1. Introduction
Cancer is an important cause of morbidity and mortality in every region of the world, irrespective of the level of human development [
1], and thus, it is considered a major obstacle in increasing life expectancy [
2]. In 2019, cancer ranked second globally in the number of deaths, years of life lost, and disability-adjusted life years (DALYs), with an estimated 23.6 million new incident cases (17.2 million when excluding nonmelanoma skin cancer), 10.0 million deaths, and an estimated 250 million DALYs due to cancer [
3]. Additionally, in recent decades, the overall incidence and mortality rates of cancer have shown an increasing trend [
4]. Consequently, the global cancer burden is expected to rise to 28.4 million cases by 2040, which represents a 47% rise from 2020 [
5]. Furthermore, if the exposure to behavioral and environmental risk factors that contribute to the burden of cancer continues to rise [
6], then the expected increase in the global burden of cancer may be further exacerbated.
The United Nations (UN), through the Sustainable Development Goals (SDGs) and the World Health Organization (WHO), recognizes the need to reduce the cancer burden; thus, it has focused on strategies that involve planning and implementing cancer control at the national level [
7]. However, there are regional and national differences in the cancer morbidity and mortality associated with the distinct level of exposure to population risk factors due to socioeconomic changes [
4]. Therefore, knowing local cancer epidemiology is fundamental to informing cancer control through prioritizing resource allocation, implementing public health policy, and improving health system planning [
8]. In this regard, in Mexico, previous studies have described the cancer-specific burden for some groups of cancer at the national and state level, including colorectal cancer [
9], lung cancer [
10], prostate cancer [
11,
12], cervical cancer [
13], and breast cancer [
14,
15], among others. Furthermore, some other studies have reported an overall assessment of the national burden of cancer that included several groups of malignant neoplasms from the period between 1970 and 2015 [
16,
17,
18,
19,
20]. Nevertheless, given the growing trend in the burden of cancer and its changing pattern, there is a need to provide updated national reliable and accurate estimates of the burden of cancer.
The present study aims to comparatively describe by sex and age the incidence, mortality, and DALYs due to 29 groups of cancer in Mexico in 2019 with trends from 1990 to 2019. To account for this, we used publicly available data from the most recent iteration of the Global Burden of Disease Study 2019 (GBD 2019), which is the most comprehensive global effort to systematically assess the main causes of health loss at the global, regional, and national levels [
21]. The results from the present study may add valuable and updated information to allow a better understanding of the current context of evolution and the growing trend of the national burden of cancer in Mexico and facilitate the implementation of concrete actions in public health to promote cancer control, diagnosis, and treatment programs.
2. Methods
2.1. GBD study overview
This observational study represents a secondary analysis of the results published in the Global Burden of Disease Study 2019 (GBD 2019). The GBD 2019 is produced by the Institute of Health Metrics and Evaluation (IHME), which includes a vast network of global collaborators, institutions, and partnerships involved in health policy and practice. This annual iteration was published in a series of four capstone papers [
21,
22,
23,
24] that describe in full detail the trends in fertility, demographics, and health loss due to 369 diseases and injuries with their corresponding 87 risk factors from 1990 to 2019. The estimates produced by the GBD 2019 represent the most comprehensive assessment of global health and thus provide timely and reliable results for 204 countries and territories by sex and age group. This study was produced and supervised by members of the GBD Collaborative Network from Mexico and complies with the protocol of the GBD [
11,
25,
26].
2.2. Estimation of the burden of cancer in Mexico
The GBD 2019 integrates fatal and nonfatal outcomes for a comprehensive hierarchical cause list of four levels. GBD includes “neoplasms” (both benign and malignant) as one of 22 groups of level 2 hierarchy, whereas among the cause 3 level hierarchy includes 29 malignant neoplasms (cancers) and one group of benign neoplasms (
https://vizhub.healthdata.org/gbd-compare/ accessed on 31 October 2023).
A detailed description of the approach, modeling framework, and steps followed by the GBD to produce the specific burden for neoplasms (total, benign, and malignant) are provided elsewhere [
21]. In addition, previous studies from the GBD have reported the methodology including case definition, data input sources, data processing, and statistical analysis used to estimate the global, national, and regional burden of the 29 groups of cancer mapped by the GBD [
3,
8]. The specific analytical flowchart to produce cancer estimates is available online at
https://ghdx.healthdata.org/gbd-2019/code/cod-2 (accessed on 2 November 2023).
This secondary analysis was produced using publicly available data from the Global Health Data Exchange (GHDx), which is an online repository of the IHME (
https://ghdx.healthdata.org accessed on 11 August 2023) where the results from the GBD are available for use in scientific publications, health policy, dissemination, and reporting because the GBD is considered a public health.
2.3. Estimation of the burden of cancer in Mexico and reporting standards
The results generated for Mexico by the GBD 2019 were downloaded as csv files from the online query tool of the GHDx at
https://vizhub.healthdata.org/gbd-results/ (accessed on 11 August 2023). To describe the burden of cancer in Mexico from 1990 to 2019, crude counts of the incidence, deaths, and disability-adjusted lived years (DALYs) due to total neoplasms and the 29 groups of malignant neoplasms were used. DALYs were used as a measure of the fatal and nondatal burden caused by neoplasms (total and malignant) because they represent the sum of the years of life lost and the years lived with disability due to these diseases [
21]. Additionally, the crude and age-standardized rates per 100,000 people were also retrieved at the national level for each year, sex, and age group (5 years each). In addition, to compare the trends in the measures, the annual percentage of change from 1990 to 2019 was downloaded. The age-standardized rate allows comparisons between distinct populations because the measure adjusts differences in the age structure [
27].
We prepared tables and figures to present a comparative description of the burden of total neoplasms and the 29 groups of cancer in Mexico for 2019 and for the trends from 1990 to 2019. All data are presented as point estimates with 95% uncertainty intervals (95% UI) produced by the GBD 2019.
3. Results
3.1. National and global burden of total neoplasms in 2019 and changes from 1990 to 2019
In 2019, among the general population of Mexico, there were an estimated 5.53 million (95% UI, 4.68 to 6.56 million) incident cases of total neoplasms (benign and malignant). From 1990 to 2019, the incidence of this group of diseases increased by 101.4%, and their national incidence rank passed from 12th to 10th highest among the 21 groups of the cause 2 level hierarchy of the GBD. Globally, neoplasms occupied the 12th highest incidence by 2019, with 305.1 million (258.6 to 364.6 million) new incident cases that corresponded to an increase of 57.0% with respect to 1990 (
Supplementary Figure S1).
In Mexico, the number of deaths attributed to total neoplasms increased 126.0% from 47,077 (45,314 to 48,538) in 1990 to 106,421 (92,194 to 121,749) deaths in 2019. Nevertheless, despite this substantial increase during the period, in 2019, the national rank of causes of death showed that the rank of total neoplasms decreased from the second to the third position below cardiovascular diseases and diabetes and chronic kidney disease. In contrast, total neoplasms remained between 1990 and 2019 as the second global cause of death, with 10.1 million deaths (9.4 to 10.7 million) in 2019 that represented a 75.1% increase with respect to 1990 (
Supplementary Figure S2).
During 2019, there was an estimated 2.87 million DALYs counts (2.50 to 3.27 million) due to total neoplasms in Mexico, representing a 94.1% increase from 1990 to 2019. DALYs due to total neoplasms scaled from the 8th to the 3rd highest national rank, whereas at the global level, this group of diseases was ranked as the 2nd highest, with 251.4 million counts (235.7 to 265.7 million) in 2019 and an increase of 52.6% during the period (
Supplementary Figure S3).
