Testicular simple cysts (SCs) are infrequent benign cystic lesions that contain clear serous fluid within the testicular parenchyma [
1]. These cysts exhibit a bimodal distribution in adults and infants, with peaks at eight months and 60 years of age [
2]. The lining of the testicular SC typically consists of a flat to cuboidal epithelium, specifically mesothelial cells [
3].
The SC has no spermatozoa and ranges from 2 to 18 mm in diameter [
2]. In the present study, we elucidated the pathological features of an SC in the right testis of an elderly Japanese man with prostatic acinar adenocarcinoma of the bilateral lobes.
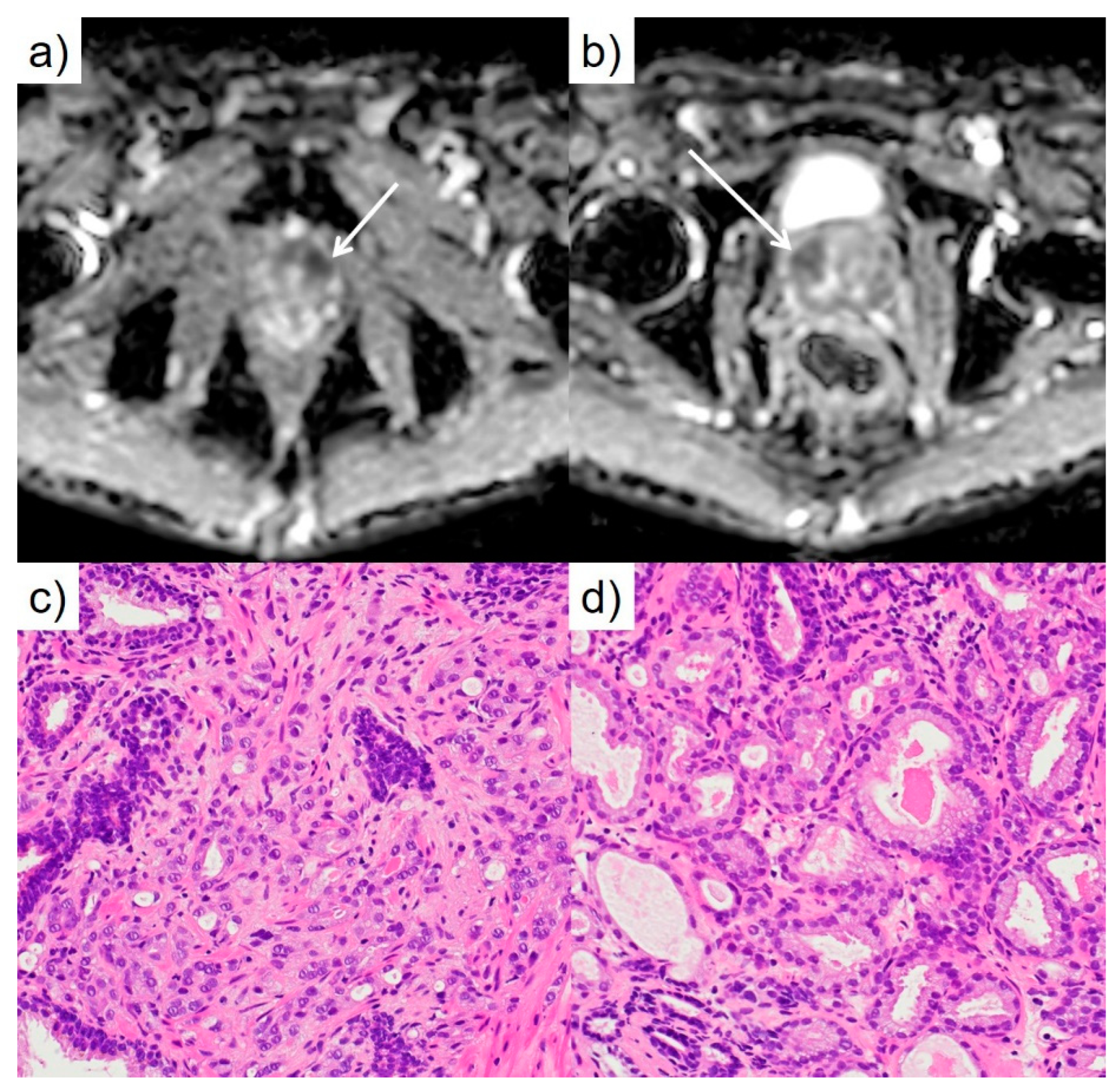
A Japanese man in his 90s regularly visited our hospital and was referred from another hospital with dysuria and high prostatic specific antigen. Laboratory findings on admission showed elevated prostatic specific antigen (27.4ng/mL). Magnetic resonance image revealed a broad capsular lesion in the bilateral transition zone (
Figure 1a, b). The results of the prostatic needle biopsies revealed prostate cancer (PC), prostatic acinar adenocarcinoma, and Grade group 3 of the bilateral lobes (7/7) (
Figure 1c, d).
