1. Introduction
Schistosomiasis is one of the most important human helminthiasis in terms of morbidity and mortality (McManus & Loukas, 2008). The disease is endemic in many developing countries mainly affects children, farmers, and women who are frequently in contact with water inhabited by snail intermediate hosts. According to the WHO, in 2019, 236.6 million people will need preventive treatment in 78 countries (Ossai et al., 2014; WHO 2022), with the heaviest burden in sub-Saharan Africa (90%) (4).
According to the results of the national surveys carried out by the Schistosomiasis National Schistosomiasis Control Programme (SNCP) in 1984-1989, then in 2004-2006, schistosomiasis due to Schistosoma mansoni and S. haematobium and Soil-transmitted helminths (STH) are still endemic throughout the country (5). For instance, in 2004, the prevalence of S. haematobium and those of S. mansoni were 61.7% and 12.7% respectively in the Office du Niger irrigated area (6). Along the Senegal river, the prevalence were higher than 70% in some villages (7)
Recommended by the WHO from 1970 to 1980 (8,9), large-scale chemotherapy to control morbidity with coverage rate of 75% in school-age children have been formally considered as an essential public health strategy to combat schistosomiasis by the fifty Fourth World Health Assembly (WHA 54.19) in 2001. As indicated in the WHO guidelines, a new initiative to resume the national control activities has been in place in Mali since 2004, targeting school-aged children (SAC) and adults at risk in order to achieve the WHA54.19 recommendation with technical and financial support from the Schistosomiasis control Initiative (SCI), USAID/RTI/HKI, The organization for the development of the Senegal River (OMVS) and Sight savers in all endemic regions (10,11). Following this initiative, MDA with PZQ, four regions first benefited from the strategy in 2005, targeting only school-age children (7–14 years old) attending schools. By 2006, the strategy was expanding to other regions, targeting all school-age children (5–15 years old) (11). In 2007, the Schistosomiasis and Soil-transmitted National Control Programme (SNCP) devoted to combat schistosomiasis were integrated into the National NTDs Control Programme. Since that date, an annual or bi-annual treatment campaign carried out in all endemic areas (Ségou, Mopti, Koulikoro and Kayes regions) based on the current prevalence threshold as recommended by the WHO. However, since the NSCP has adopted the community directed intervention (CDI) approach in 2005, the programme has faced some difficulties which led to very low coverage, particularly in some endemic areas such as the Diéma district in Kayes region. In addition to these difficulties, its impact needs to be assessed regularly, particularly in sentinel sites. The current study was carried out with a view to a global fight against schistosomiasis in line of the WHO’s 2021-2030 road map to achieve the target for eliminating schistosomiasis as a public health problem and the interruption of transmission in humans in selected countries adopted in 2022. It aimed to assess the impact of MDA with PZQ on the prevalence and intensity of schistosomiasis and STH in sentinel sites identified by Schistosomiasis National Control Programme (SNCP).
