Submitted:
09 November 2023
Posted:
13 November 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and methods
Study Design
Assessment of Nutritional Status
- 1)
- Serum laboratory parameters: hemoglobin (g/dl), lymphocytes(/nl), albumin(g/dl), pre-albumin (mg/l), transferrin (mg/dl), and C-reactive protein (CRP) (mg/dl).
- 2)
- Body mass index (BMI) and nutritional risk index (NRI) calculations were based on the following formulas: BMI= weight(kg)/(height(m))2 and NRI= (1.489 x Serum Albumin g/l) + 41.7 x (current weight/ usual weight) [12].
- 3)
- Nutritional Risk Screening Score (NRS-2002), a validated score, was determined in each patient to classify the risk for malnutrition [23]. We classified the patients with a score of ≥3 as high-risk for malnutrition.
- 4)
- Bio-electrical Impedance Analysis (BIA) is a relatively simple, inexpensive and non-invasive technique to measure body composition [24]. Each patient underwent BIA to measure body composition.
Intra- and Post-operative Data Collection
Statistical Analysis
Results
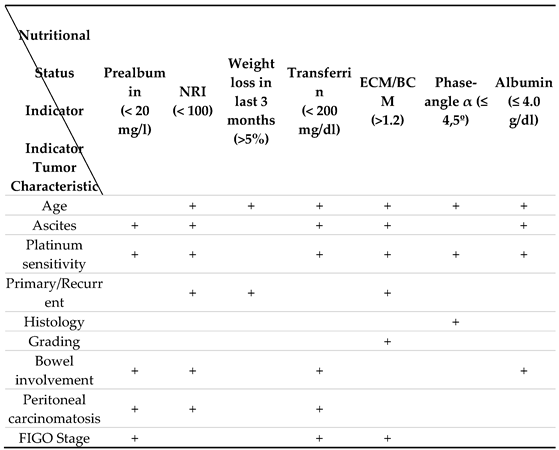
Risk Factors for Malnutrition
Predictive Value of Malnutrition
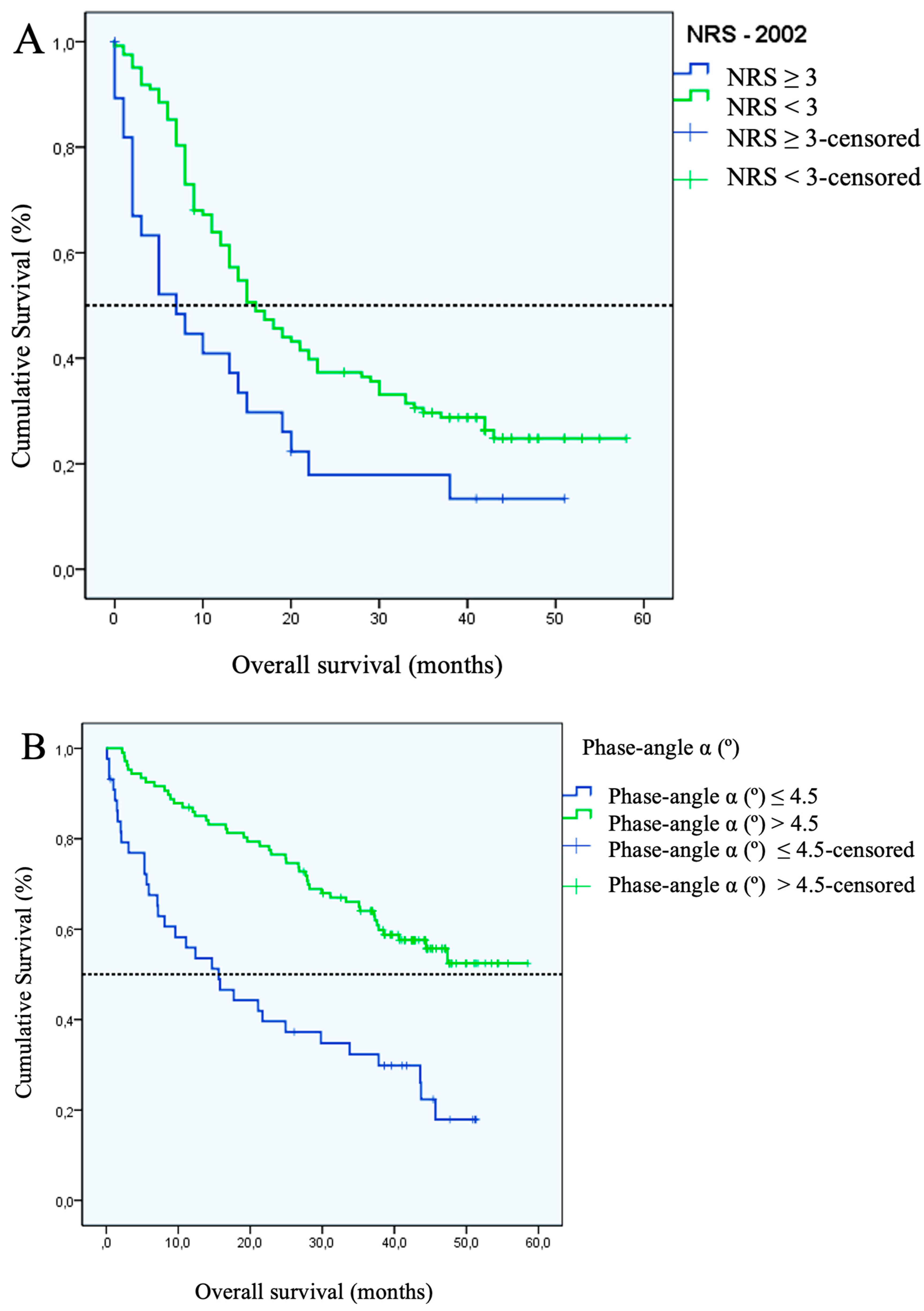
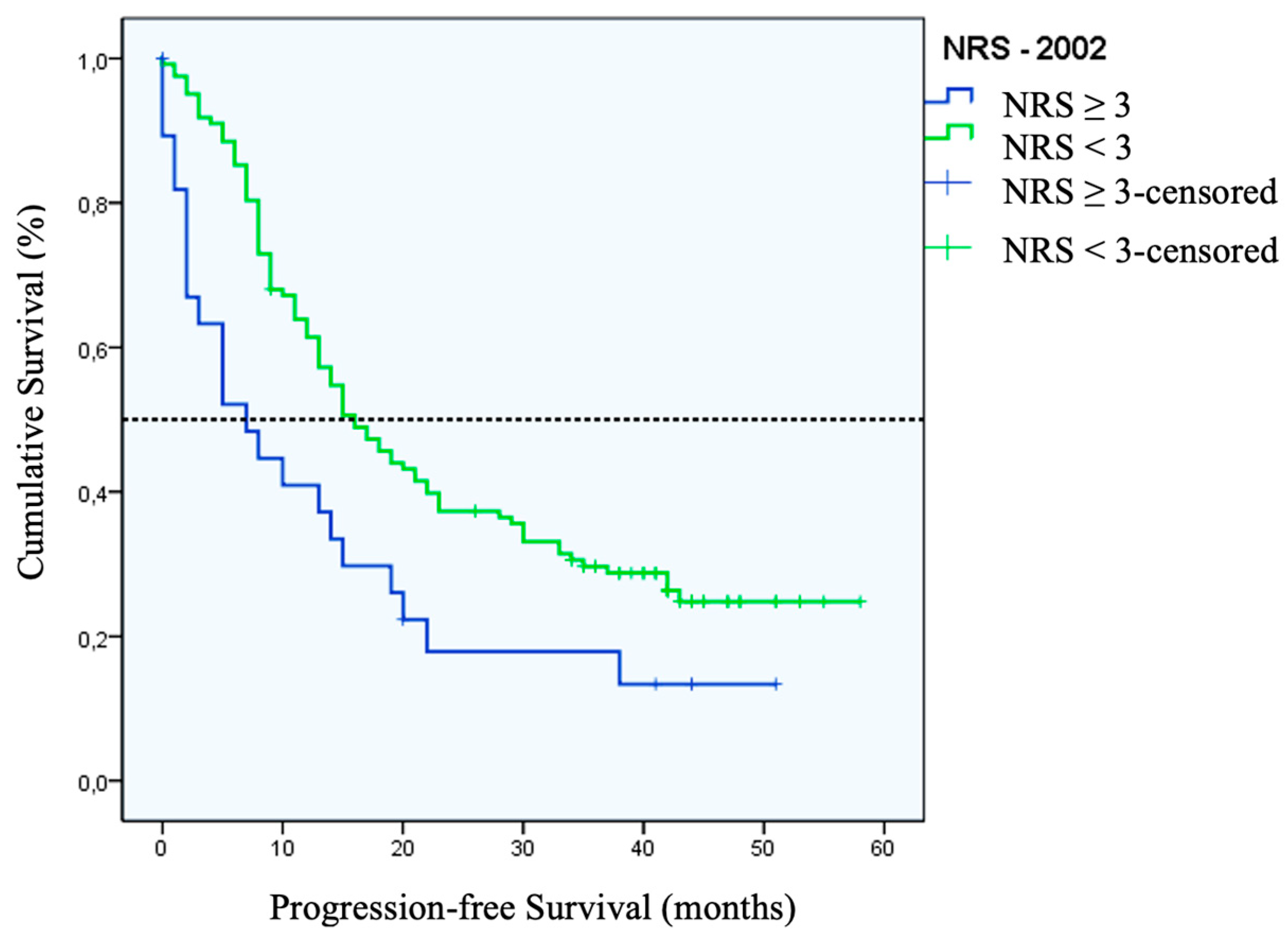
Prognostic Value of Malnutrition
Discussion
Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Polanski: J., et al., Relationship between Nutritional Status and Clinical Outcome in Patients Treated for Lung Cancer. Nutrients, 2021. 13(10). [CrossRef]