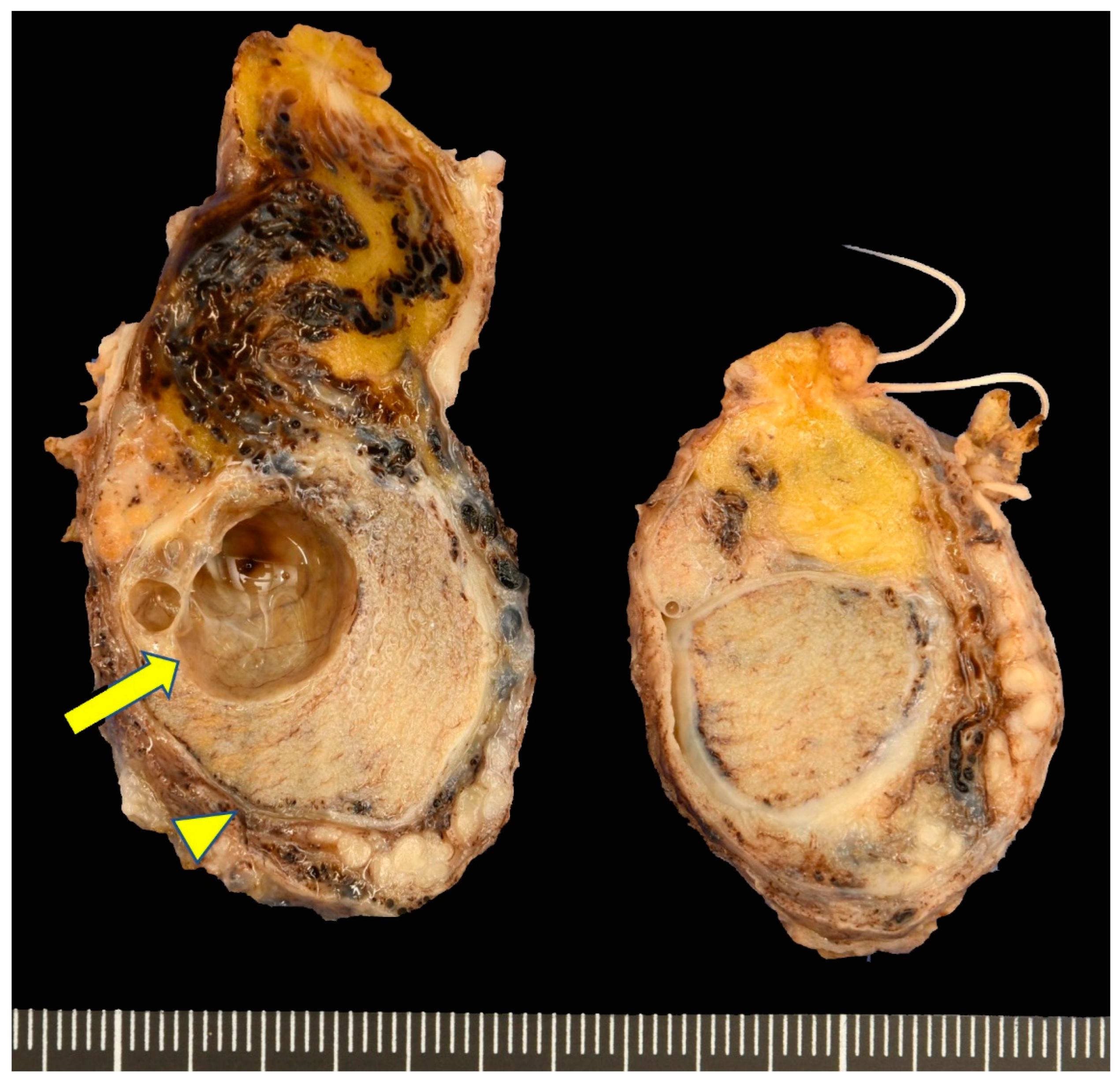
Testes measured 6.5×3.5×2.1 cm in size, 22 g in weight (right) and 4.5×3.0×2.3 cm in length, 16 g in weight (left). Hemisection of the right testis revealed a unilocular cyst within the parenchyma (
Figure 2, arrow). The cyst measured 16×15 mm in size. The cystic fluid was serous, yellow and transparent. No significant abnormalities were observed in the left testes.
