Submitted:
12 October 2023
Posted:
13 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
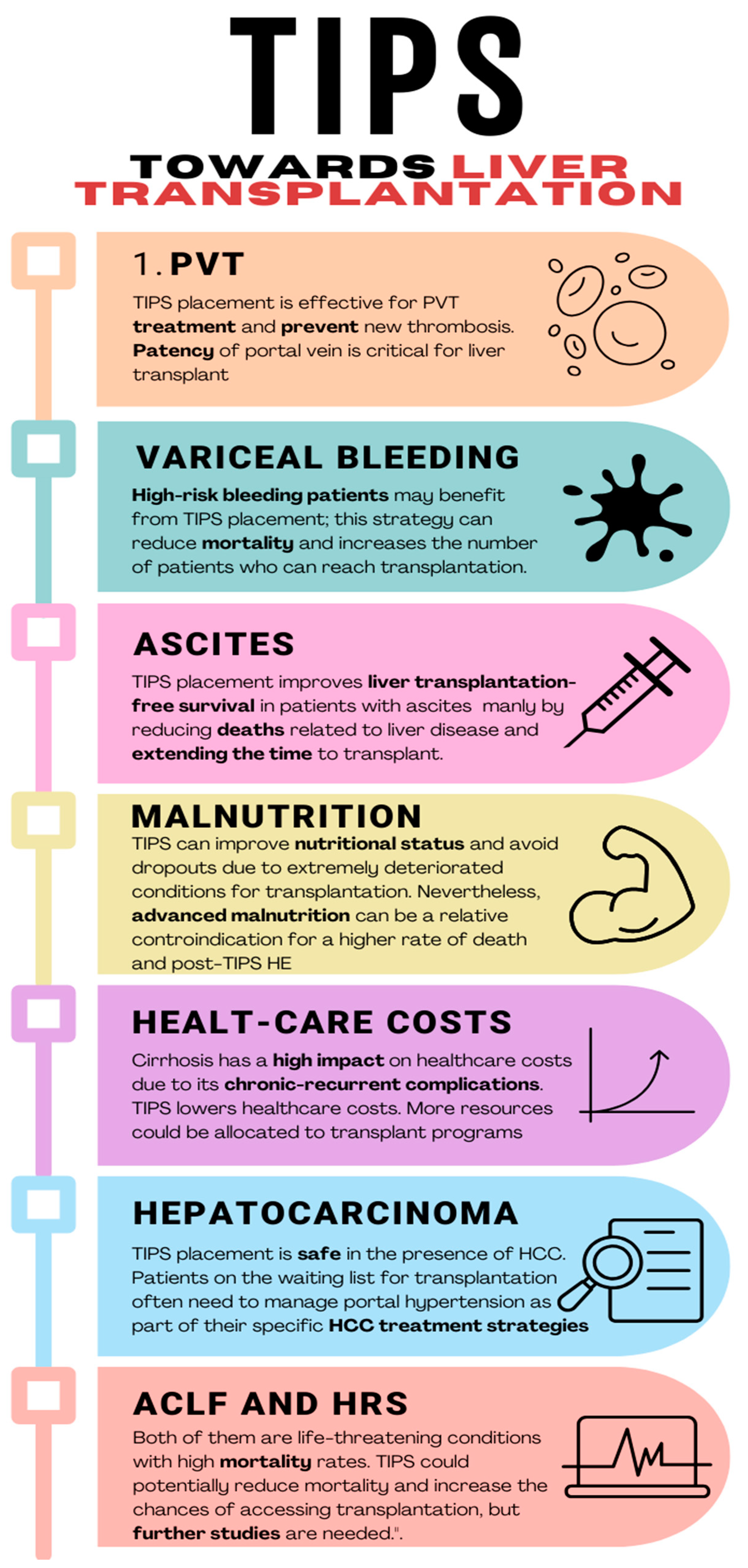
2. TIPS towards Liver Transplant: Role and Timing
3. TIPS in “Special” Liver Transplant Settings
3.1. Hepatocellular Carcinoma (HCC)
3.2. Acute-on-Chronic Liver Failure (ACLF)
3.3. Hepatorenal Syndrome
3.4. Cirrhotic Cardiomyopathy
4. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death.
