1. Introduction
Autoimmune thyroid diseases (AITD) are among the most common autoimmune pathology. Among AITD, Hashimoto’s thyroiditis is the leading one, while Graves’ disease is less common. The main autoantibody (Ab) target proteins in AITD are thyroperoxidase (TPO), an enzyme involved in the biosynthesis of thyroid hormones, thyroid hormone precursor thyroglobulin (Tg) and thyroid hormone receptor. The low molecular weight hormones thyroxine (T4) and 3,5,3’-triiodothyronine (T3) in complex with proteins may also act as targets for Abs [
1]. Abs can be directed against Na/I symporter, megalin, pendrin (PDS) [
2,
3]. Antibodies to pyruvate kinase (PK) and carboanhydrase 2 (CA2) may contribute to thyroid neoplasia development [
4,
5].
Autoantibodies to major thyroid proteins can often be detected in individuals without AITD [
6]. It is unknown whether autoantibody carriers are those who will develop the disease in the future. Prevalence of thyroid Abs in the general population are 8–30% for AbTPO and 5–20% for AbTg [
2]. In differentiated thyroid cancer, the proportion of patients with positive AbTg increases to 25% [
7]. Increased incidence is seen in other autoimmune diseases, particularly AbTPO prevalence in rheumatoid arthritis - 16-37%; in type 1 diabetes mellitus (T1D) - 40%; in celiac disease - 12-30%; AbTg prevalence in rheumatoid arthritis - 12-23%; in T1D, - 30%; in celiac disease - 11-32% [
5].
Currently, autoantibodies are thought to consist of a polyclonal mixture with different affinities for the autoantigen. An additional characterization of a heterogeneous group of detectable autoantibodies that can be obtained by immunoassay is the binding strength of the antibodies to their target antigen resulting from multidimensional affinity interactions. This binding strength is called functional affinity or avidity and is widely used in the diagnosis of infectious diseases to distinguish between primary and chronic forms [
8]. It has now been suggested that in autoimmune diseases, autoantibody avidity may influence their pathogenicity [
9]. The majority of studies investigating autoantibody avidity in autoimmune diseases have focused on systemic diseases such as systemic lupus erythematosus and antiphospholipid syndrome [
10,
11,
12]. A number of studies have been performed on autoantibody avidity in celiac disease and T1D [
13,
14,
15]. Known published data on autoantibody avidity in AITD are extremely limited [
16,
17].
The goal of this study was to evaluate the avidity of autoantibodies associated with thyroid disease in the sera of patients diagnosed with AITD and autoantibody carriers without AITD. Given that the thyroid gland harbors multiple known autoantigens, it seems reasonable to combine the capabilities of multiplex methods for simultaneous detection of the spectrum of autoantibodies to TPO, TG, PDS, CA2, PK, T3 and T4 thyroid hormones with introduction of a new additional characteristic of the detected autoantibodies ˗ determination of avidity index (AI). In the current work, a specialized hydrogel microarray with immobilized proteins was developed and the technique of multiplex analysis of autoantibodies with simultaneous determination of AI of autoantibodies against each of the immobilized thyroid antigens and candidate proteins was implemented.
2. Materials and Methods
2.1. Subjects
The study enrolled 240 adult patients from two independent cohorts: cohort I (n = 117) and cohort II for confirmatory studies (n = 123).
Patient characteristics for cohort I are shown in
Table 1. The mean age of the 117 patients in the cohort was 52.7 (19-84) years. 102 (87.2%) patients were female and 15 (12.8%) were male. The "AITD" group included patients diagnosed with Hashimoto’s thyroiditis (n=28), Graves’ disease (n=2), and patients with a combination of AIT and T1D (n=7). The non-autoimmune thyroid disease group included patients with non-toxic multinodular goiter (n=7), the thyroid nodules (n=7), histologically confirmed papillary and medullary thyroid cancer (n=2). The "healthy" group included patients with no endocrine pathology (autoimmune and non-autoimmune) according to the survey data. The "AbTPO+" group included AbTPO-positive patients as determined by chemiluminescence analysis without ultrasound data.
Patient characteristics for cohort II are shown in
Table 2. The mean age of the 123 patients in the cohort was 41.6 (18-76) years. 105 (85.4%) patients were female, 18 (14.6%) – male. The "AITD only" group included patients diagnosed with Hashimoto’s thyroiditis (n=11) and Graves’ disease (n=8). The "AITD +T1D" group included patients with a combination of AITD and type 1 diabetes mellitus (n=17). The "AITD + other AID" group included patients with a combination of AITD and Addison’s disease and/or Hirata’s disease and/or vitiligo and/or alopecia areata (n=61). The "AITD + PTC" group included patients with a combination of Hashimoto’s thyroiditis and histologically confirmed papillary thyroid cancer (n=6). Patients with type 1 diabetes mellitus without diagnosed AITD were included in the "T1D" group. The "healthy" group included patients with no endocrine pathology (autoimmune and non-autoimmune) according to survey data.
2.2. Microarray manufacturing
Molecular profiling of autoantibodies in serum samples was performed using hydrogel-based low density microarrays [
18]. All proteins were spotted on each microarray slide in quadruplicate. The following proteins were used: TPO and Tg #8TG52 (HyTest, Turku, Finland), Tg # R132, T3-HRP, and T4-HRP (Xema Co., Ltd., Moscow, Russia), PDS, PK, CA2 (Cusabio, Wuhan, China) (
Figure S1). In addition, the microarray structure included empty elements without immobilized proteins in 8 replicates, marker elements and control elements for antibody detection and control of interference of high concentrations of autoantigens in serum (titration of human IgG (Athens Research and Technology, Athens, GA, USA); mouse monoclonal Abs against autoantigens (mAb Tg, mAb TPO, mAb T4, mAb T3 (HyTest, Turku, Finland)).
2.3. Modified multiplex assay
The assay was performed as described previously [
19] with minor modifications. Patient serum samples were diluted 1:100 and applied to microarray elements (100 µl). After incubation with the sample (for two hours, 37 °C), intermediate washing (PBS with 0.1% Tween 20, 20 min), rinsing and drying, 5M urea solution (denaturing conditions) or PBS (control) was applied to the corresponding microarrays, incubated for 10 min and then washed (PBS with 0.1% Tween 20, 20 min). The binding was revealed with anti-human IgG-Cy5.5 (2.5 μg/mL; 50 μL). After overnight incubation at 37 °C, the microarrays were washed (PBS with 0.1% Tween 20, 30 min), rinsed and dried by centrifugation.
2.4. Analysis of fluorescence and interpretation of results
Fluorescence images of microarrays were obtained using a proprietary laser-excited microarray analyzer (Moscow, Russia) [
20]. Fluorescence signals were calculated using proprietary software. For each group of n elements containing the same antigens, the resulting I
n signal value was calculated as the median of the values of four corresponding fluorescence signals. In order to compensate for the influence of the total IgG concentration on the result of the Abs assay, the individual background signal from empty gel elements (I
n/I
ref) was taken into account in the analysis of the results for each sample. Specific signals from element with immobilized antigen I
n that were at least two times greater than the individual background signal of I
ref were considered positive.
2.5. Chemiluminescence immunoassay
The level of AbTPO was determined by chemiluminescent immunoassay on an automated analyzer ARCHITECT i2000 (Abbott, IL, USA). AbTg levels were determined by electrochemiluminescence analysis on a Cobas 6000 automated analyzer (Roche Diagnostics, Mannheim, Germany). Cohort I: AbTPO levels were determined in all samples. Cohort II: AbTPO and AbTg levels were determined in all samples.
2.6. ELISA with a chaotropic agent
For all samples (cohort II) with positive AbTPO and AbTg, avidity index were measured by modified ELISA. Kits from Xema Co., Ltd. (Moscow, Russia) were used. A chaotropic agent incubation step was added to the manufacturer’s standard protocol: after incubation with samples and washing, 100 µl of PBS or 5M urea were added to the respective wells and incubated for 5 min at 37 °C, then washed and further steps were performed without modification.
2.7. Avidity index of autoantibodies
Only samples with positive autoantibodies were included in the calculation of the index. The avidity index for the multiplex immunoassay was calculated by taking the ratio of the fluorescence signals from the elements with the immobilized antigen for the denaturing agent-treated sample to that of the immunoassay buffer-treated sample. For ELISA analysis, we calculated AI in a similar way by using the optical densities of microplate wells that were both treated and untreated with the denaturing agent.
