1. Introduction
3D printing allows us to construct a three-dimensional object from a digital model. Compared with traditional subtractive manufacturing processes, 3D printing creates a complex shape or geometries that would be otherwise infeasible to construct by other technologies. With improvements in precision, accuracy and 3D printable materials, various industries have been using 3D printing technology not only to create functional prototypes, but also to make a final product for their unique applications in an efficient and cost-effective manner. In medicine and dentistry, the evolution of 3D printing technology has also transformed the delivery of clinical care and provided various applications which improve the clinical outcome.
Technological advancements have allowed clinicians to provide more patient specific medical devices. These devices are custom made based on an individual patient’s anatomy, using imaging data and 3D models to create medical appliances [
1]. There are two main types of manufacturing technology, subtractive and additive. The additive manufacturing technology, also known as, 3D printing, provides versatile and customized applications beyond those possible through subtractive milling[
2]. Researchers are exploring 3D bio-printing technology to replicate living tissues and organs for transplantation and replace damaged tissues. Some of these printing applications have also spurred a paradigm shift in dental workflows. Among the technological advances that have played a role in this development are Digital Light Processing (DLP) [
3] and Stereolithography (SLA) [
1,
3]. Other 3D printing technologies include Fused Deposition Modeling (FDM), Selective Laser Sintering (SLS), Selective Laser Melting (SLM), Photopolymer Jetting, Power Binder Printing, and Laser Bioprinting. However, due to various limitations, these 3D printing technologies have limited usage in dentistry.
The most commonly used material in 3D printing technology is light-cured resin. The curing resin techniques have been most influential in shaping the trajectory of practical dental 3D printing procedures [
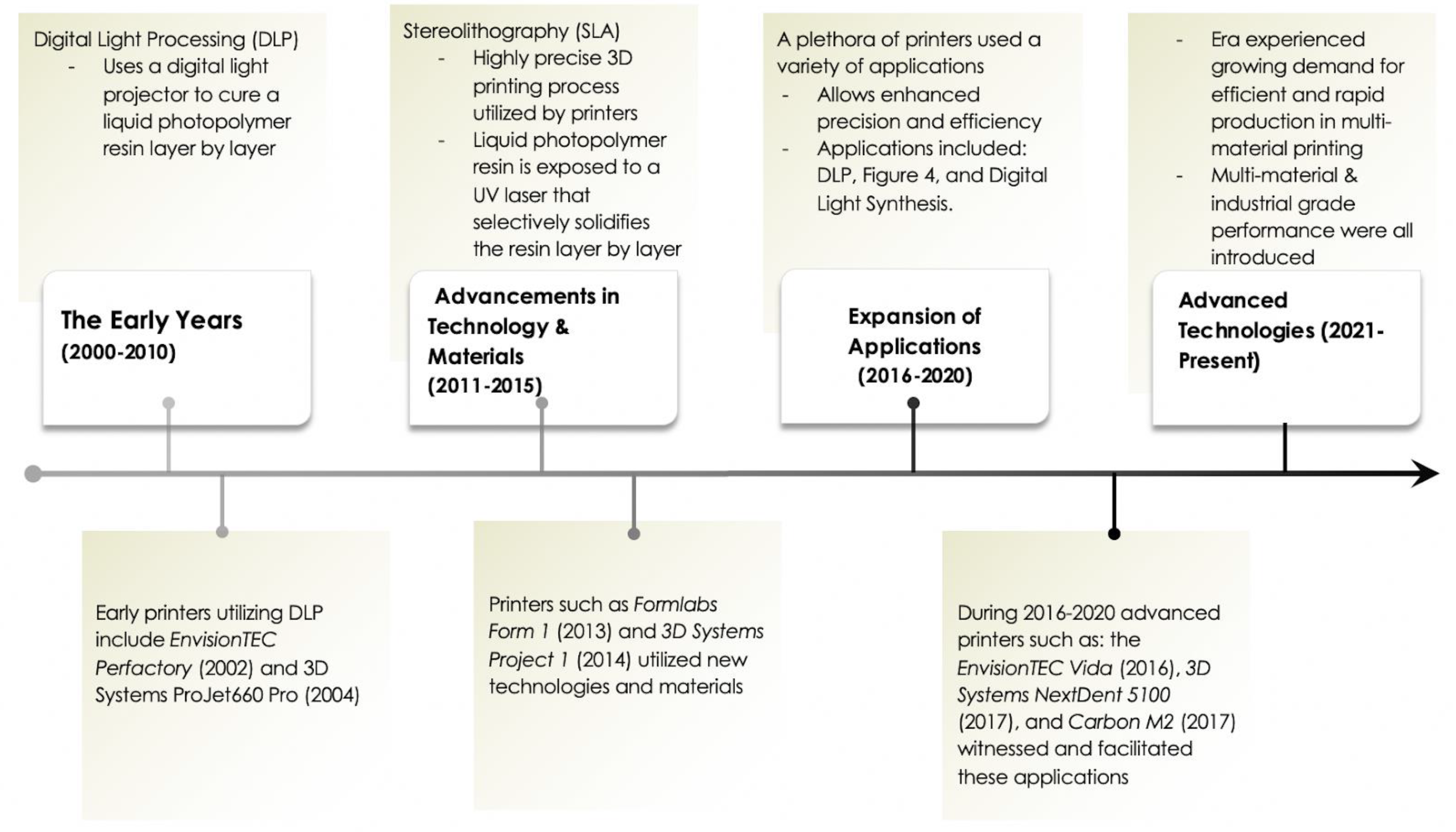
4]. The chronological development of curing techniques are divided into four time periods. The Early Years (2000-2010), is the beginning of Digital Light Processing (DLP) technology [
3]. The mechanism introduced the process of precision layer-by-layer printing [
5,
7]. The second phase, "Advancements in Materials and Technologies (2011-2015)", utilized the Stereolithography (SLA) technique, bringing high-resolution dental models into focus [
8]. Continuing with, the period of "Expansion of Applications (2016-2020)," marked by the introduction of the DLP 3D printer that expands a wider range of dental applications [
2].
The current era, "Advanced Technologies and Larger Platforms (2021-Present)," witnessed the unfolding of large-format dental 3D printing. This is designed for high-throughput production of dental models and appliances [
5,
8] and multi-material capabilities, providing dedication to dental and medical-grade applications [
6].