- Brinksma, A., et al., Malnutrition is associated with worse health-related quality of life in children with cancer. Support Care Cancer, 2015. 23(10): p. 3043-52. [CrossRef]
- Zhang, Q., et al., Prevalence and Prognostic Value of Malnutrition Among Elderly Cancer Patients Using Three Scoring Systems. Front Nutr, 2021. 8: p. 738550. [CrossRef]
- Albrecht, J.T. and T.W. Canada, Cachexia and anorexia in malignancy. Hematol Oncol Clin North Am, 1996. 10(4): p. 791-800. [CrossRef]
- Dewys, W.D., et al., Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med, 1980. 69(4): p. 491-7.
- Nitenberg, G. and B. Raynard, Nutritional support of the cancer patient: issues and dilemmas. Crit Rev Oncol Hematol, 2000. 34(3): p. 137-68. [CrossRef]
- Santoso, J.T., et al., Prognostic nutritional index in relation to hospital stay in women with gynecologic cancer. Obstet Gynecol, 2000. 95(6 Pt 1): p. 844-6.
- Ravasco, P., et al., Nutritional deterioration in cancer: the role of disease and diet. Clin Oncol (R Coll Radiol), 2003. 15(8): p. 443-50. [CrossRef]
- Shike, M., Nutrition therapy for the cancer patient. Hematol Oncol Clin North Am, 1996. 10(1): p. 221-34. [CrossRef]
- Pressoir, M., et al., Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer, 2010. 102(6): p. 966-71. [CrossRef]
