Submitted:
07 November 2023
Posted:
07 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Patients and Methods
2.1. Patient Population
2.2. Data Collection
2.3. Surgical Technique
2.3.1. Patient and Robot Setup
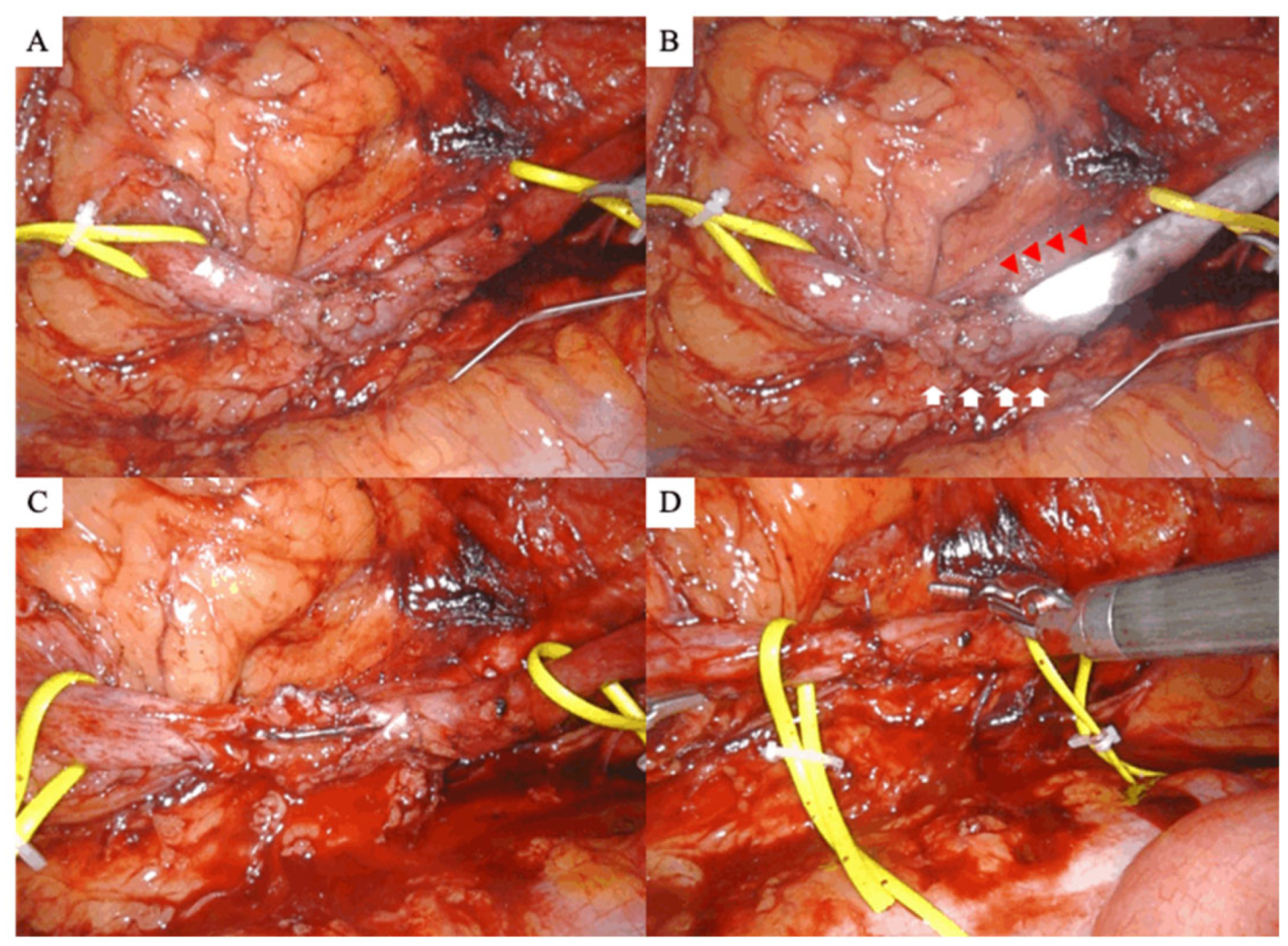
2.4. Stricture Identification
2.5. Dissection of the Ureteral Stricture, Anastomosis and Stenting
2.6. Statistical Analysis
3. Results
3.1. Clinical Characteristics
3.2. Surgical Outcomes
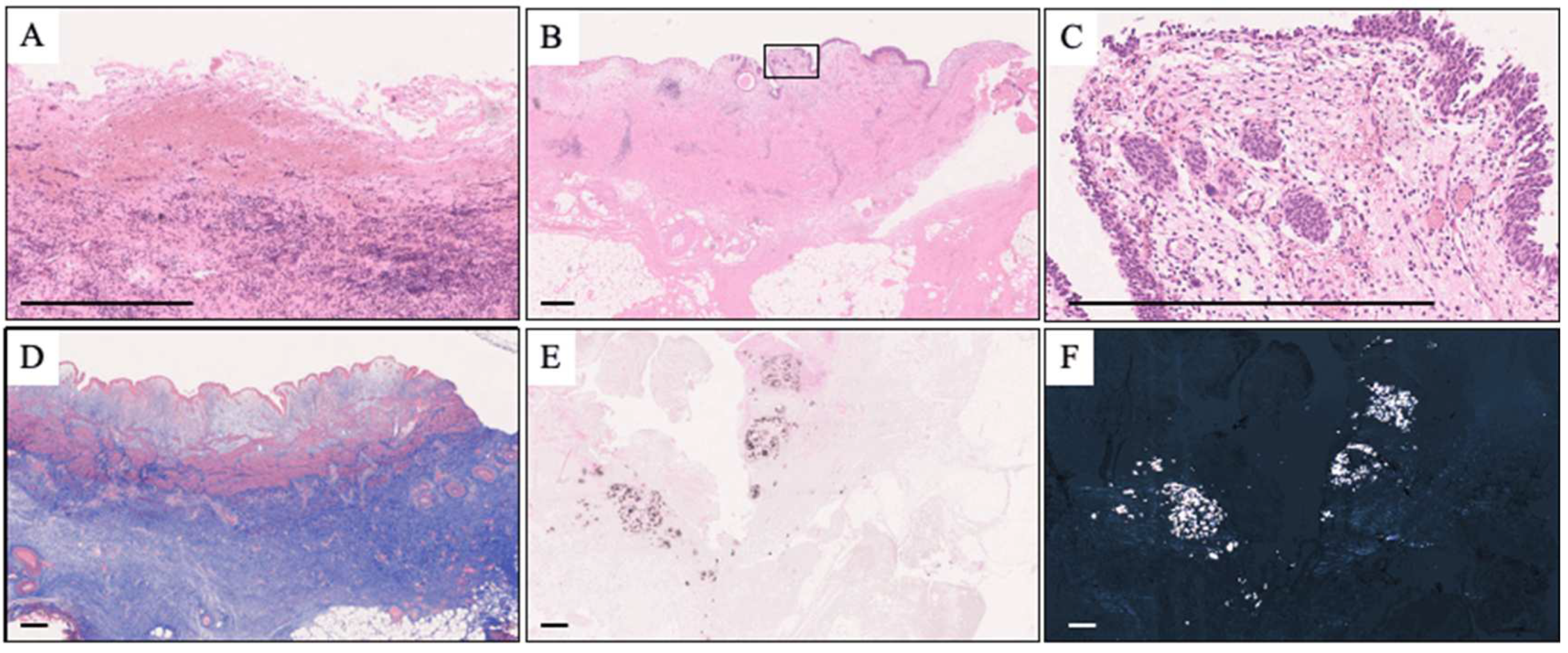
3.3. Pathological Analysis
4. Discussion
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chung, K.J.; Kim, J.H.; Min, G.E.; Park, H.K.; Li, S.; Del Giudice, F.; Han, D.H.; Chung, B.I. Changing trends in the treatment of nephrolithiasis in the real world. J Endourol 2019, 33, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, S.; Miyazawa, K.; Yasui, T.; Iguchi, T.; Fujita, M.; Nishimatsu, H.; Masaki, T.; Hasegawa, T.; Hibi, H.; Arakawa, T.; et al. Chronological changes in epidemiological characteristics of lower urinary tract urolithiasis in Japan. Int J Urol 2019, 26, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Sunaryo, P.L.; May, P.C.; Holt, S.K.; Sorensen, M.D.; Sweet, R.M.; Harper, J.D. Ureteral strictures following ureteroscopy for kidney stone disease: A population-based assessment. J Urol 2022, 208, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Ulvik, Ø.; Harneshaug, J.R.; Gjengstø, P. Ureteral strictures following ureteroscopic stone treatment. J Endourol 2021, 35, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Sugino, T.; Taguchi, K.; Hamamoto, S.; Okada, T.; Isogai, M.; Tanaka, Y.; Unno, R.; Fujii, Y.; Hamakawa, T.; Ando, R.; et al. Risk factors for failure of endoscopic management of stone-related ureteral strictures. Urol J 2021, 19, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Carlton, C.E. Jr.; Guthrie, A.G.; Scott, R. Jr. Surgical correction of ureteral injury. J Trauma 1969, 9, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Simmons, M.N.; Gill, I.S.; Fergany, A.F.; Kaouk, J.H.; Desai, M.M. Laparoscopic ureteral reconstruction for benign stricture disease. Urology 2007, 69, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Kolontarev, K.; Kasyan, G.; Pushkar, D. Robot-assisted laparoscopic ureteral reconstruction: а systematic review of literature. Cent Eur J Urol 2018, 71, 221–227. [Google Scholar] [CrossRef]