From previously established 3D printing mechanisms, we aim to chronicle the evolution of DLP and SLA technologies within the dental 3D printing landscape, highlighting their vital role in transforming not only dentistry but also the broader medical field [
9,
10]. These techniques have not only advanced in terms of precision and material diversity, but have also opened new avenues for medical applications as a whole [
1].
This paper will review the mechanisms of 3D printing technologies and how this technology has been applied in dentistry alongside the development of printable dental materials. Additionally, an overview of unique applications for 3D printing within different dental specialties will provide a holistic perspective on the impact of this technology in the dental field.
Figure 1.
Historical timeline of 3D printing.
Figure 1.
Historical timeline of 3D printing.
2. 3D Printing Technologies
There are different mechanisms for how 3D printing technologies work. Depending on its 3D printing mechanism, the product has unique features which fit the use.
Table 1 summarizes the advantages and disadvantages of various 3D print technologies.
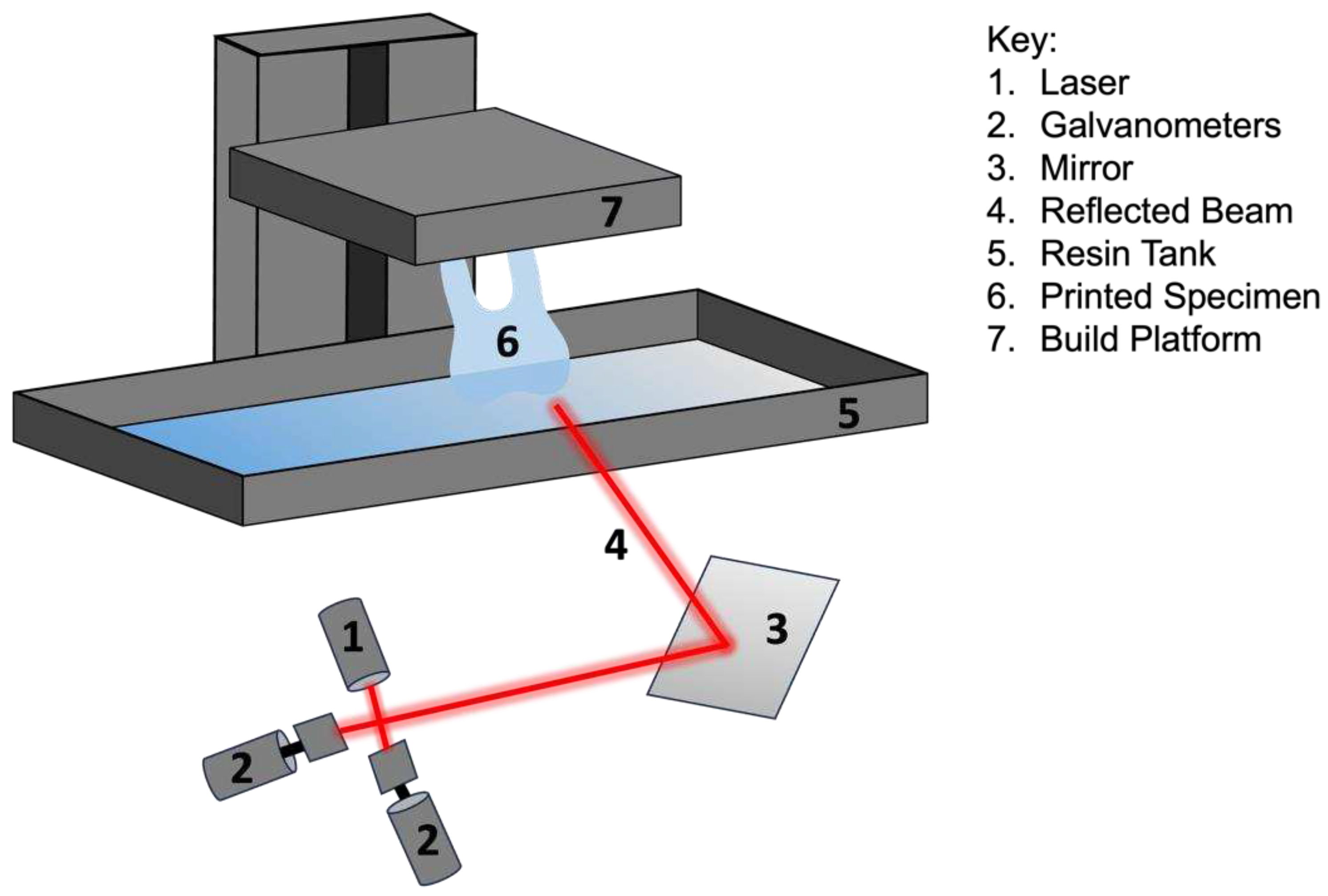
2.1. Stereolithography (SLA)
Stereolithography (SLA) has proven to be a 3D printing technology with numerous applications, speed, and high accuracy. SLA utilizes photochemical processes to cure liquid resins layer by layer, resulting in highly accurate and finely detailed designs [
11]. The beam curing capability of SLA technology is time consuming but leads to highly accurate and smooth final products [
11]. The technology's ability to produce custom, patient-specific designs has developed significant interest within the dental community. As referenced in
Table 1, SLA produces highly accurate designs and is often utilized in dentistry for temporary and permanent crown and fixed partial denture work, surgical guides, and templates as well as diagnostic casts and models [
12]. One of the major downsides of the technology is that since the cured material follows a laser beam, the process can be time consuming even for small designs [
11]. SLA technology in dentistry has largely paved the way for a more efficient and less time-consuming approach to dental care.
Figure 2.
Diagram of stereolithography (SLA) technology.
Figure 2.
Diagram of stereolithography (SLA) technology.
