1. Introduction
The introduction of computer-aided designing/computer-aided manufacturing (CAD-CAM) technology allowed high-strength ceramic materials to be clinically used, such as alumina and zirconia [
1]. High-strength ceramics tend to have more opacity which imposes a challenge upon color matching; nevertheless, they can obscure existing tooth discolorations. Zirconia is a white crystalline oxide of the metal ’zirconium’ and is available in three distinct allotropic forms; monoclinic, tetragonal, and cubic [
2,
3]. It has been meta-stabilized in its tetragonal form at room temperature by the addition of stabilizing oxides [
4]. Stabilized tetragonal zirconia polycrystalline (3Y-TZP) is used in dental restorations and usually contains yttria (3 mol%) as a stabilizer.
To achieve a tooth-like appearance, 3Y-TZP copings for dental restorations still need the application of veneering ceramics [
5,
6]. Even though the esthetics can be partially restored by these layers, the total layers lack the fluorescence that natural teeth have [
7]. Another drawback of veneered zirconia restorations is that the veneering porcelain of a Y-TZP core becomes the weak link of the restoration and has a high incidence of chipping, which is considered the most frequently reported type of failure [
8,
9]. The failure rate observed is between 3% and 50% for both tooth or implant-supported zirconia restorations as reported in different studies [
3,
10,
11,
12].
Several techniques try to reduce these drawbacks, including modifying core design [
13], minimal veneering porcelain layer to zirconia core ratio [
14], veneering porcelain materials with a lower coefficient of thermal expansion (CTE) than zirconia cores [
15], and changing layering technique using the press-on [
16,
17] and CAD-on technique [
18].
Still, these various layering methods have not fully solved the problem, so there was a suggestion to extend the core material itself to occupy the full thickness of the restoration, which is called full-contour or monolithic. Monolithic zirconia restorations provide acceptable esthetics, overcome the chipping of porcelain veneering layers [
9,
19,
20], and help clinicians make less destructive tooth preparations [
21]. The better translucency and opalescence of the new monolithic zirconia systems were achieved by modifications in the microstructure which aim to reduce alumina content, grain size, and the number of impurities [
22].
More recent versions of translucent zirconia have increased the content of yttria around 4 to 5 mol%, resulting in structures with more cubic polycrystals (approximately 50%) and light transmission, allowing them to produce highly translucent monolithic zirconia. This was attributed to the cubic phase change resulting in an increase in the volume and the isotropic cube shape [
23,
24,
25,
26].
Translucent zirconia materials have been marketed for all types of anterior and posterior dental restorations. There is a lack of studies that investigate the full range of properties of these new types of zirconia as addressed recently from a study on optical properties of CAD-CAM ceramic systems for monolithic restorations[
27]. A PUBMED search for related articles using the captions (monolithic, translucent, zirconia, mechanical) revealed 66 results; most of these publications are between 2018 and 2021 and are peer-reviewed. This search revealed the increased interest in the study of mechanical properties of these recent dental ceramics, marketed as ’esthetic’. However, not all marketed materials have been backed up by independent scientific published reports, nor did many of the published reports use the ISO standards for sample production. This will ensure that the esthetic drive for their production is guaranteed along with sufficient mechanical properties which might affect their strength and durability
in vivo or limit their recommended clinical use. Consequently, it is paramount to assess the
in vitro mechanical properties of these materials to be able to predict the clinical performance, limitations, and indications of such esthetic restorative materials away from the effects of the
in vivo confounding variables.
So, this
in vitro study aimed to evaluate and compare the mechanical properties of a variety of CAD-CAM esthetic polycrystalline ceramic systems used for monolithic restorations with a CAD-CAM glass-ceramic system. Their optical properties have been compared in a predecessor study [
27].
The null hypothesis is that there are no differences in the mechanical properties between three CAD-CAM monolithic polycrystalline ceramics nor when compared with a CAD-CAM monolithic glass-ceramic.
2. Materials and Methods
Four brands of monolithic esthetic CAD-CAM ceramic materials were used (A2-shaded). Three brands were polychromatic super-high translucent multi-layered zirconia discs: Ceramill
® Zolid FX Multilayer (ZF) (Amann Girrbach AG, Austria), IPS e.max
® ZirCAD MT Multi (ZM) (Ivoclar Vivadent, Schaan, Zurich), and KATANA
TM STML (KS) (Kuraray Noritake, Japan). The fourth brand was lithium disilicate glass-ceramic IPS e.max
® CAD LT (MC) (Ivoclar Vivadent, Schaan, Zurich). The tested materials are summarized in
Table 1. Samples were derived for each brand material from the same lot number as specified by the manufacturing company and were designed according to ISO no. 6872 testing procedures.
As adopted in the sample size determination of the predecessor study [
27], "power analysis" using G*Power statistical software (G*Power Ver. 3.0.10, Franz Faul, Universität Kiel, Germany) was performed to determine the sample size of this study. The number of samples per group was set according to power: 0.75, α: 0.23, and effect size: 0.38. Accordingly, a total of 80 samples was set for all the materials to be tested.
Each material comprised 10 samples for the flexural strength and elastic modulus tests and 10 for the hardness test. Samples were milled from the materials blocks and discs while in their green stage, according to the required dimensions using a computer-aided manufacturing (CAM) device (K5+, vhf camfacture AG, Ammerbuch, Germany), taking into account the amount of shrinkage that occurs during dense sintering. A polishing device (echo LAB POLI-1X/250, Devco S.r.l, Italy) was used to polish the samples (60 seconds at 300 rpm; 600, 800, and 1000 grit silicon carbide (SiC) papers). According to the manufacturers’ recommendations, water was only used for polishing the samples of lithium disilicate. A digital caliper (Insize 1111-75A, Brazil) was used to verify the final dimensions (±0.01mm) of the samples.
The samples were fully crystallized/sintered based on the following manufacturers’ specifications: for the ZF group, (Furnace: Ceramill Therm, Amann Girrbach, Austria) heating rate of 8°C/min till 1450°C, holding time of 120min, and cooling rate of 10°C/min; for the ZM group, (Furnace: inFire HTC speed, Dentsply Sirona, USA) heating rate of 10°C/min till 900°C, holding time of 30min, then 3°C/min till 1500°C, holding time of 120min, and cooling rate of -10°C/min to 900°C and then -8°C/min to 300°C; for the KS group, (Furnace: Ceramill Therm, Amann Girrbach, Austria) heating rate of 10°C/min till 1550°C, holding time of 120min, and cooling rate of -10°C/min; and for the MC group, (Furnace: Programat P5010 Ivoclar Vivadent, Zurich) heating rate of 90°C/min till 820°C, holding time of 10min, then 30°C/min till 840°C, holding time of 7min, and cooling rate of 0°C/min.
