Submitted:
08 November 2023
Posted:
09 November 2023
You are already at the latest version
Abstract
Keywords:
Introduction:
- METHODOLOGY:
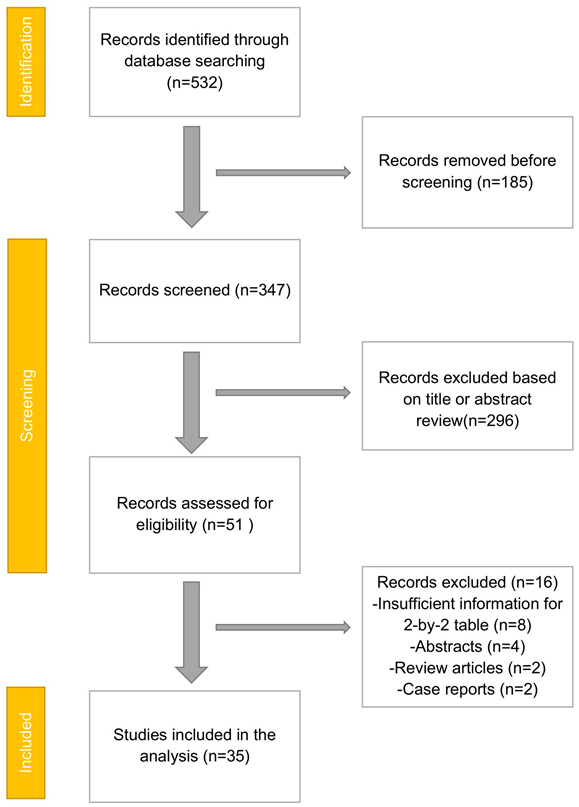
- PRISMA Flowchart (Figure 1)
- DATA COLLECTION
- INCLUSION AND EXCLUSION CRITERIA
- DATA EXTRACTION
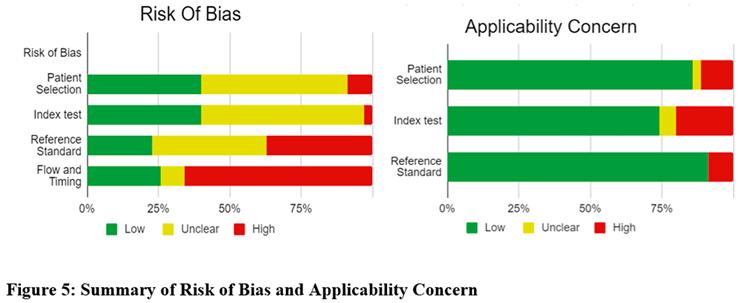
- ASSESSMENT OF STUDY QUALITY
- STATISTICAL ANALYSIS
- BIAS STUDY
- RESULT:
| First Author | Year | Location | Study type | Study dates | Index test | Reference standard | Total Patients | Females | Mean Age |
| Aggawala [12] |
2018 | Australia | Prospective | 2017-2018 | MRI | Histology or Follow-Up | 52 | 37 | Unclear (range 10-39 years) |
| Aguilera [13] | 2018 | U.S.A | Retrospective | 2014-2016 | MRI | Histology or Follow-Up | 52 | 52 | Median age 25 |
| Amitai [14] | 2016 | Isreal | Retrospective | 2007-2013 | MRI | Histology or Follow-Up | 49 | 49 | Unclear |
| Aspelund [15] | 2014 | U.S.A | Retrospective | 2008-2012 | MRI | Histology or Follow-Up | 397 | Unclear | Unclear |
| Avcu [16] | 2013 | Turkey | Prospective | 2009-2010 | MRI | Histology or Follow-Up | 55 | 26 | 35.6 |
| Batool [17] | 2016 | Canada | Prospective | Unclear | MRI | Histology or Follow-Up | 100 | 56 | Unclear |
