1. Introduction
The role of the radiographer in producing X-ray mammography images of high quality is very crucial, as breast positioning is one of the most important factors ensuring proper visualization and correct diagnosis of detected lesions [
1,
2,
3,
4]. Amongst the main factors that lead to incorrect interpretations of mammography tissue is the improper positioning of the breast [
5,
6], which results in "parts of the breast missing" [
2], such as the pectoralis muscle [
7]. This also leads to false-negative or false-positive findings. Because of unsatisfactory quality of mammograms, patients are recalled for re-examination which results in increased radiation dose received by patients as well as discomfort to patients [
8] and unnecessary financial burdens [
9]. Further, patients are subjected to stress and undertake unnecessary additional examinations, for instance during magnetic resonance imaging or ultrasound of the breast.
Strøm
et al [
10] have studied which are the current challenges in mammography education from the perspectives of radiography teachers, mentors and students. Amongst the main limitations in mammography education were the insufficient study period allocated to this discipline as well as a lack of material resources. These limitations directly impacted the development of students’ skills in the field. Since a key factor to significantly influence mammography performance was the breast positioning, this should be prioritized as the central focus in mammography education. Other challenges are related to coping with pain and imaging of breast implants [
11,
12], and the need for further education. Metsälä
et al [
13] have shown that high quality in mammography services can be achieved via additional radiographer training. In addition, the comparison of radiographers’ mammography practice in five European countries showed the need radiographers to question their own practice and teachers to review and revise the training programmes [
3].
To enhance teaching approaches and foster the acquisition of knowledge and skills, a modernization approach in training programs involves the utilization of realistic anatomical models through the implementation of 3D printing technologies. They offer possibilities for printing anatomical objects for medical education as well as to introduce the 3D printers as a core tool in basic and advanced elective courses in BSc and MSc study programs [
14,
15]. The source of the 3D printing model is the digital model that may be created from medical simulators or patient specific data [
16,
17]. In the latter case data from X-ray modalities, such as Computed Tomography (CT), as well as data from MRI and 3D ultrasound may be exploited. The patient specific images are in the form of digital imaging and communication in medicine format (DICOM) and when anonymized they can be used in the design of various anatomical cases. Another approach is by use of medical simulators, which are capable of producing anthropomorphic models. This approach is fast and flexible and does not require preparation and submission of data to ethical committees.
Printed realistic medical phantoms are already introduced in the training of medical specialties, such as surgery [
18,
19], pediatrics [
20], traumatology [
21] as well as anatomy [
22,
23,
24,
25,
26] and pathology [
27]. The results of these studies showed high level of students’ satisfaction and confirm that the introduction of 3D printed models within the curriculum positively influences the teaching-learning outcome, such as increased confidence in identifying pathologies and enriching students’ learning experience. Overall, 53% of medical students believe that the technology can enhance their confidence when it comes to utilizing medical devices [
28]. However, these technologies primarily benefit university students in the fields of Medicine and Dental Medicine. The utilization of 3D printing technologies has the potential to advance the knowledge and skills of Radiologic technologists. Use of 3D printed models in the curriculum of Radiologic technologists was not reported in the literature.
The aim of this study is to introduce and evaluate a new approach in teaching X-ray techniques, and specifically the mammography technique to Radiologic technologists by use of 3D specific printed models. For this purpose, we manufactured anthropomorphic breast models and organised practical sessions with radiography students. Outcomes were measured by processing the data from a dedicated survey as well as assessing the cost of and the time taken to manufacture the reported 3D breast model.
2. Materials and Methods
In order to complete the work, the following main steps are considered: (a) Designing of a mammary gland model with a dedicated software; (b) Processing of the computer model and creation of a stl file; (c) Determination of the material for 3D printing; (d) 3D printing and cleaning of the models; (e) Assembling of the wholesome model of a mammary gland; (f) Creation and conduct of a specialized training for work with a mammography machine and with the new phantom, and (g) Evaluation of the mammary gland model as a training model.
