Submitted:
12 October 2023
Posted:
13 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study design and population.
2.2. Outcome variables.
- Radiological Explanatory variables
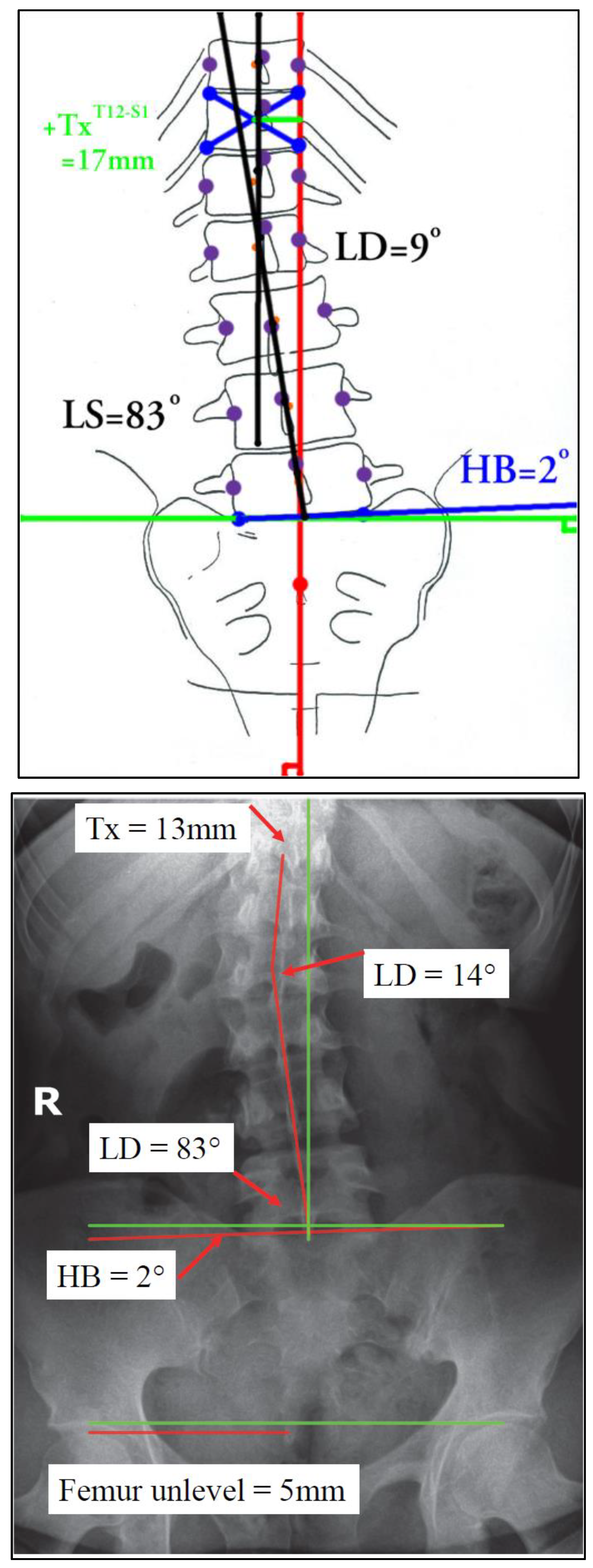
- T12-S1 centroid horizontal displacement for trunk lateral translation is measured using a vertical line drawn up from mid-S1 or S2 tubercle. The amount of trunk shift (lateral translation) is measured as the displacement of the centroid (Risser-Ferguson method) of T12 vertebra from this vertical line in millimeters (Tx). Figure 2.
- Sacral unleveling is measured relative to a line drawn across the sacral base and compared with a true horizontal line (HB angle). Figure 2.
- Lumbo Sacral angle is the lower lumbar vertebra centroid line relative to the sacral base line and is the LS angle; this is similar to the FLSC in lumbar scoliotic deformity analysis. Figure 2.
- Lumbo-dorsal angle or mid lumbar scoliosis angle is similar in concept to a Cobb angle but it uses all the vertebrae to create the angle and thus is more representative of actual lumbar coronal bending alignment. Figure 2.
2.3. Data analysis
3. Results
Participant demographics and characteristics
4. Discussion
4.1. Radiological parameters.
4.2. Limitations and future investigations.
4.3. Conclusions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alexander, C.; Varacallo, M. Lumbosacral radiculopathy. StatPearls 2022, 1–8.
