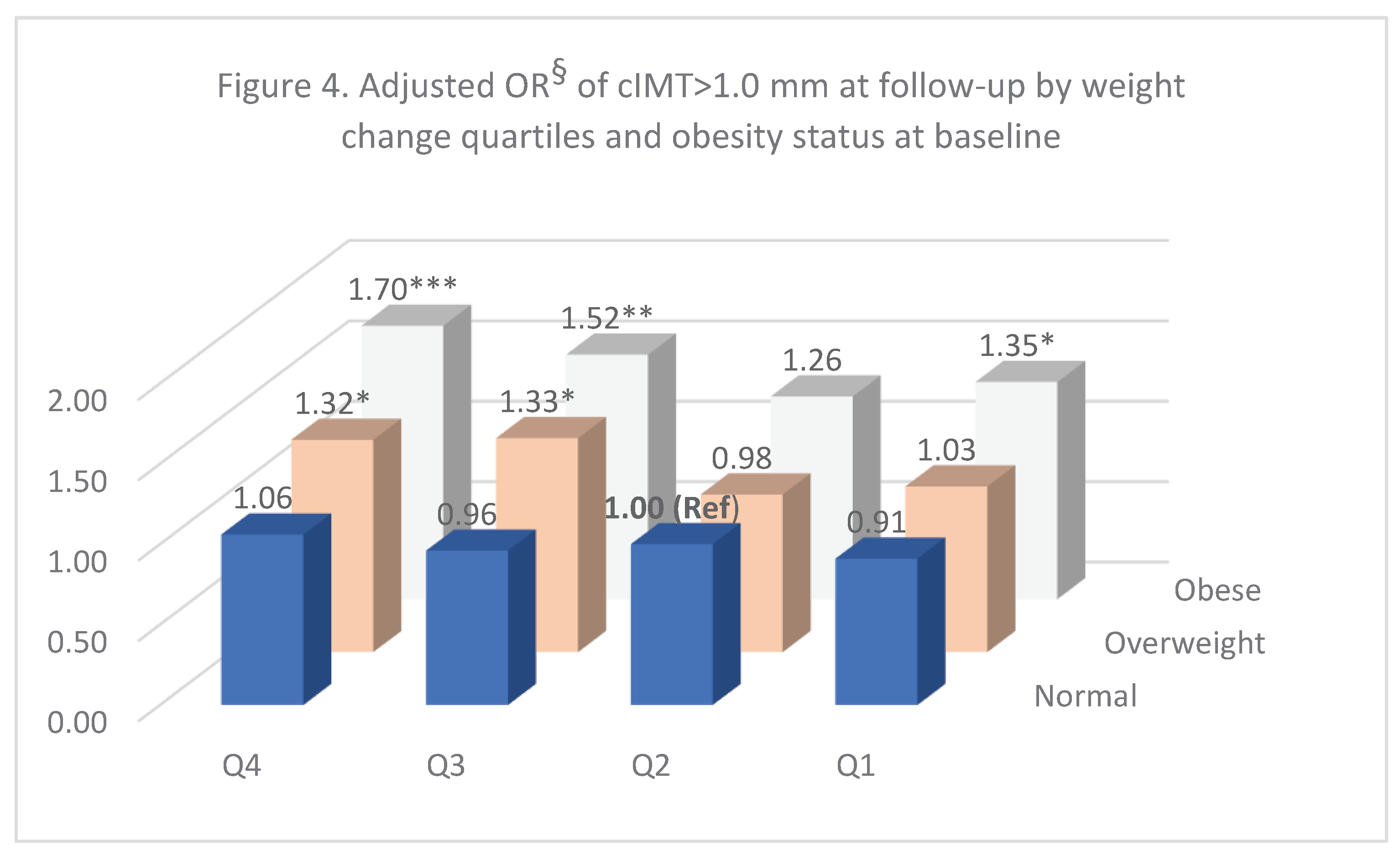
Results from previous studies indicate that cIMT values were positively associated with BMI and age [8-11,22]. In this study, we have also observed the positive correlations between cIMT levels at follow-up and BMI or age at baseline though those correlations were weak (Appendix). However, we did not observe that weight loss for obese people reduced their cIMT, which was suggested by the intervention studies in which diet, exercise, surgery, and/or pharmacologic methods were used to lower weight [
12]. There were no statistical differences in mean levels of cIMT at follow-up for people between different weight change quartiles, this suggests that weight change either gain or loss did not affect their mean cIMT. Additionally, the overall adjusted OR for those with weight loss (Q1) was similar to the reference group (Q2) indicating that the prevalence rates of cIMT > 1.0 mm were comparable. However, we observed an increased odds of cIMT > 1.0 mm for people who were obese at baseline but lost weight at follow-up. This could be due to the fact that the CLSA is an observational cohort study, making it difficult to evaluate the relationship between cIMT and weight loss since unintentional weight loss is different from intentional loss. Weight loss unintentionally is usually a sign of poor health for old people [
23,
24]. In fact, the average weight loss for those who were obese at baseline was only 5.6 kg over 36 months follow-up in this study, compared to 16 kg weight loss, on average, over 20 months for obese people from the Skilton’s meta-analysis of intervention studies [
12]. Therefore, the weight loss might be too small to influence the progress of cIMT, even if their weight loss was intentional. Furthermore, people from the intervention studies highlighted by Skilton et al [
12] were much younger compared to the participants of the CLSA (the mean age of eight of nine studies in that meta-analysis were 48 years or less vs. the average age of 60 at baseline for the CLSA). Since atherosclerosis has
a long asymptomatic phase of development and it usually begins early in life, often during childhood [
25]
, its reverse progress would be more challenging for older individuals in comparison to younger individuals.
