1. Introduction
The included teeth are those positioned inside the bone/mucosal tissues at the time of their physiological eruption. The main reasons for impaction are the inadequate length of the dental arch, incorrect tooth angulation, delayed facial growth, and late mineralization of the third molar, in addition to the presence of pathological lesions capable of mechanically impeding the eruption path, the presence of very bulky teeth, and dense bone/mucous tissue [
1,
2].
Impacted teeth can cause changes in adjacent structures leading to the development of pericoronitis, primary and/or secondary crowding of the dentition, tumors, and odontogenic cysts, associated periodontal defects, caries, and myofascial and neurogenic pain [
3]. The extraction of mandibular third molars is a procedure well performed in the dental office, and it requires adequate planning, seeking to minimize the occurrence of severe pain, edema, discomfort, and/or dysfunction, which may be temporary or permanent, the latter due to injury to the inferior alveolar nerve [
4,
5,
6]. The planning of third molar extraction always carried out before carrying out any type of intervention, consists of carrying out an accurate study of the case. The analysis of the clinical picture (visual physical examination and palpation) together with imaging tests facilitate the diagnosis and evaluation of the relationship of these teeth with adjacent structures, such as the mandibular canal and lower second molars, to prevent possible accidents in the transoperative period and postoperative complications [
4].
Among the existing options for imaging exams, panoramic radiography has been indicated as the standard method of choice when investigating third molars, as this image provides a general perspective of the teeth and bone structures [
7,
8,
9]. Studies have highlighted that panoramic radiography is a limited exam because it provides a two-dimensional image of three-dimensional structures resulting in the overlapping of underlying structures, and cone-beam computed tomography provides more accurate information with less distortion compared to conventional imaging exams [
10,
11,
12,
13,
14,
15,
16,
17].
The position of mandibular third molars has been carefully analyzed prior to surgical procedures due to the serious risks of injury to the inferior alveolar nerve. In this context, the appropriate application of new imaging resources, such as cone beam computed tomography with navigation dynamics and sophisticated software, can avoid such unpleasant surgical disorders. Thus, this study evaluated the spatial position and anatomical characteristics related to impacted mandibular third molars by map-reading strategy using cone beam computed tomography (CBCT) scans.
2. Materials and Methods
The present study had as a sample 200 cone beam computed tomography scans of patients of both sexes aged between 18 and 80 years, selected from a private clinic database (Center for Radiology and Orofacial Images of Cuiabá, Brazil, CROIF). The patients were referred to the radiology service for different diagnostic purposes, in the period from January 2015 to December 2020. This work is part of a more comprehensive study, approved by the Research Ethics Committee of the Federal University of Goiás (CAAE: 06486919.0.0000.5083).
Inclusion criteria for imaging examinations involved those with the presence of unerupted or impacted mandibular third molars and the presence of mandibular second molars. Exclusion criteria included imaging tests that showed images of orthodontic appliances, teeth with internal inflammatory resorption, bone changes associated with systemic diseases, and benign and/or malignant neoplasms in the mandible.
CBCT images were acquired using the CS 8100 3D CBCT system (Carestream, Marne-la-Valée, France) calibrated to thickness: 0.15 mm; FOV: 8 x 9 cm; and voxel: 75. Tube voltage was 90 kVp and tube current was 3 mA, with an exposure time of 15 s. The acquired tomographic data were converted into DICOM (Digital Imaging and Communications in Medicine). The following, images were examined using software (e-Vol DX, CDT Software; São José dos Campos, SP, Brazil) [
15] running on a PC workstation equipped with an Intel i7-7700K processor, 4, 20 GHz (Intel Corp., Santa Clara, CA), NVIDIA GeForce GTX 1070 Graphics Card (NVIDIA Corporation, Santa Clara, CA, USA), Dell P2719H monitor with 1920X1080 pixel resolution (Dell Technologies Inc., Texas, USA) and Windows 10 Pro (Microsoft Corp., Redmond, WA, USA). High-resolution images were used to ensure diagnostic accuracy.
The criteria for determining the positioning of impacted third molars on cone beam computed tomography images were based on the classifications of Winter [
18] and Pell & Gregory [
19].
The Winter’s classification [
18] evaluates the angulation of the long axis of the unerupted third molar with the long axis of the adjacent second molar: 1 - Vertical - the long axis of the third molar follows the same direction as the long axis of the adjacent second molar; 2 - Horizontal - the long axis of the third molar is perpendicular to the long axis of the second molar; 3 - Mesioangular - the crown of the third molar is inclined towards the second molar; 4 - Distoangular – the long axis of the third molar is inclined distally to the second molar; 5 - Inverted – the crown assumes the opposite direction to the occlusal plane; 6 - Vestibuloversion – the crown of the third molar facing the buccal surface; 7 - Linguoversion – the crown of the third molar facing the lingual face.