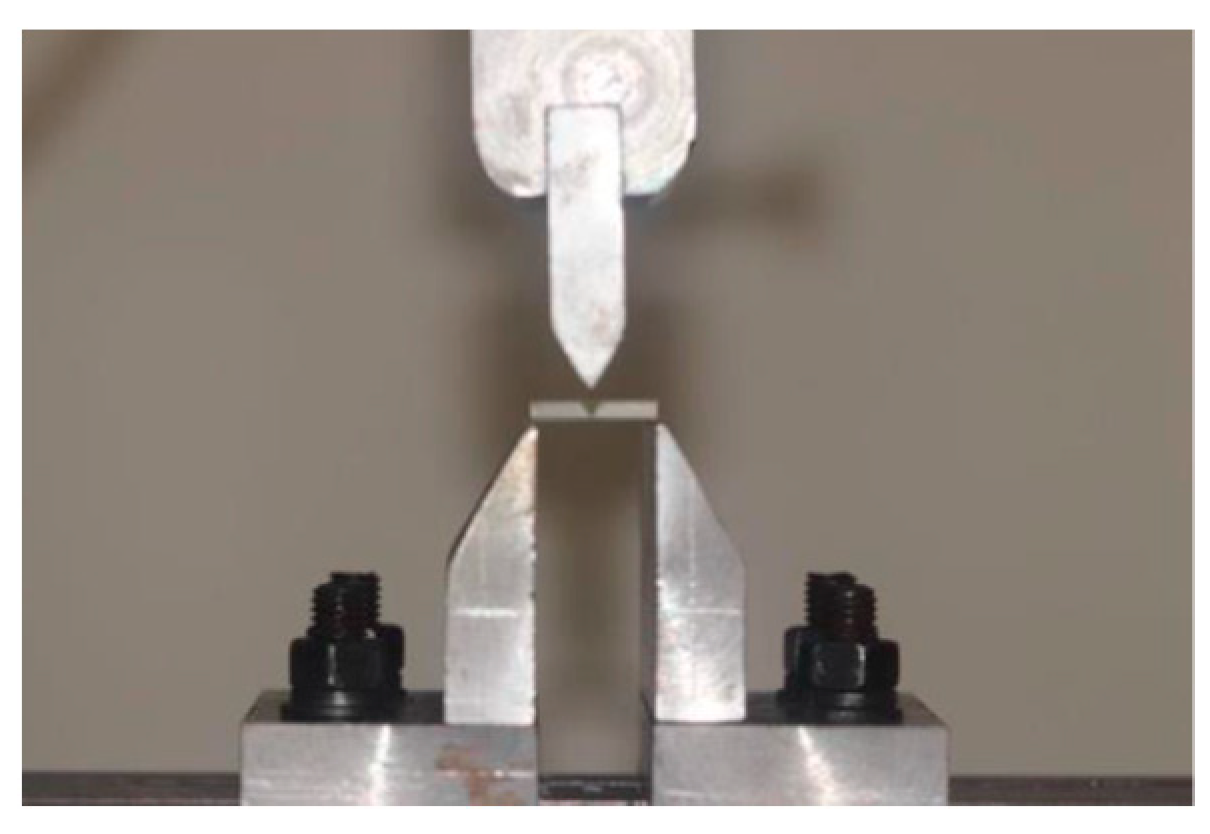
Flexural Strength and Elastic Modulus
Testing of flexural strength and elastic modulus was done according to the ISO standard 6872
28). Materials were milled into bars (N=40/n=10) to end into the following dimensions after firing 18×4×3mm, with a 45-degree chamfer edge [
28]. Distilled water was used at 37°C to store these bars for 24h, then the samples were subjected to load in a 3-PBT (16mm span) using a universal testing machine (Computer control electromechanical universal testing machine, Jinan corp., China) at a crosshead speed of 1.0mm/min (
Figure 1).
The flexural strength (σf) was determined in MPa from the following formula (Equation (1)) [
29]:
where P stands for the breaking load (newton), L for the roller span (16 mm), B for the sample width (millimeter), and D for the sample thickness (millimeter).
The elastic modulus (Em) was calculated in GPa from the following formula (Equation 2) using data obtained from 3-PBT [
29,
30]:
where d stands for the deflection corresponding to load P.