2.8. Data Presentation
Statistical analysis was performed using MedCalc (Ostend, Belgium). Heat map of normalized fluorescent signals from microarray elements was generated using Galaxy server (
https://usegalaxy.org/, accessed on 8 May 2023).
3. Results
3.1. Development of the multiplex avidity assay.
A microarray with immobilized autoantigens TPO, Tg (two proteins from different manufacturers), PDS, CA2, PK and thyroid hormone T3 and T4 conjugated to horseradish peroxidase was constructed according to a previously developed and validated method for multiplex autoantibody assay [
19] (
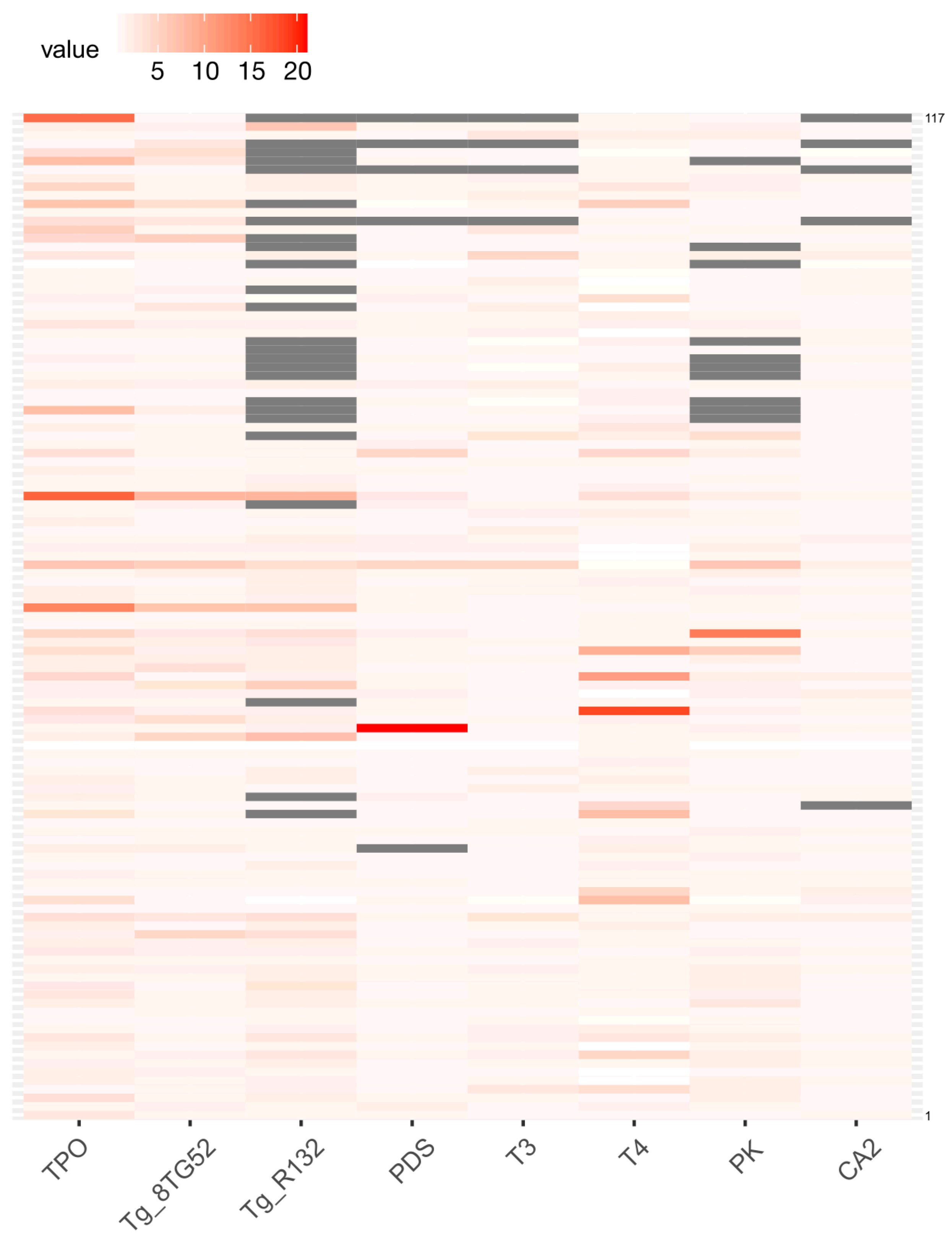
Figure S1). A total of 117 patient serum samples from cohort I were examined using a multiplex platform: AITD patients (n=28), patients with non-autoimmune thyroid diseases (n=16), patients with no endocrine pathology, whether autoimmune or not (n=31), and AbTPO+ patients without thyroid ultrasound investigation (n=42) were included in the study. The multiplex immunoassay revealed that the highest quantity of positive autoantibody signals were obtained from immobilized TPO, Tg and T4 antigens (
Figure 1). For all other antigens, single samples with positive autoantibodies were identified. The results of the multiplex method showed the following frequencies of autoantibodies to different proteins for cohort I: AbTPO 35.0% (41/117); AbTg 23.1% (27/117); AbPDS 3.4% (4/117); AbT3 6.8% (8/117); AbT4 13.7% (16/117); AbCA2 0.85% (1/117); and AbPK 5.1% (6/117).
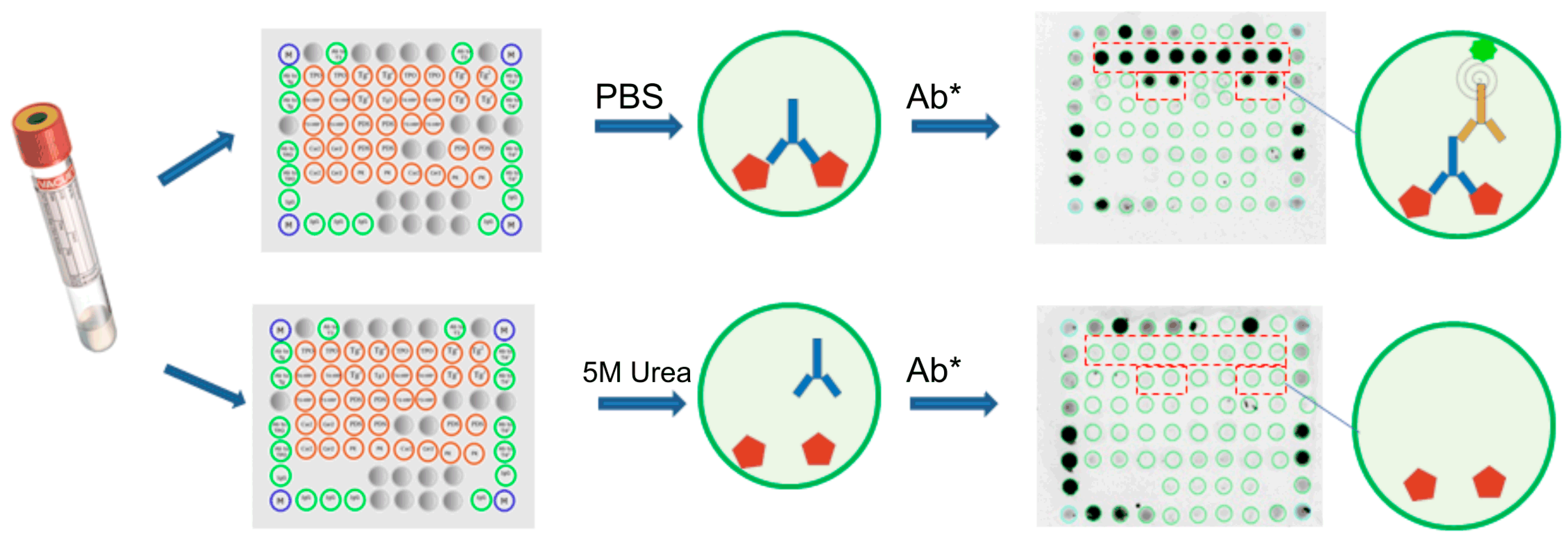
A modified multiplex method was proposed to determine the avidity index of autoantibodies. Three experimental assay schemes were tested: the first scheme consisted in the destruction of weak interactions by a denaturing agent after the formation of the antigen-Ab complex, the second - in the addition of an agent at the stage of incubation with the sample, and the third - in the addition of an disruption agent after the formation of the triple ’’Antigen-Ab-anti-human Ab*’’ complex. Five different denaturants were tested: urea (0.25-10 M), thiourea (0.5-10 M), guanidine thiocyanate (0.5-2 M), sodium chloride (0.4-1 M), and polyethylene glycol (20-80% in phosphate-buffered saline (PBS)). When the sample was tested repeatedly, the use of urea at the stage after the formation of the antigen-Ab complex gave the most reproducible results (coefficient of variation for AI was less than 15%). The fluorescence intensity varied only slightly at urea concentrations ranging from 0 to 4 M and began to decrease at 5 M. Consequently, 5 M urea was selected as the chaotropic agent.
