1. Introduction
Localized damage to the skin and underlying tissues at the site of bony prominence due to sustained pressure or shear force has been referred to as bed sores, pressure sores, and pressure ulcers, with the most recent term being pressure injury (PI) [
1]. The number of PI patients in Korea increased by 9.1% from 23,354 in 2017 to 25,843 in 2021 [
2]. The prevalence of PI varies widely depending on the type of medical institution and patient population, with the prevalence of PI ranging from 3.9–39.0% in general wards and 14.9–33.0% in intensive care units in foreign countries [
3,
4], to 9.7–12.0% in general wards [
5,
6] and 28.2–45.5% in intensive care units [
7,
8] in Korea. In acute care hospitals, PI is most likely to occur within two weeks of admission [
7], and in ICU, the risk of PI is even higher, with PI occurring mostly within 72 hours of admission [
9] and are reported to increase mortality by two to four times in elderly patients [
8].
In addition to the economic losses associated with prolonged hospitalization and unnecessary medical expenditures for treatment and testing, PI outbreaks can lead to complications such as infection and even death if initial PI assessment and treatment are not provided appropriately [
10]. Thus, PI prevention and management ensures patient safety and reduces medical costs, and many hospitals are actively performing preventive nursing care for PI, as PI-related items are included as evaluation data in the medical institution certification evaluation. PI is one of the activities for patient safety, and preventing and managing PI and evaluating the healing status is an important part of improving the quality of nursing care. The independent activities of nurses for preventing and managing PI should be based on the latest evidence [
11].
The nurses’ role is to assess risk factors through daily direct nursing care by palpating the skin at PI-prone sites to identify the early stages of preventable PI and if present, provide necessary interventions to prevent them worsening [
12]. Accurately assessing PI and providing scientifically based nursing care is an important step [
13]. In particular, nurses' abilities to differentiate between pre and evident PI, incorporating the stages of PI during skin assessment is critical [
6].
The National Pressure Ulcer Advisory Panel (NPUAP) and the European Pressure Ulcer Advisory Panel (EPUAP) heavily informed the NPUAP-EPUAP International Classification System (2007) publication for PIs. After adopting the term “pressure injury” to include skin lesions without ulceration, it was renamed the National Pressure Injury Advisory Panel (NPIAP), which revised its classification in 2016 to include six stages: Ⅰ, Ⅱ, Ⅲ, Ⅳ, unstageable PI, and, lastly, deep tissue pressure injury (DTPI) [
14].
Conversely, incontinence-associated dermatitis (IAD) is an incontinence-related skin problem that results in inflammation and erythema due to prolonged exposure of the tissue to moisture from incontinence, enzyme irritation from feces, and perspiration [
15]. IAD contributes to and aggravates the development of PI and since 2000, PI and IAD have been evaluated separately [
16]. The perineal area, where incontinence typically occurs, is anatomically close to the PI trigger site, and the high-risk populations for IAD and PI are similar [
17]. Hence, differentiating between IAD and PI is challenging and can lead to inappropriate preventive care, treatment, reporting errors, and serious problems with nursing quality indicators [
18], hence there is a need to improve nurses' ability to differentiate between the two conditions to select the appropriate management approach based on the cause of the occurrence [
19].
Nurses' knowledge is important for improving PI nursing performance [
20]. The knowledge-attitude-practice (K-A-P) model [
21], which is utilized to explain human performance, shows that performance is influenced by knowledge and attitude. It has been reported that nurses' PI nursing performance is low because nurses' lack of PI nursing knowledge leads to poor understanding of PI-related practices [
22], and lack of PI nursing knowledge and skeptical attitudes toward PI nursing negatively affect PI nursing performance [
23]. It has also been shown that the higher the actual PI nursing knowledge, the higher the PI nursing performance [
24].
Therefore, it is important for nurses to develop accurate knowledge of PI and IAD to accurately assess PI, detect it early, and provide efficient nursing care. However, previous studies in Korea have shown that nurses' knowledge of PI is not high [
25,
26] and, in particular, their knowledge of PI status is relatively low compared to their knowledge of treatment and prevention of PI [
27].
