Introduction:
Hyperpigmentation is characterized by presence of excess melanocytes in the skin. Various pigmentation patterns include epidermal, dermal, mixed and indeterminate types [
1,
2]. Pigmentation disorders are commonly diagnosed, evaluated, and treated in primary care practices. Typical hyperpigmentation disorders include post inflammatory hyperpigmentation, melasma, ephelides (freckles) and café au lait macules
. Dermal pigmentation is caused by melanin within the dermis, between the bundles of collagen, or within melanophages [
2]. Dermal pigmentary disorders are seen in a significant proportion of patients visiting a skin clinic in both private and government set up in India. The dermal pigmentation can be broadly classified as congenital and acquired pigmentation. The congenital dermal pigmentation mainly includes dermal nevi including nevus of ota, becker’s nevus, nevus spilus, café au lait macule etc. Acquired dermal pigmentation includes dermal macular pigmentation, dermal tattoos, and dermal melasma.
Treatment of dermal pigmentation can be very challenging for the treating dermatologists. Also, considering the Indian subcontinent where maximum people have a Fitzpatrick skin type of III to V with high melanin content there is higher incidence of photo damage and pigmentary disorders [
3]
. There is lack of evidence in literature for evaluating the efficacy and safety as well as the treatment protocols of laser therapy in the treatment of resistant dermal pigmentation. Therefore, we carried out this retrospective study to evaluate the efficacy and safety of lasers as well as to suggest the safe treatment protocols regarding the use of lasers in different categories of dermal pigmentation in Indian skin type.
Methods:
This is a retrospective observational study conducted in a tertiary care laser and aesthetic dermatology institute. The aim of the study was to evaluate the efficacy and safety of sequential lasers treatments in the management of resistant dermal pigmentation in Indian skin type.
A total of one hundred and thirty-one patients with resistant dermal pigmentation, attending the OPD over a period of past 5 years (January 2018 - January 2023) of either sex and age range between 21 and 65 years were enrolled in the study. The patients were clinically and dermoscopically diagnosed by a dermatologist at the time of first visit and were offered sequential laser treatments along with recommended topical therapies and sun protection. Out of these, nine patients who had not received minimum 3 sessions of laser therapy or minimum 6 months of follow up after the cessation of treatment were excluded. The remaining 122 patients were finally recruited for the study and divided into 4 groups, comprising of dermal melasma (n= 51), acquired dermal hyperpigmentation i.e. lichen planus pigmentosus and ashy dermatosis (n=11), dermal nevi (n=21) and tattoos (n=39). The demographic data of these patients including the age at presentation, type of lasers used, number of treatment sessions and duration of follow up was methodically tabulated.
The response to therapy was assessed subjectively using both physician and patient-based scales. Physician based assessment was done by analyzing photographs of patients by two independent dermatologists on a power point presentation. Photographs at baseline, after every session, at one month after the last session and on successive follow up visits at 6 months were analyzed. The response was graded as per the proforma [ >90% improvement from the baseline photographs (excellent improvement), 75-90% (Good improvement), 50-74% (Moderate improvement), 25-49% (Mild improvement) and 0-24% (No improvement)]. The subjective patient based response and side effects were also analyzed by evaluating routine patient feedback proformas that were routinely filled by all patients in clinic for pigmentary disorders. The patients had given feedback on the treatment responses on a scale of 1-10 at the time of the last session and 6 months follow up. Relapse was defined as >25 % (of baseline) increase in pigmentation at the end of 6 months follow up as compared to end of treatment. Aggravation was defined as >25% increase in pigmentation from the baseline images.
As per standard protocol in the clinic, a detailed diet history was taken for every patient, underlying vitamin or mineral deficiencies detected on blood tests were corrected beforehand [
4] The patients were suggested to be on early morning high protein diet respecting the circadian rhythm. The contraindications to laser therapy like pregnancy, lactation, photosensitivity, malignancy, connective tissue disorders and a tendency towards hypertrophic scar or keloid formation are routinely screened. Patients who had consented for laser treatments before every session as a standard protocol in the clinic were enrolled. The treatment procedure followed in the clinic was according to ethical guidelines of Helsinki as revised in 2013.
For each of the four groups the laser protocols that were followed included:
Group 1: Dermal Melasma
Fifty-one patients with dermal melasma were enrolled and various lasers used at an interval of 3-4 weeks in the following sequence:
1st and 2nd session: non-ablative laser –SSR 540(Alma Harmony XL platform): 7-8J/cm2, 30 Hz, two shots in succession.