- Hahne, Andrew J. BPhysio*; Ford, Jon J. PhD*; McMeeken, Joan M. MSc†. Conservative management of lumbar disc herniation with associated radiculopathy: A systematic review. Spine 35(11):p E488-E504, May 15, 2010. [CrossRef]
- Lewis RA, Williams NH, Sutton AJ, et al. Comparative clinical effectiveness of management strategies for sciatica: systematic review and network meta-analyses. Spine J. 2015;15(6):1461 1477.
- Yang S, Kim W, Kong HH, Do KH, Choi KH. Epidural steroid injection versus conservative treatment for patients with lumbosacral radicular pain: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99(30):e21283. [CrossRef]
- Vanti C, Saccardo K, Panizzolo A, Turone L, Guccione AA, Pillastrini P. The effects of the addition of mechanical traction to physical therapy on low back pain? A systematic review with meta-analysis. Acta Orthop Traumatol Turc. 2023;57(1):3-16. [CrossRef]
- Azharuddin, A.; Aryandono, T.; Magetsari, R.; Dwiprahasto, I. Predictors of the conservative management outcomes in patients with lumbar herniated nucleus pulposus: A prospective study in Indonesia. Asian J. Surg. 2022, 45, 277–283. [CrossRef]
- Parker, S.L.; Godil, S.S.; Mendenhall, S.K.; Zuckerman, S.L.; Shau, D.N.; Mcgirt, M.J. Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc Herniation): A value analysis of cost, pain, disability, and quality of life: clinical article. J. Neurosurg. Spine 2014, 21, 143–149. [CrossRef]
- Suri, P.; Rainville, J.; Gellhorn, A. Predictors of patient-reported recovery from motor or sensory deficits two years after acute symptomatic lumbar disk herniation. PM R 2012, 4. [CrossRef]
- Varlotta, C.G.; Ge, D.H.; Stekas, N.; Frangella, N.J.; Manning, J.H.; Steinmetz, L.; Vasquez-Montes, D.; Errico, T.J.; Bendo, J.A.; Kim, Y.H.; et al. MRI radiological predictors of requiring microscopic lumbar discectomy after lumbar disc herniation. Glob. spine J. 2020, 10, 63–68. [CrossRef]
- Chun, S.W.; Lim, C.Y.; Kim, K.; Hwang, J.; Chung, S.G. The relationship between low back pain and lumbar lordosis: A systematic review and meta-analysis. Spine J. 2017, 17, 1180–1191.
- Sadler, S.G.; Spink, M.J.; Ho, A.; De Jonge, X.J.; Chuter, V.H. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet. Disord. 2017, 18, 179.
- Mekhael, E.; El Rachkidi, R.; Saliby, R.M.; Nassim, N.; Semaan, K.; Massaad, A.; Karam, M.; Saade, M.; Ayoub, E.; Rteil, A.; et al. Functional assessment using 3D movement analysis can better predict health-related quality of life outcomes in patients with adult spinal deformity: A machine learning approach. Front. Surg. 2023, 10, 1166734. [Google Scholar] [CrossRef] [PubMed]