The Pell & Gregory’s classification [
19] evaluates two criteria - First criterion - depth of the tooth in the arch concerning the occlusal plane: 1 - Position A – the surface of the third molar is at the level or above the occlusal plane of the adjacent second molar; 2 - Position B – the surface of the third molar between the occlusal plane and the cervical line of the adjacent second molar; 3 - Position C – the surface of the third molar is located below the cervical line of the adjacent second molar. - Second criterion - depth of the element in the ramus of the mandible: 1 - Class I - the third molar crown is located completely in front of the anterior edge of the ramus; 2 - Class II – third molar crown partially inside the mandibular ramus; 3 - Class III – third molar crown completely within the mandibular ramus.
The findings related to the relationship of the third molar root apex with the mandibular canal (inferior alveolar nerve) were based on the following aspects [
20]: 1 - Superimposition of the root apex of the third molar with the mandibular canal; 2 - Presence of contact between the root apex of the third molar and the mandibular canal (inferior alveolar nerve); 3 - Absence of contact between the root apex of the third molar and the mandibular canal (inferior alveolar nerve).
The findings regarding external root resorption in the distal part of the lower second molar were based on a previous study that evaluated this same condition for upper teeth [
16]: 0 - Absence of external root resorption; 1 - Presence of external root resorption.
All CBCT scans were standardized so that the third molar was axially aligned; the sagittal and coronal planes were used to keep the long axis of the sample transversely to the ground, oriented to correct the parallax error. The analysis of the CBCT images was performed using a specific filter of the e-Vol DX software [
