1. Introduction
Tinnitus is defined as the perception of sounds without any external auditory stimulation [
1] and can be indicative of various dysfunctions in the auditory hearing system [
2,
3]. Although different types of tinnitus and treatments have been identified [
4,
5], its origins are often unknown, and complete cure is rarely achieved [
6]. While occasional short-lived tinnitus noise is common, chronic tinnitus lasting longer than three months [
7] can be highly bothersome. Prevalence rates vary in the literature, ranging from conservative 10-19% [
6] to 11.9-30.3% [
8], with higher rates among older individuals and males [
8].
Decompensated tinnitus, characterized by difficulties concentrating, sleep disturbances, depression, anxiety, and reduced quality of life, can have a significant impact on an individual’s well-being [
9,
10]. It has even been demonstrated that patients with decompensated tinnitus bear a substantial psychopathological burden comparable to that of patients receiving inpatient treatment for major depression [
10]. The potential link between tinnitus and the risk of suicide has also been the subject of discussion [
11]. Notably, during the COVID-19 pandemic, an increase in tinnitus distress was observed among individuals experiencing loneliness, reduced social interactions, anxiety, and worry [
12]. Furthermore, tinnitus imposes a significant socioeconomic cost, estimated to be approximately 22 billion euros per year in Germany alone [
13]. Consequently, there is a need for relatively inexpensive home-based treatments to alleviate tinnitus symptoms.
1.1. Somatosensory Tinnitus
Somatosensory tinnitus (ST) is a sub-type of tinnitus and patients with ST have the ability to modulate the perception of their tinnitus through specific movements [
14]. Haider et al. [
15],p. 2. define tinnitus modulation as the
“capability of changing the tinnitus perception (frequency or intensity) by means of performing a certain maneuver or movement of the head or neck or jaw or limbs or the eyes.” Importantly,
“somatic modulation of tinnitus has been reported to be observable, when actively looked for, in up to 83% of tinnitus patients” [
6], p. 35.
Recent research suggests that ST is associated with neural connections and integration between the auditory and somatosensory systems in the central nervous system, as well as complex interactions with visual-motor, neuro-cognitive, and neuro-emotional networks [
15]. Inputs from the somatosensory and somatomotor systems, such as motor manipulation, muscle contractions of the head, neck, and limbs, orofacial movements, myofascial trigger points, cutaneous stimulation, and joint movements, can trigger or modify ST [
4,
15]. Pathological processes in the cervical spine and temporomandibular joint [
16] have been identified as potential causes of tinnitus, highlighting the significant influence of global cervical spine mobility on tinnitus [
17]. Moreover, movements of the eyes, fingers, hands, face have also been reported to affect ST see [
6,
15], for a summary.
1.2. Diagnosis and Treatment of Chronic ST
The diagnostic process aims to identify the underlying factors and degree of tinnitus while also addressing any coexisting hearing impairment. This serves as an essential foundation for any subsequent therapeutic intervention. In cases of acute tinnitus, particularly when it’s linked to sudden hearing loss, it is advised to consult the guideline for acute hearing loss [
18]. For chronic tinnitus, lasting longer than three month, referencing the S3 Guideline for Chronic Tinnitus is recommended [
7].
Given the diverse causes of tinnitus, the diagnosis of ST should involve a multidisciplinary team, including dentists and physical therapists. Symptoms such as
“head or neck problems, tooth or jaw diseases, frequent pain in the head, neck or shoulder girdle, poor posture, and severe bruxism” [
15], p. 4, along with the ability to modulate the volume or intensity of tinnitus, are indicative of ST see [
15]. Various approaches, including physiotherapeutic and stomatognathic treatments, chiropractic therapy, muscle relaxation, somatic modulation, electrical stimulation, and pharmaceutical and surgical interventions, are being explored to reduce ST see [
15], for a summary. In 2016, a meta-analysis examined the effectiveness of physical therapy on ST based on six studies [
19]. Two studies focused on temporomandibular disorders, and four studies investigated cervical spine treatments. The cervical spine studies included interventions such as stabilizing and mobilizing exercises [
20], cervical spine manipulations [
21], stretching, postural exercises, and auricular acupuncture [
22], or a combination of ischemic compression therapy, stretching, and posture exercises [
23]. Despite the risk of bias in these studies, the authors observed a significant positive treatment effect and recommended further controlled investigations [
19].
In the same year, Oostendorp et al. [
24] published a study on the effectiveness of “Manual Therapy Utrecht” (MTU) combined with education on Tinnitus Sensitization (TS). TS was defined as exhibiting five out of eight symptoms, including (1) widespread hyperalgesia and pain remote from the symptomatic region, such as shoulder and back pain; (2) vision impairments, (3) burning eyes; (4) modulation of tinnitus by (5) psychological stress or (6) sensory stimulation; (6) headache, (7) dizziness, or (8) tingling in legs or arms [
4], p. 107. The MTU
“focuses on static and dynamic posture, preference of movements, and selective somatosensory mechanical stimulation of spine joints, pelvis, and extremities” [
4], p. 107, performed by a therapist using gentle, low-velocity passive movements. The study included 126 patients with cervicogenic ST who were divided into two groups based on the presence (TS+) or absence (TS-) of tinnitus sensitization. The MTU treatment sessions were administered once or once every two weeks, with a maximum of 12 sessions. The TS+ group showed a clinically relevant mean reduction on a Tinnitus Visual Analogue Scale (TVAS) of -18.2, which was significantly larger than the -5.9 reduction in the TS- group that did not reach clinical relevance [
24].
A recent study by Van der Wal et al. [
25] compared the effectiveness of orofacial treatment, including physical therapy and occlusal splints for grinding, on tinnitus complaints in patients with temporomandibular ST. The study included 80 participants in a randomized controlled trial with a delayed treatment design. They observed a clinically relevant improvement of
on the tinnitus questionnaire TQ, [
26] in 34% of the patients immediately after the treatment. Similarly, 41% of the patients showed a relevant improvement of
points on the Tinnitus Functional Index TFI, [
27,
28].
1.3. Feldenkrais Method
The Feldenkrais Method, named after its creator Moshé Feldenkrais, a physicist, and martial arts expert, is a form of somatic education aimed at enhancing self-awareness, movement and overall well-being [
29]. It employs two techniques. In Functional Integration, a Feldenkrais practitioner provides individual sessions by gently touching and manually guiding the client’s body without verbal communication [
30]. In Awareness Through Movement (ATM) group lessons, clients typically lie or sit on the floor and follow verbal instructions or use visualization to imagine movements while paying attention to bodily sensations [
29,
30]. For example, clients may be instructed to look left while rolling their head to the right, simultaneously moving their lower jaw and/or tongue to the left. Other exercises involve exploring different options for performing a movement task and discerning which feels more effortless. These perceptual distinctions are based on individual positive feedback (pleasant, easy, and less effortful) compared to less favorable signals such as pain or discomfort [
30].
The Feldenkrais method is comparable to other physical therapy techniques [
29]. It has been shown to improve balance, mobility, fear of falling, quality of life, and gait speed in elderly individuals [
31,
32,
33]. In patients with chronic low back pain, it has demonstrated similar or better benefits compared to stability exercises and back school programs [
34,
35,
36]. For patients with Parkinson’s disease, Feldenkrais has been found to reduce depression and improve quality of life, balance, mobility, strength, and gait speed [
37,
38]. And recently, patients with stroke were found to benefit from the method in a group-setting in terms of improved body awareness, quality of life, and better arm and leg control [
39]. Overall, accumulating evidence suggests that Feldenkrais can enhance well-being and physical functioning.
In summary, there is accumulating evidence that Feldenkrais increases well-being and physical functioning. This suggests a high likelihood that Feldenkrais ATM lessons have the potential to alleviate neck pain and improve overall well-being, offering potential benefits for individuals with ST. Moreover, the home teaching situation has not only benefits in pandemic situations, it may provide greater convenience and reduce costs, making online Feldenkrais lessons an attractive option.
1.4. Aims of the Current Study
Our principal aim was to conduct a pilot investigation to evaluate the efficacy of twelve weeks of online Feldenkrais ATM lessons. The objective was to assess their impact on diminishing the perceived distress and severity of somatosensory tinnitus and the severity of neck complaints. Similar to the MTU (see description above), the Feldenkrais Method employs gentle, slow-paced movements to heighten own-body awareness and explore movement alternatives. Given its successful implementation in studies involving back pain and the success of other physiotherapeutic approaches to tinnitus, we postulated that this approach could also yield a reduction in neck pain complaints and, importantly also tinnitus distress.
Furthermore, we postulated that the reduction in tinnitus distress would be correlated with the following factors: i) decreased reports of neck pain complaints, ii) decreased influence of head movements on tinnitus, iii) enhanced overall quality of life, and iv) heightened bodily awareness. The assessment of bodily awareness was conducted using the multidimensional assessment of interoceptive awareness (MAIA) questionnaire, as outlined in the work by Mehling et al. [
40].
As secondary outcomes, we aimed to measure the effects of the ATM lessons on participants by assessing state anxiety and perceived tinnitus intensity administered before and after each lesson. Different outcomes are plausible: On one hand, relaxation and focused attention on various body parts, movement, and breath could lead to a reduction in perceived tinnitus intensity, as participants’ attention is diverted from the tinnitus, and relaxation of neck/jaw muscles or other muscle groups may contribute to decreased perceived tinnitus intensity. On the other hand, the context of lying on the floor in quiet and engaging in concentrated movements and inner processes could temporarily heighten tinnitus perception, and depending on the subjective experience individual state anxiety levels may either decrease or increase.
In an exploratory manner, we aim to investigate factors associated with a positive treatment effect and examine correlations between the initial screening measures and changes in tinnitus severity and neck pain.
2. Materials and Methods
2.1. Participants
2.1.1. Considerations on Sample Size
In a preceding investigation conducted by Van der Wal et al. [
25], the efficacy of a non-invasive orofacial treatment in mitigating tinnitus severity among patients afflicted with temporomandibular somatosensory tinnitus was illustrated. This investigation employed both an early and a late intervention group, each consisting of 40 patients. The Tinnitus Functional Index (TFI) was utilized to gauge treatment effectiveness, revealing an average reduction of 13.8 points in the early intervention group and 5.0 points in the late intervention group. The findings were notably significant within the early intervention group,
t(38) = 4.254,
p < .001, and the trend approached significance within the late intervention group,
t(37) = 1.825,
p = .076.
Given that comprehensive data including effect sizes and standard deviations/errors were not provided, calculations were conducted for Cohen’s
d [
41] and the Pearson product-moment correlation coefficient
r using the formulas
and
[
42] for pre-and post-treatment comparisons. For the early intervention group (
N = 40), Cohen’s
d was computed as 1.380, corresponding to an effect size of
r = 0.568. In the late intervention group (
N = 39), the computed Cohen’s
d was 0.600, yielding an effect size of
r = 0.287.
However, due to the paucity of research investigating the impact of Feldenkrais Awareness Through Movement (ATM) lessons on tinnitus, our initial intention was to incorporate a total of 40 participants, considering this sample size to be conducive to detecting potential effects. Regrettably, our feasibility study could only accommodate a cohort of 20 patients in its initial phase, as patient recruitment was heavily influenced by the Corona pandemic, as fewer patients than normal visited the Tinnitus Centre of the Jena University Hospital (TC JUH). These patients were instructed by two Feldenkrais practitioners, with group sizes consisting of 10 individuals each. The allocation of patients to specific groups was based on relevant and quasi-random criteria, primarily hinging on their preferred availability on either Monday or Wednesday.
2.1.2. Inclusion and Exclusion Criteria
The primary inclusion criteria were tinnitus modulation along with a TFI score ≥ 6 and a Neck Bournemouth Questionnaire NBQ, [
43,
44] score ≥ 6 [
19,
45]. Additional inclusion criteria were: (i) a minimum age of 18 years; (ii) no other therapies were initiated or discontinued during study participation; (iii) the dosage of regularly taken medications were not changed during study participation; (iv) no traumatic injuries to the cervical spine or temporomandibular joints within six months prior to the start of the procedure; (v) no orofacial surgery within six months prior to the start of the intervention; (vi) the technical requirements and skills were met; (vii) excellent knowledge of German; (viii) complete understanding of the verbal instructions; (i) the execution of the instructed movements was not restricted by physical limitations.
