1. Introduction
Podocalyxin (PODXL) is a CD34-related transmembrane sialomucin glycoprotein [
1]. The 53-kDa PODXL core protein undergoes extensive
N- and
O-linked glycosylation leading to a mature protein with a molecular weight of 150,000–200,000 [
2]. PODXL is normally expressed by embryonic stem cells [
3], early hematopoietic progenitors [
4], adult vascular/lymphatic endothelial cells [
5], and kidney podocytes [
6]. PODXL plays a critical role in the development, and PODXL-knockout (KO) mice display lethality before birth [
7]. Importantly, PODXL is aberrantly expressed in a broad range of human tumors including oral squamous cell carcinoma [
8], brain tumors [
9], colorectal cancer [
10], renal cell carcinoma [
11], and pancreatic ductal adenocarcinoma (PDAC) [
12]. The increased PODXL expression could have adverse effects on overall survival, disease-specific survival, and disease-free survival in several cancers [
13].
PODXL regulates epithelial and tumor cell motility through interaction with the actin polymerization complexes including ERM (ezrin–radixin–moesin) family [
14] and the PDZ protein Na
+/H
+ exchanger regulatory factor 1 and 2 (NHERF-1/2) [
15]. Ezrin and NHERF-1/2 are adaptor proteins that have diverse binding partners and facilitate the interaction of PODXL with the cytoskeleton in tumor cells [
13]. The interactions between PODXL, ezrin, and NHERF-1/2 have been reported to activate intracellular signaling including Rac1, RhoA, Cdc42, mitogen-activated protein kinase, and phosphatidylinositol-3 kinase pathways to promote the motility [
13]. The PODXL gain- or loss-of-function studies have been revealed to play an essential role in tumor progression by promoting the migration, invasiveness, stemness, and metastasis in a variety of cancer cells [
16]. Therefore, PODXL has acquired increasing attention as a target of tumor immunotherapy.
Pre-clinical studies have shown the promising efficacy of anti-PODXL monoclonal antibodies (mAbs). A core protein binding anti-PODXL mAb (PODO83/PODOC1) suppressed MDA-MB-231 xenograft growth and blocked the metastasis to the lung [
17]
. Our group also established an anti-PODXL mAb, PcMab-47
(mouse IgG1, kappa) which is useful for flow cytometry and immunohistochemistry [
18]. We
engineered PcMab-47 into 47-mG2a, a mouse IgG2a-type mAb, to add antibody-dependent cellular cytotoxicity
(ADCC), further developed 47-mG2a-f, a core fucose-deficient type of 47-mG2a to augment its ADCC. Both 47-mG2a and 47-mG2a-f showed antitumor activity against PODXL-expressing oral squamous cell carcinoma-bearing mouse models [
19]
. Furthermore, we developed
a mouse-human chimeric PcMab-47, chPcMab-47, and showed antitumor efficacy against PODXL-positive colorectal adenocarcinomas [
20]
.
Nevertheless, further development of anti-PODXL mAbs targeting tumors has been hampered by concerns about the possible toxicities to normal vascular/lymphatic endothelial cells [
5] and kidney podocytes [
6]. For the development of antibody therapy against PODXL-positive cancers, cancer-specificity is necessary to reduce the risk of adverse effects on normal tissues. In this study, we developed a cancer-specific anti-PODXL mAb, PcMab-6 (IgG
1, kappa) by screening of more than one hundred hybridoma clones. We engineered PcMab-6 into a mouse IgG
2a type (PcMab-6-mG
2a) and a humanized IgG
1-type (humPcMab-6), and further produced the core fucose-deficient types (PcMab-6-mG
2a-f and humPcMab-6-f, respectively) to potentiate the ADCC. This technique is clinically applied to mogamulizumab (Poteligeo), a defucosylated antibody targeting CCR4 [
21]. We then examined the antitumor activity against mouse xenograft models of PDAC.
2. Materials and Methods
2.1. Cell Lines
A mouse myeloma cell line P3X63Ag8U.1 (P3U1), a human glioblastoma cell line (LN229), and a PDAC cell line (Capan-2) were obtained from the American Type Culture Collection (Manassas, VA). Two PDAC cell lines (MIA PaCa-2 and PK-45H) were obtained from the Cell Resource Center for the Biomedical Research Institute of Development, Aging and Cancer Tohoku University (Miyagi, Japan). The LN229/PODXL ectodomain (LN229/PODXLec) was produced in our previous study [
18]. PODXL-KO LN229 (PDIS-13) was generated as described previously [
20]. LN229, PDIS-13, LN229/PODXLec, and MIA PaCa-2 were cultured in Dulbecco’s modified Eagle’s medium (DMEM) medium (Nacalai Tesque, Inc., Kyoto, Japan). Capan-2 was cultured in McCoy’s 5A medium (Cytiva, Tokyo, Japan). P3U1 and PK-45H were cultured in Roswell Park Memorial Institute (RPMI)-1640 medium (Nacalai Tesque, Inc.). All media were supplemented with 10% heat-inactivated fetal bovine serum (FBS; Thermo Fisher Scientific Inc., Waltham, MA), 100 units/ml of penicillin, 100 μg/mL of streptomycin, and 0.25 μg/mL of amphotericin B (Nacalai Tesque, Inc.). A lymphatic endothelial cell line (HDMVEC/TERT164-B) was purchased from EVERCYTE (Vienna, Austria), and was cultured in an Endopan MV kit (PAN Biotech, Germany) supplemented with G418. All cells were cultured at 37◦C in a humidified atmosphere containing 5% CO
2 and 95% air.
2.2. Animals
For the establishment of mAbs against PODXL, the animal experiment was approved by the Animal Care and Use Committee of Tohoku University (permit number: 2019NiA-001). For ADCC assay and antitumor activity in mouse xenograft models, the animal experiments were approved by the Institutional Committee for Experiments of the Institute of Microbial Chemistry. The loss of original body weight to a point >25% and/or a maximum tumor size >3000 mm3 were identified as humane endpoints for euthanasia.
2.3. Hybridoma Production
Female BALB/c mice (CLEA, Tokyo, Japan) were immunized with the purified PODXLec (100 μg) [
18] together with Imject Alum (Thermo Fisher Scientific Inc.) by intraperitoneal injection. After several additional immunizations of PODXLec, the spleen cells were harvested and fused with P3U1 cells using PEG1500 (Roche Diagnostics, Indianapolis, IN). Hybridomas were grown in RPMI-1640 medium, including L-glutamine with hypoxanthine, aminopterin, and thymidine (HAT) selection medium supplement (Thermo Fisher Scientific Inc.). Culture supernatants were screened using enzyme-linked immunosorbent assay (ELISA) for binding to PODXLec.
2.4. ELISA
PODXLec was immobilized on Nunc Maxisorp 96-well immunoplates (Thermo Fisher Scientific, Inc.) at 1 μg/mL for 30 min. After blocking with 1% bovine serum albumin (BSA) in 0.05% Tween 20/phosphate-buffered saline (PBS, Nacalai Tesque, Inc.), the plates were incubated with culture supernatant followed by 1:2000 diluted peroxidase-conjugated anti-mouse immunoglobulins (Agilent Technologies, Inc., Santa Clara, CA). The enzymatic reaction was produced with a 1-Step Ultra TMB-ELISA (Thermo Fisher Scientific, Inc.). The optical density was measured at 655 nm using an iMark microplate reader (Bio-Rad Laboratories, Inc., Berkeley, CA).