As PI assessment is the starting point for appropriate PI prevention nursing care, it is important to accurately determine nurses' knowledge of PI assessment, which should be assessed by utilizing a visual differentiation ability test in conjunction with knowledge of their ability to accurately assess PI. In fact, there are previous studies on visual differentiation ability and knowledge to assess whether nurses can accurately assess PI according to the PI classification method [
28,
29,
30].
Therefore, it is necessary to investigate nurses' visual differentiation ability of PI and to identify the factors that influence nurses' visual differentiation ability of PI, such as knowledge and general characteristics of PI. Therefore, this study aimed to determine the knowledge and visual differentiation ability of clinical nurses regarding the six-stage PI classification system and IAD needing to be differentiated from PI, and to identify the factors that affect them, so that it can be utilized as a basis for developing educational programs that can help efficient PI nursing practice in the future.
2. Research Methods
2.1. Research Design
This is a descriptive study to determine the knowledge and visual differentiation ability of nurses in a hospital utilizing the PI classification system with IAD and to identify factors affecting their visual differentiation ability.
2.2. Participants
The subjects of this study were 262 nurses at Chungbuk National University Hospital who agreed to participate and answer the questionnaire, with 248 finally analyzed after excluding 8 nurses who met the exclusion criteria and 6 whose questionnaires were not completed.
The minimum sample size for this study was calculated as 245 utilizing the G*Power 3.1.9.7 program (Düsseldorf University, Dusseldorf, Germany), a sample number calculation program, through regression analysis with a significance level of 0.05, a power of 0.95, a medium effect size of 0.10, and 9 predictors.
2.3. Ethical Considerations
This study was conducted after review by the Institutional Review Board of Chungbuk National University Hospital (IRB No. 2023-05-028-001). The purpose and contents of the study were explained to the subjects, including voluntary participation, that the responses would not be utilized for any purpose other than the purpose of the study. Confidentiality of personal information was guaranteed, and that the subjects could withdraw at any time if they wished. After confirming their willingness to participate in the study and obtaining their written consent, the study was conducted.
2.4. Measurement
2.4.1. General Characteristics
The general characteristics of the subjects included demographic characteristics and PI nursing-related characteristics. Demographic characteristics included age, education, position, career length and unit. PI nursing-related characteristics included frequency of caring patient with PI or IAD experience, management of PI nursing care (PI risk assessment, wound assessment, dressing and debridement) and participation of wound care education.
2.4.2. PI Classification System and IAD Knowledge Test (PICS & IAD KT)
PI knowledge was measured with a 19-item instrument developed by Lee et al. [
6] based on Kim's [
31] instrument for PI knowledge and the literature on the PI classification system and IAD. It consists of statements about the knowledge required to differentiate between PI assessment and IAD, including the pathogenesis, contributing factors, and wound characteristics of the PI classification system and IAD, which were reconstructed in six steps, with 1 point for correct answers and 0 points for incorrect answers. Scores range from 0–19, with higher scores indicating greater knowledge. The reliability at the time of development was Kuder-Richardson Formula 20 (K-R 20)=.76, and the validity was Content Validity Index (CVI)=.80. The reliability in this study was K-R 20=.67.
2.4.3. Visual Differentiation Ability Test of the PI Classification System and IAD (VDAT-PICS & IAD)
This is a tool developed by Lee et al. [
6] to differentiate between the PI classification system and IAD and includes 21 photographs with information on the patient's clinical condition, including medical diagnosis, patient mobility, bowel movement, presence or absence of percutaneous fluid infusion, and wound holding period. The 21 photographs consist of 16 pictures of each of the 6 stages of PI, 2 pictures of Blanching erythema, and 3 pictures of IAD, with 1 point for a correct answer and 0 points for an incorrect answer, and the score ranges from 0–21 points, with higher scores indicating higher visual differentiation ability. The reliability at the time of development was Multi-rater kappa=.81 (p<.001), and the validity was CVI=.83. In this study, the reliability was K-R 20=.82.