2.1.3. Final Sample
A total of 17 (10 female, 7 male) participants took part in the study. It is important to note that two additional participants were initially enrolled in the study; however, they withdrew before the commencement of the first Awareness Through Movement (ATM) lesson due to personal commitments and constraints in their available time resources. The mean age of participants was 49.8 years (
SD = 10.9, range: 25-63,
N = 17). Please refer to
Table 1 for a more detailed overview of participant demographics. In order to provide an outline of the sample characteristics prior to the implementation of the treatment, Spearman correlations (two-tailed) were conducted using data from the
Initial Screening. Details on these correlations can be found in
Supplemental Material Section 1.
Prior to their involvement, all participants provided written informed consent. The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and adhered to the ethical standards set by the American Psychological Association. The research protocol was approved by the Ethics Committee of the University Hospital Jena (Reference 2021-2378-BO).
2.2. Feldenkrais Practitioners
The weekly lessons were conducted by two experienced Feldenkrais practitioners, namely authors SH and MS, who conducted the sessions on Mondays and Wednesdays, respectively. Both attended the official FELDENKRAIS® training program (SH between 1990-1993 in Brig, Switzerland, and MS between 2008-2012 in Berlin, Germany, respectively) and have been working as professional Feldenkrais practitioners since then. They both have other related qualifications. MS is a professional physical therapist with several additional certifications, and SH worked as a professional occupational therapist from 1988 to 2010 before studying psychology. She completed both her Diplom and her Ph.D. in Psychology before obtaining her licence to work as a therapeutic psychologist in 2018.
2.3. Materials
2.3.1. Feldenkrais-Workprogram
The 12-week-treatment program was based on the manual titled
“Spannungen lösen – Stress bewältigen mit der Feldenkrais-Methode, Kurskonzeption nach §20 SGB V”(engl. “Release tension - manage stress with the Feldenkrais method”, course concept according to §20 SGB V) [
46]. This manual included ten Awareness Through Movement lessons. Lesson 8 was divided into two parts and taught during sessions eight and nine. Additionally, Lesson 1 was repeated in the final group meeting to allow participants to compare changes, experiences in awareness, body-state, and their ability to follow instructions.
2.3.2. Primary Outcome Measures
TQ: The German version [
47] of the Tinnitus-Questionnaire (TQ) [
26] was used as a primary outcome measure. It consists of 52 items and includes scales to assess emotional and cognitive stress, urgency, differences in auditory perception, sleep disorders, and associated somatic complaints. Participants respond to the questions using a three-point scale (“Agree - partly - not”). The TQ is commonly employed in clinical care and scientific studies to assess the severity of psycho-social tinnitus stress (
tinnitus distress) and evaluate the effects of therapy e.g.,[
25]. A change of 8.72 points is considered clinically relevant [
48]. The TQ is routinely administered at the TC JUH.
TFI: The German version [
49] of the Tinnitus Functional Index (TFI) [
27] was used as another primary outcome measure. It comprises 25 items that are rated on a Likert scale from 1 to 10, with higher scores indicating greater limitations. The TFI assesses the inconvenience of tinnitus over the past week across eight scales: intrusiveness, reduced sense of control, cognitive interference, sleep disturbance, auditory difficulties, interference with relaxation, reduced quality of life, and emotional distress. It provides a measure of
tinnitus severity following an intervention e.g.,[
25] and allows for more detailed gradations compared to the TQ. A reduction of 13 points on the total TFI score after a clinical treatment is considered clinically relevant and indicative of subjective improvement [
25,
27,
28].
NBQ: The German version [
43] of the Neck Bournemouth Questionnaire (NBQ) [
44] was used to assess neck disorders. It consists of seven questions that are answered on a Likert scale from 0 to 10, measuring the severity of neck disorders and their impact on well-being, professional activities, and daily activities. The total score on the NBQ can range from 0 to 70, and a reduction of 17% has been identified as clinically relevant [
44], p. 146.
2.3.3. Secondary and Control Outcome Measures
HMM: The Head Movement Modulation (HMM) measure was developed specifically for this study to assess the strength of tinnitus modulation by head movements. Participants were asked to rate, on a scale of 0 to 10, how strongly eight different movements (i.e., head turn, head nod, head tilt, jaw open and close, jaw move sideways, clench teeth, shoulder movements, eye movements) modulated their tinnitus during the last week. The HMM score is the sum of the ratings for the eight items.
STAI-State: The German version [
50] of the State-Trait Anxiety Inventory (STAI) [
51] was used to assess participants’ well-being directly before and after each weekly treatment. The state scale consists of 20 items and measures the current emotional state of anxiety, characterized by tension, anxiety, nervousness, inner turmoil, and fear of future events. Higher scores on the STAI-State indicate higher levels of anxiety. It is sensitive to situational influences and intrapsychic processes, making it suitable for assessing anxiety in the context of this study.
TVAS: The Tinnitus Visual Analogue Scale (TVAS) [
4] is a line ranging from 0 (no tinnitus) to 100 (worst imaginable tinnitus intensity) used to assess participants’ subjective perception of tinnitus intensity at the moment of measurement. While the length of the line on participants’ output devices was not controlled, the relative changes in TVAS scores could be captured as participants tended to use the same device for both pre- and post-ATM questionnaires.
MAIA: The German translation of the Multidimensional Assessment of Interoceptive Awareness (MAIA) questionnaire [
40] was used to measure participants’ own body awareness and perception of their internal bodily sensations. The questionnaire consists of 32 items covering eight aspects of interoceptive perception: Noticing, Non-Distraction, Not Worrying, Attention Regulation, Emotional Awareness, Self-Regulation, Listening to the Body, and Trust. Participants rate their experience with each item on a 6-point Likert scale from “0 - never” to “5 - always”.
WHO: The German version of the short World Health Organisation (WHO) health questionnaire WHO-BREF,[
52] consists of 26 items. In addition to one item assessing overall health and one item assessing overall quality of life, the remaining items are divided into four domains. The
Physical Health domain assesses various aspects of physical well-being, including activities of daily living, dependence on medical substances or aids, energy levels and fatigue, mobility, pain and discomfort, sleep and rest, and work capacity. The
Psychological Health focuses on psychological well-being and includes items related to bodily image and appearance, negative and positive feelings, self-esteem, spirituality, religion, personal beliefs, thinking, learning, memory, and concentration. The
Social Relationships domain explores the individual’s social relationships, including personal relationships, social support, and sexual activity. The
Environment domain pertain to the individual’s environment and its impact on their well-being. It covers aspects such as financial resources, freedom, physical safety, security, accessibility and quality of health and social care, home environment, opportunities for acquiring new information and skills, participation in and opportunities for recreation and leisure activities, and the physical environment in terms of pollution, noise, traffic, and climate, as well as transportation. The WHO questionnaire provides a comprehensive assessment of health-related quality of life, considering physical, psychological, social, and environmental dimensions.
2.4. General Procedure
The participant recruitment took place between January and June 2022. Potential participants were identified through patient records at the TC JUH. Patients with records, mentioning tinnitus modulation diagnosed by medical doctors of the Institute for Physiotherapy of the JUH were contacted and invited to participate in the study. Interested individuals were provided with participant information, consent forms, and a link to the Initial Screening questionnaire via email. Note that these patients have already completed a one-week outpatient tinnitus therapy at the TC JUH. In addition, two patients (AEB02A and WCL52A) learned about the study through personal contacts and provided a tinnitus diagnosis from their attending ear-nose-throat specialist.
Individual online information meetings were conducted via videotelephony implemented in Zoom [
53], for which the Jena University Hospital has a licensed version. Participants were briefed about the study’s conditions and had the opportunity to ask questions. To proceed with participation, participants were required to sign the informed consent form and send it back to the TC JUH.
Group sessions were scheduled from 6:00 to 7:30 p.m. and commenced on Wednesday, April 12, 2022, and Monday, June 13, 2022. Each session began with a personalized welcome, followed by providing participants with the link to the five-minute ATM Screening questionnaire (see below for details). Before each ATM lesson, participants had the opportunity to ask questions. After the lesson, during a break, participants were required to fill out the ATM Screening questionnaire once again. The feedback round, which typically occurred from approximately 7:00 to 7:30 p.m., involved discussing individual experiences and perceptions during the ATM lesson and the past week. Relevant information related to Feldenkrais, stress, embodiment of emotions, etc., was shared during the feedback round, aligning with the guidelines outlined in the Work Program Manual. Participants were given small homework assignments, such as focusing on specific tasks or making changes to their daily routines. The feedback sessions were led by either EB and/or VGS, alongside the Feldenkrais practitioner.
Note that participants who were unable to attend the ATM session in the group setting received an email with a download link to the audio recording of the ATM lesson in MP3 format. They were instructed to complete the lesson as soon as possible and were provided with a link to the ATM Screening questionnaire.
The weekly ATM lessons were conducted by either MS (on Wednesdays) or SH (on Mondays), except for lesson 7 of the Monday group, which was taught by MS due to SH’s unavailability on that day. Participants were in a private setting, such as their homes, while lying or sitting within the camera’s range. The Feldenkrais practitioner provided verbal instructions for a sequence of slow and attentive movements. The movements were gentle and performed at a slow pace, potentially leading to a slight feeling of coldness depending on individual constitution. Participants with physical limitations were instructed to make necessary adjustments, such as supporting themselves with pillows to ensure comfort and alleviate any discomfort or pain. If certain movements were challenging, participants were encouraged to modify their positions (e.g., raising their legs instead of lying down) or imagine the movement without physically performing it. Participants were advised to wear warm, comfortable, non-restrictive clothing and have a blanket nearby to prevent feeling cold during the session.
Data collection for the study was conducted using LimeSurvey [
54] and Psytoolkit [
55,
56]. To ensure privacy and confidentiality, no personal identifying information was collected in any of the questionnaires. Instead, participants were assigned individual pseudonymization codes that they had to enter each time to correctly match their data across different sessions. The following questionnaires were administered at different stages of the study (cf.
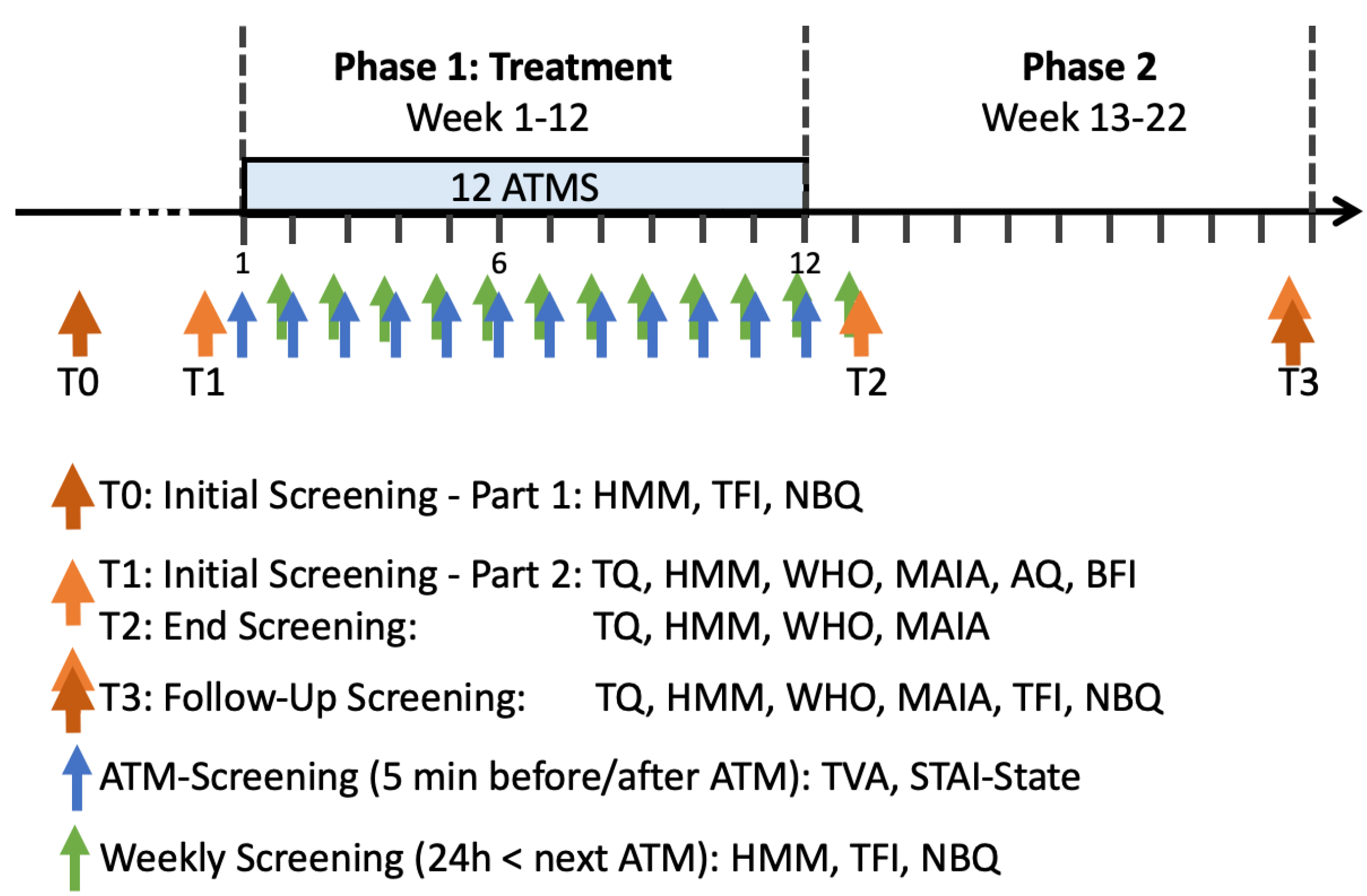
Figure 1):
Initial Screening - Part 1: This questionnaire was collected immediately after the initial contact. It consisted of demographic information, including age, gender, education, hobbies, habits, and preferred time slots for study participation. Additionally, it included the TFI, NBQ, and the HMM questionnaire.
