Submitted:
18 September 2023
Posted:
20 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
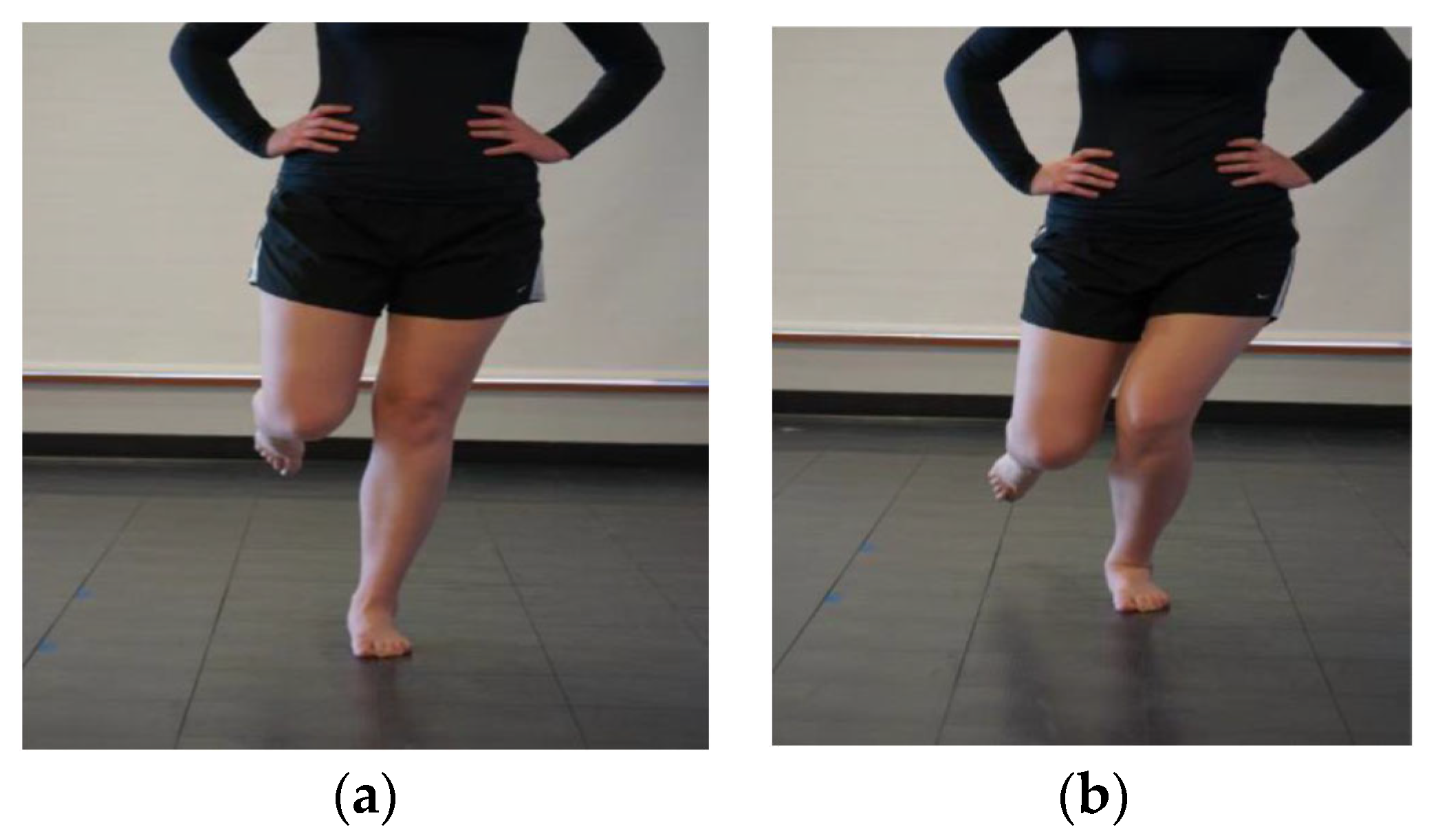
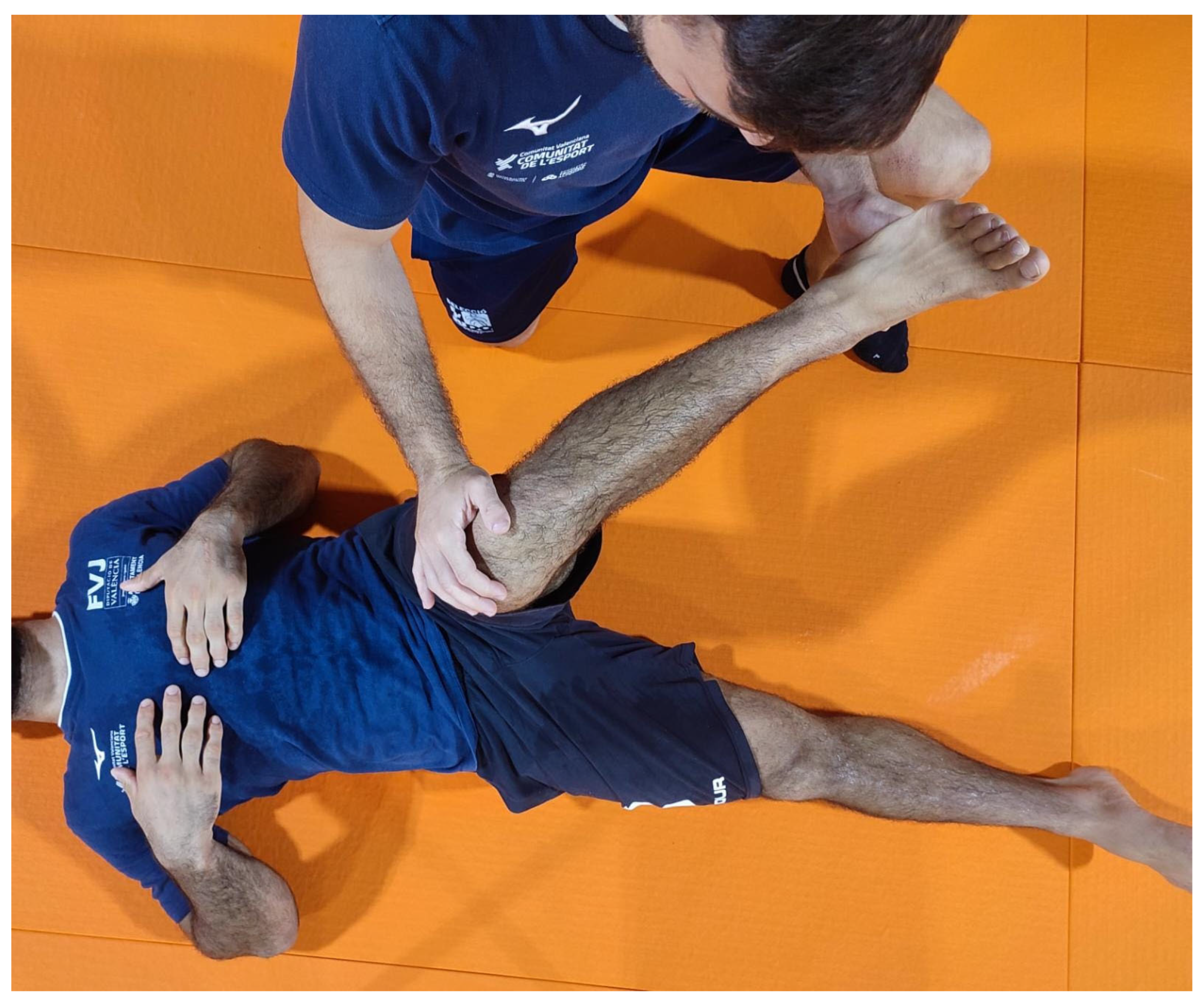
2.3. Clinical Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pocecco, E.; Ruedl, G.; Stankovic, N.; Sterkowicz, S.; Del Vecchio, F.B.; Gutiérrez-García, C.; Rousseau, R.; Wolf, M.; Kopp, M.; Miarka, B.; et al. Injuries in judo: a systematic literature review including suggestions for prevention. Br. J. Sports Med. 2013, 47, 1139–1143. [Google Scholar] [CrossRef] [PubMed]
- Akoto, R.; Lambert, C.; Balke, M.; Bouillon, B.; Frosch, K.-H.; Höher, J. Epidemiology of injuries in judo: a cross-sectional survey of severe injuries based on time loss and reduction in sporting level. Br. J. Sports Med. 2017, 52, 1109–1115. [Google Scholar] [CrossRef]
- von Gerhardt, A.L.; Vriend, I.; Verhagen, E.; Tol, J.L.; Kerkhoffs, G.M.M.J.; Reurink, G. Systematic development of an injury prevention programme for judo athletes: the IPPON intervention. BMJ Open Sport Exerc. Med. 2020, 6, e000791. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Romero EA, Lim T, Alonso Pérez JL, Castaldo M, Martínez Lozano P, Villafañe JH. Identifying Clinical and MRI Characteristics Associated with Quality of Life in Patients with Anterior Cruciate Ligament Injury: Prognostic Factors for Long-Term. Int J Environ Res Public Health. 2021 Dec 6;18(23):12845. [CrossRef]
- Koshida, S.; Deguchi, T.; Miyashita, K.; Iwai, K.; Urabe, Y. The common mechanisms of anterior cruciate ligament injuries in judo: a retrospective analysis. Br. J. Sports Med. 2008, 44, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Larwa, J.; Stoy, C.; Chafetz, R.S.; Boniello, M.; Franklin, C. Stiff Landings, Core Stability, and Dynamic Knee Valgus: A Systematic Review on Documented Anterior Cruciate Ligament Ruptures in Male and Female Athletes. Int. J. Environ. Res. Public Heal. 2021, 18, 3826. [Google Scholar] [CrossRef]
- Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: Cut risk with three sharpened and validated tools: ACL INJURY PREVENTION. J Orthop Res. noviembre de 2016;34(11):1843-55. [CrossRef]
- Mehl, J.; Diermeier, T.; Herbst, E.; Imhoff, A.B.; Stoffels, T.; Zantop, T.; Petersen, W.; Achtnich, A. Evidence-based concepts for prevention of knee and ACL injuries. 2017 guidelines of the ligament committee of the German Knee Society (DKG). Arch. Orthop. Trauma Surg. 2017, 138, 51–61. [Google Scholar] [CrossRef]
- Wilczyński, B.; Zorena, K.; Ślęzak, D. Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review. Int. J. Environ. Res. Public Heal. 2020, 17, 8208. [Google Scholar] [CrossRef]
- Jeong, J.; Choi, D.-H.; Shin, C.S. Core Strength Training Can Alter Neuromuscular and Biomechanical Risk Factors for Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2020, 49, 183–192. [Google Scholar] [CrossRef]
- LaBella, C.R.; Hennrikus, W.; Hewett, T.E.; Brenner, J.S.; Brookes, M.A.; Demorest, R.A.; Halstead, M.E.; Kelly, A.K.W.; Koutures, C.G.; LaBotz, M.; et al. Anterior Cruciate Ligament Injuries: Diagnosis, Treatment, and Prevention. PEDIATRICS 2014, 133, e1437–e1450. [Google Scholar] [CrossRef]
- Hewett TE, Ford KR, Hoogenboom BJ, Myer GD. UNDERSTANDING AND PREVENTING ACL INJURIES: CURRENT BIOMECHANICAL AND EPIDEMIOLOGIC CONSIDERATIONS - UPDATE 2010. :18.