3rd and 4th session: Pixel Q switch 1064(Alma Harmony XL platform): pixel tip, (1200mJ/cm2fluency, 4-8 passes), for resistant cases-conventional 3 or 5mm tip (1000mj/cm2 fluency, single or double passes)
5th session: ablative laser – pixel Erbium YAG 2940(Alma Harmony XL platform) with pixel tip (1100-1200m/j/p, stack mode, long pulse, 4-5 passes)
For residual pigmentation: Over the last one year 8 patients with residual pigmentation were subjected to Alma Hybrid laser comprising of CO2 and 1570 nm Erbium Glass fiber laser over the resistant areas using the following settings; Power output 20W, on time 0.4ms, energy 8mj/ px for CO2 laser combined with erbium glass fibre laser (1570nm wavelength) power 8W, on time 3ms, energy 24mj/px with a density 4 and double passes for skin type IV. As a final step in the treatment with this laser an ultrasonic infuser IMPACT was used to infuse proteoglycan solution or platelet rich plasma.
Group 2: Acquired Dermal Macular Hyperpigmentation
Lichen Planus Pigmentosus (LPP): A total of 11 patients with burnt out disease for atleast past 6 months duration were enrolled in order to avoid activity or koebnerisation with laser induced injury. The following protocol was followed:
First 3 sessions: Pixel Q switch lasers with pixel tip, 1200mj fluency and 4-6 passes.
4th and 5th sessions: Conventional Q switch tips sized 3mm and 5mm at 1000mj fluence in single pass.
6th and 7th sessions: Ablative lasers like Pixel erbium YAG laser (Harmony xl platform), pixel tip, with fluency 1200mj per pass and a total of 5 passes on long pulse mode.
For resistant areas: Alma Hybrid laser was used over the resistant areas similar to melisma protocol.
Group 3: Nevus
a) Nevus of Ota: Pixel Q-switch laser was used for 4-6 sessions starting with 1200mj with 20 passes, gradually number of passes were increased up to 40-50 passes. After 3 sessions for more resistant areas conventional 3 mm or 5 mm tips were utilized at 1000-1200mj/p fluency with single or double passes.
b) Becker’s Nevus: A cocktail of lasers was utilized in each session for 5 patients of Becker’s nevus with Q switch and hair reduction laser to address all components of the nevus. Hair removal was targeted first with diode (10J/cm2 X 4 passes), followed by Alex (13J/cm2 X 10 passes) for finer hair in subsequent session. Once the hair become even finer, Intense pulsed light (10J/cm2 X 4 passes on HR mode) with SHR hand piece with Harmony XL platform was used due to its bigger hand piece and faster coverage in each subsequent session. The pigment component was targeted with the help of Q-switch Nd:YAG laser (5-6 sessions) with 5 or 3 mm tip with 1000 mj/ pass and 1-2 passes.
c) Café au lait macules (CALMs) –
Q Switch 1064 laser (Alma Harmony XL) was used in the 9 patients with CALMs with pixel tip (1200mj/p, 20-40 shots). Conventional tips (3mm or 5 mm) with fluency of 1000 mj and single passes of Q switch laser were used for more resistant areas.
The Hybrid laser as mentioned in Melasma and LPP was used in this group at same fluence and output protocol.
Group 4: Tattoo:
Our innovative ABLIQ protocol was used for removal of tattoo which stands for ablative lasers (ABL), followed by intense pulsed light (I) and Q switch laser(Q) to minimize the total number of sessions and reduce the ghost effect. Thirty-nine patients were treated with this protocol for a total of 6-7 sessions.
The data pertaining to the diagnosis of the patients in each of the 4 categories, their demographics, the number of sessions needed, duration of follow up, improvement in pigmentation as per both physician and patient scales, adverse effects if any were recorded and the data was analyzed.
Results:
The demographic profile of patients including the average age and sex ratio for each of the four groups has been tabulated in
Table 1. There were 39 males and 83 females enrolled in the study. The maximum average age was for the melasma group (44.5± 8.2) and the minimum was for nevus (6.4 ± 1.5).
The average number of sessions required was minimal for the tattoo group with the ABLIQ technique with an average of 5.9 ± 1.4 sessions and maximum for melasma with an average of 8.3 ± 1.8 sessions.