Initial Screening - Part 2: Administered a few days before the first lesson, this questionnaire included the TQ, HMM, WHO, MAIA, and separately, for exploratory analyses we assessed personality traits using the Autism Quotient [
57,
58] and a short Big Five inventory [
59].
Weekly Screening: This questionnaire was sent six days after each ATM lesson and included the HMM, TFI, and NBQ. Participants were requested to complete it within twenty-four hours before the next lesson.
ATM Screening: Conducted directly before and after each lesson, this questionnaire included the STAI and the TVAS.
End Screening: Administered at the end of the study, this questionnaire included the TQ, HMM, WHO, MAIA, and additional questions to evaluate participants’ experiences and the effects of Feldenkrais on their tinnitus and everyday life.
Follow-Up Screening: Administered 8-9 weeks after the End Screening, this questionnaire included all previously mentioned questionnaires (HMM, TQ, MAIA, WHO, TFI, NBQ) and asked participants about the frequency of their practice per week using the recordings of the lessons.
Note that all lessons and feedback sessions were recorded using Zoom [
53].
2.5. Analysis Plan
To analyze our data, we established the following plan:
Treatment effects were estimated by comparing pre- and post-treatment measures, (i.e., the Initial and End Screening data TQ, MAIA, WHO, HMM) using paired t-tests (one-tailed), based on the following directional hypothesis: the treatment reduces tinnitus distress and our HMM measure (i.e., how strong head-movements modulate the tinnitus) and increases interoceptive awareness and health.
Considering the presence of missing values and incomplete Weekly Screening data, linear mixed modeling (LMM) was used, as it allows allows for the inclusion of subjects with missing data, thus maximizing the sample size and reducing bias. Separate analyses were conducted for the TFI, NBQ, and HMM to analyse the effect of time (treatment) on these variables. Model comparisons were done using Analysis of Variance (ANOVA).
We used LMM to estimate the effect of the ATM lesson on well-being (STAI) and perceived tinnitus intensity (TVAS) by analysing the ATM Screening data that was gathered directly before and after each ATM. We further tested, weather there was an effect of time (treatment) on the mean STAI or mean TVAS (per ATM and participant).
To capture the magnitude of changes for each variable, we calculated difference scores for the dependent variables. Spearman correlation analysis (two-tailed) was then performed on the difference scores to explore effects of the treatment in greater depth.
In an exploratory analysis, the under 4) mentioned difference scores were correlated with the Initial Screening data to identify potential treatment beneficiaries.
All analysis were done in
R (Version 4.2.2., 2022-10-31) [
60] using lme4 [
61] version 1.1-34, for linear mixed modeling and the anova() function of the stats package version 4.2.2 [
62] for model comparisons. Unless stated otherwise, we report means and standard errors of the mean (
M ±
SEM) and Cohen’s
d as an effect size measure for paired samples [
41,
63].
3. Results
3.1. Missing Data
Participants AIM33A and ISE22I quit the study after the seventh session. Participant AIM33A reported substantial problems with relaxedly lying on the floor due to a scoliosis and overwhelming tinnitus noise. Participant ISE22I stated time issues to be the reason for leaving. Participants AIS02A and ARS81A did not fill out the
End Screening questionnaire. Participant RHH19U’s
Initial Screening Part 1 was not recorded properly. From participant EIR79H, we only analysed data gathered before the 24th of May, as she started a stationary tinnitus rehabilitation therapy that day. Note that some participants occasionally missed the ATM or missed to fill out the questionnaire(s), see
Table 1 for more details.
It is important to note that the responses to the additional questions in the
End-Screening, which aimed to evaluate participants’ experiences and the effects of Feldenkrais on their tinnitus and everyday life, were not subject to formal analysis. An overview of participants’ responses can be found in the
Supplemental Material Section 2. Furthermore, the data from the
Follow-up Screening was not formally analyzed due to a substantial amount of missing data, with only ten participants providing complete data.
3.2. Comparing Initial and End Screening
The results of the statistical analyses indicate significant changes in several measures after the treatment. Specifically:
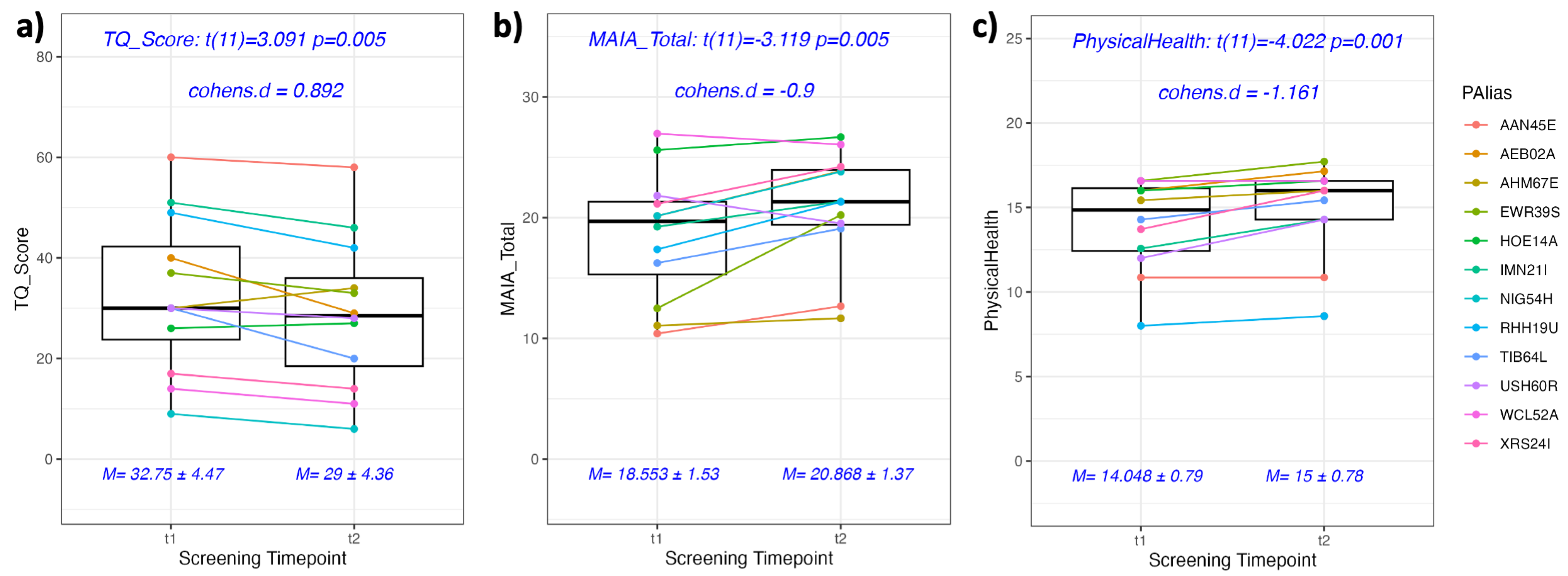
The Tinnitus Questionnaire (TQ) score decreased significantly by 3.75 points from an initial value of 32.75 ± 4.47 to a post-treatment value of 29.00 ± 4.36,
t(11) = 3.091,
p = .005, Cohen’s
d = 0.892. This large effect underscores a notable decrease in tinnitus distress subsequent to the intervention (see
Figure 2a).
The measure of subjective interoceptive awareness (MAIA) increased significantly by 2.31 points from 18.55 ± 1.53 to 20.86 ± 1.37,
t(11) = -3.119,
p = .005,
d = -0.900. Accordingly, this is also a large effect revealing an improvement in participants’ awareness of internal bodily sensations following the intervention (see
Figure 2b).
The scores for physical health, also assessed by the WHO questionnaire, showed a significant increase from 14.0 ± 0.79 to 15.0 ± 0.78,
t(11) = -4.022,
p = .001,
d = -1.161 (see
Figure 2c), which indicates a large effect and suggests an improvement in participants’ perception of their physical health.
The scores for overall quality of life, as assessed by the World Health Organization (WHO) questionnaire, showed a significant increase from an initial value of 12.0 ± 0.85 to a post-treatment value of 14.0 ± 1.04, t(11) = 2.569, p = .013, d = 0.742 , revealing a medium sized effect, and indicating a positive change in participants’ perception of their overall quality of life.
There was no significant change in the measure of how strongly head movements (HMM) affect the tinnitus, t(11) = 1.066, p = .845, indicating that there are no general changes in how far head movements affect the Somatosensory Tinnitus (ST) following the intervention, measured at this stage.
Please note that we report unadjusted p-values as our analyses were pre-planned and aligned with our hypotheses. After adjustments (For five comparisons the alpha level increases from 5% to 22.6% due to multiple tests. To maintain a global significance level
of 5%, each test would require a more stringent alpha of .0102), the TQ, MAIA, and the WHO’s physical health component still show significant differences between initial and final screenings, with the WHO’s quality of life measure narrowly exceeding the local significance by only .0028.
In summary, our measurements reveal significant improvements, including moderate to strong effects in reductions in tinnitus distress, increased self-awareness, improved physical health, and quality of life.