2.5. Antibodies
A mouse anti-PODXL mAb, PcMab-47 (IgG
1, kappa), was developed as described previously [
18]. Normal mouse IgG (mIgG) was purchased from FUJIFILM Wako Pure Chemical Corporation (Osaka, Japan). Mouse IgG
2a (mIgG
2a) and normal human IgG (hIgG) were purchased from Sigma-Aldrich Corp. (St. Louis, MO). To generate PcMab-6-mG
2a, the V
H cDNA of PcMab-6 and C
H of mouse IgG
2a were subcloned into pCAG-Ble vector (FUJIFILM Wako Pure Chemical Corporation), and V
L and C
L cDNAs of PcMab-6 were subcloned into pCAG-Neo vector (FUJIFILM Wako Pure Chemical Corporation). To generate a humanized PcMab-6 (humPcMab-6), the complementarity determining region (CDR) of PcMab-6 V
H, frame sequences of V
H in human Ig, and C
H of human IgG
1 were cloned into the pCAG-Neo vector. The CDR of PcMab-6 V
L, frame sequences of V
L in human Ig, and C
L of human kappa chain were cloned into the pCAG-Ble vector. To generate PcMab-6-mG
2a-f and humPcMab-6-f, antibody expression vectors were also transfected into BINDS-09 (Fut8-knocked out ExpiCHO-S cells) [
22] using the ExpiCHO Expression System. PcMab-6, PcMab-6-mG
2a-f, and humPcMab-6-f were purified using Protein G-Sepharose (GE Healthcare Bio-Sciences, Pittsburgh, PA).
2.6. Flow Cytometry
Cell lines were harvested via a brief exposure to 0.25% trypsin/1 mM ethylenediaminetetraacetic acid (EDTA; Nacalai Tesque, Inc.). After washing with 0.1% BSA in PBS, the cells were treated with primary mAbs for 30 min at 4◦C, followed by treatment with Alexa Fluor 488-conjugated anti-mouse IgG (1:1000; Cell Signaling Technology, Danvers, MA) or fluorescein isothiocyanate (FITC)-conjugated anti-human IgG (1:2000; Sigma-Aldrich Corp.). Fluorescence data were collected using an SA3800 Cell Analyzer (Sony Corp., Tokyo, Japan).
2.7. ADCC
The ADCC activity of PcMab-6-mG2a-f was measured as follows. In brief, effector cells were obtained from the spleen of female BALB/c nude mice (Jackson Laboratory Japan, Inc., Kanagawa, Japan). We labeled target cells (MIA PaCa-2, Capan-2, and PK-45H) using 10 µg/mL Calcein AM (Thermo Fisher Scientific, Inc.), plated in 96-well plates (1 × 104 cells/well), and mixed with the effector cells (effector to target ratio, 100:1) with 100 μg/ml of control mIgG2a or PcMab-6-mG2a-f. After a 4.5-hour incubation at 37°C, the Calcein release into the medium was measured using a microplate reader (Power Scan HT; BioTek Instruments, Inc., Winooski, VT).
The ADCC activity of humPcMab-6-f was measured as follows. The Calcein AM-labeled target cells (MIA PaCa-2, Capan-2, and PK-45H) were mixed with human NK cells (Takara Bio, Inc., Shiga, Japan; effector to target ratio, 50:1) with 100 μg/ml of control hIgG or humPcMab-6-f. The Calcein release to the medium was measured after a 4.5-hour incubation.
The cytolyticity (% lysis) was determined: % lysis is calculated as (E - S)/(M - S) x 100, where “E” denotes the fluorescence in effector and target cell cultures, “S” denotes the spontaneous fluorescence of only target cells, and “M” denotes the maximum fluorescence after treatment with a lysis buffer [10 mM Tris-HCl (pH 7.4), 10 mM EDTA, and 0.5% Triton X-100]. All data are shown as mean ± standard error of the mean (SEM). Welch’s t-test was used for the statistical analyses.
2.8. CDC
The Calcein AM-labeled target cells (MIA PaCa-2, Capan-2, and PK-45H) were plated and mixed with rabbit complement (final dilution 1:10, Low-Tox-M Rabbit Complement; Cedarlane Laboratories, Hornby, ON, Canada) and 100 μg/ml of control mIgG2a, PcMab-6-mG2a-f, control hIgG, or humPcMab-6-f. Following incubation for 4.5 h at 37˚C, the Calcein release into the medium was measured, as described above.
2.9. Antitumor Activity of Anti-PODXL Antibodies
Female BALB/c nude mice were purchased from Jackson Laboratory Japan, Inc. The cells (0.3 mL of 1.33 × 108/mL in DMEM) were mixed with 0.5 mL of BD Matrigel Matrix Growth Factor Reduced (BD Biosciences, San Jose, CA). A 100 μL suspension (containing 5 × 106 cells) was injected subcutaneously into the left flanks of nude mice. The 100 μg of PcMab-6-mG2a-f or control mIgG in 100 μL PBS were injected into the peritoneal cavity of each mouse at day 4 (PK-45H) or day 7 (MIA PaCa-2 and Capan-2). Additional antibodies were injected on days 11 and 13 (PK-45H) or days 14 and 16 (MIA PaCa-2 and Capan-2). The mice were euthanized on day 25 (PK-45H) or day 28 (MIA PaCa-2 and Capan-2) after the cell inoculation.
To measure the antitumor activity of humPcMab-6-f, 100 μg of humPcMab-6-f or control hIgG in 100 μL PBS was injected into the peritoneal cavity of each tumor xenograft-bearing mouse on day 7. Additional antibodies were injected on day 14. Furthermore, human NK cells (8.0 × 105 cells) were injected around the tumors on days 7 and 14. The mice were euthanized on day 21 after the cell inoculation.
The tumor diameter was measured and the tumor volume was calculated using the following formula: volume=W2 × L/2, where W is the short diameter and L is the long diameter. All mice were euthanized by cervical dislocation on twenty-five days after cell inoculation. All data were expressed as the mean ± SEM. Statistical analysis was performed using ANOVA with Sidak’s post hoc test. P< 0.05 was considered statistically significant.
4. Discussion
Pancreatic cancer has become the third leading cause of death in men and women combined in the United States, 2023 [
23]. PDAC is the most common type of pancreatic cancer and exhibits an extremely poor prognosis with a 5-year survival rate of approximately 10% [
24]. The four common oncogenic events including
KRAS, CDKN2A, SMAD4, and
TP53 play critical roles in the development [
25,
26]. In contrast, PDAC is a heterogenous tumor with various histology [
27], heterogenous molecular landscapes [
28], and clinical outcomes. Therefore, the identification of early diagnostic markers and therapeutic targets in each group has been desired. In this study, we provided evidence that PODXL could be a promising target for antibody-based therapy, especially PcMab-6 (
Figure 1) and its derivatives including PcMab-6-mG
2a-f (
Figure 2 and
Figure 3) and humPcMab-6-f (
Figure 4,
Figure 5, and
Figure 6).
High PODXL expression was significantly associated with worse overall survival and was predictive of shorter overall survival in multiple cancers, especially PDAC [
29]. Furthermore, PODXL is upregulated during epithelial-mesenchymal transition [
30] and plays a key role in the extravasation of mesenchymal PDAC cells [
31]. PODXL enhances the extravasation through direct binding to ezrin, a cytoskeletal linker protein, which enables the transition of tumor cells from a non-polarized, rounded cell shape to an invasive extravasation-competent morphology [
31]. These results suggest that PODXL mediates the process of extravasation during tumor metastasis. Although the requirement of PODXL ligands such as E-selectin [
32] on endothelial cells is unknown, it would be interesting whether PcMab-6 affects the PODXL ligand interaction, tumor cell extravasation, and metastasis.