3.2. National burden of disease due to 29 malignant neoplasms during 2019
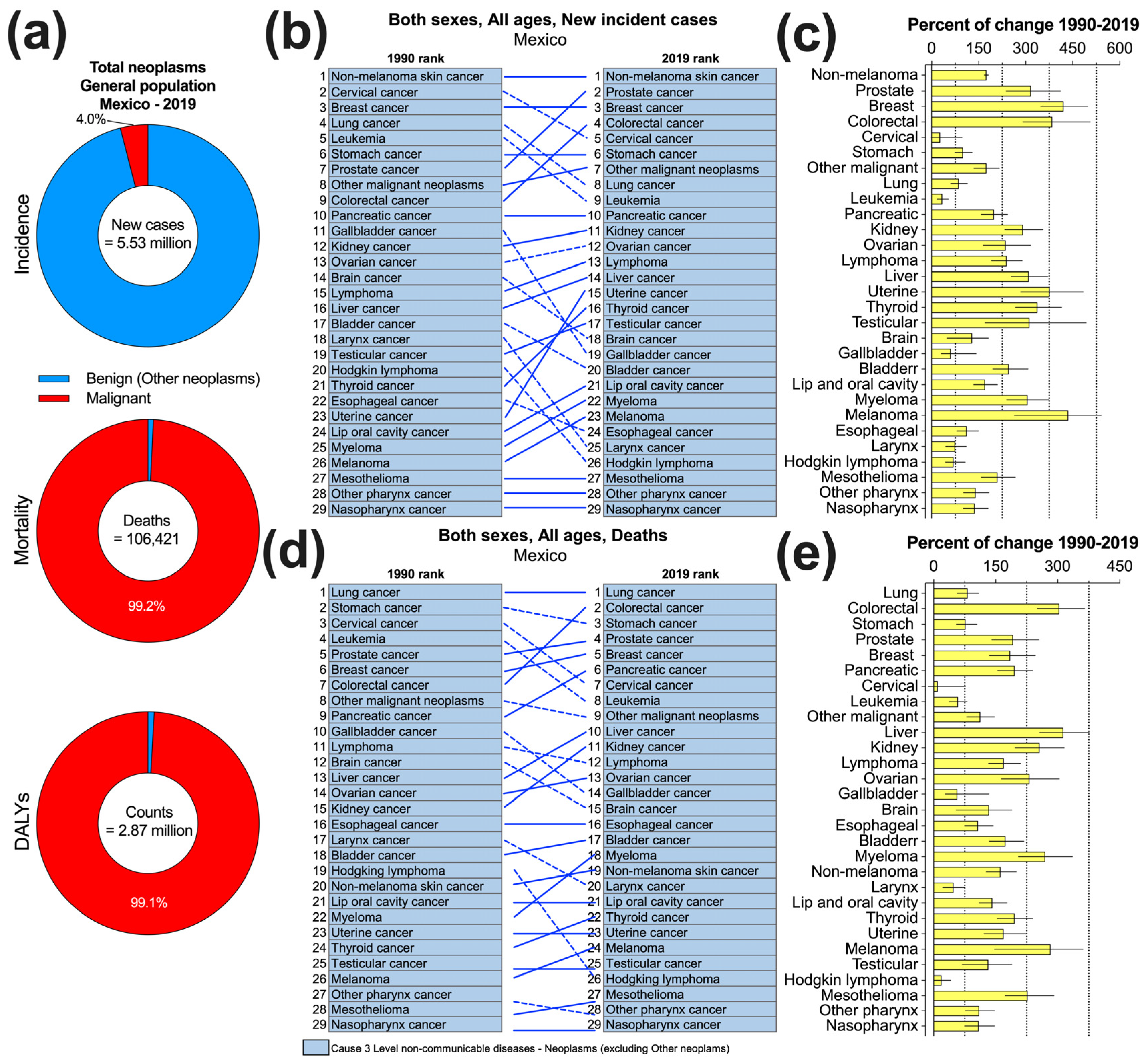
In Mexico, the 29 groups of malignant neoplasms mapped by the GBD caused an estimated 222,060 new cases in 2019, which accounted for 4.0% of the incident cases of total neoplasms (
Figure 1a). According to their national incidence (thousand new cases, 95% CI), nonmelanoma skin cancer (41.3, 34.3 to 48.7), prostate cancer (27.1, 20.6 to 36.0), breast cancer (24.4, 19.9 to 29.9), colorectal cancer (17.5, 15.0 to 20.1), cervical cancer (12.2, 9.6 to 16.5), and stomach cancer (11.3, 9.8 to 13.0) were the top six ranked cancer groups in 2019 and contributed 60.2% of the total cases due to malignant neoplasm. In contrast, with incidence estimates ranging from 213 to 439 new cases, mesothelioma, other pharynx cancer, and nasopharyngeal cancer were the least incident groups of cancer in Mexico during 2019 (
Figure 1b and
Table 1). The age-standardized rate of incidence of these 29 malignant neoplasms varied substantially between 0.18 and 35.66 cases per 100,000 people, with nonmelanoma skin cancer and nasopharyngeal cancer having the highest and lowest rates, respectively (
Supplementary Table S1).
As depicted in
Figure 1a, 99.2% of the deaths caused by total neoplasms in the general population of Mexico in 2019 were due to the 29 groups of cancer (105,591 deaths). In total, 52.9% of the mortality attributed to these malignant neoplasms was caused by only six groups of cancer: lung (11,002 deaths, 10.4% of the total), colorectal (10,518, 9.9%), stomach (10,0`95, 9.6%), prostate (9,257, 8.8%), breast (8,097, 7.7%), and pancreatic (6,853, 6.5%). Nationally, with values ranging between 174 and 353, mesothelioma, other pharynx cancer, and nasopharyngeal cancer caused the lowest number of deaths due to cancer in 2019 (
Table 1 and
Figure 1d). Additionally, lung cancer, colorectal cancer, stomach cancer, and prostate cancer had the highest age-standardized rates of death (range, 8.78 to 9.74 per 100,000 people,
Supplementary Table S1).
As depicted in
Figure 1a, 99.1% of the DALYs due to total neoplasms were attributed to the 29 malignant neoplasms in Mexico during 2019. At the national level, the top six causes of DALYs due to cancer were colorectal cancer, breast cancer, lung cancer, stomach cancer, leukemia, and cervical cancer, which in conjunction contributed 50.47% of the total 2.84 million DALYs caused by this disease (
Supplementary Figure S4). There was a contrasting pattern of DALYs counts (
Supplementary Table S2) and age-standardized rates among the 29 groups of cancer (
Supplementary Table S1). For instance, colorectal cancer (the top highest) caused an estimated 260.2 thousand (223.5 to 299.5 thousand) DALYs counts with an age-standardized rate of 215.34 (185.07 to 247.20) DALYs per 100,000 persons. In contrast, the corresponding estimate for nasopharyngeal cancer (the lowest) was 5.2 thousand (4.3 to 6.1 thousand) counts, with a rate of 4.17 (3.51 to 4.91) DALYs per 100,000 people.
3.3. National trends of the crude incidence, mortality, and DALYs due to 29 malignant neoplasms from 1990 to 2019
According to
Figure 1b, nonmelanoma skin cancer, breast cancer, stomach cancer, pancreatic cancer, mesothelioma, nasopharyngeal cancer, and other pharynx cancer remained in the same rank according to their incidence between 1990 and 2019 in Mexico. In addition, among the 13 cancer groups that showed an increase in their ranking during the period, prostate cancer, colorectal cancer, uterine cancer, and thyroid cancer showed the greatest number of advanced positions. In contrast, laryngeal cancer and Hodgkin lymphoma, gallbladder cancer, and brain cancer exhibited the greatest reduction in their rankings. Despite this differential pattern of change in the incidence rankings, it is worth mentioning that all 29 groups of cancer had a positive, though variable, percentage of annual change from 1990 to 2019 (
Figure 1c). As summarized in
Supplementary Table S3, during this period, the incident cases increased between 27% (-1 to 97) for cervical cancer and 436% (264 to 541) for melanoma. Other cancer groups with substantial increases were colorectal cancer, prostate cancer, uterine cancer, thyroid cancer, breast cancer, testicular cancer, and liver cancer (range 310% to 421%).
Between 1990 and 2019, the national rankings of deaths caused by malignant neoplasms revealed that six cancer groups (lung, esophageal lip oral cavity, uterine, testicular, and nasopharynx) maintained the same position, while 13 cancer groups rose in rank (
Figure 1d). Colorectal cancer showed the highest increase, moving from the 7th to the 2nd national rank during the period. On the other hand, 10 cancer groups experienced a decline in their rankings, with Hodgkin lymphoma, cervical cancer, leukemia, and brain cancer showing the most substantial reductions. All 29 groups of cancer had a positive percentage of annual change in their mortality from 1990 to 2019 (
Figure 1e). With values ranging from 232% to 314%, liver cancer, colorectal cancer, melanoma, myeloma, kidney cancer, and ovarian cancer showed the top six highest increases in the deaths they caused (
Supplementary Table S3).
Regarding the temporal trends for DALYs, colorectal cancer and breast cancer increased from the 7th and 6th positions in 1990 to the top and second highest positions by 2019, whereas lung cancer and stomach cancer remained unchanged (
Supplementary Figure S4a). In contrast, leukemia and cervical cancer, which were the two main causes of DALYs in 1990, decreased to the 5th and 6th positions by 2019, respectively. The DALYs ranks due to Hodgkin lymphoma and myeloma decreased substantially by ten and six positions during the period, respectively. Except for Hodgkin lymphoma, which showed a reduction in the percentage of change from 1990 to 2019, the remaining cancer groups increased their percentage of DALYs during the period (
Supplementary Figure S4b). With percentages that varied between 205% and 289%, colorectal cancer, liver cancer, myeloma, melanoma, and ovarian cancer showed the highest increases in their DALYs caused by malignant neoplasms from 1990 to 2019 (
Supplementary Table S3).
