Submitted:
21 November 2023
Posted:
22 November 2023
You are already at the latest version
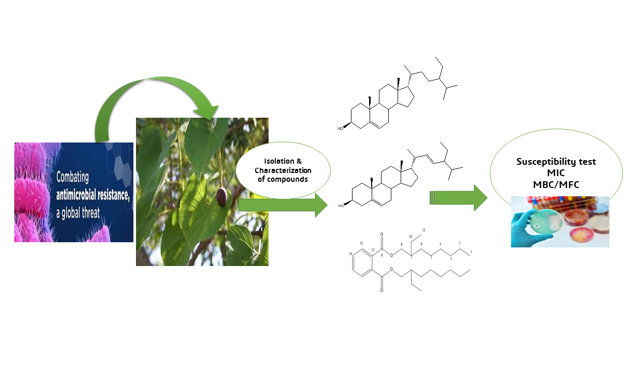
Abstract
Keywords:
1. Introduction
2. Results
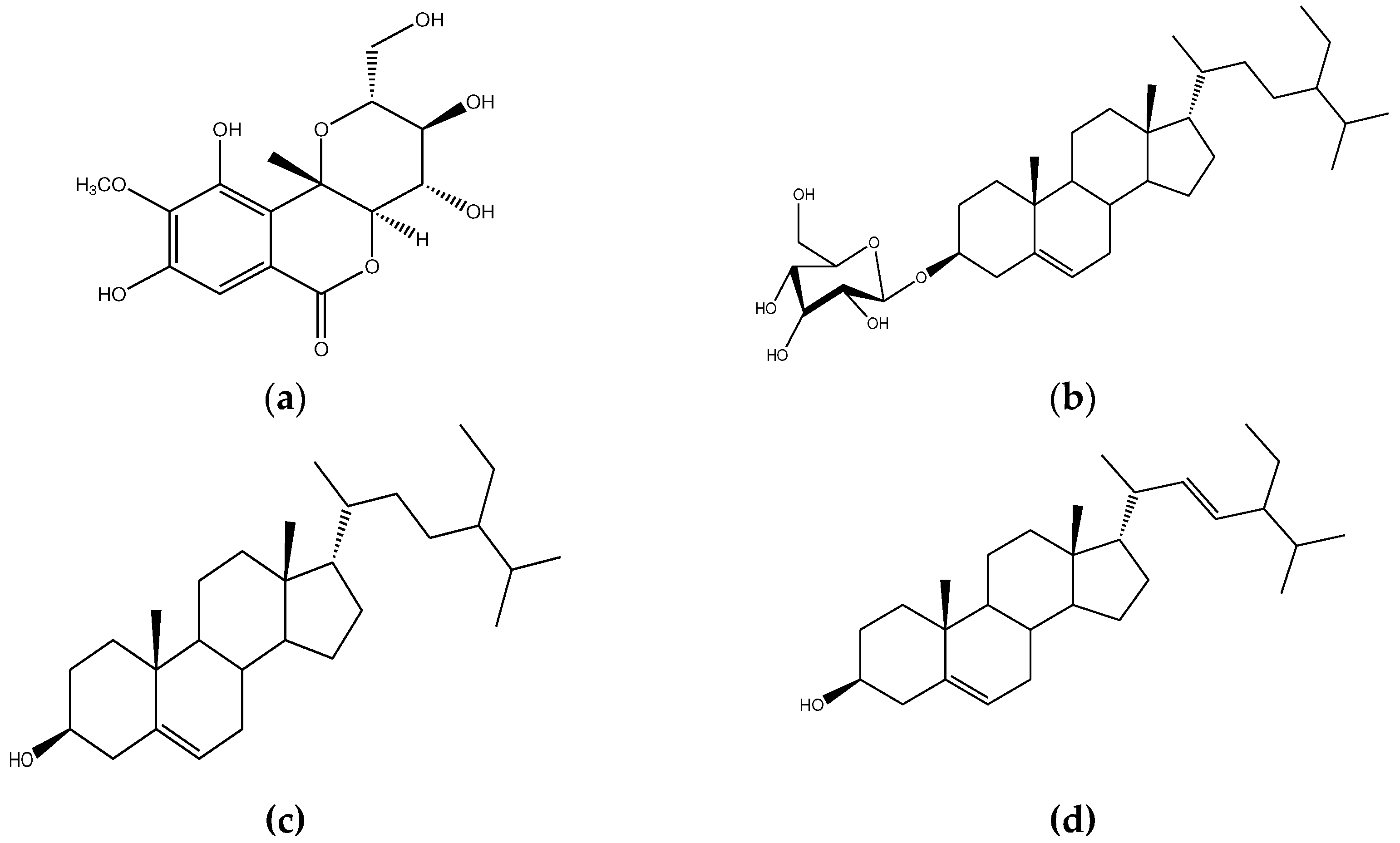
2.1. Isolation and Characterization of Compounds
2.1.1. Compound C1
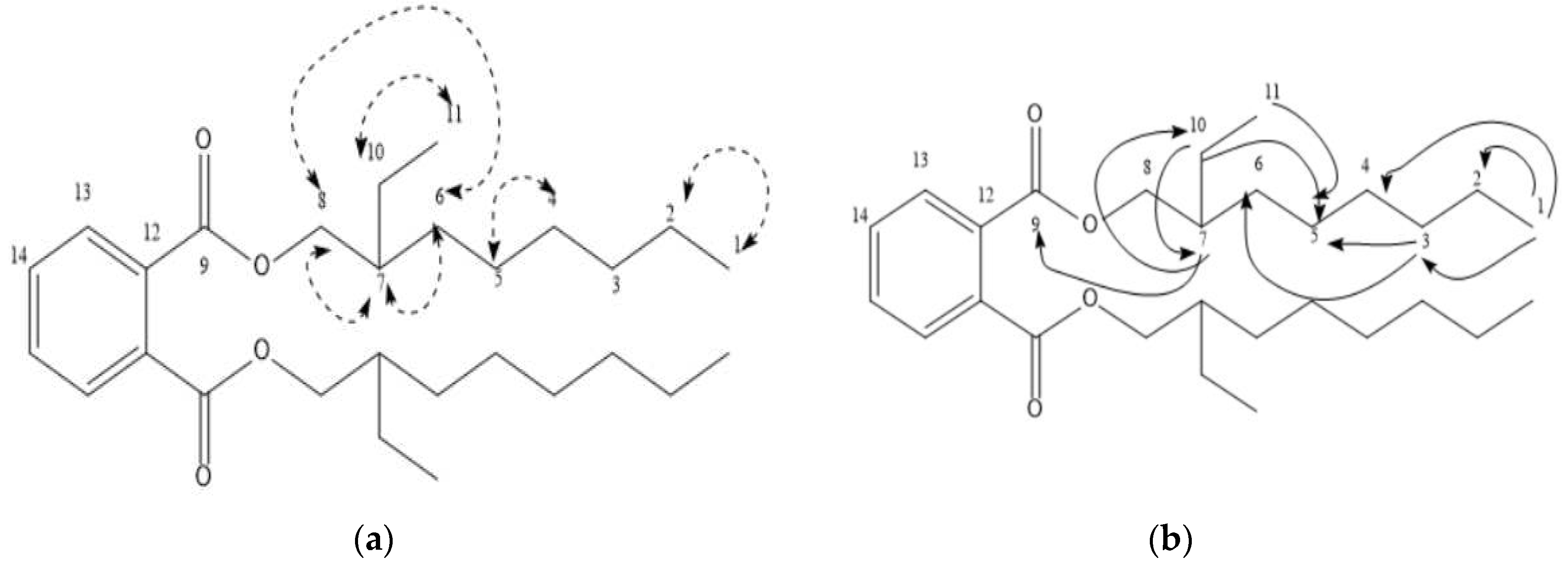
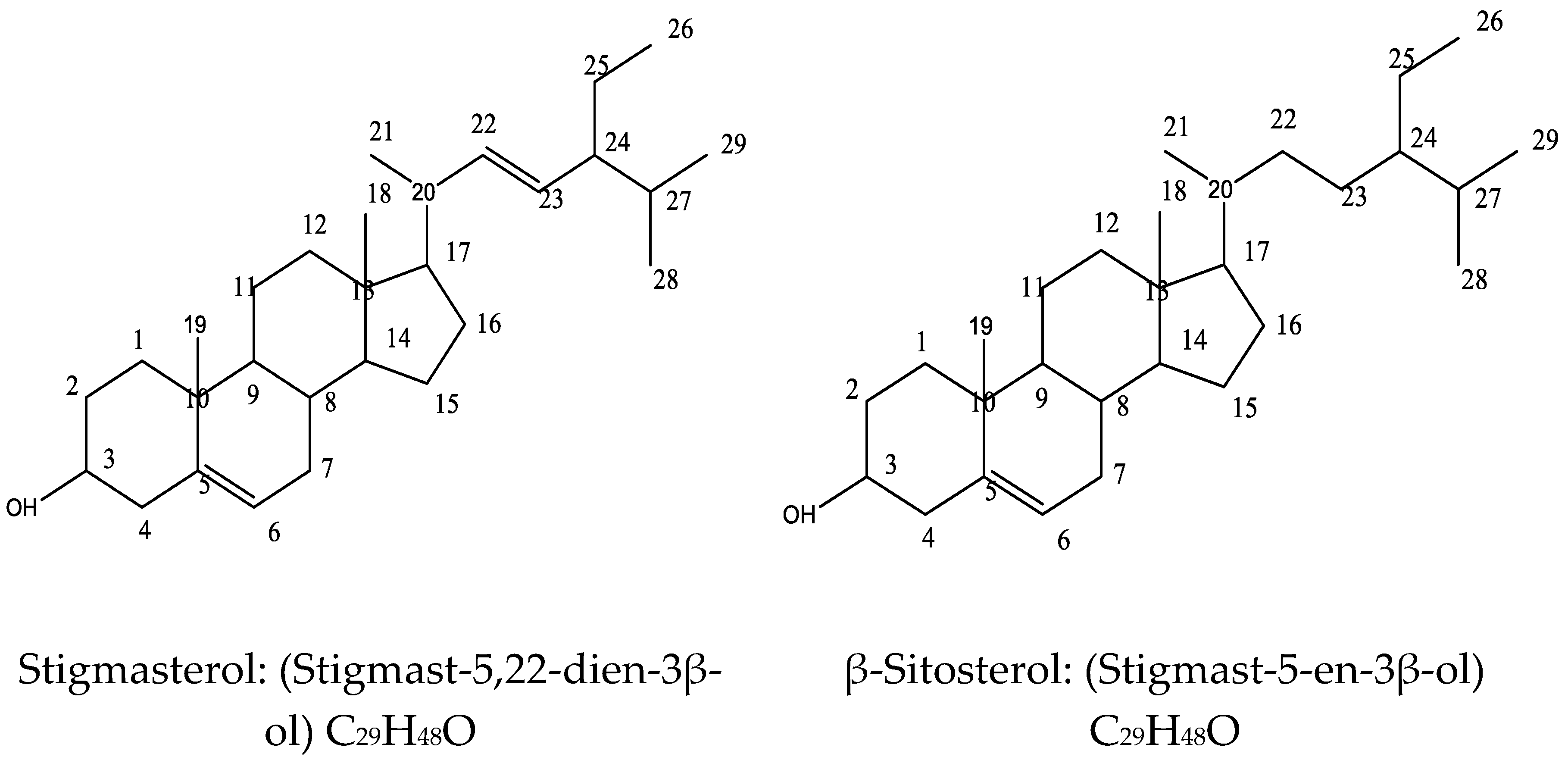
2.1.1. Compound C4C5
2.2. Antimicrobial activity of C4C5
2.2.1. Susceptibility test of C4C5
2.2.2. Zone of Inhibition of C4C5
2.2.3. MIC of C4C5 against the Test Organisms
2.2.4. MBC/MFC of C4C5 against the Test Organisms
3. Discussion
4. Materials and Methods
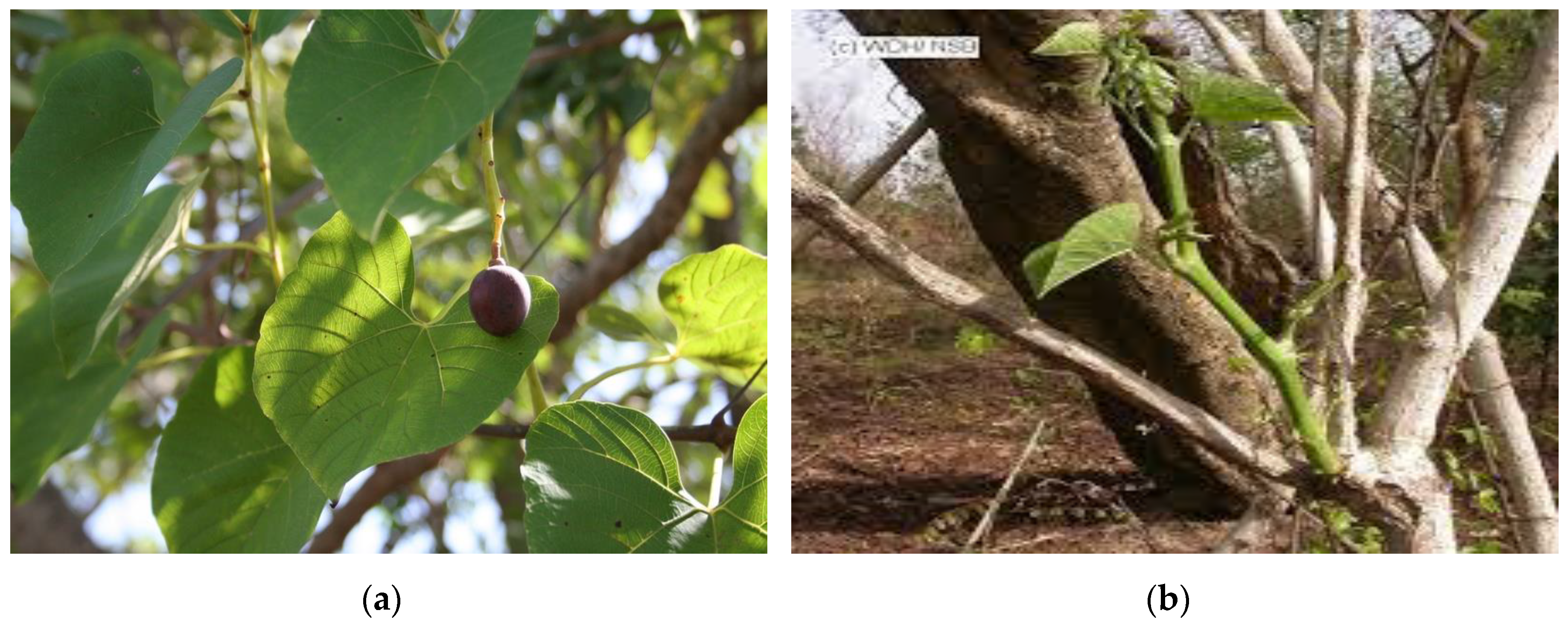
4.1. Collection, Identification and Preparation of Plant Material
4.2. Extraction and Partitioning of Plant Material
4.3. Chromatographic studies
4.4. Antimicrobial activity of C4C5
4.4.1. Microbial species