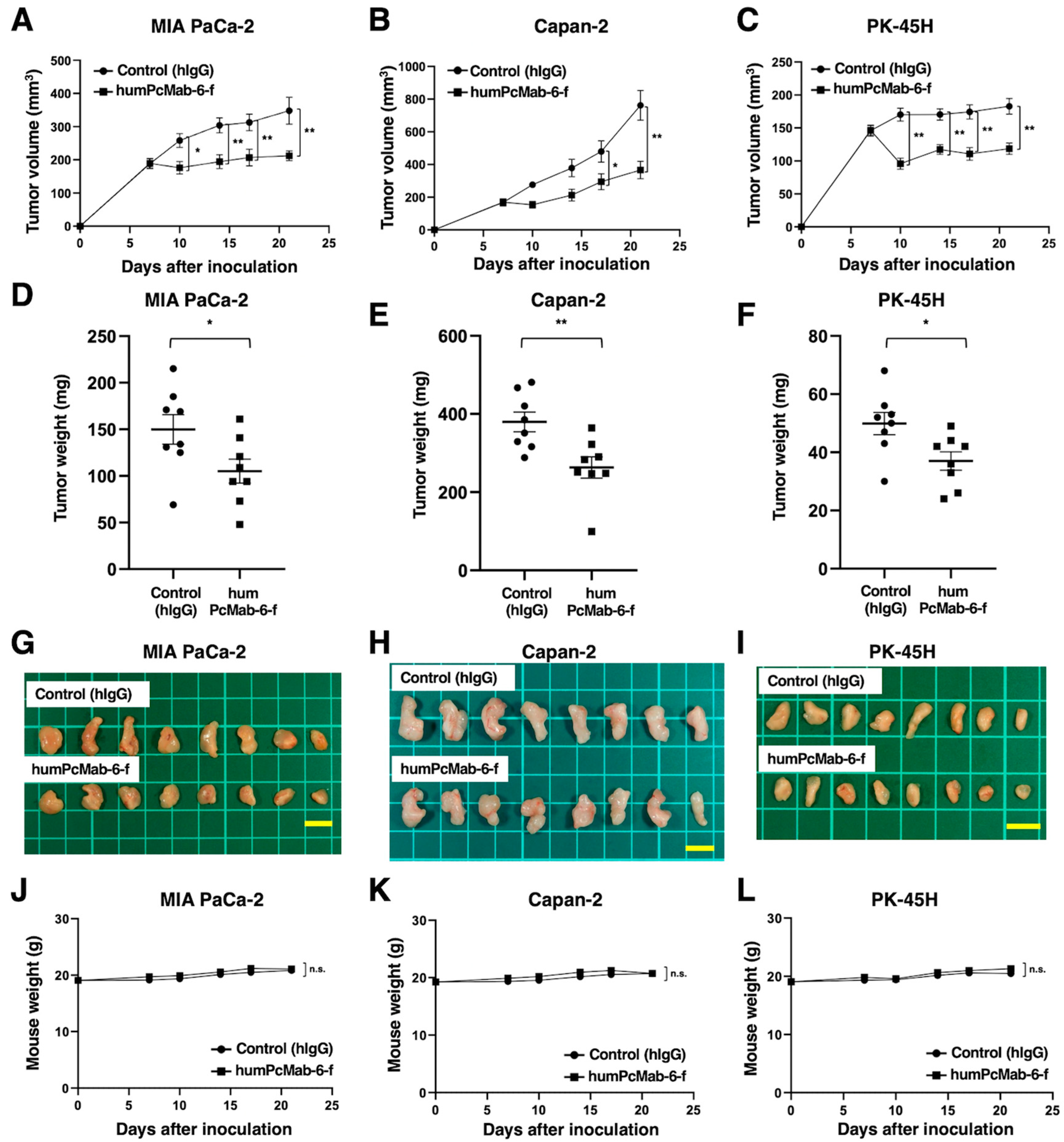
We developed a PODXL-targeting CasMab on cancer cells by the screening of more than one hundred clones of anti-PODXL mAbs. PcMab-6 can recognize PDAC cells, but not normal LECs in flow cytometry (
Figure 1). We previously developed CasMabs against podoplanin (PDPN) [
33]. The CasMabs were selected by flow cytometry and immunohistochemistry, and exhibited reactivity with cancer cells but reduced reactivity with normal cells [
34]. An anti-PDPN CasMab (clone LpMab-2), which has been applied to chimeric antigen receptor (CAR)-T therapy in mice preclinical models [
35], recognizes the glycopeptide from Thr55 to Leu64 of PDPN [
34]. Another CasMab, LpMab-23, recognizes a peptide from Gly54 to Leu64 of PDPN [
36]. We recently developed CasMabs (clone H
2Mab-214 [
37] and clone H
2Mab-250 [
38]) against HER2. These anti-HER2 CasMabs exhibited reactivity with cancer cells but no reactivity with normal cells [
37,
38]. The minimum epitope of H
2Mab-214 and H
2Mab-250 was determined to be the
Lys615/Phe616-including peptide of HER2 and the Trp614
-including peptide of HER2
, respectively [
37,
38]
.
The minimum epitope of one of anti-PODXL non-CasMabs (clone PcMab-47) and another anti-PODXL CasMab (clone
PcMab-60 [
39]
) was determined to be the peptide sequence, including
Asp207, His208, Leu209, and Met210 of PODXL [
40]
and the peptide sequence, including
Arg109, Gly110, Gly111, Gly112, Ser113, Gly114, Asn115, and Pro116 of PODXL[
41]
, respectively. In contrast, PcMab-6 has not been identified yet.
The identification of the PcMab-6 epitope is essential for understanding the mechanism of cancer-specific recognition. Furthermore, the recognition by PcMab-6 in flow cytometry was lower than that of PcMab-47 (
Figure 1), which can be attributed to the possibility that the epitope sequence is partially exposed or modified in cancer cells, but not in normal cells in living cells. The strategy of CasMab selection can contribute to the development of novel mAbs against a variety of antigens.
Glycosylation in tumors is frequently altered [
42]. Anti-PODXL mAbs which recognize tumor-specific glyco-epitopes on PODXL but do not react with PODXL expressed on normal cells, were developed [
43]. One of the mAbs, PODO447, exhibits exquisite specificity for a tumor glycoform of PODXL but lacks reactivity with normal adult human tissue. Using an array of glycosylation defective cell lines, the epitope of PODO447 was revealed as an
O-linked core 1 glycan presented in the context of the PODXL peptide backbone [
43]. Furthermore, PODO447 coupled to monomethyl auristatin E (MMAE) showed efficacy in targeting human pancreatic and ovarian tumor xenografts in mouse models [
44]. In our studies, we investigated whether PODO447 shows cancer-specificity against normal cell lines by flow cytometry, but reacted with both cancer and normal cells (data not shown), indicating that the cancer-specificity of PODO447 might be limited to immunohistochemistry. PcMab-6 reacted with PODXL, which is overexpressed in glycan-deficient cell lines, such as Lec1, Lec2, and Lec8 (data not shown) in the same way with PcMab-47 [
18], suggesting that PcMab-6 might react with the glycan-independent conformational epitope of PODXL.
All therapeutic mAbs exhibit adverse effects probably due to the recognition of antigens expressed in normal cells.
The majority of patients treated with anti-EGFR therapeutic mAbs
experience dermatological disorders, which affect the quality of life and adherence to the therapy [
45]
. The major adverse effect associated with anti-HER2 therapeutic mAbs is cardiotoxicity [
46]. Since PODXL is expressed in normal adult tissues including vascular/lymphatic endothelial cells [
5] and kidney podocytes [
6], the evaluation of
in vivo toxicity of PcMab-6 derivatives is essential. We have investigated the toxicity against cynomolgus monkeys. The first protocol is one intravenous injection of 20 mg/kg mouse-human chimeric antibody of PcMab-6 (chPcMab-6) and observation for one week. The second protocol is four intravenous injections of 10 mg/kg chPcMab-6 (every week) and observation for one month. We confirmed that chPcMab-6 did not show any toxicities against cynomolgus monkeys in both protocols (data not shown).