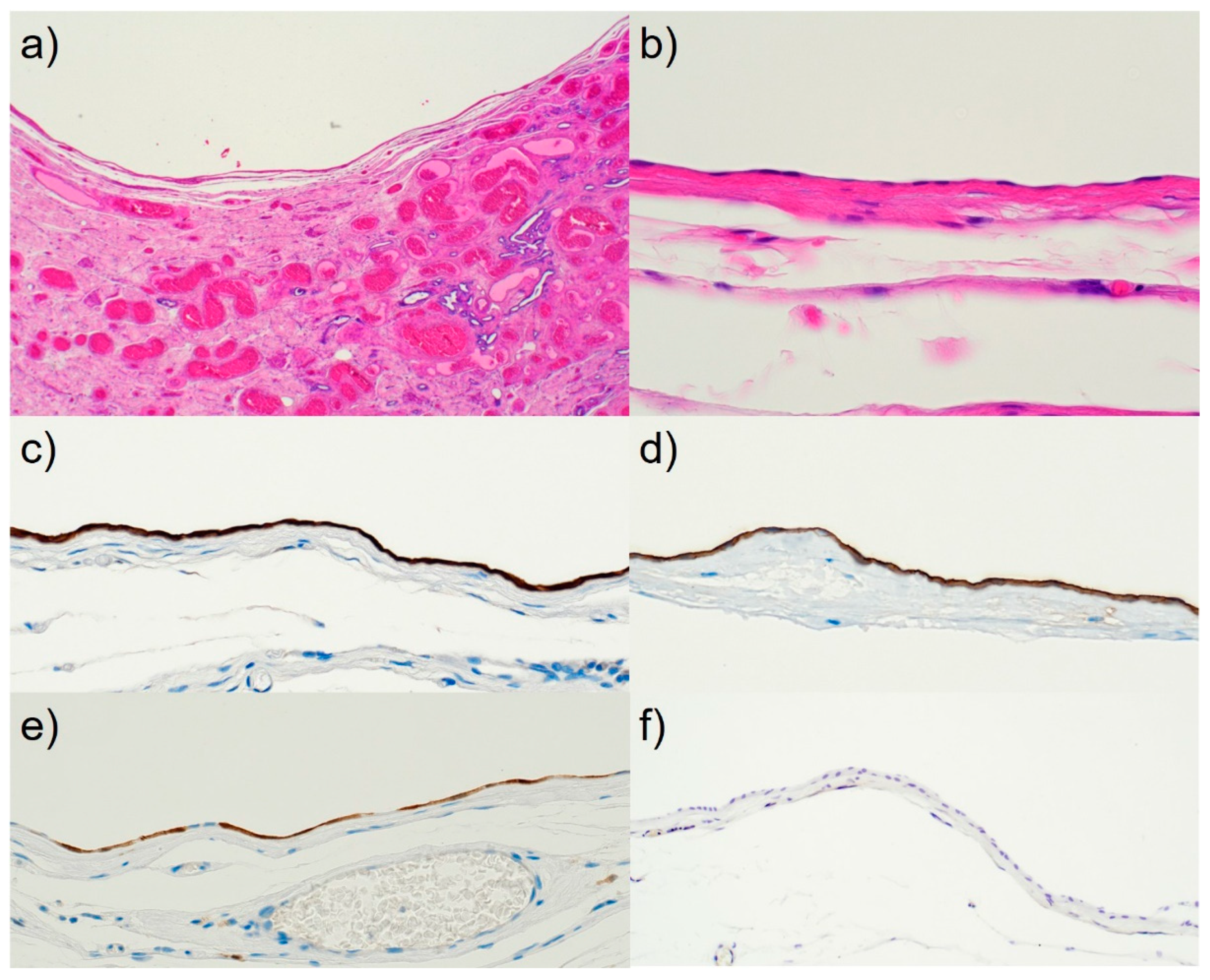
Microscopically, the cyst existed entirely within the parenchyma of the testis near the rete testis and was separated from the rete testis, tunica albuginea, and epididymis (
Figure 3a). The empty cyst lumen had no spermatozoa, and the lining epithelium had a flat layer on the cuboidal epithelium (
Figure 3b). The seminiferous tubules showed atrophy with hyalinization in the surrounding areas. Immunohistochemically, the cystic lining epithelial cells revealed diffuse strong immunoreactivity for cytokeratin (CK) AE1/AE3 (
Figure 3c), Wilms tumor (WT)-1, calretinin, Hector Battifora mesothelial epitope-1 (HBME-1) (
Figure 3d), p16
INK4a (clone: G175-405) (
Figure 3e), and weak positivity for thrombomodulin and EMA. Human papillomavirus (HPV) in situ hybridization was negative (
Figure 3f), podoplanin (clone: D2-40), p63, mesothelin, CK 5/6, and Ki-67 (clone: MIB-1) labeling index was as high as 1%.