2. Materials and Method
2.1. Study Site
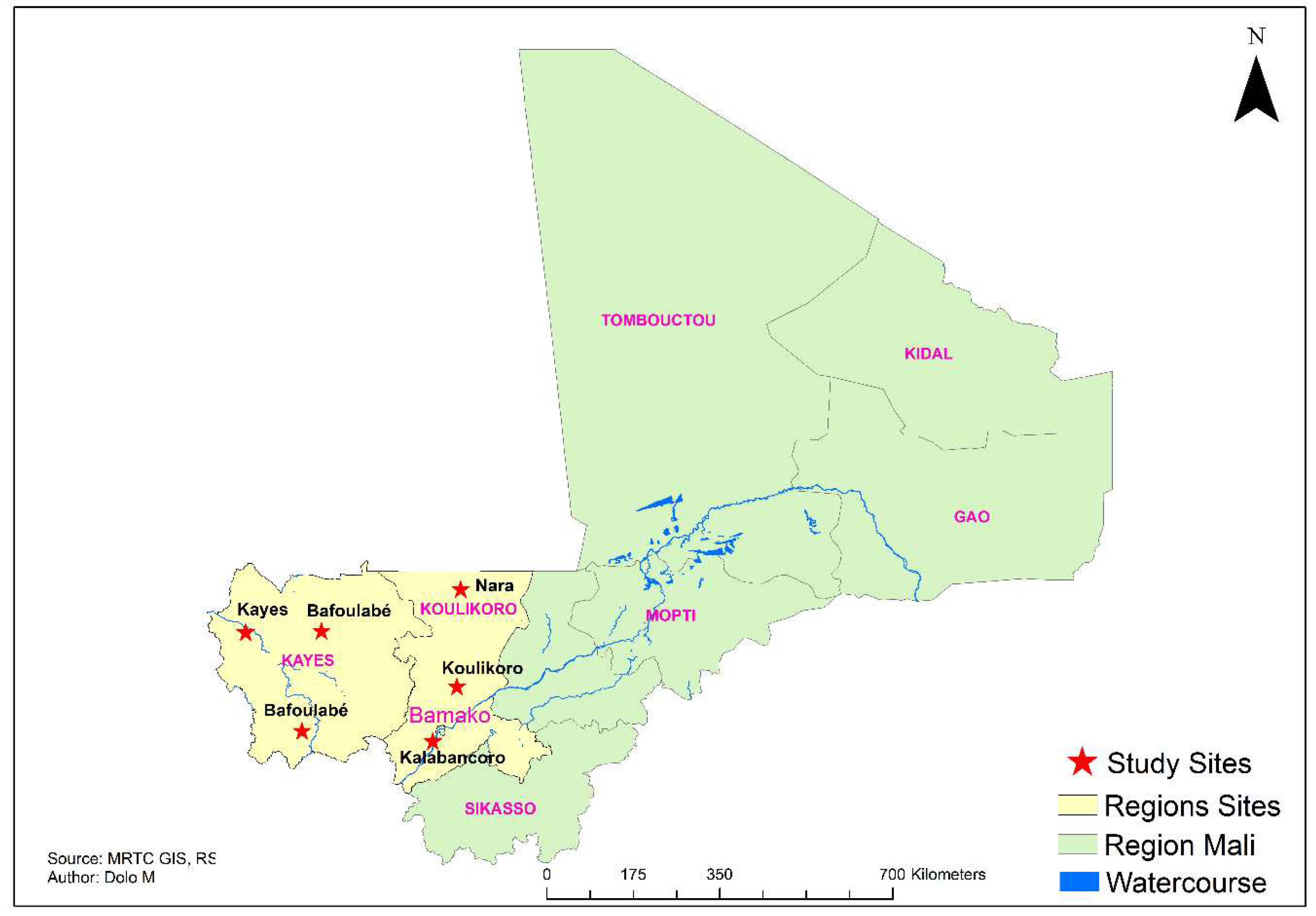
The study was carried out in twelve villages spread over six districts: Bafoulabé, Diéma and Kayes (in Kayes region); Kalabancoro, Koulikoro and Nara (in Koulikoro region) (
Figure 1). The Hydrographically network in the study is made up of Senegal River and its tributaries in Kayes region, and Niger River and its tributaries in Koulikoro region. It also composed by the lake system (Lac Magui) and pools (Doro and Goumbaye) in the Kayes region. The economic life in the study area is dominated by agro-pastoral activities which occupy more than 80% of the population. The health system is precarious, with high infant and maternal mortality, low life expectancy, chronic malnutrition among children and inadequate infrastructure and equipment (12). The study site is recognized as a highly endemic area for schistosomiasis (8,13,14). The Kayes region, particularly the Diéma district, is characterized by a low treatment coverage rate of less than 60% ((oral communication from the PNLSH’s coordinator).
2.2. Population and Study
School-aged children 6- to 14 years old were primarily identified as study population. We carried out a two-round observational cross sectional study: the first baseline round was conducted in December 2014-2015 and the second in April 2018. According to SNCP officials, from December 2014-2015 to April 2018, children were regularly submitted to MDA with PZQ. During each pass, stool and urine samples were examined. The time lag between the different treatment rounds is due to the treatment agenda of the SNCP in relation to each district planned treatment frequency.
2.3. Sampling Design and Sample Size Calculation
For the 2018 study students were randomly selected from schools from the list of students present in each class on the day of the survey. A random draw without discount was adopted for the selection of participants. The sample size was calculated on the basis of the prevalence of S. haematobium (the most frequent schistosome species) described in 2009. The assumed precision around the prevalence rates to be measured was 6% with an alpha risk of 5%. We added 10% to this sample size to compensate for the loss of sight. The Schwartz formula was used to calculate the minimum sample size. The results of this study were compared to those of 2014-2015 carried out by the NSCP. According to the officials of the programme, the sample size examined in 2014-2015 (n=720) was calculated according to WHO sample size estimation (15).
