Submitted:
10 October 2023
Posted:
11 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Surgical procedures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fujiwara M, Kodera Y, Misawa K, Kinoshita M, Kinoshita T, Miura S, et al. Longterm outcomes of early-stage gastric carcinoma patients treated with laparoscopy-assisted surgery. J Am Coll Surg. 2008, 206, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Ohtani H, Tamamori Y, Noguchi K, Azuma T, Fujimoto S, Oba H, et al. A meta-analysis of randomized controlled trials that compared laparoscopy-assisted and open distal gastrectomy for early gastric cancer. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2010, 14, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Passerotti CC, Begg N, Penna FJ, Passerotti AMAMS, Leite KRM, Antunes AA, et al. Safety profile of trocar and insufflation needle access systems in laparoscopic surgery. J Am Coll Surg. 2009, 209, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Pickett SD, Rodewald KJ, Billow MR, Giannios NM, Hurd WW. Avoiding major vessel injury during laparoscopic instrument insertion. Obstet Gynecol Clin North Am. 2010, 37, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Simforoosh N, Basiri A, Ziaee S-A-M, Tabibi A, Nouralizadeh A, Radfar MH, et al. Major vascular injury in laparoscopic urology. JSLS. 2014, 18, e2014–00283. [Google Scholar]
- Tanaka C, Fujiwara M, Kanda M, Murotani K, Iwata N, Hayashi M, et al. Optical trocar access for initial trocar placement in laparoscopic gastrointestinal surgery: A propensity score-matching analysis. Asian J Endosc Surg. 2019, 12, 37–42. [Google Scholar] [CrossRef]
- Altun H, Banli O, Kavlakoglu B, Kücükkayikci B, Kelesoglu C, Erez N. Comparison between direct trocar and Veress needle insertion in laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2007, 17, 709–712. [Google Scholar] [CrossRef]
- Chapron C, Fauconnier A, Goffinet F, Bréart G, Dubuisson JB. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a meta-analysis. Hum Reprod Oxf Engl. 2002, 17, 1334–1342. [Google Scholar] [CrossRef]
- Tuveri M, Tuveri A. Laparoscopic cholecystectomy: complications and conversions with the 3-trocar technique: a 10-year review. Surg Laparosc Endosc Percutan Tech. 2007, 17, 380–384.
- Vilos, G.A. The ABCs of a safer laparoscopic entry. J Minim Invasive Gynecol 2006, 13, 249–251. [Google Scholar] [CrossRef]
- Vilos GA, Ternamian A, Dempster J, Laberge PY, CLINICAL PRACTICE GYNAECOLOGY COMMITTEE. Laparoscopic entry: a review of techniques, technologies, and complications. J Obstet Gynecol Can JOGC. 2007, 29, 433–447. [Google Scholar] [CrossRef] [PubMed]
- Yanke BV, Horowitz M. Safety of the Veress needle in pediatric laparoscopy. J Endourol. 2007, 21, 695–697. [Google Scholar] [CrossRef]
- Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicentre observational study. Br J Obstet Gynaecol. 1997, 104, 595–600. [Google Scholar] [CrossRef]
- Magrina, JF. Complications of laparoscopic surgery. Clin Obstet Gynecol. 2002, 45, 469–480. [Google Scholar] [CrossRef]
- Catarci M, Carlini M, Gentileschi P, Santoro E. Major and minor injuries during the creation of pneumoperitoneum. A multicenter study on 12,919 cases. Surg Endosc. 2001, 15, 566–569. [Google Scholar] [CrossRef] [PubMed]
- Fuller J, Ashar BS, Carey-Corrado J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005, 12, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Jansen FW, Kolkman W, Bakkum EA, de Kroon CD, Trimbos-Kemper TCM, Trimbos JB. Complications of laparoscopy: an inquiry about closed- versus open-entry technique. Am J Obstet Gynecol. 2004, 190, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Kaistha S, Kumar A, Gangavatiker R, Br S, Sisodiya N. Laparoscopic Access: Direct Trocar Insertion Versus Open Technique. J Laparoendosc Adv Surg Tech A. 2019, 29, 489–494. [Google Scholar] [CrossRef]
- Munro, MG. Laparoscopic access: complications, technologies, and techniques. Curr Opin Obstet Gynecol. 2002, 14, 365–374. [Google Scholar] [CrossRef]
- Agresta F, Mazzarolo G, Bedin N. Direct trocar insertion for laparoscopy. JSLS 2012, 16, 255–259. [Google Scholar] [CrossRef]
- Shirk GJ, Johns A, Redwine DB. Complications of laparoscopic surgery: How to avoid them and how to repair them. J Minim Invasive Gynecol. 2006, 13, 352–359. [Google Scholar] [CrossRef]
- Taye MK, Fazal SA, Pegu D, Saikia D. Open Versus Closed Laparoscopy: Yet an Unresolved Controversy. J Clin Diagn Res JCDR 2016, 10, QC04–QC07.
- Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002, 16, 1121–1143. [Google Scholar] [CrossRef]
- Krishnakumar S, Tambe P. Entry complications in laparoscopic surgery. J Gynecol Endosc Surg. 2009, 1, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Bonjer HJ, Hazebroek EJ, Kazemier G, Giuffrida MC, Meijer WS, Lange JF. Open versus closed establishment of pneumoperitoneum in laparoscopic surgery. Br J Surg. 1997, 84, 599–602. [Google Scholar]
- Chapron C, Cravello L, Chopin N, Kreiker G, Blanc B, Dubuisson JB. Complications during set-up procedures for laparoscopy in gynecology: open laparoscopy does not reduce the risk of major complications. Acta Obstet Gynecol Scand. 2003, 82, 1125–1129. [Google Scholar] [CrossRef]
- Larobina M, Nottle P. Complete evidence regarding major vascular injuries during laparoscopic access. Surg Laparosc Endosc Percutan Tech. 2005, 15, 119–123. [Google Scholar] [CrossRef]
- Molloy D, Kaloo PD, Cooper M, Nguyen TV. Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002, 42, 246–254. [Google Scholar] [CrossRef]
- Schäfer M, Lauper M, Krähenbühl L. Trocar and Veress needle injuries during laparoscopy. Surg Endosc. 2001, 15, 275–280. [Google Scholar] [CrossRef]
- Zaraca F, Catarci M, Gossetti F, Mulieri G, Carboni M. Routine use of open laparoscopy: 1,006 consecutive cases. J Laparoendosc Adv Surg Tech A. 1999, 9, 75–80. [Google Scholar] [CrossRef]
- Kaali, S.G. Introduction of the Opti-trocar. J Am Assoc Gynecol Laparosc. 1993, 1, 50–53. [Google Scholar] [CrossRef]