4.4.2. Susceptibility test
4.4.3. Minimum inhibitory concentration (MIC)
4.4.4. Minimum bactericidal/ fungicidal concentration (MBC/MFC)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Center for Disease Control (CDC). Methicillin Resistant Staph Aureus. https://www.cdc.gov/mrsa/community/index.html. [Date Accessed June 26th 2019].
- Centers for Disease Control and Prevention (CDC). About Antimicrobial Resistance. https://www.cdc.gov/drugresistance/about.html. [Date Accessed, 5th October, 2022].
- World Health Organization (WHO). Antimicrobial Resistance. https://www.who.int/health-topics/antimicrobial-resistance. [Date Accessed 17th November, 2021].
- World Health Organization (WHO). Antibiotic Resistance. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. [Date Accessed 27th October, 2023].
- Yusuf, A.J.; Abdullahi, M.I.; Aleku, G.A.; Ibrahim, I.A.A.; Alebiosu, C.O.; Yahaya, M. et al. Antimicrobial activity of stigmasterol from the stem bark of Neocarya macrophylla. Journal of Medicinal Plants for Economic Development 2018, 2: a38. 1-5. [CrossRef]
- Chukwu, A.C.O. Primary evaluation of C. populnea gum as binder in sodium sachylate tablet formulation. Drug Development Industry Pharm. 1989, 15, 325—330.
- Hutchinson, J.; Dalziel, J.M. Flora of West Tropical Africa. Second edition part 2. Mdibert London. Crown agents for oversea Government and Admin, 1958, pp 672-683.
- Danladi, A.H; Ushie, O.A.; Egwaikhide, P.A. β-Sitosterol isolated from Ethylacetate extract of Cissus populnea and the Antimicrobial activity. J. Chem. Soc. Nigeria, 2023, 48, 257 – 269.
- Achikanu, C.; Ani, O. Nutritional and Phytochemical Content of Cissus populnea (Okoho) Stem Bark. Asian Journal of Research in Biochemistry, 2020, 8-15. [CrossRef]
- Soladoye, M.O.; Chukwuma, E.C. Phytochemical analysis of the stem and root of C. populnea (Vitaceae) - an important medicinal plant in Central Nigeria. Phytologia Balcanica, 2012a, 18, 149-153.
- Ojekale, A.B.; Lawal, O.A.; Lasisi, A.K.; Adeleke, T.I. Phytochemistry and spermatogenic potentials of aqueous extract of Cissus populnea (Guill. and Per) stem bark. The Scientific World Journal, 2006, 6, 2140 – 2146. [CrossRef]
- Burkill, H.M. The Useful Plants of West Tropical Africa. Vol. 2, Royal Botanical Garden, University Press of Virginia, Charlottesville, 2000, p636.
- Belmain, S.R.; Golo, P.; Andan, H.F.; Atarigiya, H.; Chare, F.A.; Carr, P. Toxicity and repellency of ethnobaotanicals used in Ghana as post-harvest protectants, in Abstracts of presentations on selected topics at the XIVth International Plant Protection Congress (IPPC). Phytoparasitica, 2000, 28, 87 – 90.