2.4. Data Collection Techniques and Procedures
All urine samples were collected between 10.00 am and 2.00 pm in the field, by trained laboratory technicians to determine prevalence and intensity of S. haematobium infection. Urine was collected from each subject in a properly labeled specimen container. Filtration technique was used to analyse the samples. A total of 10 ml of urine was taken from each specimen bottle after mixing it. The mixed sample was filtered through a Whatman filter (CAT N° 1001-025, 25 mm) which was stained with 3% ninhydrin solution, before being sent to Bamako to be examined under a microscope using ×10 magnifications for S. haematobium egg characteristics. One single stool sample from each child was collected and examined immediately on fields with the standard Kato-Katz method for S. mansoni and STH eggs. The intensity of S haematobium infection was expressed as the number of eggs per 10 ml of urine and was classified into three categories: i) no egg; ii) slight (1–49 eggs per 10 ml of urine); and iii) heavy (≥50 eggs per 10 ml of urine). The intensity of S. mansoni intensity was expressed as eggs per gram of stool (pg) and classified into four classes: i) no egg; ii) 1–99 EPG (eggs per gram of stool); iii) 100–399 EPG; and iv) ≥ 400 EPG (11). To ensure quality control, 10% of the filters and slides were randomly selected and recounted by another senior biologist. At the end of the study, all the positive children were treated with PZQ (40 mg/kg body eight) according to the Schistosomiasis and STH National Control Programme in Mali (PNLSH).
2.5. Mass Drug Administration
The preventive chemotherapy strategies recommended by the WHO has been adopted by the Mali’s schistosomiasis control programme since 2005 in four endemic areas (8,12) . To perform this strategy, a MDA campaign is designed each year in schools and health authorities at regional, district and community school personal are mobilized. Drugs are distributed through the school-based delivery in schools targeting school-going children. This drug delivery strategy is carried out by trained school teachers. PZQ tablets (600 mg) were delivered using the WHO dose pole method to determine the dosage for each child (16). Current WHO guidelines (17) use heavy-intensity infections (≥50 S. haematobium eggs per 10 mL of urine or ≥400 S. mansoni eggs per gram of stool (12) to categorize a target population’s status. Target populations with a prevalence of heavy-intensity infections (PHI) <5% are classified as having controlled schistosomiasis morbidity, and when a target population has <1% PHI, that population has eliminated schistosomiasis as a public health problem.
2.6. Ethics
Before currying out the survey in each sentinel school, informed verbal consent was first obtained from the schoolteachers before the children were recruited. These were recorded by the survey team leader. During recruiting, informed verbal consent was obtained from each child with the presence of the school teachers. Any children who did not wish to participate were free to leave without prejudice to their support for the treatment. Study participants who tested positive for S. haematobium or S. mansoni were treated with praziquantel at the standard dose of 40 mg/kg body weight as recommended by the SNCP. The drug was administered orally after the child had eaten. The proposal was reviewed and approved by the Institutional Review Board (IRB) of the Faculty of Medicine, Pharmacy and Dentistry of the University of Bamako (N°2017/135/CE/FMPOS).
2.7. Statistical Analysis
Data were entered in duplicate using Access and Prevalence, and intensity of infection with 95% confidence intervals was calculated using SPSS (IBM, version 19). Differences in proportions were tested using the chi-square test or Fisher’s exact test depending on the data. P values less than 0.05 were considered to be significant.
3. Results
In December, 734 schoolchildren were examined with320 females and 414 males. In April 2018, 1836 schoolchildren have been screened from which 1708 were successfully examined including 733 females and 975 males. They were aged between 7 to 14 years with an average age of 9 ± 1.970 years. As shown in the
Table 1,
S. haematobium prevalence in 2014 varied from zero in Boudjiguiré to 96.8% in Babaroto. In 2018, the prevalence increased to 11% in Boudjiguiré while it decreased significantly to 33.95% in Babaroto (
p<0.001). Overall, from 2014 to 2018, the prevalence decreased significantly in Babaroto, Saorane, Torodo and Koussané (p< 0.001) and Dianguirdé (p=0.004), increased significantly in Diakalel (p<0.001), but not significantly in Kolly and Boudjiguiré (
p>0.05). From 2015 to 2018, the prevalence increased significantly in Samaya (
p=0.006) and Kokoun (
p=0.02) (
Table 1).