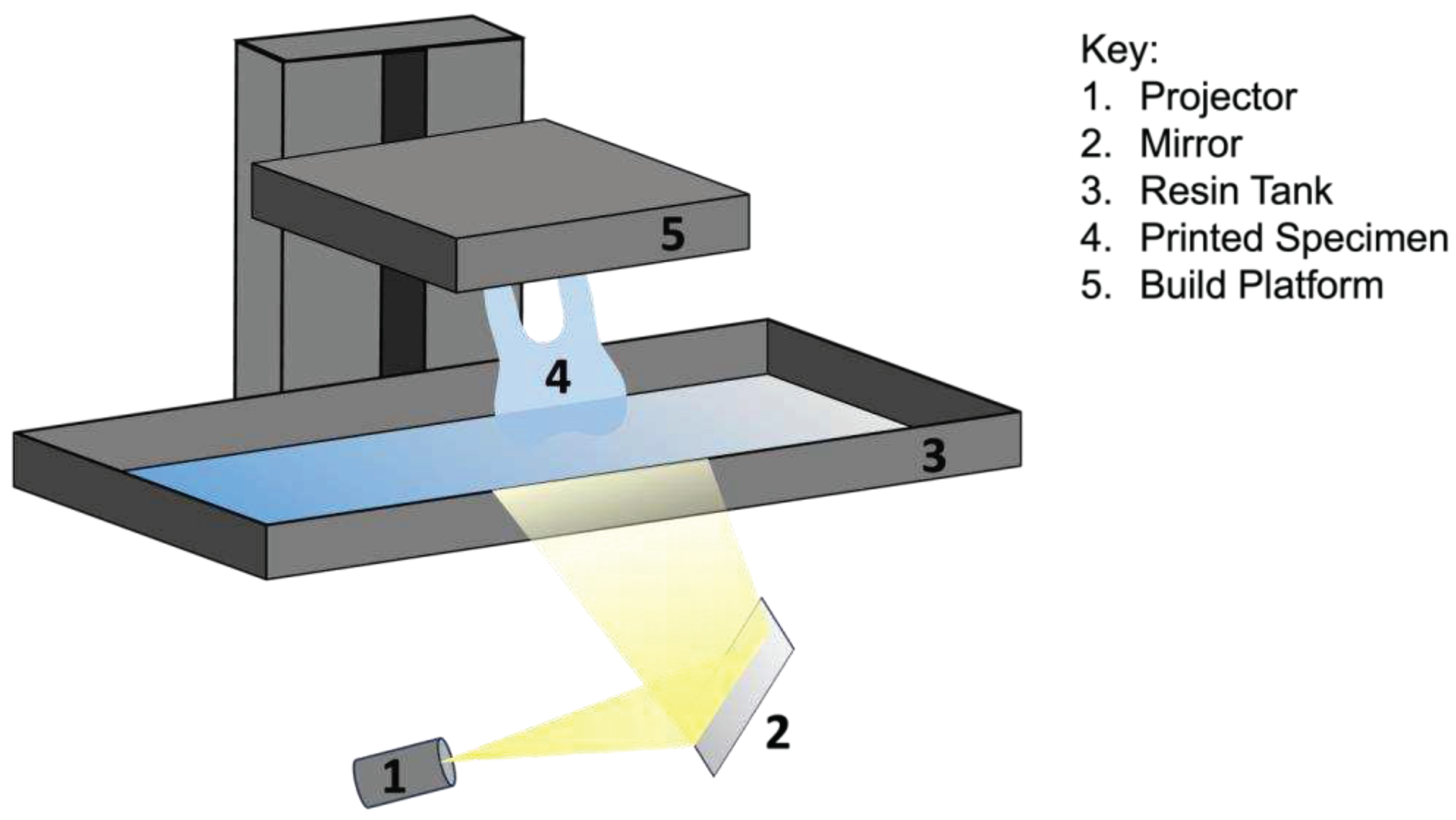
2.2. Digital Light Processing (DLP)
Digital Light Processing (DLP) printing has emerged as an immensely valuable 3D printing technology solving the issues of long fabrication durations [
13]. DLP utilizes a light source to cure photopolymer resins layer by layer, resulting in highly precise and intricate designs [
14]. This light curing technology solves the issue of slower speeds seen in SLA printing, as DLP can cure an entire layer with one flash of light. The large disadvantage of this technology, though, exists around the size of each voxel. A voxel is essentially what a ‘pixel’ is to resolution, except in a 3D perspective [
15]. Therefore, the larger voxel size would lead to lower resolutions (blockier and squarer) while smaller voxels would lead to higher resolutions (smoother design) [
15]. DLP printing currently produces clinically acceptable crown and fixed partial denture temporary and permanent restorations as well as removable prosthetic devices [
12]. Overall, DLP printing offers clinicians innovative time saving solutions for more predictable treatment outcomes.
Figure 3.
Diagram of digital light processing (DLP) technology.
Figure 3.
Diagram of digital light processing (DLP) technology.
2.3. Fused Deposition Modeling (FMD)
Fused Deposition Modeling (FDM) is a useful printing modality with applications in many areas of health care. FDM utilizes thermoplastic filaments that are extruded once heated at a semi-solid state and deposited layer by layer [
16]. The layers will harden when cooled yet will form a molecular bond with the heated filament as they are deposited onto the previous layer [
16]. The technology provides great bonding of the material layers but only works with thermoplastic materials (
Table 1). Currently, this technology has been used to produce occlusal appliances and has also been used in pharmaceutical applications, such as controlled released drug delivery systems [
12]. While Fused Deposition Modeling provides useful applications throughout various healthcare settings its use in dental applications is limited.
2.4. Selective Laser Sintering (SLS)
Selective Laser Sintering (SLS) has proven to be a large time-saving 3D printing modality within the realm of prosthodontics. SLS utilizes a high-temperature laser to selectively fuse powdered materials [
17]. The materials are wide ranging from ceramics to metals and even polymers [
17]. This provides very useful as it is one of the only modalities that can produce high density materials for dental applications [
17]. The main disadvantage of this technology is that it requires a large infrastructure for proper printing [
1]. SLS has demonstrated significant uses in dentistry in the fabrication of removable partial denture frameworks, which significantly reduces human error from traditional techniques [
12]. Selective Laser Sintering provides a safer and more predictable outcome when compared to traditional casting of metal in dental applications. An alternative to SLS printing is selective laser melting (SLM). The SLM printing modality is comparable to SLS printing through materials and processes, with the major difference being that in SLM, the material will be fully melted rather than sintered [
18].
2.5. Photopolymer Jetting
Photopolymer jetting printing, commonly referred to as PolyJet 3D printing, provides a unique advantage to dentistry, namely the ability to print in multiple colors. PolyJet utilizes inkjet printheads to dispense droplets of fusing agent on multiple voxels of a powder bed [
19]. This process will cause the polymer powder to melt and then be cured through infrared lights [
19]. The technology's ability to create multi-material and multi-color components yields huge advantages to other printing modalities. One of the major disadvantages revolves around the necessity of maintenance of the print heads, as they can clog easily [
1]. Currently, PolyJet printing has displayed uses for the fabrication of dental models as well as temporary crowns [
12]. The material does not currently provide great mechanical properties and for that reason possesses limited advantages in the oral environment [
12]. Photopolymer jetting printing holds tremendous promise for revolutionizing the dental industry by providing multiple color options during a print, which is highly valued in esthetic dentistry.