- Terran, J.; Schwab, F.; Shaffrey, C.I.; Smith, J.S.; Devos, P.; Ames, C.P.; Fu, K.M.; Burton, D.; Hostin, R.; Klineberg, E.; et al. The SRS-Schwab adult spinal deformity classification: Assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 2013, 73, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Pellisé, F.; Vila-Casademunt, A.; Ferrer, M.; Domingo-Sàbat, M.; Bagó, J.; Pérez-Grueso, F.J.; Alanay, A.; Mannion, A.F.; Acaroglu, E.; European Spine Study Group (ESSG). Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur. Spine J. 2015, 24, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Kyrölä, K.; Repo, J.; Mecklin, J.P.; Ylinen, J.; Kautiainen, H.; Häkkinen, A. Spinopelvic changes based on the simplified SRS-Schwab adult spinal deformity classification: relationships with disability and health-related quality of life in adult patients with prolonged degenerative spinal disorders. Spine 2018, 43, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A. Extension traction treatment for patients with discogenic lumbosacral radiculopathy: A randomized controlled trial. Clin. Rehabil. 2013, 27, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Moustafa IM, Diab AA. The effect of adding forward head posture corrective exercises in the management of lumbosacral radiculopathy: a randomized controlled study. J Manipulative Physiol Ther. 2015;38(3):167-178. [CrossRef]
- Moustafa IM, Diab AA, Harrison DE. The efficacy of cervical lordosis rehabilitation for nerve root function and pain in cervical spondylotic radiculopathy: A randomized trial with 2-year follow-up. J Clin Med. 2022;11(21):6515. Published 2022 Nov 2. [CrossRef]
- Moustafa IM, Diab AAM, Harrison DE. Does improvement towards a normal cervical sagittal configuration aid in the management of lumbosacral radiculopathy: A randomized controlled trial. J Clin Med. 2022;11(19):5768. Published 2022 Sep 29. [CrossRef]
- Acaroglu, E.; Guler, U.O.; Olgun, Z.D.; Yavuz, Y.; Pellise, F.; Domingo-Sabat, M.; Yakici, S.; Alanay, A.; Perez-Grueso, F.S.; Yavuz, Y. Multiple regression analysis of factors affecting health-related quality of life in adult spinal deformity. Spine Deform. 2015, 3, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Daubs, M.D.; Lenke, L.G.; Bridwell, K.H.; Kim, Y.J.; Hung, M.; Cheh, G.; Koester, L.A. Does correction of preoperative coronal imbalance make a difference in outcomes of adult patients with deformity? Spine (Phila. Pa. 1976). 2013, 38, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Koller, H.; Pfanz, C.; Meier, O.; Hitzl, W.; Mayer, M.; Bullmann, V.; Schulte, T.L. Factors influencing radiographic and clinical outcomes in adult scoliosis surgery: A study of 448 European patients. Eur. Spine J. 2016, 25, 532–548. [Google Scholar] [CrossRef] [PubMed]