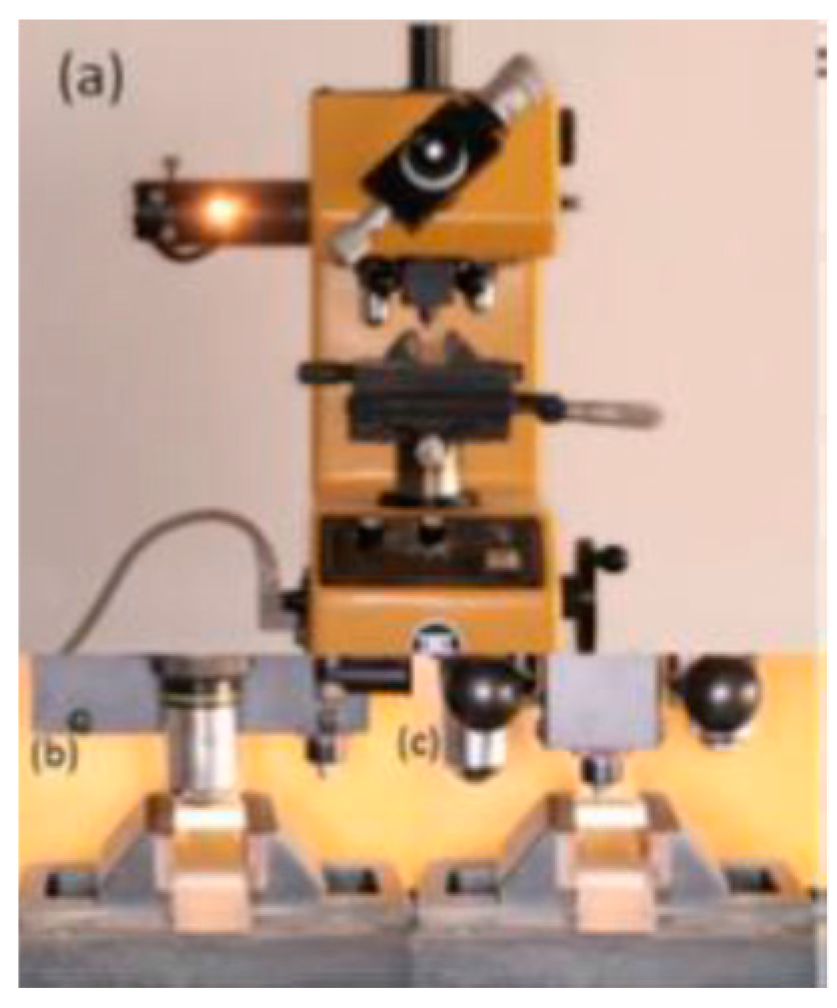
Vickers Microhardness
Cuboidal samples (N=40/n=10) of 18×14×5mm from each material were fabricated. After polishing and sintering as described previously, storage of all samples in distilled water was carried out at 37°C for 24h. After that, the samples were placed in a microhardness indenter (Microhardness tester, Matsuzawa Seiki CO. LTD, Japan). A Vickers diamond indenter with a load of 300g and a dwell time of 10sec was used according to the specifications of ASTM C1327 [
31] (
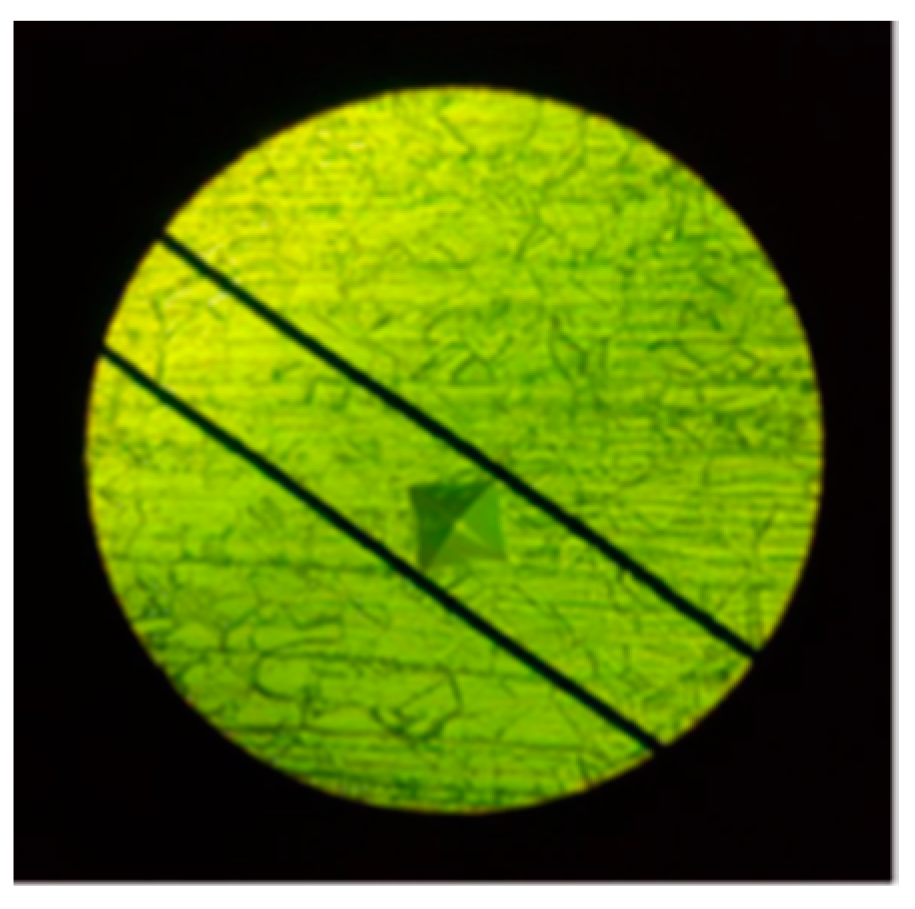
Figure 2). Five indentations were carried out for each sample around its center, at least 0.5mm apart. The diameters of the Vickers indentations (d1 and d2) were assessed using an optical microscope (
Figure 3), and the following formula (Equation 3) was used to calculate the hardness [
31]:
where L stands for the load (newton) and d1 and d2 are the indentation diagonal length (millimeter).
Means and standard deviations were calculated for each mechanical property (flexural strength, elastic modulus, and hardness) within each material group. Measured data were analyzed statistically by using statistical software (SPSS Statistics v.25.0; Chicago, USA). Normalities of distributions were explored using the Kolmogorov-smirnov test and the groups were found to be distributed normally. Flexural strength, elastic modulus, and Vickers microhardness data were analyzed using one-way ANOVA. To adjust for multiple comparisons, the Bonferroni correction test was used for elastic modulus and hardness whereas Games-Howell multiple comparison test was used for the flexural strength. Statistical significance was set at P<0.05.