2.5. Data Collection Method
Data collection for this study was conducted on June 22, 2023 and August 29, 2023. This study measured PICS & IAD knowledge and visual differentiation ability utilizing questionnaires and photographs testing the subjects. The questionnaire was completed directly by the subjects, and the PICS & IAD visual differentiation ability was measured via their assessments of the photographs and information provided in the printout utilized to complete the questionnaire. The time required to complete the questionnaire was approximately 15 minutes.
2.6. Data Analysis
Data were analyzed utilizing the SPSS WIN 27.0 program (IBM Corp, Armonk, NY, USA).
The general characteristics of the subjects and the PICS & IAD knowledge test and visual differentiation ability test were analyzed utilizing frequencies, percentages, means, and standard deviations.
Differences in PICS & IAD knowledge test and visual differentiation ability test scores according to the general characteristics of the subjects were tested by independent t-test and one-way ANOVA, and post hoc tests were analyzed via the Scheffé test.
Multiple regression analysis was conducted to identify factors affecting visual differentiation ability.
3. Results
3.1. General Characteristics
The subjects’ general characteristics are shown in
Table 1. The mean age was 30.56±8.03 years. About 84% of subjects graduated with bachelor’s degree or higher, 89.1% were staff nurses. Clinical experience was <5 years (50.0%), 5–9 years (26.6%), and ≥10 years (23.4%), with nurses with less than 5 years of experience being the most common, and departments were internal medicine wards (32.3%), surgical wards (25.4%), intensive care units (21.8%), other (12.1%), and emergency departments (8.5%). The frequency of caring for patients with PI or IAD was frequently (36.3%), usually (32.7%), sometimes (21.0%), and never (10.1%). Regarding experience in caring for patients with PI, 81.5% had experience in performing PI risk assessment (Braden scale), followed by general wound assessment (68.5%), dressings (65.7%), and debridement (14.5%). A majority (62.5%) of subjects had received wound care education at least once.
3.2. Descriptive Statistics of PICS & IAD Knowledge Test and Visual Differentiation ability Test
As a result of measuring PICS & IAD knowledge test, the score was 12.65±2.90 out of 19 points, with a correct answer rate of 66.5%. When looking at the percentage of correct answers by item, " Moisture associated skin damage such as urinary and fecal incontinence is related to the development of pressure injuries." was the highest at 96.8%, and " A stage Ⅲ pressure injury involves the fat tissue and fascia." was the lowest at 10.9%. " There is no necrotic tissue on wound bed in patients with incontinence-associated dermatitis." was also the least correct at 27.0% (