Discussion
Testicular SC is uncommon; however, its identification has become more frequent due to the widespread use of advanced, high-resolution ultrasound technology for scrotal examinations [
4]. These SCs are classified into two clinical categories: infantile and adult types. The adult variant typically presents with no symptoms and remains non-palpable. They are found incidentally on urological examination, castration as a PC or even autopsy treatment [
3]. Pathology is the gold standard for diagnosing testicular SCs. Microscopically, the SCs of the testes were defined as follows.
They must lie within the parenchyma of the testis, contain clear fluid free from sperm, and be surrounded by a wall lined by flat or cuboidal epithelial cells.
The wall must be separated from the tunica albuginea; neither the wall nor the parenchyma contained teratomatous elements.
The remaining testes showed no evidence of chronic inflammation or fibrosis [
4].
The present case fulfilled these criteria. The management of SC in the testes remains controversial. Orchiectomy, testicular parenchyma-preserving enucleation of the cyst, and conservative surveillance using ultrasonography are the three options available to patients and doctors. Ultrasound studies have indicated that the SC of the testis has little potential for growth [
2]. More and more doctors are advocating a “watch and wait” strategy in recent years. This “watch and wait” strategy is an excellent choice for patients with asymptomatic cysts, both infant and adult types. In addition, we recommend orchiectomy if the patient is > 50 years of age [
4]. Rete testes showed weak focal calretinin staining [
3]. The lining epithelium of the SC of the testes is composed of mesothelial cells derived from the ectopic rete testes [
2].
Our patient also showed diffuse immunoreactivity for p16
INK4a (
Figure 3e); however, HPV was undetectable by in situ hybridization (
Figure 3f). According to the research conducted by the human protein atlas [
5], it has been reported that high levels of p16
INK4a expression occur in male genital tissue, particularly in the testis. Therefore, this observation may be a normal finding.
Here, we report a rare incidental case of SC of the right testis in an adult castration and confirm by immunohistochemistry that the lesion was derived from an ectopic rete testis. This is the rare report of SC in a testis found incidentally during castration for prostatic cancer in English literature.
Author Contributions
Conceptualization, M.T.; methodology, M.T.; validation, M.T., H.H., and S.F.; investigation, M.T., and H.H.; resources, Hi.Na.and Ha.No.; data curation, S.F.; writing—original draft preparation, M.T.; writing—review and editing, H.H. and S.F.; supervision, S.F.; project administration, S.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki (1975) and approved by the Ethics Committee of Shimada General Medical Center, Shimada, Shizuoka, Japan (ref: R5-9, approval date: 19 September 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The patient has written informed consent.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Naoki Ooishi, Takayoshi Hirota, and Kuniaki Muramatsu (Division of Pathology and Oral Pathology, Shimada General Medical Center, Shimada, Shizuoka, Japan) and Mina Honda (Division of Pathology, Hamamatsu University Hospital, Hamamatsu, Shizuoka, Japan) for performing immunohistochemical staining and Tina Tajima for editing our English manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Contributor Information
Mitsuhiro Tachibana, Email: 0206mtachi@gmail.com
Hideki Hamayasu, Email: hamayasu@shimada-gmc.jp
ORCIDiD: None
Hiromichi Nakagawa, Email: hiromichi1145@gmail.com
Hayato Nozawa, Email: hnzw.0941@gmail.com
Shigeki Fukuzawa, Email: vhd00735@nifty.ne.jp
Abbreviations
| SC |
simple cyst |
| PC |
prostate cancer |
| CK |
cytokeratin |
| HBME-1 |
Hector Battifora mesothelial epitope-1 |
| WT-1 |
Wilms tumor1 |
| p16INK4a |
cyclin-dependent kinase inhibitor p16 |
| HPV |
human papillomavirus |
References
- Hatsiopoulou, O. , Dawson, C. Simple intratesticular cysts in adults: A diagnostic dilemma. BJU Int 2001, 88, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Nistal, M. , R., González-Peramato, P. Nonneoplastic diseases of the testis. In UROLOGIC SURGICAL PATHOLOGY., 4th ed.; Cheng, L., MacLennan, G.T., Bostwick, D.G., Eds.; ELSEVIER: Philadelphia, USA, 2020; p. 725. [Google Scholar]
- Kuwamoto, S. , Okuno, K., Kato, M., Hayashi, K. Simple cysts of testis with immunohistochemical evidence of mesothelial origin. Pathol Int 2009, 59, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y. , Zhao, L., Yan, F., Cui, X., Zhou, F. Strategy for treating simple testicular cyst in adults. Am J Men Health 2011, 5, 193–197. [Google Scholar] [CrossRef] [PubMed]
- The human protein atlas. Available online: https://www.proteinatlas.org/ENSG00000147889-CDKN2A/tissue (accessed on 30 September 2023).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).