2.6. Powder Binder Jetting
Powder binder printing, also known as binder jetting, displays a useful modality for maxillofacial prostheses involving medical grade silicones and biocompatible elastomers [
20]. Binder jetting often employs a water-based binder to selectively bond layers of starch-based powdered which is then infiltrated with silicone polymers [
20]. The resulting material then experiences post processing to harden the material into acceptable properties [
20]. The technology's capability to produce patient-specific and color matched maxillofacial designs is unmatched. These materials often have weaker mechanical properties and, as a result, are delicate [
1]. As stated previously, the powder binder jetting provides an extremely early and revolutionary solution to patient specific maxillofacial applications [
12]. Powder binder printing holds great promise in advancing dental manufacturing processes involving a less invasive production process for this unique patient population.
2.7. Laser Bioprinting (LAB)
3D laser bioprinting (LAB) entered the markets as an innovative amalgam of additive manufacturing and biotechnology. This modality has displayed excellent advancements for dental regenerative therapies. LAB printing utilizes precise laser-based techniques, which enable the layer-by-layer deposition of bioinks, including living cells and various types of biomaterials [
21]. This innovative technology developed printing in the field of producing tissue-engineered constructs for periodontal regeneration, bone augmentation, and oral mucosal reconstruction [
21]. Overall, 3D laser bioprinting holds remarkable promise in reshaping the landscape of dental therapies, offering clinicians innovative tools to engineer patient-specific, regenerative solutions for complex oral and maxillofacial challenges with the potential to enhance patient well-being and quality of life.
3. Dental Materials in 3D print technology
Printable dental materials are rapidly advancing with research focused on the development of additive manufacturing (AM) printing parameters to fine-tune the mechanical properties of conventionally used materials. In
Table 2, a summary is provided of some common 3D printed materials and their measured properties compared to their comparable conventional counterparts. The main printable materials can be categorized into synthetic polymers, metals, and ceramics.
3.1. Synthetic Polymers
Polymers are the most common materials used for dental applications due to the low cost and diverse properties and capabilities. Examples of polymers include polyether ether ketone (PEEK), polycaprolactone (PCL), polymethyl methacrylate (PMMA), polylactic acid (PLA), poly (lactic-co-glycolic acid) (PLGA), and ultraviolet (UV) resins. In a systematic review of in vitro studies, Valenti et al. [
29] found that the mechanical properties of AM-printed polymeric materials were generally lower than those of materials produced by the conventional methods. Wesemann et al. [
30] investigated the wear resistance and mechanical properties of AM-printed occlusal appliances compared to the conventional injection molding method and found that there was a significant difference between their mechnial properties. Prpic´ et al. [
27] investigated the mechanical properties of AM-printed PMMA compared to conventional heat-polymerized and injection pressing PMMA, as used for denture bases. The authors found that although the AM-printed group had the lowest flexural strength, it still met the ISO requirement of 65 MPa.
3.2. Metals
The mechanical properties of titanium (Ti) and cobalt-chromium (Co-Cr) alloys are ideal for many dental applications. A review by Revilla-Leon et al. [
28] compared different printed alloys with conventional casting methods. The authors found that while the mechanical properties were satisfactory, improvements between the 3D printed metals and ceramic interfaces are required to match the precision obtained with conventional casting methods . Previous studies have noted higher hardness values for 3D-printed CoCr metal alloys (371 ± 10 HV) compared to conventional casting methods
1. In general, an increase in fit accuracy is reported in AM-printed removable partial denture metal clasps, compared to conventional casting methods [
29].
Table 2.
Summary of mechanical properties for oral tissue, common AM-printed materials, and conventional dental materials.
Table 2.
Summary of mechanical properties for oral tissue, common AM-printed materials, and conventional dental materials.
| Materials |
Density (g/cm3) |
Martens Hardness (N/mm2) |
Vickers Hardness (GPa) |
Tensile Strength (MPa) |
Elastic Modulus (GPa) |
Bending Strength (MPa) |
| Cortical bone* [27] |
1.92 |
NP |
NP |
104-121 |
6-30 |
225 |
| Dentin* [27] |
NP |
468.2 ± 30.8 |
NP |
104 |
12-18.6 |
NP |
| Dental enamel [27] |
NP |
2263.6 ± 405.2 |
NP |
47.5 |
40-83 |
NP |
| PEEK* [27] |
1.3 |
189.55 ± 16.89 |
NP |
87.53–100 |
3-4 |
99.25–170 |
| PEEK, FDM [27] |
NP |
NP |
NP |
97.34 |
2.6-3.45 |
104.65 |
| PMMA* [27,31] |
1.18 |
180 |
19.9 ± 1.0 |
NP |
2.3 ± 0.3 |
85 ± 16 |
| PMMA, SLA [31] |
NP |
NP |
18.1 ± 1.0 |
NP |
1.2 ± 0.3 |
95 ± 9 |
| PMMA, DLP [31] |
NP |
NP |
14.7 ± 1.5 |
NP |
0.7 ± 0.2 |
37 ± 6 |
| PLA* [25] |
1.25 |
NP |
NP |
59 |
3500 |
106 |
| PLA, FDM [25] |
NP |
NP |
NP |
28-48 |
2000 |
NP |
| Ti* [27] |
4.5 |
300-400 |
NP |
954-976 |
102-110 |
NP |
| Ti, SLS [29] |
4.42 |
NP |
38 |
1089 |
129 |
NP |
| CoCr* [27] |
6.5 |
1200 |
350 |
680 |
205 |
800-1400 |
| CoCr, SLS [29] |
8.3 |
NP |
350-450 |
1100 |
200 |
NP |
| ZrO2 * [26] |
NP |
5000-15000 |
NP |
115-711 |
100-250 |
177-1000 |
| ZrO2, SLA [26] |
5.97 |
NP |
12.6 |
NP |
209.4 |
300-1000 |
| Al2O3* [26] |
NP |
22000 |
NP |
267 |
380 |
500 |
| Al2O3, SLA [26] |
NP |
NP |
NP |
NP |
NP |
271.7-273.8 |
3.3. Ceramics
Ceramic materials are considered a favorable material for dental restorations due to their excellent mechanical properties, biocompatibility, good abrasion and corrosion resistance, and esthetic properties. This category can be further divided into glass, zirconia, and alumina ceramics. A challenge with 3D printing ceramics is inherent to the high melting points and introduction of cracks during the cooling processes. Additionally, the characteristic of the raw materials affects the porosity and final mechanical properties. For AM-printed ceramics, the reports of mechanical properties are inconsistent [
29]. This is largely due to the different types of ceramic materials, variability in prosthetic use, and printing parameters
4. This category of dental materials is a prime example of an area where further laboratory and clinical investigation is required to achieve widespread use.