- Berch BR, Torquati A, Lutfi RE, Richards WO. Experience with the optical access trocar for safe and rapid entry in the performance of laparoscopic gastric bypass. Surg Endosc. 2006, 20, 1238–1241. [Google Scholar] [CrossRef] [PubMed]
- Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002, 99, 553–555. [Google Scholar]
- Tinelli A, Malvasi A, Mynbaev OA, Tsin DA, Davila F, Dominguez G, et al. Bladeless direct optical trocar insertion in laparoscopic procedures on the obese patient. JSLS 2013, 17, 521–528. [Google Scholar] [CrossRef] [PubMed]
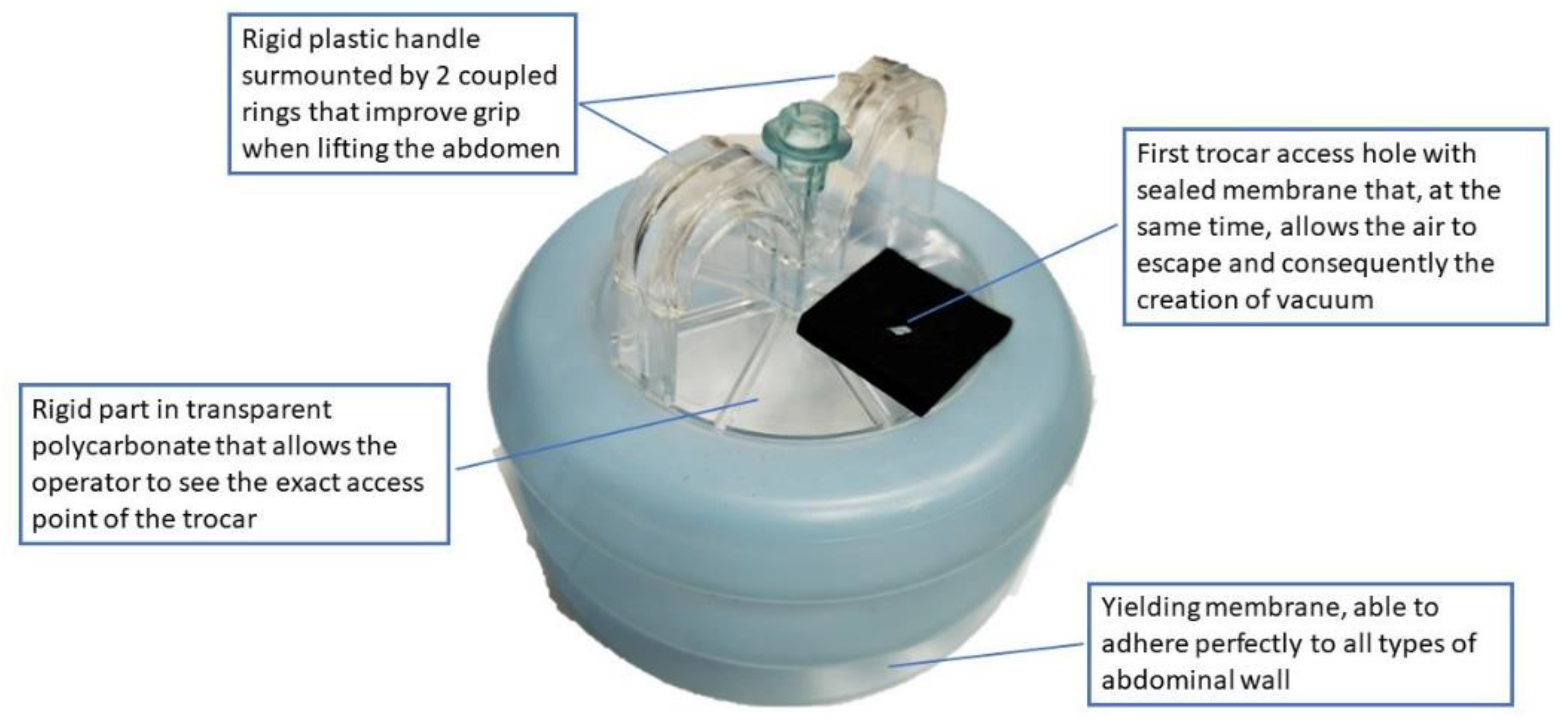
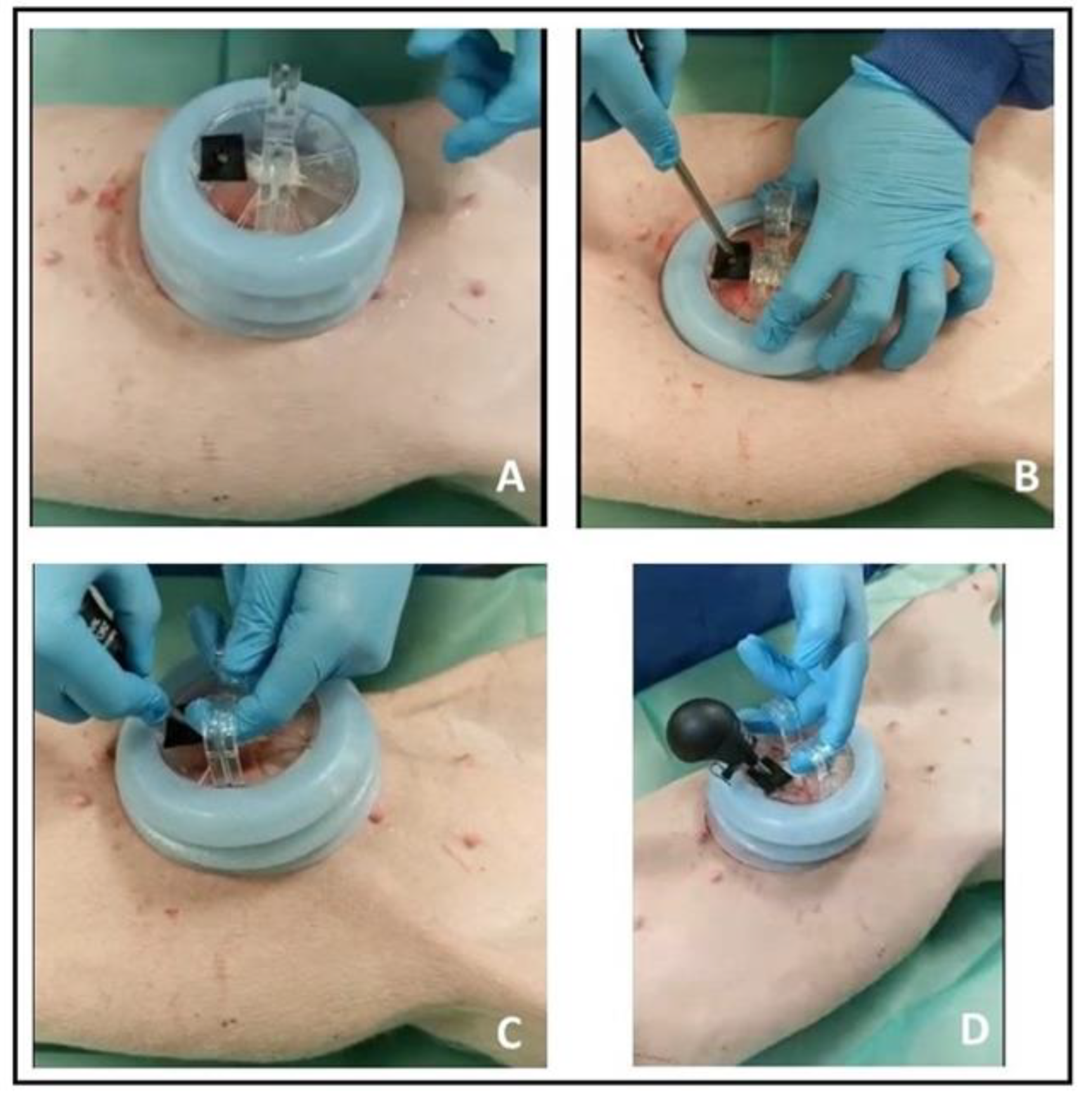
- Cassata G, Palumbo V, Cicero L, De Luca A, Damiano G, Fazzotta S, et al. OneShot-M: A New Device for Close Laparoscopy Pneumoperitoneum. Surg Innov. 2018, 25, 570–577. [Google Scholar] [CrossRef]
- Daniel, W.W. Applied Nonparametric Statistics; PWS-KENT: Boston, MA, USA, 1990. [Google Scholar]
- Philips PA, Amaral JF. Abdominal access complications in laparoscopic surgery. J Am Coll Surg. 2001, 192, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Blunt versus bladed trocars in laparoscopic surgery: a systematic review and meta-analysis of randomized trials. Surg Endosc. 2013, 27, 2312–2320. [Google Scholar] [CrossRef] [PubMed]
- Chandler JG, Corson SL, Way LW. Three spectra of laparoscopic entry access injuries. J Am Coll Surg. 2001, 192, 478–490. [Google Scholar] [CrossRef]