Figure 2 presents a graphical representation of the modified multiplex assay and fluorescence images of hydrogel microarray after sample assay, both with and without a 5 M urea treatment. The treatment with the chaotropic agent removes low avidity antibodies from the resulting antigen-Ab complex. Thus, one microarray detects all autoantibodies in the sample, while the second microarray detects only high-avidity autoantibodies. The measurement of avidity is expressed as the avidity index (AI, %), which is calculated by the ratio of fluorescence intensity from the corresponding immobilized antigen after treatment with a denaturing agent and without treatment.
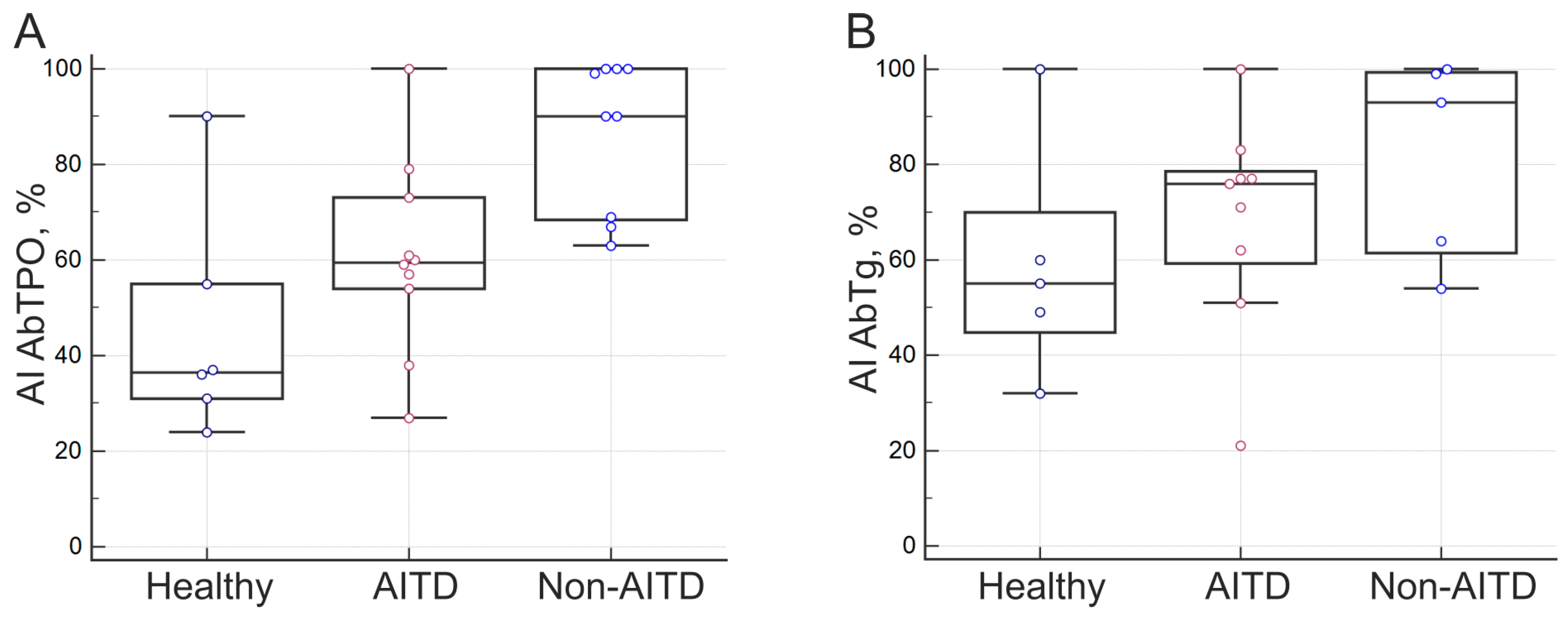
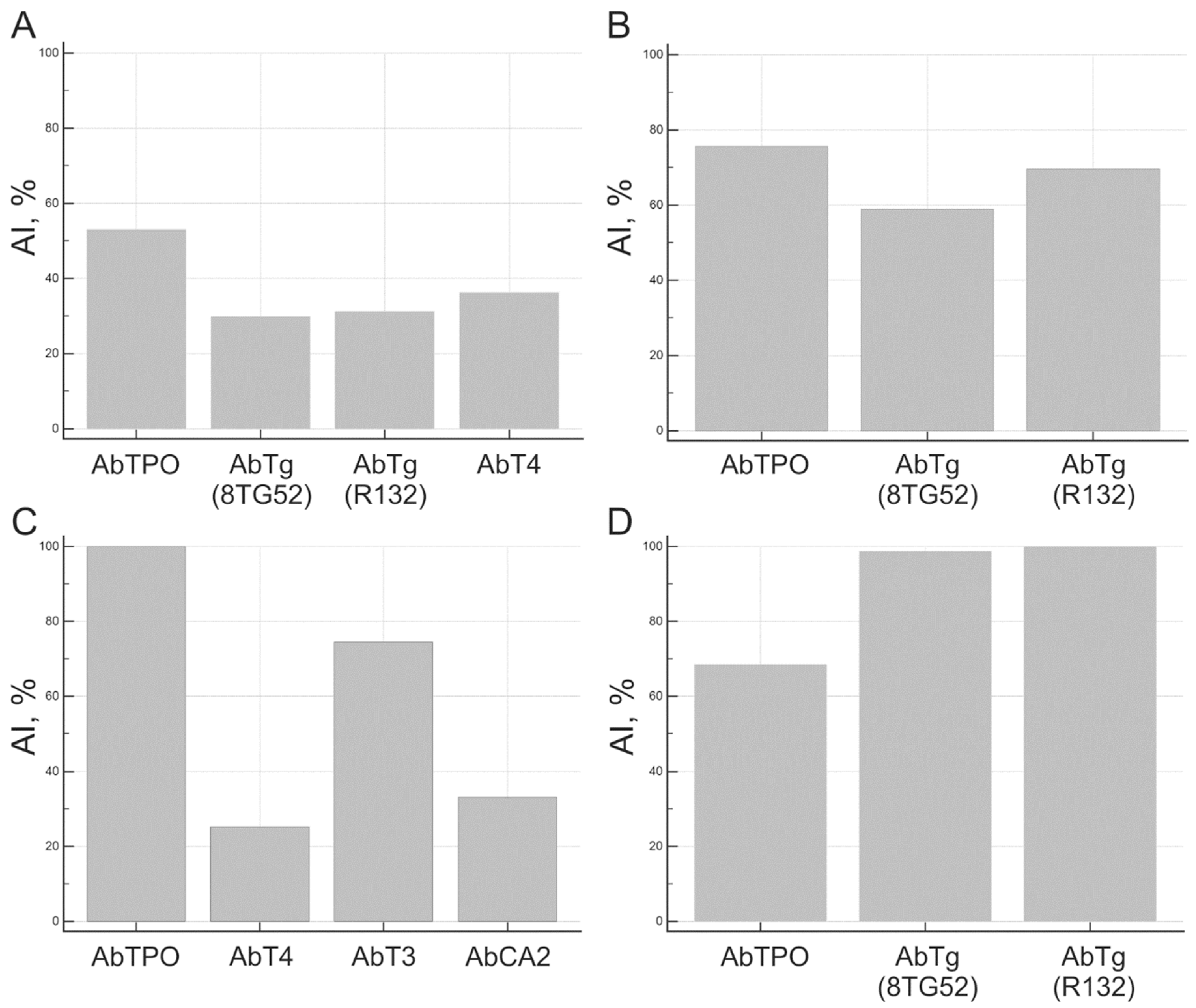
Avidity indexes were calculated for samples positive for at least one autoantibody in the multiplex assay. AI autoantibodies in patient groups with confirmed diagnoses from cohort I (
Figure 3) were compared in terms of AI AbTPO (n=25) and AI AbTg (n=19). For other antigens, avidity indexes were determined for individual samples with positive Ab (total n=19); however, the outcomes showed significant variation.