15]. The map-reading strategy in CBCT scans was performed in axial, sagittal, and coronal sections of 0.1 x 0.1 mm, from the most coronal point of the impacted tooth to the most apical point of the root apex. The dynamic navigation in CBCT scans also included all adjacent regions, such as the mandibular second molar, the relationship of the apex of the impacted tooth to the mandibular canal, the relationship of the impacted tooth and the mandibular ramus. The entire positioning of the mandibular third molar was carefully observed and tabulated.
All analyzes were performed jointly by two examiners, with experience in cone-beam computed tomography scans for more than ten years. The examiners were previously calibrated through the analysis of exams that follow the inclusion and exclusion criteria of the study, with a total corresponding to 10% of the sample. In the absence of consensus, a third examiner, with the same qualification, was summoned for the final decision.
The statistical treatment used described the variables as frequencies and percentages, using the Jamovi software - 1.1.9 (The Jamovi Project, 2019). Fisher’s exact test was used to comparative statistical analysis between the position of the apex of the impacted third molar/mandibular canal in both classifications used. The significance level considered was 5%.
3. Results
3.1. Patient Characteristics
In the 200 imaging exams evaluated, a total of 310 impacted third molars were observed. The distribution of teeth according to gender registered 55.16% (171) of female individuals and 44.83% (139) of males. The age group indicated that 47.7% (148) were between 18 and 30 years old, 43.9% (136) were between 31 and 50 years old, and 8.4% (26) were between 51 and 80 years old. The proportion of impacted teeth ranged between 51.3% (159) for tooth 38, and 48.7% (151) for tooth 48.
3.2. Positioning of impacted third molars
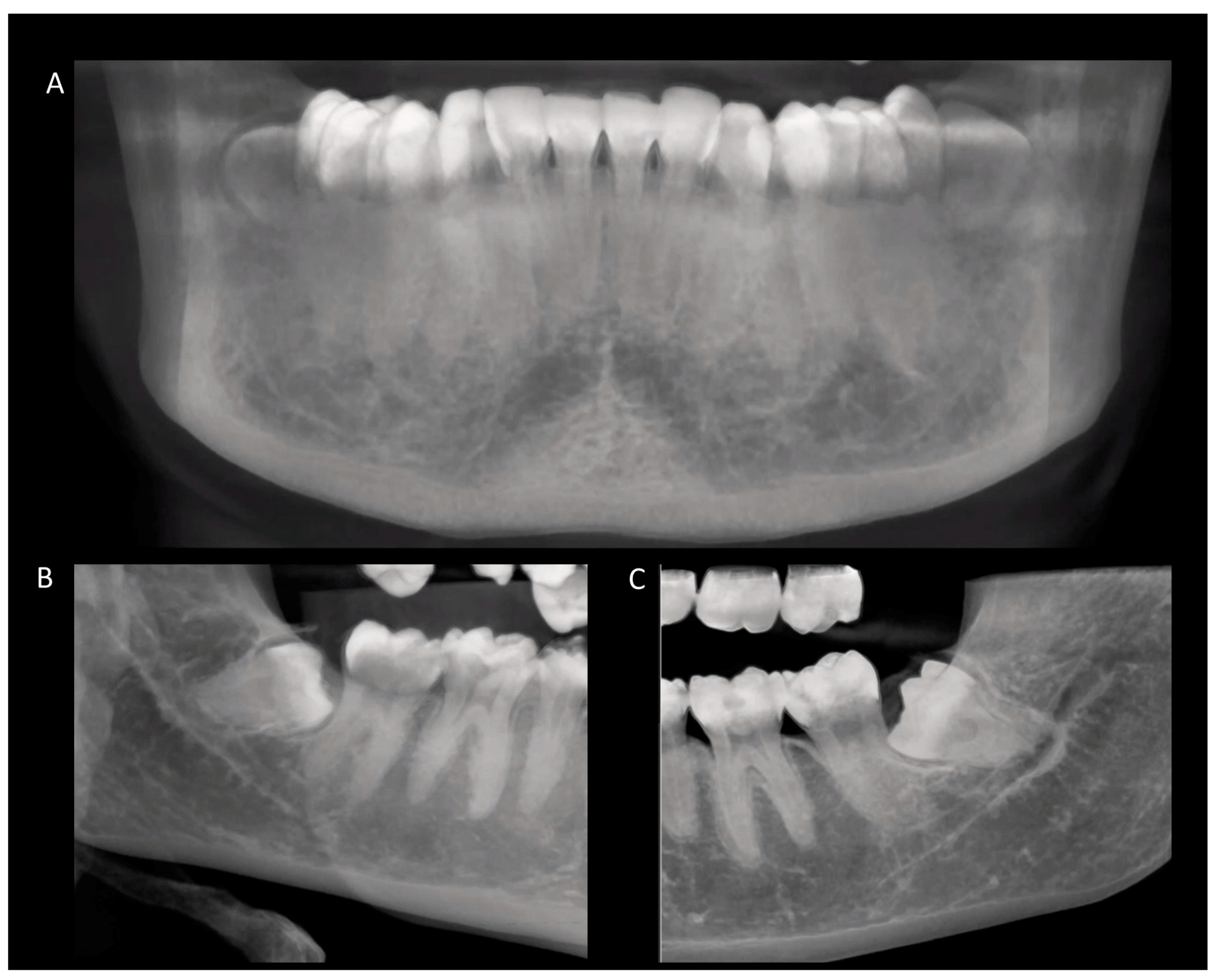
Based on Winter’s classification (18) (long axis of the third molar with the long axis of the second molar), it was observed that 48.06 % of impacted teeth were in the mesioangular position, followed by the vertical, distoangular, and vertical positions. horizontal and vestibuloversion. In this sample, no inverted or linguoversion teeth were observed (
Table 1).