3.4. National cancer-specific trends from 1990 to 2019 of the age-standardized rates of incidence, mortality, and DALYs
Among the three measures included in the study, their age-standardized rates (per 100,000) showed a contrasting pattern of change from 1990 to 2019 that varied across the 29 groups of cancer in Mexico (
Supplementary Table S4). As shown in
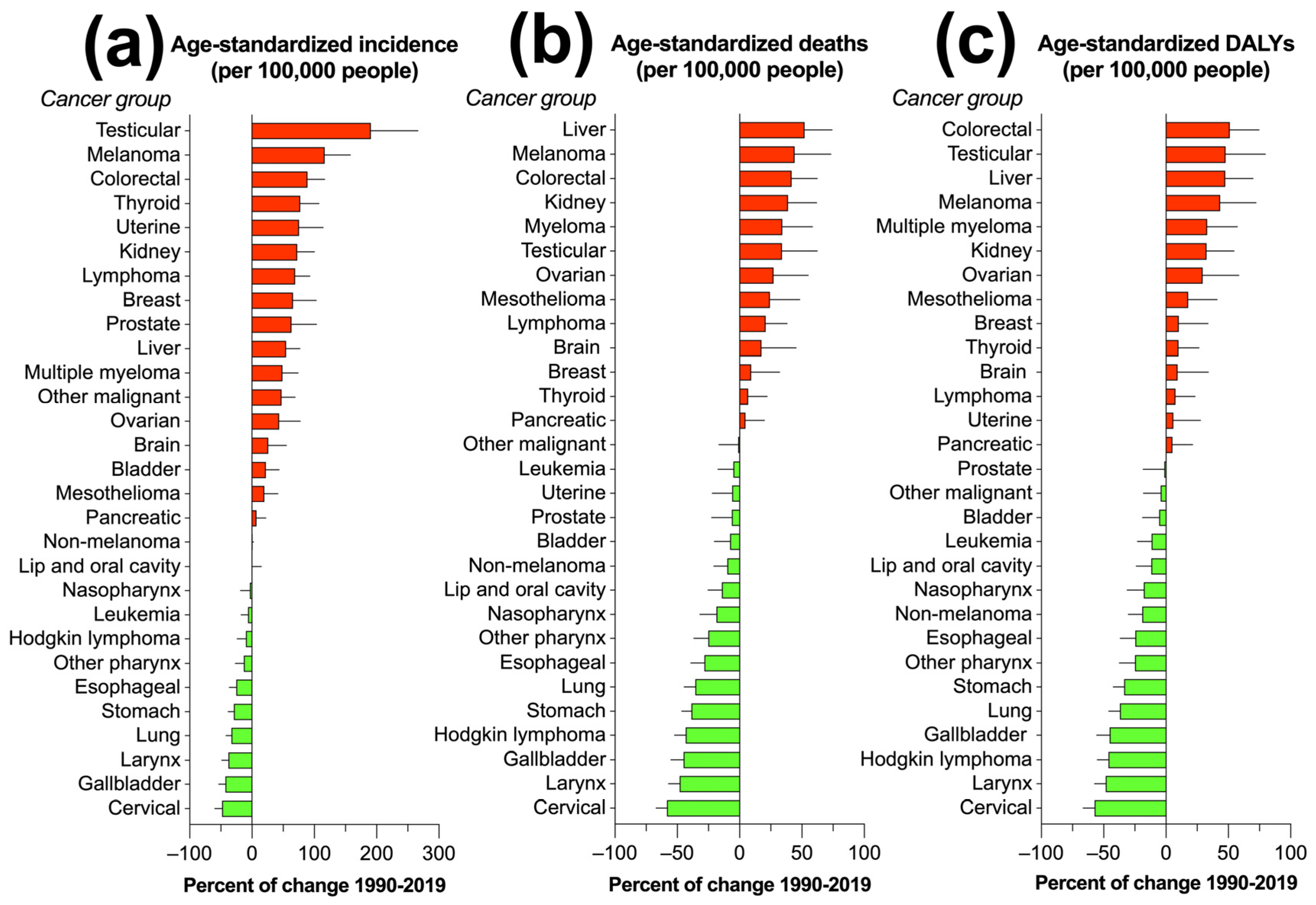
Supplementary Figure S5, 17/29 malignant neoplasms had a trend toward an increased age-standardized rate of incidence during the period, with testicular cancer (190.7%), melanoma (116.8%), and colorectal cancer (89.2%) showing the greatest increase in their rates. In contrast, cervical cancer (-47.9%), gallbladder cancer (-42.7%), laryngeal cancer (-37.6%), and lung cancer (-32.8%) were among the 13 groups of cancer that experienced the greatest reduction in their age-standardized rate of incidence per 100,000 people.
Regarding the age-standardized rate of death, 16/29 cancer groups decreased over the period, though with a broad variability in their time series (
Figure 2). Cervical cancer, laryngeal cancer, gallbladder cancer, Hodgkin lymphoma, stomach cancer, and lung cancer had the greatest reductions (range, -35.5% to -58.3%), whereas liver cancer (52.1%), melanoma (44.3%), and colorectal cancer (41.7%) showed a substantial increase in their age-standardized rate of death. With respect to DALYs, 14 malignant neoplasms increased their age-standardized rate, including colorectal cancer, testicular cancer, liver cancer, and melanoma, with a percentage of change between 43.2% and 51.33%, whereas Hodgkin lymphoma (-46.1%), larynx cancer (-48.2%), and cervical cancer (-57.2%) had the greatest reductions in their rates (
Supplementary Figure S6).
To facilitate the interpretation of these complex patterns of results,
Figure 3 summarizes the percentage of change in the age-standardized rates ordered from the cancer with the greatest increase to the cancer with the greatest decrease. As depicted in the figure, the percentage of change varied according to the measure and the specific group of cancer.
3.5. National burden of 29 groups of cancer by sex and age group in 2109
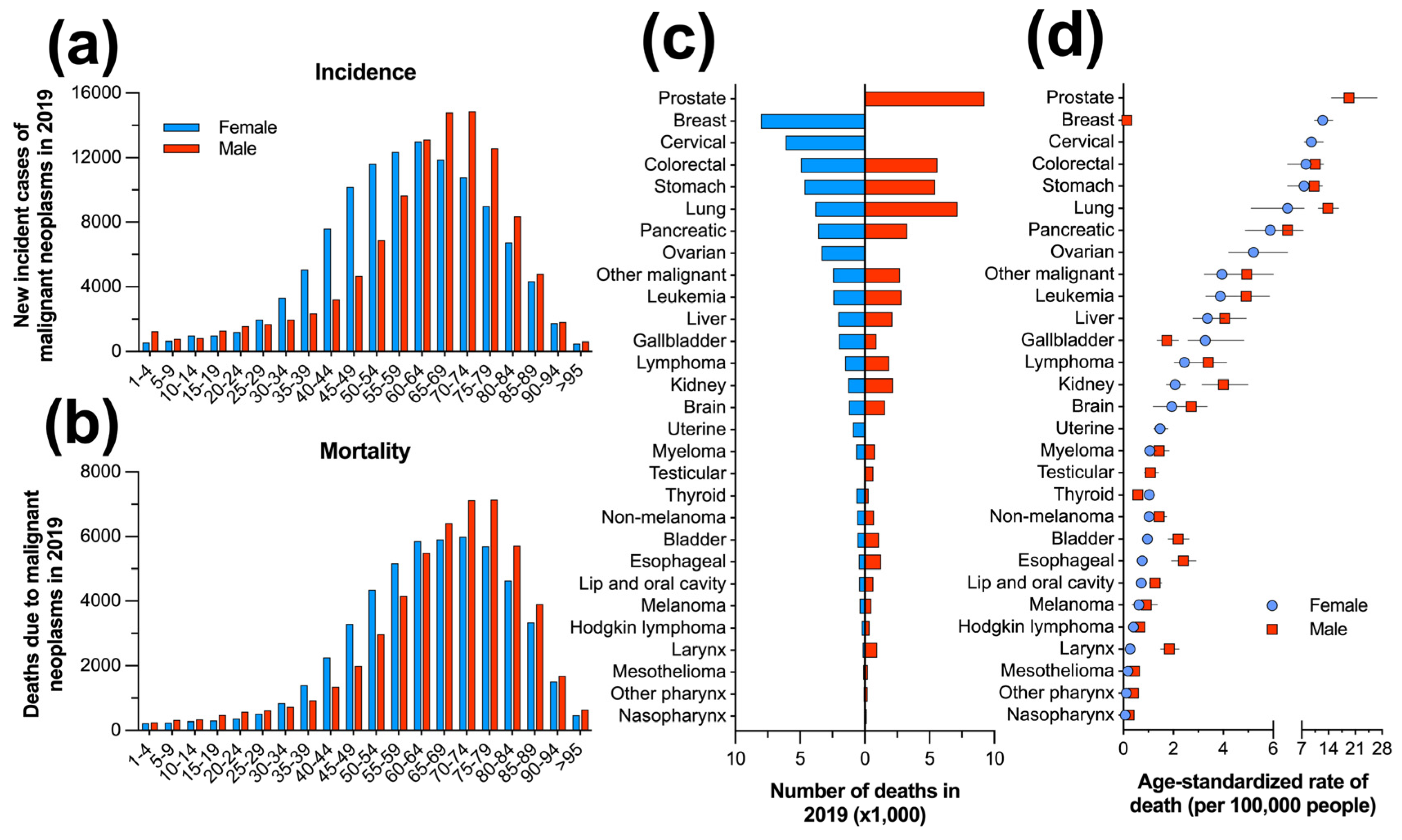
In 2019, the age-specific distribution of the burden of disease due to cancer by sex in Mexico showed a distinctive pattern. While for both sexes, the crude incidence was lower in the early age groups (1-24 years), in females, there was a rapid increase in cancer incidence that started at 35-39 years of age and concentrated the highest number of cases between 40 and 84 years of age, with a peak of 14,853 new cases in the 60-64 age group. In contrast, the increase in incident cases was more gradual in males and occurred at older ages, starting from 45-49 years of age and reaching a peak at 70-74 years with 12,291 new cases (
Figure 4a). Although a similar pattern was found in mortality, the highest number of deaths was reached in the 70-74 years group (5,999 deaths) for females, whereas deaths due to cancer caused the highest mortality (7,146 deaths) in the 75-79 years group in males (
Figure 4b). With respect to DALYs, the age-specific distribution showed a slightly greater negative effect due to cancer on males at younger (1 to 24) and older (65 to >95) years of age, whereas the DALYs counts were higher in females from 30 to 64 years (
Supplementary Figure S7a).