- Azevedo JLMC, Azevedo OC, Miyahira SA, Miguel GPS, Becker OM, Hypólito OHM, et al. Injuries caused by Veress needle insertion for creation of pneumoperitoneum: a systematic literature review. Surg Endosc. 2009, 23, 1428–1432. [Google Scholar] [CrossRef]
- Chapron C, Querleu D, Bruhat MA, Madelenat P, Fernandez H, Pierre F, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod Oxf Engl. 1998, 13, 867–872. [Google Scholar] [CrossRef]
- Dunne N, Booth MI, Dehn TCB. Establishing pneumoperitoneum: Verres or Hasson? The debate continues. Ann R Coll Surg Engl. 2011, 93, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Makai G, Isaacson K. Complications of gynecologic laparoscopy. Clin Obstet Gynecol. 2009, 52, 401–411. [Google Scholar] [CrossRef] [PubMed]
- McDonald PT, Rich NM, Collins GJ, Andersen CA, Kozloff L. Vascular trauma secondary to diagnostic and therapeutic procedures: laparoscopy. Am J Surg. 1978, 135, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Opitz I, Gantert W, Giger U, Kocher T, Krähenbühl L. Bleeding remains a major complication during laparoscopic surgery: analysis of the SALTS database. Langenbecks Arch Surg. 2005, 390, 128–133. [Google Scholar] [CrossRef]
- Ahmad G, Duffy JMN, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2008, 16, CD006583. [Google Scholar]
- Tinelli A, Malvasi A, Istre O, Keckstein J, Stark M, Mettler L. Abdominal access in gynaecological laparoscopy: a comparison between direct optical and blind closed access by Verres needle. Eur J Obstet Gynecol Reprod Biol. 2010, 148, 191–194. [Google Scholar] [CrossRef]