3.2. Confirmation studies with independent patient cohort
Serum samples from 113 patients (n=103 with AITD, n=10 with T1D) and ten healthy donors from independent cohort II were analyzed using multiplex avidity assay. Subgroups of AITD patients were identified, including those with isolated AITD (n=19), AITD and T1D (n=17), AITD and other endocrine and comorbid autoimmune diseases (n=61), and AITD and papillary thyroid carcinoma (n=6).
The frequencies of autoantibodies targeting different proteins in cohort II, as determined by the multiplex method, were as follows: AbTPO 68.3% (84/123), AbTg 35.8% (44/123), AbPDS 0% (0/123), AbT3 1.6% (2/123), AbT4 8.1% (10/123), AbCA2 0.8% (1/123), AbPK 1.6% (2/123). Avidity indexes were calculated in a multiplex assay for samples positive for at least one autoantibody. Avidity indexes were also measured for AbTPO and AbTg positive samples using a modified enzyme-linked immunosorbent assay (ELISA) by including an additional incubation step with 5M urea or blank buffer to the standard protocol. In cohort II patients, AbTPO and AbTg levels were also measured by chemiluminescent immunoassay (CLIA).
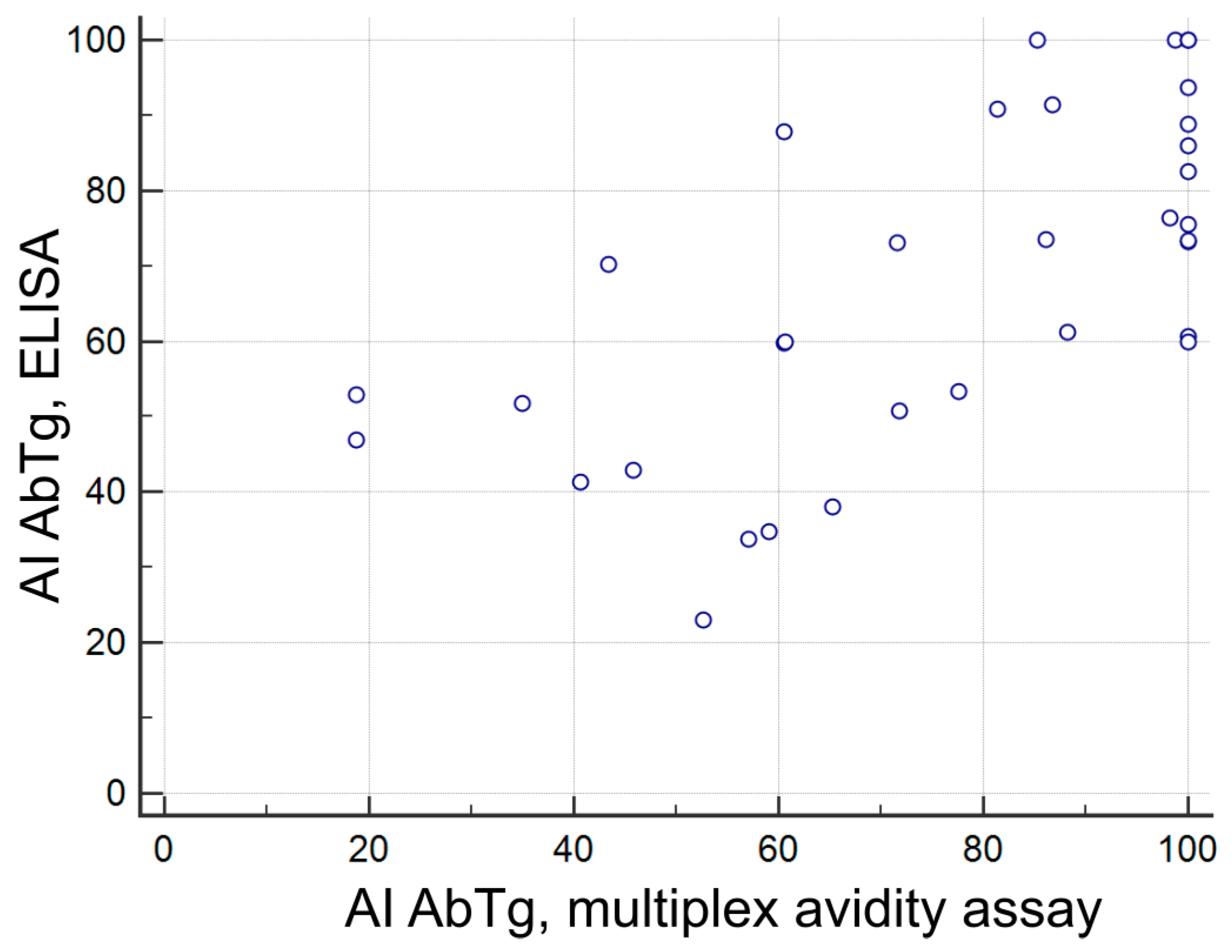
A comparison of AbTg detection results using different methods (multiplex avidity assay, CLIA, and ELISA) revealed a satisfactory correlation. The correlation between CLIA and multiplex avidity assay measurements was r= 0.6412 (p<0.0001, n=121), while the correlation between ELISA and multiplex avidity assay measurements was r= 0.6417 (p<0.0001, n=44). The correlation between the CLIA and ELISA measurements was r=0.6286 (p<0.0001, n=42). A correlation was found between the AbTg avidity score assessed by multiplex avidity assay and ELISA with a positive correlation coefficient of r= 0.6539, p<0.001, and a sample size of n=34 (
Figure 4).
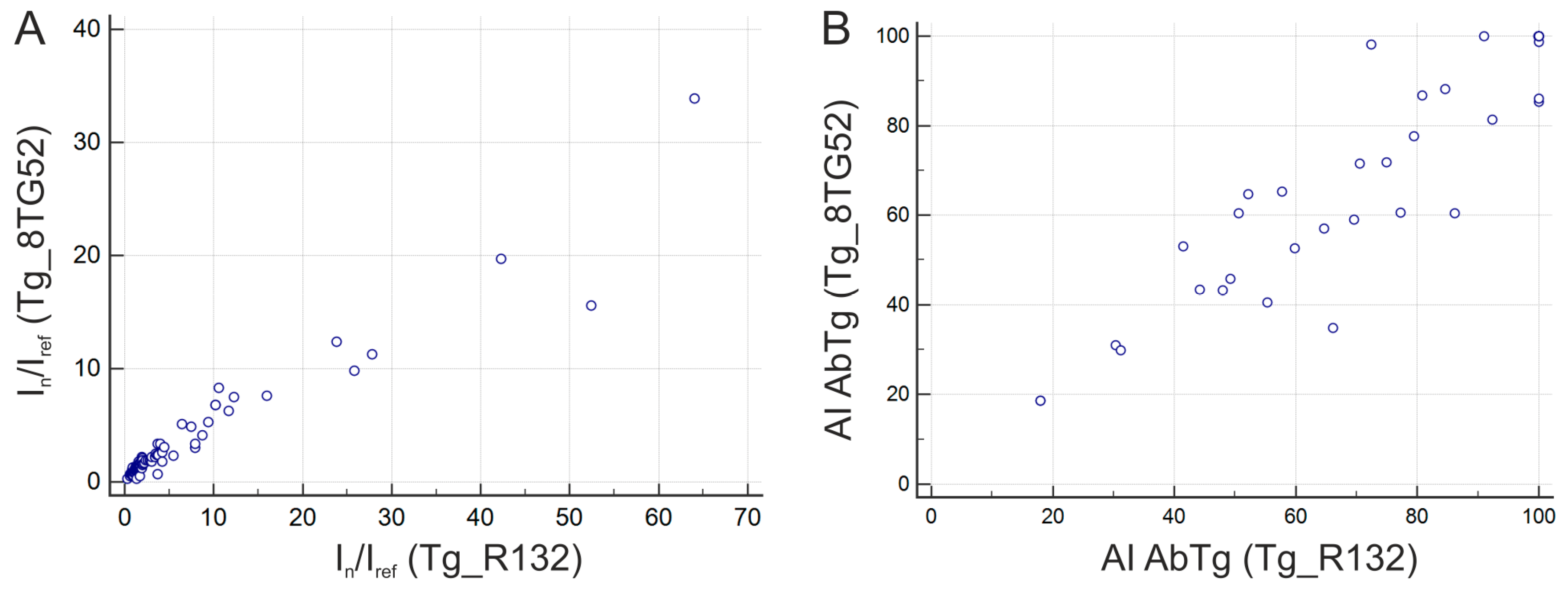
Tg antigens from two different suppliers (Hytest, Finland and Xema Co., Ltd., Moscow, Russia) were used for immobilization on the microarray. The serum sample analysis presented excellent agreement among fluorescence signals obtained from various immobilized preparations (r= 0.9659, p<0.001, n=123) and high agreement when measuring the avidity index of AbTg (r= 0.9266, p<0.001, n=41) (
Figure 5.).