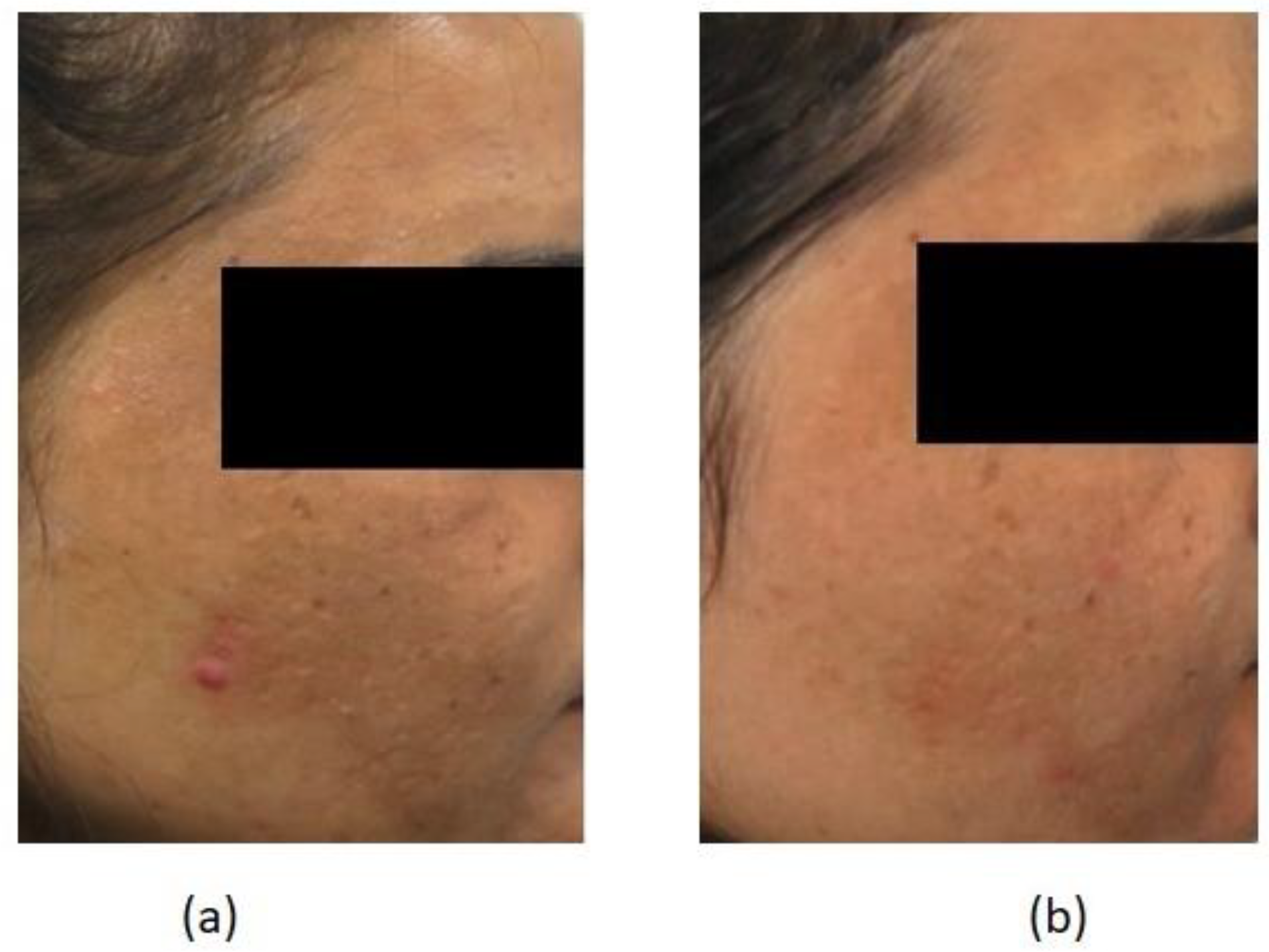
The treatment outcomes were recorded at the end of treatment and after 6 months of completion of treatment. The response increased at the end of treatment when 16 patients (31.3%) had an excellent improvement, 13 (25.4%) had a good improvement and 15 (29.4%) had a moderate improvement. Only one patient reported no improvement at the end of treatment (
Table 2). Average patient satisfaction at the end of treatment was 6.9 ± 2.5 out of 10. At the end of 6 months, out of 51 patients of dermal melasma, 12 patients had an excellent improvement, 11 had a good improvement (
Figure 1) and 23 had a moderate improvement with only 5 patients who had no or mild improvement.