| Bayraktutan [18] | 2014 | Turkey | Prospective | Unclear | MRI | Histology or Follow-Up | 45 | 19 | 7 |
| Burke [19] | 2015 | U.S.A,multicentre | Retrospective | 2009-2014 | MRI | Histology or Follow-Up | 709 | 709 | 27.5 |
| Burns [20] | 2018 | Canada | Retrospective | 2006-2012 | MRI | Histology or Follow-Up | 63 | 63 | 31 |
| Corkum [21] | 2018 | U.S.A | Retrospective | 2015-2016 | MRI | Histology or Follow-Up | 135 | Unclear | 11.5 |
| des Plantes [22] | 2016 | Netherlands | Prospective | Unclear | MRI | Histology or Follow-Up | 112 | 112 | 22 |
| Dibble [23] | 2017 | U.S.A | Retrospective | 2011-2012 | MRI | Histology or Follow-Up | 77 | Unclear | 11.5 |
| Didier [24] | 2017 | U.S.A | Retrospective | 2013-2015 | MRI | Histology or Follow-Up | 98 | 60 | 11 |
| Dillman [25] | 2016 | U.S.A | Retrospective | 2013-2014 | MRI | Histology or Follow-Up | 103 | 56 | 11.5 |
| Donlon [26] | 2015 | Ireland | Retrospective | 2008-2014 | MRI | Histology or Follow-Up | 29 | 29 | Unclear |
| Fonseca [27] | 2014 | U.S.A | Retrospective | 2000-2011 | MRI | Histology or Follow-Up | 31 | 31 | Unclear |