The comparison of AbTPO detection results using three methods demonstrated a satisfactory correlation. The CLIA and multiplex avidity assay measurements showed an r-value of 0.6255 (p<0.0001, n=121). ELISA and multiplex avidity assay measurements had an r-value of 0.5795 (p<0.0001, n=44). Additionally, the CLIA and ELISA measurements yielded an r-value of 0.6286 (p<0.0001, n=42). However, the results for AI AbTPO obtained using two methods (ELISA and multiplex) did not correlate. There was no correlation found between the level of fluorescent signals and AI for either AbTg or AbTPO. For the other antigens (PDS, T3, T4, CA2, PK), single samples with positive autoantibodies were identified; the AI varied in a wide range (23.3-100%).
Differences in autoantibody avidity were studied and found to be personalized to each patient for various thyroid antigens. As an example,
Figure 6 displays the avidity indexes of serum samples analyzed from AITD patients (B, C) and autoantibody carriers (A, D).
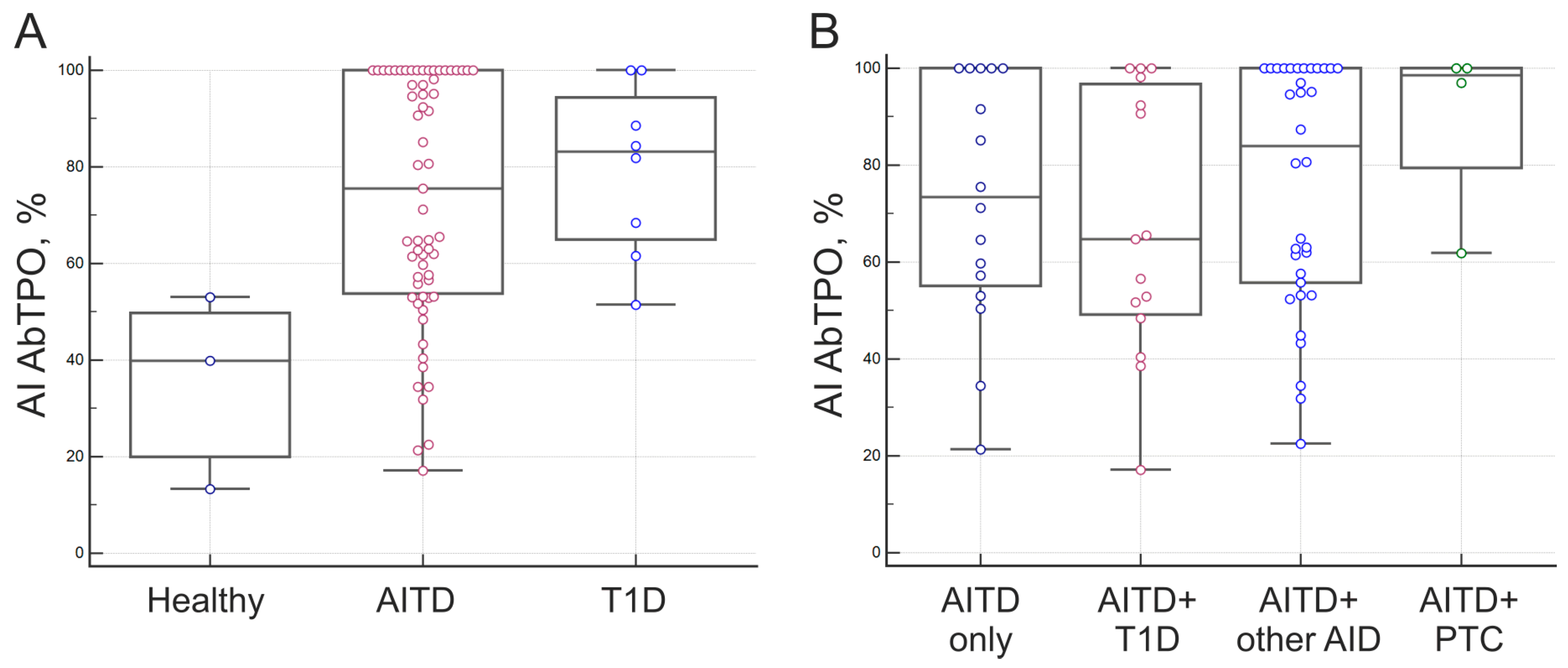
AI was calculated for AbTPO-positive samples from 79 AITD patients and 11 autoantibody carriers from T1D patient groups and healthy donors. The median AI AbTPO were 39.9% for healthy autoantibody carriers, 73.4% for patients with isolated AITD, 64.8-80.6% for patients with other AID combined with AITD, 98.5% for patients with papillary thyroid carcinoma combined with AITD, and 83.2% for patients of autoantibody carriers with type 1 diabetes (T1D) (
Figure 7). The median AI AbTPO difference between the presented groups was found to be statistically significant in the AITD/Healthy (p=0.0223) and T1D/Healthy (p=0.0247) groups, but not in the AITD/T1D groups (p>0.05) (
Figure 7A). Patients with AITD were divided into subgroups based on isolated AITD (AITD only), AITD combined with other autoimmune endocrine and comorbid pathologies (AITD + other AID; AITD + T1D), or thyroid autoimmunity combined with papillary carcinoma (AITD + PTC). There were no significant differences in the medians of AI Ab TPO for these subgroups (p>0.05) (
Figure 7 B).
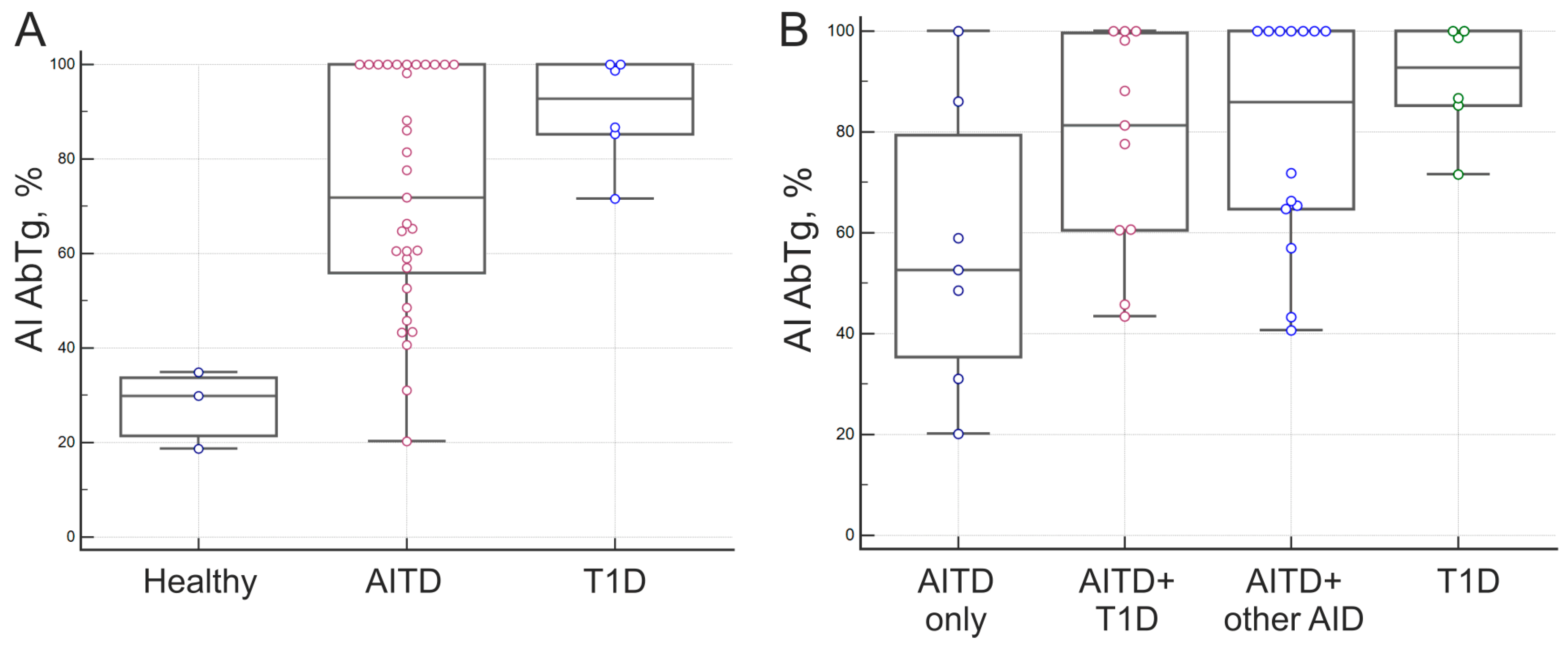
AI values were obtained for AbTg positive samples from patients with AITD (n=35) and autoantibody carriers (n=9) from the T1D patient groups and healthy donors. According to
Figure 8, the median AI values for AbTg were 29.9% in healthy autoantibody carriers, 52.6% in patients with isolated AITD, 81.4-85.9% in patients with combined AITD and other AIDs, and 92.7% in autoantibody positive patients with T1D. The medians of AI AbTg in the presented groups showed statistically significant differences for Healthy/AITD (p=0.0071) and Healthy/T1D (p = 0.0201) groups (
Figure 8A), but not for AITD/T1D groups (P>0.05). Furthermore, patients with T1D had different AI AbTg medians than those with isolated AITD without comorbid pathologies (P=0.0452). Median AI AbTg differences among subgroups of AITD patients were statistically insignificant (P>0.05) (
Figure 8B). The presence of high-avidity autoantibodies to Tg in patients with T1D was also confirmed by a modified ELISA.