Table 2).
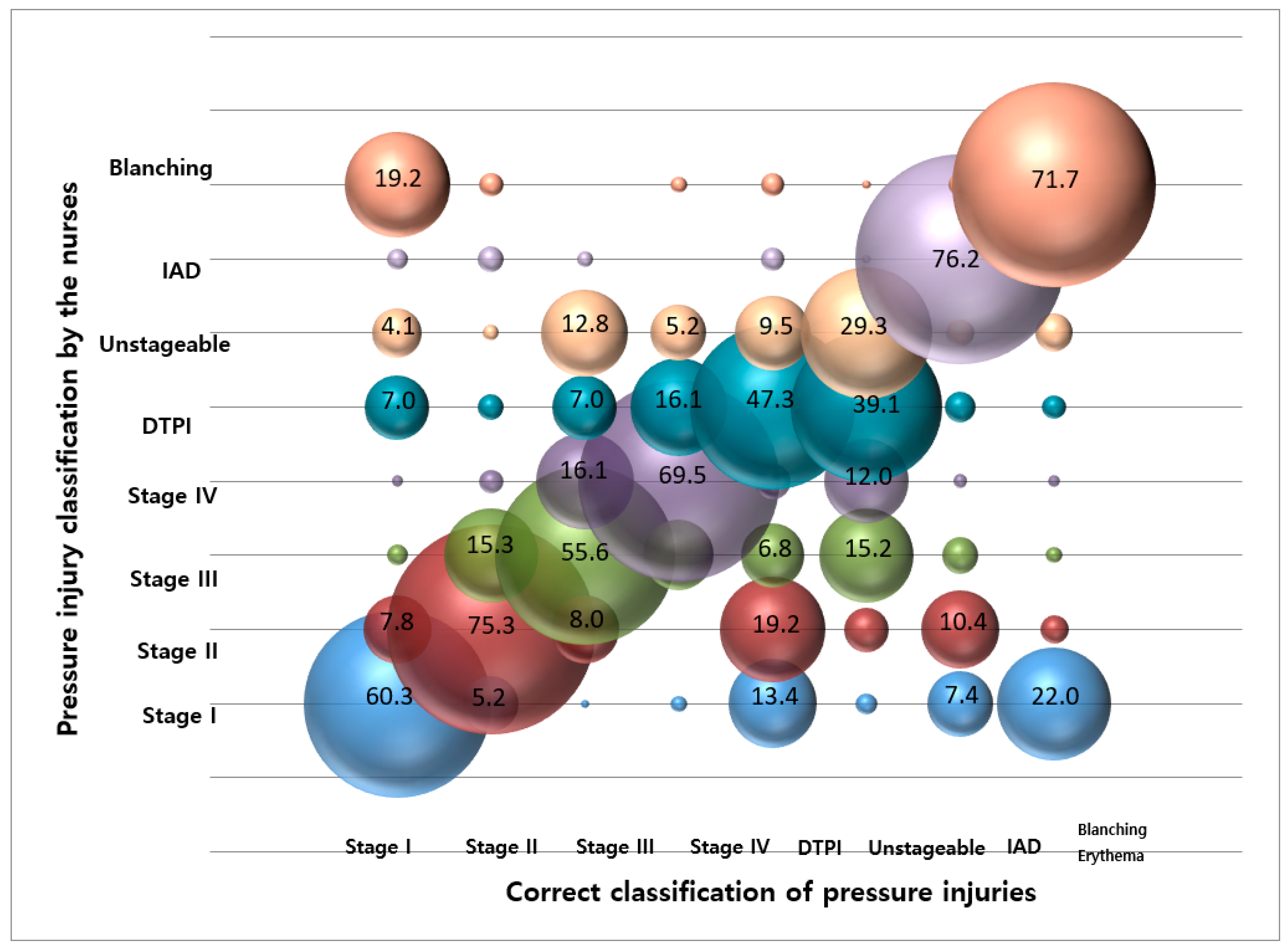
When PI & IAD visual differentiation ability was measured by presenting photographs containing PI-related clinical information, the mean score was 11.43±4.57 out of 21, with a correct response rate of 54.4%. The lowest response rate was 29.3% for unstageable PI photographs, followed by deep tissue pressure injury (DTPI) (47.3%) and stage Ⅲ (55.6%). IAD, conversely, had the highest percentage of correct answers at 76.2% (
Figure 1). When looking at nurses' visual differentiation ability test errors, DTPI was most often confused with unstageable PI, followed by stage Ⅳ. Unstageable PI was the most difficult to distinguish from stage Ⅲ, followed by DTPI and stage Ⅳ. Stage Ⅲ was found to be confused with stage Ⅱ and unstageable PI, in that order (
Figure 1).
3.3. Differences between PICS & IAD Knowledge and Visual Differentiation Ability According to General Characteristics
The difference between PICS & IAD knowledge and visual differentiation ability according to the general characteristics of the subjects is shown in
Table 1. Comparing the PICS & IAD visual differentiation ability according to the general characteristics of the subjects, the results showed that frequency of caring patient with PI or IAD (F=3.15, p=.026), experience in nursing patients with PI was significantly higher in wound assessment (t=-2.71, p=.007), dressing (t=2. 62, p=.009), and debridement (t=2.54, p=.012). Hence, the more frequently PI care is performed and the higher the level of PI nursing performance, a more statistically significant higher visual differentiation ability test resulted.
3.4. Factors Affecting PICS & IAD Knowledge and Visual Differentiation Ability
There was a significant positive correlation (r=.252, p<.001) between PICS & IAD knowledge test and visual differentiation ability test (
Table 3). To identify factors affecting PICS & IAD visual differentiation ability, a regression model was built with significant PI management-related characteristics and PICS & IAD knowledge. Frequency of caring patient with PI or IAD and experience in PI management such as assessing wound, dressing, and debridement were entered as dummy variables, and PICS & IAD knowledge test were entered as continuous variables to build a regression model for PICS & IAD visual differentiation ability. The input variable selection method was utilized to build the model. The regression model of PICS & IAD visual differentiation ability was significant (F=5.46,
p<.001), and among the PICS & IAD knowledge, experience in debridement, and frequency of PI and IAD management were significant factors. The explanatory power of the regression model constructed with these three variables for PICS & IAD visual differentiation ability was 13.7% (
Table 4).