| Kearl [28] | 2016 | U.S.A | Retrospective | 2010-2013 | MRI | Histology or Follow-Up | 192 | Unclear | 14.8 |
| Kennedy [29] | 2018 | U.S.A | Retrospective | 2014-2017 | MRI | Histology or Follow-Up | 612 | 353 | 11.7 |
| Khalil [30] | 2018 | U.S.A | Retrospective | 2014-2017 | MRI | Histology or Follow-Up | 568 | Unclear | Unclear |
| Kinner [31] | 2017 | U.S.A | Prospective | 2012-2014 | MRI | Histology or Follow-Up | 230 | 28 | 17.1 |
| Koning [32] | 2014 | U.S.A | Retrospective | 2012-2013 | MRI | Histology or Follow-Up | 364 | 223 | 11.3 |
| Konrad [33] | 2015 | U.S.A | Retrospective | 2009-2011 | MRI | Histology or Follow-Up | 114 | 114 | Unclear |
| Kulaylat [34] | 2015 | U.S.A | Retrospective | 2011-2013 | MRI | Histology or Follow-Up | 510 | 23 | 11.3 |
| Shin [35] | 2017 | Korea | Retrospective | 2008-2015 | MRI | Histology or Follow-Up | 125 | 125 | 30.6 |
| Theilen [36] | 2015 | U.S.A | Retrospective | 2007-2012 | MRI | Histology or Follow-Up | 171 | 171 | Unclear |
| Thieme [37] | 2014 | Netherlands | Prospective | 2009 | MRI | Histology or Follow-Up | 104 | 57 | 12 |
| Tsai [38] | 2017 | U.S.A | Retrospective | 2003-2015 | MRI | Histology or Follow-Up | 233 | 233 | 28.4 |