- Kone, W.M.; Atindehou, K.K.; Terreaux, C.; Hosetettman, K.; Traore, D.; Dosso, M. Traditional medicine in north Cote-d’Ivoire: screening of 50 medicinal plants for antibacterial activity. Ethnopharmacol Bul, 2004, 93, 43 – 49. [CrossRef]
- Aguoru, C.U.; Ameh, S.J.; Olasan, O. Comparative phytochemical studies on the presence and quantification of various bioactive compounds in three major organs of okoho plant (Cissus populnea Guill and Perr) in Benue State North-Central Nigeria, Western Africa. European journal of advanced research in Biological and Life Sciences 2014, 2, 28-29.
- Soladoye, M.O.; Chukwuma, E.C. Quantitative phytochemical profile of the leaves of C. populnea Guill. & Perr. (Vitaceae)- an important medicinal plant in central Nigeria. Archives of Applied Science Research, 2012b, 4, 200 - 206.
- Nyemb, J.N.; Djankou, M.T.; Talla, E.; Tchinda, A.T.; Ngoudjou, D.T.; Iqbal, J.; Mbafor, J.I. Antimicrobial, glucosidase and alkaline phosphate activities of Bergenin, the major constituent of Cissus populnea roots. Medchem (Los Angeles) 2018, 8, 426-430. [CrossRef]
- Osibote, E.A.S.; Ogunlesi, M.; Okiu, W.; Asekun, T.; Familoni, O.B. Assessment of the antimicrobial activity of the essential oil of the stem powder of Cissus populnea and SeIsamum radiatum, Herbal medications for male infertility factor. Research Journal of Medicinal Plants, 2010, 4, 14-20.
- Akomolafe, S.F.; Oboh, G.; Akindahunsi, A.A.; Akinyemi, A.J.; Tade, A.G. Inhibitory Effect of Aqueous Extract of Stem Bark of Cissus populnea on Ferrous Sulphate- and Sodium Nitroprusside-Induced Oxidative Stress in Rat’s Testes In Vitro", International Scholarly Research Notices, 2013, 2013, Article ID 130989, 7 pages. [CrossRef]
- Adebayo, E.M.; Adeyemi, A.A.; Omolade, O.O.; Fashola, F.A.; Ajayi, T.O.; Attah, F.A.; Moody, J.O. Antisickling activity of the fresh and dried roots of Cissus populnea Guill. Et Perr (Vitaceae) Nigerian Journal of Nat. Prod. and Med., 2015, 19:134-138. [CrossRef]
- Nyemb, J.N.; Djankou, M.T.; Talla, E.; Tchinda, A.T.; Ngoudjou, D.T.; Iqbal, J.; Mbafor, J.I. DPPH antiradical scavenging, anthelmintic and phytochemical studies of Cissus populnea rhizomes. Asian Pacific Journal of Tropical Medicine, 2018, 11, 280-284.
- Halilu, M.E.; Yahaya, M.; Dangoggo, S.M.; Umar, K.J.; Ibrahim, G.; Abdullahi, M.I.; Uba, Baburo, S.I.B.; Garba, M.A.; Yusuf, A.J. Isolation and Characterization of Di-(2-ethylhexyl) Phthalate from the Leaves of Combretum micranthum (Altum) Combretceae. International Journal of Science for Global Sustainability, 2016, 2, 15-20. https://fugus-ijsgs.com.ng/index.php/ijsgs/article/view/251.
- Pateh, U.U.; Haruna, A.K.; Garba, M.; Iliya, I.; Sule, I.M.; Abubakar, M.S.; Ambi, A.A. Isolation of Stigmasterol, Beta-Sitosterol and 2-hydroxyhexadecamic acid methyl ester from the Rhizomes of Stylochiton lancifolius Pyer and Kotchy (Araceae). Nigerian Journal of Pharmaceutical Sciences, 2009, 8, 19-25.
- Yusuf, A.J.; Abdullahi, M.I.; Haruna, A.K.; Idris, A.Y.; Musa AM. Isolation and Characterization of Stigmasterol and Bis-(5,7-diacetyl-catechin-4’-α-rhamnopyranoside) from the Stem bark of Neocarya macrophylla (Sabine) Prance (Chrysobalanaceae). Nigerian Journal of Basic and Applied Science, 2015, 21, 15-22. http://www.ajol.info/index.php/njbas/index.
- Okoro, S.I.; Tor-Anyiin, A.T.; Ogbaji I.J.; Siwe, N. X.; Werner, M.K.R. Isolation and Characterisation of Stigmasterol and β–Sitosterol from Anthocleista Djalonensis A. Chev. AJOCS, 2018, 3, 1-5.