Between 2014 to 2018, there was a significant reduction in the prevalence of heavy intensity infection with
S. haematobium in the districts of Bafoulabé (Babaroto and Saorané) and Diéma (Dianguirdé et Torodo) (
p<=0.001) (
Table 2). In Diakalel, the prevalence of heavy infections rose to 19.21% from 2014 to 2018 (
p<0.001). In Kolly and Bougoudjiré, the prevalence remained zero. From 2015 to 2018, the prevalence of heavy infections increased slightly in Dougourakoro and Samaya, decreased slightly in Kokoun.
In terms of results obtained after treatment campaigns on the intensity of the disease, one SS (Saorané) have achieved the criterion of eliminating schistosomiasis as a major public health problem (prevalence of heavy intensity infection - PHI< 1%); four sites (Dianguirdé, Torodo, Koussané and Kokoun) have reached the criterion for controlling morbidity (prevalence of high excretors - PHI< 5%) and two sites (Babaroto and Diakalel) remain confined below the control criterion (PHI>5%). The status of five SS (Dougourakoro, Keniegue, Samaya, Kolly and Bougoudjire) without any havy intensity infection in 2004 did not change in 2018.
4. Discussion
This study aimed to assess the impact of the repeated MDA with Praziquantel in twelve sentinel sites among two
S. haematobium endemic areas (Kayes and Koulikoro) covered by the National Schistosomiasis Control Programme (NSCP). Children aged between 6 and -14 were identified as targeted population in regard to the peak prevalence and intensity of schistosomiasis and STH observed in this age group (12). The priority given to this age group is based on the fact that the level of infection observed in this population reflects the impact of several round of MDD with PZQ after the implementation of a control programme. In line of WHO current road map guidelines (2021-2020), only one and four out of the twelve SS reached the elimination and morbidity control of schistosomiasis criterion as public health problem (PHI<1% and PHI<5%, respectively) in 2018 after four to five MDD rounds. Reducing the prevalence of heavy infection is important as it is well known that the severity of morbidity caused by schistosomiasis is closely related to the intensity of infection. In many national control programme, cases of severe morbidity were avoided or reversed with MDA. This is in line with what was achieved in other national MDA programme particularly in East and West Africa through preventive chemotherapy (18–22). However, beside the heavier infections, there still exist a significant proportion of children with infections of relatively low intensity (1-49 eggs per 10 ml of urine), not counting those who were not detected due to the low sensitivity of the urine filtration technique. This is the case of the five sites (Dougourakoro, Keniegue, Samaya, Kolly and Boudjiguiré) where no heavy-intensity infection were observed in 2014-2015. Such low intensities of infection have long been overlooked in terms of the morbidity consequences, while recent findings suggest that light infections can cause considerable morbidity due to anaemia, chronic pain, diarrhoea, exercise intolerance and undernutrition (23). Anyway, the objective of MDD was to prevent morbidity due to schistosomiasis by regular treatment in line with WHO recommendations (12,24) as it was conducted in the sentinel sites. In other hand, in contrast to the low success rate in eliminating as a public health issue (one and four SS with PHI<1% and 5% for schistosomiasis elimination and control, respectively), the prevalence of infection was significantly reduced at 66.7% (8/12) sites. In view of the performance of such results, some authors suggested a reevaluation of the criteria for schistosomiasis control because of the inability of current PHI categorizations to differentiate the prevalence of standard morbidity markers. To this end, they propose to shift the definition of the schistosomiasis elimination as public health (EPHP) targets to a function of the prevalence of any
Schistosoma infection rather than its intensity (25). Persistence or increase of infection in some SS (
Table 1) emphasizes in line with World Health Organization (WHO) guidelines the need for a more effort associating with comprehensive control measures including reinforcement of preventive chemotherapy, intensified case management, snail’s intermediate hosts control, health education and improvement of sanitation and access to improved water sources, sanitation and hygiene (26,27). Another hypothesis in addition to the low impact of treatment would be the hybrid strains of
S. haematobium /
S. bovis or
S. haematobium/S. curassoni identified in the study site (28) and which have been found to influence parasite establishment, growth, maturation, reproductive success, and/or drug efficacy (29,30). Our study is limited by the amount of urine (10ml) or feces (25mg) examined from the filtration of a single urine sample (10 mL) or the examination of a single feces sample (25 mg of feces) with Kato-Katz technique. The two surveys (2014-2015 and 2018) although conducted by two different teams do not call into question the validity of the results obtained. The impact of MDD with PZQ resulted to a significant reduction of prevalence and intensity of infection in the NSCP SS after four to five treatment rounds. The persistence of the disease or its increase some other sites call for further investigations, including the existence of hybrid strains and their role in public health.