- Elsamra, S.E.; Theckumparampil, N.; Garden, B.; Alom, M.; Waingankar, N.; Leavitt, D.A.; Kreshover, J.; Schwartz, M.; Kavoussi, L.R.; Richstone, L. Open, laparoscopic, and robotic ureteroneocystotomy for benign and malignant ureteral lesions: a comparison of over 100 minimally invasive cases. J Endourol 2014, 28, 1455–1459. [Google Scholar] [CrossRef]
- Lee, Z.; Moore, B.; Giusto, L.; Eun, D.D. Use of indocyanine green during robot-assisted ureteral reconstructions. Eur Urol 2015, 67, 291–298. [Google Scholar] [CrossRef]
- Elbers, J.R.; Rodríguez Socarrás, M.; Rivas, J.G.; Autran, A.M.; Esperto, F.; Tortolero, L.; Carrion, D.M.; Sancha, F.G. Robotic repair of ureteral strictures: techniques and review. Curr Urol Rep 2021, 22, 39. [Google Scholar] [CrossRef] [PubMed]
- Ellenbogen, P.H.; Scheible, F.W.; Talner, L.B.; Leopold, G.R. Sensitivity of gray scale ultrasound in detecting urinary tract obstruction. AJR Am J Roentgenol 1978, 130, 731–733. [Google Scholar] [CrossRef] [PubMed]
- Tiselius, H.G.; Andersson, A. Stone burden in an average Swedish population of stone formers requiring active stone removal: how can the stone size be estimated in the clinical routine? Eur Urol 2003, 43, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Roberts, W.W.; Cadeddu, J.A.; Micali, S.; Kavoussi, L.R.; Moore, R.G. Ureteral stricture formation after removal of impacted calculi. J Urol 1998, 159, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Netto Júnior, N.R.; Ferreira, U.; Lemos, G.C.; Claro, J.F. Endourological management of ureteral strictures. J Urol 1990, 144, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Vannahme, M.; Mathur, S.; Davenport, K.; Timoney, A.G.; Keeley, F.X. Jr. The management of secondary pelvi-ureteric junction obstruction – a comparison of pyeloplasty and endopyelotomy. BJU Int 2014, 113, 108–112. [Google Scholar] [CrossRef]