3.3. Linear Mixed Modeling of Weekly Screening Data
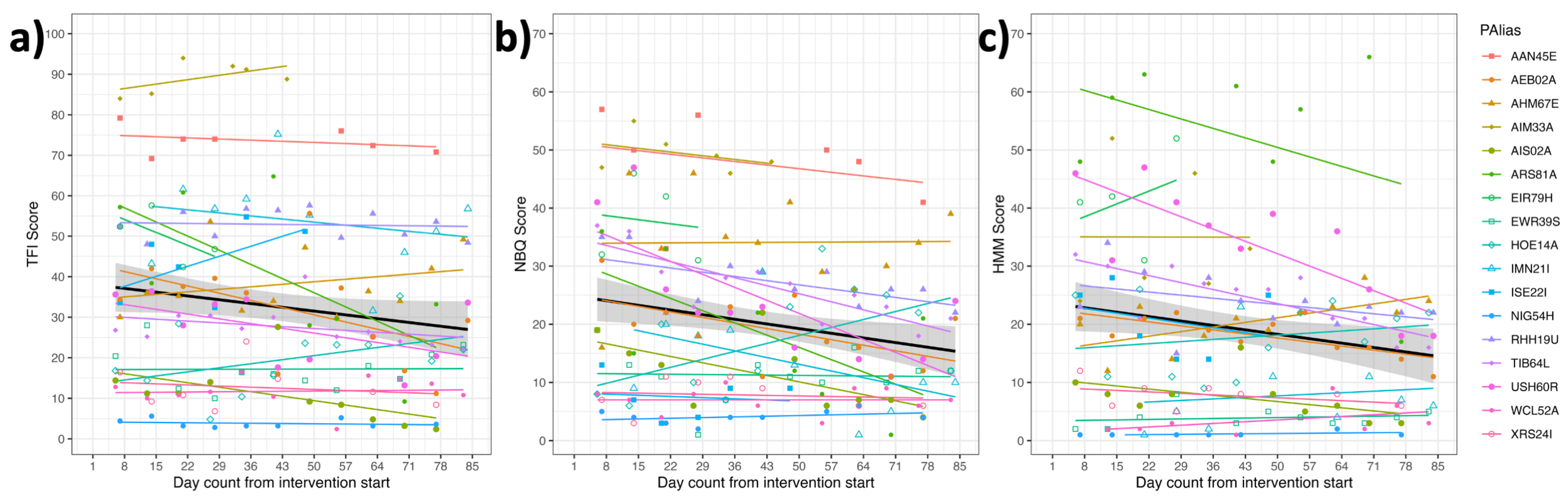
The
Weekly Screening was completed within a 24-hour window preceding the commencement of each subsequent ATM lesson. This screening encompassed the Tinnitus Functional Index (TFI), the Neck Bournemouth Questionnaire (NBQ), and our measure on how strongly head movements modulate (HMM) the tinnitus. To investigate alterations in these variables over the course of time (see
Figure 3), we employed linear mixed modeling (LMM) as described in the analysis plan. Comparisons between models were conducted using ANOVAs. Additional information is provided below for further clarity. Notably, all pertinent R outputs are presented in
Supplemental Material 3.1 to 3.4.
3.3.1. Tinnitus Functional Index (TFI) over Time
To analyze the changes in TFI over time (see
Figure 3a), two models were compared. Model 1 (
) included time measured as the number of days from the start of the intervention (DayFromStart) as a predictor with correlated random intercept and random slope for the participants (PAlias), i.e.,
Model 2 (
) only included random intercept for each participant without considering the effect of time, i.e.,
By comparing the two models via , a significant effect of time (treatment) on the TFI was found, (3) = 8.336, p=.040*.
The estimated parameters from the model with time indicate an intercept of 38.06 for the fixed effect of time and a slope of -0.065, this means a reduction of 0.065 TFI units per day. Using these estimates, we can use the following formula to estimate the TFI score at day 84 (end of week 12) of the treatment: .
Using this formula, the estimated TFI score at day 84 is 32.64. This reflects a decrease of 5.46 in the TFI score from the initial assessment. These findings indicate that the TFI scores varied significantly over time as the intervention progressed, showing a consistent decrease in tinnitus severity.
3.3.2. Neck Bournemouth Questionnaire (NBQ) over Time
As for the TFI, we conducted an analogous analysis for the NBQ (see
Figure 3b). Comparing the models
and
using the
function, we found a significant effect of time (treatment) on neck pain as measured by the NBQ,
(3) = 24.183,
p<.001. The model with time as a predictor provides a significantly better fit to the data compared to the model without time.
The estimated parameters from the model with time indicate an intercept of 24.91 for the fixed effect of time and a slope of -0.092, this means a reduction of 0.092 NBQ units per day. Using these estimates, we can use the following formula to estimate the NBQ score at day 84 (end of week 12) of the treatment: .
Based on this formula, the estimated NBQ score at day 84 is 17.18. This reflects a decrease of 7.70 points in the NBQ score and a reduction of 31.03% in neck pain severity compared to the initial assessment. These results indicate a significant improvement in neck pain as the intervention progressed.
3.3.3. Head Movements’ Modulations (HMM) of ST over Time
As for the TFI, we conducted an analogous analysis for the HMM Score (see
Figure 3c). Comparing the models
and
using the
function, we found a significant effect of time (treatment) on how strong head movements modulate the tinnitus as measured by the HMM,
(3) = 27.361,
p<.001. The model with time as a predictor provides a significantly better fit to the data compared to the model without time.
The estimated parameters from the model with time indicate an intercept of 20.93 for the fixed effect of time and a slope of -0.066, this means a reduction of 0.066 HMM units per day. Using these estimates, we can use the following formula to estimate the HMM score at day 84 (end of week 12) of the treatment: .
Based on this formula, the estimated HMM score at day 84 is 15.40. This reflects a decrease of 5.53 in the HMM score, indicating a reduction in how strongly head movements modulate the perception of tinnitus. These results suggest a significant improvement in this aspect of tinnitus modulation as the intervention progresses.
3.4. Linear Mixed Modeling of Pre and Post ATM Screening Data
Before and after each ATM lesson, participants filled out the ATM Screening questionnaire, which assessed participants’ well-being through the STAI-State score of the State-Trait Anxiety Inventory (STAI) and measured the perceived tinnitus intensity using a Tinnitus Visual Analogue Scale (TVAS). In the subsequent analysis, “PrePost” serves as a dichotomous factor indicating whether the variable was measured before (“Pre”) or after (“Post”) the lesson.
3.4.1. Effects of the ATM on the Well-Being (STAI)
From a visual examination of
Supplemental Material Figure S12, it is evident that there are substantial individual differences in the effects of the ATMs on participants’ well-being, as measured by the STAI score. To analyze the impact of the weekly ATM lessons on the STAI, we compared two models using ANOVA. The first model incorporated random intercept and random slope for participants (PAlias), random intercepts for each ATM, and a fixed effect of PrePost, as depicted by the formula
In contrast, the second model excluded the effects of PrePost, resulting in the formula
The ANOVA comparison of the two models revealed that the inclusion of the fixed effect of PrePost in the model significantly improved the fit to the data compared to the model without this fixed effect, (3) = 103.85, p < .001. We can report a significant reduction in the STAI score by on average 6.505 ± 1.140 points after the ATMs compared to before the ATMs, M = 43.7 ± 2.22, 37.2 ± 2.3, respectively. This indicates a significant decrease in state anxiety following the ATM lessons.
3.4.2. Mean STAI over Time
To test for a general reduction in state anxiety over the time-course of the treatment, we calculated the mean STAI score per session and participant and conducted a second LMM analysis analogous to the TFI analysis described above. This analysis aimed to examine the overall trend in STAI scores over time. However, the results of this analysis did not show a significant effect,
(3) = 3.137,
p > .3, indicating that there was no general improvement in mean STAI over time (cf.
Supplemental Material Section 3.5, for details).
3.4.3. Effects of the ATM on Perceived Tinnitus Intensity (TVAS)
From a visual examination of
Supplemental Material Figure S18, it is evident that there are substantial individual differences in the effects of the ATMs on participants’ perceived tinnitus intensity, as measured by the TVAS. To analyse these effects, we conducted an analogous analysis to the STAI. The first model incorporated random intercept and random slope for participants (PAlias), random intercepts for each ATM, and a fixed effect of PrePost, as depicted by the formula
As the random effect structure of this model was too complex, resulting in a singular fit, we reduced the complexity of this model to
and compared it to the model without the effect of PrePost, i.e.,
Comparing the latter two models revealed a significant difference,
(1) = 3.902,
p = .048, between the models, referring to a reduction of 2.24 ± 1.13 points on the TVAS after the ATMs compared to before the ATMs (
Ms = 45.0 ± 4.63 and 42.9 ± 4.97). The outputs of this analysis are summarized in
Supplemental Material Section 3.5.
3.4.4. Mean TVAS over Time
It is important to highlight that due to the absence of standardized length for the TVAS and the lack of consistent device usage by participants across sessions, we chose not to interpret the analysis of TVAS variations over time. For comprehensive coverage, this analysis is presented in
Supplemental Material Section 3.7. However, the analysis did not reveal a significant effect,
(3) = 3.774,
p > .2, indicating the absence of a general change in perceived tinnitus intensity as measured with the unstandardized analogue scale.
3.5. Do Changes Relate to Each Other?
Despite the small sample size, we observed substantial individual differences among participants in their reduction of tinnitus perception and neck pain. As we were interested in exploring the interrelation of changes in dependent variables, we carried out two-tailed Spearman correlations for the difference measures described below. However, due to the limited data set, which leads to reduced statistical power and a heightened susceptibility to outliers, we have chosen to graphically represent the reported correlations and approach the findings with a cautious perspective. It is further important to note that we will summarize here the most relevant correlations related to TQ, TFI, and NBQ, while a complete display of all correlation results can be found in the
Supplemental Material Section 4.
3.5.1. Calculation of Difference Scores
To capture the magnitude of changes for each dependent variable X, we calculated difference measures between the End- and the Initial Screening for the TQ, HMM, MAIA, and WHO scores as . Analogously, we calculated difference measures between the last available and the first available weekly TFI, NBQ, and HMM screening. Finally, separately per participant and ATM, we calculated the mean STAI and the mean TVAS across the pre- and post-ATM-Screening and then calculated the difference measure of the last and the first available mean score.
3.5.2. Correlations of Difference Scores
Please note that, in addition to the Spearman correlations, we also performed Pearson correlations for both raw data and outlier-corrected data (see
Supplemental Material Section 4 for more information). As shown in
Supplemental Material Figures S25 and S26, the results reveal an almost identical pattern for all three analyses with only minor differences. Given the limited number of data points in these analyses, undue emphasis should not be placed on the exact values of the correlation coefficients. Please be aware that we are reporting only the results from the Spearman correlations on the raw data here.
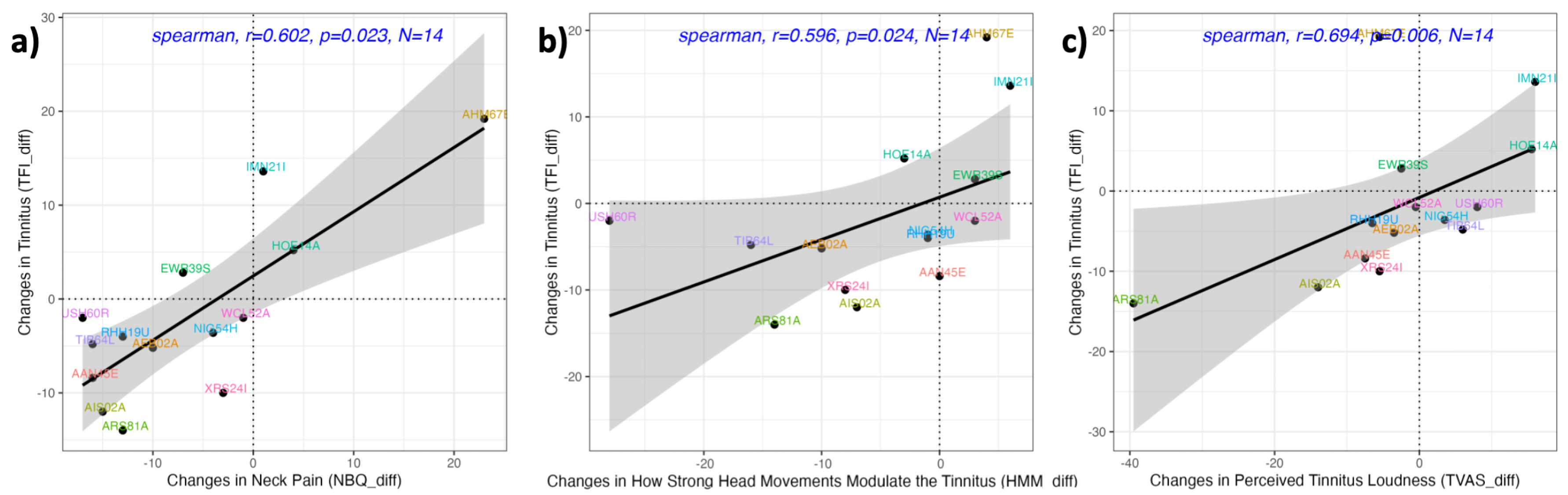
We found no significant correlation between the difference measures of TFI and TQ, suggesting that these two measures capture different aspects of tinnitus perception (
r = .380,
p = .223). However, there was a significant correlation between the difference measures of TFI and NBQ (
r = .602,
p = .023,
Figure 4a), indicating that participants who experienced a greater reduction in neck pain also experienced a greater reduction in tinnitus severity. Additionally, the change in TFI was correlated with changes in both HMM (
r = .596,
p = .024,
Figure 4b) and TVAS (
r = .694,
p = .006,
Figure 4c), suggesting that participants who had a larger decrease/increase in tinnitus severity also experienced a more pronounced decrease/increase in how strongly head movements modulate their tinnitus and in their subjective assessment of perceived tinnitus intensity.