To further explore the sex-specific differences for each of the 29 groups of cancer, the crude counts and the age-standardized rates per 100,000 people were compared (
Table 1 and
Supplementary Table S1). Regarding incidence, breast cancer (24,312 cases), nonmelanoma (21,263 cases), and cervical cancer (12,195) led the incident cases in females, just as did prostate cancer, melanoma, and colorectal cancer in males (range, 9,426 to 27,097 cases (
Supplementary Figure S8a). With an age-standardized rate of 52.3 (40.0 to 70.1) incident cases per 100,000 people, prostate cancer led the ranking in males, whereas breast cancer was the leading cause in females, with an estimated 36.81 (30.02 to 45.01) cases per 100,000 people and a negligible rate in males (0.23, 0.19 to 0.29 cases;
Supplementary Figure S8b).
In Mexico, breast cancer caused an estimated 8,024 deaths in females during 2019, followed by cervical cancer and colorectal cancer in second and third place with 6,104 and 4,917 deaths, respectively. In males, prostate cancer led the number of deaths due to malignant neoplasms (9,256), followed by 7,176 and 5,601 deaths due to lung cancer and colorectal cancer, respectively (
Figure 4c). In both sexes, the age-standardized rate of death varied broadly according to the type of cancer. In males, prostate cancer led the ranking with 19.4 (14.8 to 26.7) deaths per 100,000 people, whereas breast cancer had the highest rate of death among females (12.5, 10.3 to 15.2 deaths), and the remaining neoplasms varied between 0.07 to 9.53 and 0.1 to 13.8 deaths per 100,000 people in females and males, respectively (
Figure 4d). In females, breast cancer caused the greatest number of DALYs (254,489 counts), with an age-standardized rate of 381.12 (315.67 to 464.64) per 100,000 people, while in males, with 161,552 DALYs and 319.46 (244.06 to 432.47) counts per 100,000 people, prostate cancer caused the highest burden (Supplementary
Figure S7b,c).
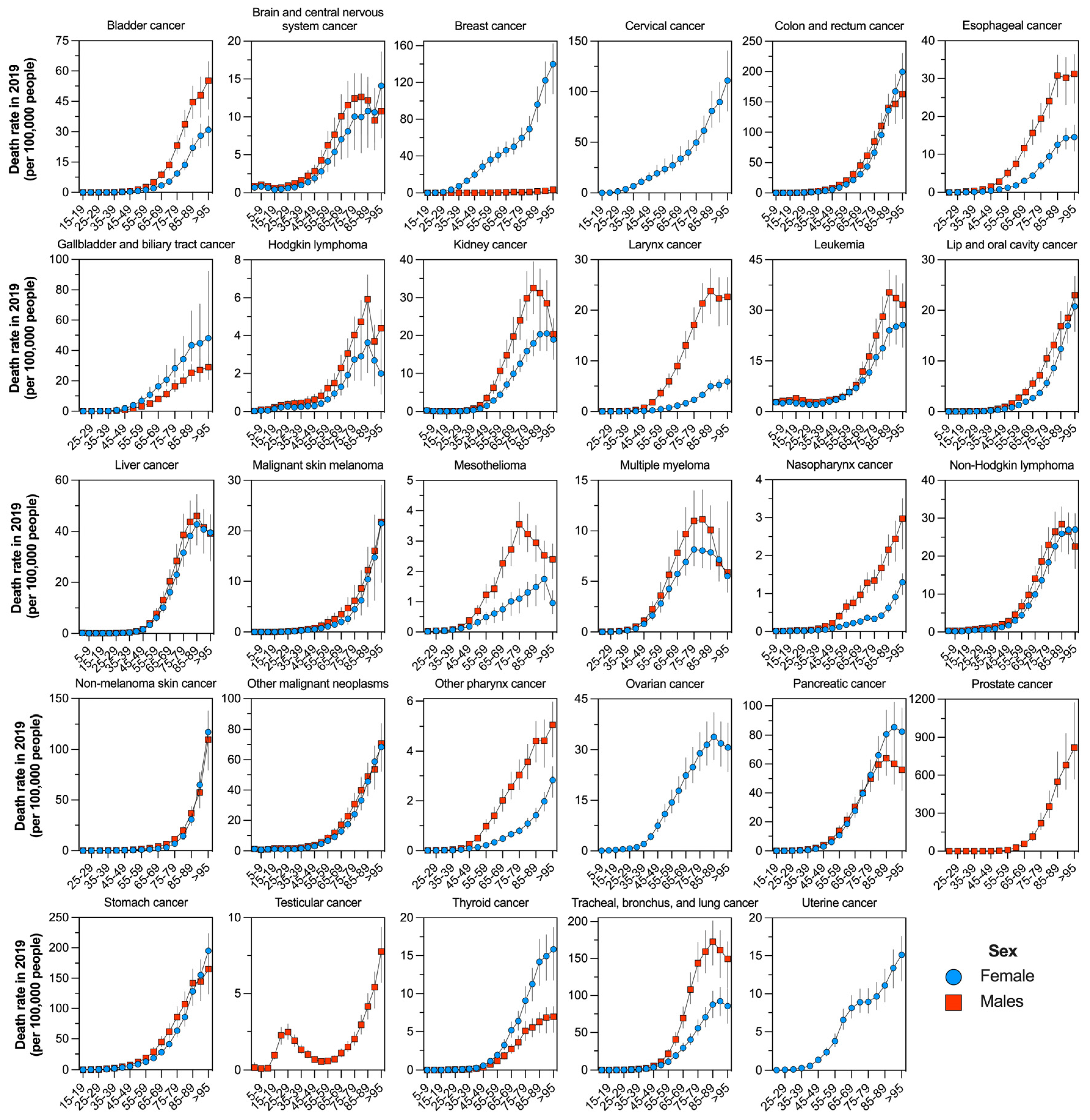
Finally, as judged by the rate of incidence (
Supplementary Figure S9), deaths (
Figure 5), and DALYs (
Supplementary Figure S10) per 100,000 people, there was a contrasting pattern of the age-specific burden between sexes that varied according to the type of cancer in Mexico during 2019. Overall, except for brain cancer, leukemia, Hodgkin lymphoma, and testicular cancer, most malignant neoplasms tend to cause the highest burden at older ages. Additionally, there were higher rates in males than in females in the 8-10 cancer groups (bladder, brain, esophageal, Hodgkin lymphoma, kidney, larynx, lip and oral cavity, mesothelioma, nasopharynx, other pharynx, and lung).
4. Discussion
Cancer is a pathological condition characterized by a notable escalation in prevalence and fatality rates globally. The present circumstances can be attributed to two primary elements: the extension of life expectancy and the heightened exposure to risk factors, many of which are associated with socioeconomic progress [
2]. Epidemiologically, it is important to describe the patterns of cancer incidence among several demographic cohorts, encompassing aspects such as diagnosis rates, mortality rates, mean age of diagnosis, and overall disease burden. This allows us to comprehend its impact on the population and create strategies to respond to the challenges it presents for society [
28]. In the current study, we described the burden of cancer in Mexico using as epidemiological measures the incidence, mortality, and DALYs, all of which showed a substantial increase in Mexico from 1990 to 2019.
4.1. Cancer burden due to the 29 groups of malignant neoplasms
Globally, total neoplasms were the second cause of death only below cardiovascular diseases in 2019 among the general population. In contrast, the national rank indicated that total neoplasms ranked third, just below diabetes and chronic kidney disease and cardiovascular diseases, which were the two first leading causes of death in Mexico during 2019. Even though the population from Mexico experienced a decline in the ranking of total neoplasms, which moved from second to third place from 1990 to 2019, the mortality due to total neoplasms increased by 126.05% between 1990 and 2019, with 29 groups of malignant neoplasms fuelling this change. During the same period, lung cancer retained 1st place in mortality due to cancer, whereas colorectal cancer increased from 7th to 2nd highest cause of death due to cancer, followed by stomach cancer, which moved from 2nd to 3rd. Prostate cancer, breast cancer, and pancreatic cancer followed the list of the top six causes of death due to cancer in Mexico during 2019. This pattern partially differs from the study conducted by Mohar-Betancourt et al. (2017) [
18], which found that between 2000 and 2013, the six leading causes of mortality due to cancer were lung cancer, stomach cancer, liver cancer, prostate cancer, breast cancer, and cervical cancer [
18].
The increase in mortality due to colorectal cancer has been confirmed by other works based on national databases from Mexico [
29] and has also been documented at the global level [
30,
31]. Although the increase in mortality due to colorectal cancer is associated with a trend toward higher incidence, even at early onset (< 50 years of age) [
32], the lack of national screening strategies in Mexico may further exacerbate such a trend for colorectal cancer because a great number of new incident cases are detected at advanced stages, thus resulting in higher mortality rates [
29,
33]. Furthermore, deficiencies in cancer mortality records and alterations in risk factors, including metabolic, behavioral, environmental, and occupational exposures, have been identified as potential contributing causes.