3.Results
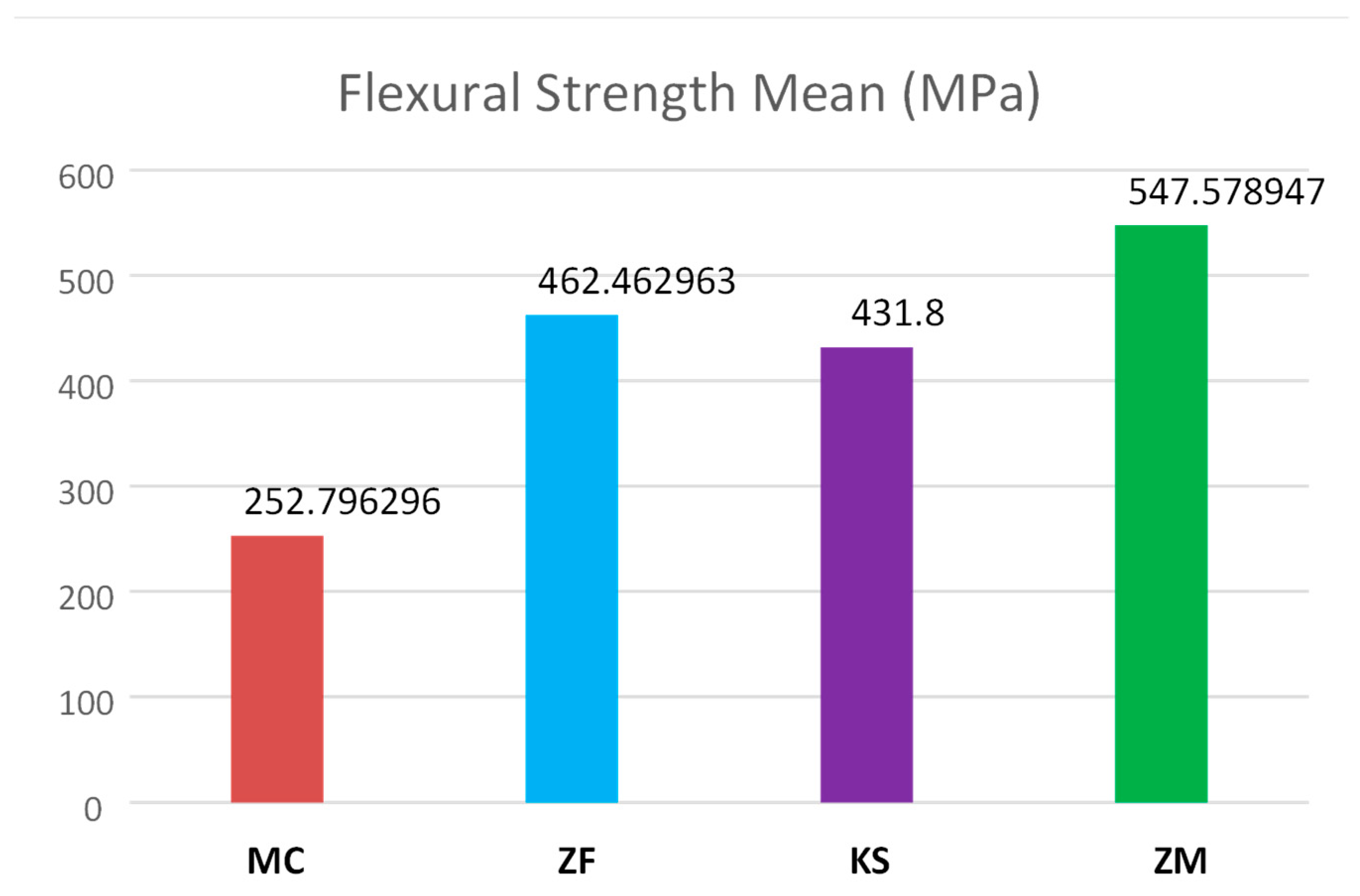
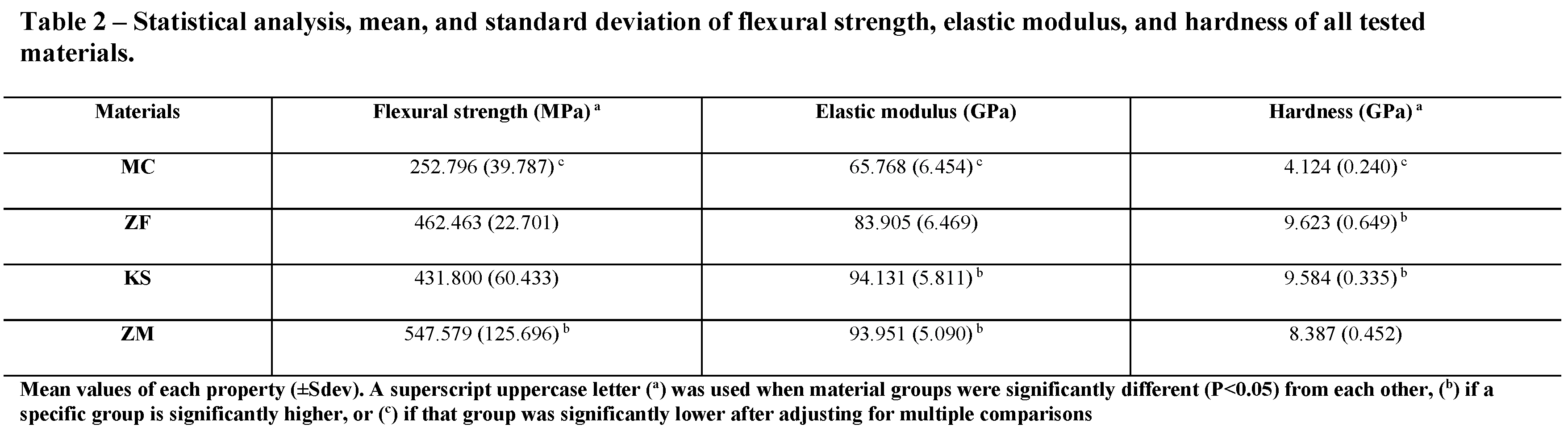
Flexural strength values ranged from 252.7 to 547.5MPa (
Table 2,
Figure 4). The analysis revealed a significant difference in flexural strength among the tested groups (P<0.05). When adjusting for multiple comparisons, the flexural strength of the ZM group [547.5(±125.6)MPa] was noted to be significantly higher (P<0.05) than the ZF [462.4(±22.7)MPa] and KS [431.8(±60.4)MPa] groups, which were also significantly higher (P<0.05) than the MC [252.7(±39.7)MPa] group. However, no significant flexural strength difference was noted between the ZF and KS (P=0.47) groups.