4. Discussion
The modified ELISA is the most commonly used method to determine antibody avidity [
8]. There are further studies investigating the use of multiplex assays to quantify antibody avidity in viral infections [
21,
22]. The modified multiplex assay presented in this study is based on indirect autoantibody detection. The methodology involves covalent copolymerization immobilization of antigens in hydrogel elements of a microarray [
18]. Next, a blood serum sample is incubated on the microarray, and fluorescently labeled antibodies against IgG are used to detect autoantibodies in the sample [
19]. In the modified assay, two microarrays are utilized, and a chaotropic agent is incubated after the serum sample on one microarray. The hydrogel microarray element contains covalently immobilized proteins, and exposure to chaotrope selectively releases autoantibodies bound to the immobilized antigen. This procedure facilitates the recognition of autoantibodies with high affinity exclusively. On the control microarray, chaotrope treatment is not performed. The autoantibody avidity index is the percentage of Abs that remain bound to the immobilized antigen after chaotrope treatment.
Resistance to chaotropic agents can evaluate antibody avidity in two ways: elution and dilution. The elution principle involves the addition of a chaotropic agent after the formation of autoantibody-antigen complexes to disrupt weak interactions, whereas the dilution principle involves the addition of a chaotropic agent to the sample prior to the assay to prevent the formation of autoantibody-antigen complexes. The optimal method (eluting Abs from autoantibody-antigen complexes) and agent (5 M urea) were selected based on findings that showed the most consistent results in repeated sample analyses.
The optimal assay scheme was tested using sera from cohort I patients (n=117). AIs were calculated for positive samples of at least one autoantibody. In the present study, no correlation was observed between the level of fluorescence signals and the AI of autoantibodies. This can be attributed to the principle of the method. The indirect ELISA and multiplex methods detect the degree of occupation of immobilized antigen autoantibodies. However, the detectable antigen occupation is not determined solely by antibody concentration, but also their affinity. The same level of occupancy can be reached by increasing the concentration of low affinity antibodies and decreasing the concentration of high affinity antibodies [
23]. However, Sliva et al. noticed a correlation between AbTPO levels and AI in a previous study with a correlation coefficient of 0.444 and a p-value of 0.008 [
16]. Other researchers have also found no correlation between the level and avidity of autoantibodies with respect to anti-beta2-glycoprotein I antibodies [
24] and anti-cardiolipin autoantibodies [
12].
When analyzing AI AbTPO and AI AbTg for cohort I using a small subset of positive samples from patients with known diagnoses, a trend toward increased antibody avidity was observed in the row ’’healthy - patients with AITD - patients with non-autoimmune thyroid disease’’, which included patients with thyroid nodules and malignant thyroid neoplasms. Since the significance of the preliminary findings was restricted by the small number of positive samples from autoantibody carrier patients, a series of confirmatory studies with independent patient cohorts was performed.
Autoantibodies are a complex analyte as they are composed of a mixture of polyclonal immunoglobulins representing various classes. Additionally, polyclonal autoantibodies from serum possess the ability to bind to multiple epitopes of the antigen. Variability can arise in some samples when they are analyzed on different systems due to the use of various automated analysis platforms and protocols. For cohort II in the present study, autoantibodies to the major thyroid autoantigens, TPO and Tg, were additionally analyzed by enzyme-linked immunosorbent assay and chemiluminescent assay. Comparison of fluorescence intensity (multiplex) with the corresponding CLIA and ELISA units revealed a satisfactory correlation between the three methods for AbTg: r= 0.6412, p<0.0001, n=121 (CLIA/ multiplex); r= 0.6417, p<0.0001, n=44 (ELISA/ multiplex); r= 0.6760, p<0.0001, n=42 (CLIA/ ELISA). Moreover, a positive correlation was observed between AI AbTg measured by multiplex and ELISA, which were similarly modified (5 M urea treatment). The multiplex method for measuring avidity provides the benefit of selectively targeting the bonding in the binary complex formed between autoantigen and autoantibody through treatment with a denaturing agent. This leaves the immobilized antigen securely covalent in the hydrogel. Passive adsorption of the protein onto the microplate plastic achieves immobilization in ELISA, which can result in the autoantigen’s detachment from the solid phase when exposed to a denaturing agent. However, the comparison of two modified methods, ELISA and multiplex, revealed an agreement for AI AbTg (r=0.6539; p<0.001, n=34), which was not observed for AI AbTPO. Notably, the correlations between the three methods were also slightly lower for AbTPO: r=0.6255, p<0.0001, n=121 (CLIA/multiplex); r=0.5795, p<0.0001, n=44 (ELISA/multiplex); r=0.6286, p<0.0001, n=42 (CLIA/ELISA). As for cohort I, there was no correlation between fluorescence signal levels and AI for either AbTg or AbTPO.
To assess the impact of various immobilized autoantigen preparations on the level of measured autoantibody avidity, two different proteins for Tg from diverse sources were incorporated into the microarray structure. The AI for AbTg remained consistent regardless of the recombinant proteins employed for immobilization (r= 0.9266, p<0.001, n=41).
In this study, we examined the avidity of various autoantibodies in a single assay for an individual patient. Earlier research highlighted the challenge of comparing results across studies due to the lack of a standardized method for detecting antibody avidity and the absence of a uniform classification of high- and low-avidity antibodies [
8]. The multiplex assay offers an advantage in determining the avidity for different autoantibodies under the same conditions in a single experiment. The consistent assay conditions allow for measuring the variation in the avidity of autoantibodies to different proteins in a single patient. It has been demonstrated that an individual can have both high and low avidity autoantibodies to various proteins in thyroid tissue. For individuals with antibodies, there were differences in median values between the AITD/healthy and T1D/healthy groups. The AI AbTPO exhibited considerable variability within the AITD group. Additional subgrouping of AITD patients based on isolated AITD (AITD only) or combined with other autoimmune endocrine and comorbid pathologies (AITD + other AID; AITD + T1D) or combination of thyroid autoimmunity with papillary carcinoma (AITD + PTC) did not reveal statistically significant differences in median AI AbTPO. Previously, Silva et al. found similar AI AbTPO in patients with subclinical (sH) and overt hypothyroidism (H), despite differing medians between the groups [
16]. The median AI AbTPO for group H was 72.5% (66.75-78.25) and for sH was 48.05% (35.4-63.35). Meanwhile, the healthy control group had a median of 34.53% (32.76-36.30), despite the authors encountering a similar issue of a limited number of autoAT carriers among the investigated healthy control group (only three AbTPO+ patients).