- D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006 Jan;44(1):217-31. [CrossRef]
- D'Amico G, Morabito A, D'Amico M, Pasta L, Malizia G, Rebora P, Valsecchi MG. Clinical states of cirrhosis and competing risks. J Hepatol. 2018 Mar;68(3):563-576. [CrossRef]
- Rudler M, Mallet M, Sultanik P, Bouzbib C, Thabut D. Optimal management of ascites. Liver Int. 2020 Feb;40 Suppl 1:128-135. Erratum in: Liver Int. 2020 May;40(5):1247. [CrossRef]
- Jakab SS, Garcia-Tsao G. Evaluation and Management of Esophageal and Gastric Varices in Patients with Cirrhosis. Clin Liver Dis. 2020 Aug;24(3):335-350. [CrossRef]
- Smith M, Durham J. Evolving Indications for Tips. Tech Vasc Interv Radiol. 2016 Mar;19(1):36-41. [CrossRef]
- Larrue H, D'Amico G, Olivas P, Lv Y, Bucsics T, Rudler M, Sauerbruch T, Hernandez-Gea V, Han G, Reiberger T, Thabut D, Vinel JP, Péron JM, García-Pagán JC, Bureau C. TIPS prevents further decompensation and improves survival in patients with cirrhosis and portal hypertension in an individual patient data meta-analysis. J Hepatol. 2023 Sep;79(3):692-703. [CrossRef]
- Bodzin AS, Baker TB. Liver Transplantation Today: Where We Are Now and Where We Are Going. Liver Transpl. 2018 Oct;24(10):1470-1475. [CrossRef]
- de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C; Baveno VII Faculty. Baveno VII - Renewing consensus in portal hypertension. J Hepatol. 2022 Apr;76(4):959-974. [CrossRef]
- Tripathi D, Stanley AJ, Hayes PC, Travis S, Armstrong MJ, Tsochatzis EA, Rowe IA, Roslund N, Ireland H, Lomax M, Leithead JA, Mehrzad H, Aspinall RJ, McDonagh J, Patch D. Transjugular intrahepatic portosystemic stent-shunt in the management of portal hypertension. Gut. 2020 Jul;69(7):1173-1192. [CrossRef]
- Villanueva C, Torres F, Sarin SK, Shah HA, Tripathi D, Brujats A, Rodrigues SG, Bhardwaj A, Azam Z, Hayes PC, Jindal A, Abid S, Alvarado E, Bosch J; Carvedilol-IPD-MA-group and the Baveno Cooperation: an EASL Consortium. Carvedilol reduces the risk of decompensation and mortality in patients with compensated cirrhosis in a competing-risk meta-analysis. J Hepatol. 2022 Oct;77(4):1014-1025. [CrossRef]
- Sinagra E, Perricone G, D'Amico M, Tinè F, D'Amico G. Systematic review with meta-analysis: the haemodynamic effects of carvedilol compared with propranolol for portal hypertension in cirrhosis. Aliment Pharmacol Ther. 2014 Mar;39(6):557-68. [CrossRef]
- Delacôte C, Favre M, El Amrani M, Ningarhari M, Lemaitre E, Ntandja-Wandji LC, Bauvin P, Boleslawski E, Millet G, Truant S, Mathurin P, Louvet A, Canva V, Lebuffe G, Pruvot FR, Dharancy S, Lassailly G; French ABM study group. Morbid obesity increases death and dropout from the liver transplantation waiting list: A prospective cohort study. United European Gastroenterol J. 2022 May;10(4):396-408. [CrossRef]
- Montenovo M, Rahnemai-Azar A, Reyes J, Perkins J. Clinical Impact and Risk Factors of Portal Vein Thrombosis for Patients on Wait List for Liver Transplant. Exp Clin Transplant. 2018 Apr;16(2):166-171. [CrossRef]
- Ponziani FR, Zocco MA, Senzolo M, Pompili M, Gasbarrini A, Avolio AW. Portal vein thrombosis and liver transplantation: implications for waiting list period, surgical approach, early and late follow-up. Transplant Rev (Orlando). 2014 Apr;28(2):92-101. [CrossRef]