For Acquired macular hyperpigmentation out of 11, 4 patients each had excellent (
Figure 2) and good improvement and one each had moderate, mild and no improvement. Patient response was 5.9 ± 1.4 out of 10 (
Table 2).
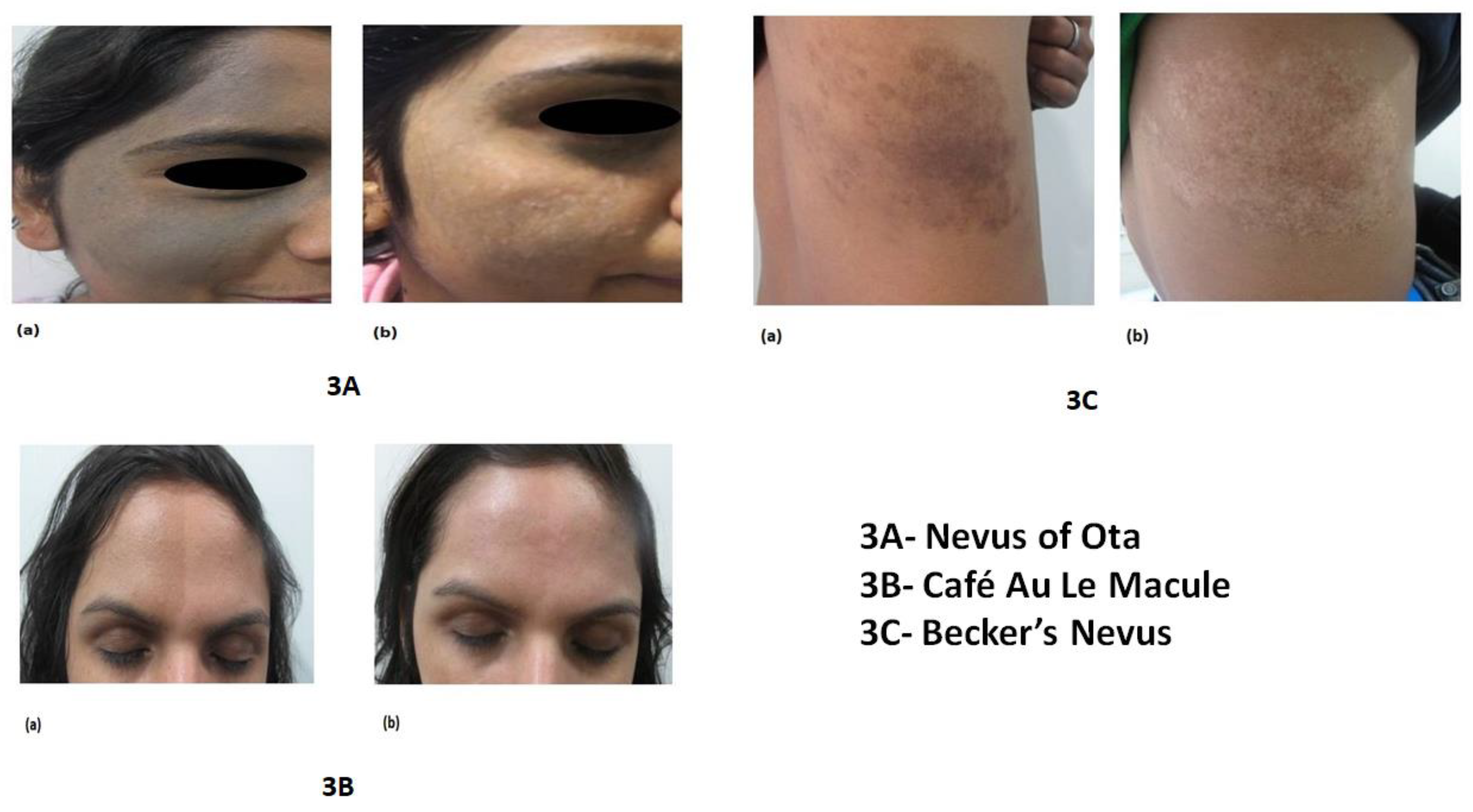
For dermal nevus 17 out of 21 patients had more than moderate improvement at the end of 6 months (
Table 3) and at the end of treatment 8 (38%) had excellent improvement (
Figure 3A and
Figure 3B), 5(23.8%) each had good and moderate improvement (
Figure 3C) and only 2 patients had mild and 1 had no improvement. Patient satisfaction was 6.2 ± 1.4 out of 10 at the end of treatment (
Table 2).