- Alves, T. M.; Silva, A. F.; Brandão, M.; Grandi, T. S.; Smânia, E.; Smânia Júnior, A.; Zani, C. L. Biological screening of Brazilian medicinal plants. Memorias do Instituto Oswaldo Cruz, 2000, 95, 367–373. [CrossRef]
- Abdullahi, M.I.; Uba, A.; Alebiosu, C.O.; Alhassan, A.M.; Mode, S.; Umar, A.; Nasir, I.; Bello, S.S.; Ibrahim, Z.Y.Y.; Yunusa, A.; Yusuf, A.J. Antimicrobial properties of the methanol leaf extract of Vernonia glaberrima Welw. Ex O. Hoffm (Asteraceae). African Journal of Pharmacy and Pharmacology, 2015, 9, 914-918. [CrossRef]
- Mahmoud, A.G.; Louis B.R. Antifungal agents: mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clinical Microbiology Reviews, 1996, 12, 501– 51.
- Tang, T.; Bremner, P.; Kortenkamp, A.; et al. Biflavonoids with cytotoxic and antibacterial activity from Ochna macrocalyx. Planta Med., 2005, 69, 247–253. [CrossRef]
- Yusuf A. J.; Abdullahi M. I.; Aleku G. A.; Ibrahim I. A. A.; Alebiosu C. O.; Yahaya M; et al. Antimicrobial activity of stigmasterol from the stem bark of Neocarya macrophylla. Journal of Medicinal Plants for Economic Development, 2018, 2, 1-5. [CrossRef]
- Alawode, T.T.; Lajide, L.; Olaleye, M.; Et al. Stigmasterol and β-Sitosterol: Antimicrobial Compounds in the Leaves of Icacina trichantha identified by GC–MS. Beni-Suef Univ J Basic Appl Sci, 2021, 10, 80. [CrossRef]
- Bakrim, S.; Benkhaira, N.; Bourais, I.; Benali, T.; Lee, L.H.; El Omari, N.; Sheikh, R.A.; Goh, K.W.; Ming, L.C.; Bouyahya, A. Health Benefits and Pharmacological Properties of Stigmasterol. Antioxidants (Basel), 2022, 11, 1912. PMID: 36290632; PMCID: PMC9598710. [CrossRef]
- Karim, N.; Khan, I.; Abdelhalim, A.; Halim, S. A.; Khan, A.; Al-Harrasi, A. Stigmasterol can be new steroidal drug for neurological disorders: Evidence of the GABAergic mechanism via receptor modulation. Phytomedicine: International Journal of Phytotherapy and Phytopharmacology, 2021, 90, 153646. [CrossRef]
- Pratiwi, R.; Nantasenamat, C.; Ruankham, W.; Suwanjang, W.; Prachayasittikul, V.; Prachayasittikul, S.; Phopin. K. Mechanisms and Neuroprotective Activities of Stigmasterol Against Oxidative Stress-Induced Neuronal Cell Death via Sirtuin Family. Front Nutr. 2021, 8, 648995. PMID: 34055852. [CrossRef]
- Foster, T. Staphylococcus. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston. Chapter 12. 1996, Available from: https://www.ncbi.nlm.nih.gov/books/NBK8448/.
- Mayer, F.L.; Wilson, D.; Hube, B. Candida albicans pathogenicity mechanisms. Virulence, 2013, 4, 119-28. Epub 2013 Jan 9. PMID: 23302789; PMCID: PMC3654610.