- Ploumis, A.; Liu, H.; Mehbod, A.A.; Transfeldt, E.E.; Winter, R.B. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine (Phila. Pa. 1976). 2009, 34, 1581–1584. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman SL, Chanbour H, Hassan FM, et al. The lumbosacral fractional curve vs maximum coronal Cobb angle in adult spinal deformity patients with coronal malalignment: Which matters more? [published online ahead of print, 2023 Mar 29]. Global Spine J. 2023;21925682231161564. [CrossRef]
- Zhang Z, Liu T, Wang Y, Wang Z, Zheng G. Factors related to preoperative coronal malalignment in degenerative lumbar scoliosis: An analysis on coronal parameters. Orthop Surg. 2022;14(8):1846-1852.
- Zhang J, Wang Z, Chi P, Chi C. Directionality of lumbosacral fractional curve relative to C7 plumb line, a novel index associated with postoperative coronal imbalance in patients with degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2021;46(6):366-373. [CrossRef]
- Zhang J, Wang Z, Chi P, Chi C. Orientation of L4 coronal tilt relative to C7 plumb line as a predictor for postoperative coronal imbalance in patients with degenerative lumbar scoliosis. Sci Rep. 2020;10(1):16148. Published 2020 Sep 30. [CrossRef]
- Mysliwiec LW, Cholewicki J, Winkelpleck MD, Eis GP. MSU classification for herniated lumbar discs on MRI: toward developing objective criteria for surgical selection. Eur Spine J. 2010;19:1087–93. [CrossRef]
- Zeppieri, G.; George, S.Z. Patient-defined desired outcome, success criteria, and expectation in outpatient physical therapy: A longitudinal assessment. Health Qual. Life Outcomes 2017, 15. [Google Scholar] [CrossRef] [PubMed]
- Brown JL, Edwards PS, Atchison JW, Lafayette-Lucey A, Wittmer VT, Robinson ME. Affiliations expand. Defining patient-centered, multidimensional success criteria for treatment of chronic spine pain. Pain Med. 2008 ;9(7):851-62. [CrossRef]
- Harrison, D.E.; Holland, B.; Harrison, D.D.; Janik, T.J. Further reliability analysis of the harrison radiographic line-drawing methods: crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J. Manipulative Physiol. Ther. 2002, 25, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, A.; Bolm-Audorff, U.; Ditchen, D.; Ellegast, R.; Grifka, J.; Haerting, J.; Hofmann, F.; Jäger, M.; Linhardt, O.; Luttmann, A.; et al. Do occupational risks for low back pain differ from risks for specific lumbar disc diseases? Results of the German lumbar spine study (EPILIFT). Spine (Phila. Pa. 1976). 2017, 42, E1204–E1211. [Google Scholar] [CrossRef] [PubMed]
- Silverplats, K.; Lind, B.; Zoëga, B.; Halldin, K.; Gellerstedt, M.; Brisby, H.; Rutberg, L. Clinical factors of importance for outcome after lumbar disc herniation surgery: Long-term follow-up. Eur. Spine J. 2010, 19, 1459–1467. [Google Scholar] [CrossRef] [PubMed]