Statistically significant differences in AI AbTg medians were observed when comparing positive samples of AITD patients and autoantibody carriers. The Healthy/AITD and Healthy/T1D groups showed differences in medians. Further categorization of AITD patients into subgroups indicated that patients with T1D and isolated AITD without comorbid pathologies had significant differences in AI AbTg medians (p = 0.0452). All samples obtained from T1D patients with high avidity AbTg detected through the multiplex method demonstrated high avidity when assessed using a modified ELISA. In a prior study, Zhang et al examined AbTg avidity in cohorts of patients with Hashimoto’s thyroiditis, and reduced avidity was observed in patients in a state of euthyroidism in comparison to those with subclinical hypothyroidism and hypothyroidism [
17]. At the same time, it was not possible to compare the results obtained as none of the studied patients had other autoimmune diseases and there was no group of autoantibody carriers without AITD.
One of the limiting factors of this study is the small sample size of non-thyroid patients positive for AbTPO and/or AbTg, as well as the lack of data on disease duration in the included patients with AITD. Nonetheless, despite the small-scale experiments conducted, they successfully demonstrated the feasibility of multiplex detection of autoantibody avidity. The results were confirmed in patient samples from an independent cohort and agreement with an alternative method, a modified ELISA, was also found for AI AbTg. The study revealed the heterogeneous avidity of autoantibodies to thyroid proteins in AITD patients. At the same time, the subgroup of autoantibodies carriers had different median values for the avidity index of major thyroid Abs. Thus, investigating both the spectrum of high-avidity autoantibodies to thyroid proteins in patients with non-thyroid autoimmune pathology, particularly with T1D, as well as low-avidity autoantibodies in healthy carriers, warrants further examination.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org. Figure S1: microarray layout.
Author Contributions
Conceptualization, E.S.; methodology E.S., V.S. and E.K; validation V.S and E.K.; writing—original draft preparation, E.S.; writing—review and editing, D.G.; visualization, E.S. and D.G.; subjects sample collection, clinical data collection, clinical data administration, M.Yu., M.I, N.N. and E.T.; project administration, E.T., D.G.
Funding
This work was supported by a grant from the Russian Science Foundation (project 22-15-00135; microarray manufacturing, multiplex method approbation (cohort I), CLIA assay (cohort I)), by the Ministry of Science and Higher Education of the Russian Federation to the EIMB Center for Precision Genome Editing and Genetic Technologies for Biomedicine under the Federal Research Program for Genetic Technologies Development for 2019-2027 (agreement number 075-15-2019-1660; confirmatory experiments (cohort II), modified ELISA and CLIA assays (cohort II)).
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local ethics committee of the Endocrinology Research Centre, Ministry of Health of Russia, Moscow, Russia (protocol .17 and date of approval 27 September 2017).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent was obtained from the patients for the publication of this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and/or its
Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ni, J.; Long, Y.; Zhang, L.; Yang, Q.; Kou, C.; Li, S.; Li, J.; Zhang, H. High prevalence of thyroid hormone autoantibody and low rate of thyroid hormone detection interference. Journal of Clinical Laboratory Analysis 2022, 36. [Google Scholar] [CrossRef]
- Vargas-uricoechea, H.; Nogueira, J.P.; Pinz, V.; Schwarzstein, D. The Usefulness of Thyroid Antibodies in the Diagnostic Approach to Autoimmune Thyroid Disease. Antibodies 2023, 12. [Google Scholar] [CrossRef]
- Alver, A.; Mentes, A.; Karahan, S.C.; Erem, C.; Keha, E.E.; Arikan, M.K.; Eminag, M.S.; Deger, O. Increased Serum Anti-Carbonic Anhydrase II Antibodies in Patients with Graves ’ Disease. Exp Clin Endocrinol Diabetes 2007, 115, 287–291. [Google Scholar] [CrossRef]
- Feng, C.; Gao, Y.; Wang, C.; Yu, X.; Zhang, W.; Guan, H.; Shan, Z.; Teng, W. Aberrant Overexpression of Pyruvate Kinase m2 is associated with aggressive tumor features and the BRAF mutation in papillary thyroid cancer. Journal of Clinical Endocrinology and Metabolism 2013, 98, 1–10. [Google Scholar] [CrossRef]
- Fröhlich, E.; Wahl, R. Thyroid Autoimmunity: Role of Anti-thyroid Antibodies in Thyroid and Extra-Thyroidal Diseases. Frontiers in Immunology 2017, 8. [Google Scholar] [CrossRef]
- Prummel, M.F.; Wiersinga, W.M. Thyroid peroxidase autoantibodies in euthyroid subjects. Best Practice and Research: Clinical Endocrinology and Metabolism 2005, 19, 1–15. [Google Scholar] [CrossRef]
- Spencer, C. Thyroglobulin antibody ( TgAb ) methods – Strengths, pitfalls and clinical utility for monitoring TgAb-positive patients with differentiated thyroid cancer. Best Practice & Research Clinical Endocrinology & Metabolism 2013, 27, 701–712. [Google Scholar] [CrossRef]
- Correa, V.A.; Rodrigues, T.S.; Portilho, A.I.; Trzewikoswki de Lima, G.; De Gaspari, E. Modified ELISA for antibody avidity evaluation: The need for standardization. Biomedical Journal 2021, 44, 433–438. [Google Scholar] [CrossRef]
- Oostindie, S.C.; Lazar, G.A.; Schuurman, J.; Parren, P.W.H.I. Avidity in antibody effector functions and biotherapeutic drug design. Nature Reviews Drug Discovery 2022, 21, 715–735. [Google Scholar] [CrossRef]
- Yuan, W.; Cao, H.; Wan, P.; Shi, R.; Zhou, S.; Zheng, J. Clinical evaluation of total and high-avidity anti-dsDNA antibody assays for the diagnosis of systemic lupus erythematosus. Lupus 2019, 1–10. [Google Scholar] [CrossRef]
- Zeng, Y.; Lin, Y.; Wang, X.; Zhang, Y.; Peng, F.; Wang, J.J.; Jiang, L.; Liang, S.; Xiao, Y. Assessment of a high-avidity IgG ANAs for the diagnosis and activity prediction of systemic lupus erythematosus. Clinical Rheumatology 2020, 39, 2619–2629. [Google Scholar] [CrossRef]
- Fialová, L.; Kuchař, O.; Petráčková, M.; Malbohan, I.; Zima, T. Avidity of anti-phospholipid antibodies in relation to their levels. Cent Eur J immunol 2020, 45, 136–143. [Google Scholar] [CrossRef]
- Westerlund, A.; Ankelo, M.; Ilonen, J.; Knip, M.; Simell, O.; Hinkkanen, A.E. Absence of avidity maturation of autoantibodies to the protein tyrosine phosphatase-like IA-2 molecule and glutamic acid decarboxylase ( GAD65 ) during progression to type 1 diabetes. Journal of Autoimmunity 2005, 24, 153–167. [Google Scholar] [CrossRef]
- Westerlund, A.; Ankelo, M.; Simell, S.; Ilonen, J.; Knip, M.; Simell, O.; Hinkkanen, A.E. Affinity maturation of immunoglobulin A anti-tissue transglutaminase autoantibodies during development of coeliac disease. Clinical and Experimental Immunology 2007, 148, 230–240. [Google Scholar] [CrossRef]
- Gelderman, K.A.; Drop, A.C.A.D.; Trouw, L.A.; Bontkes, H.J.; Bouma, G.; van Hoogstraten, I.M.W.; von Blomberg, B.M.E. Serum autoantibodies directed against transglutaminase-2 have a low avidity compared with alloantibodies against gliadin in coeliac disease. Clinical and Experimental Immunology 2014, 177, 86–93. [Google Scholar] [CrossRef]
- Silva, L.M.; Chavez, J.; Canalli, M.H.B.; Zanetti, C.R. Determination of IgG subclasses and avidity of antithyroid peroxidase antibodies in patients with subclinical hypothyroidism - a comparison with patients with overt hypothyroidism. Horm Res Paediatr. 2003, 59, 118–124. [Google Scholar] [CrossRef]
- Zhang, Y.; Gao, Y.; Li, M.; Xie, L.; Huang, Y.; Gao, Y.; Guo, X. Avidity of thyroglobulin antibody in sera from patients with Hashimoto’s thyroiditis with different thyroid functional status. Clinical and Experimental Immunology 2010, 161, 65–70. [Google Scholar] [CrossRef]
- Gryadunov, D.A.; Shaskolskiy, B.L.; Nasedkina, T. V.; Rubina, A.Y.; Zasedatelev, A.S. The EIMB Hydrogel Microarray Technology: Thirty Years Later. Acta Naturae 2018, 10, 4–18. [Google Scholar] [CrossRef]
- Savvateeva, E.N.; Yukina, M.Y.; Nuralieva, N.F.; Filippova, M.A.; Gryadunov, D.A.; Troshina, E.A. Multiplex Autoantibody Detection in Patients with Autoimmune Polyglandular Syndromes. International Journal of Molecular Sciences 2021, 22, 5502. [Google Scholar] [CrossRef]
- Lysov, Y.; Barsky, V.; Urasov, D.; Urasov, R.; Cherepanov, A.; Mamaev, D.; Yegorov, Y.; Chudinov, A.; Surzhikov, S.; Rubina, A.; et al. Microarray analyzer based on wide field fluorescent microscopy with laser illumination and a device for speckle suppression. Biomedical Optics Express 2017, 8, 4798. [Google Scholar] [CrossRef]
- Brady, A.M.; Unger, E.R.; Panicker, G. Description of a novel multiplex avidity assay for evaluating HPV antibodies. Journal of Immunological Methods 2017, 447, 31–36. [Google Scholar] [CrossRef]
- Ssewanyana, I.; Rek, J.; Rodriguez, I.; Wu, L.; Arinaitwe, E.; Nankabirwa, J.I.; Beeson, J.G.; Mayanja-kizza, H.; Rosenthal, P.J.; Dorsey, G.; et al. Impact of a Rapid Decline in Malaria Transmission on Antimalarial IgG Subclasses and Avidity. 2021, 11, 1–13. [CrossRef]
- Prechl, J. Why current quantitative serology is not quantitative and how systems immunology could provide solutions. Biologia Futura 2021, 72, 37–44. [Google Scholar] [CrossRef]
- Čučnik, S.; Kveder, T.; Artenjak, A.; Gallova, Z.U.; Swadzba, J.; Musial, J.; Iwaniec, T.; Stojanovich, L.; Alessandri, C.; Valesini, G.; et al. Avidity of anti-β2-glycoprotein i antibodies in patients with antiphospholipid syndrome. Lupus 2012, 21, 764–765. [Google Scholar] [CrossRef]
Figure 1.