2.1. Creation of breast model for the training of Radiologic technologists
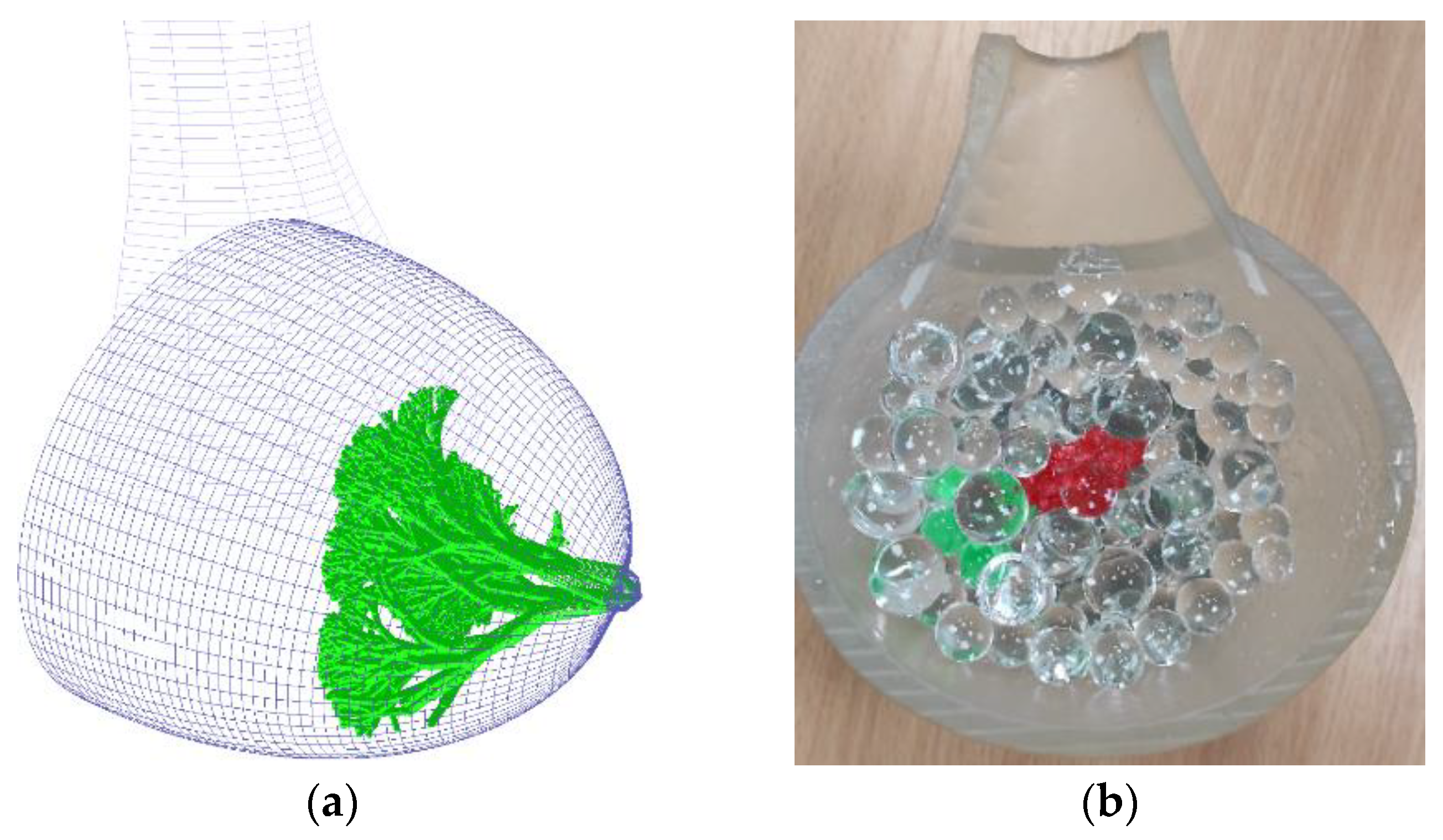
In this study, the anthropomorphic breast model is based on a computational breast model [
29] that can be generated of any size, shape and density. This model is produced by a medical simulator
BreastSimulator [
30], which consists of three basic modules for (a) generation of anthropomorphic breast phantoms based on solid geometry; (b) X-ray imaging modelling and simulation; and (c) visualization of 3D phantoms and X-ray projection images. It was used to generate a large breast model, consisting of 9447 geometrical objects (Fig. 1a). The external shape is defined by the intersection of semi-ellipsoid and semi-hyperboloid, as the size of the semi-ellipsoid is 70 mm x 60 mm x 100 mm. Within the breast, a glandular tree is generated, starting from the nipple, represented by a semi-ellipsoid. The glandular tree is modelled as a set of cylinders while the lesion is created with a mathematical algorithm [
31]. The whole model is then processed by a Matlab script, resulting in a STL file format, suitable for printing.
2.2. Printing the digital models
The training model for the Radiologic technologists was created with the stereolithographic (SLA) 3D printer Formlabs Form 3. In addition, the Formlabs Form Wash and Formlabs Form Cure devices were used for post-processing processes such as cleaning the printed models from remaining liquid resin and post curing to maximize the material properties, respectively.
The material used for printing the breast phantom was Formlabs resin Flexible 80A V1 (
https://formlabs.com/store/materials/flexible-80a-resin/), with elasticity of 80A, when post-cured and density of 1.06 g/cm
3. The model was printed at 100 µm layer thickness with supports and full raft. This included lactiferous tree as well. The lesion model was prepared separately with the same resin and settings. These models were then subjected to the following post-processing procedures. First, they were washed with Form Wash in fresh isopropyl alcohol (IPA) with concentration of 99.5% for 10 minutes and soaked in fresh IPA for another 10 minutes, then followed by post curing with Form Cure for 10 minutes at 60°C. Furthermore, water absorbing polymer balls with diameter of 8 mm were added to the printed breast phantom to simulate the adipose tissue in the breast and thus the breast heterogeneity. Diluted powder gelatine was also added.
2.3. Student assessment
The practical exercises were conducted in three groups consisting of students from the Radiologic technologists specialty at the Medical College, Medical University – Varna. The trial exercise was conducted in a dedicated training room at the Medical College Varna where a mammography machine is installed, without an X-ray tube.
A survey was developed and intended to study the opinion of the students in relation with the new practical training course. It is a part of a larger research aiming to study the opinion of the students regarding the introduction of digital technologies in curriculum of the specialities in the Medical college of MU – Varna. The research has been approved by the Ethics Committee of MU – Varna with report (Approval: 123/15/12/2021) and informed consent was obtained from every participant. The questionnaire is arranged in five sections with 13 questions in total, listed in
Table 1, and one question has open answer (Question 2). The survey is anonymous and voluntary. After the conducted practical training in the room of the mammography machine, the participants were invited to another room where they completed the surveys upon their wish, not attended by lecturers.