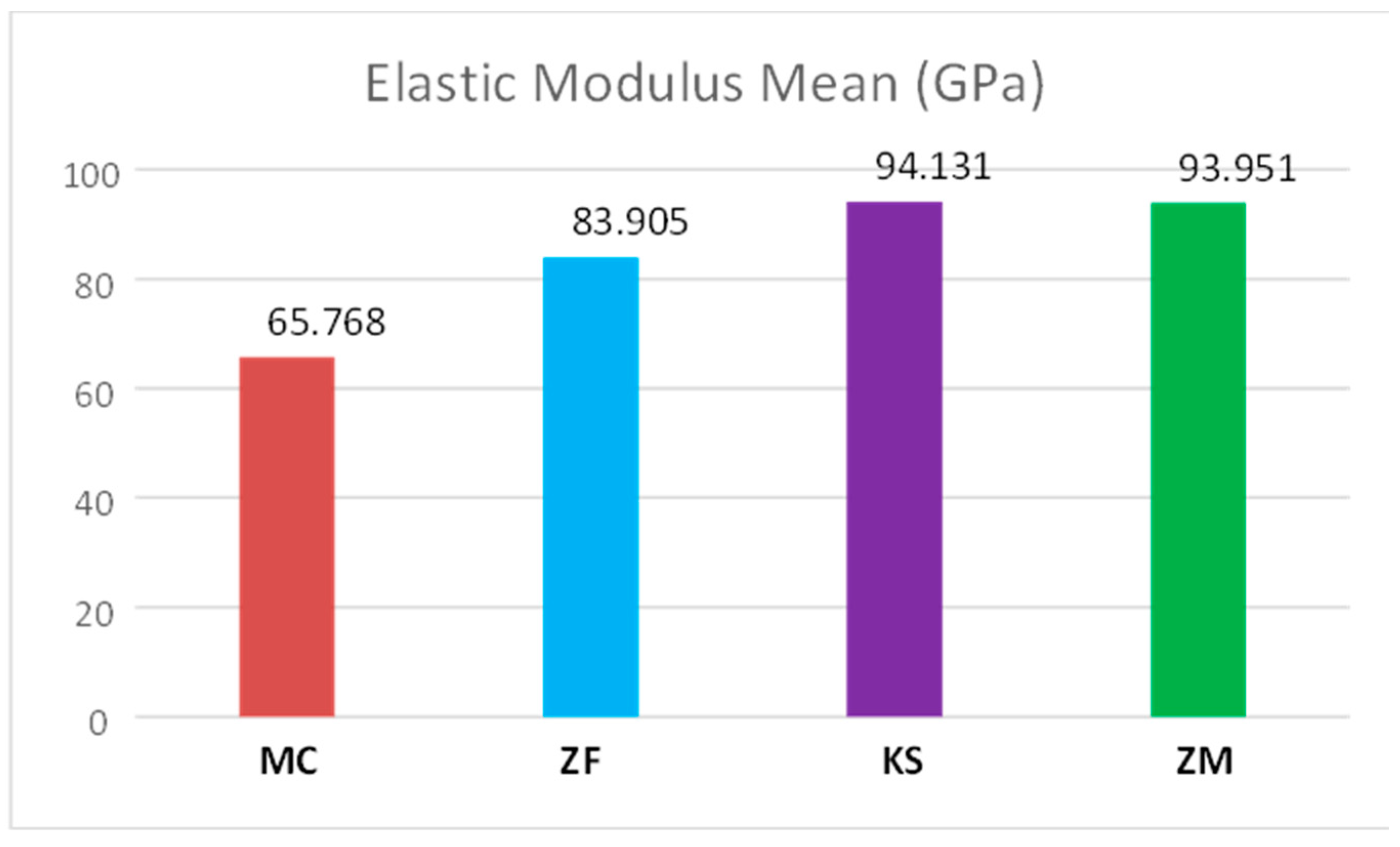
Elastic modulus values ranged from 65.7 to 94.1GPa (
Table 2,
Figure 5). KS [94.1(±5.8)GPa] and ZM [93.9(±5.08)GPa] groups showed significantly higher (P<0.05) elastic modulus than ZF [83.9(±6.4)GPa] group, which were also significantly higher (P<0.05) than the MC [65.7(±6.4)GPa] group. No significant difference was found between the KS and ZM (P=1.00) groups.
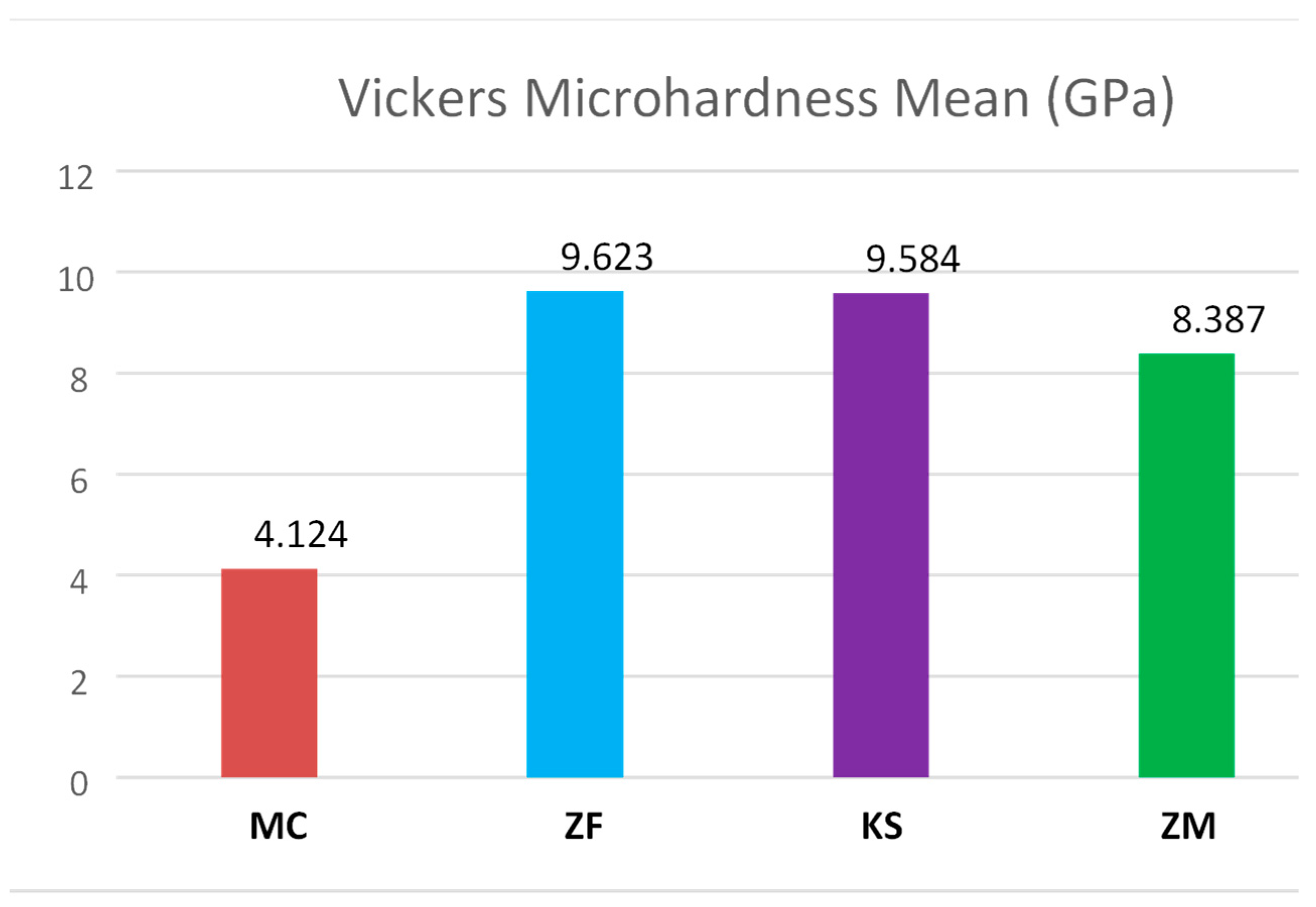
Vickers microhardness values ranged from 4.12 to 9.62GPa (
Table 2,
Figure 6). The analysis revealed that a significant difference in Vickers microhardness was noted among the groups (P<0.05). When adjusting for multiple comparisons, the Vickers microhardness of the ZF [9.62(±0.64)GPa] and KS [9.58(±0.33)GPa] groups were noted to be significantly higher (P<0.05) than the ZM [8.38(±22.7)GPa] group, which was also significantly higher (P<0.05) than the MC [4.12(±0.24)GPa] group. However, no significant Vickers microhardness difference was noted between the ZF and KS (P=1.00) groups. The MC group significantly had the lowest microhardness among all tested materials (P<0.05).