According to Pell & Gregory’s classification [
19], the two criteria were analyzed. In assessing the depth of the bone where the impacted third molar is located, it was found that 43.22% of the teeth were in position B (surface of the third molar between the occlusal plane and the cervical line of the second molar), and 43.22% in position C (surface of the third molar below the cervical line of the adjacent second molar) (
Table 2). In the evaluation of the existing space between the distal part of the second molar and the ramus of the mandible, 54.2% of the teeth were class II (crown of the third molar partially inside the ramus of the mandible) (
Table 3) (
Figure 1).
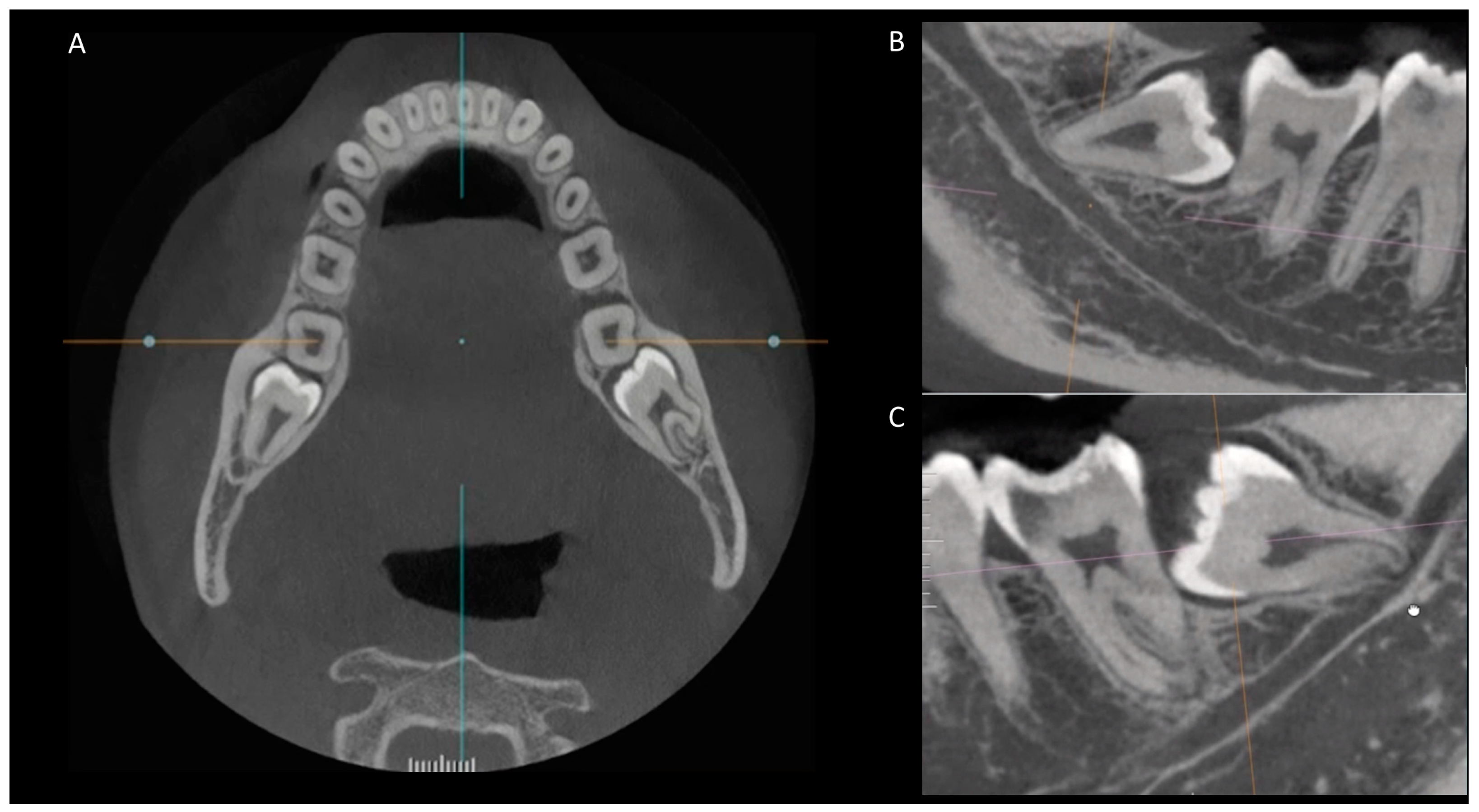
3.3. Anatomical relationship between the root apex of the impacted third molar and the mandibular canal
In the sample evaluated considering the anatomical position between the root apex of the impacted lower third molar with the mandibular canal, it was verified in 69.7% of the cases, absence of contact. In 22.9% of the cases, there was a superposition of the third molar root apex with the mandibular canal, and in 7.4% there was contact between the third molar root apex and the mandibular canal (
Table 4) (
Figure 2).
Class II, position B, the crown of the third molar partially inside the ramus of the mandible and the surface of the third molar between the occlusal plane and the cervical line of the second molar, according to the classification of Pell & Gregory [
19], were the teeth that presented overlap with the mandibular canal in greater numbers. Likewise, Class III, position C, those in which the crown of the third molar was completely within the ramus of the mandible and the surface of the third molar is below the cervical line of the adjacent second molar.
Table 5 presents the relationship between the position of the apex of the impacted third molar/mandibular canal in the Pell & Gregory [
19] classification, while
Table 6 presents the relationship between the position of the apex of the impacted third molar/mandibular canal in the classification of Winter [
18].