For tattoos, 34 out of 39 patients had an excellent (Picture 4A and 4B) or good improvement, while only 5 patients had a moderate improvement. The patient satisfaction too was 7.9 ± 1.1 out of 10.
Figure 4.
A (a) Baseline picture of tattoo on the back of neck. (b) Excellent improvement after 5 sessions of Ablative lasers (ABL) intense pulsed light (I) and Q switch laser (Q) [ABLIQ technique]. B (a) Baseline picture of patient with tattoo. (b) After 7 sessions of Ablative lasers (ABL) intense pulsed light (I) and Q switch laser (Q) [ABLIQ technique].
Figure 4.
A (a) Baseline picture of tattoo on the back of neck. (b) Excellent improvement after 5 sessions of Ablative lasers (ABL) intense pulsed light (I) and Q switch laser (Q) [ABLIQ technique]. B (a) Baseline picture of patient with tattoo. (b) After 7 sessions of Ablative lasers (ABL) intense pulsed light (I) and Q switch laser (Q) [ABLIQ technique].
Relapse was seen in 2 patients of dermal nevus, 3 patients of ADMH and 13 patients of melasma and none in tattoo group. These patients were offered maintenance sessions of lasers and counseled to follow strict photo protection and topical medication as advised to them and explained in depth about chronicity of problem.
Common side effects encountered were mild dryness, burning, itching which were tackled with mild steroid cream (fluticasone propionate 0.05%), half pea size application twice a day for first two to four days along with strict photo protection and liberal moisturizers. Rarely oral analgesics were recommended to take care of burning sensation following use of ablative lasers.
As per the records, erythema was most common adverse effect noted in 79 patients (64.75%) followed by mild pain in 64 patients (52.4%). Exacerbation of pigmentation was seen in 1 patient with melasma.
Discussion:
Dermal pigment in disorders like melasma, LPP, nevus, and tattoo sits in the deep dermis which makes it more challenging to treat. The acquired dermal pigmentation is due to increased production and accumulation of melanin. Sun exposure, chronic inflammation, hormonal changes and ageing are the triggering factors for hyperpigmentation [
2,
3]. These disorders are usually difficult to treat and have a huge effect on the quality of life. Treatment of dermal pigmentation remains an uphill task for dermatologists despite emergence of several novel modalities. Our study was an exhaustive work, comprising of a large number of patients with different types of dermal pigmentation. The results of our study are encouraging and indicate that lasers are safe, effective and promising modalities for the treatment of dermal pigmentation, provided they are used judiciously.
Several previous studies have evaluated the role of lasers in dermal pigmentation. The review article by Aurangabadkar et al demonstrated to optimize laser toning for dermal pigmentary disorders and suggested using low fluence Q-switched Nd: YAG laser at 1064nm utilizing the multi-pass technique with a large spot size [
5]. Melasma is a complex pigmentary condition with multifactorial etiologies including both exogenous and endogenous factors. Authors believe that use of combination of medical and intervention therapy along with correction of diet and deficiencies has proved to be very effective and no monotherapy is effective in reducing dermal melasma significantly. Treatment of melasma includes medications which can be topical or oral along with chemical peels and laser treatments aimed at reducing pigmentation and inflammation [
6,
7]. In an Indian study by Arora et al [
8], twenty male and female subjects with moderate to severe mixed-type melasma on both sides of the face were randomized to six weekly treatments with the low-fluency Q-switched Nd: YAG laser on one side and the low-fluency QSAL to the other side. Both laser treated sides showed a significant improvement in MMASI evaluation after two treatments (22% improvement on the QS-Nd: YAG, 17% QSAL) and each follow-up visit, but no significant difference was seen between study groups at any visit. Another study by Zhou and colleagues [
9] in which fifty patients of melasma were treated with 1064-nm QS Nd: YAG laser at low energy levels (fluence of 2.5-3.4 J/cm
2) weekly for nine sessions found 35.8% improvement from baseline. Mean MASI scores decreased by 61.3% after therapy (from 10.6–4.1, p<.001); 70% of patients had more than a 50% decrease in their MASI values, and 10% had 100% clearance. Recurrence rate at the 3-month follow-up was 64%. Our study showed better results in melasma with more than 80% patients with moderate to excellent improvement, probably owing to use of sequential laser technologies and a smaller number of sessions along with lifestyle modifications like early morning protein rich breakfast and correction of underlying vitamin B12, vitamin D3 and iron deficiencies [
4].