- Stine JG, Shah PM, Cornella SL, Rudnick SR, Ghabril MS, Stukenborg GJ, Northup PG. Portal vein thrombosis, mortality and hepatic decompensation in patients with cirrhosis: A meta-analysis. World J Hepatol. 2015 Nov 28;7(27):2774-80. [CrossRef]
- Ghabril M, Agarwal S, Lacerda M, Chalasani N, Kwo P, Tector AJ. Portal Vein Thrombosis Is a Risk Factor for Poor Early Outcomes After Liver Transplantation: Analysis of Risk Factors and Outcomes for Portal Vein Thrombosis in Waitlisted Patients. Transplantation. 2016 Jan;100(1):126-33. [CrossRef]
- Englesbe MJ, Kubus J, Muhammad W, Sonnenday CJ, Welling T, Punch JD, Lynch RJ, Marrero JA, Pelletier SJ. Portal vein thrombosis and survival in patients with cirrhosis. Liver Transpl. 2010 Jan;16(1):83-90. [CrossRef]
- Thornburg B, Desai K, Hickey R, Kulik L, Ganger D, Baker T, Abecassis M, Lewandowski RJ, Salem R. Portal Vein Recanalization and Transjugular Intrahepatic Portosystemic Shunt Creation for Chronic Portal Vein Thrombosis: Technical Considerations. Tech Vasc Interv Radiol. 2016 Mar;19(1):52-60. [CrossRef]
- Salem R, Vouche M, Baker T, Herrero JI, Caicedo JC, Fryer J, Hickey R, Habib A, Abecassis M, Koller F, Vogelzang R, Desai K, Thornburg B, Hohlastos E, Resnick S, Lewandowski RJ, Sato K, Ryu RK, Ganger D, Kulik L. Pretransplant Portal Vein Recanalization-Transjugular Intrahepatic Portosystemic Shunt in Patients With Complete Obliterative Portal Vein Thrombosis. Transplantation. 2015 Nov;99(11):2347-55. [CrossRef]
- Lapenna L, Di Cola S, Gazda J, De Felice I, Gioia S, Merli M. New Indications for TIPSs: What Do We Know So Far? J Clin Exp Hepatol. 2023 Sep-Oct;13(5):794-803. [CrossRef]
- Rodrigues SG, Sixt S, Abraldes JG, De Gottardi A, Klinger C, Bosch J, Baumgartner I, Berzigotti A. Systematic review with meta-analysis: portal vein recanalisation and transjugular intrahepatic portosystemic shunt for portal vein thrombosis. Aliment Pharmacol Ther. 2019 Jan;49(1):20-30. [CrossRef]
- Asrani SK, Kamath PS. Natural history of cirrhosis. Curr Gastroenterol Rep. 2013 Feb;15(2):308. [CrossRef]
- Monescillo A, Martínez-Lagares F, Ruiz-del-Arbol L, Sierra A, Guevara C, Jiménez E, Marrero JM, Buceta E, Sánchez J, Castellot A, Peñate M, Cruz A, Peña E. Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology. 2004 Oct;40(4):793-801. [CrossRef]
- García-Pagán JC, Caca K, Bureau C, Laleman W, Appenrodt B, Luca A, Abraldes JG, Nevens F, Vinel JP, Mössner J, Bosch J; Early TIPS (Transjugular Intrahepatic Portosystemic Shunt) Cooperative Study Group. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010 Jun 24;362(25):2370-9. [CrossRef]
- Manning C, Elzubeir A, Alam S. The role of pre-emptive Transjugular Intrahepatic Portosystemic Shunt in acute variceal bleeding: a literature review. Ther Adv Chronic Dis. 2021 Mar 5;12:2040622321995771. [CrossRef]
- Hussain I, Wong YJ, Lohan R, Lin S, Kumar R. Does preemptive transjugular intrahepatic portosystemic shunt improve survival after acute variceal bleeding? Systematic review, meta-analysis, and trial sequential analysis of randomized trials. J Gastroenterol Hepatol. 2022 Mar;37(3):455-463. [CrossRef]
- Arroyo V, Colmenero J. Ascites and hepatorenal syndrome in cirrhosis: pathophysiological basis of therapy and current management. J Hepatol. 2003;38 Suppl 1:S69-89. [CrossRef]