We observed those who gained weight at follow-up had an increased risk for atherosclerosis even their cIMT mean levels were comparable between weight change quartiles. Although the prevalence rates of cIMT > 1.0 mm at follow-up were much higher in those aged 65 or above than those less than 65 years, the risk association was much stronger in people aged less than 65 years. Results from a systematic review by van den Munckhof and colleagues [
26] suggests that cIMT are linearly associated with age in the general population, but the occurrence of cardiovascular events and age is not linear, demonstrating a sudden increase in event rate after age 60 years of age [
27]. In fact, our results do not contradict to what previous studies have observed. Since atherosclerosis starts in childhood and develops with age, thus, even the entire process appears as a linear with age, but middle age (45 – 65) would be the critical stage to observe people whose atherosclerosis risk is reaching to a point of more likely to have a CVD, especially when gaining too much weight. Therefore, we may see this odd phenoxenium that overall, middle-aged adults had a lower prevalence rate of atherosclerosis (cIMT > 1.0 mm) but were with a significantly increased risk for atherosclerosis when having weight gain; while old-aged adults seemed in opposite, having a higher prevalence rate of atherosclerosis but the increased risk was not impressive when having a similar weight gain because the differences of risk for atherosclerosis were minimal among people within different weight changes. Although medical weight loss among people who are overweight or obese does not reduce the incident cardiovascular events [
13], our results indicate that weight gain was indeed a contributing factor for increasing atherosclerotic risk (cIMT > 1.0 mm), particularly for people having cardiovascular events at baseline. We did not find an interaction between sex and weight change on the risk of atherosclerosis though generally women are more likely to lose weight (results not shown).
One limitation to the current study when interpreting the results of this study is that approximately 25% of the cohort participants were excluded from the analysis due to either missing measured weight or cIMT at follow-up. Compared to participants who were included in the study, they were older, and more likely to be male and with cardiovascular events at baseline, therefore, the results of this study may not be well generalizable to the general population, particularly for people aged 65 years or above. Nevertheless, the large sample size, population-based sampling design and weighting, and adjustment of many well-known covariates would be strengths of this study.
5. Conclusions
In conclusion, weight loss observed among middle and/or older adults from this observational cohort does not demonstrate an improvement in cIMT. Nevertheless, weight gain was associated with an increased risk for atherosclerosis, particularly among middle-aged adults, people with cardiovascular events and/or who were overweight/obese at baseline. Thus, these factors are important to consider when developing efficient prevention and promotion strategies to lower CVD risk among high-risk populations.
Authors Contributions
JL and MN applied for the accessing the CLSA data, JL and NSKS conceptualized this study, JL analyzed and interpreted the data. JL, MN, and DO draft and reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partly supported by the Ontario Regional Center of the Canadian Statistical Sciences Institute (CANSSI) and the Faculty of Arts and Science at the University of Toronto for the fee of using the CLSA data.
Institutional Review Board Statement
This study was approved by the Brock University Research Ethics Board (REB#: 20-017) for analyzing the CLSA data.
Informed Consent Statement
all participants from the CLSA have been informed of the study, which abides by the requirements of the Canadian Institutes of Health Research and relevant institutes for ethical conduct and privacy protection in health research. The detailed information can be found in the CLSA website.