- Hewett, T.E.; Ford, K.R.; Xu, Y.Y.; Khoury, J.; Myer, G.D. Utilization of ACL Injury Biomechanical and Neuromuscular Risk Profile Analysis to Determine the Effectiveness of Neuromuscular Training. Am. J. Sports Med. 2016, 44, 3146–3151. [Google Scholar] [CrossRef]
- Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The Effects of Core Proprioception on Knee Injury: A Prospective Biomechanical-Epidemiological Study. Am J Sports Med. marzo de 2007;35(3):368-73. [CrossRef]
- Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in Neuromuscular Control of the Trunk Predict Knee Injury Risk: Prospective Biomechanical-Epidemiologic Study. Am J Sports Med. julio de 2007;35(7):1123-30. [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; Van Den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Wahlstedt, C.; Rasmussen-Barr, E. Anterior cruciate ligament injury and ankle dorsiflexion. Knee Surgery, Sports Traumatol. Arthrosc. 2014, 23, 3202–3207. [Google Scholar] [CrossRef]
- Hewett, T.E.; Lindenfeld, T.N.; Riccobene, J.V.; Noyes, F.R. The Effect of Neuromuscular Training on the Incidence of Knee Injury in Female Athletes. Am. J. Sports Med. 1999, 27, 699–706. [Google Scholar] [CrossRef]
- Sasaki, S.; Tsuda, E.; Yamamoto, Y.; Maeda, S.; Kimura, Y.; Fujita, Y.; Ishibashi, Y. Core-Muscle Training and Neuromuscular Control of the Lower Limb and Trunk. J. Athl. Train. 2019, 54, 959–969. [Google Scholar] [CrossRef]
- Dargo, L.; Robinson, K.J.; Games, K.E.; Dargo Lucas Dargo, MS, ATC; Kelsey J. Robinson, MS, AT, ATC; Kenneth E. Games, PhD, LAT, ATCDepartment of Applied Medicine and Rehabilitation, Indiana State University, Terre Haute; Atc; At, A.; Lat, A. Prevention of Knee and Anterior Cruciate Ligament Injuries Through the Use of Neuromuscular and Proprioceptive Training: An Evidence-Based Review. J. Athl. Train. 2017, 52, 1171–1172. [Google Scholar] [CrossRef] [PubMed]
- Gomes, J.L.E.; de Castro, J.V.; Becker, R. Decreased Hip Range of Motion and Noncontact Injuries of the Anterior Cruciate Ligament. Arthrosc. J. Arthrosc. Relat. Surg. 2008, 24, 1034–1037. [Google Scholar] [CrossRef]
- VandenBerg, C.; Crawford, E.A.; Enselman, E.S.; Robbins, C.B.; Wojtys, E.M.; Bedi, A. Restricted Hip Rotation Is Correlated With an Increased Risk for Anterior Cruciate Ligament Injury. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 33, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Powden, C.J.; Hoch, J.M.; Hoch, M.C. Reliability and minimal detectable change of the weight-bearing lunge test: A systematic review. Man. Ther. 2015, 20, 524–532. [Google Scholar] [CrossRef] [PubMed]