In terms of incidence, our results showed that among the 29 groups of malignant neoplasms mapped by the GBD, nonmelanoma skin cancer, prostate cancer, breast cancer, colorectal cancer, cervical cancer, and stomach cancer were the top six ranked cancer groups in Mexico in 2019 [
8]. This rise in cancer morbidity and mortality could be related to several behavioral and environmental risk factors, such as smoking, drinking, diet, and radiation exposure, as well as certain infections and hormonal imbalances [
34]. In Mexico, the prevalence of risk factors such as alcohol and tobacco consumption is high [
18,
35]. Therefore, more studies are needed to unveil the pattern of association between cancer mortality and risk factors.
4.2. Cancer burden by sex
In the present study, although results are divided by sex, it is essential to mention that cancer affecting nonreproductive tissues exhibits a greater incidence and mortality rate in males, resulting in roughly double the mortality rate when compared to females [
36]. Prostate cancer has been the most often diagnosed cancer in males, while breast cancer has been the most diagnosed disease in females. Based on the GBD data, it was observed that in 2017, the most prevalent form of cancer among women globally was nonmelanoma skin cancer, which was subsequently followed by breast cancer. In the year under consideration, it was observed that nonmelanoma skin cancer had the most significant impact on men, followed by tracheal, bronchus, lung, and prostate cancer [
8].
The present study shows that in Mexico, by 2019, breast cancer became the most common cancer among females, surpassing nonmelanoma skin cancer, followed by cervical, colorectal, and stomach cancers. Among males, nonmelanoma skin cancer was overtaken by prostate cancer, followed by colorectal, tracheal, bronchus, and lung cancer. The reasons for the differences in cancer rates and outcomes between sexes are not fully understood, but recent studies suggest that genetic and environmental factors, and their complex interactions, may play a role. Biological sex significantly influences organismal development and physiology, affecting processes like cell signaling, metabolism, and immune responses [
37,
38,
39,
40]. Research indicates that X- and Y-linked tumor-suppressor genes may have differing activity in males and females [
41].
The excess risk of gallbladder and biliary tract cancer in females is likely due to the higher incidence of gallstones among women [
42,
43]. In this regard, the higher portion of the male excess in urinary bladder cancer can be attributed to factors like smoking and occupational exposures [
44]the remarkable strength and consistency of the sex disparity, coupled with the moderate association with smoking and the limited proportion of cases attributable to occupational exposures, suggest the involvement of as-yet-unidentified factors [
45,
46].
The enigmatic sex disparities in cancer incidence and mortality are unlikely to be solely explained by known environmental or genetic factors. Studies in various countries have found that female cancer patients tend to have better survival rates than men [
47,
48,
49], in contrast to the Mexican population, where overall mortality was slightly higher in females than men. The incidence of cancer in males remains understudied despite the well-known disparity, possibly due to researchers assuming known causes explain the disparity. However, for cancers not linked to smoking, alcohol, and specific occupational exposures, the sex gap largely remains unexplained [
45].
The incidence of thyroid cases is more than double in women than in men; this disparity has been seen in other countries [
50]. Currently, there is no conclusive information on the biological causes of this difference [
51]. The disparity could be partly explained by nonbiological factors, for example there is speculation that women may have more opportunities for incidental detection in clinical settings [
50].
4.3. Cancer burden by age group
As expected, a trend of higher incidence rates is observed at older ages for both sexes, this occurs because cancer arises due to mutations in cells and these mutations accumulate in tissues over time [
52]. Higher mortality rates are also observed for both men and women at older ages. Other studies also show an acceleration of the mortality rate with [
53]. The higher mortality rate among older people may respond to various factors such as comorbidities, less intense detection, and less likelihood of undergoing aggressive treatment [
53].
While the study did not categorize age groups, based on global trends, it is evident that cancer incidence among children and teenagers is notably lower when compared to older populations [
54]. Additionally, specific types of cancers disproportionately affect certain age cohorts. In this regard, leukemia and other cancers of the lymphatic system take the forefront as the primary contributors to cancer incidence among young individuals in the child and teenage age range [
55]. In a study conducted by Gomez-Dantes [
17] and colleagues, it was revealed that the combined category of leukemia and other malignant neoplasms played a significant role, contributing to nearly 70% of the overall cancer burden of the Mexican population within this younger age group. Furthermore, the present study indicates a noteworthy shift in the prevalence of leukemia over time and a decline in its ranking, moving from the fifth position in 1990 to the ninth position in 2019. This shift in the ranking of leukemia underscores the evolving landscape of cancer epidemiology, indicating potential changes in risk factors, diagnostic capabilities, or treatment modalities over the years [
56]. Despite the decrease in the ranking of leukemia, its historical prominence highlights the critical importance of ongoing research, early detection, and effective treatment strategies, especially for pediatric and adolescent populations. Understanding these trends in cancer incidence is instrumental in tailoring healthcare interventions and resource allocation to address the specific needs of children and teenagers facing these unique health challenges [
57].
Conversely, in recent decades, Latin America has witnessed a notable rise in life expectancy, leading to a subsequent phenomenon of population aging [
58]. The observed rise in incidence and mortality rates in Mexico since 1990 can be partially attributed to the aging population, which is anticipated to result in a higher number of individuals being diagnosed with cancer and experiencing cancer-related fatalities. A study conducted by Foster et al., 2010 shows that advanced age can deter oncologists from choosing intensive cancer therapy, even if patients are highly functional and lack comorbidities. Consequently, this group could have a worse prognosis and be undertreated, adding to the mortality rate [
59].
4.4. Relevant cancer groups
4.4.1. Lung cancer
Among cancers of the respiratory system, lung cancer is the leading cause of death out of malignant neoplasms; however, its occurrence in Mexico has declined since 1990. The role of tobacco smoke in the development of lung cancer is widely recognized, as it is a significant contributing factor. According to Zhang et al. (2021) [
60], it is estimated that tobacco smoke is responsible for approximately 90% of lung cancer cases in men and 78% in women. The incidence of tobacco consumption in Mexico has experienced a decline over the past few decades, particularly among the male population [
10]. The implementation of public initiatives, such as the enactment of the general tobacco control law in 2008 and the ratification of the World Health Organization’s Framework Convention on Tobacco Control in 2004, has played a significant role in reducing tobacco usage [
61]. The implementation of these rules in Mexico led to a notable decline in daily cigarette consumption among the general population, with a fall from 13.5% to 7.7% between 2002 and 2009. However, since then, there has been no significant change in the prevalence of daily tobacco consumption until the present time [
62]. The primary objective of Mexican healthcare systems is to effectively address the issue of tobacco consumption by implementing advertising campaigns and initiatives to raise public awareness, particularly concerning lung cancer. This is achieved through the implementation of policies such as the reform of Mexico’s General Law for Tobacco Control, which mandates the creation of smoke-free environments in all enclosed public spaces and workplaces, along with a complete prohibition on the advertising, promotion, and sponsorship of tobacco products [
6,
62,
63].
4.4.2. Gastrointestinal tract cancer
Of cancers of the gastrointestinal tract, colorectal cancer has a higher incidence, which has increased in recent years at the national level. This fact coincides with the global trend since, from 1990 to 2019, the global incidence of colorectal cancer has increased more than double [
64]. Like Mexico, other low- and middle-income countries are experiencing an increase in incident cases of colorectal cancer. In contrast, in developed countries, there have been trends of decrease or stabilization [
65]. It is possible that these trends are influenced by an increase in the prevalence of risk factors associated with diet and lifestyle (e.g., physical inactivity and obesity) [
64]. In this regard, obesity and physical inactivity are two factors strongly associated with colorectal cancer [
66,
67] and are increasing nationally. Currently, 17% of the population is physically inactive [
68], and more than 70% is overweight or obese [
35]. These factors are modifiable, so there is the potential to prevent these cases. The fact that this cancer is one of the cancers with the highest incidence and mortality should place it as a priority within the design of the country’s public policies, which should focus on improving access to screening tests and early detection, which would help to reduce the number of cases and deaths.
4.4.3. Genitourinary system cancer
One of the most relevant tumors of the genitourinary system is prostate cancer, which holds the second highest position in terms of incidence. There is a prevailing tendency indicating a rise in the incidence of this ailment. Nevertheless, within the Latin American and Caribbean regions, Mexico exhibits a relatively low incidence rate, surpassing only Argentina, Honduras, Ecuador, and Bolivia [
69].