Heat map displaying the fluorescent signals obtained from microarray elements with immobilized autoantigens after sample analysis (n=117). The signals are normalized and scaled by row.
Figure 1.
Heat map displaying the fluorescent signals obtained from microarray elements with immobilized autoantigens after sample analysis (n=117). The signals are normalized and scaled by row.
Figure 2.
Multiplex autoantibody avidity assay. Serum sample is added to two microarrays with immobilized autoantigens and incubated to capture the target autoantibodies. Following this, one microarray was incubated with 5 M urea for 10 minutes, while the other was incubated with a blank buffer (PBS - phosphate-buffered saline). Autoantibody binding is detected using fluorescently labeled anti-human IgG (Ab*).
Figure 2.
Multiplex autoantibody avidity assay. Serum sample is added to two microarrays with immobilized autoantigens and incubated to capture the target autoantibodies. Following this, one microarray was incubated with 5 M urea for 10 minutes, while the other was incubated with a blank buffer (PBS - phosphate-buffered saline). Autoantibody binding is detected using fluorescently labeled anti-human IgG (Ab*).
Figure 3.
Avidity indexes (%) for different patient groups: (A) for AbTPO, (B) for AbTg. Abbreviations: AITD - autoimmune thyroid disorders; non-AITD – non-autoimmune thyroid disorders.
Figure 3.
Avidity indexes (%) for different patient groups: (A) for AbTPO, (B) for AbTg. Abbreviations: AITD - autoimmune thyroid disorders; non-AITD – non-autoimmune thyroid disorders.
Figure 4.
Autoantibody avidity index (AI, %) in multiplex avidity assay and ELISA for AbTg (r= 0.6539, p<0.001, n=34).
Figure 4.
Autoantibody avidity index (AI, %) in multiplex avidity assay and ELISA for AbTg (r= 0.6539, p<0.001, n=34).
Figure 5.
Comparison of serum sample results for two different immobilized Tg preparations (8TG52 and R132): (A) Normalized fluorescence signals In/Iref obtained from the respective immobilized Tg preparations (r= 0.9659, p<0.001, n=123); (B) Avidity indexes (AI, %) calculated for positive results (r= 0.9266, p<0.001, n=41).
Figure 5.
Comparison of serum sample results for two different immobilized Tg preparations (8TG52 and R132): (A) Normalized fluorescence signals In/Iref obtained from the respective immobilized Tg preparations (r= 0.9659, p<0.001, n=123); (B) Avidity indexes (AI, %) calculated for positive results (r= 0.9266, p<0.001, n=41).
Figure 6.
Avidity index of autoantibodies to different thyroid antigens for individual patients: (A) Healthy donor; (B) Hashimoto’s thyroiditis; (C) Grave’s disease, and (D) Type 1 diabetes mellitus.
Figure 6.
Avidity index of autoantibodies to different thyroid antigens for individual patients: (A) Healthy donor; (B) Hashimoto’s thyroiditis; (C) Grave’s disease, and (D) Type 1 diabetes mellitus.
Figure 7.
Avidity of autoantibodies to TPO: (A) ˗ for groups of patients with autoimmune thyroid disease (AITD), autoantibody carriers - healthy and patients with type 1 diabetes mellitus (T1D); (B) ˗ distribution of AI AbTPO within the group of patients with AITD: isolated AITD (AITD only), AITD combined with T1D (AITD+T1D),AITD combined with other endocrine and comorbid autoimmune diseases excluding T1D (AITD+other AID), and patients with papillary thyroid carcinoma and AITD (AITD+PTC).
Figure 7.
Avidity of autoantibodies to TPO: (A) ˗ for groups of patients with autoimmune thyroid disease (AITD), autoantibody carriers - healthy and patients with type 1 diabetes mellitus (T1D); (B) ˗ distribution of AI AbTPO within the group of patients with AITD: isolated AITD (AITD only), AITD combined with T1D (AITD+T1D),AITD combined with other endocrine and comorbid autoimmune diseases excluding T1D (AITD+other AID), and patients with papillary thyroid carcinoma and AITD (AITD+PTC).
Figure 8.
Avidity of autoantibodies to Tg: (A) ˗ for autoimmune thyroid disease (AITD) patient groups, autoAT carriers - healthy and patients with type 1 diabetes mellitus (T1D); and (B) distribution of AI AbTg among the AITD patient group, which includes isolated AITD (AITD only), AITD combined with other endocrine and comorbid AIDs except type I diabetes mellitus (AIT + other AIDs), and AITD combined with type I diabetes mellitus (AITD + T1D).
Figure 8.
Avidity of autoantibodies to Tg: (A) ˗ for autoimmune thyroid disease (AITD) patient groups, autoAT carriers - healthy and patients with type 1 diabetes mellitus (T1D); and (B) distribution of AI AbTg among the AITD patient group, which includes isolated AITD (AITD only), AITD combined with other endocrine and comorbid AIDs except type I diabetes mellitus (AIT + other AIDs), and AITD combined with type I diabetes mellitus (AITD + T1D).
Table 1.
Patient characteristics of the cohort I.
Table 1.
Patient characteristics of the cohort I.
| Group |
n |
Mean age (range) |
Female |
Male |
| AITD |
28 |
54.5 (19-84) |
24 (85.7%) |
4 (14.3%) |
| Non-AITD |
16 |
52.7 (24-74) |
15 (93.75%) |
1 (6.25%) |
| Healthy |
31 |
51.0 (21-68) |
24 (77.4%) |
7 (22.6%) |
| AbTPO+ |
42 |
53.9 (21-81) |
39 (92.9%) |
3 (7.1%) |
| Total |
117 |
52.7 (19-84) |
102 (87.2%) |
15 (12.8%) |
Table 2.
Patient characteristics of the cohort II.
Table 2.
Patient characteristics of the cohort II.
| Group |
n |
Mean age (range) |
Female |
Male |
| AITD only |
19 |
45.4 (18-76) |
18 (94.7%) |
1(5.3%) |
| AITD +T1D |
17 |
39.4 (20-75) |
14 (82.3%) |
3 (17.7%) |
| AITD +others AID |
61 |
41.9 (20-76) |
56 (91.8%) |
5 (8.2%) |
| AITD + PTC |
6 |
46.2 (20-69) |
5 (83.3%) |
1 (16.7%) |
| T1D |
10 |
34.3 (19-45) |
5 (50%) |
5 (50%) |
| Healthy |
10 |
43.7 (22-66) |
8 (80%) |
2 (20%) |
| Total |
123 |
41.6 (18-76) |
105 (85.4%) |
18 (14.6%) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).