5. Conclusions
The study assessed the impact of MDD with PZQ over a period of four to five years in twelve sites sentinel of the NSCP. Despite repeated treatment campaigns, schistosomiasis remains hyperendemic (P>50%) in some sentinel sites such as Diakalel and Babaroto and hypoendemic (P<10%) in others such as Keniegue and Dougourakoro. One SS reached the criterion for schistosomiasis elimination as public health problem (PHI<1%) while four achieved the criterion of morbidity control (PHI<5%) in line of WHO’s 2021-2030 road map. However, two sites remain confined below the control criterion (PHI>5%). These results call for a major improvement in therapeutic coverage in addition to intensified case management, sanitation and hygiene to interrupt the schistosome transmission cycle.
Author Contributions
A.D. has updated the research methodology. A. D., A.P., D. M., D. S., D. S., coordinated the fieldwork. A. P., D. M. and A. D. read the filters and slides. A. P. and A. D. carried out the statistical analysis. A. P., D. M., A. D. and I. M., reviewed the manuscript prior to submission.
Funding
This study was funded by World Bank.
Acknowledgements
The authors would like to thank the directors of the various schools, the schoolchildren who provided the samples and the academy directors. We would also like to thank the World Bank for providing funding and the MRTC for providing the framework for sample analysis.
Conflicts of Interest
No conflicts of interest.
References
- McManus, D. P. & Loukas A. Current status of vaccines for schistosomiasis. Clin Microbiol Rev. 2008;21(1), 225. [CrossRef]
- WHO. Schistosomiasis and soil-transmitted helminthiases: progress report, 2021. https://www.who.int/publications/i/item/who-wer9748-621-632. 2022;(48):621–32.
- Ossai PO, Dankoli R, Nwodo C, Tukur D, Nsubuga P, Ogbuabor D, et al. Bacteriuria and urinary schistosomiasis in primary school children in rural communities in Enugu State, Nigeria, 2012. Pan Afr Med J. 2014;18:15. [CrossRef]
- Dawet A, Yakubu D., Longmut R, Benjamin C., Nannim Y., Daburum N. Prevalence and intensity of Schistosoma haematobium among residents of Gwong and Kabong in Jos North Local Government Area, Plateau State, Nigeria. Int J Biol Chem Sci. 2012 Dec 14;6(4). [CrossRef]
- Ministry of health and public hygiene. Management Plan for the control of Neglected Tropical Diseases (MTN) – (2017-2021). Natl Heal Dir. 2021;79P.
- Landouré A, Dembélé R, Goita, S., Kané M, Tuinsma M, Sacko, M. & Zhang Y. Significantly Reduced Intensity of Infection but Persistent Prevalence of Schistosomiasis in a Highly Endemic Region in Mali after Repeated Treatment. Neglected Trop deseaseseglected Trop deseases. 2012;6(7). [CrossRef]
- Traoré M, Maude G, Bradley D. Schistosomiasis haematobia in Mali: Prevalence rate in school-age children as index of endemicity in the community. Trop Med Int Heal. 1998;3(3):214–21. [CrossRef]
- WHO. Schistosomiasis and STH. Fifty-fourth World Health Assembly. Geneva. 2001.
- ODD. Agenda for sustainable development objectives, Https://www.unodc.org/unodc/fr/frontpage/2015/September. Agenda for sustainable development objectives. 2015. p. Https://www.unodc.org/unodc/fr/frontpage/2015/Sept.