- von Gerhardt, A.L.; Reurink, G.; Kerkhoffs, G.M.M.J.; Verhagen, E.; Krabben, K.; Mooren, J.; I Gal, J.S.; Brons, A.; Joorse, R.; Broek, B.v.D.; et al. Effectiveness of a judo-specific injury prevention programme: a randomised controlled trial in recreational judo athletes. Br. J. Sports Med. 2023, 57, 450–456. [Google Scholar] [CrossRef]
- Della Villa, F.; Buckthorpe, M.; Grassi, A.; Nabiuzzi, A.; Tosarelli, F.; Zaffagnini, S.; Della Villa, S. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br. J. Sports Med. 2020, 54, 1423–1432. [Google Scholar] [CrossRef] [PubMed]
- Zeller, B.L.; McCrory, J.L.; Ben Kibler, W.; Uhl, T.L. Differences in Kinematics and Electromyographic Activity between Men and Women during the Single-Legged Squat. Am. J. Sports Med. 2003, 31, 449–456. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 11, 260–265. [Google Scholar] [CrossRef]
- Baldazzi A, Molinaro L, Taborri J, Margheritini F, Rossi S, Bergamini E (2022) Reliability of wearable sensors-based parameters for the assessment of knee stability. PLoS ONE 17(9): e0274817. [CrossRef]
- Ugalde, V.; Brockman, C.; Bailowitz, Z.; Pollard, C.D. Single Leg Squat Test and Its Relationship to Dynamic Knee Valgus and Injury Risk Screening. PM&R 2014, 7, 229–235. [Google Scholar] [CrossRef]
- Ressman J, Grooten WJA, Rasmussen-Barr E. Visual assessment of movement quality: a study on intra- and interrater reliability of a multi-segmental single leg squat test. BMC Sports Sci Med Rehabil. 2021 Jun 8;13(1):66. [CrossRef]
- Simondson, D.; Brock, K.; Cotton, S. Reliability and smallest real difference of the ankle lunge test post ankle fracture. Man. Ther. 2012, 17, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Ganderton, C.; Tirosh, O.; Adams, R.; Ei-Ansary, D.; Han, J. Test-retest reliability of ankle range of motion, proprioception, and balance for symptom and gender effects in individuals with chronic ankle instability. Musculoskelet. Sci. Pr. 2023, 66, 102809. [Google Scholar] [CrossRef]
- von Gerhardt, A.L.; Reurink, G.; Kerkhoffs, G.M.M.J.; Verhagen, E.; Krabben, K.; Mooren, J.; I Gal, J.S.; Brons, A.; Joorse, R.; Broek, B.v.D.; et al. Effectiveness of a judo-specific injury prevention programme: a randomised controlled trial in recreational judo athletes. Br. J. Sports Med. 2023, 57, 450–456. [Google Scholar] [CrossRef]
- et al. encontraron que el tipo de lesión, el Lambert C, Guenther D, Schütz LM, Kern N, Ritzmann R, Reinert N, Walz M, Wafaisade A, Nagy K, Reuter S. Psychological readiness is related to return to sport in judo injuries: a cross-sectional study. BMC Sports Sci Med Rehabil. 2023 Feb 16;15(1):20. [CrossRef]