- Caccialanza, R., et al., Nutritional Support in Cancer Patients: A Position Paper from the Italian Society of Medical Oncology (AIOM) and the Italian Society of Artificial Nutrition and Metabolism (SINPE). J Cancer, 2016. 7(2): p. 131-5. [CrossRef]
- Buzby, G.P., et al., Study protocol: a randomized clinical trial of total parenteral nutrition in malnourished surgical patients. Am J Clin Nutr, 1988. 47(2 Suppl): p. 366-81. [CrossRef]
- Sung, H., et al., Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin, 2021. 71(3): p. 209-249. [CrossRef]
- Laky, B., et al., Malnutrition among gynaecological cancer patients. Eur J Clin Nutr, 2007. 61(5): p. 642-6. [CrossRef]
- Gupta, D., et al., Impact of improved nutritional status on survival in ovarian cancer. Support Care Cancer, 2010. 18(3): p. 373-81. [CrossRef]
- Kathiresan, A.S., et al., Malnutrition as a predictor of poor postoperative outcomes in gynecologic cancer patients. Arch Gynecol Obstet, 2011. 284(2): p. 445-51. [CrossRef]
- Tunca, J.C., Nutritional evaluation of gynecologic cancer patients during initial diagnosis of their disease. Am J Obstet Gynecol, 1983. 147(8): p. 893-6. [CrossRef]
- Alphs, H.H., et al., Predictors of surgical outcome and survival among elderly women diagnosed with ovarian and primary peritoneal cancer. Gynecol Oncol, 2006. 103(3): p. 1048-53. [CrossRef]
- Ottery, F.D., Cancer cachexia: prevention, early diagnosis, and management. Cancer Pract, 1994. 2(2): p. 123-31.