- Fenwick A, Webster JP, Bosque-Oliva E, Blair L, Fleming FM, Zhang Y. The Schistosomiasis Control Initiative (SCI): Rationale, development and implementation from 2002-2008. Parasitology. 2009;136(13):1719–30. [CrossRef]
- Garba A, Touré S, Dembelé R, Boisier P, Tohon Z, Bosqué-Oliva E. Present and future schistosomiasis control activities with support from the Schistosomiasis Control Initiative in West Africa. Parasitology. 2009;136(13):1731–7. [CrossRef]
- WHO. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. WHO Technical Report Series 912. 2002.
- Ministry of health and public hygiene ND of H. Master plan for the control of neglected tropical diseases (NTD) - 2017-2021. 2017. p. 79p.
- Tandina F, Doumbo SN, Koné AK, Guindo D, Goita S, Sissoko M. Épidémiologie des schistosomoses dans le village périurbain de Sotuba, dix années après la mise à échelle du traitement de masse au Mali. Med Sante Trop. 2016;26(1):51–6. [CrossRef]
- Lwanga S, Lemeshow S. Sample size determination in health studies: a practical manual. World Heal Organ. 1991;1–80.
- WHO. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030. Geneva World Heal Organ. 2020;1–2.
- WHO WH organization. Progress report 2001–2011 and Strategic plan, 2012– 2020. Geneva. available at: https://apps.who.int/iris/handle/10665/78074. 2013.
- Touré S, Zhang Y, Bosqué-oliva E, Ky C, Ouedraogo A, Koukounari A. Two-year impact of single praziquantel treatment on infection in the national control programme on schistosomiasis in Burkina Faso. 2008;048694(August). [CrossRef]
- Zhang Y, Koukounari A, Kabatereine N, Fleming F, Kazibwe F, Tukahebwa E. Parasitological impact of 2-year preventive chemotherapy on schistosomiasis and soil-transmitted helminthiasis in Uganda. BMC Med. 2007;5:1–11. [CrossRef]
- Kabatereine NB, Brooker S, Koukounari A, Kazibwe F, Tukahebwa EM, Fleming FM, et al. Impact of a national helminth control programme on infection and morbidity in Ugandan schoolchildren. Bull World Health Organ. 2007;85(2):91–9.
- Koukounari A, Gabrielli AF, Touré S, Bosqué-Oliva E, Zhang Y, Sellin B. Schistosoma haematobium infection and morbidity before and after large-scale administration of praziquantel in Burkina Faso. J Infect Dis. 2007;196(5):659–69. [CrossRef]
- Tohon ZB, Mainassara HB, Garba A, Mahamane AE, Bosqué-Oliva E, Ibrahim ML, et al. Controlling schistosomiasis: Significant decrease of anaemia prevalence one year after a single dose of praziquantel in Nigerien schoolchildren. PLoS Negl Trop Dis. 2008;2(5):1–8. [CrossRef]
- King, C. H., & Dangerfield-Cha M. The unacknowledged impact of chronic schistosomiasis. Chronic Illn. 2008;4(1), 65–7. [CrossRef]
- WHO. Preventive chemotherapy in human helminthiasis: coordinated use of anthelminthic drugs in control interventions. Geneva World Heal Organ. 2006;
- Wiegand R, Secor W, Fleming F, al. Control and elimination of schistosomiasis as a public health problem thresholds fail to differentiate schistosomiasis morbidity prevalence in children. Open Forum Infect Dis. 2021; [CrossRef]
- WHO. Working to overcome the global impact of neglected tropical diseases - First WHO report on neglected tropical diseases. Geneva: World Heal Organ. 2010;
- WHO. Accelerating work to overcome the global impact of neglected tropical diseases - a roadmap for implementation. Geneva: World Health Organization. 2012.
- Agniwo P, Boissier J, Sidibé B, Dembélé L, Diakité A, Dabo A. Genetic profiles of Schistosoma haematobium parasites from Malian transmission hotspot areas. Parasit Vectors. 2023;1–8. [CrossRef]
- Norton, A. J., Webster, J. P., Kane, R. A. & Rollinson D. Inter-specific parasite competition: mixed infections of Schistosoma mansoni and S. rodhaini in the definitive host. ,. Parasitology. 2008;135(4), 473-484. [CrossRef]
- Webster, J. P. & Gower CMEA. Evolutionary Concepts in Predicting and Evaluating the Impact of Mass Chemotherapy Schistosomiasis Control Programmes Parasites and their Hosts. Evol Appl. 2008;1, 66–83. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).