- Dionne, C.E.; Von Korff, M.; Koepsell, T.D.; Deyo, R.A.; Barlow, W.E.; Checkoway, H. Formal education and back pain: A review. J. Epidemiol. Community Heal. 2001, 55, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Hendrick, P.; Blake, H. Predictors of self-management in patients with chronic low back pain: A longitudinal study. BMC Musculoskelet. Disord. 2022, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Giles, L.G.F.; Taylor, J.R. Low-back pain associated with leg length inequality. Spine (Phila. Pa. 1976). 1981, 6, 510–521. [Google Scholar] [CrossRef] [PubMed]
- Sheha, E.D.; Steinhaus, M.E.; Kim, H.J.; Cunningham, M.E.; Fragomen, A.T.; Rozbruch, S.R. Leg-length discrepancy, functional scoliosis, and low back pain. JBJS Rev. 2018, 6, e6. [Google Scholar] [CrossRef] [PubMed]
- Friberg, O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine (Phila. Pa. 1976). 1983, 8, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Wiltse LL. The effect of the common anomalies of the lumbar spine upon disc degeneration and low back pain. Orthop Clin North Am. 1971;2(2):569-582.
- Khamis, S.; Carmeli, E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 2017, 57, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Gurney, B.; Mermier, C.; Robergs, R.; Gibson, A.; Rivero, D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J. Bone Jt. Surg. 2001, 83, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Harrison DE, Cailliet R, Betz JW, et al. A non-randomized clinical control trial of Harrison mirror image methods for correcting trunk list (lateral translations of the thoracic cage) in patients with chronic low back pain. Eur Spine J. 2005;14(2):155-162. [CrossRef]

| Demographic characteristics of the study participants | N = 901 |
|---|---|
| Age | 44 (38, 49) |
| BMI | |
| Normal | 66 (73.3%) |
| Obese | 24 (26.7%) |
| Gender | |
| Female | 41 (45.6%) |
| Male | 49 (54.4%) |
| Educational level | |
| Bachelor or Master | 68 (75.6%) |
| High school or less | 22 (24.4%) |
| Smoking | |
| Yes | 49 (54.4%) |
| No | 41 (45.6%) |
| Marital status | |
| Married | 83 (92.2%) |
| Not married | 7 (7.8%) |
| Type of dominant pain | |
| Bilateral | 27 (30.0%) |
| Unilateral | 63 (70.0%) |
| MSU Location | |
| AB | 68 (75.6%) |
| B or C | 22 (24.4%) |
| MSU Magnitude | |
| 3 | 7 (7.8%) |
| 2 | 83 (92.2%) |
| T12 S1 Centroid horizontal displacement | 7 (5, 10) |
| Sacral un-leveling | 3.00 (2.00, 5.38) |
| Lumbo-Sacral angle | 87 (86, 89) |
| Lumbo-dorsal angle | 7.5 (5.0, 10.0) |
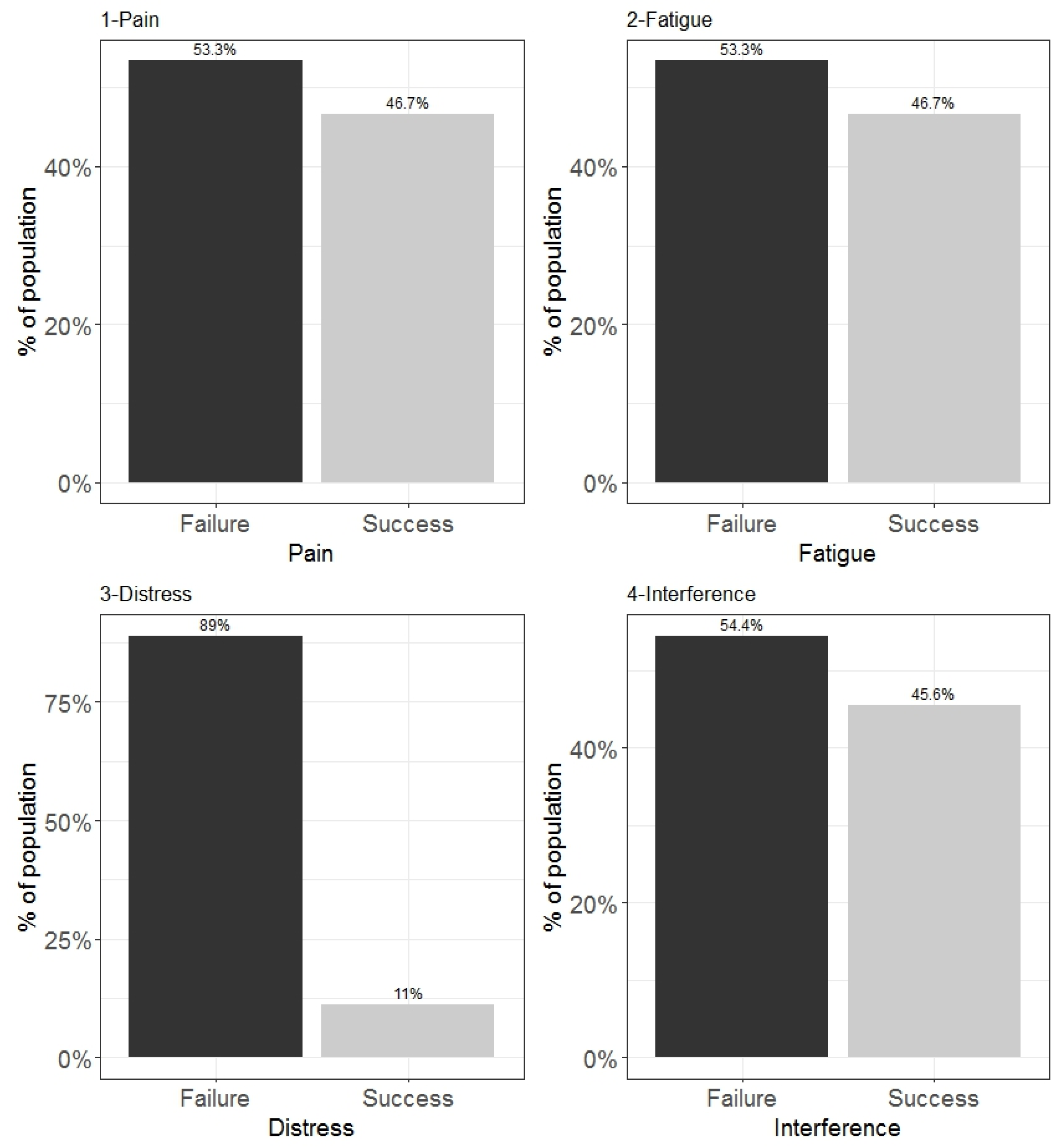
| Pain | |
| Failure | 48 (53.3%) |
| Success | 42 (46.7%) |
| Fatigue | |
| Failure | 48 (53.3%) |
| Success | 42 (46.7%) |
| Distress | |
| Failure | 80 (88.9%) |
| Success | 10 (11.1%) |
| Interference | |
| Failure | 49 (54.4%) |
| Success | 41 (45.6%) |
| Combined outcome (Pain, Fatigue, Distress, and Interference) | |