4. Applications of 3D Printing in Dentistry
3D printing has brought new applications along with the advancement of dental materials. The versatile applications have provided more predictable clinical outcomes with precision and accuracy in many dental specialties.
Table 3 summarizes the unique applications of 3D printing in various dental specialties.
4.1. Prosthodontics
4.1.1. Crown and fixed partial denture (FPD)
3D printing has always been a technology of great interest in the field of prosthodontics. This has become more apparent recently with 3D printing technologies, such as SLA and DLP, becoming more widely utilized to fabricate provisional or definitive crowns and FPDs (
Table 3). Precise virtual models are prepared by scanning prepared teeth and implant scan bodies intraorally. Computer-aided design (CAD) software is used to design the prostheses on these virtual models. Then, the designed prostheses are printed using a 3D printer. Compared to traditional methods or milling technology for fabricating crowns and FPDs, a low-cost 3D printer can fabricate precise restorations using less materials with a shorter production time [
10,
31,
32]. Some studies have even reported that provisional crowns fabricated using 3D printing are more accurate (better edges and better internal fit) than the ones fabricated using traditional or milling methods [
33,
34,
35].
4.1.2. Complete and removable partial denture (RPD)
Although there have been significant improvements in denture material and techniques, the denture fabrication process can be challenging in patients with a severe gag reflex, tumor resection, temporomandibular joint disease, or oral deformities [
37,
38]. With the advent of intraoral scanning technology and 3D printing, denture fabrication has become a patient friendly procedure with shorter production time [
39]. It also reduces traditional laboratory steps, which can lead to fewer inherent errors and better adaptability [
40,
41]. The traditional process of waxing and investing RPD frameworks is time-consuming, technique-sensitive, and cumbersome. Wax and cast distortion from this traditional process can lead to poor fit of framework, pressure-induced mucosal lesions, and ridge resorption [
42]. A recent in-vitro study showed that RPD frameworks fabricated by SLM printing resulted in a better fit than traditional lost-wax and metal casting techniques [
43]. Another author also reported that 3D printed frameworks provide more uniform contact pressure, which can reduce the risk of residual ridge resorption [
10].
4.2. Implantology
The application of 3D printing technology in implantology serves to optimize and simplify surgical procedures with higher accuracy and predictability, thereby reducing surgical risks and improving efficiency. Traditional surgical guides are usually designed based on 2-dimensional panoramic radiographs, which often lead to inaccuracy due to distortion and insufficient resolution of the radiographic image. With the introduction of advanced digital technology, surgical guides are now designed using CAD software based on cone beam computed tomography (CBCT) and intraoral scans, then printed using a 3D printer. With this technology, the accuracy of these 3D-printed surgical guides have significantly improved. Tahmaseb et al compared and found a significant difference between the accuracy of traditional surgical guides and 3D-printed surgical guides that were printed by SLA printers [
44]. For traditional surgical guides, the average distance deviations at the entrance and at the vertex were 2.1mm and 1.5mm, respectively [
44]. Meanwhile, the average distance deviations at the entrance and at the vertex of the 3D-printed surgical guide were 0.9 and 1.0 mm, respectively [
44]. Other advantages of 3D printing surgical guides over traditional ones are lower investment cost, shorter surgical time, simpler surgical process, and better adaptation to the patient’s geometry [
45,
46].
4.3. Oral and Maxillofacial
4.3.1. Surgical guides and templates
Additive manufacturing technology has been used for three decades in the oral and maxillofacial field of dentistry for model fabrication, diagnosis, surgical planning, surgical guide and template fabrication, and custom implants manufacturing [
47,
48]. Similar to the 3D-printed surgical guide for implant surgery, surgical guides and templates are designed based on the obtained CT image and CAD software analysis of the maxillomandibular defect. A 3D printed guide in combination with a 3D-printed patient-specific titanium template provides stability during the operation and ensures the precise placement of bone segments [
49]. In addition, these guides and templates result in less defects, higher accuracy, better margin control, and bone compromises [
47].
4.3.2. Custom implants
The capability of 3D printing technology to design and print complex geometries has been used to fabricate custom dental implants. 3D printers, such as SLS and SLM, have the ability to print in titanium or in implantable polymer, particularly polyether ether ketone to fabricate dental implants with adjustable porosity and mechanical properties [
50].
However, 3D printing technology is still often used in conjunction with conventional pressing and milling technologies to fabricate implants, because pressing and milling have their advantages as well, such as reduced post-processing, fast production, and predictable use of uniform and homogenous materials [
1].
4.3.3. Maxillofacial prostheses
Often, maxillofacial defects are complex in shape and size, and 3D printing technology can be extremely beneficial in fabricating prostheses for these defects due to its ability to print complex geometrics. A combination of scanning technology and 3D printing is more comfortable for patients and provides a prosthesis with higher accuracy and better fit to the defect area [
47,
51]. Other benefits of implementing 3D printing technology include reduced manufacturing time, decreased number of appointments, and repeatability allowing multiple prostheses [
52].
4.4. Orthodontics
Nowadays, in orthodontics, 3D printing technology is primarily used to fabricate orthodontic aligners for treating malocclusion. The removable, clear aligners are an alternative to conventional orthodontic braces, with improved oral hygiene and esthetics [
53].
Previously, 3D printing technologies such as SLA or FDM were used only for printing models, and the aligners were produced by a thermoforming process using thermoplastic materials [
53]. However, the thermoforming procedure itself as well as the intraoral environment can alter the properties of the material, which eventually affect the overall performance [
54].
More recently, direct 3D-printed aligners have become more popular, offering a better fit, higher efficacy, and reproducibility, without altering material properties [
55]. Tartaglia et al reported that the use of 3D direct printed aligners is a more stable way to align the teeth than thermoformed manufactured aligners due to higher accuracy, higher load resistance, and lower deformation [
55].
4.5. Endodontics
3D printing technology has been applied to every field of dentistry, and endodontics is not an exception. In endodontics, 3D printing technology has been served for various purposes, including access cavity preparation, apicoectomy, autotransplantation, education and training [
56]. There are many studies reporting high accuracy of guided cavity preparation using 3D-printed access guide [
57,
58,
59]. Buchgreitz et al reported the mean deviation of access cavities lower than 0.7mm [
57]. Similarly, Zehnder et al and Connert et al reported small deviations of 0.12-0.34mm from the intended access and a mean angular deviation of less than 2 degrees [
58,
59].