- Phippen, N.T., et al., Evaluation of the Patient-Generated Subjective Global Assessment (PG-SGA) as a predictor of febrile neutropenia in gynecologic cancer patients receiving combination chemotherapy: a pilot study. Gynecol Oncol, 2011. 123(2): p. 360-4. [CrossRef]
- Asher, V., J. Lee, and A. Bali, Preoperative serum albumin is an independent prognostic predictor of survival in ovarian cancer. Med Oncol, 2012. 29(3): p. 2005-9. [CrossRef]
- Gupta, D., et al., Can subjective global assessment of nutritional status predict survival in ovarian cancer? J Ovarian Res, 2008. 1(1): p. 5. [CrossRef]
- Kondrup, J., et al., Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr, 2003. 22(3): p. 321-36. [CrossRef]
- Jackson, A.A., et al., Body composition assessment in nutrition research: value of BIA technology. Eur J Clin Nutr, 2013. 67 Suppl 1: p. S71-8. [CrossRef]
- Sehouli, J., et al., ["IMO"--intraoperative mapping of ovarian cancer]. Zentralbl Gynakol, 2003. 125(3-4): p. 129-35.
- Sehouli J, Mustea A, Konsgen D, Lichtenegger W. [Conventional and experimental prognostic factors in ovarian cancer] Zentralbl.Gynakol. 2004;126:315-22.
- Cascio, B.L. and J.V. Logomarsino, Evaluating the effectiveness of five screening tools used to identify malnutrition risk in hospitalized elderly: A systematic review. Geriatr Nurs, 2018. 39(1): p. 95-102. [CrossRef]
- Pirlich, M., et al., The German hospital malnutrition study. Clin Nutr, 2006. 25(4): p. 563-72. [CrossRef]
- Dolz, C., et al., Ascites increases the resting energy expenditure in liver cirrhosis. Gastroenterology, 1991. 100(3): p. 738-44. [CrossRef]
- Kuhn, W.C., Therapy for recurrent ovarian cancer. Curr Womens Health Rep, 2003. 3(1): p. 33-8.
- Eisenkop, S.M. and N.M. Spirtos, The clinical significance of occult macroscopically positive retroperitoneal nodes in patients with epithelial ovarian cancer. Gynecol Oncol, 2001. 82(1): p. 143-9. [CrossRef]
- Zhang, W., et al., Preoperative prognostic nutritional index is a powerful predictor of prognosis in patients with stage III ovarian cancer. Sci Rep, 2017. 7(1): p. 9548. [CrossRef]
- Lieffers, J.R., et al., A viscerally driven cachexia syndrome in patients with advanced colorectal cancer: contributions of organ and tumor mass to whole-body energy demands. Am J Clin Nutr, 2009. 89(4): p. 1173-9. [CrossRef]
- Cao, D.X., et al., Resting energy expenditure and body composition in patients with newly detected cancer. Clin Nutr, 2010. 29(1): p. 72-7. [CrossRef]
- Elattar, A., et al., Optimal primary surgical treatment for advanced epithelial ovarian cancer. Cochrane Database Syst Rev, 2011(8): p. CD007565. [CrossRef]
- Fotopoulou, C., et al., Primary radical surgery in elderly patients with epithelial ovarian cancer: analysis of surgical outcome and long-term survival. Int J Gynecol Cancer, 2010. 20(1): p. 34-40. [CrossRef]
- Fotopoulou, C., et al., Surgical outcome and survival analysis of young patients with primary epithelial ovarian cancer. Anticancer Res, 2009. 29(7): p. 2809-15.