4. Discussion
The correct answer rate of the PICS & IAD knowledge test for the subjects was 66.5%, which is difficult to compare directly due to the different subjects and tools, but it is somewhat lower than previous studies [
23,
27] in which the nurses' PI nursing knowledge level was over 76%–80%. Looking at individual items, out of 19 items, "A stage Ⅲ pressure injury involves the fat tissue and fascia. (10.9%)", "There is no necrotic tissue on wound bed in patients with incontinence-associated dermatitis. (27.0%)", "It is not a pressure injury if there are skin injuries with blanching erythema. (40.7%),” Stage Ⅱ pressure injuries are intact skin with vesicles on pressure. (42.7%)", etc., were answered incorrectly. Therefore, it is necessary to emphasize the correct definition of stage Ⅱ and Ⅲ, the distinction from stage Ⅳ, which includes fascia damage, and the management of stable eschar.
To investigate the PICS & IAD visual differentiation ability, we evaluated the ability to classify PI and IAD utilizing photographs with clinical information, and the correct answer rate was 54.4%. In detail, unstageable PI (29.3%), DTPI (47.3%), and stage Ⅲ (55.6%) had lower answer rates, while the visual differential ability of Blanching erythema, IAD, and stage Ⅱ was over 70%. These results suggest that the nurses in the study need accurate education in unstageable PI, DTPI, and Stage III, given the low percentage of correct answers for stage Ⅲ in the knowledge questionnaire.
Looking at the incorrect answers of the items with low visual differentiation ability, DTPI was mainly confused with unstageable PI, stage Ⅳ, and unstageable PI was difficult to distinguish from stage Ⅲ and DTPI. In the case of DTPI, nurses may be confused because there are reports that despite removing pressure and applying appropriate dressings in the clinical setting, there are cases of unstageable PI covered with necrotic tissue, and then the necrotic tissue is removed to expose the wound base, which is later found to be stage Ⅲ and Ⅳ [
23]. It is also believed that this may have caused nurse confusion because it is not uncommon to see multiple PI stages such as non-blanching erythema or blanching erythema, stage Ⅱ, and unstageable PI on DTPI. Therefore, future PI and IAD-related nurse continuing education programs should include precise definitions of unstageable PI and DTPI, and clinical guidelines or changes in DTPI over time, and further clinical studies on changes in DTPI are needed.
Regarding unstageable PI, due to the difficulty in distinguishing the black desiccated necrotic tissue covering the wound base in a planar view [
23], it is likely that it was confused with DTPI, and the black desiccated tissue that had changed to yellow edible tissue on the screen was mistakenly identified as stage Ⅲ. Similarly, stage Ⅲ was incorrectly classified as unstageable PI because the adipose tissue at the base of the wound was confused with granulation tissue. Considering these results, it is necessary to provide practice-based education through simulation training or clinical practice utilizing videos on the characteristics of necrotic tissue and normal skin anatomy such as adipose tissue at different stages of skin damage. In addition, it is necessary to distinguish between blanching erythema and stage Ⅰ, which is an important part of initial PI assessment and an important predictor of PI prevention, but in this study, there were difficulties in distinguishing between blanching erythema and stage Ⅰ. These results are similar to previous studies [
18,
30].
The factors that significantly affect PICS & IAD visual differentiation ability are knowledge, experience in debridement in PI patients, and frequency of PI and IAD management, and it was suggested that the higher the level of knowledge, more experience of a high level of PI nursing practice (debridement), and the higher the frequency, the significantly higher the visual differentiation ability. In a previous study, visual differentiation ability was statistically significantly different depending on the medical staff's experience in caring for patients with wounds, skin care, and PI prevention and treatment, and the higher the frequency of managing patients with PI or IAD, the higher scores the PICS & IAD knowledge test and visual differentiation ability test [
27], showing similar results to this study. This may have been influenced by the fact that clinical nurses have more opportunities to be exposed to work environments such as the management, prevention, and treatment of wounds and skin such as surgical sites and injection sites, even if they are not pressure ulcers, and have increased their work proficiency through this.