| Nitta [39] | 2005 | Japan | Retrospective | Unclear | MRI | Histology or Follow-Up | 37 | 19 | 37.1 |
| Cobben [40] | 2009 | Netherlands | Prospective | 2005-2006 | MRI | Histology or Follow-Up | 138 | 80 | 29 |
| Singh [41] | 2009 | U.S.A | Retrospective | 2001-2007 | MRI | Histology or Follow-Up | 40 | unknown | 34 |
| Inci E [42] | 2011 | Turkey | Prospective | Unclear | MRI | Histology or Follow-Up | 119 | 36 | 27 |
| Chabanova [43] | 2011 | Denmark | Prospective | Unclear | MRI | Histology or Follow-Up | 48 | 29 | 37.1 |
| Heverhagen JT [44] | 2012 | Germany | Prospective | 2008 | MRI | Histology or Follow-Up | 52 | 21 | 44.7 |
| Zhu [45] | 2012 | China | Prospective | 2009-2011 | MRI | Histology | 41 | 23 | 41.5 |
| Leeuwenburgh [46] | 2014 | Netherlands | Prospective | 2010 | MRI | Histology or Follow-Up | 223 | 138 | 38 |
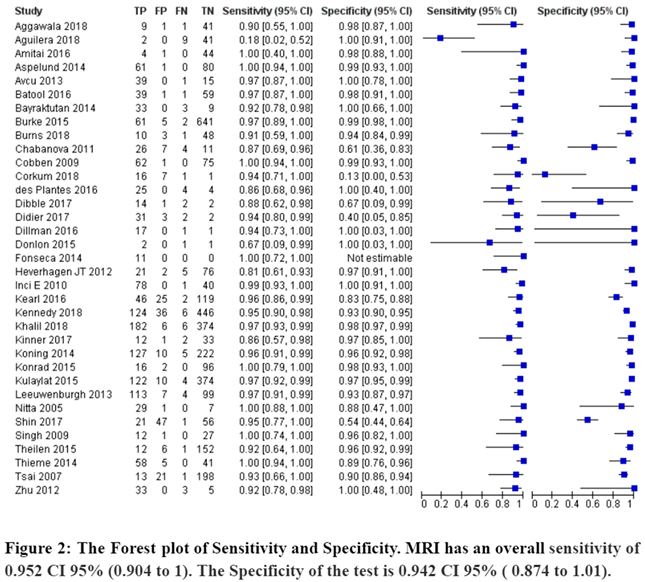
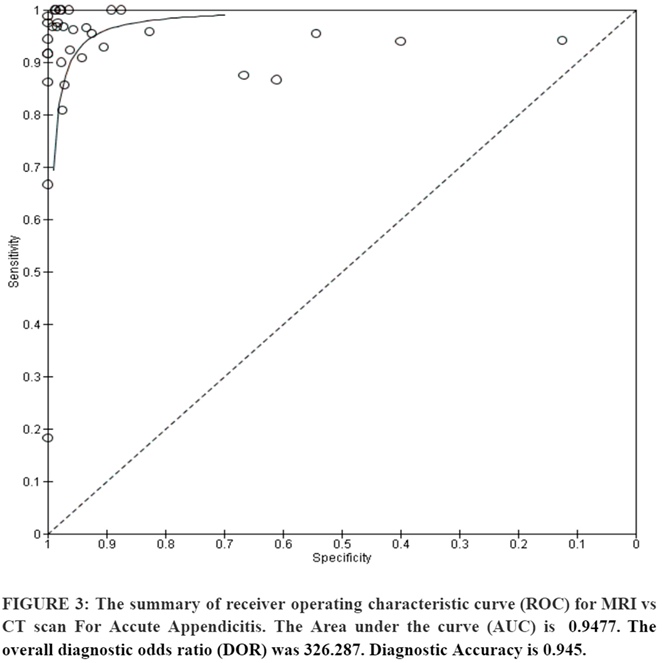
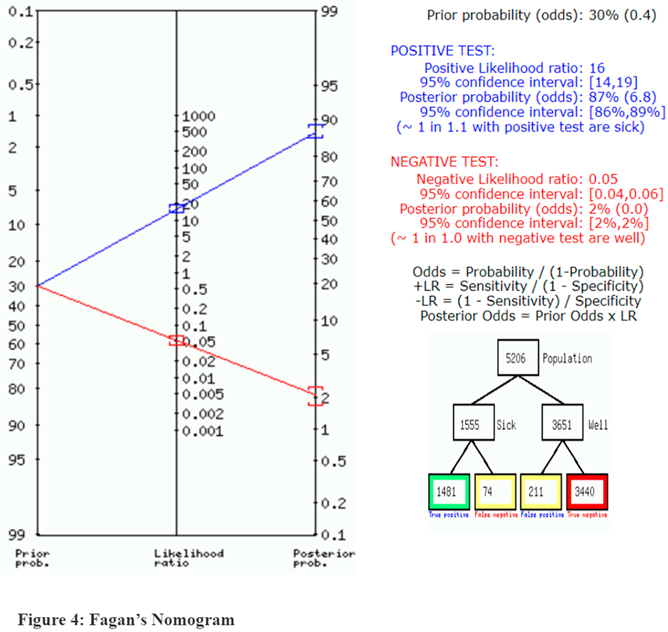
- MRI
- vs CT scan for Appendicitis
- Bias Study:
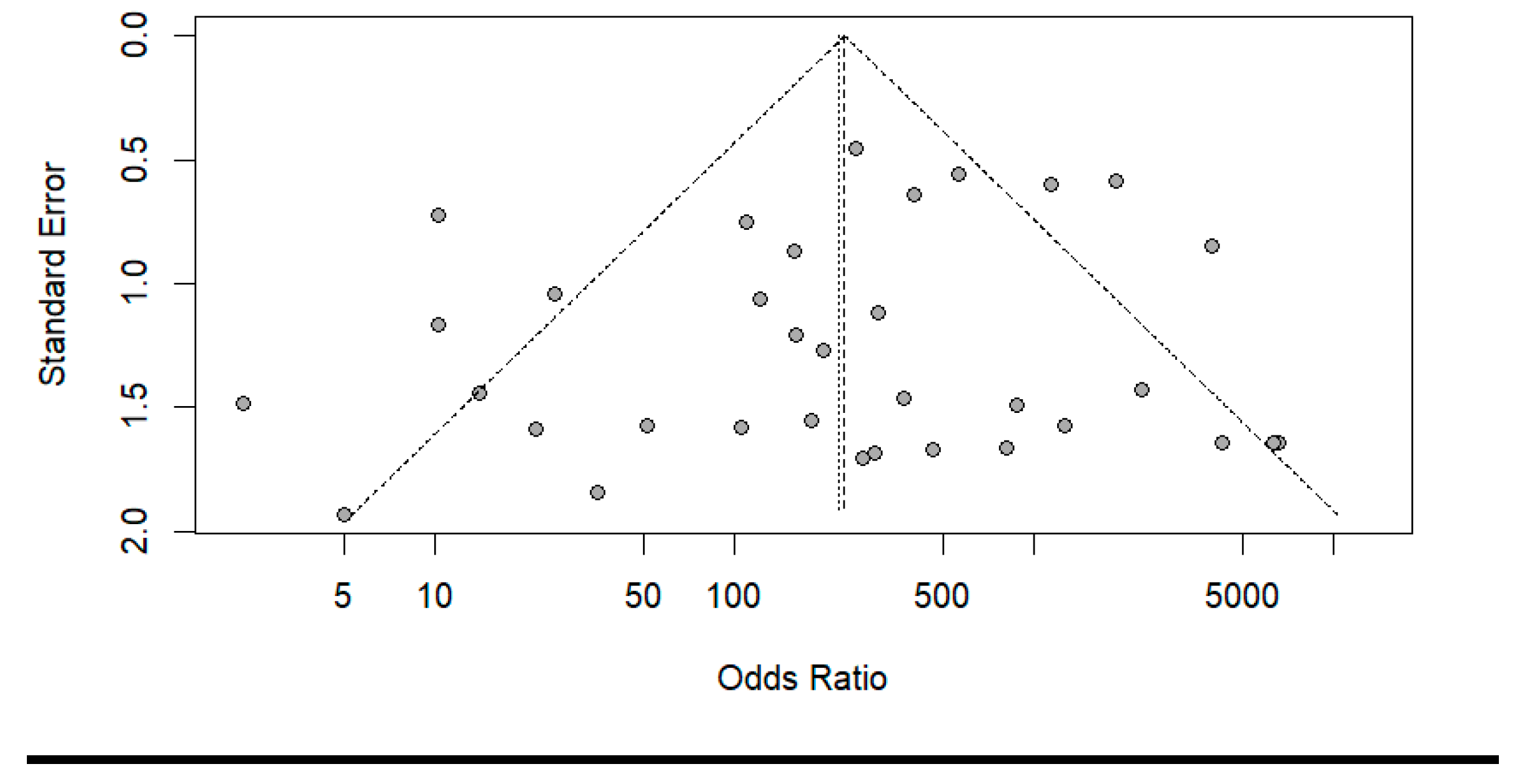
- Publication Bias:
Discussion:
Conclusion:
Limitations:
References
- Mason Rodney, J. , “Surgery for appendicitis: is it necessary?”.