- Ginès P, Uriz J, Calahorra B, Garcia-Tsao G, Kamath PS, Del Arbol LR, Planas R, Bosch J, Arroyo V, Rodés J. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology. 2002 Dec;123(6):1839-47. [CrossRef]
- Narahara Y, Kanazawa H, Fukuda T, Matsushita Y, Harimoto H, Kidokoro H, Katakura T, Atsukawa M, Taki Y, Kimura Y, Nakatsuka K, Sakamoto C. Transjugular intrahepatic portosystemic shunt versus paracentesis plus albumin in patients with refractory ascites who have good hepatic and renal function: a prospective randomized trial. J Gastroenterol. 2011 Jan;46(1):78-85. [CrossRef]
- D'Amico G, Luca A, Morabito A, Miraglia R, D'Amico M. Uncovered transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis. Gastroenterology. 2005 Oct;129(4):1282-93. [CrossRef]
- Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007 Sep;133(3):825-34. Erratum in: Gastroenterology. 2007 Nov;133(5):1746. [CrossRef]
- Bai M, Qi XS, Yang ZP, Yang M, Fan DM, Han GH. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: an updated meta-analysis. World J Gastroenterol. 2014 Mar 14;20(10):2704-14. [CrossRef]
- Gaba RC, Parvinian A, Casadaban LC, Couture PM, Zivin SP, Lakhoo J, Minocha J, Ray CE Jr, Knuttinen MG, Bui JT. Survival benefit of TIPS versus serial paracentesis in patients with refractory ascites: a single institution case-control propensity score analysis. Clin Radiol. 2015 May;70(5):e51-7. [CrossRef]
- Ronald J, Rao R, Choi SS, Kappus M, Martin JG, Sag AA, Pabon-Ramos WM, Suhocki PV, Smith TP, Kim CY. No Increased Mortality After TIPS Compared with Serial Large Volume Paracenteses in Patients with Higher Model for End-Stage Liver Disease Score and Refractory Ascites. Cardiovasc Intervent Radiol. 2019 May;42(5):720-728. [CrossRef]
- Bischoff SC, Bernal W, Dasarathy S, Merli M, Plank LD, Schütz T, Plauth M. ESPEN practical guideline: Clinical nutrition in liver disease. Clin Nutr. 2020 Dec;39(12):3533-3562. [CrossRef]
- European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; European Association for the Study of the Liver. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J Hepatol. 2019 Jan;70(1):172-193. [CrossRef]
- Amodio P, Bemeur C, Butterworth R, Cordoba J, Kato A, Montagnese S, Uribe M, Vilstrup H, Morgan MY. The nutritional management of hepatic encephalopathy in patients with cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology. 2013 Jul;58(1):325-36. [CrossRef]
- Merli M, Giusto M, Molfino A, Bonetto A, Rossi M, Ginanni Corradini S, Baccino FM, Rossi Fanelli F, Costelli P, Muscaritoli M. MuRF-1 and p-GSK3β expression in muscle atrophy of cirrhosis. Liver Int. 2013 May;33(5):714-21. [CrossRef]
- Kim G, Kang SH, Kim MY, Baik SK. Prognostic value of sarcopenia in patients with liver cirrhosis: A systematic review and meta-analysis. PLoS One. 2017 Oct 24;12(10):e0186990. [CrossRef]
- Lattanzi B, Nardelli S, Pigliacelli A, Di Cola S, Farcomeni A, D'Ambrosio D, Gioia S, Ginanni Corradini S, Lucidi C, Mennini G, Rossi M, Merli M, Riggio O. The additive value of sarcopenia, myosteatosis and hepatic encephalopathy in the predictivity of model for end-stage liver disease. Dig Liver Dis. 2019 Nov;51(11):1508-1512. [CrossRef]
- Merli M, Giusto M, Giannelli V, Lucidi C, Riggio O. Nutritional status and liver transplantation. J Clin Exp Hepatol. 2011 Dec;1(3):190-8. [CrossRef]