2.4. Statistical analysis
All statistical analyses were performed using the R programming language with RStudio IDE. The study involved categorical variables, and the results are expressed in terms of numbers and percentages. A Spearman’s correlation analysis was employed to investigate the relationship between any two variables. For items exhibiting significant correlation, a χ2 test was conducted. A statistically significant result was considered for values of p less than 0.05.
3. Results
3.1. Breast model
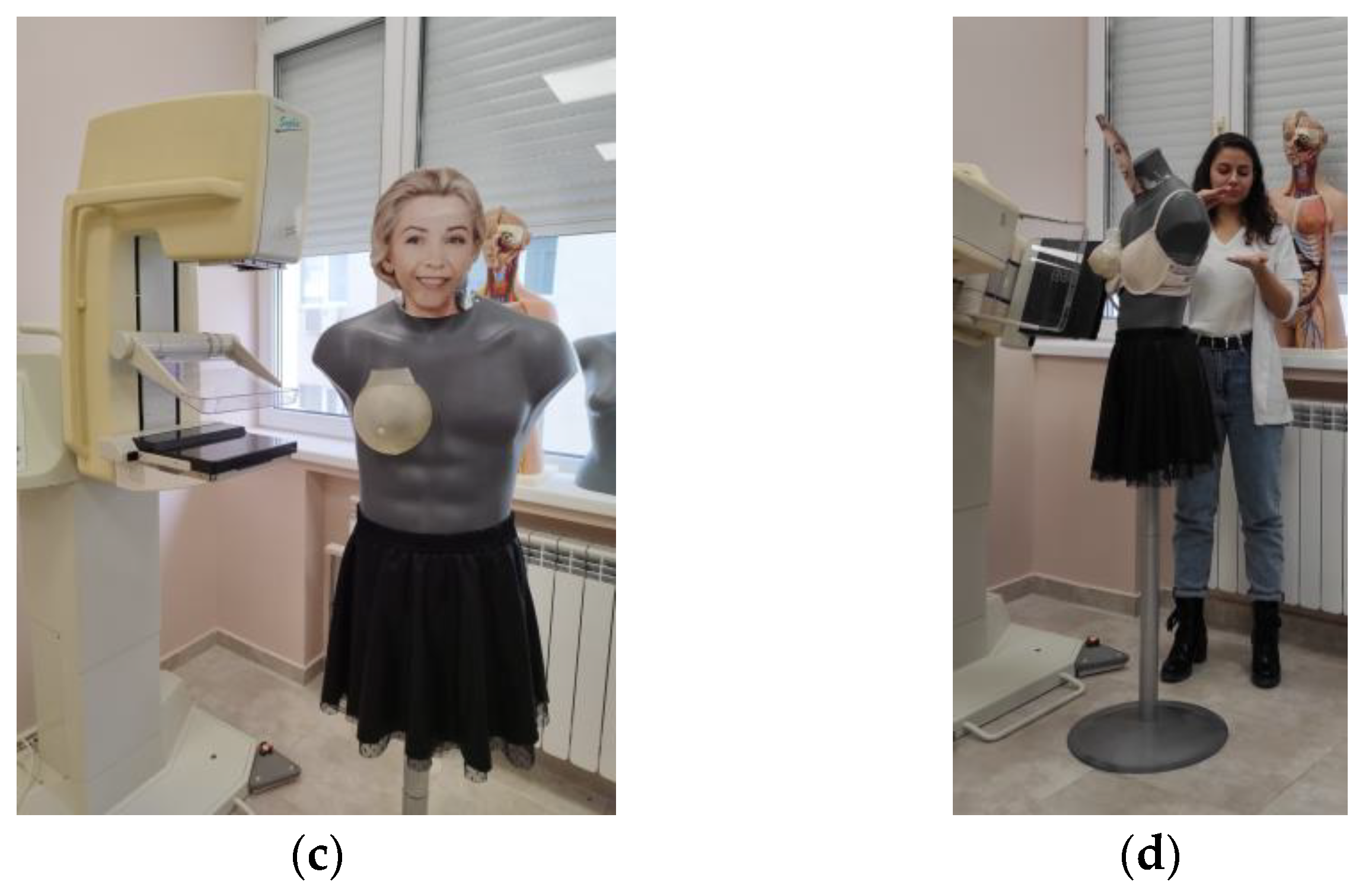
Fig 1a shows the created large computational breast model with the
BreastSimulator [
30], while the produced physical model is shown in Fig 1b. In this physical model, the breast abnormality is printed by SLA technology and coloured in red for increased visibility. The breast was mounted on a mannequin (Fig 1c) and used in practical training related to breast positioning and applying compression to the breast; thus mastering these main techniques (
Figure 1d).
3.2. Results from the survey
The survey study was carried out immediately after the practical exercise in a room in which there is no mammography machine and the lecturers who carried out the practical exercise were not there. A total of 83 students in the specialty Radiologic technologist participated in the training. From these 52 responded to the survey, of them 38 women (73%) and 14 men (27%), aged between 18 and 33, (80.77% with age in the range 18-24).
The first question addresses the students’ previous experience, revealing that they have used modern digital technology during their training.