- Alex-Asaolu, A. Isolation and Characterization of Antimicrobial Constituent(s) from the stem of Cissus populnea Guill & Perr. MSc., Usmanu Danfodiyo University, Sokoto, Nigeria. 2023. [accessed on 29th October, 2023]. [CrossRef]
- Yusuf, A.J.; Abdullahi, M.I.; Musa, A.M.; Haruna, A.K.; Mzozoyana, V.; Biambo, A.A.; Abubakar, H. A bioactive flavan-3-ol from the stem bark of Neocarya macrophylla. Scientific African 2020, 7, e00273. [CrossRef]
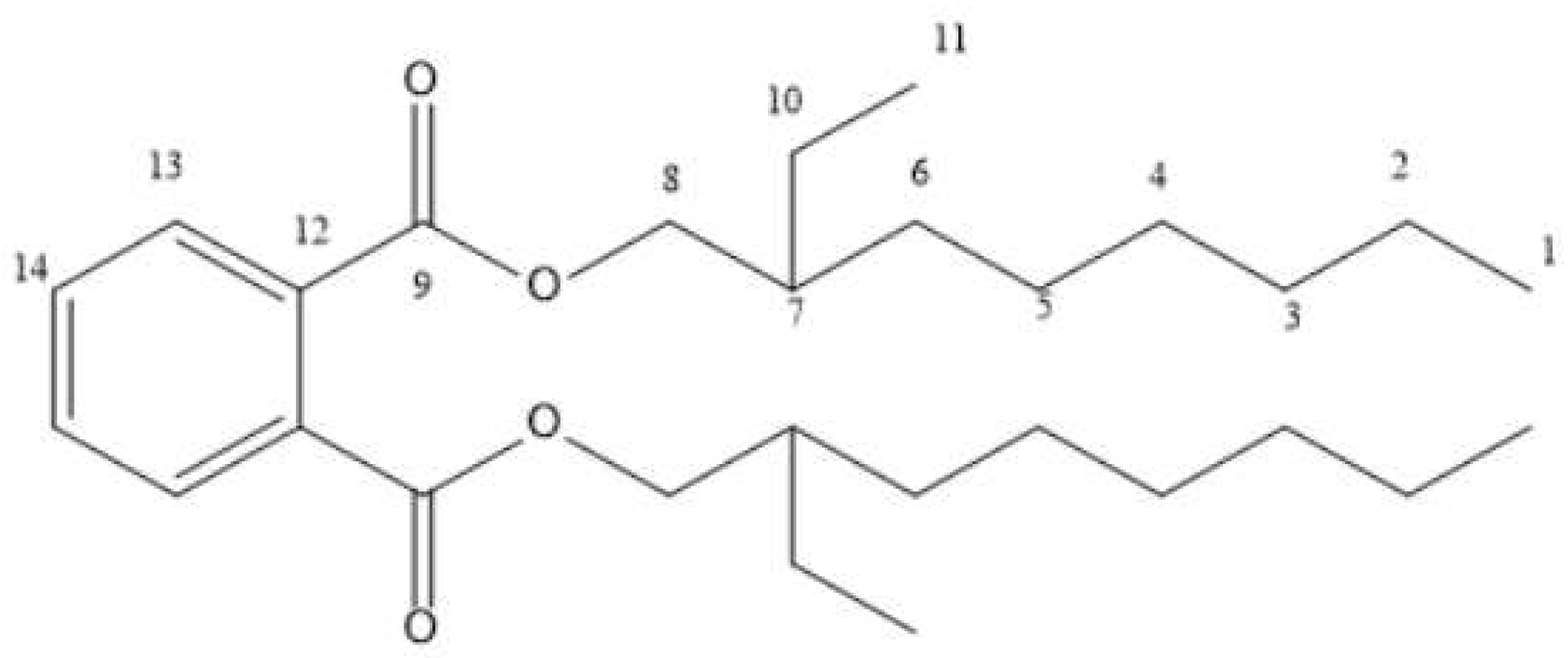
| Position | 1H-NMR | 13C-NMR | DEPT | COSY | HMBC |
|---|---|---|---|---|---|
| 1 | 0.82 | 14.3 | CH3 | H-2 | C-3, C-4, C-5, C-2 |
| 2 | 1.30 | 21.6 | CH2 | H-1 | - |
| 3 | 1.16 | 45.6 | CH2 | - | C-3, C-6, C-10, C-5 |
| 4 | 1.00 | 24.9 | CH2 | H-5 | C-3, C-5 |
| 5 | 1.28 | 22.9 | CH2 | H-4 | C-6, C-7, C-10, C-4, C-5 |
| 6 | 1.63 | 29.2 | CH2 | H-7, H-8, H-5, H-11 | C-9, C-7, C-10, C-4, C-5 |
| 7 | 2.37 | 32.2 | CH | H-6 | C-9, C-5, C-7, C-10 |
| 8 | 4.23 | 68.4 | CH2 | H-6 | C-7 |
| 9 | - | 178.7 | C | - | - |
| 10 | 1.61 | 27.3 | CH2 | H-11 | - |
| 11 | 0.84 | 20.9 | CH3 | H-10 | C-7, C-5 |
| 12 | - | 131.9 | C | - | - |
| 13 | 7.72 | 129.1 | CH | - | - |
| 14 | 7.54 | 132.7 | CH | - | - |
| Position | 1H-NMR C4C5 | 1H-NMR* | 13C-NMR C4C5 | 13C-NMR* | DEPT C4C5 |
|---|---|---|---|---|---|
| 1 2 |
1.85 1.46 |
1.85 1.46 |
37.27 31.67 |
37.26 31.67 |
CH2 CH2 |
| 3 | 3.55 | 3.52 | 71.83 | 71.81 | CH |
| 4 | 2.28 | 2.27 | 42.31 | 42.31 | CH2 |
| 5 | - | - | 140.77 | 140.76 | C |
| 6 | 5.37 | 5.35 | 121.72 | 121.71 | CH |
| 7 | 1.97 | 1.96 | 31.92 | 31.90 | CH2 |
| 8 | 1.49 | 1.48 | - | 31.90 | CH |
| 9 | 0.93 | 0.93 | 50.15 | 50.16 | CH |
| 10 | - | - | 36.52 | 36.51 | C |
| 11 | 1.50 | 1.49 | 21.22 | 21.21 | CH2 |
| 12 | 1.16 | 1.16 | 39.70 | 39.68 | CH2 |
| 13 | - | - | 42.23 | 42.22 | C |
| 14 | 1.05 | 1.05 | 56.88 | 56.87 | CH |
| 15 | 1.56 | 1.56 | 24.37 | 24.36 | CH2 |
| 16 | 1.71 | 1.70 | 28.92 | 28.92 | CH2 |
| 17 | 1.14 | 1.13 | 55.98 | 55.96 | CH |
| 18 | 0.70 | 0.69 | 12.05 | 12.05 | CH3 |
| 19 | 1.03 | 1.03 | 21.09 | 21.08 | CH3 |
| 20 | 2.02 | 2.02 | 40.49 | 40.49 | CH |
| 21 | 1.00 | 1.02 | 23.09 | 23.07 | CH3 |
| 22 | 5.16 | 5.10 | 138.31 | 138.31 | CH |