- Fotopoulou, C., et al., Can complete tumor resection be predicted in advanced primary epithelial ovarian cancer? A systematic evaluation of 360 consecutive patients. Eur J Surg Oncol, 2010. 36(12): p. 1202-10. [CrossRef]
- Sehouli, J., et al., Intra-abdominal tumor dissemination pattern and surgical outcome in 214 patients with primary ovarian cancer. J Surg Oncol, 2009. 99(7): p. 424-7. [CrossRef]
- Gil-Ibanez, B., et al., Predictive factors in relapsed ovarian cancer for complete tumor resection. Anticancer Res, 2011. 31(8): p. 2583-7.
- Tian, W.J., et al., A risk model for secondary cytoreductive surgery in recurrent ovarian cancer: an evidence-based proposal for patient selection. Ann Surg Oncol, 2012. 19(2): p. 597-604. [CrossRef]
- Al-Refaie, W.B., et al., Blood transfusion and cancer surgery outcomes: a continued reason for concern. Surgery, 2012. 152(3): p. 344-54. [CrossRef]
- Nielsen, H.J., Detrimental effects of perioperative blood transfusion. Br J Surg, 1995. 82(5): p. 582-7. [CrossRef]
- Golub, R., et al., A multivariate analysis of factors contributing to leakage of intestinal anastomoses. J Am Coll Surg, 1997. 184(4): p. 364-72. [PubMed]
- Barbosa-Silva, M.C. and A.J. Barros, Bioelectric impedance and individual characteristics as prognostic factors for post-operative complications. Clin Nutr, 2005. 24(5): p. 830-8. [CrossRef]
- Makela, J.T., et al., Morbidity and mortality after abdominal operations for cancer. Hepatogastroenterology, 1992. 39(5): p. 420-3. [PubMed]
- Laky, B., et al., Pretreatment malnutrition and quality of life - association with prolonged length of hospital stay among patients with gynecological cancer: a cohort study. BMC Cancer, 2010. 10: p. 232. [CrossRef]
- Van Cutsem, E. and J. Arends, The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs, 2005. 9 Suppl 2: p. S51-63. [CrossRef]
- Sehouli, J., et al., Effects of sarcopenia and malnutrition on morbidity and mortality in gynecologic cancer surgery: results of a prospective study. J Cachexia Sarcopenia Muscle, 2021. 12(2): p. 393-402. [CrossRef]
| Characteristic | Number (%) |
|---|---|
| Age (years) | 56 (19 – 84)* |
| Weight (kg) | 65 (45 – 141)* |
| BMI (kg/m²) | 24,4 (17,8 – 48,8)* |
| Primary OC | 79 (52.0) |
| FIGO Staging (Primary OC only) | |
| I | 8 (10.3) |
| II | 8 (10.3) |
| III | 39 (50) |
| IV | 22 (28.2) |
| Unknown | 2 (2.5) |
| Recurrent OC | 73 (48.0) |
| Platin Response (Recurrent OC only) | |
| Platin sensitive | 48 (65.8) |
| Platin resistant | 25 (34.2) |
| Grading | |
| I | 4 (2.6) |
| II | 40 (26.3) |
| III | 82 (53.9) |
| Unknown | 26 (17.1) |
| Histology | |
| Serous | 119 (78.3) |
| Endometrioid | 7 (4.6) |
| Mucinous | 6 (3.9) |