CARs are synthetic modular proteins that redirect immune cell reactivity toward a target of interest. The platform has shown substantial clinical effects against B cell and plasma cell malignancies, and the potential to expand the application to solid tumors [
47]. The optimal epitope for PODXL-targeting CAR has not yet been evaluated. However, it would be worthwhile to investigate the cancer specificity of the PcMab-6 single-chain variable fragment and the efficacy of CAR-T therapy against PODXL-positive tumors.
Figure 1.
The reactivity of anti-PODXL mAbs (PcMab-6 and PcMab-47) against cancer and normal cells using flow cytometry. (A) LN229 and PODXL-KO LN229 (PDIS-13) cells were treated with 10 µg/ml of PcMab-6, PcMab-47, or buffer control. (B) Pancreatic cancer MIA PaCa-2, Capan-2, and PK-45H cells were treated with 10 µg/ml of PcMab-6, PcMab-47, or buffer control. (C) A lymphatic endothelial HDMVEC/TERT164-B cells were treated with 10 µg/ml of PcMab-6, PcMab-47, or buffer control. Then, cells were treated with Alexa Fluor 488-conjugated anti-mouse IgG. The black line represents the negative control (blocking buffer).
Figure 1.
The reactivity of anti-PODXL mAbs (PcMab-6 and PcMab-47) against cancer and normal cells using flow cytometry. (A) LN229 and PODXL-KO LN229 (PDIS-13) cells were treated with 10 µg/ml of PcMab-6, PcMab-47, or buffer control. (B) Pancreatic cancer MIA PaCa-2, Capan-2, and PK-45H cells were treated with 10 µg/ml of PcMab-6, PcMab-47, or buffer control. (C) A lymphatic endothelial HDMVEC/TERT164-B cells were treated with 10 µg/ml of PcMab-6, PcMab-47, or buffer control. Then, cells were treated with Alexa Fluor 488-conjugated anti-mouse IgG. The black line represents the negative control (blocking buffer).
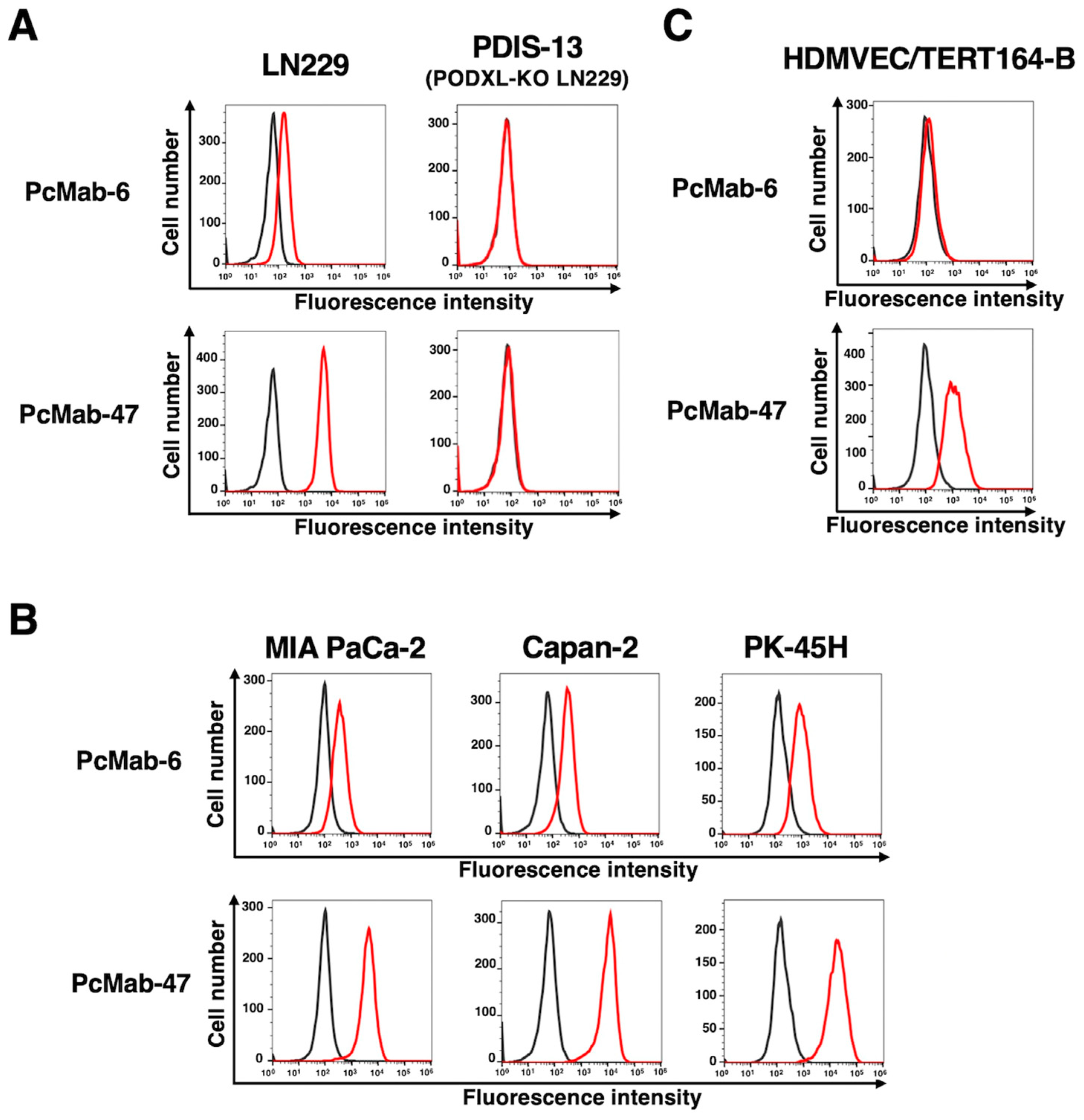
Figure 2.
ADCC and CDC by PcMab-6-mG2a-f. (A) A core-fucose-deficient mouse IgG2a mAb, PcMab-6-mG2a-f was established from PcMab-6 (mouse IgG1). (B) ADCC induced by PcMab-6-mG2a-f or control mouse IgG2a (mIgG2a) against MIA PaCa-2, Capan-2, and PK-45H cells. (C) CDC induced by PcMab-6-mG2a-f or control mIgG2a against MIA PaCa-2, Capan-2, and PK-45H cells. Values are shown as mean ± SEM. Asterisks indicate statistical significance (**P< 0.01, *P< 0.05; Welch’s t-test).
Figure 2.
ADCC and CDC by PcMab-6-mG2a-f. (A) A core-fucose-deficient mouse IgG2a mAb, PcMab-6-mG2a-f was established from PcMab-6 (mouse IgG1). (B) ADCC induced by PcMab-6-mG2a-f or control mouse IgG2a (mIgG2a) against MIA PaCa-2, Capan-2, and PK-45H cells. (C) CDC induced by PcMab-6-mG2a-f or control mIgG2a against MIA PaCa-2, Capan-2, and PK-45H cells. Values are shown as mean ± SEM. Asterisks indicate statistical significance (**P< 0.01, *P< 0.05; Welch’s t-test).