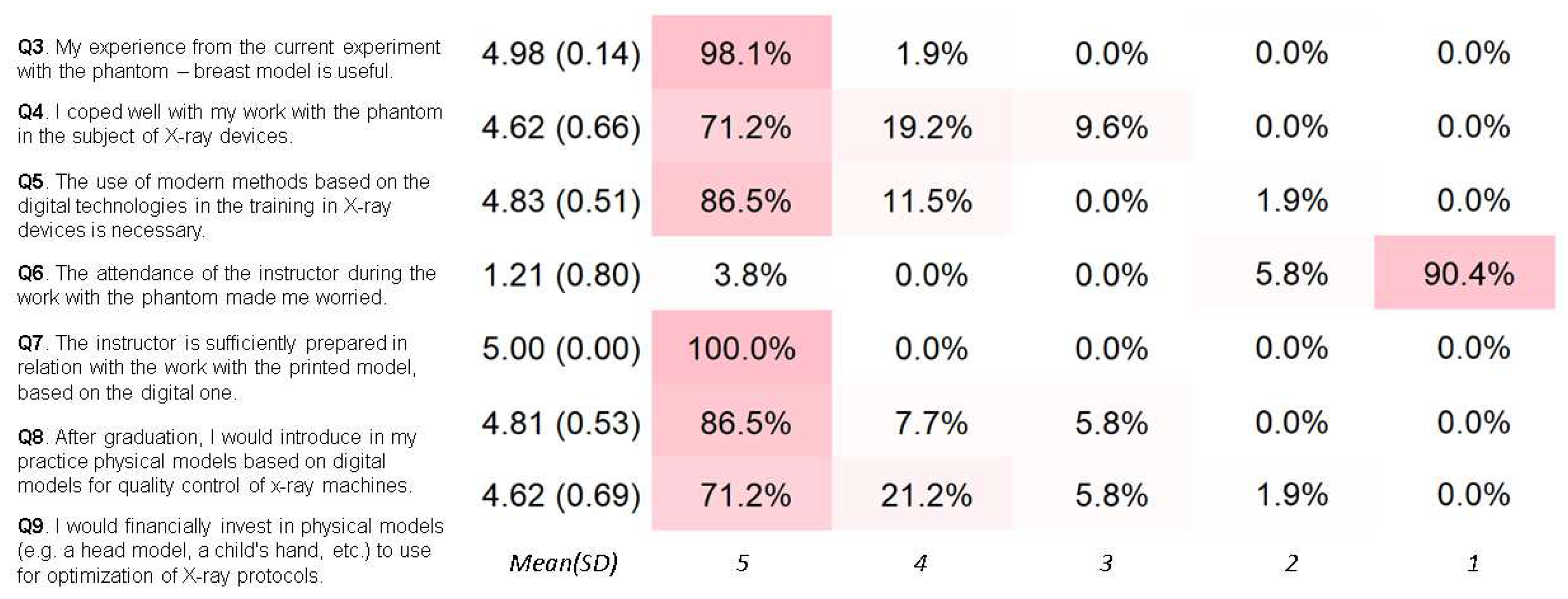
Figure 2 presents a Likert summary of the remaining survey questions. An overwhelming majority of the students (98.1%) found their experience with the physical breast phantom to be valuable for their future practice. More than half of the students (71.2%) reported that they successfully handled the exercise with the physical phantom (Q4). Additionally, a substantial number of students expressed the belief that incorporating modern methods based on digital technologies into their X-ray device training is essential (Q5).
The lecturer’s role in teaching mammography examinations was also crucial. Nearly all students were comfortable with the presence of a lecturer during the training (Q6), and all students acknowledged the lecturer’s preparedness for the exercise (Q7). Furthermore, 86.5% of the students indicated that they could implement anthropomorphic breast phantoms as quality control tools in their routine work, particularly for exercises related to compression techniques and breast positioning (Q8). Such an approach would be highly advantageous, as the phantom would closely mimic the elasticity and "translucency" to X-rays of actual mammary gland tissues. That is why the majority of the future X-ray technologists expressed their intention to utilize anthropomorphic models in their practice (Q9).