- Bernard, A. Birnbaum and Stephanie R. Wilson, “Appendicitis at the Millennium”.
- Thomas Jaschinski, Mosch Christoph G, Eikermann Michaela, Edmund Am Neugebauer, and Stefan Sauerland, “Laparoscopic versus open surgery for suspected appendicitis”.
- Adrienne van Randen, Boermeester Marja A, Zwinderman Aeilko H, Ubbink Dirk T, Stoke Jaap, and Bipat Shandra, “Acute appendicitis: a meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease”.
- K F Borushok, R R Townsend, F C Laing, and R B Jeffrey Jr, “Sonographic diagnosis of perforation in patients with acute appendicitis”.
- Jason D Fraser et al., “Accuracy of computed tomography in predicting appendiceal perforation”.
- Thomas A Foley, Frank Earnest 4th, David M Hough, Mark A Nathan, Henry J Schiller, and Tanya L Hoskin, “Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay”.
- Suk Won Suh et al., “Clinical factors for distinguishing perforated from nonperforated appendicitis: a comparison using multidetector computed tomography in 528 laparoscopic appendectomies”.
- Marjolein M N Leeuwenburgh et al., “Comparison of imaging strategies with conditional contrast-enhanced CT and unenhanced MR imaging in patients suspected of having appendicitis: a multicenter diagnostic performance study”.
- Lodewijk Cobben, Emile Coerkamp, Ingrid Groot, Lucas Kingma, Julien Puylaert, and Johan Blickman, “A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on the outcome of appendectomy”.
- Dr. Dev Desai, “Dev’s Formulae for Diagnostic Test Accuracy Meta-analysis”.
- S. Aggarwala et al., “The role of a rapid protocol abdominal MRI for patients with clinically suspected Appendicitis”.
- Fabiola Aguilera, Brian F Gilchrist, and Daniel T Farkas, “Accuracy of MRI in Diagnosing Appendicitis during Pregnancy”.
- Michal M Amitai et al., “Role of Emergency Magnetic Resonance Imaging for the Workup of Suspected Appendicitis in Pregnant Women”.
- Gudrun Aspelund et al., “Ultrasonography/MRI versus CT for diagnosing appendicitis”.
- Serhat Avcu, Halil Arslan, Feray Altun Çetin, Özgur Kemik, and Ahmet Cumhur Dülger, “The value of diffusion-weighted imaging and apparent diffusion coefficient quantification in the diagnosis of perforated and nonperforated appendicitis”.
- Batool S, Thomson G, Ortiz C, Bhandal S, and Gupta P, “Diagnostic accuracy of MR imaging for evaluation of acute appendicitis: a prime prospective study of Canadian pediatric population”.
- Ümmugulsum Bayraktutan et al., “Diagnostic performance of diffusion-weighted MR imaging in detecting acute appendicitis in children: comparison with conventional MRI and surgical findings”.