- Mangana Del Rio T, Sacleux SC, Vionnet J, Ichaï P, Denys A, Schneider A, Coilly A, Fraga M, Wetzel A, Koerfer J, Chiche JD, Saliba F, Moradpour D, Becce F, Artru F. Body composition and short-term mortality in patients critically ill with acute-on-chronic liver failure. JHEP Rep. 2023 Apr 7;5(8):100758. [CrossRef]
- Nardelli S, Lattanzi B, Torrisi S, Greco F, Farcomeni A, Gioia S, Merli M, Riggio O. Sarcopenia Is Risk Factor for Development of Hepatic Encephalopathy After Transjugular Intrahepatic Portosystemic Shunt Placement. Clin Gastroenterol Hepatol. 2017 Jun;15(6):934-936. [CrossRef]
- Praktiknjo M, Clees C, Pigliacelli A, Fischer S, Jansen C, Lehmann J, Pohlmann A, Lattanzi B, Krabbe VK, Strassburg CP, Arroyo V, Merli M, Meyer C, Trebicka J. Sarcopenia Is Associated With Development of Acute-on-Chronic Liver Failure in Decompensated Liver Cirrhosis Receiving Transjugular Intrahepatic Portosystemic Shunt. Clin Transl Gastroenterol. 2019 Apr;10(4):e00025. [CrossRef]
- Gazda J, Di Cola S, Lapenna L, Khan S, Merli M. The Impact of Transjugular Intrahepatic Portosystemic Shunt on Nutrition in Liver Cirrhosis Patients: A Systematic Review. Nutrients. 2023 Mar 27;15(7):1617. [CrossRef]
- Montomoli J, Holland-Fischer P, Bianchi G, Grønbaek H, Vilstrup H, Marchesini G, Zoli M. Body composition changes after transjugular intrahepatic portosystemic shunt in patients with cirrhosis. World J Gastroenterol. 2010 Jan 21;16(3):348-53. [CrossRef]
- Bañares R, Albillos A, Nakum M, Gea S, Varghese A, Green W. An Economic Analysis of Transjugular Intrahepatic Portosystemic Covered Stent Shunt for Variceal Bleeding and Refractory Ascites in a Spanish Setting. Adv Ther. 2023 Jul;40(7):3006-3020. [CrossRef]
- Casadaban LC, Parvinian A, Couture PM, Minocha J, Knuttinen MG, Bui JT, Gaba RC. Characterization of liver function parameter alterations after transjugular intrahepatic portosystemic shunt creation and association with early mortality. AJR Am J Roentgenol. 2014 Dec;203(6):1363-70. [CrossRef]
- Vizzutti F, Arena U, Rega L, Zipoli M, Abraldes JG, Romanelli RG, Tarquini R, Laffi G, Pinzani M. Liver failure complicating segmental hepatic ischaemia induced by a PTFE-coated TIPS stent. Gut. 2009 Apr;58(4):582-4. [CrossRef]
- 51. Cazzaniga M, Salerno F, Pagnozzi G, et al. Diastolic dysfunction is associated with poor survival in patients with cirrhosis with transjugular intrahepatic portosystemic shunt. Gut.
- 52. Billey C, Billet S, Robic MA, et al. A prospective study identifying predictive factors of cardiac decompensation after TIPS: the Toulouse algorithm. Hepatology.
- Riggio O, Angeloni S, Salvatori FM, De Santis A, Cerini F, Farcomeni A, Attili AF, Merli M. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol. 2008 Nov;103(11):2738-46. [CrossRef]
- Riggio O, Nardelli S, Moscucci F, Pasquale C, Ridola L, Merli M. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Clin Liver Dis. 2012 Feb;16(1):133-46. [CrossRef]
- Bureau C, Thabut D, Jezequel C, Archambeaud I, D'Alteroche L, Dharancy S, Borentain P, Oberti F, Plessier A, De Ledinghen V, Ganne-Carrié N, Carbonell N, Rousseau V, Sommet A, Péron JM, Vinel JP. The Use of Rifaximin in the Prevention of Overt Hepatic Encephalopathy After Transjugular Intrahepatic Portosystemic Shunt : A Randomized Controlled Trial. Ann Intern Med. 2021 May;174(5):633-640. [CrossRef]
- 2023.