Data Availability Statement
the CLSA data is available for approved proposals. The detailed information can be found at Canadian Longitudinal Study on Aging | Canadian Longitudinal Study on Aging (clsa-elcv.ca)
Acknowledgments
This research was made possible using the data/biospecimens collected by the Canadian Longitudinal Study on Aging (CLSA). Funding for the CLSA is provided by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference: LSA 9447 and the Canada Foundation for Innovation. This research has been conducted using the CLSA Baseline Comprehensive Dataset CoP5 and the CLSA First Follow-up Dataset CoP3 under “Application Number 2010012.” The CLSA is led by Drs. Parminder Raina, Christina Wolfson, and Susan Kirkland.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ravani, A.; Werba, J.P.; Frigerio, B.; Sansaro, D.; Amato, M.; Tremoli, E.; Baldassarre, D. Assessment and relevance of carotid intima-media thickness (C-IMT) in primary and secondary cardiovascular prevention. Curr Pharm Des 2015, 21, 1164–1171. [Google Scholar] [CrossRef] [PubMed]
- Den Ruijter, H.M.; Peters, S.A.; Anderson, T.J.; Britton, A.R.; Dekker, J.M.; Eijkemans, M.J.; Engstrom, G.; Evans, G.W.; de Graaf, J.; Grobbee, D.E.; et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA 2012, 308, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Willeit, P.; Tschiderer, L.; Allara, E.; Reuber, K.; Seekircher, L.; Gao, L.; Liao, X.; Lonn, E.; Gerstein, H.C.; Yusuf, S.; et al. Carotid Intima-Media Thickness Progression as Surrogate Marker for Cardiovascular Risk: Meta-Analysis of 119 Clinical Trials Involving 100 667 Patients. Circulation 2020, 142, 621–642. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Kritchevsky, S.B.; Harris, T.B.; Tylavsky, F.; Rubin, S.M.; Newman, A.B. Short-term weight changes in community-dwelling older adults: the Health, Aging, and Body Composition Weight Change Substudy. Am J Clin Nutr 2005, 82, 644–650. [Google Scholar] [CrossRef]
- Suh, J.; Cho, Y.J.; Kim, H.J.; Choi, S.S. Age-Related Difference in Weight Change and All-Cause Mortality in Middle-Aged and Older Korean Populations: Korean Longitudinal Study of Aging. Korean J Fam Med 2021, 42, 297–302. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Despres, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- James, W.P.T. Obesity: A Global Public Health Challenge. Clin Chem 2018, 64, 24–29. [Google Scholar] [CrossRef]
- Charakida, M.; Khan, T.; Johnson, W.; Finer, N.; Woodside, J.; Whincup, P.H.; Sattar, N.; Kuh, D.; Hardy, R.; Deanfield, J. Lifelong patterns of BMI and cardiovascular phenotype in individuals aged 60-64 years in the 1946 British birth cohort study: an epidemiological study. Lancet Diabetes Endocrinol 2014, 2, 648–654. [Google Scholar] [CrossRef]
- Magnussen, C.G.; Venn, A.; Thomson, R.; Juonala, M.; Srinivasan, S.R.; Viikari, J.S.; Berenson, G.S.; Dwyer, T.; Raitakari, O.T. The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J Am Coll Cardiol 2009, 53, 860–869. [Google Scholar] [CrossRef]
- Gentile, M.; Iannuzzi, A.; Iannuzzo, G.; Covetti, G.; Panico, S.; Mattiello, A.; De Michele, M.; Rubba, P. Relation of body mass index with carotid intima-media thickness and diameter is independent of metabolic syndrome in postmenopausal Mediterranean women. Menopause 2012, 19, 1104–1108. [Google Scholar] [CrossRef]
- Peters, S.A.; Lind, L.; Palmer, M.K.; Grobbee, D.E.; Crouse, J.R., 3rd; O'Leary, D.H.; Evans, G.W.; Raichlen, J.; Bots, M.L.; den Ruijter, H.M.; et al. Increased age, high body mass index and low HDL-C levels are related to an echolucent carotid intima-media: the METEOR study. J Intern Med 2012, 272, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Skilton, M.R.; Yeo, S.Q.; Ne, J.Y.; Celermajer, D.S.; Caterson, I.D.; Lee, C.M. Weight loss and carotid intima-media thickness-a meta-analysis. Obesity (Silver Spring) 2017, 25, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Look, A.R.G.; Wing, R.R.; Bolin, P.; Brancati, F.L.; Bray, G.A.; Clark, J.M.; Coday, M.; Crow, R.S.; Curtis, J.M.; Egan, C.M.; et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013, 369, 145–154. [Google Scholar] [CrossRef]