- Lauren M B Burke et al., “Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study”.
- Michael Burns, Patrick Vos, Cameron J Hague, Pari Tiwari, and Sam M Wiseman, “Utility of Magnetic Resonance Imaging for the Diagnosis of Appendicitis During Pregnancy: A Canadian Experience”.
- Kristine, S. Corkum, Julia E Grabowski, Tolulope A.Oyetunji, Cynthia K. Rigsby, and Timothy B. Lautz, “Absolute neutrophil count as a diagnostic guide for the use of MRI in the workup of suspected appendicitis in children ”.
- C M P Ziedses des Plantes, M J F van Veen, J van der Palen, J M Klaase, H A J Gielkens, and R H Geelkerken, “The Effect of Unenhanced MRI on the Surgeons’ Decision-Making Process in Females with Suspected Appendicitis”.
- Elizabeth H Dibble, Grayson L Baird, David W Swenson, Claudia Cartagena, and Thaddeus W Herliczek, “Effectiveness of a Staged US and Unenhanced MR Imaging Algorithm in the Diagnosis of Pediatric Appendicitis”.
- Ryne A Didier, Fergus V Coakley, Sanjay Krishnaswami, David M Spiro, Bryan R Foster, and Katharine L Hopkins, “Performance characteristics of magnetic resonance imaging without contrast agents or sedation in pediatric appendicitis”.
- Jonathan R Dillman et al., “Equivocal Pediatric Appendicitis: Unenhanced MR Imaging Protocol for Nonsedated Children-A Clinical Effectiveness Study”.
- Donlon N, Cormick P, Larkin J, and Mehigan B, “The use of MRI to diagnose appendicitis during pregnancy”.
- Annabelle L Fonseca, Adrian A Maung, Kevin M Schuster, Lewis J Kaplan, Felix Y Lui, and Kimberly A Davis, “The use of magnetic resonance imaging in the diagnosis of suspected appendicitis in pregnancy: shortened length of stay without an increase in hospital charges”.
- Y Liza Kearl et al., “Accuracy of Magnetic Resonance Imaging and Ultrasound for Appendicitis in Diagnostic and Nondiagnostic Studies”.
- Thomas M Kennedy, Amy D Thompson, Arabinda K Choudhary, Richard J Caplan, Kathleen E Schenker, and Andrew D DePiero, “Utility of applying white blood cell cutoffs to non-diagnostic MRI and ultrasound studies for suspected pediatric appendicitis”.
- Khalil S, Tripathee N, Skaug M, Shiralkar K, and Surabhi V, “Accuracy of unenhanced MR imaging in the detection of perforated acute appendicitis in pediatric patients”.
- Sonja Kinner et al., “Diagnostic Accuracy of MRI Versus CT for the Evaluation of Acute Appendicitis in Children and Young Adults”.
- Jeffrey L Koning, John H Naheedy, and Peter G Kruk, “Diagnostic performance of contrast-enhanced MR for acute appendicitis and alternative causes of abdominal pain in children”.
- Joseph Konrad, David Grand, and Ana Lourenco, “MRI: first-line imaging modality for pregnant patients with suspected appendicitis”.
- Afif N Kulaylat et al., “An implemented MRI program to eliminate radiation from the evaluation of pediatric appendicitis”.
- Ilah Shin, Joon Seok Lim, Chansik An, Myeong-Jin Kim, and Yong Eun Chung, “T1 bright appendix sign to exclude acute appendicitis in pregnant women”.
- Lauren H Theilen et al., “Utility of magnetic resonance imaging for suspected appendicitis in pregnant women”.
- Mai, E. Thieme et al., “Diagnostic accuracy and patient acceptance of MRI in children with suspected appendicitis”.