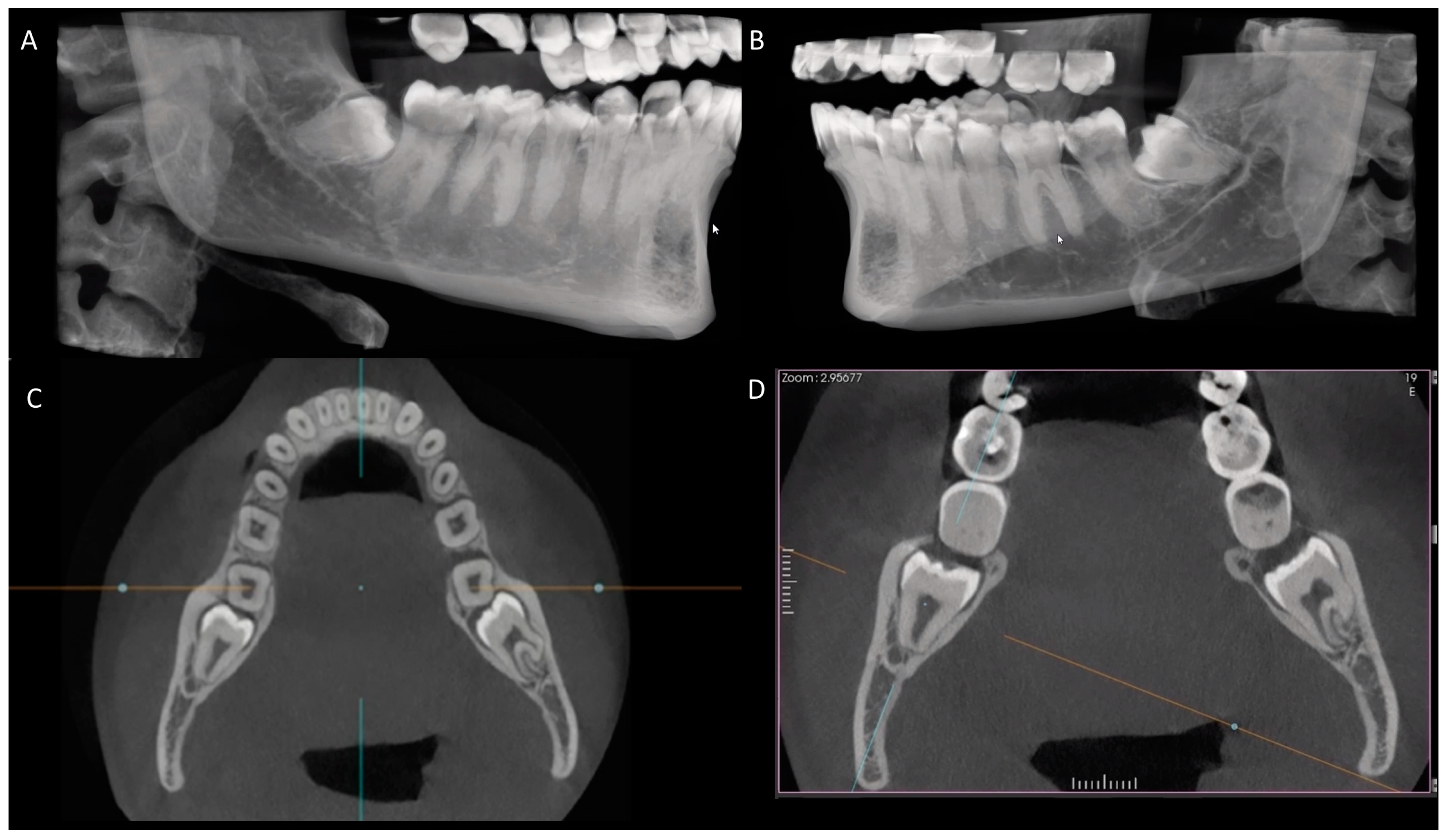
3.4. Occurrence of external root resorption on the distal side of the mandibular second molar
The analysis demonstrated external root resorption in the distal part of the lower second molar in 11.3 % of the cases, and in 88.7% of the samples, there was no such occurrence. Among the impacted lower third molars, the one that most caused external root resorption in the distal part of the lower second molar was tooth 48 (7.41%) while tooth 38 (3.87%) (
Figure 3).
4. Discussion
Knowledge of the spatial position and anatomical characteristics related to impacted third molars facilitates the diagnosis, planning, and surgical follow-up of the patient, in addition to reducing surgical complications. With accurate surgical planning in cases of impacted teeth, a series of complications can be avoided during the operative procedures and including the resulting legal issues. The map-reading strategy using a modern CBCT software to identify anatomical positions and characteristics of impacted third molars increases professional confidence and establishes a parameter of quality and safety in the surgical procedure for the patient.
Panoramic radiography has been used when investigating third molars, to provide a general perspective of the teeth and bone structures [
8,
9]. Panoramic radiography is considered a good imaging exam for the evaluation of the oral and maxillofacial complex in a population, since it is simple to perform, low cost, and offers a comprehensive analysis of the examined area. However, it is possible to observe limitations of conventional radiographic techniques, which reinforces the need for more advanced exams, using those that provide clearer images, with more accurate and more detailed information. Added to this is the possibility of differentiating soft and hard tissues, and visualization of the area of interest in more precise sections or cuts, as is the case with cone beam computed tomography [
10,
11,
12,
13,
14,
15,
16,
17,
21]. The relationship between impacted third molars and the mandibular canal in panoramic radiographs and CBCT was previously evaluated [
11], and the results showed that CBCT provides more accurate information. Peker et al. [
13] analyzed the correlation between CBCT and digital panoramic radiography in detecting the number of roots of impacted third molars and the relationship of these roots with the mandibular canal. The number of roots cannot be accurately determined on panoramic radiographs and CBCT is necessary in the preoperative evaluation of impacted third molars when darkening of the roots and interruption of the margins of the mandibular canal are observed on panoramic radiographs. Baena et al. [
14] reported that in risk cases, the use of CBCT allows a better assessment of the anatomical relationship between the mandibular canal and the root of the third molar, in addition to being possible to observe the presence of cortical bone around the inferior alveolar nerve.