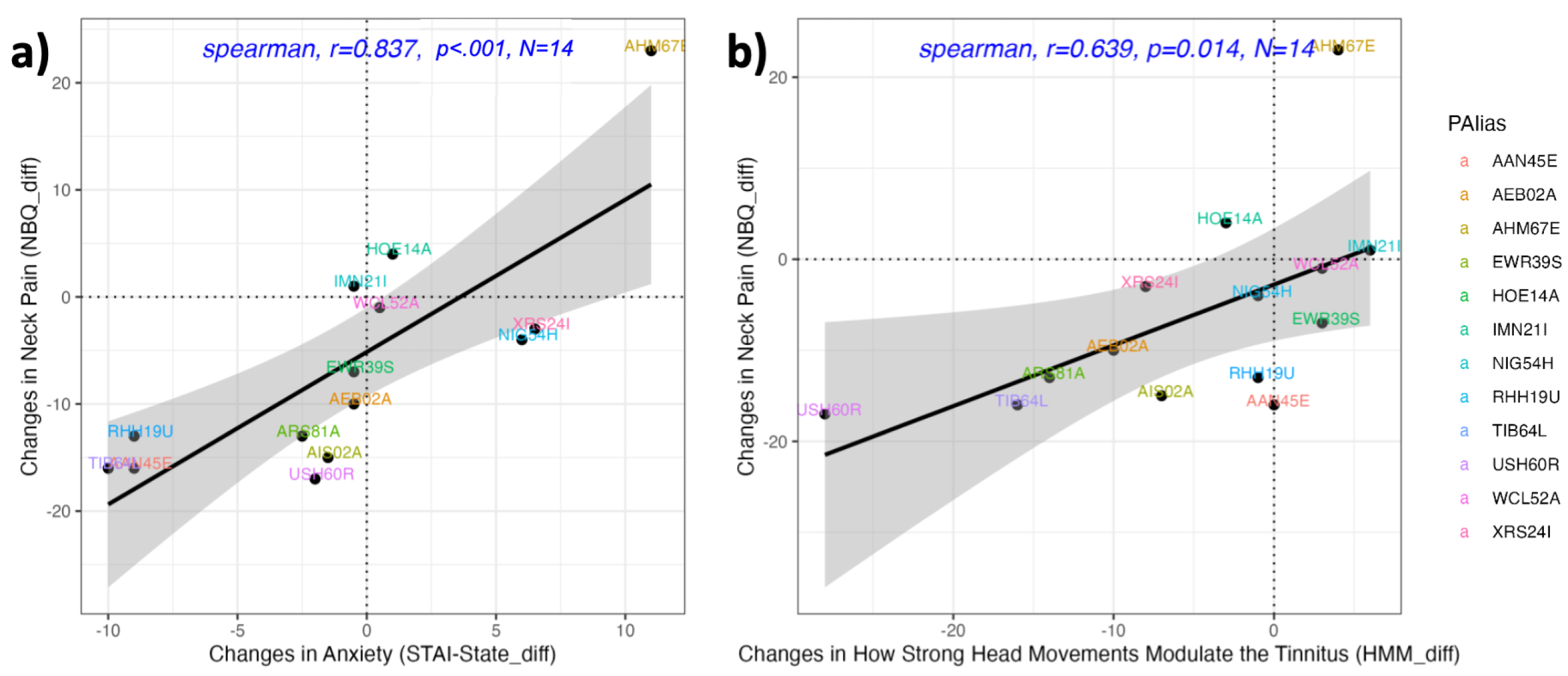
The NBQ difference measure was also correlated with both the HMM and the STAI difference measures (
rs >= .639,
ps <= .014;
Figure 5a and b). These correlations suggest that participants who experienced a greater reduction in neck pain also showed a greater reduction in how strongly head movements modulate their tinnitus and, importantly, in their state anxiety levels. This suggests that as neck pain decreased, participants reported lower levels of tension, anxiety, and nervousness.
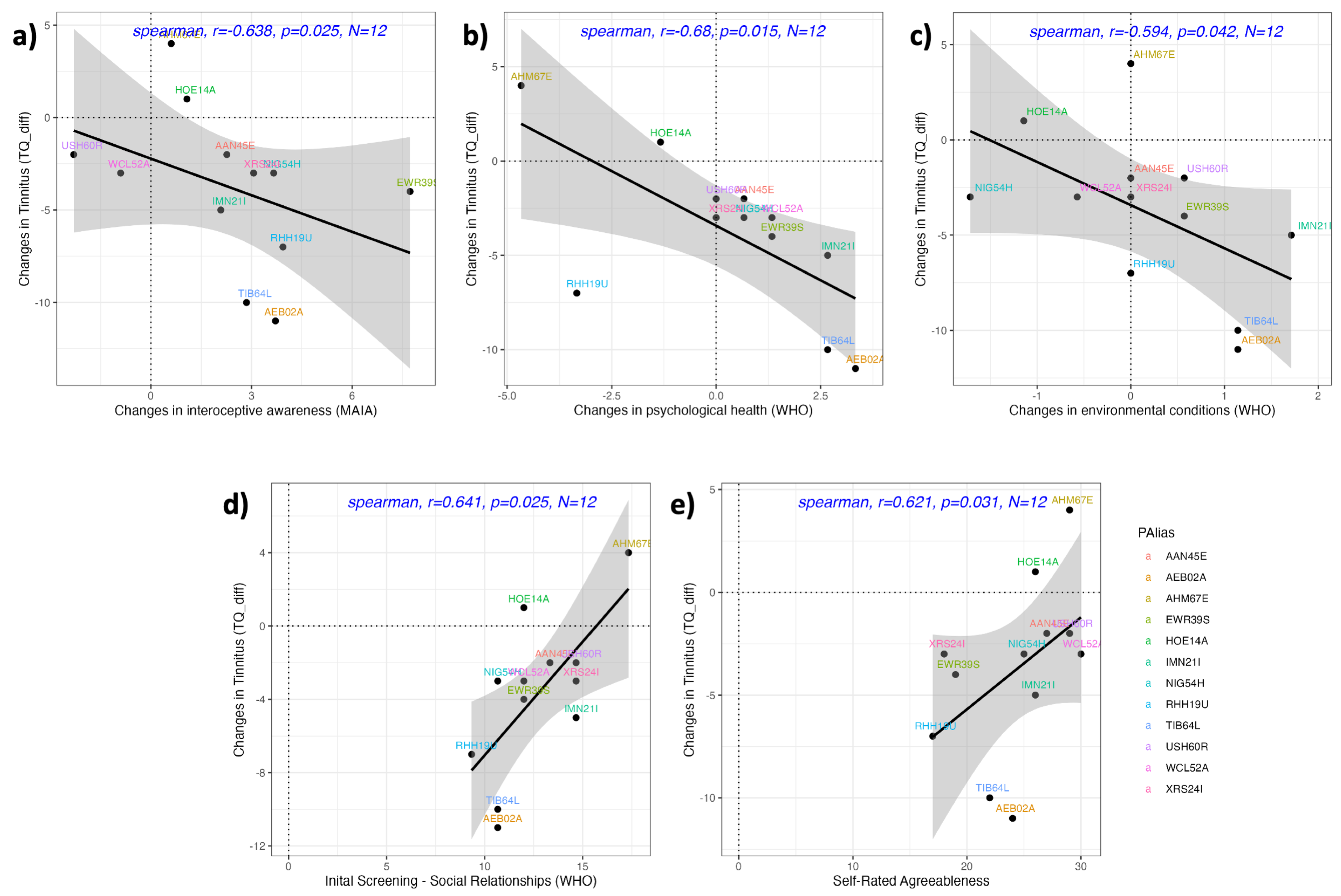
In addition, the TQ difference measure showed negative correlations with the difference measures for MAIA, and the WHO sub score for psychological health, and environmental factors (
rs <= -.594,
ps <= .042,
N = 12,
Figure 6a–c). These correlations suggest that a reduction in tinnitus distress may be associated with an increase in interoceptive awareness, better psychological health, and improved environmental conditions. Further a trend with for a positive correlation between the TQ difference measure and the STAI difference measure (
r = .500,
p = .098,
N = 12), suggest, that patients who experience a more profound reduction in tension, anxiety, and nervousness experiences greater tinnitus distress reduction.
3.5.3. Correlations of Difference Scores with Initial Screening Data
We found positive correlations only between the TQ difference measure and the
Initial Screening measures for participants’ self rated agreeableness, and the WHO subscore for social relationships (
rs >= .621,
ps <= .031,
Ns = 12,
Figure 6d,e). These correlations suggest that participants who were initially less satisfied with their social relationships and comprised lower levels of self-rated agreeableness showed greater reductions in their TQ scores.
4. Discussion
4.1. General Treatment Effects
This pilot study aimed to assess the effectiveness of online Feldenkrais Awareness Through Movement (ATM) group lessons in individuals with somatosensory tinnitus (ST) and neck discomfort. Notably, effects consistent with our hypotheses were observed in all primary dependent variables, including the Tinnitus Questionnaire TQ;[
26,
47] measuring tinnitus distress, the Tinnitus Functional Index TFI;[
27,
49] measuring tinnitus severity, and the Neck Bournemouth Questionnaire NBQ;[
43,
44] measuring neck pain. Moreover, small but significant improvements with substantial effect sizes were found for quality of life and physical health as measured with the short form of the WHO health questionnaire [
52], and interoceptive awareness, as measured with the Multidimensional Assessment of Interoceptive Awareness questionnaire MAIA;[
40], aligning with earlier reports on the effectiveness of Feldenkrais [
29,
30].
In our study, the most significant symptom improvement was observed in the reduction of neck pain. Despite the relatively small sample size consisting of 17 participants, not all of whom presented severe symptoms, the improvement rate surpassed 30%, which is nearly twice the clinically relevant threshold of 17% as defined by Bolton et al. [
44].
Regarding tinnitus perception, the significant reduction by on average 5.46 points of the TFI score remained below the clinically noteworthy threshold of 13 points, as established by Meikle et al. [
27]. Nevertheless, it is imperative to note that despite our limited sample size, our effects surpassed the improvement reported by Van der Wal et al. [
25] for their cohort undergoing delayed treatment in a randomized controlled trial focused on nine weeks of orofacial treatment in ST. Their documented improvement rates were 13.8 and 5.0 for their early and delayed treatment groups, each consisting of 40 patients. Notably, both groups initially exhibited more severe tinnitus symptoms as assessed by the TFI. Specifically, while our TFI averaged 43, their mean TFI scores were 55 and 48 for the early and delayed treatment groups, respectively. This compels us to acknowledge that achieving a mean improvement of 13 points on the TFI would have presented a challenge given our relatively small patient cohort, which included several patients with initial TFI scores below 13.
The average decrease of 3.75 points in the TQ score fell short of a suggested clinically meaningful threshold of 5 points [
64] but see [
48], for a threshold of 8.72. This apparent discrepancy might stem from the floor effect, which arises due to the baseline TQ Score of 36.5 within our patient cohort. This baseline score indicates compensated tinnitus, characterized by either either negligible or minimal tinnitus distress, with no apparent recommended treatment based on the guideline’s criteria [
6]. Note further that, Van der Wal’s early treatment group exhibited a similar reduction of 4.1 points, whereas their late treatment group (whose TFI reduction was lower than ours) did not demonstrate any significant alteration in the TQ [
25]. It is noteworthy that both of Van der Wal’s initial mean TQ scores
Ms = 37 and 34, [
25] were comparable to ours (
M = 36.5).