| Failure | 81 (90.0%) |
| Success | 9 (10.0%) |
| 1 Median (IQR); n (%) | |
| Demographic characteristics of the study participants | Gender | p-value2 | |
| Female, N = 411 |
Male, N = 491 |
||
| Age | 45 (42, 49) | 44 (37, 49) | 0.455 |
| BMI | 0.639 | ||
| Normal | 29 (70.7%) | 37 (75.5%) | |
| Obese | 12 (29.3%) | 12 (24.5%) | |
| Educational level | 0.615 | ||
| Bachelor or Master | 32 (78.0%) | 36 (73.5%) | |
| High school or less | 9 (22.0%) | 13 (26.5%) | |
| Smoking | 0.773 | ||
| Yes | 23 (56.1%) | 26 (53.1%) | |
| No | 18 (43.9%) | 23 (46.9%) | |
| Marital status | 0.121 | ||
| Married | 40 (97.6%) | 43 (87.8%) | |
| Not married | 1 (2.4%) | 6 (12.2%) | |
| Type of dominant pain | 0.890 | ||
| bilateral | 12 (29.3%) | 15 (30.6%) | |
| unilateral | 29 (70.7%) | 34 (69.4%) | |
| MSU Location | 0.615 | ||
| AB | 32 (78.0%) | 36 (73.5%) | |
| B or C | 9 (22.0%) | 13 (26.5%) | |
| MSU Magnitude | > 0.999 | ||
| 3 | 3 (7.3%) | 4 (8.2%) | |
| 2 | 38 (92.7%) | 45 (91.8%) | |
| T12 S1 Centroid horizontal displacement | 7 (5, 10) | 6 (4, 10) | 0.418 |
| Sacral un-leveling | 4.00 (2.00, 5.00) | 3.00 (2.00, 5.50) | 0.533 |
| Lumbo Sacral angle | 88.00 (87.00, 89.00) | 87.00 (86.00, 89.00) | 0.918 |
| Lumbo dorsal angle | 8.0 (6.0, 10.0) | 7.0 (5.0, 10.0) | 0.418 |
| Pain | 0.184 | ||
| Failure | 25 (61.0%) | 23 (46.9%) | |
| Success | 16 (39.0%) | 26 (53.1%) | |
| Fatigue | 0.184 | ||
| Failure | 25 (61.0%) | 23 (46.9%) | |
| Success | 16 (39.0%) | 26 (53.1%) | |
| Distress | 0.750 | ||
| Failure | 37 (90.2%) | 43 (87.8%) | |
| Success | 4 (9.8%) | 6 (12.2%) | |
| Interference | 0.255 | ||
| Failure | 25 (61.0%) | 24 (49.0%) | |
| Success | 16 (39.0%) | 25 (51.0%) | |
| Combined outcome | > 0.999 | ||
| Failure | 37 (90.2%) | 44 (89.8%) | |
| Success | 4 (9.8%) | 5 (10.2%) | |
| 1 Median (IQR); n (%) | |||
| 2 Wilcoxon rank sum test; Fisher's exact test; Pearson's Chi-squared test | |||
| T12 S1 Centroid horizontal displacement | Sacral unleveling | Lumbo Sacral angle | Lumbo dorsal angle | |
| T12 S1 Centroid horizontal displacement | 1 | |||
| Sacral unleveling | 0.994 (< .001) |
1 | ||
| Lumbosacral angle | -0.796 (< .001) |
-0.791 (< .001) |
1 | |
| Lumbodorsal angle | 0.995 (< .001) |
0.993 ( < .001) |
-0.794 (< .001) |
1 |
| Computed correlation used spearman-method with listwise-deletion. | ||||
| Pain | Fatigue | Distress | Interference | |||||
| Predictors of success | Odds Ratios (95% CI) | p | Odds Ratios (95% CI) |
p | Odds Ratios (95% CI) |
p | Odds Ratios (95% CI) |
P |
| Age | 0.85 (0.73 – 0.96) |
0.016 | 0.85 (0.73 – 0.96) |
0.016 | 0.88 (0.73 – 1.03) |
0.138 | 0.89 (0.79 – 0.99) |
0.042 |
| BMI [Obese] | 0.26 (0.03 – 1.78) |
0.187 | 0.26 (0.03 – 1.78) |
0.187 | 0.72 (0.01 – 26.33) |
0.866 | 0.16 (0.02 – 0.99) |