The panoramic radiography tends to underestimate the space for the accommodation of the third molar when compared to CBCT [
22]. The impact of CBCT examination on the diagnosis and treatment of mandibular third molars among oral and maxillofacial surgeons indicates a higher level of professional confidence in the judgment of clinical cases. CBCT improved the level of confidence in the diagnosis and treatment of these teeth, in addition to increasing the perception of the level of surgical complexity. In this way, one can verify the need to consider the use of CBCT for the diagnosis and treatment of lower third molars [
17].
Some details of the methodology were carefully considered. The minimum age of participants in this study was 18 years, considering that the literature reports that at 17 years of age, jaw growth is completed [
23]. A relevant factor concerns the process of analysis of CBCT exams. Browsing through the CBCT images with a model used in previous studies allows better visualization and identification of the aspects to be analyzed. This methodology maintains multidimensional visualization, millimeter by millimeter, and in all planes [
24].
In the present study, it was verified that 55.1% of impacted third molars belonged to female individuals. The predominant age group was 18 to 30 years old (47.7%) and the percentage of impacted third molars corresponded to 51.3% for 38 (mandibular left third molar) and 48.7% for 48 (third molar bottom right). These findings are in line with previous studies [
1,
11]. Another aspect identified in the current study, considering Winter’s classification [
18] 48.06% of impacted teeth were in the mesioangular position. Based on the classification by Pell & Gregory [
19], 43.22% of the teeth were in position B (the surface of the third molar between the occlusal plane and the cervical line of the adjacent second molar) and position C (the surface of the third molar is located below the cervical line of the adjacent second molar). Considering the existence of space between the distal part of the second molar and the ramus of the mandible, 54.2% of the teeth were class II and 40.32% they were class III [
19]. In the 69.7% of teeth observed showed an absence of contact between the root apex and the mandibular canal, in 22.9% there was a superimposition and in 7.4% there was contact between the third molar root apex and the mandibular canal. Gu et al. [
26] reported that 92.7% of the third molars had no direct contact with the mandibular canal. Tassoker [
27] evaluated the relationship between the mandibular canal and the impacted mandibular third molar, using panoramic radiography and CBCT. The analysis showed that when the deviation of the mandibular canal is observed, the CBCT exam is recommended, as it allows the reduction of the risk of injury to the inferior alveolar nerve. Recent studies [
17,
28] have also demonstrated the superiority of CBCT in detecting details related to impacted third molars, such as the presence of second molar resorption and contact with the inferior alveolar nerve, and an increase in the level of confidence in the diagnosis and treatment plan for mandibular third molars.
The resorption of the distal surface of the second molar, caused by an impacted third molar, is considered an irreversible pathology and, according to The National Institute for Health and Care, when this pathology is observed, the intervention of choice: surgical removal of the impacted third molar. Most studies comparing the use of imaging exams to investigate the presence of external root resorption in second molars adjacent to impacted third molars reported a low prevalence (0.3 to 7%) [
29,
30]. This study verified an index of 11.3% of the occurrence of external root resorption in the distal part of the mandibular second molar. Oenning et al. [
5,
31] reported 14.3% of external root resorption in the distal second molar using CBCT, and Li et al. [
32] showed a prevalence of 52.9%.
The relevance and clinical application of this study are determined by the importance due to better planning, diagnosis, and prognosis, which implies decision-making with greater confidence for the professional, and greater comfort and safety for the patient. The reduction of unpleasant intercurrences, given the possibility of accidents such as aggression to the neurovascular bundle present in the mandibular canal, and a more predictable analysis of buccal and lingual bone thickness are aspects that should always be considered when planning surgeries for mandibular third molars.
5. Conclusions
Based on dynamics of navigation, it was observed that 48.06 % of impacted teeth were in the mesioangular position, 69.7% showed an absence of contact between the root apex and the mandibular canal, 22.9% there was a superimposition and in 7.4% there was contact between the third molar root apex and the mandibular canal. The dynamics of navigation in CBCT images for analyzing the anatomical positions of impacted third molars, using sophisticated post-processing software, increases professional confidence and establishes a parameter of greater quality and safety in the surgical procedure for the patient.