Guided apicoectomy, endodontic microsurgery (EMS), requires a 3D-printed surgical guide to perform targeted osteotomy and root resection. As in other specialties, the surgical guide is designed and printed based on CBCT and CAD software. This application of 3D printing technology results in higher accuracy of osteotomies than the traditional free-hand technique [
56,
60,
61]. In addition, the 3D-printed guide for apicoectomy allows for easier inspection of root apices, smaller osteotomies, lower risk of nerve or sinus perforation, better root-end preparation, better healing, and shorter surgical time [
56,
60,
61].
4.6. Periodontics
4.6.1. Scaffolds for hard and soft tissue regeneration
Application of 3D printing in periodontics is useful for both hard and soft tissue regeneration as well as guided gingivectomy. There has been a lot of research focusing on fabrication of 3D-printed scaffolds for hard and soft tissue regeneration. The concept of additive biomanufacturing using 3D printing technology serves to restore the resorbed periodontal tissue and bone deficiencies in a customized manner[
47].
3D printing enables the custom printing of scaffolds that can be loaded with stem cells, where the stem cells can be placed at precise locations, allowing more intimate contact with bone surfaces [
62]. These advantages can lead to a better healing process and better esthetic results than conventional scaffolds [
47]. 3D printing can also be used for soft tissue regeneration. Recently, 3D printed soft tissue grafts have been developed for keratinized tissue augmentation. These printed soft tissue grafts can cover larger and more complicated defects with high accuracy, without being limited by donor site availability [
63].
4.6.2. Gingivectomy surgical guide
A common application of 3D printing in periodontics is the use of a surgical guide for gingivectomy and smile designing [
47]. With the help of intraoral scanning and CAD software, a patient-specific surgical guide for esthetic gingivectomy can be designed and printed. Using the surgical guide, more esthetic results can be achieved due to their accuracy, precision, and customization [
47].
5. Conclusions
This review article gives an overview of the history and evolution of 3D printing technology, as well as its associated advantages and disadvantages. Material selection and applications in dentistry have expanded significantly over the years alongside the ever evolving 3D printing technologies. This technology is now able to offer us a wide variety of potential applications in different fields of dentistry, including prosthodontics, implantology, oral and maxillofacial, orthodontics, endodontics, and periodontics. With further research being done, 3D printing will continue to elevate the quality and delivery of patient care, education, and research in the years to come.
Author Contributions
Conceptualization, S.J.L. and J.D.L.; methodology, M.J., K.R., D.L., and J.T.L.; data curation, M.J., K.R., D.L., and J.T.L.; writing-original draft preparation, M.J., K.R., D.L., and J.T.L.; writing-review and editing, M.J., S.J.L., and J.D.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V. 3D printing in dentistry. Br Dent J 2015, 219, 521–9. [Google Scholar] [CrossRef]
- Park, S.; Park, J.; Kim, S.; Heo, S.; Koak, J. Flexural strength of 3D-printing resin materials for provisional fixed dental prosthesis. Materials (Basel) 2020, 13, 3970. [Google Scholar] [CrossRef]
- Tsolakis, I.; Papaioannou, W.; Papdopoulou, E.; Dalampira, M.; Tsolakis, A. Comparison in terms of accuracy between DLP and LCD printing technology for dental model printing. Dent J 2022, 10, 181. [Google Scholar] [CrossRef]
- Tsolakis, I.; Gizani, S.; Panayi; Antonopoulos, G. Three-dimensional printing technology in orthodontics for dental models: a systematic review. Children (Basel) 2022, 9, 1106. [Google Scholar] [CrossRef]
- Rungrojwittayakul, O.; Kan, J.; Shiozaki, K.; Swamidass, R.; Goodacre, B.; Goodacre, C.; Lazada, J. Technologies of printers with different designs of model base. J Prosthodont 2020, 29, 124–8. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Peng, T.; Lin, Y.; Zhang, M.; Ren, G. Effect of internal structures on the accuracy of 3D printed full-arch dentition preparation models in different printing systems. J Adv Prosthodont 2023, 15, 145–54. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Guth, J. 3D printing in digital prosthetic dentistry: an overview of recent developments in additive manufacturing. J Clin Med 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Muzaffar, A.; Zafar, H. Application of 3D printing technology in dentistry: a review. Saudi J Dent Research 2018. [Google Scholar]
- Moser, N.; Santander, P.; Quast, A. From 3D imaging to 3D printing in dentistry- a practice guide. Int J Comput Dent 2018, 21, 345–6. [Google Scholar]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.; Jiang, H. A review of 3D printing in dentistry: technologies, affecting factors, and applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: a systematic review. Dent Mater 2021, 37, 336–50. [Google Scholar] [CrossRef]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; Mohammadinejad, R.; Shabani, M.; Mazzolai, B.; Mattoli, V.; Tay, F.R.; Makvandi, P. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater 2021, 122, 26–49. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al-Rashdan, B.A.; Ayyad, J.Q.; Al Omrani, L.M.; Sharoh, A.M.; Al Nimri, A.M.; Al-Kaff, F.T. Additive Manufacturing of Dental Ceramics: A Systematic Review and Meta-Analysis. J Prosthodont 2022, 31, e67–86. [Google Scholar] [CrossRef] [PubMed]
- SLA vs. DLP: Guide to resin 3D printers. Available online: https://formlabs.com/blog/resin-3d-printer-comparison-sla-vs-dlp/ (accessed on 07 July 2023).
- The main benefits and disadvantages of Voxel Modeling. Available online: https://blog.spatial.com/the-main-benefits-and-disadvantages-of-voxel-modeling (accessed on 07 July 2023).