Another cancer of the genitourinary system with relevance in our country is testicular cancer, whose national incidence differs from that observed for the rest of the world. In Mexico, studies on the epidemiology and risk factors for this cancer type are lacking. This highlights the necessity for more studies in testicular cancer epidemiology to implement public policies, which could reduce the burden of this disease that presents a high number of DALYs when globally compared. Although the global incidence rate has increased, the mortality rate has improved [
70]; unfortunately, in this regard, Mexico has one of the highest mortality rates [
71]
4.4.4. Gynecological cancers
In the realm of gynecological cancers, breast and cervical cancer are the most frequently diagnosed. Over the past three decades, breast cancer has remained in the same position as the 3rd most prevalent malignant neoplasm, and by 2019, it represented 7.67% of total deaths, ranking in the fifth position, with a slight increase over the period. This increase can be attributed to numerous factors, such as changes in diet, physical activity, reproductive choices, and detection at a more advanced stage [
72,
73,
74,
75]. In Mexico, the prevalence of obesity continues to increase regardless of socioeconomic level, region, or locality, and numerous studies have found that obesity is a significant risk factor for developing this neoplasia [
72,
76,
77,
78]. A study found that women who followed the “World Cancer Research Fund” and the “American Institute of Cancer Research” recommendations regarding weight control had a 3-fold lower risk of developing breast cancer [
79]; meanwhile, Alarcon-Rojas showed that the Mexican population has a positive association between obesity and breast cancer [
80]. Lower-income populations have a greater burden of breast cancer, but it affects women of all ages and income levels [
14]. To assess this health challenge, in 2002, the Ministry of Health extended and expanded official health regulations and legislation concerning the management of breast cancer through a technical directive (Norma Oficial Mexicana) [
81].
The incidence of cervical cancer in Mexico has decreased significantly in recent years, thanks to successful campaigns aimed at combating human papillomavirus (HPV), such as the “HPV: Vaccination: Toward the elimination of Cervical Cancer in the Americas”. Chronic infection by oncogenic subtypes of HPV causes most cervical cancer cases; for instance, approximately 90% of cervical cancer cases occur in low- and middle-income countries where the absence of HPV vaccination and screening programs is evident [
82]. In 2012, Mexico launched a vaccination program for girls aged 11 years, which has since expanded to include boys as well. The program aims to reduce the overall burden of cervical cancer and other diseases caused by HPV [
83]. Approximately 80% of 11-year-old girls in Mexico were covered by these vaccination programs. However, in recent years, there has been a drastic decrease in coverage, from 11.22% in 2020 to 0.45% in 2021. This decline is mainly because health efforts were focused on managing the COVID-19 pandemic [
13].
5. Conclusions
In summary, it can be concluded that cancer remains a significant public health issue in Mexico, characterized by rising incidence and mortality rates. While these statistical trends do not apply directly to an individual patient, they play a pivotal role in helping governments, policymakers, health professionals, and researchers because they help understand the effect of cancer on the population. These trends allow them to create strategies to reduce the cancer burden and to control and treat cancer. The rising cancer burden in Mexico highlights the necessity for continuing efforts to address the underlying risk factors and improve access to screening tests, treatment, and patient care. However, with the right strategies and investments, it is possible to reduce the impact of cancer on the health of the Mexican population and improve the outcomes for people affected by this disease.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Supplementary Figure S1. National rank for 1990 and 2019 and global rank for 2019 of the number of new incident cases of the 21 groups of injuries and disease of the cause 2 level hierarchy of the GBD. Supplementary Figure S2. National rank for 1990 and 2019 and global rank for 2019 of the number of deaths due to the 21 groups of injuries and disease of the cause 2 level hierarchy of the GBD. Supplementary Figure S3. National rank for 1990 and 2019 and global rank for 2019 of the DALY counts due to the 21 groups of injuries and disease of the cause 2 level hierarchy of the GBD. Supplementary Figure S4. (a) National ranking and (b) percentage of annual change from 1990 to 2019 of the DALY counts due to each of the 29 groups of malignant neoplasms mapped by the GBD. Supplementary Figure S5. Cancer-specific trends and annual percentage of change from 1990 to 2019 of the age-standardized rate of incidence (per 100,000 people) in Mexico. Supplementary Figure S6. Cancer-specific trends and annual percentage of change from 1990 to 2019 of the age-standardized rate of DALYs (per 100,000 people) in Mexico. Supplementary Figure S7. Sex- and age-specific distribution of DALYs (a) due to malignant neoplasms in Mexico during 2019, cancer-specific DALY counts (b) and age-standardized rate of death per 100,000 people (c) by sex. Supplementary Figure S8. Cancer-specific incident cases and age-standardized rate of death (per 100,000 people) by sex (b) in Mexico during 2019. Supplementary Figure S9. Age-specific rate of incidence (per 100,000 people) by sex for each group of cancers in Mexico during 2019. Supplementary Figure S10. Age-specific rate of DALYs (per 100,000 people) by sex for each group of cancers in Mexico during 2019. Supplementary Table S1. Total and sex-specific age-standardized rates of incidence, mortality, and DALYs (per 100,000 people) by cancer group in Mexico during 2019. Supplementary Table S2. Total and sex-specific DALY counts by cancer group in Mexico during 2019. Supplementary Table S3. Percentage of change from 1990 to 2019 of the crude incidence, deaths, and DALYs due to 29 malignant neoplasms in Mexico. Supplementary Table S4. Percentage of change from 1990 to 2019 of the age-standardized rate of incidence, deaths, and DALYs (per 100,000 people) due to 29 malignant neoplasms in Mexico.
Author Contributions
Conceptualization, SABO and DD; methodology, DD; software and formal analysis, DD; investigation, ELV, EPGG, KLL; resources, JACG; data curation, DD; writing—original draft preparation, SABO, ELV, KLL, and DD; writing—review and editing, EHLF, MATR, JMMO, DLCA, ELL, JRZL, HMCD, MMM, BAB, JLRT, DECL, VACR, RL, LCA, ECU, and FGV; visualization, DD; supervision, SABO and DD; project administration, SABO and DD. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Given that this is a secondary analysis of publicly available results, the study did not require ethical approval.
Informed Consent Statement
Not applicable because this study did not involve humans because it was based on estimations produced by another study.
Data Availability Statement
All data used to produce this study are publicly available from the GBD Results tool at the online website of the Global Health Data Exchange
https://ghdx.healthdata.org.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018, 68, 394-424. [CrossRef]
- Bray, F.; Laversanne, M.; Weiderpass, E.; Soerjomataram, I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer 2021, 127, 3029-3030. [CrossRef]
- Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; Xu, R.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol 2022, 8, 420-444. [CrossRef]
- Lin, L.; Li, Z.; Yan, L.; Liu, Y.; Yang, H.; Li, H. Global, regional, and national cancer incidence and death for 29 cancer groups in 2019 and trends analysis of the global cancer burden, 1990-2019. J Hematol Oncol 2021, 14, 197. [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021, 71, 209-249. [CrossRef]
- Tran, K.B.; Lang, J.J.; Compton, K.; Xu, R.; Acheson, A.R.; Henrikson, H.J.; Kocarnik, J.M.; Penberthy, L.; Aali, A.; Abbas, Q. The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2022, 400, 563-591. [CrossRef]
- United Nations. Sustainable Development Goals: Mexico Partnership Landscape Assessment; United Nations: Geneve, 2021; p. 37.
- Fitzmaurice, C.; Abate, D.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdel-Rahman, O.; Abdelalim, A.; Abdoli, A.; Abdollahpour, I.; Abdulle, A.S.M.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2019, 5, 1749-1768. [CrossRef]
- Espinosa-Tamez, P.; Suazo-Zepeda, E.; Sánchez-Blas, H.; Meneses-Medina, M.; Huitzil-Meléndez, F.D.; Van Loon, K.; Potter, M.B.; Lajous, M. National and state-level colorectal cancer mortality trends in Mexico, 1998-2018. salud pública de méxico 2022, 64, 5-13. [CrossRef]
- Torres-Dominguez, J.A.; Betancourt, A.M.; Mejia, L.S.P.; Noveron, N.R. Lung cancer mortality trends in Mexico, 1998-2018: the impact of the General Law on Tobacco Control. Rev Bras Epidemiol 2022, 25, e220003. [CrossRef]
- Beltran-Ontiveros, S.A.; Fernandez-Galindo, M.A.; Moreno-Ortiz, J.M.; Contreras-Gutierrez, J.A.; Madueña-Molina, J.; Arambula-Meraz, E.; Leal-Leon, E.; Becerril-Camacho, D.M.; Picos-Cardenas, V.J.; Angulo-Rojo, C. Incidence, Mortality, and Trends of Prostate Cancer in Mexico from 2000 to 2019: Results from the Global Burden of Disease Study 2019. Cancers 2022, 14, 3184. [CrossRef]
- Torres-Sánchez, L.E.; Espinoza-Giacinto, R.; Rojas-Martínez, R.; Escamilla-Nuñez, C.; Vázquez-Salas, R.A.; Campuzano, J.C.; Lazcano-Ponce, E. Comportamiento de la mortalidad por cáncer de próstata en México de acuerdo al índice de marginación estatal, de 1980 a 2013. Salud Pública de México 2016, 58, 179-186.