- Unger LW, Stork T, Bucsics T, Rasoul-Rockenschaub S, Staufer K, Trauner M, Maschke S, Pawloff M, Soliman T, Reiberger T, Berlakovich GA. The role of TIPS in the management of liver transplant candidates. United European Gastroenterol J. 2017 Dec;5(8):1100-1107. [CrossRef]
- Freeman RB Jr, FitzMaurice SE, Greenfield AE, Halin N, Haug CE, Rohrer RJ. Is the transjugular intrahepatic portocaval shunt procedure beneficial for liver transplant recipients? Transplantation. 1994 Aug 15;58(3):297-300. Erratum in: Transplantation 1994 Nov 27;58(10):1144.
- Menegaux F, Baker E, Keeffe EB, Monge H, Egawa H, Esquivel CO. Impact of transjugular intrahepatic portosystemic shunt on orthotopic liver transplantation. World J Surg. 1994 Nov-Dec;18(6):866-70; discussion 870-1. [CrossRef]
- Martin M, Zajko AB, Orons PD, Dodd G, Wright H, Colangelo J, Tartar R. Transjugular intrahepatic portosystemic shunt in the management of variceal bleeding: indications and clinical results. Surgery. 1993 Oct;114(4):719-26; discussion 726-7.
- Woodle ES, Darcy M, White HM, Perdrizet GA, Vesely TM, Picus D, Hicks M, So SK, Jendrisak MD, McCullough CS, et al. Intrahepatic portosystemic vascular stents: a bridge to hepatic transplantation. Surgery. 1993 Mar;113(3):344-51.
- Moreno A, Meneu JC, Moreno E, Fraile M, García I, Loinaz C, Abradelo M, Jiménez C, Gomez R, García-Sesma A, Manrique A, Gimeno A. Liver transplantation and transjugular intrahepatic portosystemic shunt. Transplant Proc. 2003 Aug;35(5):1869-70. [CrossRef]
- Dell'Era A, Grande L, Barros-Schelotto P, Turnes J, Fuster J, Charco R, García-Valdecasas JC, Bosch J, García-Pagán JC. Impact of prior portosystemic shunt procedures on outcome of liver transplantation. Surgery. 2005 Jun;137(6):620-5. [CrossRef]
- Guerrini GP, Pleguezuelo M, Maimone S, Calvaruso V, Xirouchakis E, Patch D, Rolando N, Davidson B, Rolles K, Burroughs A. Impact of tips preliver transplantation for the outcome posttransplantation. Am J Transplant. 2009 Jan;9(1):192-200. [CrossRef]
- Barbier L, Hardwigsen J, Borentain P, Biance N, Daghfous A, Louis G, Botta-Fridlund D, Le Treut YP. Impact of transjugular intrahepatic portosystemic shunting on liver transplantation: 12-year single-center experience. Clin Res Hepatol Gastroenterol. 2014 Apr;38(2):155-63. [CrossRef]
- Sellers CM, Nezami N, Schilsky ML, Kim HS. Transjugular intrahepatic portosystemic shunt as a bridge to liver transplant: Current state and future directions. Transplant Rev (Orlando). 2019 Apr;33(2):64-71. [CrossRef]
- Balducci D, Montori M, De Blasio F, Di Bucchianico A, Argenziano ME, Baroni GS, Scarpellini E. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in Treating Portal Hypertension in Patients with Hepatocellular Carcinoma. Medicina (Kaunas). 2023 Jun 15;59(6):1150. [CrossRef]
- Chen, Z.X. , Qiu Z.K., Wang G.B., Wang G.S., Jiang W.W., Gao F. Safety and effectiveness of transjugular intrahepatic portosystemic shunt in hepatocellular carcinoma patients with portal hypertension: A systematic review and meta-analysis. Clin. Radiol. [CrossRef]
- Bjørneboe M, Andersen JR, Christensen U, Skinhøj P, Jensen OM. Does a portal-systemic shunt increase the risk of primary hepatic carcinoma in cirrhosis of the liver? Scand J Gastroenterol. 1985 Jan;20(1):59-64. [CrossRef]