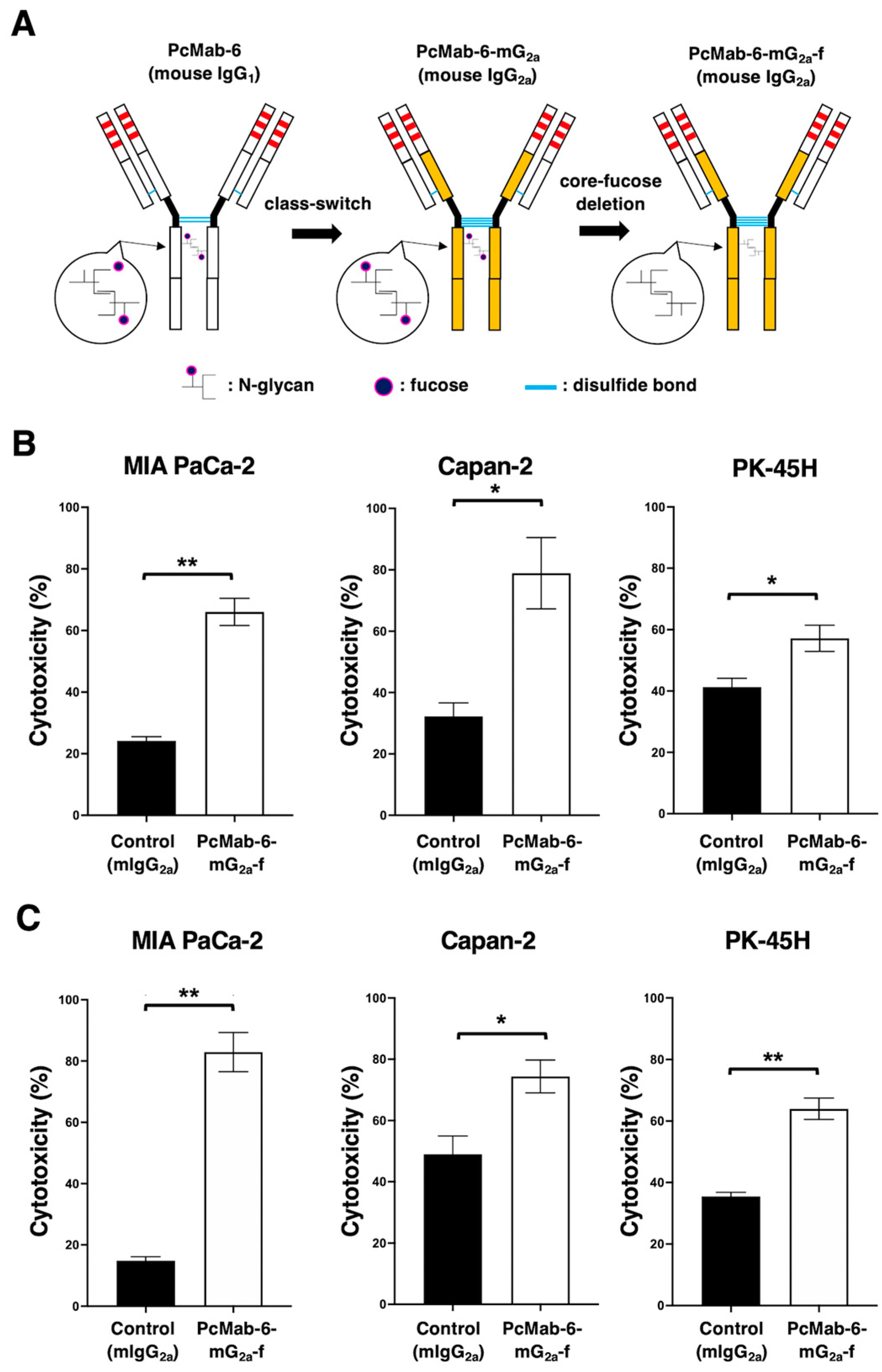
Figure 3.
Antitumor activity of PcMab-6-mG2a-f against pancreatic cancer xenografts. (A-C) MIA PaCa-2 (A), Capan-2 (B), and PK-45H (C) cells were subcutaneously injected into BALB/c nude mice (day 0). The 100 μg of PcMab-6-mG2a-f or control mouse IgG (mIgG) were intraperitoneally injected into each mouse on day 4 (PK-45H) or day 7 (MIA PaCa-2 and Capan-2). Additional antibodies were injected on days 11 and 13 (PK-45H) or days 14 and 16 (MIA PaCa-2 and Capan-2). The tumor volume is represented as the mean ± SEM. **P <0.01, *P <0.05 (ANOVA and Sidak’s multiple comparisons test). (D-F) The mice were euthanized on day 25 (PK-45H) or day 28 (MIA PaCa-2 and Capan-2) after cell implantation. The tumor weight of MIA PaCa-2 (D), Capan-2 (E), and PK-45H (F) xenografts was measured. Values are presented as the mean ± SEM. **P <0.01, *P <0.05 (Welch’s t-test). (G-I) The MIA PaCa-2 (G), Capan-2 (H), and PK-45H (I) xenograft tumors (scale bar, 1 cm). (J-L) The body weight of MIA PaCa-2 (J), Capan-2 (K), and PK-45H (L) xenograft-bearing mice treated with control mIgG or PcMab-6-mG2a-f. n.s., not significant.
Figure 3.
Antitumor activity of PcMab-6-mG2a-f against pancreatic cancer xenografts. (A-C) MIA PaCa-2 (A), Capan-2 (B), and PK-45H (C) cells were subcutaneously injected into BALB/c nude mice (day 0). The 100 μg of PcMab-6-mG2a-f or control mouse IgG (mIgG) were intraperitoneally injected into each mouse on day 4 (PK-45H) or day 7 (MIA PaCa-2 and Capan-2). Additional antibodies were injected on days 11 and 13 (PK-45H) or days 14 and 16 (MIA PaCa-2 and Capan-2). The tumor volume is represented as the mean ± SEM. **P <0.01, *P <0.05 (ANOVA and Sidak’s multiple comparisons test). (D-F) The mice were euthanized on day 25 (PK-45H) or day 28 (MIA PaCa-2 and Capan-2) after cell implantation. The tumor weight of MIA PaCa-2 (D), Capan-2 (E), and PK-45H (F) xenografts was measured. Values are presented as the mean ± SEM. **P <0.01, *P <0.05 (Welch’s t-test). (G-I) The MIA PaCa-2 (G), Capan-2 (H), and PK-45H (I) xenograft tumors (scale bar, 1 cm). (J-L) The body weight of MIA PaCa-2 (J), Capan-2 (K), and PK-45H (L) xenograft-bearing mice treated with control mIgG or PcMab-6-mG2a-f. n.s., not significant.