4. Discussion
The null hypothesis of this study was rejected, as the differences in the mechanical properties of the tested materials were statistically significant. This in vitro study evaluated and compared the mechanical properties of three commercially available CAD-CAM multi-layered zirconia ceramics, marketed as ’esthetic zirconia’, with lithium disilicate glass-ceramic as a control. so far, no previous study has compared these specific materials together in terms of their mechanical properties.
For this present study, flexural strength was examined because it is considered a proven test to compare the mechanical behavior of brittle materials; that are significantly stronger in compression than tension, such as ceramics [
32]. The test adopted in this study was 3-PBT; one of the recommended methods by ISO 6872;2015. The results of the study showed that the ZM group has a statistically significant higher flexural strength [547.5(± 125.6)MPa] among the tested materials, while the MC group has the lowest [252.7(± 39.7)MPa]. There is no significant difference between ZF [462.4(± 22.7)MPa] and KS [431.8(± 60.4)MP] groups.
Different zirconia systems do not necessarily behave in a similar pattern, and the microstructure seems to play an important role in the zirconia material behavior. Also, the mechanical properties for each material brand differ according to the optical properties; as the final shade variation is mainly based on microstructure; e.g., Ceramill® Zolid FX (Amann Girrbach AG, Austria) zirconia has two subtypes: Ceramill® Zolid FX white and Ceramill® Zolid FX multilayer; IPS e.max® ZirCAD (Ivoclar Vivadent, Schaan, Zurich) zirconia has five different subtypes: IPS e.max® ZirCAD Prime, IPS e.max® ZirCAD MT Multi, IPS e.max® ZirCAD MT, IPS e.max® ZirCAD LT, and IPS e.max® ZirCAD MO; KATANATM (Kuraray Noritake, Japan) zirconia has four different subtypes: KATANATM STML, KATANATM UTML, KATANATM HTML, and HT. The control group IPS e.max® CAD (Ivoclar Vivadent, Schaan, Zurich) glass-ceramic has five subtypes: IPS e.max® CAD HT, IPS e.max® CAD MT, IPS e.max® CAD LT, IPS e.max® CAD MO, and IPS e.max® CAD I. Each brand subtype has a slightly different microstructure and thus different mechanical properties and indications. This wide variation in the microstructure of each ceramic material brand might explain the variation in the results obtained from different studies.
In this investigation, the obtained flexural strength values were generally less than those claimed by the manufacturing companies, i.e., 850MPa for ZM, 700(±150)MPa for ZF, 748MPa for KS, and 360MPa for MC. However, the mean values obtained are within the threshold recommended by ISO for clinical indications. Few data are available in the literature regarding multi-layered zirconia ceramics to be directly compared with this study outcome.
For the MC group, the flexural strength values achieved in this study are similar to those stated by Zarone et al. [262(±88)MPa] in their narrative review [
33]. Goujat et al. in another
in vitro study reported a lower value [210.2(±14)MPa] which had been obtained from samples of a dissimilar size but of similar shape and method to this study
34). In contrast, various studies reported higher values [348.33(±28.69)MPa] and [381.04(±42.02)MPa] than those obtained in this study [
29,
35]. Data for ZF and KS are still limited. Zadeh et al. [
36] and Elsaka [
37] reported higher values than the present study [557(±88)MPa] and [676(±49.7)MPa], respectively. Paek et al. also reported flexural strength of KS [762.16(±200.96)MPa] higher than those reported in this study [
38]. No available data was found in the literature regarding the ZM flexural strength.
It appears infeasible to definitively state the ceramic material strength due to the various factors impacting measurements, such as the method of testing, sample shape and dimensions, environment of testing, polishing procedures, support, and load spans [
39]. For example, Leung et al. tested samples of size 15×2×2mm with supporting rollers span length at 10mm apart, which is different from the present study (sample size of 18×4×3mm with the supporting rollers span length at 16mm apart) [
40].
No statistically significant differences between zirconia groups were found in elastic modulus, except for the ZF group. The elastic moduli of all zirconia materials were higher than that of lithium disilicate material tested, which is also in agreement with recent laboratory studies [
24,
41]. ZM and KS groups have significantly higher elastic moduli than all tested materials and there is no statistically significant difference found between them, but the values were variable. These findings showed that the force required for zirconia deformation is greater than that of commonly used lithium disilicate glass-ceramics. Furthermore, other studies found that better machinability and adaptation are present with a lower elastic modulus [
42,
43,
44].
In this study, microhardness testing revealed that the MC group had lower values of hardness than those for zirconia materials. The hardness of ceramic materials contributes to their ease in finishability, polishability, and wear resistance [
45]. Also, it is important to measure the hardness of dental materials to be able to describe the abrasiveness to which the natural dentition will be subjected
46). Previous studies have reported that ceramics produced greater opposing tooth structure wear than other restorative materials [
47,
48,
49]. Also, it is generally confirmed that harder materials may cause more severe wear on the antagonist tooth structure [
50]. MC microhardness value is slightly higher than that of human enamel (3.5GPa) [
51,
52]. Advantageously, the lower hardness values of MC compared to the tested zirconia materials may protect the antagonist tooth structure from the wear process. On the other hand, more studies are needed to advocate; as material hardness is not the only factor in the complicated process of tooth wear. The results displayed here were lower than the data from other
in vitro studies. Goujat et al. reported a Vickers microhardness value of 5.98(±0.94)GPa for MC, on the other hand, Elsaka et al. reported 11.36(±0.61)GPa for ZF [
34,
37]. Furthermore, data provided by manufacturers and previous studies for other zirconia materials were available as a dimensionless Vickers hardness number, a unit other than GPa. No data for ZM was provided. Results discrepancy could result from variations in the preparation of material samples and other external factors (e.g., measuring system, the indenter shape, and applied load) [
52].