- Dingfelder, JR. Direct laparoscope trocar insertion without prior pneumoperitoneum. J Reprod Med. 1978, 21, 45–47. [Google Scholar]
- Günenç MZ, Yesildaglar N, Bingöl B, Onalan G, Tabak S, Gökmen B. The safety and efficacy of direct trocar insertion with elevation of the rectus sheath instead of the skin for pneumoperitoneum. Surg Laparosc Endosc Percutan Tech. 2005, 15, 80–81. [Google Scholar] [CrossRef]
- Inan A, Sen M, Dener C, Bozer M. Comparison of direct trocar and veress needle insertion in the performance of pneumoperitoneum in laparoscopic cholecystectomy. Acta Chir Belg. 2005, 105, 515–518. [Google Scholar] [CrossRef]
- Moreno DG, Pereira CAM, Sant Anna RK, de Azevedo RU, Savio LF, Duarte RJ, et al. Laparoscopic Insertion of Various Shaped Trocars in a Porcine Model. JSLS 2019, 23, e2019–00002. [Google Scholar]
- Theodoropoulou K, Lethaby DR, Bradpiece HA, Lo TL, Parihar A. Direct trocar insertion technique: an alternative for creation of pneumoperitoneum. JSLS 2008, 12, 156–158. [Google Scholar]
- Zakherah, MS. Direct trocar versus veress needle entry for laparoscopy: a randomized clinical trial. Gynecol Obstet Invest. 2010, 69, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Nezhat FR, Silfen SL, Evans D, Nezhat C. Comparison of direct insertion of disposable and standard reusable laparoscopic trocars and previous pneumoperitoneum with Veress needle. Obstet Gynecol. 1991, 148–150. [Google Scholar]