- Nakano N, Bartlett J, Khanduja V. Is restricted hip movement a risk factor for anterior cruciate ligament injury? J Orthop Surg (Hong Kong). 1 de septiembre de 2018;26(3):230949901879952. [CrossRef]
- Pappas, E.; Shiyko, M.P.; Ford, K.R.; Myer, G.D.; Hewett, T.E. Biomechanical Deficit Profiles Associated with ACL Injury Risk in Female Athletes. Med. Sci. Sports Exerc. 2016, 48, 107–113. [Google Scholar] [CrossRef]
- Prill, R.; Michel, S.; Schulz, R.; Coriolano, H.-J.A. Body Composition and Strength Parameters in Elite Judo Athletes 5 Years after Anterior Cruciate Ligament Reconstruction. Int. J. Sports Med. 2018, 40, 38–42. [Google Scholar] [CrossRef]
- Martin, R.L.; Enseki, K.R.; Draovitch, P.; Trapuzzano, T.; Philippon, M.J. Acetabular Labral Tears of the Hip: Examination and Diagnostic Challenges. J. Orthop. Sports Phys. Ther. 2006, 36, 503–515. [Google Scholar] [CrossRef] [PubMed]
- Henriques, I.A.D.; Lattari, E.; Torres, G.; Rodrigues, G.M.; Oliveira, B.R.R.; Neto, G.A.M.; Neto, S.R.M.; Machado, S. Can transcranial direct current stimulation improve range of motion and modulate pain perception in healthy individuals? Neurosci. Lett. 2019, 707, 134311. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, T.; Aramaki, Y. Cathodal transcranial direct current stimulation over the Cz increases joint flexibility. Neurosci. Res. 2017, 114, 55–61. [Google Scholar] [CrossRef] [PubMed]








| n. | 23 | |
| Gender, n(%) | Female | 9 (39.1) |
| Male | 14 (60.9) | |
| Dominant leg, n(%) | Left | 7 (30.4) |
| Right | 16 (69.6) | |
| SLS dominant leg, n(%) | Arms | 2 (8.7) |
| Nothing | 12 (52.2) | |
| Pelvis | 1 (4.3) | |
| Valgus | 6 (26.1) | |
| Valgus and arms | 1 (4.3) | |
| Valgus, arms and pelvis | 1 (4.3) | |
| SLS non-dominant leg, n(%) | Arms | 5 (21.7) |
| Arms and pelvis | 2 (8.7) | |
| Nothing | 10 (43.5) | |
| Pelvis and valgus | 2 (8.7) | |
| Valgus | 2 (8.7) | |
| Valgus and arms | 1 (4.3) | |
| Valgus and pelvis | 1 (4.3) | |
| Lunge test dominant leg | 13.04±3.47 | |
| Lunge test non-dominant leg | 13.17±3.02 | |
| External rotation dominant leg (º) | 90.52±8.70 | |
| Internal rotation dominant leg (º) | 54.35±12.32 | |
| External rotation non-dominant leg (º) | 87.91±10.25 | |
| Internal rotation non-dominant leg (º) | 52.91±11.72 | |
| Data expressed as mean±standard deviation or with absolute and relative values (%); SLS: Single Leg Squat test. |
| Female | Male | Levene test p valuea | ap value | Average difference (95%CI) | Effect size (95%CI) | ||