PI nursing knowledge is positively correlated with PI nursing attitudes, and PI nursing attitudes are positively correlated with PI nursing performance [
25,
32], while other studies have shown no correlation between PI nursing performance and PI nursing knowledge [
33]. The results of these studies suggest many complex factors regarding the relationship between PI nursing knowledge and PI nursing practice. In general, it has been reported that even when knowledge is present, it is only likely to lead to practice when there is a high degree of certainty that the perceived knowledge is correct. Therefore, since PI nursing knowledge is acquired through relevant education, and PI nursing is performed based on PI nursing knowledge, a standardized PI nursing education system is needed so that PI nursing knowledge in clinical practice can be transferred to PI nursing performance [
34]. In particular, PI classification system education program should be provided to nurses to distinguish between IAD and PI, which are similar to PI and require differential diagnosis, and to increase visual differentiation ability for PI, and changes in theoretical knowledge and visual differentiation ability should be studied after education. Based on the results of this study, it is necessary to develop a PI education program that improves visual differentiation ability by increasing PICS & IAD knowledge to help nurses accurately assess PI and perform appropriate nursing care. In developing a PI education program, it is recommended that the contents of stage Ⅱ, stage Ⅲ, and IAD (which are items that clinical nurses had low knowledge of as shown in the results of this study), and DTPI, unstageable PI, and stage Ⅲ (which have difficulty in visual differentiation ability) should be strengthened and supplemented compared to existing PI programs.
The limitations of this study include the fact that it was conducted among clinical nurses in a single hospital and that the PICS & IAD knowledge test tool utilized in the study was modified and supplemented from an existing tool, and it needs to be validated through future repeated studies.
5. Conclusions
Accurate assessment and differentiation of PI from other skin lesions is crucial for the prevention and management of PI. In this study, the overall state of theoretical knowledge about PI and its risk factors was good, but the visual differentiation ability test for unstageable PI and DTPI was low, and confusion between stage Ⅰ and blanching erythema and DTPI and unstageable PI was found. The visual differentiation ability was significantly influenced by knowledge of PICS&IAD, experience in debridement in PI patients, and frequency of caring for PI-related patients. Therefore, greater PI nursing education experience is needed to promote nurses' accurate PICS & IAD visual differentiation ability and improve the quality of nursing care to perform effective PI management, and it is believed that nurses' knowledge can be improved through repeated education that progresses from basic to advanced stages rather than one-time education on PICS&IAD. To this end, the current PI-related nurse continuing education should be further refined by subdividing it into introductory courses for nurses who manage PI and IAD patients infrequently, advanced courses for those who manage them frequently or have attended many related trainings, and in-depth courses for wound nurses, and adjusting the level of difficulty to match the knowledge level of the participants. In addition, we recommend a follow-up study to evaluate the effectiveness of continuous education by utilizing the PICS & IAD visual differentiation ability utilized in this study as a tool to measure the effectiveness of PI and IAD-related education for nurses, measuring it before education and after a certain period after education.
Author Contributions
Conceptualization, S.P, E.J.K and J.E.H.; methodology, S.P.; formal analysis, J.E.H.; investigation, S.P, E.J.K, S.J.L, E.J.K, J.Y.L and J.E.H.; resources, S.P.; data curation, S.P, J.E.H.; writing—original draft preparation, S.P, J.E.H.; writing—review and editing, S.P, E.J.K, S.J.L, E.J.K, J.Y.L and J.E.H.; visualization, J.E.H.; supervision, S.P.; project administration, S.P.; funding acquisition, S.P, J.E.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Chungbuk National University Korea National University Development Project (2023).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Chungbuk National University Hospital (IRB No. 2023-05-028-001).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- National Pressure Injury Advisory Panel (NPIAP) announces a change in terminology from pressure ulcer to pressure injury and updates the stages of pressure injury. Available online: npuap-position-statement-on-.pdf (ymaws.com).