Acquired dermal macular hyperpigmentation can be defined as darkening of skin due to alteration in melanocytes production and melanin deposition in epidermis or dermis such as in lichen planus pigmentosus. In a recent study from Italy [
10], 96 patients asking for benign hyperpigmentation removal were consecutively enrolled and treated with 1064 nm Nd:YAG laser with pulse duration of 6 nanoseconds (ns) for dermis lesions and 532 nm with 6 ns for epidermal ones. Up to five treatments with a minimum interval of thirty days between laser treatments were performed. All patients reached a good to complete pigmentation removal with a mean VAS score of 8.91 ± 1.07. In another study by Neetu et al nine patients of lichen planus pigmentosus were treated with Q switched Nd:YAG laser. Six sessions were done at 2 weeks intervals. A mean of 25.7% improvement was seen at end of six sessions [
11]. In our study better results were seen with 60% of excellent to good improvement in a smaller number of sessions with less recurrence rate. Use of sequential lasers, lifestyle modifications, along with correction of protein, vitamin and mineral deficiency again were addressed in all the patients.
Nevus is usually a benign growth on the skin formed by proliferation of melanocytes. Most of these lesions are pigmented and sun exposure leads to greater number of lesions. In a Korean study, Park et al [
12] treated dermal pigmentations like nevus of Ota and congenital nevus with the combined therapy of a resurfacing laser (CO2) and a selective photothermolytic laser (the Q-Switched Ruby Laser [QSRL]) and the results were compared with those treated with the QSRL alone. Combined laser therapy was performed in 47 patients with nevus of Ota. Out of 47 patients, excellent results were seen in 98 % of patients. Combined laser therapy was used in 15 patients with congenital nevus, and 12 (80%) showed good to excellent results. By combining resurfacing and pigment selective lasers, the treatment period was reduced by 2 to 3 months, and the number of treatments was reduced two to threefold. The results were superior to our study in which 60 % of dermal nevus showed excellent to good response. The superior results in their study can be attributed to different skin types in Korean patients as compared to Indian patients, different assessment parameters and different laser modalities used. In another study by Hemanta et al (13), fifty patients of nevus of Ota underwent multiple treatments (average 5 sessions) at monthly intervals carried out over a period of 2 years with QSNYL. Near total improvement was seen in 8%, marked improvement in 22%, moderate improvement in 38% and 32% patients reported less than 25% clearing of the lesion. All patients reported some improvement. Transient post inflammatory hyperpigmentation was observed in 4 (8%) patients, which cleared with use of sunscreens and bleaching agents within 2 months. No textural change or scarring was observed in any patient. In our study more than 70% of the patients showed improvement with a smaller number of sessions and minimal side effects.
A tattoo can be defined as a mark, design or word intentionally placed or fixed by insertion of pigment under the skin. The reasons of getting tattoo can be numerous including religious purposes, as a status symbol or simply for artistic or cosmetic purposes. But unfortunately, removal of tattoo is much more time consuming, frustrating and expensive for the patient. A detailed history and examination with baseline pictures should be done prior to the treatment. In one study from Italy (14) in which 52 patients were enrolled for tattoo removal by laser, black and blue tattoos were treated with a 1064 nm laser, with a pulse duration of 6 ns and a fluence up to 10 J/cm2, while colored tattoos were treated with sessions of 532 nm laser, with a pulse duration of 6 ns and a fluence up to 5 J/cm2. Up to nine treatments with a minimum interval of 8 weeks between each session were performed. A six-month follow-up visit assessed patient satisfaction (Visual Analogue Scale). Lapidoth and Aharonowitz studied tattoo removal in 404 subjects of Ethiopian origin with skin types V and VI. All tattoos were blue/black and had been made by injecting charcoal into the skin and underwent three to six laser treatments with the Q-switched Nd:YAG (380 patients) or ruby (24 patients) laser at intervals of at least 8 weeks. At the last follow-up, a clearance of 75–100% was achieved in 92% of the patients. Transient (2–4 months) mild hyperpigmentation was noted in 44% of the patients, and mild textural changes in two patients. There were no cases of scarring or permanent pigmentary changes (15). The mean number of sessions required to obtain a result in our study were 5.9±1.4, and using ABLIQ technique with cocktail of lasers helped in reducing total number of sessions without compromising the safety.