- Bañares R, Núñez O, Escudero M, Fernández C, Vaquero J, Beceiro I, Echenagusía A, Clemente G, Santos L. Patients with cirrhosis and bare-stent TIPS may have increased risk of hepatocellular carcinoma. Hepatology. 2005 Mar;41(3):566-71. [CrossRef]
- Chen, B. , Pang L., Chen HBin Wu D.B., Wang Y.H., Chen E.Q. TIPS Is Not Associated with a Higher Risk of Developing HCC in Cirrhotic Patients: A Systematic Review and Meta-analysis. J. Clin. Transl. Hepatol. [CrossRef]
- Kang, J.W. , Kim J.H., Ko G.Y., Gwon DIl Yoon H.K., Sung K.B. Transarterial chemoembolization for hepatocellular carcinoma after transjugular intrahepatic portosystemic shunt. Acta Radiol. [CrossRef]
- Tesdal IK, Wikström M, Flechtenmacher C, Filser T, Dueber C. Percutaneous treatment of hepatocellular carcinoma in patients with transjugular intrahepatic portosystemic shunts. Cardiovasc Intervent Radiol. 2006 Sep-Oct;29(5):778-84. [CrossRef]
- Wang, Z. , Zhang H., Zhao H., Wang X., Tsauo J., Luo X., Li X. Repeated transcatheter arterial chemoembolization is safe for hepatocellular carcinoma in cirrhotic patients with transjugular intrahepatic portosystemic shunt. Diagn. Interv. Radiol. [CrossRef]
- Donahue LA, Kulik L, Baker T, Ganger DR, Gupta R, Memon K, Abecassis MM, Salem R, Lewandowski RJ. Yttrium-90 radioembolization for the treatment of unresectable hepatocellular carcinoma in patients with transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 2013 Jan;24(1):74-80. [CrossRef]
- Park JK, Al-Tariq QZ, Zaw TM, Raman SS, Lu DS. Radiofrequency Ablation for the Treatment of Hepatocellular Carcinoma in Patients with Transjugular Intrahepatic Portosystemic Shunts. Cardiovasc Intervent Radiol. 2015 Oct;38(5):1211-7. [CrossRef]
- Kohi MP, Fidelman N, Naeger DM, LaBerge JM, Gordon RL, Kerlan RK Jr. Hepatotoxicity after transarterial chemoembolization and transjugular intrahepatic portosystemic shunt: do two rights make a wrong? J Vasc Interv Radiol. 2013 Jan;24(1):68-73. [CrossRef]
- Kuo YC, Kohi MP, Naeger DM, Tong RT, Kolli KP, Taylor AG, Laberge JM, Kerlan RK Jr, Fidelman N. Efficacy of TACE in TIPS patients: comparison of treatment response to chemoembolization for hepatocellular carcinoma in patients with and without a transjugular intrahepatic portosystemic shunt. Cardiovasc Intervent Radiol. 2013 Oct;36(5):1336-43. [CrossRef]
- Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, Durand F, Gustot T, Saliba F, Domenicali M, Gerbes A, Wendon J, Alessandria C, Laleman W, Zeuzem S, Trebicka J, Bernardi M, Arroyo V; CANONIC Study Investigators of the EASL–CLIF Consortium. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013 Jun; 144(7): 1426-37, 1437. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018 Aug;69(2):406-460. Erratum in: J Hepatol. 2018 Nov;69(5):1207. [CrossRef]
- Gu W, Kimmann M, Laleman W, Praktiknjo M, Trebicka J. To TIPS or Not to TIPS in High Risk of Variceal Rebleeding and Acute-on-Chronic Liver Failure. Semin Liver Dis. 2023 May;43(2):189-205. [CrossRef]
- Wong F, Pantea L, Sniderman K. Midodrine, octreotide, albumin, and TIPS in selected patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology. 2004 Jul;40(1):55-64. [CrossRef]
- Testino G, Leone S, Ferro C, Borro P. Severe acute alcoholic hepatitis and hepatorenal syndrome: role of transjugular intrahepatic portosystemic stent shunt. J Med Life. 2012 Jun 12;5(2):203-5. Epub 2012 Jun 18.