- 1, 1, 2, Richard Tsai 1, Kathryn J Fowler, Constantine Raptis, Joseph W Owen, and Vincent M Mellnick, “MRI of suspected appendicitis during pregnancy: interradiologist agreement, indeterminate interpretation and the meaning of non-visualization of the appendix”.
- Norihisa Nitta, Kiyoshi Murata, Masashi Takahashi, Akira Furukawa, Masayuki Mori, and Masanobu Fukushima, “MR imaging of the normal appendix and acute appendicitis”.
- Lodewijk Cobben, Emile Coerkamp, Ingrid Groot, Lucas Kingma, Julien Puylaert, and Johan Blickman, “A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on the outcome of appendectomy”.
- Ajay K Singh, Hemali Desai, and Robert A Novelline, “Emergency MRI of acute pelvic pain: MR protocol with no oral contrast”.
- Ercan Inci, Elif Hocaoglu, Ozgur Kilickesmez, Sibel Aydin, Sibel Bayramoglu, and Tan Cimilli, “Utility of diffusion-weighted imaging in the diagnosis of acute appendicitis”.
- Elizaveta Chabanova et al., “Unenhanced MR Imaging in adults with clinically suspected acute appendicitis”.
- Johannes T Heverhagen, Klaus J Klose, Kathrin Pfestroff, Anna E Heverhagen, Katharina Kessler, and Helmut Sitter, “Diagnostic accuracy of magnetic resonance imaging: a prospective evaluation of patients with suspected appendicitis (diamond)”.
- Bin Zhu, Bing Zhang, Ming Li, Shifu Xi, Decai Yu, and Yitao Ding, “An evaluation of a superfast MRI sequence in the diagnosis of suspected acute appendicitis”.
- M M N Leeuwenburgh et al., “Accuracy of MRI compared with ultrasound imaging and selective use of CT to discriminate simply from perforated appendicitis”.
- D J Humes and J Simpson, “Acute appendicitis”.
- J B Puylaert, “Acute appendicitis: US evaluation using graded compression”.
- R B Jeffrey Jr, F C Laing, and R R Townsend, “Acute appendicitis: sonographic criteria based on 250 cases”.
- M M Abu-Yousef, J J Bleicher, J W Maher, L F Urdaneta, E A Franken Jr, and A M Metcalf, “High-resolution sonography of acute appendicitis”.
- M Rioux, “Sonographic detection of the normal and abnormal appendix”.
- E J Balthazar, B A Birnbaum, J Yee, A J Megibow, J Roshkow, and C Gray, “Acute appendicitis: CT and US correlation in 100 patients”.
- K R Curtin, S W Fitzgerald, A A Nemcek Jr, F L Hoff, and R L Vogelzang, “CT diagnosis of acute appendicitis: imaging findings”.
- E J Balthazar, A J Megibow, S E Siegel, and B A Birnbaum, “Appendicitis: prospective evaluation with high-resolution CT”.
- A J Malone Jr, C R Wolf, A S Malmed, and B F Melliere, “Diagnosis of acute appendicitis: the value of unenhanced CT”.
- E J Balthazar, J Roshkow, B A Birnbaum, J Yee, A J Megibow, and C Gray, “Acute appendicitis: CT and US correlation in 100 patients”.
- E J Balthazar, A J Megibow, S E Siegel, and B A Birnbaum, “Appendicitis: prospective evaluation with high-resolution CT”.
- Jesse M Pines, “Trends in the rates of radiography use and important diagnoses in emergency department patients with abdominal pain”.
- Lodewijk Cobben, Emile Coerkamp, Lucas Kingma, Julien Puylaert, Johan Blickman, and Ingrid Groot, “A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on the outcome of appendectomy”.
- C. M. P. Ziedses des Plantes, M. J. F. van Veen, J. van der Palen, J. M. Klaase, H. A. J. Gielkens, and R. H. Geelkerken, “The Effect of Unenhanced MRI on the Surgeons’ Decision-Making Process in Females with Suspected Appendicitis”.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