|---|---|---|---|---|---|---|---|
| n | 9 | 14 | NA | NA | |||
| SLS dominant leg, n(%) | Arms | 0 (0.0) | 2 (14.3) | NA | 0.486 | 0.44 (0.466, 1)✣ | |
| Nothing | 5 (55.6) | 7 (50.0) | NA | NA | |||
| Pelvis | 0 (0.0) | 1 (7.1) | NA | NA | |||
| Valgus | 3 (33.3) | 3 (21.4) | NA | NA | |||
| Valgus and arms | 0 (0.0) | 1 (7.1) | NA | NA | |||
| Valgus, arms and pelvis | 1 (11.1) | 0 (0.0) | NA | NA | |||
| SLS non-dominant leg, n(%) | Arms | 2 (22.2) | 3 (21.4) | NA | 0.719 | 0.4 (0.511, 1)✣ | |
| Arms and pelvis | 1 (11.1) | 1 (7.1) | NA | NA | |||
| Nothing | 4 (44.4) | 6 (42.9) | NA | NA | |||
| Pelvis and valgus | 0 (0.0) | 2 (14.3) | NA | NA | |||
| Valgus | 1 (11.1) | 1 (7.1) | NA | NA | |||
| Valgus and arms | 0 (0.0) | 1 (7.1) | NA | NA | |||
| Valgus and pelvis | 1 (11.1) | 0 (0.0) | NA | NA | |||
| Lunge test dominant leg | 12.11±2.98 | 13.64±3.73 | 0.354 | 0.313 | -1.532 (-4.468, 1.405) | -0.442 (-1.341, 0.457)* | |
| Lunge test non-dominant leg | 12.33±2.65 | 13.71±3.22 | 0.451 | 0.296 | -1.381 (-3.955, 1.193) | -0.458 (-1.358, 0.441)* | |
| External rotation dominant leg (º) | 93.11±8.88 | 88.86±8.47 | 0.698 | 0.262 | 4.254 (-3.624, 12.132) | 0.493 (-0.408, 1.394)* | |
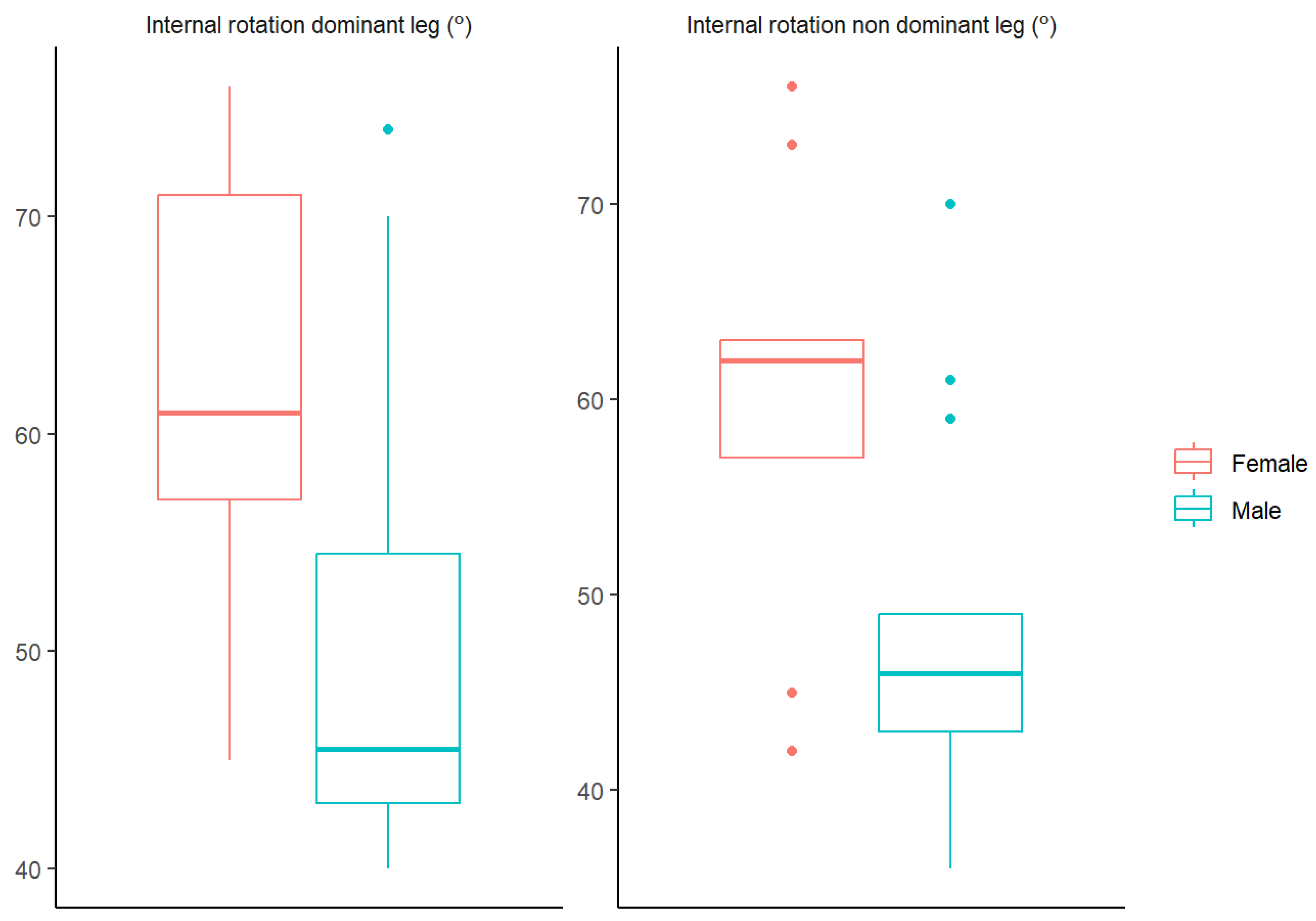
| Internal rotation dominant leg (º) | 61.89±10.69 | 49.50±11.04 | 0.884 | 0.01 | 12.389 (2.651, 22.127) | 0.54 (0.16, 0.798)☨ | |
| External rotation non-dominant leg (º) | 92.56±12.95 | 84.93±7.08 | 0.017 | 0.134 | 7.627 (-2.735, 17.989) | 0.783 (-0.137, 1.703)* | |
| Internal rotation non-dominant leg (º) | 60.00±11.18 | 48.00±9.65 | 0.79 | 0.014 | 12 (2.253, 21.747) | 1.166 (0.19, 2.142)* |
| Gender | Lunge test dominant leg | F(1)=1.154, p=0.296 | External rotation dominant leg (º) | F(1)=1.23, p=0.281 | External rotation non-dominant leg (º) | F(1)=3.793, p=0.066 | SLS dominant leg | Z=0.438, p=0.661 |
| Dominant leg | F(1)=3.642, p=0.072 | F(1)=0.27, p=0.609 | F(1)=4.157, p=0.056 | Z=-0.299, p=0.765 | ||||
| Gender:Dominant leg | F(1)=0, p=0.987 | F(1)=0.149, p=0.703 | F(1)=0.565, p=0.461 | Z=-0.244, p=0.807 | ||||
| Gender | Lunge test non-dominant leg | F(1)=1.269, p=0.274 | Internal rotation dominant leg (º) | F(1)=7.36, p=0.014 | Internal rotation non-dominant leg (º) | F(1)=7.616, p=0.013 | SLS non-dominant leg | Z=0.008, p=0.993 |
| Dominant leg | F(1)=4.159, p=0.056 | F(1)=2.334, p=0.143 | F(1)=1.161, p=0.295 | Z=1.546, p=0.122 | ||||
| Gender:Dominant leg | F(1)=0.018, p=0.895 | F(1)=0.551, p=0.467 | F(1)=1.903, p=0.185 | Z=-0.009, p=0.993 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