- Moscardi, P.R.; Barbosa, J.A.; Andrade, H.S.; Mello, M.F.; Cezarino, B.N.; Oliveira, L.M.; Srougi, M.; Dénes, F.T.; Lopes, R.I. Reoperative laparoscopic ureteropelvic junction obstruction repair in children: safety and efficacy of the technique. J Urol 2017, 197, 798–804. [Google Scholar] [CrossRef]
- Lee, M.; Lee, Z.; Houston, N.; Strauss, D.; Lee, R.; Asghar, A.M.; Corse, T.; Zhao, L.C.; Stifelman, M.D.; Eun, D.D.; et al. Robotic ureteral reconstruction for recurrent strictures after prior failed management. BJUI Compass 2023, 4, 298–304. [Google Scholar] [CrossRef]
- Buffi, N.; Cestari, A.; Lughezzani, G.; Bellinzoni, P.; Sangalli, M.; Scapaticci, E.; Zanoni, M.; Annino, F.; Larcher, A.; Lazzeri, M.; et al. Robot-assisted uretero-ureterostomy for iatrogenic lumbar and iliac ureteral stricture: technical details and preliminary clinical results. Eur Urol 2011, 60, 1221–1225. [Google Scholar] [CrossRef]
- White, C.; Stifelman, M. Ureteral reimplantation, psoas hitch, and Boari flap. J Endourol 2020, 34, S25–S30. [Google Scholar] [CrossRef] [PubMed]
- Buffi, N.M.; Lughezzani, G.; Hurle, R.; Lazzeri, M.; Taverna, G.; Bozzini, G.; Bertolo, R.; Checcucci, E.; Porpiglia, F.; Fossati, N.; et al. Robot-assisted surgery for benign ureteral strictures: experience and outcomes from four tertiary care institutions. Eur Urol 2017, 71, 945–951. [Google Scholar] [CrossRef]
- Heijkoop, B.; Kahokehr, A.A. Buccal mucosal ureteroplasty for the management of ureteric strictures: A systematic review of the literature. Int J Urol 2021, 28, 189–195. [Google Scholar] [CrossRef]
- Yang, K.; Wang, X.; Xu, C.; Li, Z.; Han, G.; Fan, S.; Chen, S.; Li, X.; Zhu, H.; Zhou, L.; et al. Totally intracorporeal robot-assisted unilateral or bilateral ileal ureter replacement for the treatment of ureteral strictures: technique and outcomes from a Single Center. Eur Urol 2023. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Lu, Y.; Hu, H.; Zhang, J.; Qin, B.; Zhu, J.; Dirie, N.I.; Zhang, Z.; Wang, S. Management of recurrent ureteral stricture: a retrospectively comparative study with robot-assisted laparoscopic surgery versus open approach. PeerJ 2019, 7, e8166. [Google Scholar] [CrossRef] [PubMed]