We also found increased benefit in some patients with Hybrid laser which was used in only the patients treated over the last one year. Hybrid laser was only used over the resistant areas and gave excellent results in these areas where all other modalities had failed.
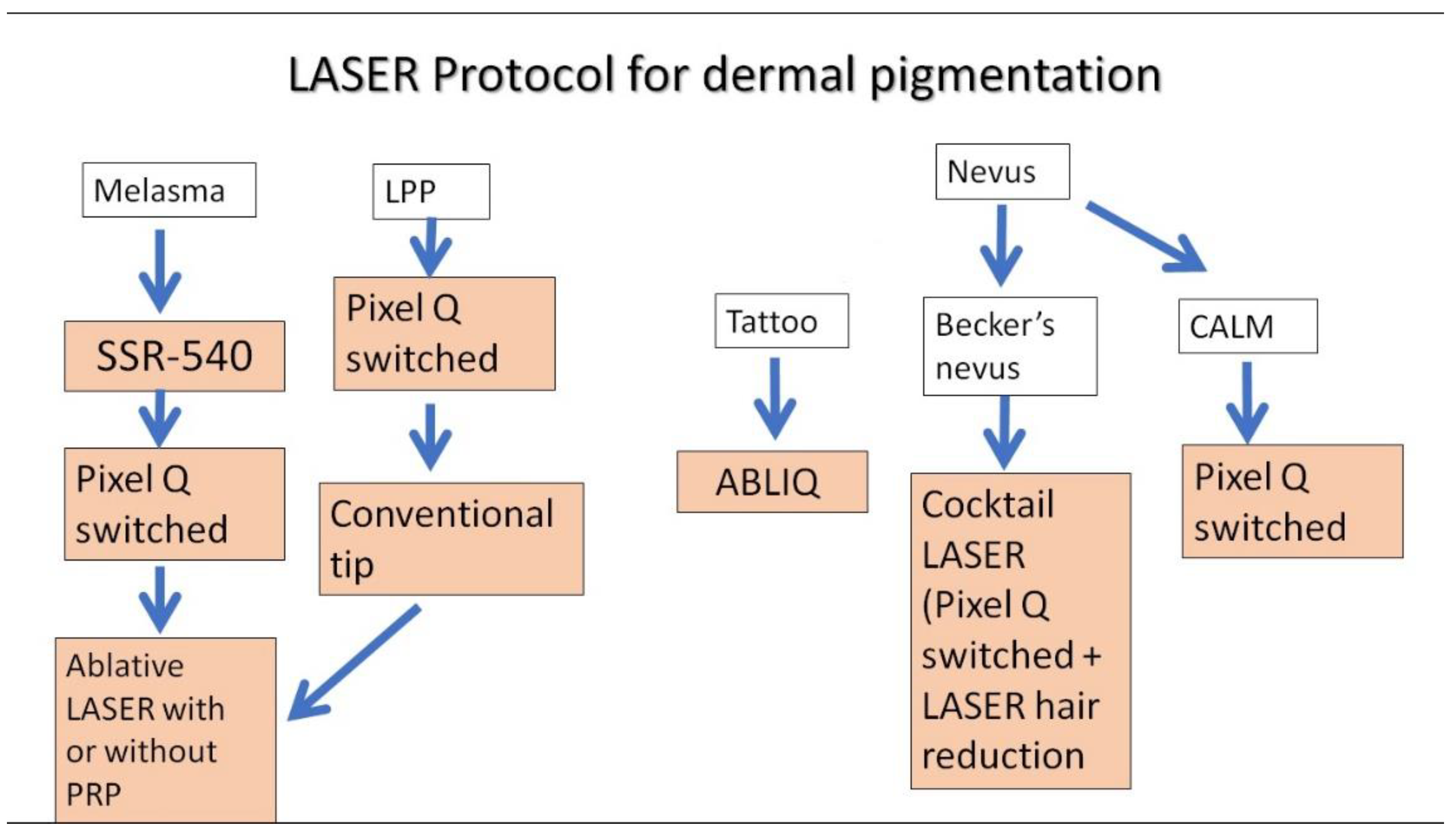
Our study is one of the largest studies in Indian skin type with different types of dermal pigmentation. The use of laser is considered tricky here, owing to risk of post inflammatory hyperpigmentation. Nonetheless, lasers were found to be an effective modality with good safety profile in treatment of different kinds of dermal pigmentation. Various strengths of our study include a large sample size, a longer follow up along with study of relapse rates. Another strength of our study was that it was a patient centric study as sequential and cocktail of lasers were given as per patient’s response to the treatment. The study is a single centered study with retrospective study design and this is a major limitation. Based on our study, we propose a plausible protocol for the management of dermal pigmentation with lasers which has been illustrated in
Figure 5.