One of the limitations of this study is that the protocol which was used for finishing and polishing was consistent for all tested materials, due to ease and standardization. Also, this in vitro investigation could not completely simulate clinical conditions in which the samples were not subjected to cyclic loading and thermal variations. Moreover, the effects of abutment materials and cement bonding on the results have not been evaluated in this study. Only in vivo studies will reveal the predictable clinical applications, survival rate, and shortcomings of these innovations of translucent esthetic zirconia.
Future research should assess the impact of variable polishing materials and techniques on the mechanical properties of monolithic multi-layered zirconia ceramics. In addition, fatigue behavior, fractographic analysis, biocompatibility, and aging, have not yet been tested and should be investigated. Further studies simulating the variables of the in vivo environment are needed to extrapolate definitive clinical recommendations.
5. Conclusions
Taking into consideration the limitations of this in vitro study, it could be concluded that multi-layered esthetic zirconia showed superior mechanical properties when compared with lithium disilicate glass-ceramic and thus can be considered as a predictable alternative restorative material in cases where both strength and esthetics are needed. Long-term in vivo studies are required to validate this extrapolation.
Author Contributions
Conceptualization, L.A.A. and S.N.A.; Formal analysis, T.Z.; Funding acquisition, T.Z.; Investigation, S.N.A., T.Z. and L.A.A.; Methodology, L.A.A. and S.N.A.; Project administration, L.A.A. and S.N.A.; Supervision, S.N.A. and L.A.A.; Writing—original draft, S.N.A., T.Z. and L.A.A.; Writing—review & editing, S.N.A. and L.A.A. and T.Z.. All authors have read and agreed to the published version of the manuscript. and agreed to the published version of the manuscript.
Funding
This research was funded by the Faculty of Scientific Research (grant number 375).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to acknowledge the dental technologists and the mechanical engineers who participated in conducting the experiment of this study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Rosentritt M, Sikora M, Behr M, Handel G. in vitro fracture resistance and marginal adaptation of metallic and tooth-colored post systems. J. Oral Rehabil. 2004, 31, 675–81. [CrossRef]
- Kisi EH, Howard CJ. Crystal structures of zirconia phases and their inter-relation. Key Eng. Mater. 1998, 153–54, 1–36. [CrossRef]
- Denry I, Kelly J. State of the art of zirconia for dental applications. Dent Mater. 2008, 24, 299–307. [CrossRef]
- Ruff O EF, Stephen E. Contributions to the ceramics of highly refractory materials: II. System zirconia-lime. Z Anorg Allg Chem. 1929, 180, 215–24.
- Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zirconia and other non-silicate ceramics: Where are we now? Dent Mater. 2011, 27, 71–82. [CrossRef]
- Elsaka SE. Influence of surface treatments on the surface properties of different zirconia cores and adhesion of zirconia-veneering ceramic systems. Dent Mater. 2013, 29, 239–51. [CrossRef]
- Anusavice KJ. Phillips’ Science of Dental Materials - eBook. 11th ed. Elsevier Health Sciences; 2003.
- Magne P, Belser U. Esthetic improvements and in vitro testing of In-Ceram Alumina and Spinell ceramic. Int J Prosthodont. 1997, 10.
- Marchack BW, Sato S, Marchack CB, White SN. Complete and partial contour zirconia designs for crowns and fixed dental prostheses: a clinical report. J Prosthet Dent. 2011, 106, 145–52. [CrossRef] [PubMed]
- Stawarczyk B, Özcan M, Roos M, Trottmann A, Sailer I, Hammerle C. Load-bearing capacity and failure types of anterior zirconia crowns veneered with overpressing and layering techniques. Dent Mater. 2011, 27, 1045–53. [CrossRef] [PubMed]
- Kelly JR, Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Aust. Dent. J.. 2011, 56 Suppl 1, 84–96. [CrossRef] [PubMed]
- Örtorp A, Kihl ML, Carlsson GE. A 3-year retrospective and clinical follow-up study of zirconia single crowns performed in a private practice. J Dent. 2009, 37, 731–6. [CrossRef]
- Zeynep Ozkurt, Ender Kazazoglu. Clinical success of zirconia in dental applications. J Prosthodont. 2010, 19, 64–8. [CrossRef]
- Guess PC, Bonfante EA, Silva NRFA, Coelho PG, Thompson VP. Effect of core design and veneering technique on damage and reliability of Y-TZP-supported crowns. Dent Mater. 2013, 29, 307–16. [Google Scholar] [CrossRef]
- Swain, MV. Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures. Acta Biomater. 2009, 5, 1668–77. [Google Scholar] [CrossRef] [PubMed]
- Komine F, Strub JR, Matsumura H. Bonding between layering materials and zirconia frameworks. Jpn Dent Sci Rev.. 2012, 48, 153–61. [Google Scholar] [CrossRef]
- Ishibe M, Raigrodski AJ, Flinn BD, Chung K-H, Spiekerman C, Winter RR. Shear bond strengths of pressed and layered veneering ceramics to high-noble alloy and zirconia cores. J Prosthet Dent. 2011, 106, 29–37. [CrossRef] [PubMed]
- Christensen RP, Ploeger BJ. A clinical comparison of zirconia, metal and alumina fixed-prosthesis frameworks veneered with layered or pressed ceramic. J Am Dent Assoc. 2010, 141, 1317–29. [CrossRef] [PubMed]
- Schmitter M, Mueller D, Rues S. Chipping behaviour of all-ceramic crowns with zirconia framework and CAD/CAM manufactured veneer. J Dent. 2012, 40, 154–62. [CrossRef]
- Culp L, McLaren EA. Lithium disilicate: the restorative material of multiple options. Compend Contin Educ Dent. 2010, 31, 716–20. [Google Scholar]
- Schley J-S, Heussen N, Reich S, Fischer J, Haselhuhn K, Wolfart S. Survival probability of zirconia-based fixed dental prostheses up to 5 yr: a systematic review of the literature. Eur J Oral Sci. 2010, 118, 443–50. [Google Scholar] [CrossRef]
- Silva LH da, Lima E de, Miranda RB de P, Favero SS, Lohbauer U, Cesar PF. Dental ceramics: a review of new materials and processing methods. Braz Oral Res. 2017, 31, e58. [CrossRef]
- Burgess JO. Zirconia: the material, its evolution, and composition. Compend Contin Educ Dent. 2018, 39 (suppl 4), 4–8.