- Hemal, A.K.; Nayyar, R.; Gupta, N.P.; Dorairajan, L.N. Experience with robot assisted laparoscopic surgery for upper and lower benign and malignant ureteral pathologies. Urology 2010, 76, 1387–1393. [Google Scholar] [CrossRef]
- Yang, K.K.; Asghar, A.M.; Lee, R.A.; Strauss, D.; Kuppa, S.; Lee, Z.; Metro, M.; Eun, D.D. Robot-assisted laparoscopic distal ureteroureterostomy for distal benign ureteral strictures with long-term follow-up. J Endourol 2022, 36, 203–208. [Google Scholar] [CrossRef]
- Lee, Z.; Llukani, E.; Reilly, C.E.; Mydlo, J.H.; Lee, D.I.; Eun, D.D. Single surgeon experience with robot-assisted ureteroureterostomy for pathologies at the proximal, middle, and distal ureter in adults. J Endourol 2013, 27, 994–999. [Google Scholar] [CrossRef]
- Ueshima, E.; Fujimori, M.; Kodama, H.; Felsen, D.; Chen, J.; Durack, J.C.; Solomon, S.B.; Coleman, J.A.; Srimathveeravalli, G. Macrophage-secreted TGF-β1 contributes to fibroblast activation and ureteral stricture after ablation injury. Am J Physiol Ren Physiol 2019, 317, F52–F64. [Google Scholar] [CrossRef]
- Dretler, S.P.; Young, R.H. Stone granuloma: a cause of ureteral stricture. J Urol 1993, 150, 1800–1802. [Google Scholar] [CrossRef] [PubMed]
- Traxer, O.; Thomas, A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol 2013, 189, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Wollin, D.A.; Carlos, E.C.; Tom, W.R.; Simmons, W.N.; Preminger, G.M.; Lipkin, M.E. Effect of laser settings and irrigation rates on ureteral temperature during holmium laser lithotripsy, an in vitro model. J Endourol 2018, 32, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Pietropaolo, A.; Massella, V.; Ripa, F.; Sinha, M.M.; Somani, B.K. Ureteroscopy and lasertripsy with pop dusting using high power holmium laser for large urinary stones > 15 mm: 6.5-year prospective outcomes from a high-volume stone center. World J Urol 2023, 41, 1935–1941. [Google Scholar] [CrossRef] [PubMed]
| Patient characteristics | |||
| age | y.o. | 49.8 | (10.2) |
| sex (%) | |||
| male | 10 | (71.4) | |
| female | 4 | (28.6) | |
| laterality (%) | |||
| right | 6 | (42.9) | |
| left | 8 | (57.1) | |
| BMI | kg/m2 | 23.07 | (2.11) |
| Characteristics of previous urinary calculi | |||