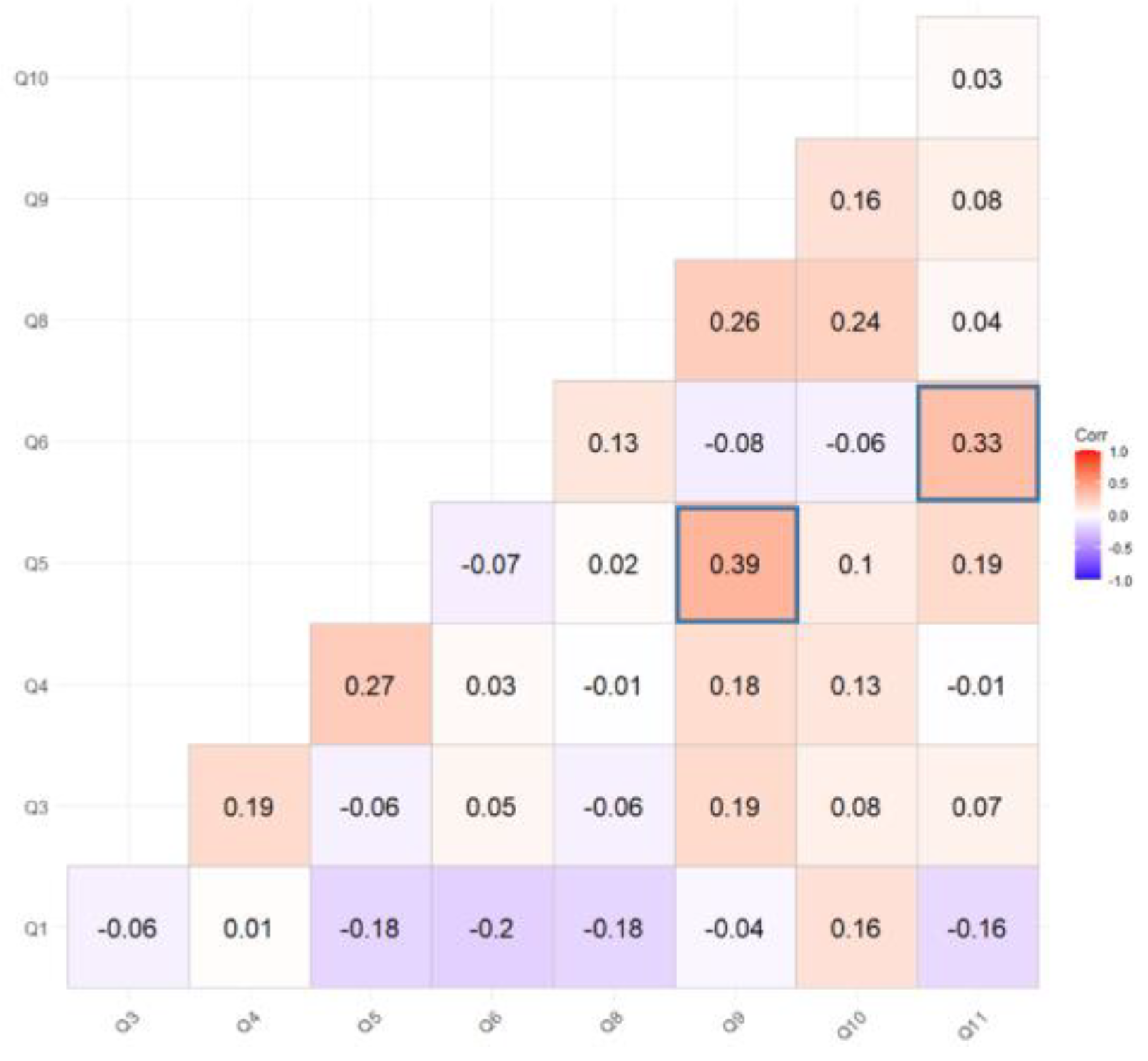
Figure 3 shows the complete item correlation matrix. The Spearman correlation analysis revealed two statistically significant results (p<0.05), which are underlined in the corresponding figure. The Chi-squared test results from the survey have been summarized in
Table 2 and
Table 3 specifically for these significant findings.
In respect to the open question (Q2): “
According to you, what are the advantages of using the digital technologies compared with the analogue technologies?” – the answers of the students are summarized in
Table 4. Some students provided more than one feedback.
4. Discussion
The 3D printing plays an increasingly important role in the field of education. The use of 3D printed anatomical models as a basic educational tool may improve student education, and students’ understanding of complex anatomical structures [
32,
33]. Methods based on 3D printed anatomical models are also appreciated in college education. They greatly assist the integration of students into the clinical environment and handle cases where they need to demonstrate creativity. It was previously demonstrated that X-ray technologists who have followed extra hands-on training in positioning perform mammograms of higher positioning quality [
7,
34]. Providing additional hands-on training within the curriculum in positioning is one of the most effective approaches for enhancing the quality of mammography positioning, considering that numerous technologists have not received such supplementary training.
In this study, radiography students from the Medical College of the Medical University of Varna participated in a practical session using an anthropomorphic breast phantom. Prior to the exercises, the students expressed that they had not previously engaged in such practical exercises and had only received theoretical instruction on these materials and techniques in lectures. The results from the descriptive statistics, presented in Fig.2, highlight the students’ highest awareness of digital medical technologies. This can be attributed to the fact that these students have been involved in training with modern medical imaging devices from the onset of their three-year college program at the University Hospital. This is important in order to decrease the significant knowledge gap in this profession as reported by [
35].
Another benefit of using of 3D printed models in education activities of students is that they can be well motivated to introduce new technologies in their professional practice, as outlined by them during their training. For instance, students noted out the easy procedure for obtaining the radiological images as well as the significantly reduced time between the image acquisition and its reading by the Radiologists (
Table 4). Amongst the lectures during the first semester of their education is the lecture for image formation by using X-ray films. Then they move to digital radiography systems and may judge and easily understand the difference related to the analogue technology. Moreover, during the specific X-ray techniques course they have exercises related to radiation dose, as exercises are organized with dedicated X-ray software simulator. With the introduction of physical anthropomorphic phantoms in the practical work of the students, the terms dose, image quality, reduced sharpness due to patient movement are better understood. This is also well compared to [
36], where only 10% of participants disagreed or were unsure about the potential of 3D models to replace the anatomical specimens for teaching.
Overall, students were very satisfied from their experience with anthropomorphic models, as seen from
Figure 2. The breast phantom was printed out with transparent resin and during compression process, the students were able to observe how the different breast structures: glandular tree, lesion and adipose structures are compressed, how to adjust the compression plate and most importantly, why there is a need for compression. The students were able to better understand the role of the compression plate, and why the breast is scanned at different positions of the X-ray tube. Therefore, almost 89% of the students agreed on the necessity to use new technologies, such as the case of 3D printed anatomical models for training. A similar level of satisfaction is reported by Valverde
et. al. [
37], where more than 95% of the participants agreed or strongly agreed that 3D models aided in better understanding medical images.