- Brensing KA, Textor J, Perz J, Schiedermaier P, Raab P, Strunk H, Klehr HU, Kramer HJ, Spengler U, Schild H, Sauerbruch T. Long term outcome after transjugular intrahepatic portosystemic stent-shunt in non-transplant cirrhotics with hepatorenal syndrome: a phase II study. Gut. 2000 Aug;47(2):288-95. [CrossRef]
- Song T, Rössle M, He F, Liu F, Guo X, Qi X. Transjugular intrahepatic portosystemic shunt for hepatorenal syndrome: A systematic review and meta-analysis. Dig Liver Dis. 2018 Apr;50(4):323-330. [CrossRef]
- Ripoll C, Platzer S, Franken P, Aschenbach R, Wienke A, Schuhmacher U, Teichgräber U, Stallmach A, Steighardt J, Zipprich A; Liver-HERO Study Group. Liver-HERO: hepatorenal syndrome-acute kidney injury (HRS-AKI) treatment with transjugular intrahepatic portosystemic shunt in patients with cirrhosis-a randomized controlled trial. Trials. 2023 Apr 5;24(1):258. [CrossRef]
- Ripoll C, Platzer S, Franken P, Aschenbach R, Wienke A, Schuhmacher U, Teichgräber U, Stallmach A, Steighardt J, Zipprich A; Liver-HERO Study Group. Liver-HERO: hepatorenal syndrome-acute kidney injury (HRS-AKI) treatment with transjugular intrahepatic portosystemic shunt in patients with cirrhosis-a randomized controlled trial. Trials. 2023 Apr 5;24(1):258. [CrossRef]
- Kaur H, Premkumar M. Diagnosis and Management of Cirrhotic Cardiomyopathy. J Clin Exp Hepatol. 2022 Jan-Feb;12(1):186-199. [CrossRef]
- Premkumar M, Devurgowda D, Vyas T, Shasthry SM, Khumuckham JS, Goyal R, Thomas SS, Kumar G. Left Ventricular Diastolic Dysfunction is Associated with Renal Dysfunction, Poor Survival and Low Health Related Quality of Life in Cirrhosis. J Clin Exp Hepatol. 2019 May-Jun;9(3):324-333. [CrossRef]
- Merli M, Valeriano V, Funaro S, Attili AF, Masini A, Efrati C, De CS, Riggio O. Modifications of cardiac function in cirrhotic patients treated with transjugular intrahepatic portosystemic shunt (TIPS). Am J Gastroenterol. 2002 Jan;97(1):142-8. [CrossRef]
- Radunski UK, Kluwe J, Klein M, Galante A, Lund GK, Sinning C, Bohnen S, Tahir E, Starekova J, Bannas P, Stehning C, Adam G, Lohse AW, Blankenberg S, Muellerleile K, Benten D. Cardiovascular magnetic resonance demonstrates structural cardiac changes following transjugular intrahepatic portosystemic shunt. Sci Rep. 2021 Jun 16;11(1):12719. [CrossRef]
- Filì D, Falletta C, Luca A, Hernandez Baravoglia C, Clemenza F, Miraglia R, Scardulla C, Tuzzolino F, Vizzini G, Gridelli B, Bosch J. Circulatory response to volume expansion and transjugular intrahepatic portosystemic shunt in refractory ascites: Relationship with diastolic dysfunction. Dig Liver Dis. 2015 Dec;47(12):1052-8. [CrossRef]
- Meucci MC, Hoogerduijn Strating MM, Butcher SC, van Rijswijk CSP, Van Hoek B, Delgado V, Bax JJ, Tushuizen ME, Marsan NA. Left atrial dysfunction is an independent predictor of mortality in patients with cirrhosis treated by transjugular intrahepatic portosystemic shunt. Hepatol Commun. 2022 Nov;6(11):3163-3174. [CrossRef]
- Rabie RN, Cazzaniga M, Salerno F, Wong F. The use of E/A ratio as a predictor of outcome in cirrhotic patients treated with transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 2009 Oct;104(10):2458-66. Erratum in: Am J Gastroenterol. 2009 Aug;104(8):2128. [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