Therefore, it is worth highlighting that a more significant improvement in both TQ and other measured factors could have been achievable if our analysis had encompassed a larger cohort of patients with more pronounced tinnitus symptoms. Additionally, it’s crucial to recognize that a majority of our patients had already undergone a one-week outpatient tinnitus therapy at the TC UHJ. Consequently, any potential effects could be markedly more pronounced in a cohort that had not undergone prior treatment. As such, the potential rates of improvement for the TQ scores and other assessed factors might have been substantially greater under such conditions.
Despite the limited existing research on Feldenkrais intervention, our findings align with previous reports indicating positive outcomes of Feldenkrais intervention in individuals with persistent low back pain [
34,
35,
36] and stroke [
39]. Further enhanced quality of life has been reported for patients with Parkinson’s disease [
37,
38] and stroke [
39].
4.2. Direct Effect of ATMs on Well-Being and Perceived Tinnitus Intensity
The well-being of the participants was measured with the State-Trait Anxiety Inventory STAI[
50,
51] directly before and after each ATM lesson. Importantly, comparing post- and pre ATM measurements, there was a significant and substantial decrease of on average 6.5 points on the STAI scale, indicating that the patients experienced lower levels of tension, anxiety, and nervousness directly after the ATM compared to before the ATM. As summarized in the
Supplemental Material Section 2, the patients’ feedback and subjective ratings confirmed this effect. This finding is in line with the general stress-reducing effect of Feldenkrais ATM lessons STAI[
50,
51].
Moreover, the assessed intensity of tinnitus, quantified using a Tinnitus Visual Analogue Scale (TVAS), revealed a minor yet statistically significant decrease averaging 2.24 points on a 100-point scale following the ATM, in contrast to its pre-ATM levels. This observation is particularly noteworthy, given our initial uncertainty regarding the immediate impact of the ATM on perceived tinnitus intensity. During the feedback session, certain participants noted that the ATM (or the serene state of focusing on themselves or the calm and quiet situation) resulted in heightened perceived tinnitus intensity, while others reported a decrease. Here, it would be of particular interest to explore whether it is possible to identify which subgroup of patients experiences a reduction in tinnitus loudness and which does not.
Additionally, it is important to consider that the changes in tinnitus intensity observed in pre- and post-ATM measurements are understandable, given that our participants used the same display device within a single session. However, it’s essential to acknowledge that we cannot make conclusions regarding the lack of significance in changes in the Tinnitus Visual Analogue Scale (TVAS) throughout the treatment period. This limitation stems from our inability to rule out the possibility that participants utilized different devices over the entire 12-week treatment duration, introducing an uncontrolled variable due to the non-standardized TVAS utilization.
However, note that a study investigating cervical spine manipulations [
21], also revealed no significant changes in pre- and post-treatment TVAS measures, while reporting a decrease in a second measure on tinnitus symptomatic, specifically the Tinnitus Handicap Inventory. The authors suggested that not all measures are equally suitable for capturing changes in tinnitus symptoms.
4.3. Individual Differences and Correlations Between Measures
For all measures, we observed substantial individual differences and notable variances in rates of improvement. While, it is crucial to interpret the results of the correlational analysis, bearing in mind that the limited sample size introduces instability in the estimates of correlation coefficients, reduces the statistical power, and consequently constrains the extent of generalizability, we can emphasize that we conducted correlations for raw and outlier-corrected data and observed nearly identical patterns of results, with only minor discrepancies in the magnitudes of correlation coefficients and p-values.
As anticipated, a robust correlation emerged between the amelioration of tinnitus severity (measured by the TFI) and reductions in neck pain, and the impact of head movements on tinnitus. Additionally, a decrease in the TQ could be associated with increased subjective interoceptive awareness, physical health, and the influence of environmental factors on overall health and well-being.
Our analysis did not reveal a significant correlation between the difference measures of both TQ and TFI, and several factors could account for this lack of correlation. Firstly, while both measures are intended to assess distinct facets of tinnitus perception — specifically, tinnitus distress as evaluated by the TQ and tinnitus severity as measured by the TFI — the latter is potentially more sensitive to subtle variations in impairment due to tinnitus than the former. These notions have already been highlighted by other researchers [
25,
65]. Furthermore, the inclusion of patients with milder symptoms, as previously mentioned, might partly obscure the ability to discern more pronounced improvement rates.
At the initial screening, we observed positive associations between higher tinnitus, in terms of severity (TFI) and distress (TQ), and greater neck complaints, indicating a link between tinnitus and neck problems, which is consistent with the presence of ST. The significant reduction in the degree of Head Movement Modulatio (HMM) over the course of the treatment supports the notion that improvement in neck problems can lead to a reduction in tinnitus and the impact of head movements on tinnitus perception, as reported in previous studies [
19]. This confirms that addressing and alleviating neck issues may contribute to the overall improvement in tinnitus symptoms [
19]. However, while the
Initial and the
End Screening of the HMM were not significantly different, we can report significant positive correlations between the improvement rates of both the TFI and the NBQ with the HMM.
4.4. Limitations
As it is the case with all feasibility studies, the current investigation has limitations that need recognition. Firstly, and most importantly, the study’s small sample size and lack of a control group limit generalizability and raise Type II error risk. The research inquiry was originally designed as a preliminary study intended to involve a more extensive participant cohort. However, due to limitations in both time and financial resources, and likely attributed to the reduced frequency of patient visits to the TC JUH as a result of the COVID-19 pandemic, it proved impractical to enroll a greater number of willing participants within the specified period of time. Secondly, variations in tinnitus severity and duration, long-term effects of prior treatments, and other causes within the sample may have influenced outcomes. Thirdly, the lack of blinding in this study further introduces the potential risk for bias, as it has been reported for other studies on ST [
19], for a review. Both the participants and the researchers were aware of the intervention being administered, which could have influenced their perceptions and reporting of outcomes. A control group would be desirable here that undergoes another treatment (e.g., mindfulness training) in order to rule out that the effects are merely due to the effect of a quiet hour in a stressful everyday life or the focus on oneself or things other than the tinnitus.
Lastly, and similar to other studies on ST e.g.,[
24], it is challenging to differentiate between the treatment effect of the Feldenkrais intervention and the potential effects of the feedback sessions themselves. Notably, the observation that individuals who initially reported lower levels of satisfaction in social relationships and self-assessed agreeableness exhibited more pronounced effects could potentially indicate a beneficial influence stemming from the feedback group session.
Though insightful, the study’s limitations caution against overinterpretation. Addressing these issues in future research will enhance validity. Nonetheless, the alignment of the dependent measures with hypotheses and significant results within our small group holds promise for further investigating the effectiveness of ATM on somatosensory tinnitus.
4.5. Conclusions
In conclusion, our study explored the effectiveness of online Feldenkrais group lessons for somatosensory tinnitus in a small and heterogeneous sample of patients, accounting for substantial individual differences. The results revealed significant effects across all dependent variables, suggesting the potential of this intervention in managing tinnitus symptoms. However, the findings highlight the importance of individualized medicine in addressing the unique needs of tinnitus patients cf.[
66]. Further research is crucial to deepen our understanding of the specific mechanisms and refine the application of Feldenkrais for the treatment of somatosensory tinnitus. While telemedicine is widely promoted and offers convenience, it is reasonable to assume that more substantial therapeutic effects may be achieved in a personal setting, emphasizing the value of physical interaction and tailored guidance in optimizing treatment outcomes for individuals with somatosensory tinnitus.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org
Author Contributions
Conceptualization, V.G.S; Data curation, V.G.S and E.B.; Formal analysis, V.G.S, E.B. and H.O.; Investigation, V.G.S, E.B., S.H. and M.S.; Methodology, V.G.S, E.B., S.H., M.S. and C.D.; Project administration, V.G.S; Resources, V.G.S, E.B., O.G.L and C.D.; Software, V.G.S and E.B.; Supervision, V.G.S and C.D.; Validation, V.G.S; Visualization, V.G.S; Writing – original draft, V.G.S; Writing – review and editing, V.G.S, E.B., E.B., H.O., S.H., M.S., O.G.L. and C.D..
Funding
This research was funded by the “Förderverein für Feldenkrais und somatisches Lernen e.V.”, Effnerstraße 90, D-81925 München.
Institutional Review Board Statement
The study was carried out in accordance with the Declaration of Helsinki and the American Psychological Association ethical standards and was approved by the Ethics Committee of Jena University Hospital (Reference 2021-2378-BO)
Informed Consent Statement
Participants provided their written informed consent to participate in this study and all principles outlined in the Declaration of Helsinki were met.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Acknowledgments
We would like to thank all participants, the employees of the Tinnitus Center of the University Hospital Jena, as well as Clara Breier for the help with the telephone patient acquisition and proof reading.
Conflicts of Interest
The authors declare no conflict of interest about this paper.
Abbreviations
The following abbreviations are used in this manuscript:
| ATM |
Awareness Through Movement |
| AQ |
Autistic Traits |
| BFI |
Big-Five Inventory |
| HMM |
Head Movement Modulation (of ST) |
| LMM |
Linear Mixed Modeling |
| MAIA |
Multidimensional Assessment of Interoception Awareness |
| MTU |
Manual Therapy Utrecht |
| MTU |
Neck Bournemouth Questionnaire |
| ST |
Somatosensory Tinnitus |
| STAI |
State-Trait-Anxiety-Inventory |
| TC JUH |
Tinnitus Centre of the Jena University Hospital |
| TFI |
Tinnitus Functional Index |
| TQ |
Tinnitus Questionnaire |
| TS |
Tinnitus Sensitization |
| TVAS |
Tinnitus Visual Analogue Scale |
| WHO |
World Health Organisation |
References
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. The Lancet 2013, 382, 1600–1607. [CrossRef]
- Jastreboff, P.J.; Hazell, J.W. A neurophysiological approach to tinnitus: Clinical implications. British Journal of Audiology 1993, 27, 7–17. [CrossRef]
- Bürgers, R.; Behr, M.; Gosau, M., Treatment strategies of temporomandibular joint and masticatory muscle disorders in patients with tinnitus. In Textbook of Tinnitus; Møller, A.; Langguth, B.; De Ridder, D.; Kleinjung, T., Eds.; Springer, 2011; pp. 763–767.
- Oostendorp, R.A.B.; Bakker, I.; Elvers, H.; Mikolajewska, E.; Michiels, S.; De Hertogh, W.; Samwel, H. Cervicogenic somatosensory tinnitus: An indication for manual therapy plus education? Part 2: A pilot study. Manual Therapy 2016, 23, 106–113. [CrossRef]
- Zenner, H. A systematic classification of tinnitus generator mechanisms. The international tinnitus journal 1998, 4, 109–113.