The experience with new technologies within this training seems to convince future radiographers in using these technologies in their routine work. Results from the Chi-square test of independence show that students recognize the importance of incorporating modern methods based on digital technologies in their training for exploiting X-ray devices (
Table 2). This has positive impact on their believe that they should financially invest in physical models to optimize X-ray protocols (corr. coeff. = 0.39, p = 0.004). Nevertheless, in regards to the current state of the country’s economic and social development, coupled with the substantial expenses for the necessary technologies (investment for 3D printer, materials, maintenance, etc.), only 15% of the students will have the opportunity to incorporate this innovative technology in their practical work.
The successful implementation of the used technologies heavily relies on the instructors’ knowledge and experience with them [
38]. Only in this case, the students will acquire the needed knowledge in new technologies and will further implement it in their work. This study showed that the instructor is well prepared and have the needed competence, mainly due to their involvement in innovative research projects, related to new technologies. The instructor’s presence during the exercise also affected positively the work of all students (corr. coeff. = 0.33, p = 0.016),
Table 3.
The cost of the model was also evaluated. The breast model costs about 55 EUR, not including the labour cost, electricity, deprecation and other consumables needed for post processing such as IPA. Other studies for printing the heart showed a total cost including material, time spent in segmentation, computer aided design, cleaning to be 98 USD, which is comparable to the cost of the breast phantom [
37]. For the production of these models, an investment in a SLA printer must be made, which in our case has a cost of 4300 EUR. For the manufacturing of the described models, we used Flexible A80 V1 resin, which usually comes in cartridges of one litre. One cartridge of the Flexible A80 V1 resin, costs about 240 EUR and it is sufficient for printing approximately four breast models with the tumour formations, like the one shown in Fig. 1. Furthermore, post-processing equipment was used as well, adding to the expenses with about 680 EUR for a machine for washing the models and about 870 EUR more for a post-curing equipment.
The cited costs for 3D printing of the used phantom consider a premium SLA 3D printer with the required consumables and additional equipment. The costs can be considerably reduced by using hobbyist resin 3D printers, with a rough price estimation of around 350 EUR and cheaper resins in the range of 30 to 60 EUR per litre. The quality of the printed models would most likely be reduced, but acceptable. Moreover, equivalents of the post-processing equipment can also be acquired at a lower cost.
The advantages of integrating digital technologies in medicine are well recognized, but it is crucial to acknowledge the ethical concerns that stem with the incorporation of these technologies in the education of medical students [
39,
40]. It is important that the instructor convey these ethical issues to the students at early stage of their education, thus enabling them to grasp and apply the Ethical Principles in both research and practical clinical work throughout their academic and professional journey. Utilizing anthropomorphic models for Diagnostic imaging training offers an advantage in addressing this aspect.
In summary, the presented approach aligns with the current national strategy for modernization of the Higher Education and is consistent with the European Digital Education Action Plan (EC, 2020), where it is emphasized on the development of digital competences and skills. By participating in innovative courses and acquire these skills, future radiographers will enhance their career prospects and contribute to the improvement of the quality of healthcare services.
5. Conclusions
The ability of producing anthropomorphic phantoms using 3D printing technology is of great use in improving current curricula for Radiologic technologists in medical colleges. Students readily recognize the advantages of incorporating new technologies, as they lead to reduced procedure time and improved quality in specialized procedures. Overall, Radiologic technologists were very satisfied from their experience with the physical models, as well as the presence of an instructor during the exercise also affected positively the work of all students. The experience with new technologies within this training seems to convince future Radiologic technologists in using these technologies in their routine work, which is expected to bring forth new opportunities for career development and ultimately contribute to the enhanced quality of healthcare services.
Author Contributions
Conceptualization, K.B., N.D.; methodology, All; investigation, All; software K.B.; writing—original draft preparation, K.B., N.D, M.M; writing—review and editing, N.D., M.K., M.M., Z.B.; supervision, K.Ts. All authors have read and agreed to the published version of the manuscript.
Funding
The study is implemented within the frame of a MUVE-TEAM project under contract No. BG-RRP-2.004-0009-C02 and is financed by the European Union - NextGenerationEU, through the National Plan for Recovery and Sustainability of the Republic of Bulgaria under procedure BG-RRP-2.004 - Creation of a network of research universities.
Institutional Review Board Statement
The research has been approved by the Ethics Committee of MU – Varna with report (Approval: 123/15/12/2021).
Informed Consent Statement
Informed consent was obtained from every participant.