- Munoz-Bello, J.O.; Carrillo-Garcia, A.; Lizano, M. Epidemiology and Molecular Biology of HPV Variants in Cervical Cancer: The State of the Art in Mexico. Int J Mol Sci 2022, 23, 8566. [CrossRef]
- Knaul, F.M.; Nigenda, G.; Lozano, R.; Arreola-Ornelas, H.; Langer, A.; Frenk, J. Breast cancer in Mexico: a pressing priority. Reprod Health Matters 2008, 16, 113-123. [CrossRef]
- Rojas, C.A.A.; Alvarez-Bañuelos, M.T.; Morales-Romero, J.; Suárez-Díaz, H.; Hernández-Fonseca, J.C.; Contreras-Alarcón, G. Breast cancer: metastasis, molecular subtypes, and overweight and obesity in Veracruz, Mexico. Clinical breast cancer 2019, 19, e166-e171. [CrossRef]
- Malvezzi, M.; Bosetti, C.; Chatenoud, L.; Rodriguez, T.; Levi, F.; Negri, E.; La Vecchia, C. Trends in cancer mortality in Mexico, 1970-1999. Ann Oncol 2004, 15, 1712-1718. [CrossRef]
- Gomez-Dantes, H.; Lamadrid-Figueroa, H.; Cahuana-Hurtado, L.; Silverman-Retana, O.; Montero, P.; Gonzalez-Robledo, M.C.; Fitzmaurice, C.; Pain, A.; Allen, C.; Dicker, D.J.; et al. The burden of cancer in Mexico, 1990-2013. Salud Publica Mex 2016, 58, 118-131. [CrossRef]
- Mohar-Betancourt, A.; Reynoso-Noveron, N.; Armas-Texta, D.; Gutierrez-Delgado, C.; Torres-Dominguez, J.A. Cancer Trends in Mexico: Essential Data for the Creation and Follow-Up of Public Policies. J Glob Oncol 2017, 3, 740-748. [CrossRef]
- Aldaco-Sarvide, F.; Pérez-Pérez, P.; Cervantes-Sánchez, M.G.; Torrecillas-Torres, L.; Erazo-Valle-Solís, A.A.; Cabrera-Galeana, P.; Motola-Kuba, D.; Anaya, P.; Rivera, S.; Cárdenas-Cárdenas, E. Mortality from cancer in Mexico: 2015 update. Gaceta Mexicana de Oncolog�a 2022, 17. [CrossRef]
- Chatenoud, L.; Bertuccio, P.; Bosetti, C.; Malvezzi, M.; Levi, F.; Negri, E.; La Vecchia, C. Trends in mortality from major cancers in the Americas: 1980-2010. Ann Oncol 2014, 25, 1843-1853. [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2020, 396, 1204-1222. [CrossRef]
- Murray, C.J.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2020, 396, 1223-1249. [CrossRef]
- Vollset, S.E.; Goren, E.; Yuan, C.-W.; Cao, J.; Smith, A.E.; Hsiao, T.; Bisignano, C.; Azhar, G.S.; Castro, E.; Chalek, J. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. The Lancet 2020, 396, 1285-1306.
- Wang, H.; Abbas, K.M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; Abolhassani, H.; Abreu, L.G.; Abrigo, M.R. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. The Lancet 2020, 396, 1160-1203. [CrossRef]
- Lopez-Bago, A.; Lascurain, R.; Hernandez-Carreño, P.E.; Gallardo-Vera, F.; Argueta-Donohue, J.; Jimenez-Trejo, F.; Fuentes-Zavaleta, D.A.; Beltran-Ontiveros, S.A.; Becerril-Camacho, D.M.; Contreras-Rodriguez, V.A. Sex, Age, and Regional Disparities in the Burden of Asthma in Mexico from 1990 to 2019: A Secondary Analysis of the Global Burden of Disease Study 2019. 2023. [CrossRef]
- Madueña-Angulo, S.E.; Beltran-Ontiveros, S.A.; Leal-Leon, E.; Contreras-Gutierrez, J.A.; Lizarraga-Verdugo, E.; Gutierrez-Arzapalo, P.Y.; Lizarraga-Velarde, S.; Romo-Garcia, E.; Montero-Vela, J.; Moreno-Ortiz, J.M. National sex-and age-specific burden of blindness and vision impairment by cause in Mexico in 2019: a secondary analysis of the Global Burden of Disease Study 2019. The Lancet Regional Health–Americas 2023, 24. [CrossRef]
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age standardization of rates: a new WHO standard. Geneva: World Health Organization 2001, 9, 1-14.
- Instiute, N.C. Cancer Statistics. Available online: https://www.cancer.gov/about-cancer/understanding/statistics (accessed on September).
- Espinosa-Tamez, P.; Suazo-Zepeda, E.; Sánchez-Blas, H.; Meneses-Medina, M.; Huitzil-Meléndez, F.D.; Van Loon, K.; Potter, M.; Lajous, M. National and state-level colorectal cancer mortality trends in Mexico, 1998-2018. Salud Publica Mex 2021, 64, 5-13. [CrossRef]
- Sharma, R.; Abbasi-Kangevari, M.; Abd-Rabu, R.; Abidi, H.; Abu-Gharbieh, E.; Acuna, J.M.; Adhikari, S.; Advani, S.M.; Afzal, M.S.; Meybodi, M.A. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The lancet Gastroenterology & hepatology 2022, 7, 627-647. [CrossRef]
- Morgan, E.; Arnold, M.; Gini, A.; Lorenzoni, V.; Cabasag, C.; Laversanne, M.; Vignat, J.; Ferlay, J.; Murphy, N.; Bray, F. Global burden of colorectal cancer in 2020 and 2040: Incidence and mortality estimates from GLOBOCAN. Gut 2023, 72, 338-344. [CrossRef]
- Gu, W.-J.; Pei, J.-P.; Lyu, J.; Akimoto, N.; Haruki, K.; Ogino, S.; Zhang, C.-D. The burden of early-onset colorectal cancer and its risk factors from 1990 to 2019: A systematic analysis for the global burden of disease study 2019. Cancers 2022, 14, 3502. [CrossRef]
- Reynoso-Noveron, N.; Meneses-Garcia, A.; Erazo-Valle, A.; Escudero-de Los Rios, P.; Kuri-Morales, P.A.; Mohar-Betancourt, A. Challenges in the development and implementation of the National Comprehensive Cancer Control Program in Mexico. Salud Publica Mex 2016, 58, 325-333. [CrossRef]
- Yildirim-Kahriman, S. Non-intrinsic cancer risk factors. Exp Oncol 2021, 43, 290-297. [CrossRef]
- Shamah-Levy T, V.-O.E., Heredia-Hernández O, Romero-Martínez M, Mojica-Cuevas J, Cuevas-Nasu L,; Santaella-Castell JA, R.-D.J. Encuesta Nacional de Salud y Nutrición 2018-19: Resultados Nacionales; Instituto Nacional de Salud Pública, 2020.: Cuernavaca, México, 2020.
- Haupt, S.; Caramia, F.; Klein, S.L.; Rubin, J.B.; Haupt, Y. Sex disparities matter in cancer development and therapy. Nat Rev Cancer 2021, 21, 393-407. [CrossRef]
- Dong, M.; Cioffi, G.; Wang, J.; Waite, K.A.; Ostrom, Q.T.; Kruchko, C.; Lathia, J.D.; Rubin, J.B.; Berens, M.E.; Connor, J. Sex differences in cancer incidence and survival: a pan-cancer analysis. Cancer Epidemiology, Biomarkers & Prevention 2020, 29, 1389-1397. [CrossRef]
- Dorak, M.T.; Karpuzoglu, E. Gender differences in cancer susceptibility: an inadequately addressed issue. Front Genet 2012, 3, 268. [CrossRef]
- Kim, H.I.; Lim, H.; Moon, A. Sex Differences in Cancer: Epidemiology, Genetics and Therapy. Biomol Ther (Seoul) 2018, 26, 335-342. [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat Rev Immunol 2016, 16, 626-638. [CrossRef]
- Tricarico, R.; Nicolas, E.; Hall, M.J.; Golemis, E.A. X-and Y-linked chromatin-modifying genes as regulators of sex-specific cancer incidence and prognosis. Clinical Cancer Research 2020, 26, 5567-5578. [CrossRef]
- Tazuma, S. Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best practice & research Clinical gastroenterology 2006, 20, 1075-1083. [CrossRef]
- Rawla, P.; Sunkara, T.; Thandra, K.C.; Barsouk, A. Epidemiology of gallbladder cancer. Clinical and experimental hepatology 2019, 5, 93-102. [CrossRef]
- Henley, S.J.; Thomas, C.C.; Sharapova, S.R.; Momin, B.; Massetti, G.M.; Winn, D.M.; Armour, B.S.; Richardson, L.C. Vital signs: disparities in tobacco-related cancer incidence and mortality—United States, 2004–2013. Morbidity and mortality weekly report 2016, 65, 1212-1218. [CrossRef]
- Edgren, G.; Liang, L.; Adami, H.O.; Chang, E.T. Enigmatic sex disparities in cancer incidence. Eur J Epidemiol 2012, 27, 187-196. [CrossRef]
- Fraumeni, J.F., Jr. Cancers of the pancreas and biliary tract: epidemiological considerations. Cancer Res 1975, 35, 3437-3446.