- Cima, R.; Mazurek, B.; Haider, H.; Kikidis, D.; Lapira, A.; Noreña, A.; Hoare, D. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. HNO 2019, 67, 10–42. [CrossRef]
- Mazurek, B.; Hesse, G.; Sattel, H.; Kratzsch, V.; Lahmann, C.; Dobel, C. S3 Guideline: Chronic Tinnitus : German Society for Otorhinolaryngology, Head and Neck Surgery e.V. (DGHNO-KHC). HNO 2022, 70, 795–827. [CrossRef]
- McCormack, A.; Edmondson-Jones, M.; Somerset, S.; Hall, D. A systematic review of the reporting of tinnitus prevalence and severity. Hearing Research 2016, 337, 70–79. [CrossRef]
- Lenarz, T.; Arnold, W.; Biesinger, E.; Brinkmann, U.; Edlinger, H.; Ehrenberger, K.; Goebel, G.; Greimel, K.V.; Knör, H.; Mackinger, H.; et al. Leitlinie Tinnitus der Deutschen Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- und Hals-Chirurgie. Laryngo-Rhino-Otologie 1998, 77, 531–535. [CrossRef]
- Ivansic, D.; Besteher, B.; Gantner, J.; Guntinas-Lichius, O.; Pantev, C.; Nenadic, I.; Dobel, C. Psychometric assessment of mental health in tinnitus patients, depressive and healthy controls. Psychiatry Research 2019, 281. [CrossRef]
- Lewis, J. Tinnitus and suicide. Journal of the American Academy of Audiology 2002, 13, 339. [CrossRef]
- Beukes, E.W.; Baguley, D.M.; Jacquemin, L.; Lourenco, M.P.; Allen, P.M.; Onozuka, J.; Stockdale, D.; Kaldo, V.; Andersson, G.; Manchaiah, V. Changes in tinnitus experiences during the COVID-19 pandemic. Frontiers in Public Health 2020, 8, 592878. [CrossRef]
- Tziridis, K.; Friedrich, J.; Brüeggemann, P.; Mazurek, B.; Schulze, H. Estimation of tinnitus-related socioeconomic costs in Germany. International Journal of Environmental Research and Public Health 2022, 19, 10455. [CrossRef]
- Michiels, S.; Cardon, E.; Gilles, A.; Goedhart, H.; Vesala, M.; Schlee, W. Somatosensory tinnitus diagnosis: Diagnostic value of existing criteria. Ear and Hearing 2022, 43, 143–149. [CrossRef]
- Haider, H.F.; Hoare, D.J.; Costa, R.F.P.; Potgieter, I.; Kikidis, D.; Lapira, A.; Nikitas, C.; Caria, H.; Cunha, N.T.; Paço, J.C. Pathophysiology, diagnosis and treatment of somatosensory tinnitus: A scoping review. Frontiers in Neuroscience 2017, 11. [CrossRef]
- Biesinger, E.; Reisshauer, A.; Mazurek, B. [The role of the cervical spine and the craniomandibular system in the pathogenesis of tinnitus. Somatosensory tinnitus]. HNO 2008, 56, 673–7. [CrossRef]
- Reisshauer, A.; Mathiske-Schmidt, K.; Kuchler, I.; Umland, G.; Klapp, B.F.; Mazurek, B. [Functional disturbances of the cervical spine in tinnitus]. HNO 2006, 54, 125–31. [CrossRef]
- AWMF. Leitlinie Hörsturz, Leitlinien der Deutschen Gesellschaft für Hals-Nasen-Ohren-Heilkunde. Kopf-und Halschirurgie 2014, pp. 1–10.
- Michiels, S.; Naessens, S.; Van de Heyning, P.; Braem, M.; Visscher, C.M.; Gilles, A.; De Hertogh, W. The effect of physical therapy treatment in patients with subjective tinnitus: A systematic review. Frontiers in Neuroscience 2016, 10. [CrossRef]
- Mielczarek, M.; Konopka, W.; Olszewski, J. The application of direct current electrical stimulation of the ear and cervical spine kinesitherapy in tinnitus treatment. Auris Nasus Larynx 2013, 40, 61–65. [CrossRef]
- Bonaconsa, A.; Mazzoli, M.; Magnano San Lio, A.; Milanesi, C.; Babighian, G. Posturography measures and efficacy of different physical treatments in somatic tinnitus. International Tinnitus Journal 2010, 16, 44–50.
- Latifpour, D.H.; Grenner, J.; Sjodahl, C. The effect of a new treatment based on somatosensory stimulation in a group of patients with somatically related tinnitus. International Tinnitus Journal 2009, 15, 94–99.
- Rocha, C.B.; Sanchez, T.G. Efficacy of myofascial trigger point deactivation for tinnitus control. Brazilian Journal of Otorhinolaryngology 2012, 78, 21–26. [CrossRef]
- Oostendorp, R.A.B.; Bakker, I.; Elvers, H.; Mikolajewska, E.; Michiels, S.; De Hertogh, W.; Samwel, H. Cervicogenic somatosensory tinnitus: An indication for manual therapy? Part 1: Theoretical concept. Manual Therapy 2016, 23, 120–123. [CrossRef]
- van der Wal, A.; Michiels, S.; Van de Heyning, P.; Braem, M.; Visscher, C.M.; Topsakal, V.; Gilles, A.; Jacquemin, L.; Van Rompaey, V.; De Hertogh, W. Treatment of somatosensory tinnitus: A randomized controlled trial studying the effect of orofacial treatment as part of a multidisciplinary program. Journal of Clinical Medicine 2020, 9, 705. [CrossRef]
- Hallam, R.S. Manual of the Tinnitus Questionnaire (TQ); The Psychological Corporation: London, 1996.
- Meikle, M.B.; Henry, J.A.; Griest, S.E.; Stewart, B.J.; Abrams, H.B.; McArdle, R.; Myers, P.J.; Newman, C.W.; Sandridge, S.; Turk, D.C.; et al. The Tinnitus Functional Index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear and Hearing 2012, 33, 153–176. [CrossRef]
- Hüttenrauch, E.; Jensen, M.; Ivanšić, D.; Dobel, C.; Weise, C. Improving the assessment of functional impairment in tinnitus sufferers: Validation of the German version of the Tinnitus Functional Index using a confirmatory factor analysis. International Journal of Audiology 2022, 61, 140–147. [CrossRef]
- Berland, R.; Marques-Sule, E.; Marín-Mateo, J.L.; Moreno-Segura, N.; López-Ridaura, A.; Sentandreu-Mañó, T. Effects of the Feldenkrais method as a physiotherapy tool: A systematic review and meta-analysis of randomized controlled trials. International Journal of Environmental Research and Public Health 2022, 19, 13734. [CrossRef]
- Hillier, S.; Worley, A. The effectiveness of the Feldenkrais method: A systematic review of the evidence. Evidence-Based Complementary and Alternative Medicine 2015, 2015. [CrossRef]
- Ullmann, G.; Williams, H.G.; Hussey, J.; Durstine, J.L.; McClenaghan, B.A. Effects of Feldenkrais exercises on balance, mobility, balance confidence, and gait performance in community-dwelling adults age 65 and older. The Journal of Alternative and Complementary Medicine 2010, 16, 97–105. [CrossRef]
- Nambi, G.; Trivedi, P.; Momin, S.; Patel, S.; Pancholi, D. Comparative effect of Pilates and Feldenkrais intervention on functional balance and quality of life in ambulatory geriatric population: A randomized controlled study. International Journal of Health Sciences and Research 2014, 4, 71–77.
- Vrantsidis, F.; Hill, K.D.; Moore, K.; Webb, R.; Hunt, S.; Dowson, L. Getting Grounded Gracefully©: Effectiveness and acceptability of Feldenkrais in improving balance. Journal of Aging and Physical Activity 2009, 17, 57–76. [CrossRef]
- Mohan, V.; Paungmali, A.; Sitilertpisan, P.; Henry, L.J.; Mohamad, N.B.; Kharami, N.N.B. Feldenkrais method on neck and low back pain to the type of exercises and outcome measurement tools: A systematic review. Polish Annals of Medicine 2017, 24, 77–83. [CrossRef]
- Ahmadi, H.; Adib, H.; Selk-Ghaffari, M.; Shafizad, M.; Moradi, S.; Madani, Z.; Partovi, G.; Mahmoodi, A. Comparison of the effects of the Feldenkrais method versus core stability exercise in the management of chronic low back pain: A randomised control trial. Clinical Rehabilitation 2020, 34, 1449–1457. [CrossRef]
- Paolucci, T.; Zangrando, F.; Iosa, M.; De Angelis, S.; Marzoli, C.; Piccinini, G.; Saraceni, V.M. Improved interoceptive awareness in chronic low back pain: A comparison of Back school versus Feldenkrais method. Disability and Rehabilitation 2017, 39, 994–1001. [CrossRef]
- Teixeira-Machado, L.; Araújo, F.M.; Cunha, F.A.; Menezes, M.; Menezes, T.; DeSantana, J.M. Feldenkrais method-based exercise improves quality of life in individuals with Parkinson’s disease: A controlled, randomized clinical trial. Alternative Therapies in Health and Medicine 2015, 21, 8–14.
- Teixeira-Machado, L.; de Araújo, F.M.; Menezes, M.A.; Cunha, F.A.; Menezes, T.; Ferreira, C.d.S.; DeSantana, J.M. Feldenkrais method and functionality in Parkinson’s disease: A randomized controlled clinical trial. International Journal on Disability and Human Development 2017, 16, 59–66. [CrossRef]
- Serrada, I.; Fryer, C.; Hordacre, B.; Hillier, S. Can body awareness training improve recovery following stroke: A study to assess feasibility and preliminary efficacy. Clinical Rehabilitation 2022, 36, 650–659. [CrossRef]
- Mehling, W.E.; Price, C.; Daubenmier, J.J.; Acree, M.; Bartmess, E.; Stewart, A. The Multidimensional Assessment of Interoceptive Awareness (MAIA). PLoS ONE 2012, 7, e48230. [CrossRef]
- Cohen, J. Statistical power analysis for the behavioral sciences; Routledge, 2013.
- Hemmerich, W. StatistikGuru: Cohen’s d berechnen, 2015.
- Soklic, M.; Peterson, C.; Humphreys, B.K. Translation and validation of the German version of the Bournemouth Questionnaire for neck pain. Chiropractic & Manual Therapies 2012, 20. [CrossRef]
- Bolton, J.E.; Humphreys, B.K. The Bournemouth Questionnaire: A short-form comprehensive outcome measure. II. Psychometric properties in neck pain patients. Journal of Manipulative and Physiological Therapeutics 2002, 25, 141–148. [CrossRef]
- Michiels, S.; De Hertogh, W.; Truijen, S.; Van de Heyning, P. Physical therapy treatment in patients suffering from cervicogenic somatic tinnitus: Study protocol for a randomized controlled trial. Trials 2014, 15. [CrossRef]
- Rehbock-Walter, C.; Steinmetz, B. Spannungen lösen – Stress bewältigen mit der Felenkrais Methode: Kursleitermanual, Kurskonzeption nach §20 SGB V; Feldenkrais-Verband Deutschland e.V., 2007.
- Goebel, G.; Hiller, W. Tinnitus-Fragebogen (TF): Ein Instrument zur Erfassung von Belastung und Schweregrad bei Tinnitus. Handanweisung; Hogrefe, Verlag für Psychologie, 1998.
- Zeman, F.; Koller, M.; Schecklmann, M.; Langguth, B.; Landgrebe, M. Tinnitus assessment by means of standardized self-report questionnaires: psychometric properties of the Tinnitus Questionnaire (TQ), the Tinnitus Handicap Inventory (THI), and their short versions in an international and multi-lingual sample. Health and Quality of Life Outcomes 2012, 10. [CrossRef]
- Brüggemann, P.; Szczepek, A.J.; Kleinjung, T.; Ojo, M.; Mazurek, B. Validierung der deutschen Version des Tinnitus Functional Index (TFI). Laryngo-Rhino-Otologie 2017, 96, 615–619. [CrossRef]
- Laux, L.; Glanzmann, P.; Schaffner, P.; Spielberger, C.D. Das State-Trait-Angstinventar (STAI); Beltz Test: Weinheim, 1981.
- Spielberger, C.; Gorusch, R.; Lushene, R. Manual for the State-Trait Anxiety lnventory.; Consulting Psychologists Press: Palo Alto, 1970.
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial - A report from the WHOQOL group. Quality of Life Research 2004, 13, 299–310. [CrossRef]
- Zoom Video Communication, I. Zoom, 2022.
- LimeSurvey GmbH. LimeSurvey: An open source survey tool. LimeSurvey GmbH, Hamburg, Germany, 2012.
- Stoet, G. PsyToolkit: A software package for programming psychological experiments using Linux. Behavior Research Methods 2010, 42, 1096–1104. [CrossRef]
- Stoet, G. PsyToolkit: A novel web-based method for running online questionnaires and reaction-time experiments. Teaching of Psychology 2017, 44, 24–31. [CrossRef]
- Baron-Cohen, S.; Wheelwright, S.; Skinner, R.; Martin, J.; Clubley, E. The autism-spectrum quotient (AQ): Evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders 2001, 31, 5–17. [CrossRef]
- Freitag, C.M.; Retz-Junginger, P.; Retz, W.; Seitz, C.; Palmason, H.; Meyer, J.; Rösler, M.; von Gontard, A. Evaluation der deutschen Version des Autismus-Spektrum-Quotienten (AQ) - die Kurzversion AQ-k. Zeitschrift für klinische Psychologie und Psychotherapie 2007, 36, 280–289. [CrossRef]
- Rammstedt, B.; Danner, D.; Soto, C.J.; John, O.P. Validation of the short and extra-short forms of the Big Five Inventory-2 (BFI-2) and their German adaptations. European Journal of Psychological Assessment 2020, 36, 149–161. [CrossRef]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2018. Version 4.2.2 (2022-10-31).