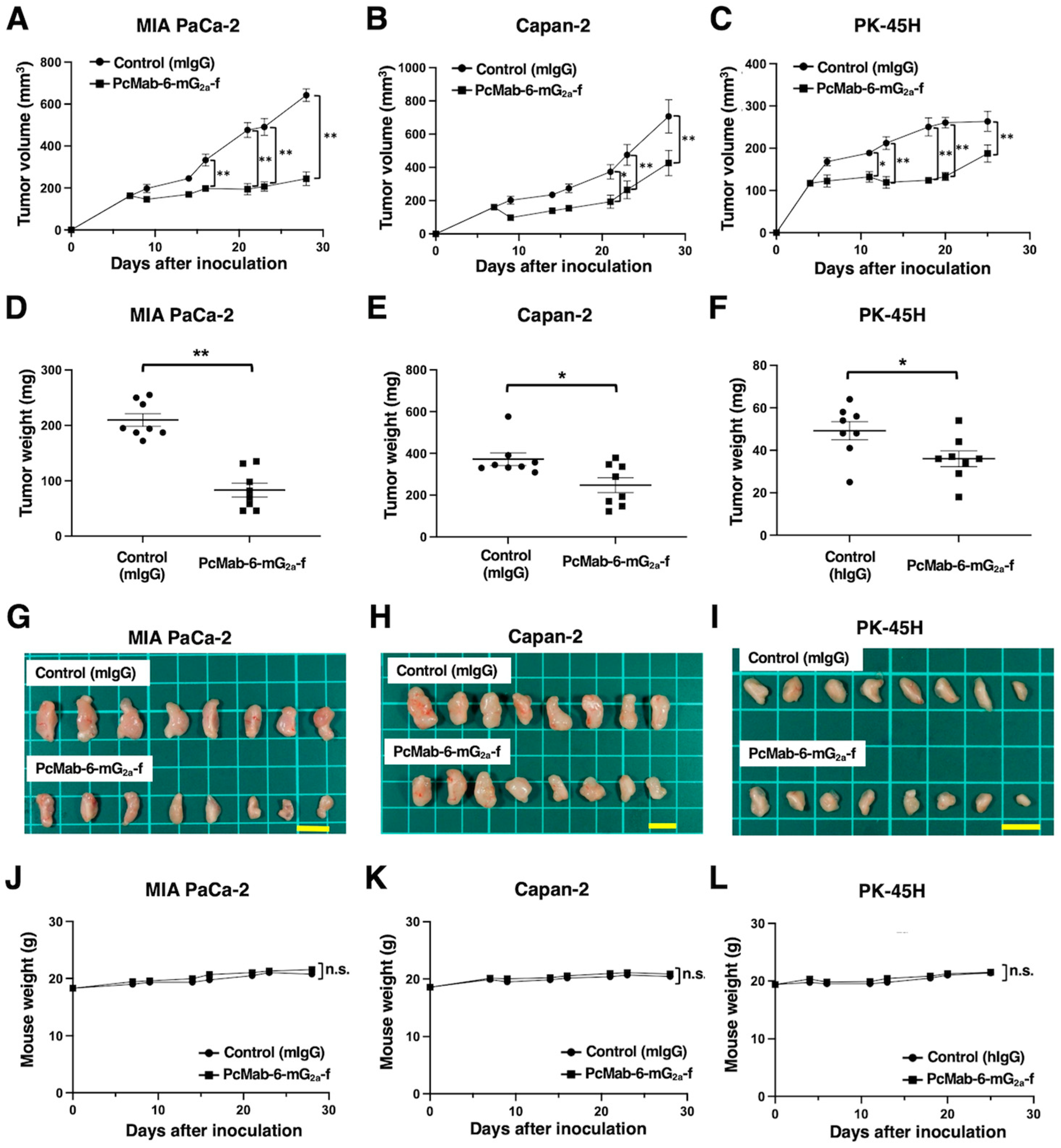
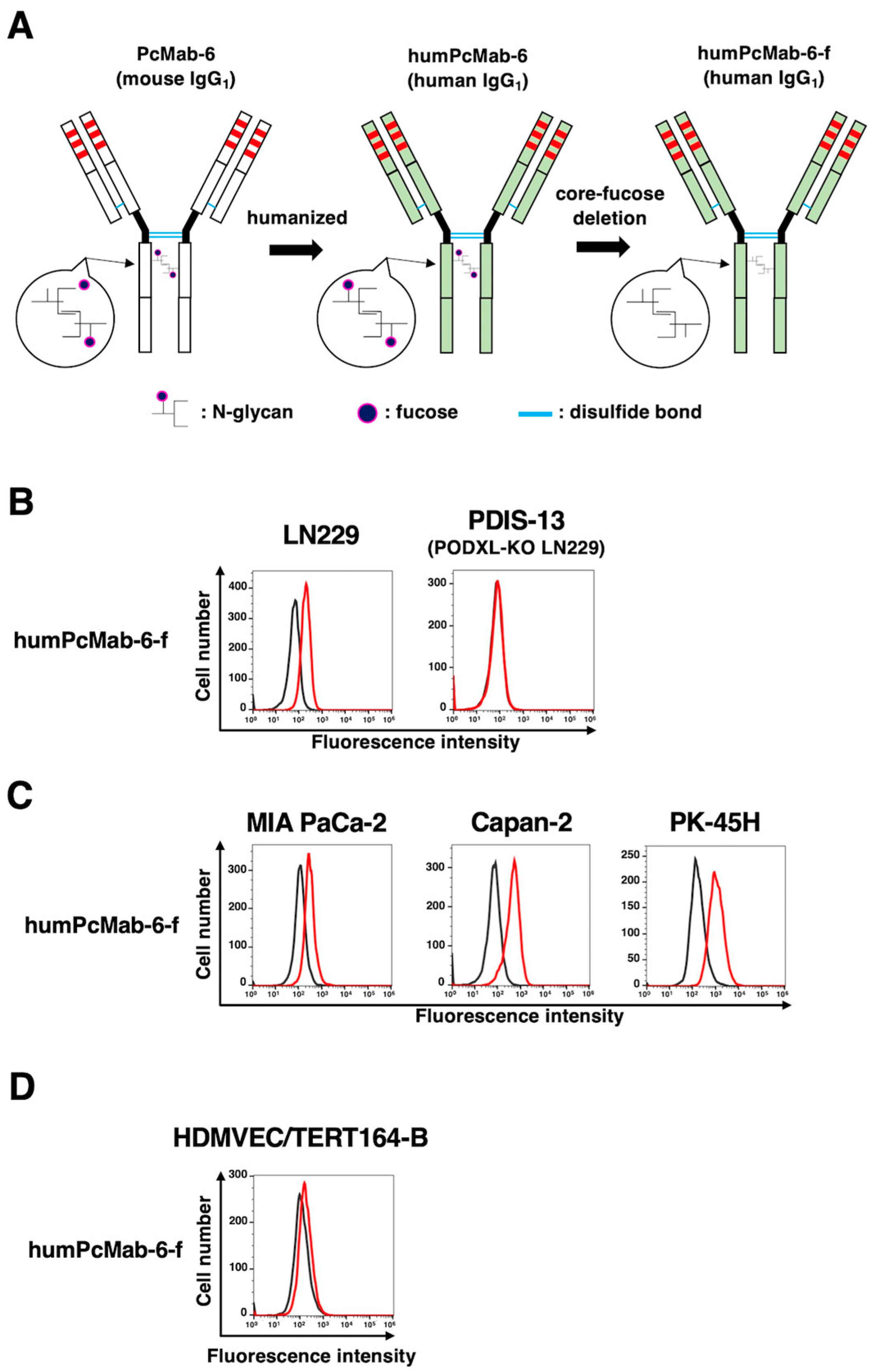
Figure 4.
Establishment of the humanized and defucosylated antibody, humPcMab-6-f. (A) A humanized IgG1 mAb, humPcMab-6 was generated from PcMab-6 (mouse IgG1). The core-fucose-deficient form (humPcMab-6-f) was established using Fut8-deficient ExpiCHO-S (BINDS-09) cells. (B) LN229 and PODXL-KO LN229 (PDIS-13) cells were treated with 10 µg/ml of humPcMab-6-f or buffer control. (C) MIA PaCa-2, Capan-2, and PK-45H cells were treated with 10 µg/ml of humPcMab-6-f or buffer control. (D) HDMVEC/TERT164-B cells were treated with 10 µg/ml of humPcMab-6-f or buffer control. Then, cells were treated with FITC-conjugated anti-human IgG. The black line represents the negative control (blocking buffer).
Figure 4.