Author Contributions
Conceptualization, D.M.L., C.M.R.B. and C.R.A.E.; Methodology, D.M.L., C.R.A.E., M.R.B., and C.E.; Validation, M.R.B., and C.E.; Formal analysis, D.M.L., C.M.R.B., and L.R.A.E.; Investigation, D.M.L., C.M.R.B and C.R.A.E.; Resources, M.R.B., and C.E.; Data curation, D.M.L., L.R.A.E., and C.R.A.E.; Writing - Original Draft Preparation, D.M.L., C.M.R.B., L.R.A.E. and C.R.A.E.; Writing - Review & Editing, M.R.B. and C.E.; Supervision, C.M.R.B., C.R.A.E. and C.E.; Project administration, C.M.R.B. and C.R.A.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with Declaration of Helsinki and approved by the Institutional Review Board of Federal University of Goiás (IRB No 4057248, 24 April 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are available in this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hatem, M.; Bugaughis, I.; Taher, E. Pattern of third molar impaction in Libyan population: A retrospective radiographic study. Saudi. J. Dent. Res. 2016, 7, 7–12. [Google Scholar] [CrossRef]
- Carvalho, J.R.S.; Leite, J.S.; Oliveira, R.S. Evaluation of impacted lower third molars using cone beam computed tomography. J. Dent. 2021, 9, 1–6. [Google Scholar] [CrossRef]
- Singh, P.; Ajmera, D.H.; Xiao, S.S.; Yang, X.Z.; Liu, X.; Peng, B. Analysis of potential dynamic concealed factors in the difficulty of lower third molar extraction. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e713–e723. [Google Scholar] [CrossRef]
- Contar, C.M.; de Oliveira, P.; Kanegusuku, K.; Berticelli, R.D.; Azevedo-Alanis, L.R.; Machado, M.A. Complications in third molar removal: a retrospective study of 588 patients. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e74–e78. [Google Scholar] [CrossRef]
- Oenning, A.C.C.; Neves, F.S.; Alencar, P.N.B.; Prado, R.F.; Groppo, F.C.; Haiter-Neto, F. External root resorption of the second molar associated with third molar impaction: comparison of panoramic radiography and cone beam computed tomography. J. Oral Maxillofac. Surg. 2014, 72, 1444–1455. [Google Scholar] [CrossRef]
- Glória, J.C.R.; Martins, C.C.; Armond, A.C.V.; Galvão, E.L.; Dos Santos, C.R.R.; Falci, S.G.M. Third molar and their relationship with caries on the distal surface of second molar: A meta-analysis. J. Oral Maxillofac. Surg. 2018, 17, 129–141. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Meijer, G.J.; Soehardi, A.; Borstlap, W.A.; Melder, J.; Berge, S.J. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int. J. Oral Maxillofac. Surg. 2009, 38, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Ghaeminia, H.; Meijer, G.J.; Soehardi, A.; Borstlap, W.A.; Mulder, J.; Vlijmen, O.J.; Berge, S.J.; Maal, T.J. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int. J. Oral Maxillofac. Surg. 2011, 40, 834–839. [Google Scholar] [CrossRef]
- Liu, M.Q.; Xu, Z.N.; Mao, W.Y.; Li, Y.; Zhang, X.H.; Bai, H.L.; Ding, P.; Fu, K.Y. Deep learning-based evaluation of the relationship between mandibular third molar and mandibular canal on CBCT. Clin. Oral Investig. 2022, 26, 981–991. [Google Scholar] [CrossRef]
- Estrela, C.; Bueno, M.R.; Leles, C.R.; Azevedo, B.; Azevedo, J.R. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J. Endod. 2008, 34, 273–279. [Google Scholar] [CrossRef]
- Dalili, Z.; Mahjoub, P.; Sigaroudi, A.K. Comparison between cone beam computed tomography and panoramic radiography in the assessment of the relationship between the mandibular canal and impacted class C mandibular third molars. Dent. Res. J. 2011, 8, 203–210. [Google Scholar] [CrossRef]
- Momin, M.A.; Matsumoto, K.; Ejima, K.; Asaumi, R.; Kawai, T.; Arai, Y.; Honda, K.; Yosue, T. Correlation of mandibular impacted tooth and bone morphology determined by cone beam computed topography on a premise of third molar operation. Surg. Radiol. Anat. 2013, 35, 311–318. [Google Scholar] [CrossRef]
- Peker, I.; Sarikir, C.; Alkurt, M.T.; Zor, Z.F. Panoramic radiography and cone-beam computed tomography findings in the preoperative examination of impacted mandibular third molars. BMC Oral Health 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Baena, R.R.; Beltrami, R.; Tagliabo, A.; Rizzo, S.; Lupi, S.M. Differences between panoramic and cone beam-CT in the surgical evaluation of lower third molars. J. Clin. Exp. Dent. 2017, 9, e259–e265. [Google Scholar] [CrossRef]
- Bueno, M.R.; Estrela, C.; Azevedo, B.C.; Diogenes, A. Development of a new cone-beam computed tomography software for endodontic diagnosis. Braz. Dent. J. 2018, 29, 517–529. [Google Scholar] [CrossRef]
- Hermann, L.; Wenzel, A.; Schropp, L.; Matzen, L.H. Impact of CBCT on treatment decision related to surgical removal of impacted maxillary third molars: does CBCT change the surgical approach? Dentomaxillofac. Radiol. 2019, 48, 20190209. [Google Scholar] [CrossRef]
- Wanzeler, A.M.V.; Silveira, H.L.D.; Buligon, R.P.; Corsetti, A.; Vieira, H.T.; Arus, N.A.; Vizotto, M.B. Can CBCT change the level of confidence of oral maxillofacial surgeons in mandibular third molar management? Braz. Oral Res. 2022, 36, e078. [Google Scholar] [CrossRef] [PubMed]
- Winter, G.B. Principles of exodontia as applied to the impacted third molar: a complete treatise on the operative technique with clinical diagnosis and radiographic interpretations, American Medical books: St Louis, United States of America, 1926.