- Bots, M.L.; Groenewegen, K.A.; Anderson, T.J.; Britton, A.R.; Dekker, J.M.; Engstrom, G.; Evans, G.W.; de Graaf, J.; Grobbee, D.E.; Hedblad, B.; et al. Common carotid intima-media thickness measurements do not improve cardiovascular risk prediction in individuals with elevated blood pressure: the USE-IMT collaboration. Hypertension 2014, 63, 1173–1181. [Google Scholar] [CrossRef]
- Gardin, J.M.; Bartz, T.M.; Polak, J.F.; O'Leary, D.H.; Wong, N.D. What do carotid intima-media thickness and plaque add to the prediction of stroke and cardiovascular disease risk in older adults? The cardiovascular health study. J Am Soc Echocardiogr 2014, 27, 998–1005. [Google Scholar] [CrossRef]
- Raina, P.S.; Wolfson, C.; Kirkland, S.A.; Griffith, L.E.; Oremus, M.; Patterson, C.; Tuokko, H.; Penning, M.; Balion, C.M.; Hogan, D.; et al. The Canadian longitudinal study on aging (CLSA). Can J Aging 2009, 28, 221–229. [Google Scholar] [CrossRef]
- Raina, P.; Wolfson, C.; Kirkland, S.; Griffith, L.E.; Balion, C.; Cossette, B.; Dionne, I.; Hofer, S.; Hogan, D.; van den Heuvel, E.R.; et al. Cohort Profile: The Canadian Longitudinal Study on Aging (CLSA). Int J Epidemiol 2019, 48, 1752–1753j. [Google Scholar] [CrossRef]
- CLSA, Canadian Longitudinal Study on Aging: SOP_DCS_0011 Carotid Intima Media Thickness. 2015, CLSA. 27 July.
- CLSA, Canadian Longitudinal Study on Aging: SOP_DCS_0006 Standing Height and Weight Measurement. 2016, CLSA. 18 April.
- Yano, T.; Godai, K.; Kabayama, M.; Akasaka, H.; Takeya, Y.; Yamamoto, K.; Yasumoto, S.; Masui, Y.; Arai, Y.; Ikebe, K.; et al. Factors associated with weight loss by age among community-dwelling older people. BMC Geriatr 2023, 23, 277. [Google Scholar] [CrossRef]
- CLSA, CLSA Technical Document (version 1.2) Sampling and Computation of Response Rates and Sample Weights for the Tracking (Telephone Interview) Participants and Comprehensive Participants. 2020, CLSA.
- Asaleye, A.A.; Braimoh, K.T.; Oyinloye, O.I.; Asaleye, C.M.; Omisore, A.D. Variation of Carotid Intima Media Thickness With Body Mass Index in Healthy Adults of Black African Descent. J Ultrasound Med 2019, 38, 123–130. [Google Scholar] [CrossRef]
- Bosch, X.; Monclus, E.; Escoda, O.; Guerra-Garcia, M.; Moreno, P.; Guasch, N.; Lopez-Soto, A. Unintentional weight loss: Clinical characteristics and outcomes in a prospective cohort of 2677 patients. PLoS One 2017, 12, e0175125. [Google Scholar] [CrossRef]
- Nicholson, B.D.; Hamilton, W.; O'Sullivan, J.; Aveyard, P.; Hobbs, F.R. Weight loss as a predictor of cancer in primary care: a systematic review and meta-analysis. Br J Gen Pract 2018, 68, e311–e322. [Google Scholar] [CrossRef] [PubMed]
- McGill, H.C., Jr.; McMahan, C.A.; Herderick, E.E.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr 2000, 72, 1307S–1315S. [Google Scholar] [CrossRef] [PubMed]
- van den Munckhof, I.C.L.; Jones, H.; Hopman, M.T.E.; de Graaf, J.; Nyakayiru, J.; van Dijk, B.; Eijsvogels, T.M.H.; Thijssen, D.H.J. Relation between age and carotid artery intima-medial thickness: a systematic review. Clin Cardiol 2018, 41, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J Cardiovasc Dev Dis 2019, 6. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Unadjusted mean levels of cIMT (mm) by weight change quartile at the follow-up.
Figure 1.
Unadjusted mean levels of cIMT (mm) by weight change quartile at the follow-up.