Establishment of the humanized and defucosylated antibody, humPcMab-6-f. (A) A humanized IgG1 mAb, humPcMab-6 was generated from PcMab-6 (mouse IgG1). The core-fucose-deficient form (humPcMab-6-f) was established using Fut8-deficient ExpiCHO-S (BINDS-09) cells. (B) LN229 and PODXL-KO LN229 (PDIS-13) cells were treated with 10 µg/ml of humPcMab-6-f or buffer control. (C) MIA PaCa-2, Capan-2, and PK-45H cells were treated with 10 µg/ml of humPcMab-6-f or buffer control. (D) HDMVEC/TERT164-B cells were treated with 10 µg/ml of humPcMab-6-f or buffer control. Then, cells were treated with FITC-conjugated anti-human IgG. The black line represents the negative control (blocking buffer).
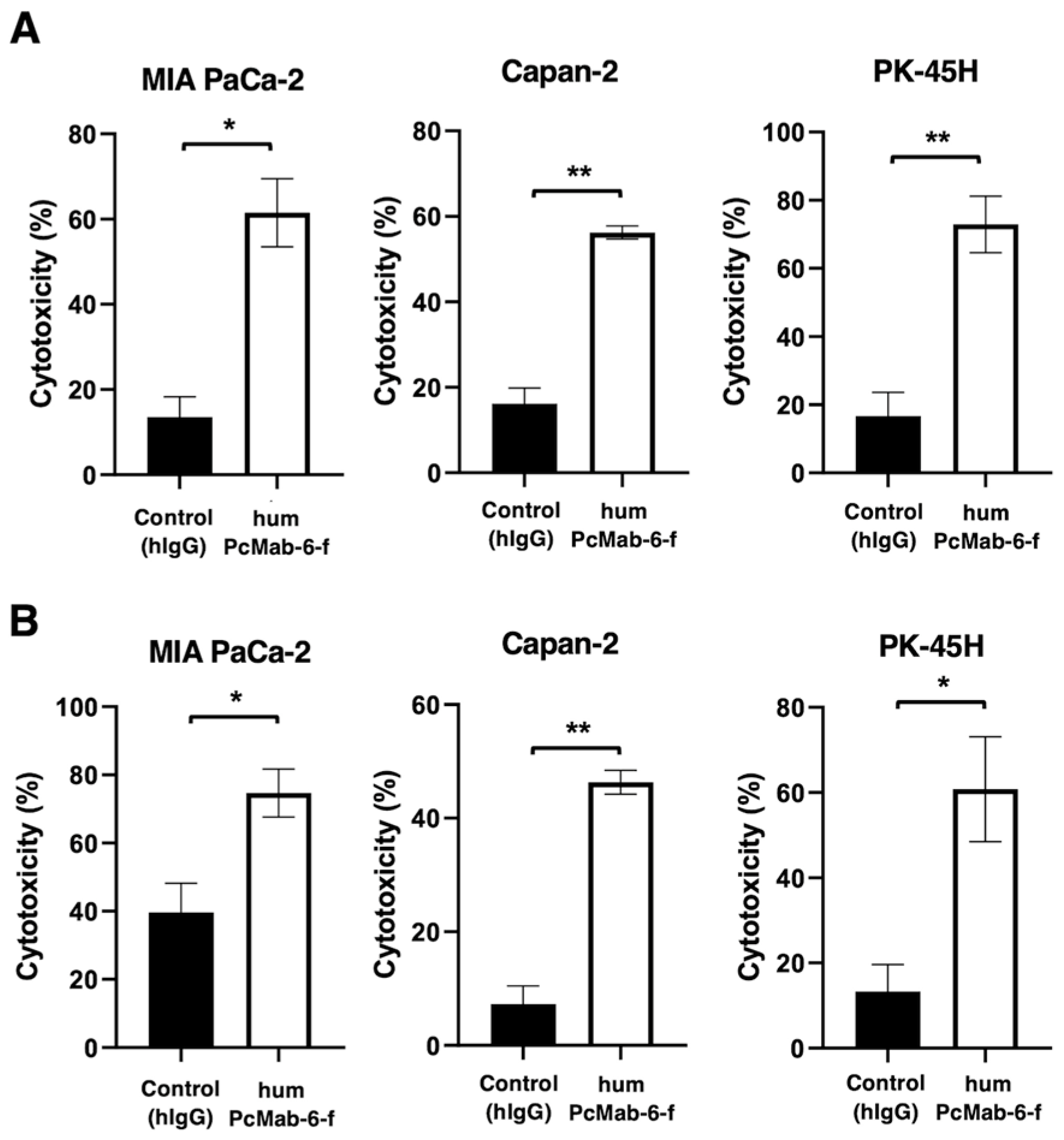
Figure 5.
ADCC and CDC by humPcMab-6-f against pancreatic cancers. (A) ADCC induced by humPcMab-6-f or control human IgG (hIgG) against MIA PaCa-2, Capan-2, and PK-45H cells. (B) CDC induced by humPcMab-6-f or control hIgG against MIA PaCa-2, Capan-2, and PK-45H cells. Values are shown as mean ± SEM. Asterisks indicate statistical significance (**P< 0.01, *P< 0.05; Welch’s t-test).
Figure 5.
ADCC and CDC by humPcMab-6-f against pancreatic cancers. (A) ADCC induced by humPcMab-6-f or control human IgG (hIgG) against MIA PaCa-2, Capan-2, and PK-45H cells. (B) CDC induced by humPcMab-6-f or control hIgG against MIA PaCa-2, Capan-2, and PK-45H cells. Values are shown as mean ± SEM. Asterisks indicate statistical significance (**P< 0.01, *P< 0.05; Welch’s t-test).
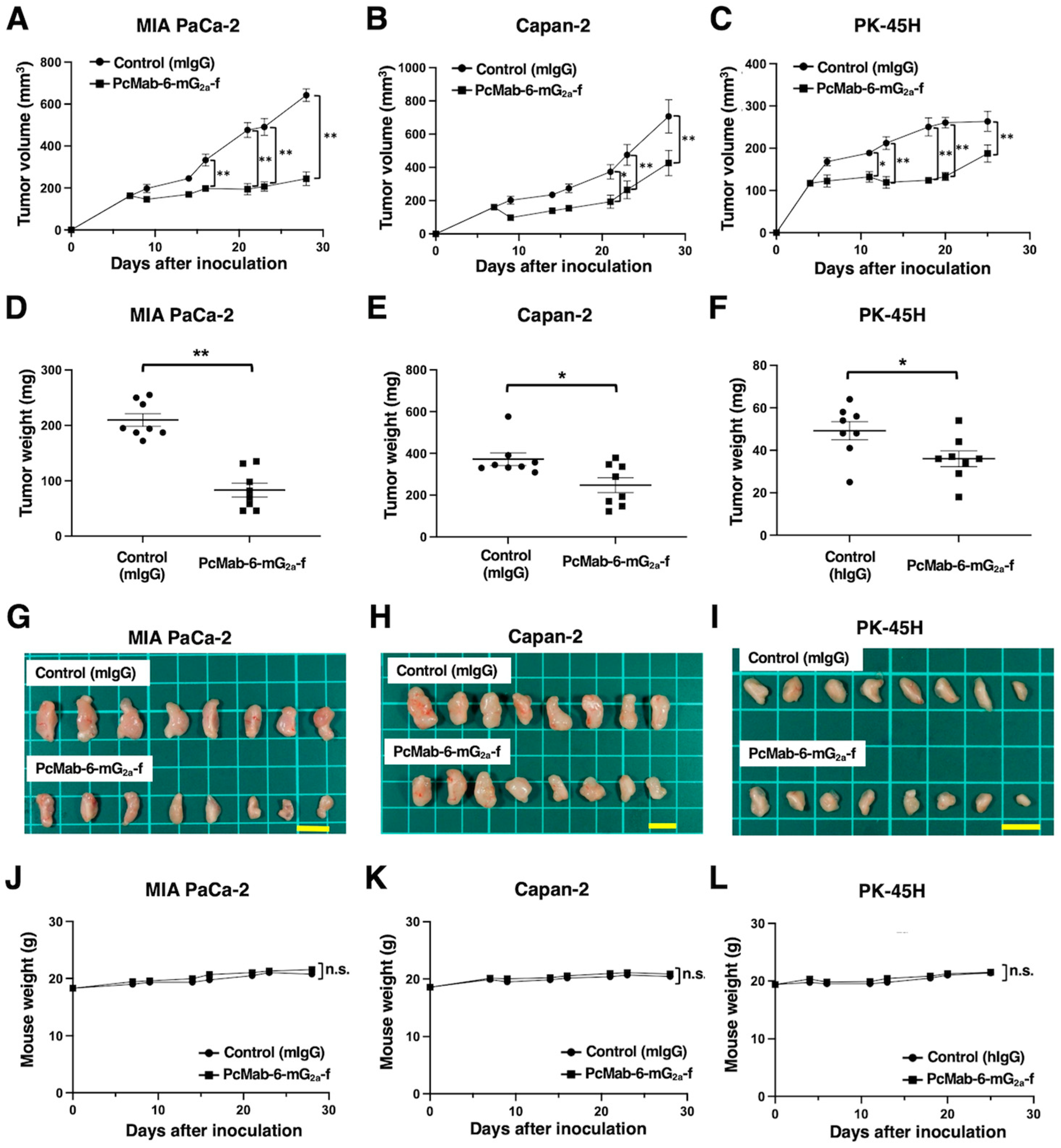
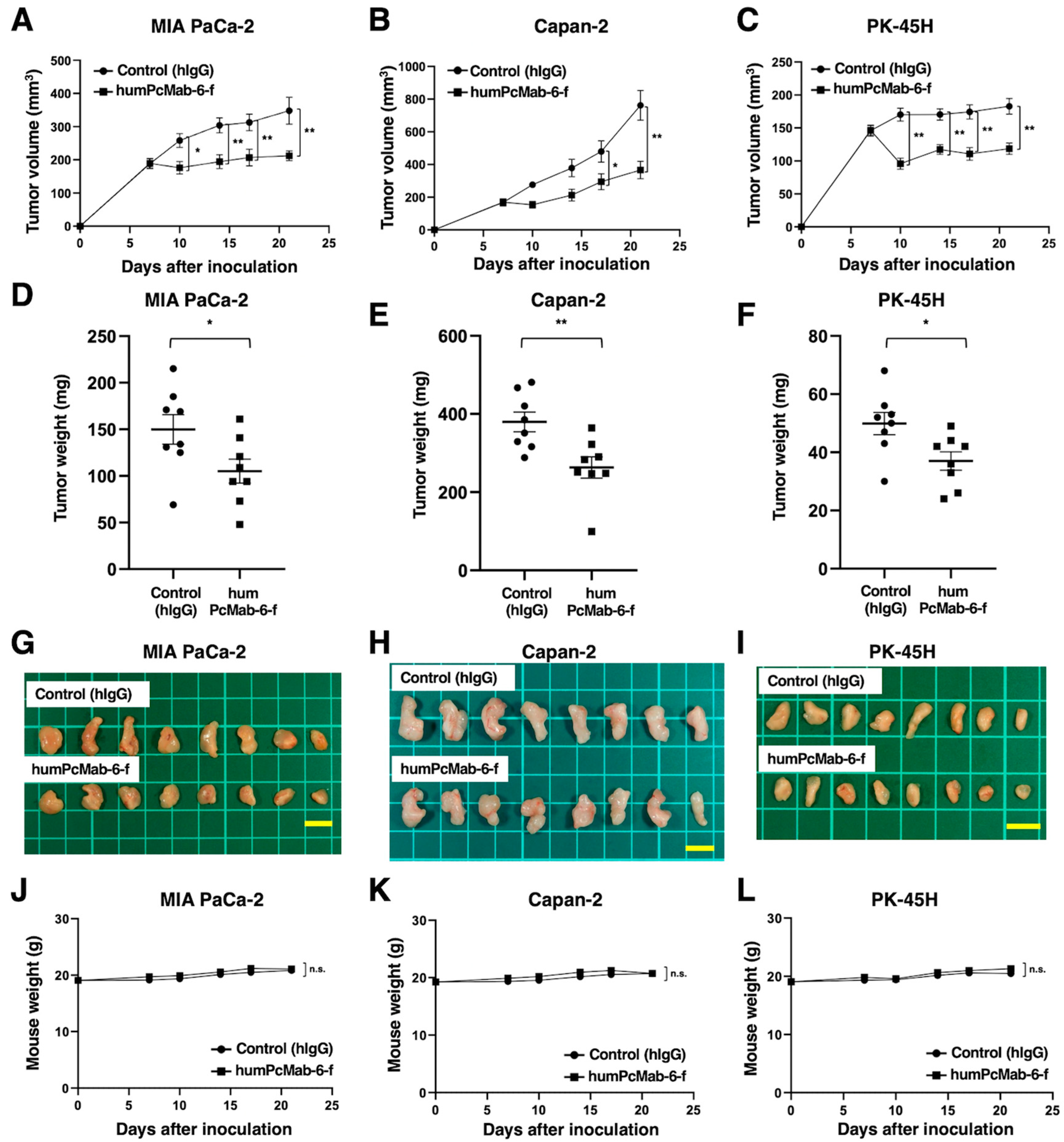
Figure 6.