Conclusion:
Asian /Indian skin type is considered one of the most challenging skin types for treatment of the dermal pigmentation through lasers. A proper treatment protocol using sequential and cocktail of lasers along with addressal of underlying protein and micronutrient deficiencies and lifestyle modification can help in reducing overall number of sessions and majority of complications.
Conflict of interest
The authors state that there is no conflict of Interest.
References
- Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, Mihm MC Jr. Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol. 1981 Jun;4(6):698-710. [CrossRef]
- Nicolaidou E, Katsambas AD. Pigmentation disorders: hyperpigmentation and hypopigmentation. Clin Dermatol. 2014 Jan-Feb;32(1):66-72. [CrossRef]
- Ho SG, Chan HH. The Asian dermatologic patient: review of common pigmentary disorders and cutaneous diseases. Am J Clin Dermatol. 2009;10(3):153-68. [CrossRef]
- Garg S, Sangwan A. Dietary Protein Deficit and Deregulated Autophagy: A New Clinico-diagnostic Perspective in Pathogenesis of Early Aging, Skin, and Hair Disorders. Indian Dermatol Online J. 2019 Mar-Apr;10(2):115-124. [CrossRef]
- Aurangabadkar SJ. Optimizing Q-switched lasers for melasma and acquired dermal melanoses. Indian J Dermatol VenereolLeprol. 2019 Jan-Feb;85(1):10-17. [CrossRef]
- Trivedi MK, Yang FC, Cho BK. A review of laser and light therapy in melasma. Int J Womens Dermatol. 2017 Mar 21;3(1):11-20. [CrossRef]
- Garg S, Vashisht KR, Makadia S. A prospective randomized comparative study on 60 Indian patients of melasma, comparing pixel Q-switched NdYAG (1064 nm), super skin rejuvenation (540 nm) and ablative pixel erbium YAG (2940 nm) lasers, with a review of the literature. J Cosmet Laser Ther. 2019 Aug;21(5):297-307. [CrossRef]
- Arora P, Sarkar R, Garg VK, Arya L. Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J CutanAesthet Surg. 2012 Apr;5(2):93-103. [CrossRef]
- Zhou X, Gold MH, Lu Z, Li Y. Efficacy and safety of Q-switched 1,064-nm neodymium-doped yttrium aluminum garnet laser treatment of melasma. Dermatol Surg. 2011 Jul;37(7):962-70. [CrossRef]
- Nisticò SP, Cannarozzo G, Provenzano E, Tamburi F, Fazia G, Sannino M, Negosanti F, Del Duca E, Patruno C, Bennardo L. Nanosecond Q-Switched 1064/532 nm Laser to Treat Hyperpigmentations: A Double Center Retrospective Study. Clin Pract. 2021 Sep 23;11(4):708-714. [CrossRef]
- Bhari N, Sharma VK, Singh S, Parihar A, Arava S. Effect of Q-switched Nd-YAG laser on the clinical, pigmentary, and immunological markers in patients with lichen planus pigmentosus: A pilot study. Dermatol Ther. 2020 Mar;33(2):e13208. [CrossRef]
- Park SH, Koo SH, Choi EO. Combined laser therapy for difficult dermal pigmentation: resurfacing and selective photothermolysis. Ann Plast Surg. 2001 Jul;47(1):31-6. [CrossRef]
- Kar HK, Gupta L. 1064 nm Q switched Nd: YAG laser treatment of nevus of Ota: an Indian open label prospective study of 50 patients. Indian J Dermatol VenereolLeprol. 2011 Sep-Oct;77(5):565-70. [CrossRef]
- Briganti S, Camera E, Picardo M. Chemical and instrumental approaches to treat hyperpigmentation. Pigment Cell Res. 2003 Apr;16(2):101-10. [CrossRef]
- Lapidoth M, Aharonowitz G. Tattoo removal among Ethiopian Jews in Israel: tradition faces technology. J Am Acad Dermatol. 2004 Dec;51(6):906-9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).