| 23 | 5.08 | 5.03 | 129.3 | 129.28 | CH |
| 24 | 1.54 | 1.53 | 51.25 | 51.24 | CH |
| 25 | 1.65 | 1.65 | 29.18 | 29.15 | CH2 |
| 26 | 0.83 | 0.82 | 18.99 | 18.98 | CH3 |
| 27 | 0.79 | 0.78 | 19.4 | 19.40 | CH |
| 28 | 1.17 | 1.15 | 25.40 | 25.40 | CH3 |
| 29 | 0.81 | 0.80 | 12.24 | 12.25 | CH3 |
| Test Organism | C4C5 | Ciprofloxacin | Fluconazole | Fulcin |
|---|---|---|---|---|
| Methicillin Resistant Staph aureus | S | R | R | R |
| Staphylococcus aureus | S | R | R | R |
| Vancomycin resistant enterococci | R | S | R | R |
| Escherichia coli | S | S | R | R |
| Bacillus subtilis | R | R | R | R |
| Pseudomonas aeruginosa | R | S | R | R |
| Candida albicans | S | R | S | R |
| Aspergillus niger | R | R | R | S |
| Trichophyton rubrum | S | R | R | S |
| Trichophyton mentagrophyte | S | R | R | S |
| Test Organism | C4C5 | Ciprofloxacin | Fluconazole | Fulcin |
|---|---|---|---|---|
| Methicillin Resistant Staph aureus | 27 | 0 | 0 | 0 |
| Staphylococcus aureus | 25 | 0 | 0 | 0 |
| Vancomycin resistant enterococci | 0 | 29 | 0 | 0 |
| Escherichia coli | 28 | 37 | 0 | 0 |
| Bacillus subtilis | 0 | 0 | 0 | 0 |
| Pseudomonas aeruginosa | 0 | 27 | 0 | 0 |
| Candida albicans | 29 | 0 | 34 | 0 |
| Aspergillus niger | 0 | 0 | 0 | 29 |
| Trichophyton rubrum | 24 | 0 | 0 | 32 |
| Trichophyton mentagrophyte | 26 | 0 | 0 | 30 |
| Test Organism | Concentration (µg/cm3) | ||||
|---|---|---|---|---|---|
| 100 | 50 | 25 | 12.5 | 6.25 | |
| MRSA | - | - | - | 0* | + |
| Staphylococcus aureus | - | - | 0* | + | ++ |
| Escherichia coli | - | - | - | 0* | + |
| Candida albicans | - | - | - | 0* | + |
| Trichophyton rubrum | - | - | 0* | + | ++ |
| Trichophyton mentagrophyte | - | - | 0* | + | ++ |
| Test Organism | Concentration (µg/cm3) | ||||
|---|---|---|---|---|---|
| 100 | 50 | 25 | 12.5 | 6.25 | |
| MRSA | - | 0* | + | + | ++ |
| Staphylococcus aureus | - | 0* | + | + | ++ |
| Escherichia coli | - | - | 0* | + | ++ |
| Candida albicans | - | - | 0* | + | ++ |
| Trichophyton rubrum | - | 0* | + | + | ++ |
| Trichophyton mentagrophyte | - | 0* | + | + | ++ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