| Clear cell | 7 (4.6) |
| Other | 3 (2.0) |
| Unknown | 10 (6.6) |
| Ascites | |
| ≥ 500 ml | 26 (17.1) |
| < 500 ml | 49 (32.2) |
| No ascites | 75 (49.3) |
| Unknown | 2 (1.3) |
| Tumor Spread | |
| Small bowel involvement | 56 (36.8) |
| Large bowel involvement | 83 (54.6) |
| Peritoneal carcinomatosis | 120 (78.9) |
| Residual Tumor | |
| None | 94 (61.8) |
| ≤ 1 cm | 30 (19.8) |
| > 1 cm | 28 (17.7) |
| Nutritional Status Indicator* | Cut-off value for malnutrition | Number (%) | Area under the ROC curve | Sensitivity (%) |
Specificity (%) |
CI (95%) |
|---|---|---|---|---|---|---|
| NRS–2002 | ≥ 3 | 28 (18.4) | NA | NA | NA | NA |
| Prealbumin (mg/l) | < 20 | 51 (37.2) | 0,807 | 77.8 | 72.7 | 0.708-0.906 |
| NRI | < 100 | 47 (31.8) | 0,801 | 67.9 | 76.7 | 0.707-0.896 |
| Weight Loss in last 3 months (%) | > 5 | 29 (19.1) | 0,780 | 64.3 | 91.1 | 0.665-0.895 |
| Transferrin (mg/dl) | < 200 | 41 (28.1) | 0,785 | 65.4 | 80 | 0.680-0.890 |
| ECM/BCM Ratio | > 1,2 | 58 (38.4) | 0,762 | 77.8 | 70.2 | 0.653-0.871 |
| Phase-angle α (º) | ≤ 4,5 | 44 (29.1) | 0,760 | 66.7 | 79 | 0.651-0.869 |
| Albumin (g/dl) | ≤ 4,0 | 53 (35.3) | 0,769 | 75 | 73.8 | 0.665-0.872 |
| Characteristic | Label | Total (n=152) (%) |
Patients with NRS ≥ 3 (n=28) (%) |
p-Value |
|---|---|---|---|---|
| Age | > 65 years | 42 (27,6) | 13 (46,4) | p = 0.014 |
| ≤ 65 years | 110 (72,3) | 15 (53,6) | ||
| Diagnosis | Primary | 79 (51,9) | 18 (64,3) | NS |
| Recurrent | 73 (48,0) | 10 (35,7) | ||
| Ascites | > 500 ml | 28 (18,4) | 11 (39,3) | p = 0.001 |
| < 500 ml | 124 (81,6) | 17 (60,7) | ||
| Histology | Serous | 123 (80,9) | 22 (78,6) | NS |
| Non-serous | 29 (19,1) | 6 (21,4) | ||
| Grading | I + II | 50 (32,9) | 9 (32,1) | NS |
| III | 87 (57,3) | 18 (64,3) | ||
| Bowel involvement | Yes | 93 (61,2) | 17 (60,7) | NS |
| No | 59 (38,8) | 11 (39,3) | ||
| Peritoneal carcinomatosis | Yes | 120 (78,9) | 24 (85,7) | NS |
| No | 30 (19,7) | 4 (14,2) | ||
| FIGO Stage | I + II | 16 (10,5) | 3 (10,7) | NS |
| III + IV | 63 (41,4) | 15 (53,6) | ||
| Platinum sensitivity | Platinum sensitive | 49 (32,2) | 3 (10,7) | p = 0.007 |
| Platinum resistant | 24 (15,8) | 7 (25,0) |
| Nutritional Status Indicators | Number of fields with tumor load – IMO-Script (median) | p-value | |
| Malnourished | Non-malnourished | ||
| NRS–2002 (≥ 3) | 5 | 3 | 0,044 |
| NRI (< 100) | 6 | 3 | < 0,001 |
| Prealbumin (< 20 mg/l) | 6 | 3 | < 0,001 |
| Transferrin (< 200 mg/dl) | 6 | 3 | < 0,001 |
| Albumin (≤ 4.0 g/dl) | 5 | 3 | 0,001 |
| ECM/BCM (>1.2) | 4 | 3 | 0,024 |
| Phase-angle α (≤ 4,5º) | 4 | 3 | 0,041 |
| Weight loss in last 3 months (>5%) | 4 | 3 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