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. Journal of Statistical Software 2015, 67, 1–48. [CrossRef]
- R Core Team. stats: The R Stats Package, 2023. R package version 4.2.2.
- Cumming, G.; Calin-Jageman, R., The paired design. In Introduction to the new statistics: Estimation, open science, and beyond; Routledge, 2017; chapter 8, pp. 195–221.
- Adamchic, I.; Tass, P.A.; Langguth, B.; Hauptmann, C.; Koller, M.; Schecklmann, M.; Zeman, F.; Landgrebe, M. Linking the Tinnitus Questionnaire and the subjective Clinical Global Impression: Which differences are clinically important? Health and Quality of Life Outcomes 2012, 10. [CrossRef]
- Jacquemin, L.; Mertens, G.; Van de Heyning, P.; Vanderveken, O.M.; Topsakal, V.; De Hertogh, W.; Michiels, S.; Van Rompaey, V.; Gilles, A. Sensitivity to change and convergent validity of the Tinnitus Functional Index (TFI) and the Tinnitus Questionnaire (TQ): Clinical and research perspectives. Hearing Research 2019, 382. [CrossRef]
- Mazurek, B.; Rose, M.; Schulze, H.; Dobel, C. Systems Medicine Approach for Tinnitus with Comorbid Disorders. Nutrients 2022, 14. [CrossRef]
Figure 1.
Overview of data collection time-points and screening questionnaires. Repeatedly administered at various time points (T0, T1, T2, T3), within 24 hours (h) before the next Awareness Through Movement (ATM) lesson (Weekly screening), and directly before and after ATM lesson were the following questionnaires: Tinnitus-Functional-Index (TFI), Neck Bournemouth Questionnaire (NBQ), assessment of how head movements modulate tinnitus (HMM), Tinnitus Questionnaire (TQ), Multidimensional Assessment of Interoceptive Awareness (MAIA), short WHO-health questionnaire (WHO), State-Trait-Anxiety-Inventory (STAI), and Tinnitus Visual Analogue Scale (TVAS). Further details on the questionnaires can be found in the Materials section of the main manuscript.
Figure 1.
Overview of data collection time-points and screening questionnaires. Repeatedly administered at various time points (T0, T1, T2, T3), within 24 hours (h) before the next Awareness Through Movement (ATM) lesson (Weekly screening), and directly before and after ATM lesson were the following questionnaires: Tinnitus-Functional-Index (TFI), Neck Bournemouth Questionnaire (NBQ), assessment of how head movements modulate tinnitus (HMM), Tinnitus Questionnaire (TQ), Multidimensional Assessment of Interoceptive Awareness (MAIA), short WHO-health questionnaire (WHO), State-Trait-Anxiety-Inventory (STAI), and Tinnitus Visual Analogue Scale (TVAS). Further details on the questionnaires can be found in the Materials section of the main manuscript.
Figure 2.
Pre-post treatment comparisons of TQ, MAIA, and WHO Physical Health. Comparison of pre- and post-treatment scores gathered at the Initial Screening (t1) and the End Screening (t2) reveals significant changes in: a) in tinnitus distress, as measured by the Tinnitus Questionnaire (TQ), b) interoceptive awareness (MAIA), and c) scores on the World Health Organization (WHO) questionnaire indicating changes in physical health and overall quality of life (not displayed, refer to text).
Figure 2.
Pre-post treatment comparisons of TQ, MAIA, and WHO Physical Health. Comparison of pre- and post-treatment scores gathered at the Initial Screening (t1) and the End Screening (t2) reveals significant changes in: a) in tinnitus distress, as measured by the Tinnitus Questionnaire (TQ), b) interoceptive awareness (MAIA), and c) scores on the World Health Organization (WHO) questionnaire indicating changes in physical health and overall quality of life (not displayed, refer to text).
Figure 3.
Decrease of weekly measured TFI, NBQ, and HMM over time. Linear Fits (M and 95%-CI represented by black line and grey area, respectively) of the weekly captured measures for a total of N = 17 participants (PAlias), with individual data points coded by color and shape. Participants exhibit varying intercepts and slopes. Utilizing linear mixed modeling, our analysis revealed a significant decrease in the following measures over time: a) Tinnitus Functional Index (TFI), assessing perceived tinnitus strength over the last week. b) Neck Bournemouth Questionnaire (NBQ), evaluating experienced neck pain over the last week. c) Head Movement Modulation (HMM) score, indicating the impact of head movements on tinnitus modulation over the last week.
Figure 3.
Decrease of weekly measured TFI, NBQ, and HMM over time. Linear Fits (M and 95%-CI represented by black line and grey area, respectively) of the weekly captured measures for a total of N = 17 participants (PAlias), with individual data points coded by color and shape. Participants exhibit varying intercepts and slopes. Utilizing linear mixed modeling, our analysis revealed a significant decrease in the following measures over time: a) Tinnitus Functional Index (TFI), assessing perceived tinnitus strength over the last week. b) Neck Bournemouth Questionnaire (NBQ), evaluating experienced neck pain over the last week. c) Head Movement Modulation (HMM) score, indicating the impact of head movements on tinnitus modulation over the last week.
Figure 4.
Correlations between difference scores related to tinnitus strength (TFI). The black line represents the linear fit, while the grey area represents the 95% CI. A greater reduction in tinnitus severity (more negative ) correlates with a greater reductions in a) neck pain () b) how strongly head movements (HMM) modulate the ST (), and c) Tinnitus Visual Analogue Scale ().
Figure 4.
Correlations between difference scores related to tinnitus strength (TFI). The black line represents the linear fit, while the grey area represents the 95% CI. A greater reduction in tinnitus severity (more negative ) correlates with a greater reductions in a) neck pain () b) how strongly head movements (HMM) modulate the ST (), and c) Tinnitus Visual Analogue Scale ().
Figure 5.
Correlations between difference scores related to neck pain (NBQ). The black line represents the linear fit, while the grey area represents the 95% CI. A greater reduction in neck pain (more negative ) correlates with a greater reduction in a) state anxiety () and b) how strongly head movements modulate the tinnitus ().
Figure 5.
Correlations between difference scores related to neck pain (NBQ). The black line represents the linear fit, while the grey area represents the 95% CI. A greater reduction in neck pain (more negative ) correlates with a greater reduction in a) state anxiety () and b) how strongly head movements modulate the tinnitus ().
Figure 6.
Correlations between difference scores related to tinnitus distress (TQ). The black line represents the linear fit, while the grey area represents the 95% CI. A greater reduction in tinnitus distress (more negative ) can be associated with an increase in a) interoceptive awareness (), b) psychological health, and improvement of c) environmental conditions. A greater reduction of tinnitus can further be reported for individuals with d) lower social relationships, and e) lower agreeableness as measured in the Initial Screening.
Figure 6.
Correlations between difference scores related to tinnitus distress (TQ). The black line represents the linear fit, while the grey area represents the 95% CI. A greater reduction in tinnitus distress (more negative ) can be associated with an increase in a) interoceptive awareness (), b) psychological health, and improvement of c) environmental conditions. A greater reduction of tinnitus can further be reported for individuals with d) lower social relationships, and e) lower agreeableness as measured in the Initial Screening.
Table 1.
Participant demographics, initial and end screening data and information on missing data
Table 1.
Participant demographics, initial and end screening data and information on missing data
| |
|
|
|
|
Initial Screening |
|
|
|
|
|
|
Missing Data (ATMs) |
| |
|
|
|
|
Part 1 |
|
Part 2 |
|
End Screening |
|
ATM
Screening
|
|
Weekly
Screening
|
| PAlias |
Sex |
Age |
Group |
|
TFI |
NBQ |
HMM |
|
TQ |
HMM |
MAIA |
WHO |
|
TQ |
HMM |
MAIA |
WHO |
|
STAI, TVAS |
|
TFI, NBQ, HMM |
| AAN45E |
f |
32 |
Wed |
|
83.6 |
60 |
0 |
|
60 |
0 |
10.4 |
8 |
|
58 |
0 |
12.7 |
8 |
|
6-8, 11 |
|
5-7, 10, 12 |
| AEB02A |
f |
25 |
Mon |
|
60.0 |
49 |
39 |
|
40 |
21 |
20.1 |
12 |
|
29 |
28 |
23.9 |
20 |
|
- |
|
- |
| AHM67E |
f |
52 |
Mon |
|
32.8 |
33 |
20 |
|
30 |
20 |
11.1 |
16 |
|
34 |
28 |
11.7 |
16 |
|
7 |
|
- |
| AIM33A* |
f |
53 |
Mon |
|
89.2 |
16 |
0 |
|
72 |
26 |
16.2 |
8 |
|
- |
- |
- |
- |
|
8-12 |
|
7-12 |
| AIS02A |
f |
31 |
Wed |
|
11.2 |
20 |
8 |
|
21 |
14 |
17.4 |
16 |
|
- |
- |
- |
- |
|
4, 6 |
|
5, 12 |
| ARS81A |
f |
52 |
Mon |
|
83.2 |
53 |
60 |
|
55 |
44 |
9.6 |
12 |
|
- |
- |
- |
- |
|
6, 9, 10 |
|
4, 5, 9 |
| EIR79H** |
f |
57 |
Wed |
|
60.0 |
27 |
31 |
|
52 |
44 |
16.7 |
16 |
|
46 |
44 |
22.7 |
16 |
|
- |
|
- |
| EWR39S |
f |
57 |
Wed |
|
29.2 |
17 |
37 |
|
37 |
13 |
12.5 |
12 |
|
33 |
5 |
20.2 |
12 |
|
4 |
|
- |
| HOE14A |
m |
58 |
Mon |
|
26.4 |
17 |
20 |
|
26 |
23 |
25.6 |
12 |
|
27 |
9 |
26.7 |
16 |
|
- |
|
- |
| IMN21I |
f |
56 |
Wed |
|
70.0 |
31 |
18 |
|
51 |
1 |
19.3 |
12 |
|
46 |
6 |
21.3 |
12 |
|
2, 9 |
|
1, 8 |
| ISE22I* |
m |
63 |
Wed |
|
39.6 |
27 |
21 |
|
27 |
30 |
22.6 |
16 |
|
- |
- |
- |
- |
|
5-12 |
|
6, 8-12 |
| NIG54H |
f |
61 |
Mon |
|
6.4 |
6 |
0 |
|
9 |
2 |
20.2 |
12 |
|
6 |
0 |
23.8 |
16 |
|
- |
|
7, 10 |
| RHH19U |
m |
51 |
Wed |
|
- |
- |
- |
|
49 |
25 |
17.4 |
8 |
|
42 |
30 |
21.3 |
8 |
|
- |
|
- |
| TIB64L |
m |
44 |
Wed |
|
30.0 |
23 |
14 |
|
30 |
32 |
16.2 |
8 |
|
20 |
18 |
19.1 |
12 |
|
- |
|
- |
| USH60R |
m |
48 |
Mon |
|
35.6 |
27 |
55 |
|
30 |
51 |
21.8 |
16 |
|
28 |
24 |
19.5 |
16 |
|
9 |
|
8 |
| WCL52A |
m |
56 |
Mon |
|
25.2 |
9 |
0 |
|
14 |
0 |
27.0 |
12 |
|
11 |
6 |
26.1 |
16 |
|
8 |
|
7 |
| XRS24I |
m |
51 |
Mon |
|
17.2 |
8 |
17 |
|
17 |
10 |
21.2 |
16 |
|
14 |
4 |
24.2 |
16 |
|
9 |
|
7, 8, 10 |
| M |
|
49.8 |
|
|
43.7 |
26.4 |
21.3 |
|
36.5 |
20.9 |
18.0 |
12.5 |
|
30.3 |
15.5 |
21.0 |
14.2 |
|
|
|
|
| SD |
|
10.9 |
|
|
26.9 |
15.9 |
18.9 |
|
17.6 |
16.0 |
5.1 |
3.1 |
|
15.2 |
14.0 |
4.6 |
3.5 |
|
|
|
|
| N |
|
17 |
|
|
16 |
16 |
16 |
|
17 |
17 |
17 |
17 |
|
13 |
13 |
13.0 |
13 |
|
|
|
|
| *quit after the 7th ATM, **Tinnitus Reha after the 5th ATM |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).