- Afshar, N.; English, D.R.; Thursfield, V.; Mitchell, P.L.; Te Marvelde, L.; Farrugia, H.; Giles, G.G.; Milne, R.L. Differences in cancer survival by sex: a population-based study using cancer registry data. Cancer Causes & Control 2018, 29, 1059-1069. [CrossRef]
- Jung, K.-W.; Park, S.; Shin, A.; Oh, C.-M.; Kong, H.-J.; Jun, J.K.; Won, Y.-J. Do female cancer patients display better survival rates compared with males? Analysis of the Korean National Registry data, 2005–2009. PloS one 2012, 7, e52457. [CrossRef]
- Oberaigner, W.; Siebert, U. Do women with cancer have better survival as compared to men after adjusting for staging distribution? The European Journal of Public Health 2011, 21, 387-391. [CrossRef]
- Kitahara, C.M.; Schneider, A.B. Epidemiology of thyroid cancer. Cancer epidemiology, biomarkers & prevention 2022, 31, 1284-1297. [CrossRef]
- LeClair, K.; Bell, K.J.; Furuya-Kanamori, L.; Doi, S.A.; Francis, D.O.; Davies, L. Evaluation of gender inequity in thyroid cancer diagnosis: differences by sex in US thyroid cancer incidence compared with a meta-analysis of subclinical thyroid cancer rates at autopsy. JAMA internal medicine 2021, 181, 1351-1358. [CrossRef]
- Laconi, E.; Marongiu, F.; DeGregori, J. Cancer as a disease of old age: changing mutational and microenvironmental landscapes. British journal of cancer 2020, 122, 943-952. [CrossRef]
- Hashim, D.; Carioli, G.; Malvezzi, M.; Bertuccio, P.; Waxman, S.; Negri, E.; La Vecchia, C.; Boffetta, P. Cancer mortality in the oldest old: a global overview. Aging (Albany NY) 2020, 12, 16744-16758. [CrossRef]
- Bhakta, N.; Force, L.M.; Allemani, C.; Atun, R.; Bray, F.; Coleman, M.P.; Steliarova-Foucher, E.; Frazier, A.L.; Robison, L.L.; Rodriguez-Galindo, C. Childhood cancer burden: a review of global estimates. The lancet oncology 2019, 20, e42-e53. [CrossRef]
- Miller, K.D.; Fidler-Benaoudia, M.; Keegan, T.H.; Hipp, H.S.; Jemal, A.; Siegel, R.L. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin 2020, 70, 443-459. [CrossRef]
- Ruiz-Arguelles, G.J. Advances in the diagnosis and treatment of acute and chronic leukemia in Mexico. Salud Publica Mex 2016, 58, 291-295. [CrossRef]
- Sullivan, R.; Kowalczyk, J.R.; Agarwal, B.; Ladenstein, R.; Fitzgerald, E.; Barr, R.; Steliarova-Foucher, E.; Magrath, I.; Howard, S.C.; Kruger, M.; et al. New policies to address the global burden of childhood cancers. Lancet Oncol 2013, 14, e125-135. [CrossRef]
- Cotlear, D. Population aging: is Latin America ready?; World Bank Publications: 2010.
- Foster, J.A.; Salinas, G.D.; Mansell, D.; Williamson, J.C.; Casebeer, L.L. How does older age influence oncologists’ cancer management? The Oncologist 2010, 15, 584-592. [CrossRef]
- Zhang, Y.; Luo, G.; Etxeberria, J.; Hao, Y. Global Patterns and Trends in Lung Cancer Incidence: A Population-Based Study. J Thorac Oncol 2021, 16, 933-944. [CrossRef]
- DOF. Diario Oficial de la Federación, Ley General para el Control del Tabaco. 2008.
- Organization, P.A.H. Reform of Mexico’s General Law on Tobacco Control establishes 100% smoke-free environments. Available online: https://www.paho.org/en/news/17-12-2021-reform-mexicos-general-law-tobacco-control-establishes-100-smoke-free-environments (accessed on june).
- Whiteman, D.C.; Wilson, L.F. The fractions of cancer attributable to modifiable factors: A global review. Cancer Epidemiol 2016, 44, 203-221. [CrossRef]
- Sharma, R.; Abbasi-Kangevari, M.; Abd-Rabu, R.; Abidi, H.; Abu-Gharbieh, E.; Acuna, J.M.; Adhikari, S.; Advani, S.M.; Afzal, M.S.; Aghaie Meybodi, M.; et al. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Gastroenterology & Hepatology 2022, 7, 627-647. [CrossRef]
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683-691. [CrossRef]
- Cong, Y.J.; Gan, Y.; Sun, H.L.; Deng, J.; Cao, S.Y.; Xu, X.; Lu, Z.X. Association of sedentary behaviour with colon and rectal cancer: a meta-analysis of observational studies. Br J Cancer 2014, 110, 817-826. [CrossRef]
- Mandic, M.; Li, H.; Safizadeh, F.; Niedermaier, T.; Hoffmeister, M.; Brenner, H. Is the association of overweight and obesity with colorectal cancer underestimated? An umbrella review of systematic reviews and meta-analyses. European Journal of Epidemiology 2023, 38, 135-144. [CrossRef]
- Medina, C.; Jauregui, A.; Hernandez, C.; Shamah, T.; Barquera, S. Physical inactivity and sitting time prevalence and trends in Mexican adults. Results from three national surveys. PLoS One 2021, 16, e0253137. [CrossRef]
- Piñeros, M.; Laversanne, M.; Barrios, E.; Cancela, M.C.; de Vries, E.; Pardo, C.; Bray, F. An updated profile of the cancer burden, patterns and trends in Latin America and the Caribbean. Lancet Reg Health Am 2022, 13, None. [CrossRef]
- Pishgar, F.; Haj-Mirzaian, A.; Ebrahimi, H.; Saeedi Moghaddam, S.; Mohajer, B.; Nowroozi, M.R.; Ayati, M.; Farzadfar, F.; Fitzmaurice, C.; Amini, E. Global, regional and national burden of testicular cancer, 1990-2016: results from the Global Burden of Disease Study 2016. BJU Int 2019, 124, 386-394. [CrossRef]
- Znaor, A.; Skakkebaek, N.E.; Rajpert-De Meyts, E.; Kulis, T.; Laversanne, M.; Gurney, J.; Sarfati, D.; McGlynn, K.A.; Bray, F. Global patterns in testicular cancer incidence and mortality in 2020. Int J Cancer 2022, 151, 692-698. [CrossRef]
- Avgerinos, K.I.; Spyrou, N.; Mantzoros, C.S.; Dalamaga, M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism 2019, 92, 121-135. [CrossRef]
- Chavarri-Guerra, Y.; Villarreal-Garza, C.; Liedke, P.E.; Knaul, F.; Mohar, A.; Finkelstein, D.M.; Goss, P.E. Breast cancer in Mexico: a growing challenge to health and the health system. Lancet Oncol 2012, 13, e335-343. [CrossRef]
- Ginsburg, O.; Bray, F.; Coleman, M.P.; Vanderpuye, V.; Eniu, A.; Kotha, S.R.; Sarker, M.; Huong, T.T.; Allemani, C.; Dvaladze, A.; et al. The global burden of women’s cancers: a grand challenge in global health. Lancet 2017, 389, 847-860. [CrossRef]
- Sharma, R. Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990-2016: evidence from Global Burden of Disease Study 2016. Breast Cancer 2019, 26, 428-445. [CrossRef]
- Baena Ruiz, R.; Salinas Hernández, P. Diet and cancer: Risk factors and epidemiological evidence. Maturitas 2014, 77, 202-208. [CrossRef]
- González Svatetz, C.A.; Goday Arnó, A. Obesidad y cáncer:«las amistades peligrosas». Med. clín (Ed. impr.) 2015, 24-30.
- Barquera, S.; Hernández-Barrera, L.; Trejo, B.; Shamah, T.; Campos-Nonato, I.; Rivera-Dommarco, J. Obesity in Mexico, prevalence and trends in adults. Ensanut 2018-19. Salud Pública de México 2020, 62, 682-692. [CrossRef]
- Castello, A.; Martin, M.; Ruiz, A.; Casas, A.M.; Baena-Cañada, J.M.; Lope, V.; Antolin, S.; Sanchez, P.; Ramos, M.; Anton, A. Lower breast cancer risk among women following the World Cancer Research Fund and American Institute for Cancer Research lifestyle recommendations: EpiGEICAM case-control study. PloS one 2015, 10, e0126096. [CrossRef]
- Alarcón Rojas, C.A.; Alvarez-Bañuelos, M.T.; Morales-Romero, J.; Suárez-Díaz, H.; Hernández-Fonseca, J.C.; Contreras-Alarcón, G. Breast Cancer: Metastasis, Molecular Subtypes, and Overweight and Obesity in Veracruz, Mexico. Clinical Breast Cancer 2019, 19, e166-e171. [CrossRef]
- Diario Oficial de la Federación. NORMA Oficial Mexicana NOM-041-SSA2-2011, Para la prevención, diagnóstico, tratamiento, control y vigilancia epidemiológica del cáncer de mama. Recuperado desde http://www. dof. gob. mx/nota_detalle. php% 3Fcodigo% 3D5194157% 26fecha% 3D09/06 2011.
- Cohen, P.A.; Jhingran, A.; Oaknin, A.; Denny, L. Cervical cancer. Lancet 2019, 393, 169-182. [CrossRef]
- Restrepo, F.D.l.H.; Guzman, N.A.; Gomez, A.D.l.H.; Ruiz, C. Policies and processes for human papillomavirus vaccination in Latin America and the Caribbean. Revista Panamericana de Salud Pública 2018, 41, e124.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).