Data Availability Statement
The content generated and analyzed in this study is available from the corresponding author on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- P.V. Zujić, A. P.V. Zujić, A. Božanić, S. Jurković, D. Šegota, E.G. Dujmić, B. Čandrlić, M. Karić, The role of self-evaluation and education of radiographers involved in a breast cancer screening program at Clinical Hospital Center Rijeka. Radiography 2021, 27, 1162–1165. [Google Scholar] [CrossRef] [PubMed]
- Hofvind, S.; Vee, B.; Sørum, R.; Hauge, M.; Ertzaas, A.-K.O. Quality assurance of mammograms in the Norwegian Breast Cancer Screening Program. Eur. J. Radiogr. 2009, 1, 22–29. [Google Scholar] [CrossRef]
- N. Richli Meystre, A. N. Richli Meystre, A. Henner, C. Sà dos Reis, B. Strøm, J.A. Pires Jorge, T. Kukkes, E. Metsälä, Characterization of radiographers’ mammography practice in five European countries: a pilot study. Insights Imaging 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Albeshan, S.; Alashban, Y.; Shubayr, N.; Alkhudairy, A.; Eliraqi, F. Evaluation of Radiographers’ Experience in Mammography: An Explanatory Study. Iran. J. Radiol. 2022, 19. [Google Scholar] [CrossRef]
- G.H. Rauscher, E.F. G.H. Rauscher, E.F. Conant, J.A. Khan, M.L. Berbaum, Mammogram image quality as a potential contributor to disparities in breast cancer stage at diagnosis: an observational study. BMC Cancer 2013, 13. [Google Scholar] [CrossRef]
- Taylor, K.; Parashar, D.; Bouverat, G.; Poulos, A.; Gullien, R.; Stewart, E.; Aarre, R.; Crystal, P.; Wallis, M. Mammographic image quality in relation to positioning of the breast: A multicentre international evaluation of the assessment systems currently used, to provide an evidence base for establishing a standardised method of assessment. Radiography 2017, 23, 343–349. [Google Scholar] [CrossRef]
- Dos Reis, C.S.; Pascoal, A.; Radu, L.; De Oliveira, M.F.; Alves, J. Overview of the radiographers’ practice in 65 healthcare centers using digital mammography systems in Portugal. Insights into Imaging 2017, 8, 345–355. [Google Scholar] [CrossRef]
- Dumky, H.; Leifland, K.; Fridell, K. The Art of Mammography With Respect to Positioning and Compression—A Swedish Perspective. J. Radiol. Nurs. 2018, 37, 41–48. [Google Scholar] [CrossRef]
- Mercieca, N.; Portelli, J.; Jadva-Patel, H. Mammographic image reject rate analysis and cause – A National Maltese Study. Radiography 2016, 23, 25–31. [Google Scholar] [CrossRef]
- B. Strøm, J.A. B. Strøm, J.A. Pires Jorge, N. Richli Meystre, A. Henner, T. Kukkes, E. Metsälä, C. Sà dos Reis, Challenges in mammography education and training today: The perspectives of radiography teachers/mentors and students in five European countries. Radiography 2018, 24, 41–46. [Google Scholar] [CrossRef]
- Park, J.; Ko, E.Y.; Han, B.-K.; Choi, J.S.; Kim, H. Appropriate screening mammography method for patients with breast implants. Sci. Rep. 2023, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- dos Reis, C.S.; Gremion, I.; Meystre, N.R. Study of breast implants mammography examinations for identification of suitable image quality criteria. Insights into Imaging 2020, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Metsälä, E.; Meystre, N.R.; Jorge, J.P.; Henner, A.; Kukkes, T.; dos Reis, C.S. European radiographers’ challenges from mammography education and clinical practice – an integrative review. Insights into Imaging 2017, 8, 329–343. [Google Scholar] [CrossRef] [PubMed]
- Harmon, D.J.; Klein, B.A.; Im, C.; Romero, D. Development and implementation of a three-dimensional (3D) printing elective course for health science students. Anat. Sci. Educ. 2021, 15, 620–627. [Google Scholar] [CrossRef]
- Chernogorova, Y.; Kalinov, T.; Dukov, N.; Bliznakova, K.; Zlatarov, A.; Kolev, N.; Bliznakov, Z. Transforming Scientific Results into Educational Materials - Added Value of a Research Project. TEM J. 2022, 11, 120–124. [Google Scholar] [CrossRef]
- Bliznakova, K. The advent of anthropomorphic three-dimensional breast phantoms for X-ray imaging. Phys. Medica 2020, 79, 145–161. [Google Scholar] [CrossRef] [PubMed]
- Glick, S.J.; Ikejimba, L.C. Advances in digital and physical anthropomorphic breast phantoms for x-ray imaging. Med Phys. 2018, 45, E870–E885. [Google Scholar] [CrossRef]
- Liu, G.; Bian, W.; Zu, G.; Liu, J.; Zhang, G.; Li, C.; Jiang, G. Development of a 3D Printed Lung Model Made of Synthetic Materials for Simulation. Thorac. Cardiovasc. Surg. 2021, 70, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; McWilliam, M.; Ahlin, J.; Davidson, J.; Quantz, M.A.; Bütter, A. A simulated training model for laparoscopic pyloromyotomy: Is 3D printing the way of the future? J. Pediatr. Surg. 2018, 53, 937–941. [Google Scholar] [CrossRef]
- Asif, A.; Lee, E.; Caputo, M.; Biglino, G.; Shearn, A.I.U. Role of 3D printing technology in paediatric teaching and training: a systematic review. BMJ Paediatr. Open 2021, 5, e001050. [Google Scholar] [CrossRef]