- Roy GM, Bazzurini L, Solima E, Luciano AA. Safe technique for laparoscopic entry into the abdominal cavity. J Am Assoc Gynecol Laparosc. 2001, 8, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Corson SL, Brooks PG, Soderstrom RM. Safe technique for laparoscopic entry into the abdominal cavity. J Am Assoc Gynecol Laparosc. 2002, 9, 399. [Google Scholar]
- Hill DJ, Maher PJ. Direct cannula entry for laparoscopy. J Am Assoc Gynecol Laparosc. 1996, 4, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Jacobson MT, Osias J, Bizhang R, Tsang M, Lata S, Helmy M, et al. The direct trocar technique: an alternative approach to abdominal entry for laparoscopy. JSLS. 2002, 6, 169–174. [Google Scholar]
- Copeland C, Wing R, Hulka JF. Direct trocar insertion at laparoscopy: an evaluation. Obstet Gynecol. 1983, 62, 655–659. [Google Scholar]
- Saidi, MH. Direct laparoscopy without prior pneumoperitoneum. J Reprod Med. 1986, 31, 684–686. [Google Scholar]
- Jarrett, JC. Laparoscopy: direct trocar insertion without pneumoperitoneum. Obstet Gynecol. 1990, 75, 725–727. [Google Scholar]
- Falahatkar S, Nadjafi-Semnani M, Panahandeh Z, Allahkhah A, Emadi S, Motevali S, et al. Direct Trocar Insertion Compare With Open Laparoscopy [Hasson Technique] in Patients Undergoing Urolaparoscopic Surgery. Urotoday Int J 2009, 2.
- Byron JW, Fujiyoshi CA, Miyazawa K. Evaluation of the direct trocar insertion technique at laparoscopy. Obstet Gynecol. 1989, 74 Pt 1, 423–425. [Google Scholar]
- Borgatta L, Gruss L, Barad D, Kaali SG. Direct trocar insertion vs. Verres needle use for laparoscopic sterilization. J Reprod Med. 1990, 35, 891–894.