0.067 |
| Educational [High school or less] | 26.18 (3.36 – 365.34) |
0.006 | 26.18 (3.36 – 365.34) |
0.006 |
1.2 (0.98 - 46.45) |
0.8 | 7.50 (1.40 – 56.53) |
0.029 |
| Type of dominantpain [unilateral] | 1.33 (0.16 – 10.72) |
0.781 | 1.33 (0.16 – 10.72) |
0.781 | 1.35 (0.08 – 38.89) |
0.834 | 4.12 (0.61 – 31.65) |
0.150 |
| Smoking [No] | 1.40 (0.34 – 6.20) |
0.642 | 1.40 (0.34 – 6.20) |
0.642 | 0.33 (0.03 – 2.77) |
0.329 | 1.81 (0.47 – 7.64) |
0.393 |
| Marital status[Not married] | 1.54 (0.00 – 1487.04) |
0.943 | 1.54 (0.00 – 1487.04) |
0.943 | 2.31 (0.01 – 909.88) |
0.846 | ||
| MSU Location [B or C] | 2.58 (0.41 – 20.50) |
0.325 | 2.58 (0.41 – 20.50) |
0.325 | 0.07 (0.00 – 0.80) |
0.067 | 2.45 (0.44 – 16.65) |
0.320 |
| MSU Magnitude [2] | 0.06 (0.00 – 2.53) |
0.157 | 0.06 (0.00 – 2.53) |
0.157 | 0.10 (0.00 – 4.00) |
0.266 | ||
| Lumbo Sacral angle | 3.52 (1.94 – 8.03) |
<0.001 | 3.52 (1.94 – 8.03) |
<0.001 | 27.99 (4.99 – 473.94) |
0.003 | 2.55 (1.54 – 4.91) |
0.001 |
| Observations | 90 | 90 | 90 | 90 | ||||
| Dependent: | Crude OR | Adjusted OR | |
|---|---|---|---|
| Combined Outcome | |||
| Age | - | 1.01 (0.92 - 1.12, p = 0.836) | 0.92 (0.76 - 1.07, p = 0.296) |
| BMI | Normal | - | - |
| Obese | 0.32 (0.02 - 1.86, p = 0.289) | 0.85 (0.02 - 26.16, p = 0.926) | |
| Smoking | Yes | - | - |
| No | 0.57 (0.11 - 2.30, p = 0.442) | 0.62 (0.06 - 5.49, p = 0.665) | |
| MSU Location | AB | - | - |
| B or C | 0.87 (0.12 - 3.96, p = 0.870) | 0.12 (0.01 - 1.25, p = 0.115) | |
| Lumbo -sacral angle | - | 13.24 (3.52 - 98.70, p = 0.002) | 29.89 (4.95-504.31, p = 0.003) |
| Dependent= pain scores | Beta | 95% CI1 | p-value |
|---|---|---|---|
| Time | |||
| Baseline | — | — | |
| After completion of treatment | -47 | -51, -44 | < 0.001 |
| After 6 months | -38 | -42, -34 | < 0.001 |
| Age | 0.01 | -0.24, 0.25 | 0.960 |
| BMI | |||
| Normal | — | — | |
| Obese | 1.2 | -2.6, 4.9 | 0.540 |
| Gender | |||
| Female | — | — | |
| Male | -1.7 | -5.0, 1.6 | 0.303 |
| Educational level | |||
| Bachelor or Master | — | — | |
| High school or less | 3.0 | -1.6, 7.6 | 0.202 |
| Smoking | |||
| Yes | — | — | |
| No | -0.02 | -3.2, 3.1 | 0.991 |
| Marital status | |||
| Married | — | — | |
| Not married | -2.6 | -9.0, 3.9 | 0.437 |
| Type of dominant pain | |||
| Bilateral | — | — | |
| Unilateral | -2.7 | -7.3, 1.8 | 0.237 |
| MSU Location | |||
| AB | — | — | |
| B or C | 1.2 | -3.4, 5.8 | 0.614 |
| MSU Magnitude | |||
| 3 | — | — | |
| 2 | 0.61 | -7.6, 8.8 | 0.884 |
| Lumbo Sacral angle | -4.4 | -5.7, -3.2 | < 0.001 |
| 1 CI = Confidence Interval | |||
| Dependent= Fatigue scores | Beta | 95% CI1 | p-value |
|---|---|---|---|
| Time | |||
| Baseline | — | — | |
| After disposal | -48 | -51, -45 | < 0.001 |
| After 6 months | -31 | -36, -26 | < 0.001 |