- Cailleaux, S.; Sanchez-Ballester, N.M.; Gueche, Y.A.; Bataille, B.; Soulairol, I. Fused Deposition Modeling (FDM), the new asset for the production of tailored medicines. J Control Release 2021, 10, 821–41. [Google Scholar] [CrossRef]
- Yang, J.; Li, H.; Xu, L.; Wang, Y. Selective laser sintering versus conventional lost-wax casting for single metal copings: A systematic review and meta-analysis. J Prosthet Dent 2022, 128, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Goguta, L.; Lungeanu, D.; Negru, R.; Birdeanu, M.; Jivanescu, A.; Sinescu, C. Selective Laser Sintering versus Selective Laser Melting and Computer Aided Design - Computer Aided Manufacturing in Double Crowns Retention. J Prosthodont Res 2021, 65, 371–8. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhao, L.; Zhou, K. Multi-Jet Fusion 3D Voxel Printing of Conductive Elastomers. Adv Mater 2022, 34, e2205909. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Zheng, J.; Kuo, J.; Acosta-Vélez, G.F.; Linsley, C.S.; Wu, B.M. Binder Jetting of Custom Silicone Powder for Direct Three-Dimensional Printing of Maxillofacial Prostheses. 3D Print Addit Manuf 2022, 9, 520–34. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.H.; Lee, J.; Park, S.A.; Kim, W.D. Three-dimensional bio-printing equipment technologies for tissue engineering and regenerative medicine. Tissue Eng Regen Med 2016, 13, 663–76. [Google Scholar] [CrossRef]
- Al Jabbari, Y.S.; Koutsoukis, T.; Barmpagadaki, X.; Zinelis, S. Metallurgical and Interfacial Characterization of PFM Co–Cr dental alloys fabricated via casting, milling or selective laser melting. Dent Mater 2014, 30, e79–88. [Google Scholar] [CrossRef]
- Dehurtevent, M.; Robberecht, L.; Hornez, J.-C.; Thuault, A.; Deveaux, E.; Béhin, P. Stereolithography: A new method for processing dental ceramics by additive computer-aided manufacturing. Dent Mater 2017, 33, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Farah, S.; Anderson, D.G.; Langer, R. Physical and mechanical properties of PLA, and their functions in widespread applications — a comprehensive review. Adv Drug Deliv Rev 2016, 107, 367–92. [Google Scholar] [CrossRef] [PubMed]
- Galante, R.; Figueiredo-Pina, C.G.; Serro, A.P. Additive Manufacturing of ceramics for Dental Applications: A Review. Dent Mater 2019, 35, 825–46. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Liu, Y.; Peng, B.; Chen, M.; Liu, Z.; Li, Z.; Kuang, H.; Gong, B.; Li, Z.; Sun, H. Peek for oral applications: Recent advances in mechanical and adhesive properties. Polymers 2023, 15. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; & Čimić, S. Comparison of mechanical properties of 3d-printed, CAD/CAM, and conventional denture base materials. J Prosthodont 2020, 29, 524–8. [Google Scholar] [CrossRef]
- Revilla-León, M.; & Özcan, M. Additive Manufacturing Technologies used for 3D Metal Printing in Dentistry. Current Oral Health Reports 2017, 4, 201–8. [Google Scholar] [CrossRef]
- Valenti, C.; Isabella Federici, M.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. The J Prosthet Dent 2022, S0022-3913(22)00415-2. [Google Scholar] [CrossRef]
- Wesemann, C.; Spies, B.C.; Sterzenbach, G.; Beuer, F.; Kohal, R.; Wemken, G.; Krügel, M.; Pieralli, S. Polymers for conventional, subtractive, and additive manufacturing of occlusal devices differ in hardness and flexural properties but not in wear resistance. Dent Mater 2021, 37, 432–42. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A. Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventional cured provisional crown and bridge dental materials. Dent Mater 2018, 34, 192–200. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent Mater 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Mai, H.N.; Lee, K.B.; Lee, D.H. Fit of interim crowns fabricated using photopolymer jetting 3D printing. J Prosthet Dent 2017, 118, 208–15. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.S.; Lee, D.H.; Lee, K.B. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J Adv Prosthodont 2017, 9, 265–70. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, S.; Alqahtani, N.M.; Addas, M.K.; Alfarsi, M.A. Marginal and internal fit of provisional crowns fabricated using 3D printing technology. Technol Health Care 2020, 28, 635–42. [Google Scholar] [CrossRef]
- Freedman, G.A. Contemporary esthetic dentistry-e-book; Elsevier Health Sciences: Toronto, ON, USA, 2001. [Google Scholar]
- Hacker, T.; Heydecke, G.; Reissmann, D.R. Impact of procedures during prosthodontic treatment on patients’ perceived burden. J Dent 2015, 43, 51–7. [Google Scholar] [CrossRef] [PubMed]
- Kim, J-E; Kim, N-H; Shin, J-S. Fabrication of complete, removable dental prosthesis from a digital intraoral impression for a patient with excessively tight reconstructed lip after oral can treatment: a clinical report. J Prosthet Dent 2017, 117, 205–208. [Google Scholar] [CrossRef]
- Hu, F.; Pei, Z.; Wen, Y. Using intraoral scanning technology for three-dimensional printing of Kennedy class I removable partial denture metal framework: a clinical report. J Prosthdont 2017, 1–4. [Google Scholar] [CrossRef]
- Gan, N.; Ruan, Y.; Sun, J.; Xiong, Y.; Jiao, T. Comparison of adaptation between the major connectors fabricated from intraoral digital impression and extraoral digital impressions. Sci. Rep 2018, 8, 529. [Google Scholar] [CrossRef]
- Yoon, S.N.; Oh, K.C.; Lee, S.J.; Han, J.S.; Yoon, H.I. Tissue surface adaptation of CAD-CAM maxillary and mandibular complete denture bases manufactured by digital light processing: a clinical study. J Prosthet Dent 2020, 124, 682–9. [Google Scholar] [CrossRef]
- Bilgin, M.S.; Baytaroglu, E.N.; Erdem, A.; Dilber, E. A review of computer-aided design/computer-aided manufacture techniques for removable denture fabrication. Eur J of Dent 2016, 10, 286–91. [Google Scholar] [CrossRef]
- Bajunaid, S.O.; Altwaim, B.; Alhassan, M.; Alammari, R. The fit accuracy of removable partial denture metal frameworks using conventional and 3D printed techniques: an in vitro study. J Contemp Dent Pract 2019, 20, 476–81. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 2014, 29, Suppl:25-4. [Google Scholar] [CrossRef] [PubMed]