Figure 2.
Age and sex adjusted mean levels of cIMT (mm) by quartile of weight change at the follow-up.
Figure 2.
Age and sex adjusted mean levels of cIMT (mm) by quartile of weight change at the follow-up.
Figure 3.
Proportion (%) of cIMT > 1.0 mm by quartile of weight change at the 1st follow up.
Figure 3.
Proportion (%) of cIMT > 1.0 mm by quartile of weight change at the 1st follow up.
Figure 4.
Adjusted OR§ of cIMT>1.0 mm at follow-up by weight change quartiles and obesity status at baseline. § adjusted for age, sex, marriage, education, birth country, general health, current smoking, alcohol drinking, SBP, HDL-c, CVD status, right side cIMT, and height measured at the baseline.
Figure 4.
Adjusted OR§ of cIMT>1.0 mm at follow-up by weight change quartiles and obesity status at baseline. § adjusted for age, sex, marriage, education, birth country, general health, current smoking, alcohol drinking, SBP, HDL-c, CVD status, right side cIMT, and height measured at the baseline.
Figure 5.
Adjusted OR§ of cIMT>1.0 mm at follow-up by weight change in quartiles and CVD status at baseline. ** p<0.01, ^ p=0.052. § adjusted for age, sex, marriage, education, birth country, general health, current smoking, alcohol drinking, SBP, HDL-c, height, right side cIMT, and BMI measured at the baseline.
Figure 5.
Adjusted OR§ of cIMT>1.0 mm at follow-up by weight change in quartiles and CVD status at baseline. ** p<0.01, ^ p=0.052. § adjusted for age, sex, marriage, education, birth country, general health, current smoking, alcohol drinking, SBP, HDL-c, height, right side cIMT, and BMI measured at the baseline.
Table 1.
Baseline selected characteristics by weight change quartiles in the first follow-up of CLSA.
Table 1.
Baseline selected characteristics by weight change quartiles in the first follow-up of CLSA.
| |
|
Weight change quartiles (kg) |
|
|
| |
< -2.25 |
~0.10 |
~2.35 |
>=2.35 |
P-value |
| n |
4967 |
5336 |
5263 |
5134 |
|
| Age (yrs. mean [SE]) |
60.9 (0.3) |
61.0 (0.3) |
59.0 (0.3) |
56.6 (0.2) |
*** |
| Male (%) |
51.2 |
46.1 |
46.5 |
48.4 |
^ |
| Married (%) |
72.7 |
75.4 |
79.4 |
75.6 |
*** |
| Birth of country as Canada (%) |
82.0 |
78.2 |
80.4 |
83.7 |
** |
| Bachelor’s degree received (%) |
40.6 |
44.3 |
45.5 |
41.6 |
*** |
| General health^ (%) |
89.2 |
92.0 |
93.5 |
90.6 |
*** |
| Current smoking (%) |
12.3 |
8.2 |
8.8 |
12.1 |
*** |
| Alcohol (%) |
84.8 |
87.9 |
87.7 |
86.9 |
*** |
| CESD10^ (mean [SE]) |
5.83 (0.14) |
5.21 (0.14) |
5.12 (0.14) |
5.67 (0.12) |
ns |
| Total cholesterol (mol/L, mean [SE]) |
5.16 (0.03) |
5.22 (0.03) |
5.23 (0.03) |
5.16 (0.03) |
ns |
| HDL cholesterol (mol/L, mean [SE]) |
1.42 (0.01) |
1.52 (0.01) |
1.52 (0.01) |
1.46 (0.01) |
*** |
| non-HDL cholesterol (mol/L, mean [SE]) |
3.74 (0.03) |
3.70 (0.03) |
3.71 (0.03) |
3.70 (0.03) |
ns |
| SBP (mmHg, mean [SE]) |
122.9 (0.6) |
120.1 (0.4) |
118.3 (0.4) |
118.9 (0.4) |
*** |
| DBP (mmHg, mean [SE]) |
75.9 (0.3) |
74.5 (0.3) |
74.3 (0.2) |
75.5 (0.3) |
* |
| BMI (kg/m2, mean [SE]) |
29.7 (0.2) |
27.1 (0.1) |
26.9 (0.1) |
28.6 (0.2) |
*** |
| Waist circumference (cm, mean [SE]) |
98.7 (0.5) |
91.3 (0.4) |
90.7 (0.4) |
94.7 (0.5) |
*** |
| Height (m, mean [SE]) |
1.691 (0.003) |
1.675 (0.003) |
1.680 (0.003) |
1.693 (0.003) |
* |
| Weight (kg, mean [SE]) |
85.1 (0.6) |
76.2 (0.4) |
76.2 (0.4) |
82.2 (0.5) |
*** |
| Weight change at the 1st follow-up (kg, mean [SE]) |
-5.79 (0.12) |
-0.95 (0.02) |
1.18 (0.02) |
5.29 (0.09) |
*** |
| Cardiovascular diseases (%) |
50.7 |
40.6 |
38.4 |
42.2 |
*** |
Table 2.