- Zhang Y, Lawn BR. Novel zirconia materials in dentistry. J. Dent. Res. 2018, 97, 140–7. [CrossRef] [PubMed]
- Zhang F, Inokoshi M, Batuk M, Hadermann J, Naert I, Van Meerbeek B, et al.. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater 2016, 32, e327–37. [CrossRef]
- Harada K, Raigrodski AJ, Chung KH, Flinn BD, Dogan S, Mancl LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J Prosthet Dent 2016, 116, 257–63. [CrossRef] [PubMed]
- Tareq A. Ziyad, Layla A. Abu-Naba’a, Saleh N. Almohammed. Optical properties of CAD-CAM monolithic systems compared: three multi-layered zirconia and one lithium disilicate system. Heliyon 2021, 7, e08151. [CrossRef]
- International Organization for Standardization. ISO-6872:2015. Dentistry ceramic materials. Geneva: International Organization for Standardization;2015. p. 36.
- Elsaka SE, Elnaghy AM. Mechanical properties of zirconia reinforced lithium silicate glass-ceramics. Dent Mater. 2016, 32, 908–14. [CrossRef]
- Coldea A, Swain M V, Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent Mater. 2013, 24, 419–26. [CrossRef]
- ASTM C1327-15. Standard test method for Vickers indentation hardness of advanced ceramics; 2019. p. 10.
- Della Bona A, Anusavice KJ, Mecholsky JJ. Failure analysis of resin composite bonded to ceramic. Dent Mater. 2003, 19, 693–9. [CrossRef] [PubMed]
- Zarone F, Di Mauro MI, Ausiello P, Ruggiero G, Sorrentino R. Current status on lithium disilicate and zirconia: a narrative review. BMC Oral Health. 2019, 19, 134. [CrossRef]
- Goujat A, Abouelleil H, Colon P, Jeannin C, Pradelle N, Seux D, et al.. Mechanical properties and internal fit of 4 CAD-CAM block materials. J Prosthet Dent. 2018, 119, 384–9. [CrossRef] [PubMed]
- Fabian Fonzar R, Carrabba M, Sedda M, Ferrari M, Goracci C, Vichi A. Flexural resistance of heat-pressed and CAD-CAM lithium disilicate with different translucencies. Dent Mater. 2017, 33, 63–70. [CrossRef] [PubMed]
- Nassary Zadeh P, Lümkemann N, Sener B, Eichberger M, Stawarczyk B. Flexural strength, fracture toughness, and translucency of cubic/tetragonal zirconia materials. J Prosthet Dent. 2018, 120, 948–54. [CrossRef] [PubMed]
- Elsaka SE. Optical and mechanical properties of newly developed monolithic multilayer zirconia. J Prosthodont. 2019, 28, 279–84. [CrossRef]
- Paek T, Fan Y, Giordano R. Mechanical properties of translucent multilayered dental zirconia. J Dent Oral Disord [Internet]. 2020 [cited 2020 Jul 25];6. Available from: https://austinpublishinggroup.com/dental-disorders/fulltext/jdod-v6-id1124.php.
- Albakry M, Guazzato M, Swain M. Biaxial flexural strength, elastic moduli, and X-ray diffraction characterization of three pressable all-ceramic materials. J Prosthet Dent. 2003, 89, 374–80. [CrossRef]
- Leung BTW, Tsoi JKH, Matinlinna JP, Pow EHN. Comparison of mechanical properties of three machinable ceramics with an experimental fluorophlogopite glass ceramic. J Prosthet Dent. 2015, 114, 440–6. [CrossRef] [PubMed]
- Todd D. Church, Jeffrey P. Jessup, Villa L. Guillory. Translucency and strength of high translucency monolithic zirconium oxide materials. Gen Dent. 2017, 5.
- sitrou EA, Northeast SE, van Noort R. Brittleness index of machinable dental materials and its relation to the marginal chipping factor. J Dent. 2007, 35, 897–902. [CrossRef]
- Schaefer O, Watts DC, Sigusch BW, Kuepper H, Guentsch A. Marginal and internal fit of pressed lithium disilicate partial crowns in vitro: a three-dimensional analysis of accuracy and reproducibility. Dent Mater. 2012, 28, 320–6. [CrossRef]
- Bottino MA, Campos F, Ramos NC, Rippe MP, Valandro LF, Melo RM. Inlays made from a hybrid material: adaptation and bond strengths. Oper. Dent. 2015, 40, 83–91. [CrossRef]
- Charlton D, Roberts HW, Tiba A. Measurement of select physical and mechanical properties of 3 machinable ceramic materials. Quintessence Int. 2008, 39, 573–9.
- Ronald L. Sakaguchi, John M. Powers. Craig’s Restorative Dental Materials [Internet]. 13th Ed. Elsevier; 2011 [cited 2020 Jul 27]. Available from: https://linkinghub.elsevier.com/retrieve/pii/C20100657543.
- Hudson JD, Goldstein GR, Georgescu M. Enamel wear caused by three different restorative materials. J Prosthet Dent. 1995, 74, 647–54. [CrossRef] [PubMed]
- Jagger DC, Harrison A. An in vitro investigation into the wear effects of selected restorative materials on dentine. J. Oral Rehabil. 1995, 22, 349–54. [CrossRef] [PubMed]
- Olivera AB, Marques MM. Esthetic restorative materials and opposing enamel wear. Oper. Dent. 2008, 33, 332–7. [CrossRef] [PubMed]
- Gore GJ, Gates JD. Effect of hardness on three very different forms of wear. Wear. 1997, 203–4, 544–63. [CrossRef]
- Roy S, Basu B. Mechanical and tribological characterization of human tooth. Mater Charact. 2008, 59, 747–56. [CrossRef]
- Zhang Y-R, Du W, Zhou X-D, Yu H-Y. Review of research on the mechanical properties of the human tooth. Int. J. Oral Sci. 2014, 6, 61–9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).