| location (%) | |||
| UPJ | 4 | (28.6) | |
| proximal ureter | 7 | (50.0) | |
| middle ureter | 2 | (14.3) | |
| distal ureter | 1 | (7.1) | |
| stone size | mm | 11.85 | [11.00, 14.75] |
| stone volume | mm2 | 78.11 | [72.76, 99.11] |
| number of previous stone treatment | |||
| SWL | 0.00 | [0.00, 0.00] | |
| URSL | 2.00 | [1.00, 2.00] | |
| PCNL | 0.00 | [0.00, 0.00] | |
| stone analysis (%) | |||
| calcium stone | 8 | (57.1) | |
| ammonium Acid Urate | 1 | (7.1) | |
| cystine | 1 | (7.1) | |
| unknown | 4 | (28.6) | |
| stricture location (%) | |||
|---|---|---|---|
| UPJ | 3 | (21.4) | |
| proximal ureter | 7 | (50.0) | |
| middle ureter | 3 | (21.4) | |
| distal ureter | 1 | (7.1) | |
| deviation from the previous stone site (%) | 4 | (28.6) | |
| stricture length on radiography | mm | 22.66 | (7.38) |
| prior treatment for stricture (%) | |||
| none | 5 | (35.7) | |
| balloon dilation | 1 | (7.1) | |
| endoscopic incision plus balloon dilation | 8 | (57.1) | |
| frequency of prior treatment for stricture | times | 1.00 | [0.00, 1.00] |
| perioperative hydronephrosis (%) | |||
| no obstruction | 0 | (0) | |
| mild | 0 | (0) | |
| moderate | 4 | (28.6) | |
| severe | 10 | (71.4) | |
| split renal function of the affected side | % | 29.28 | (15.31) |
| stricture identification | |||
|---|---|---|---|
| ICG | 8 | (57.1) | |
| IRIS catheter | 6 | (42.9) | |
| transected ureter length | mm | 26.36 | (9.60) |
| surgery time | minutes | 205.53 | (46.51) |
| console time | minutes | 164.36 | (44.18) |
| blood loss | ml | 10.00 | [0.00, 57.00] |
| postoperative complication (Clavien-Dindo grade; %) | |||
| 0 | 12 | (85.7) | |
| I | 1 | (7.1) | |
| II | 1 | (7.1) | |
| >= III | 0 | (0) | |
| postoperative hydronephrosis 3 months after surgery (%) | |||
| none | 3 | (21.4) | |
| mild | 10 | (71.4) | |
| moderate | 1 | (7.1) | |
| severe | 0 | ||
| success rate (%) | 13 | (92.9) | |
| pathological features (%) | |||
| inflammatory cell infiltration | 13 | (92.9) | |
| fibrosis | 13 | (92.9) | |
| calcification | 8 | (57.1) | |
| loss of urothelium | 4 | (28.6) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