- Alzit, F.R.; Cade, R.; Naveau, A.; Babilotte, J.; Meglioli, M.; Catros, S. Accuracy of commercial 3D printers for the fabrication of surgical guides in dental implantology. J Dent 2022, 117, 1–9. [Google Scholar]
- Skjerven, H.; Riis, U.H.; Herlofsson, B.B.; Ellingsen, J.E. In vivo accuracy of implant placement using a full digital planning modality and stereolithographic guides. Int J Oral Maxillofac Implants 2019, 34, 124–32. [Google Scholar] [CrossRef] [PubMed]
- Oberoi, G.; Nitsch, S.; Edelmayer, M.; Janijic, K.; Muller, A.S.; Agis, H. 3D printing-encompassing the facets of dentistry. Biotechnol 2018, 6, 1–13. [Google Scholar] [CrossRef]
- Erickson, D.M.; Chance, D.; Schmitt, S.; Mathis, J. An opinion survey of reported benefits from the use of stereolithographic models. J Oral Maxillofac Surg 1999, 57, 1040–3. [Google Scholar] [CrossRef]
- Polley, J.W.; Figueroa, A.A. Orthognathic positioning system: intraoperative system to transfer virtual surgical plan to operating field during orthognathic surgery. J Oral Maxillofac Surg 2013, 71, 911–20. [Google Scholar] [CrossRef]
- Farre-Guasch, E.; Wolff, J.; Helder, M.N.; Schulten, E.; Forouzanfar, T.; Klein-Nulend, J. Application of additive manufacturing in oral and maxillofacial surgery. J Oral Maxillofac Surg 2015, 73, 2408–18. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive technology: update on current materials and applications in dentistry. J Prosthodont 2017, 26, 156–63. [Google Scholar] [CrossRef]
- Sherwood, R.G.; Murphy, N.; Kearns, G.; Barry, C. The use of 3D printing technology in the creation of patient-specific facial prostheses. Ir J Med Sci 2020, 189, 1215–21. [Google Scholar] [CrossRef]
- Martorelli, M.; Gerbino, S.; Giudice, M.; Ausiello, P. A comparison between customized clear and removable orthodontic appliances manufactured using RP and CNC techniques. Dent Mater 2013, 29, e1–10. [Google Scholar] [CrossRef]
- Gerard Bradley, T.; Teske, L.; Eliades, G.; Zinelis, S.; Eliades, T. Do the mechanical and chemical properties of Invisalign TM appliances change after use? A retrieval analysis. Eur J Orthod 2015, 38, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials (Basel) 2021, 14, 1799. [Google Scholar] [CrossRef] [PubMed]
- Buniag, A.G.; Pratt, A.M.; Ray, J.J. Targeted endodontic microsurgery: a retrospective outcomes assessment of 24 cases. J Endod 2021, 47, 762–9. [Google Scholar] [CrossRef] [PubMed]
- Buchgreitz, J.; Buchgreitz, M.; Mortensen, D.; Bjorndal, L. Guided access cavity preparation sing cone-beam computed tomography and optical surface scans – an ex vivo study. Int Endod J 2016, 49, 790–5. [Google Scholar] [CrossRef]
- Zehnder, M.S.; Connert, T.; Weiger, R.; Krastl, G.; Kuhl, S. Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J 2016, 49, 966–72. [Google Scholar] [CrossRef]
- Connert, T.; Zehnder, M.S.; Weiger, R.; Kuhl, S.; Krast, l G. Microguided endodontics: accuracy of a miniaturized technique for apically extended access cavity preparation in anterior teeth. J Endod 2017, 43, 787–790. [Google Scholar] [CrossRef]
- Strbac, G.D.; Schnappauf, A.; Giannis, K.; Moritz, A.; Ulm, C. Guided Modern endodontic surgery: a novel approach for guided osteotomy and root resection. J Endod 2017, 43, 496–501. [Google Scholar] [CrossRef]
- Kim, S.; Kratchman, S. Modern endodontic surgery concepts and practice: a review. J Endod 2006, 32, 601–23. [Google Scholar] [CrossRef]
- Salah, M.; Tayebi, L.; Moharamzadeh, K.; Naini, F.B. Three-dimensional bio-printing and bone tissue engineering: technical innovations and potentional applications in maxillofacial reconstructive surgery. Maxillofac Plast Reconstr Surg 2020, 42, 18. [Google Scholar] [CrossRef]
- Nesic, D.; Schaefer, B.M.; Sun, Y.; Saulacic, N. 3D printing approach in dentistry: the future for personalized oral soft tissue regeneration. J Clin Med 2020, 7, 2238. [Google Scholar] [CrossRef]
Table 1.
Advantages and disadvantages of each 3D printing technologies.
Table 1.
Advantages and disadvantages of each 3D printing technologies.
| 3D technology |
Advantages |
Disadvantages |
| Stereolithography (SLA) |
Quick production speed Precise and highly accurate Can accommodate complex designs Numerous material options |
|
| Digital Light Processing (DLP) |
High speed Precise and highly accurate Can accommodate complex designs Numerous material options |
|
| Fused Deposition Modeling (FDM) |
Cheaper technology Great layer bonding |
|
| Selective Laser Sintering (SLS) and Selective Laser Melting (SLM) |
|
|
| Photopolymer Jetting |
|
|
| Powder Binder Printing |
|
|
| 3D Laser Bio-Printing (LAB) |
|
|
Table 3.
Applications of 3D printing.
Table 3.
Applications of 3D printing.
| Specialty |
Applications |
Technology |
Advantages |
| Prosthodontics |
Crowns and fixed partial dentures |
SLA, DLP. Photopolymer jetting |
|
| Complete dentures |
SLA, DLP |
Patient friendly Fewer laboratory steps High accuracy Close adaptability |
| Removable partial dentures |
SLS, SLM, EBM |
Reducing manufacturing time and cost Minimizing operation errors High accuracy Good marginal fit Good mechanical properties |
| Implantology |
Surgical guide |
SLA, DLP, Photopolymer jetting |
|
| Custom tray |
SLA, FDM |
High efficiency High accuracy |
| Oral and Maxillofacial |
Surgical guide and template |
SLA, DLP, photopolymer jetting |
|
| Custom implants |
SLS, Photopolymer jetting |
|
| Maxillofacial prostheses |
SLA, Photopolymer jetting, SLS, FDM |
|
| Orthodontics |
Aligners |
SLA, DLP, FDM |
Accurate Predictable Reducing production time Saving money |
| Orthotic appliances |
SLA |
|
| Endodontics |
Surgical guide |
SLA, Photopolymer jetting |
|
| Periodontics |
Scaffolds for hard and soft tissue regeneration |
LAB |
Precise More intimate contact of scaffolds with bone surfaces Larger quantity Permitting more complicated designs Accurate Reducing post-operation discomfort |
| Gingivectomy surgical guide |
SLA, DLP, Photopolymer jetting |
Accurate Customized Precise |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).