- Angioli R, Terranova C, De Cicco Nardone C, Cafà EV, Damiani P, Portuesi R, et al. A comparison of three different entry techniques in gynecological laparoscopic surgery: a randomized prospective trial. Eur J Obstet Gynecol Reprod Biol. 2013, 171, 339–342. [Google Scholar] [CrossRef]
- Byron JW, Markenson G, Miyazawa K. A randomized comparison of Verres needle and direct trocar insertion for laparoscopy. Surg Gynecol Obstet. 1993, 177, 259–262. [Google Scholar]
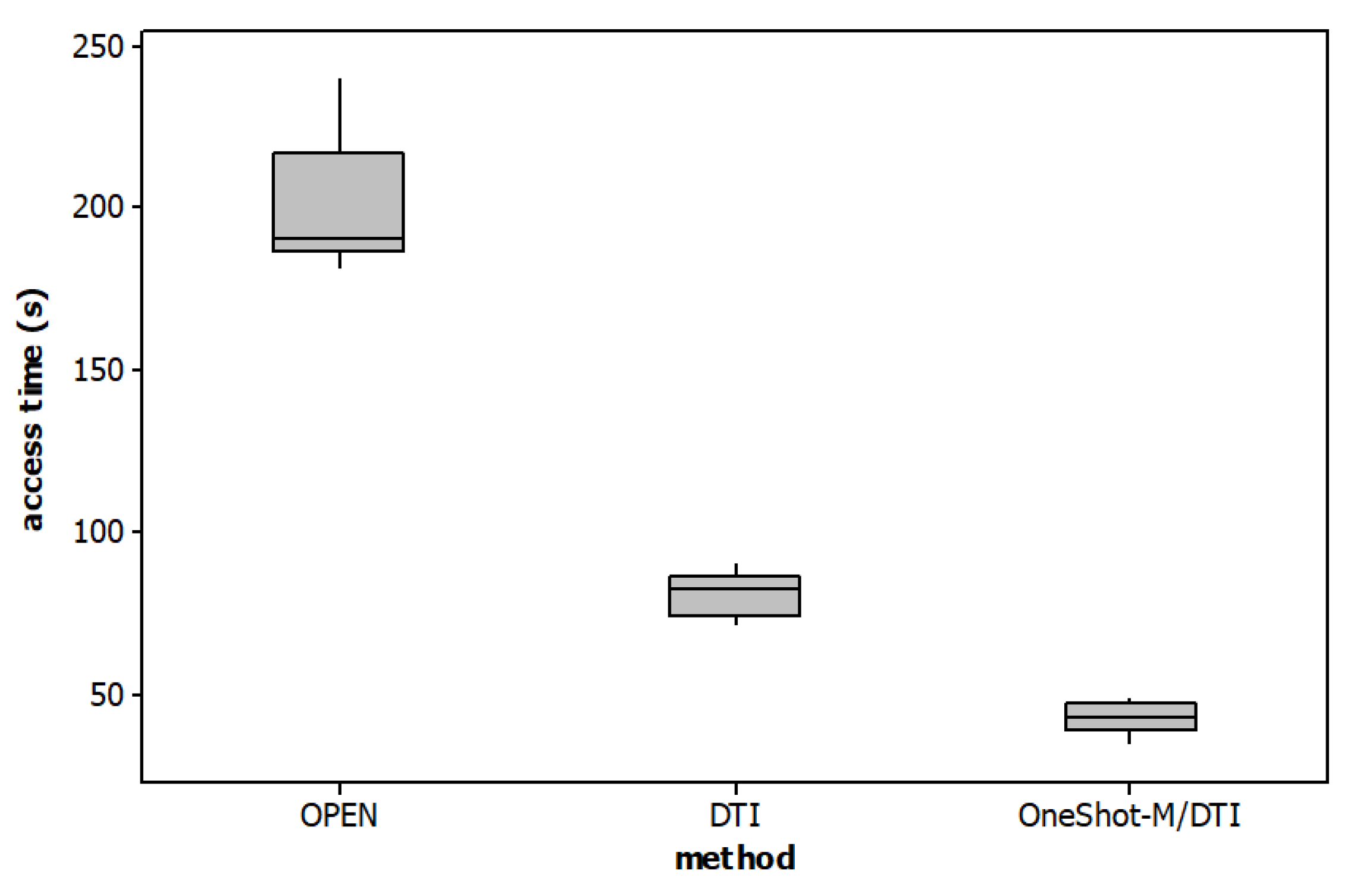
| Methods | Median (range) | Kruskal-Wallis Test (p-value) | Comparison | Dunn’s post hoc test (p-value) |
|
|---|---|---|---|---|---|
| Weight | Group A: OPEN | 33.15 (31.2 – 3) | 0.725 | ||
| Group B: DTI | 32.5 (30 – 35) | ||||
| Group C: OneShot-M/DTI | 33.25 (31.3 – 35) | ||||
| Access time | Group A: OPEN | 190.5 (182 – 240) | 0.0005 | A vs B | 0.155 |
| Group B: DTI | 82.5 (72 – 90) | A vs C | <0.001 | ||
| Group C: OneShot-M/DTI | 43 (35 – 49) | B vs C | 0. 155 |
|
Complication % (number) |
Group A OPEN(n = 6) |
Group B DTI (n = 6) |
Group C OneShot-M/DTI (n = 6) |
| Difficulty in entry | 33.33 (2) | 50 (3) | 16.67 (1) |
| Localized emphysema | 16.67 (1) | 16.67 (1) | - |
| Leakage of gas | 50.00 (3) | 16.67 (1) | - |
| Bruise/haematoma at port site | 16.67 (1) | 50.00 (3) | - |
| Omental injury | - | - | - |
| Bowel perforation | - | 16.67 (1) | - |
| Mesenteric vascular injury | - | - | - |
| Solid-organ injury | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