- Health care big data hub. Domestic pressure injury statistics [Internet]. Wonju: Health Care Big Data Hub; From 2017 to 2021. Available online: https://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsInfoTab1.do.
- Lahmann, N.A.; Kottner, J.; Dassen, T.; Tannen, A. Higher pressure ulcer risk on intensive care? Comparison between general wards and intensive care units. J Clin Nurs 2012, 21, 354–361. [Google Scholar] [CrossRef]
- Martel, T.; Orgill, D.P. Cutting edge care Delivery in response to the Covid-19 pandemic: Medical device–related pressure injuries during the COVID-19 pandemic. J Wound Ostomy Continence Nurs 2020, 47, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K. The relationship of risk assessment using Braden scale and development of pressure sore in neurologic intensive care unit. J Korean Acad Adult Nurs 2003, 267–277. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, J.Y.; Lee, T.W. Inter-rater reliability of the pressure ulcer classification system. Korean Wound Manag Soc 2011, 7, 75–80. [Google Scholar] [CrossRef]
- Moon, M. The characteristics related to the development of pressure ulcers in long term care facilities: The use of 2009 National Patient Sample. J Korea Acad-Ind Coop Soc 2013, 14, 3390–3399. [Google Scholar] [CrossRef]
- Song, K.Y.; Jung, S.K.; Yang, J.H.; Choi, D.W.; Kim, Y.H.; Kim, S.S.; et al. Fundamentals of Nursing. Seoul: Soomoonsa, 2021.
- García-Fernández, F.P.; Pancorbo-Hidalgo, P.L.; Agreda, J.J.S. Predictive capacity of risk assessment scales and clinical judgment for pressure ulcers: A meta-analysis. J Wound Ostomy Continence Nurs 2014, 41, 24–34. [Google Scholar] [CrossRef]
- Labeau, S.O.; Afonso, E.; Benbenishty, J.; Blackwood, B.; Boulanger, C.; Brett, S.J.; Calvino-Gunther, S.; Chaboyer, W.; Coyer, F.; Deschepper, M.; et al. Correction to: Prevalence, associated factors, and outcomes of pressure injuries in adult intensive care unit patients: The DecubICUs study. Intensive Care Med. 2021, 47, 503–520. [Google Scholar] [CrossRef]
- Kim, J.Y.; Park, K.H.; Park, O.K.; Park, J.H.; Lee, Y.J.; Hwang, J.H. Updates of evidence-based nursing practice guidelines for pressure injury. J. Korean Clin. Nurs. Res. 2023, 29, 12–23. [Google Scholar] [CrossRef]
- Aydin, A.K.; Karadağ, A. Assessment of nurses’ knowledge and practice in prevention and management of deep tissue injury and stage I pressure ulcer. J. Wound Ostomy Continence Nurs. 2010, 37, 487–494. [Google Scholar] [CrossRef]
- Bennett, G.; Dealey, C.; Posnett, J. The cost of pressure ulcers in the UK. Age Ageing 2004, 33, 230–235. [Google Scholar] [CrossRef]
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/ Injuries: Clinical Practice Guideline, 3rd ed.; Haesler, E., Ed.; Cambridge Media: Cambridge, UK, 2019; Available online: internationalguideline.com.
- Smart, H.; Sibbald, R. Skin care for the protection and treatment of incontinence associated dermatitis (IAD) to minimize susceptibility for pressure injury (PI) development. World Counc. Enterostomal Therapists J. 2020, 40, 40–44. [Google Scholar] [CrossRef]
- Proceedings of the Global IAD Expert Panel.. Incontinence associated dermatitis: Moving prevention forward. Available online: https://www.woundsinternational.com, 2015.