Adjusted ORs of cIMT > 1.0 mm for weight change quartiles at the 1st follow-up, CLSA.
Table 2.
Adjusted ORs of cIMT > 1.0 mm for weight change quartiles at the 1st follow-up, CLSA.
| |
|
|
Weight change at the first follow-up |
|
|
|
| |
|
Q1 |
|
Q2 (Ref) |
Q3 |
|
Q4 |
|
| |
|
OR |
95% CI |
OR |
OR |
95% CI |
OR |
95% CI |
| Model one |
n = 17,828 |
1.14 |
(1.01, 129) |
1.00 |
1.09 |
(0.96, 1.23) |
1.29 |
(1.14, 1.46) |
| |
|
|
|
|
|
|
|
|
| Model two |
n = 17,458 |
1.12 |
(0.98, 1.27) |
1.00 |
1.09 |
(0.96, 1.23) |
1.28 |
(1.13, 1.46) |
| |
|
|
|
|
|
|
|
|
| Model three |
n = 13,731 |
1.07 |
(0.92, 1.23) |
1.00 |
1.19 |
(1.03, 1.37) |
1.31 |
(1.13, 1.51) |
| |
|
|
|
|
|
|
|
|
| Model four |
n = 13,715 |
1.00 |
(0.86, 1.15) |
1.00 |
1.19 |
(1.03, 1.38) |
1.25 |
(1.08, 1.45) |
| |
|
|
|
|
|
|
|
|
| cIMT: carotid intima media thickness |
|
|
|
|
| Model one: adjusted for age, sex, marriage, education, and country of birth |
|
|
|
|
| Model two: further adjusted for general health, current smoking, and alcohol drinking |
|
|
|
| Model three: further adjusted for systolic blood pressure, HDL cholesterol, right side cIMT, and height measured at the baseline. |
| Model four: further adjusted for BMI and CVD status at baseline. |
|
|
|
Table 3.
Statistics^ of cIMT for weight change quartiles at follow-up by age group, CLSA.
Table 3.
Statistics^ of cIMT for weight change quartiles at follow-up by age group, CLSA.
| |
Weight change quartile at the follow-up |
| |
Q1 |
Q2 (Ref) |
Q3 |
Q4 |
Total |
| Age |
| < 65 years (n = 8,718) |
| Right cIMT (mm, mean [SE]) |
0.729 (0.005) |
0.716 (0.005) |
0.715 (0.005) |
0.718 (0.005) |
0.720 (0.005) |
| Left cIMT (mm, mean [SE]) |
0.751 (0.005) |
0.746 (0.006) |
0.744 (0.005) |
0.749 (0.005) |
0.749 (0.005) |
| cIMT > 1.0 mm (%) |
11.6 |
9.6 |
9.3 |
12.3 |
11.0 |
| OR^ (95% CI) |
1.20 (0.98, 1.48) |
1.00 |
1.36 (1.11,1.66) |
1.41 (1.17, 1.72) |
|
| 65 + years (n = 4,977) |
| Right cIMT (mm, mean [SE]) |
0.867 (0.008) |
0.849 (0.007) |
0.838 (0.007) |
0.861 (0.010) |
0.853 (0.008) |
| Left cIMT (mm, mean [SE]) |
0.886 (0.007) |
0.872 (0.008) |
0.868 (0.007) |
0.870 (0.010) |
0.874 (0.008) |
| cIMT > 1.0 mm (%) |
32.9 |
29.7 |
26.7 |
30.9 |
30.0 |
| OR (95% CI) |
0.98 (0.81, 1.15) |
1.00 |
1.09 (0.91, 1.30) |
1.21 (1.00, 1.48) |
|
| cIMT: carotid intima media thickness |
| ^ mean (SE): raw mean (standard error) |
| %: unadjusted prevalence |
| OR (95% CI): adjusted odds ratio (95% confidence interval) from the same as the model 4 in Table 2. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).