- Pell, G.J.; Gregory, G.T. Impacted mandibular third molars: classification and modified technique for removal. Dent. Digest. 1933, 9, 330–338. [Google Scholar]
- Deppe, H.; Mücke, T.; Wagenpfeil, S.; Kesting, M.; Linsenmeyer, E.; Tölle, T. Trigeminal nerve injuries after mandibular oral surgery in a university outpatient setting--a retrospective analysis of 1,559 cases. Clin. Oral Investig. 2015, 9, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Venta, I.; Mattila, M.; Turtola, L.; Vehmas, T.; Peltola, J.S. Reliability of CBCT and other radiographic methods in preoperative evaluation of lower third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 276–284. [Google Scholar] [CrossRef]
- Brasil, D.M.; Nascimento, E.H.L.; Gaêta-Araujo, H.; Oliveira-Santos, C.; Almeida, S.M. Is panoramic imaging equivalent to cone-beam computed tomography for classifying impacted lower third molars? J. Oral Maxillofac. Surg. 2019, 77, 1968–1974. [Google Scholar] [CrossRef]
- Almpani, K.; Kolokitha, O.E. Role of third molars in orthodontics. World J. Clin. Cases 2015, 3, 132–140. [Google Scholar] [CrossRef]
- Estrela, C.R.A.; Bueno, M.R.; Estrela, M.R.A.; Estrela, L.R.A.; Guedes, O.A.; Azevedo, B.C.; Cintra, L.T.A.; Estrela, C. Frequency and risk factors of maxillary sinusitis of endodontic origin evaluated by a dynamic navigation and a new filter of cone-beam computed tomography. J. Endod. 2022, 48, 1263–1272. [Google Scholar] [CrossRef]
- Lopes, L.S.; Cardoso, L.S.; Morais, M.N.S.; Ferreira, U.M.; Paula, L.G.F.; Mariano-Júnior, W.J. Prevalência dos tipos de impacção de terceiros molares na clínica odontológica de ensino do Centro Universitário de Anápolis – UniEvangélica. Sci. Invest. Dent. 2019, 24, 13–22. [Google Scholar] [CrossRef]
- Gu, L.; Zhu, C.; Chen, K.; Liu, X.; Tang, Z. Anatomic study of the position of the mandibular canal and corresponding mandibular third molar on cone beam computed tomography images. Surg. Radiol. Anat. 2018, 40, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Tassoker, M. Diversion of the mandibular canal: Is it the best predictor of inferior alveolar nerve damage during mandibular third molar surgery on panoramic radiographs? Imaging Sci. Dent. 2019, 49, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, L.M.; Gaêta-Araujo, H.; Cruvinel, P.B.; Tosin, I.W.; Azenha, M.R.; Ferraz, E.P.; Oliveira-Santos, C.; Tirapelli, C. Can diagnostic changes caused by cone beam computed tomography alter the clinical decision in impacted lower third molar treatment plan? Dentomaxillofac. Radiol. 2021, 50, 20200412. [Google Scholar] [CrossRef] [PubMed]
- Nitzan, D.; Keren, T.; Marmary, Y. Does an impacted tooth cause root resorption of the adjacent one? Oral Surg. Oral Med. Oral Pathol. 1981, 51, 221. [Google Scholar] [CrossRef] [PubMed]
- Akarslan, Z.Z.; Kocabay, C. Assessment of the associated symptoms, pathologies, positions, and angulations of bilateral occurring mandibular third molars: Is there any similarity? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, e26–e32. [Google Scholar] [CrossRef] [PubMed]
- Oenning, A.C.; Melo, S.L.; Groppo, F.C.; Haiter-Neto, F. Mesial inclination of impacted third molars and its propensity to stimulate external root resorption in second molars--a cone-beam computed tomographic evaluation. J. Oral Maxillofac. Surg. 2015, 73, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Tao, Y.; Cui, M.; Zhang, W.; Zhang, X.; Hu, X. External root resorption in maxillary and mandibular second molars associated with impacted third molars: a cone-beam computed tomographic study. Clin. Oral Investig. 2019, 23, 4195–4203. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).