- Beeckman, D.; Schoonhoven, L.; Boucqué, H.; Van Maele, G.; Defloor, T. Pressure ulcers: E-learning to improve classification by nurses and nursing students. J. Clin. Nurs. 2008, 17, 1697–1707. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Ryu, J.M. Canonical correlation between knowledge-barriers/facilitators for pressure ulcer prevention nursing variables and attitude-performance variables. J. Health Info. Stat. 2019, 44, 227–236. [Google Scholar] [CrossRef]
- Launiala, A. How much can a KAP survey tell us about people’s knowledge, attitudes and practices? Some observations from medical anthropology research on malaria in pregnancy in Malawi. Anthropol. Matters 2009, 11. [Google Scholar] [CrossRef]
- Jo, E.H.; Kim, H.S.; Lee, S.J. A study on the knowledge of nurses, performance, and preventive practice of pressure ulcer among nurses in long-term care hospital. J. Korea Contents Assoc. 2015, 15, 356–365. [Google Scholar] [CrossRef]
- Kang, M.J.; Kim, M.S. Correlations among attitude toward pressure ulcer prevention, knowledge and non-compliance risk for pressure ulcer prevention practice and degree of nursing performance. J. Korea Acad.-Ind. Coop. Soc. 2018, 19, 408–419. [Google Scholar] [CrossRef]
- Lee, E.J.; Yang, S.O. Clinical knowledge and actual performance of pressure ulcer care by hospital nurses. J. Korean Clin. Nurs. Res. 2011, 17, 251–261. [Google Scholar] [CrossRef]
- Kang, Y.R.; Jo, M.J. The effects of a pressure ulcer Education Program on the nursing knowledge, preventive attitude and nursing performance of pressure ulcer of nurses in comprehensive nursing care service units. J. Korea Acad.-Ind. Coop. Soc. 2022, 23, 256–264. [Google Scholar] [CrossRef]
- Kim, S.O.; Kim, S.M. The effects of pressure injury nursing knowledge and pressure injury nursing attitude on pressure injury nursing practices of nurses in geriatric hospitals. J. Korean Biol. Nurs. Sci. 2022, 24, 190–199. [Google Scholar] [CrossRef]
- Jin, Y.S. Knowledge, Performance, and Awareness of Importance on Pressure Ulcer Care Among Nurses at a General Hospital. Unpublished Master’s Thesis; Yonsei University: Seoul, 2009. [Google Scholar]
- Lee, Y.J.; Park, S.; Kim, J.Y.; Kim, C.G.; Cha, S.K. Clinical nurses’ knowledge and visual differentiation ability in pressure ulcer classification system and incontinence-associated dermatitis (in Korean). J. Korean Acad. Nurs. 2013, 43, 526–535. [Google Scholar] [CrossRef]
- Fergus, P.; Chalmers, C.; Henderson, W.; Roberts, D.; Waraich, A. Pressure ulcer categorization and reporting in domiciliary settings using deep learning and mobile devices: A clinical trial to evaluate end-to-end performance. IEEE Access 2023, 11, 65138–65152. [Google Scholar] [CrossRef]
- Tschannen, D.; Mckay, M.; Steven, M. Improving pressure ulcer staging accuracy through a nursing student experiential intervention. J. Nurs. Educ. 2016, 55, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Henry, M. Nursing education program for hospital-acquired pressure injury prevention in adult acute care setting: A quality improvement project. J. Wound Ostomy Continence Nurs. 2019, 46, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Defloor, T.; Schoonhoven, L.; Katrien, V.; Weststrate, J.; Myny, D. Reliability of the European Pressure Ulcer Advisory Panel classification system. J. Adv. Nurs. 2006, 54, 189–198. [Google Scholar] [CrossRef]
- KIM, H. Y. The knowledge of pressure ulcer and the nursing intervention of nurse in hospital. Unpublished master's thesis, Dong-A University, Busan, 2003.
- KANG, Min Kyeong; KIM, Myoung Soo. Effects of Attitude, Barriers/Facilitators, and Visual Differentiation on Oral Mucosa Pressure Ulcer Prevention Performance Intention. In: Healthcare. MDPI, 2021. p. 76.
- Yang, N.Y.; Moon, S.Y. Perceived importance, educational needs, knowledge and performance concerning pressure ulcer care by clinical nurses. J. Korean Acad. Adult Nurs. 2009, 95–104. [Google Scholar]
- Lee, S.J.; Park, O.K.; Park, M.Y. A structural equation model of pressure ulcer prevention action in clinical nurses. J. Korean Acad. Nurs. 2016, 46, 572–582. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).