| Age | 0.38 | 0.08, 0.67 | 0.012 |
| BMI | |||
| Normal | — | — | |
| Obese | 1.8 | -2.4, 6.1 | 0.399 |
| Gender | |||
| Female | — | — | |
| Male | -2.3 | -6.0, 1.4 | 0.232 |
| Educational level | |||
| Bachelor or Master | — | — | |
| High school or less | -7.6 | -13, -2.3 | 0.005 |
| Smoking | |||
| Yes | — | — | |
| No | -0.36 | -4.0, 3.2 | 0.842 |
| Marital status | |||
| Married | — | — | |
| Not married | 1.5 | -4.6, 7.7 | 0.626 |
| Type of dominant pain | |||
| Bilateral | — | — | |
| Unilateral | 1.3 | -3.7, 6.3 | 0.603 |
| MSU Location | |||
| AB | — | — | |
| B or C | 0.83 | -4.5, 6.1 | 0.759 |
| MSU Magnitude | |||
| 3 | — | — | |
| 2 | 7.3 | -0.88, 15 | 0.080 |
| Lumbo Sacral angle | -2.2 | -3.5, -0.92 | < 0.001 |
| 1 CI = Confidence Interval | |||
| Dependent= Distress scores | Beta | 95% CI1 | p-value |
|---|---|---|---|
| Time | |||
| Baseline | — | — | |
| After disposal | -42 | -46, -39 | < 0.001 |
| After 6 months | -19 | -24, -14 | < 0.001 |
| Age | 0.39 | 0.08, 0.69 | 0.013 |
| BMI | |||
| Normal | — | — | |
| Obese | -1.1 | -6.0, 3.7 | 0.645 |
| Gender | |||
| Female | — | — | |
| Male | -2.0 | -5.9, 1.8 | 0.300 |
| Educational level | |||
| Bachelor or Master | — | — | |
| High school or less | 1.1 | -3.7, 6.0 | 0.652 |
| Smoking | |||
| Yes | — | — | |
| No | 0.77 | -3.0, 4.6 | 0.690 |
| Marital status | |||
| Married | — | — | |
| Not married | -1.5 | -8.1, 5.2 | 0.667 |
| Type of dominant pain | |||
| Bilateral | — | — | |
| Unilateral | 0.04 | -5.9, 6.0 | 0.988 |
| MSU Location | |||
| AB | — | — | |
| B or C | -4.2 | -9.7, 1.4 | 0.142 |
| MSU Magnitude | |||
| 3 | — | — | |
| 2 | -4.8 | -13, 3.6 | 0.262 |
| Lumbosacral angle | -2.5 | -4.0, -1.0 | < 0.001 |
| 1 CI = Confidence Interval | |||
| Dependent=Interference scores | Beta | 95% CI1 | p-value |
|---|---|---|---|
| Time | |||
| Baseline | — | — | |
| After disposal | -49 | -52, -46 | < 0.001 |
| After 6 months | -28 | -32, -23 | < 0.001 |
| Age | 0.24 | -0.03, 0.52 | 0.086 |
| BMI | |||
| Normal | — | — | |
| Obese | 3.2 | -0.66, 7.2 | 0.104 |
| Gender | |||
| Female | — | — | |
| Male | -2.2 | -5.8, 1.4 | 0.225 |
| Educational level | |||
| Bachelor or Master | — | — | |
| High school or less | 1.6 | -3.7, 6.8 | 0.553 |
| Smoking | |||
| Yes | — | — | |
| No | 1.1 | -2.5, 4.6 | 0.554 |
| Marital status | |||
| Married | — | — | |
| Not married | 0.27 | -6.3, 6.9 | 0.936 |
| Type of dominant pain | |||
| Bilateral | — | — | |
| Unilateral | -3.8 | -8.7, 1.1 | 0.125 |
| MSU Location | |||
| AB | — | — | |
| B or C | 0.20 | -4.3, 4.7 | 0.932 |
| MSU Magnitude | |||
| 3 | — | — | |
| 2 | 6.0 | -2.9, 15 | 0.185 |
| Lumbo Sacral angle | -5.1 | -6.4, -3.9 | < 0.001 |
| 1 CI = Confidence Interval | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