Antitumor activity of humPcMab-6-f against pancreatic cancer xenografts. (A-C) MIA PaCa-2 (A), Capan-2 (B), and PK-45H (C) cells were subcutaneously injected into BALB/c nude mice (day 0). The 100 μg of humPcMab-6-f or control hIgG were intraperitoneally injected into each mouse on day 7. Additional antibodies were injected on day 14. Human NK cells were also injected around the tumors on days 7 and 14. The tumor volume is represented as the mean ± SEM. **P <0.01, *P <0.05 (ANOVA and Sidak’s multiple comparisons test). (D-F) The mice were euthanized at day 21 after cell implantation. The tumor weight of MIA PaCa-2 (D), Capan-2 (E), and PK-45H (F) xenografts was measured. Values are presented as the mean ± SEM. **P <0.01, *P <0.05 (Welch’s t-test). (G-I) The MIA PaCa-2 (G), Capan-2 (H), and PK-45H (I) xenograft tumors (scale bar, 1 cm). (J-L) The body weight of MIA PaCa-2 (J), Capan-2 (K), and PK-45H (L) xenograft-bearing mice treated with control hIgG or humPcMab-6-f. n.s., not significant.
Figure 6.
Antitumor activity of humPcMab-6-f against pancreatic cancer xenografts. (A-C) MIA PaCa-2 (A), Capan-2 (B), and PK-45H (C) cells were subcutaneously injected into BALB/c nude mice (day 0). The 100 μg of humPcMab-6-f or control hIgG were intraperitoneally injected into each mouse on day 7. Additional antibodies were injected on day 14. Human NK cells were also injected around the tumors on days 7 and 14. The tumor volume is represented as the mean ± SEM. **P <0.01, *P <0.05 (ANOVA and Sidak’s multiple comparisons test). (D-F) The mice were euthanized at day 21 after cell implantation. The tumor weight of MIA PaCa-2 (D), Capan-2 (E), and PK-45H (F) xenografts was measured. Values are presented as the mean ± SEM. **P <0.01, *P <0.05 (Welch’s t-test). (G-I) The MIA PaCa-2 (G), Capan-2 (H), and PK-45H (I) xenograft tumors (scale bar, 1 cm). (J-L) The body weight of MIA PaCa-2 (J), Capan-2 (K), and PK-45H (L) xenograft-bearing mice treated with control hIgG or humPcMab-6-f. n.s., not significant.