- Hasenstein, T.; Patel, K.P.; Moore, J.L.; Meyr, A.J. Printed 3-Dimensional Computed Tomography Scanned Ankle Fractures as an Educational Instrument. J. Foot Ankle Surg. 2019, 58, 1081–1084. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, M.K.; Reese, S.; Herlihy, T.; Geoghegan, T.; Cantwell, C.P.; Feeney, R.N.; Jones, J.F. Fabrication and assessment of 3D printed anatomical models of the lower limb for anatomical teaching and femoral vessel access training in medicine. Anat. Sci. Educ. 2015, 9, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Vaccarezza, M.; Papa, V. 3D printing: a valuable resource in human anatomy education. Anat. Sci. Int. 2014, 90, 64–65. [Google Scholar] [CrossRef]
- Ye, Z.; Dun, A.; Jiang, H.; Nie, C.; Zhao, S.; Wang, T.; Zhai, J. The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC Med Educ. 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lozano, M.T.U.; Haro, F.B.; Ruggiero, A.; Manzoor, S.; Méndez, J.A.J. Evaluation of the Applicability of 3d Models as Perceived by the Students of Health Sciences. J. Med Syst. 2019, 43, 108. [Google Scholar] [CrossRef]
- Cai, B.; Rajendran, K.; Bay, B.H.; Lee, J.; Yen, C. The Effects of a Functional Three-dimensional (3D) Printed Knee Joint Simulator in Improving Anatomical Spatial Knowledge. Anat. Sci. Educ. 2018, 12, 610–618. [Google Scholar] [CrossRef]
- Youman, S.; Dang, E.; Jones, M.; Duran, D.; Brenseke, B. The Use of 3D Printers in Medical Education with a Focus on Bone Pathology. Med Sci. Educ. 2021, 31, 581–588. [Google Scholar] [CrossRef]
- Cercenelli, L.; De Stefano, A.; Billi, A.M.; Ruggeri, A.; Marcelli, E.; Marchetti, C.; Manzoli, L.; Ratti, S.; Badiali, G. AEducaAR, Anatomical Education in Augmented Reality: A Pilot Experience of an Innovative Educational Tool Combining AR Technology and 3D Printing. Int. J. Environ. Res. Public Heal. 2022, 19, 1024. [Google Scholar] [CrossRef]
- Bliznakova, K.; Bliznakov, Z.; Bravou, V.; Kolitsi, Z.; Pallikarakis, N. A three-dimensional breast software phantom for mammography simulation. Phys. Med. Biol. 2003, 48, 3699–3719. [Google Scholar] [CrossRef]
- Bliznakova, K.; Sechopoulos, I.; Buliev, I.; Pallikarakis, N. BreastSimulator: A software platform for breast x-ray imaging research. J. Biomed. Graph. Comput. 2012, 2, p1. [Google Scholar] [CrossRef]
- Bliznakova, K.; Dukov, N.; Feradov, F.; Gospodinova, G.; Bliznakov, Z.; Russo, P.; Mettivier, G.; Bosmans, H.; Cockmartin, L.; Sarno, A.; et al. Development of breast lesions models database. European Congress of Medical Physics (ECMP). LOCATION OF CONFERENCE, COUNTRYDATE OF CONFERENCE; pp. 293–303.
- Salazar, D.; Thompson, M.; Rosen, A.; Zuniga, J. Using 3D Printing to Improve Student Education of Complex Anatomy: a Systematic Review and Meta-analysis. Med Sci. Educ. 2022, 32, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.G. Three-dimensional Printing in Anatomy Education: Assessing Potential Ethical Dimensions. Anat. Sci. Educ. 2018, 12, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Guertin, M.-H.; Théberge, I.; Zomahoun, H.T.V.; Dufresne, M.-P.; Pelletier. ; Brisson, J. Technologists’ Characteristics and Quality of Positioning in Daily Practice in a Canadian Breast Cancer Screening Program. Acad. Radiol. 2016, 23, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Seitzman, R.L.; Pushkin, J.; A Berg, W. Radiologic Technologist and Radiologist Knowledge Gaps about Breast Density Revealed by an Online Continuing Education Course. J. Breast Imaging 2020, 2, 315–329. [Google Scholar] [CrossRef]
- Valverde, I.; Gomez, G.; Byrne, N.; Anwar, S.; Cerpa, M.A.S.; Talavera, M.M.; Pushparajah, K.; Forte, M.N.V. Criss-cross heart three-dimensional printed models in medical education: A multicenter study on their value as a supporting tool to conventional imaging. Anat. Sci. Educ. 2021, 15, 719–730. [Google Scholar] [CrossRef] [PubMed]
- Valverde, I.; Gomez, G.; Byrne, N.; Anwar, S.; Cerpa, M.A.S.; Talavera, M.M.; Pushparajah, K.; Forte, M.N.V. Criss-cross heart three-dimensional printed models in medical education: A multicenter study on their value as a supporting tool to conventional imaging. Anat. Sci. Educ. 2021, 15, 719–730. [Google Scholar] [CrossRef]
- Pagnucci, N.; Carnevale, F.A.; Bagnasco, A.; Tolotti, A.; Cadorin, L.; Sasso, L. A cross-sectional study of pedagogical strategies in nursing education: opportunities and constraints toward using effective pedagogy. BMC Med Educ. 2015, 15, 138. [Google Scholar] [CrossRef]
- N.H. Ghazali, A. N.H. Ghazali, A. Abd Manaf, G. Sulong, Review of watermarking techniques for medical images. Int. J. Appl. Eng. Res. 2015, 10, 4991–5003. [Google Scholar]
- Singh, K.U.; Abu-Hamatta, H.S.; Kumar, A.; Singhal, A.; Rashid, M.; Bashir, A.K. Secure Watermarking Scheme for Color DICOM Images in Telemedicine Applications. Comput. Mater. Contin. 2022, 70, 2525–2542. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).