Submitted:
30 November 2023
Posted:
30 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
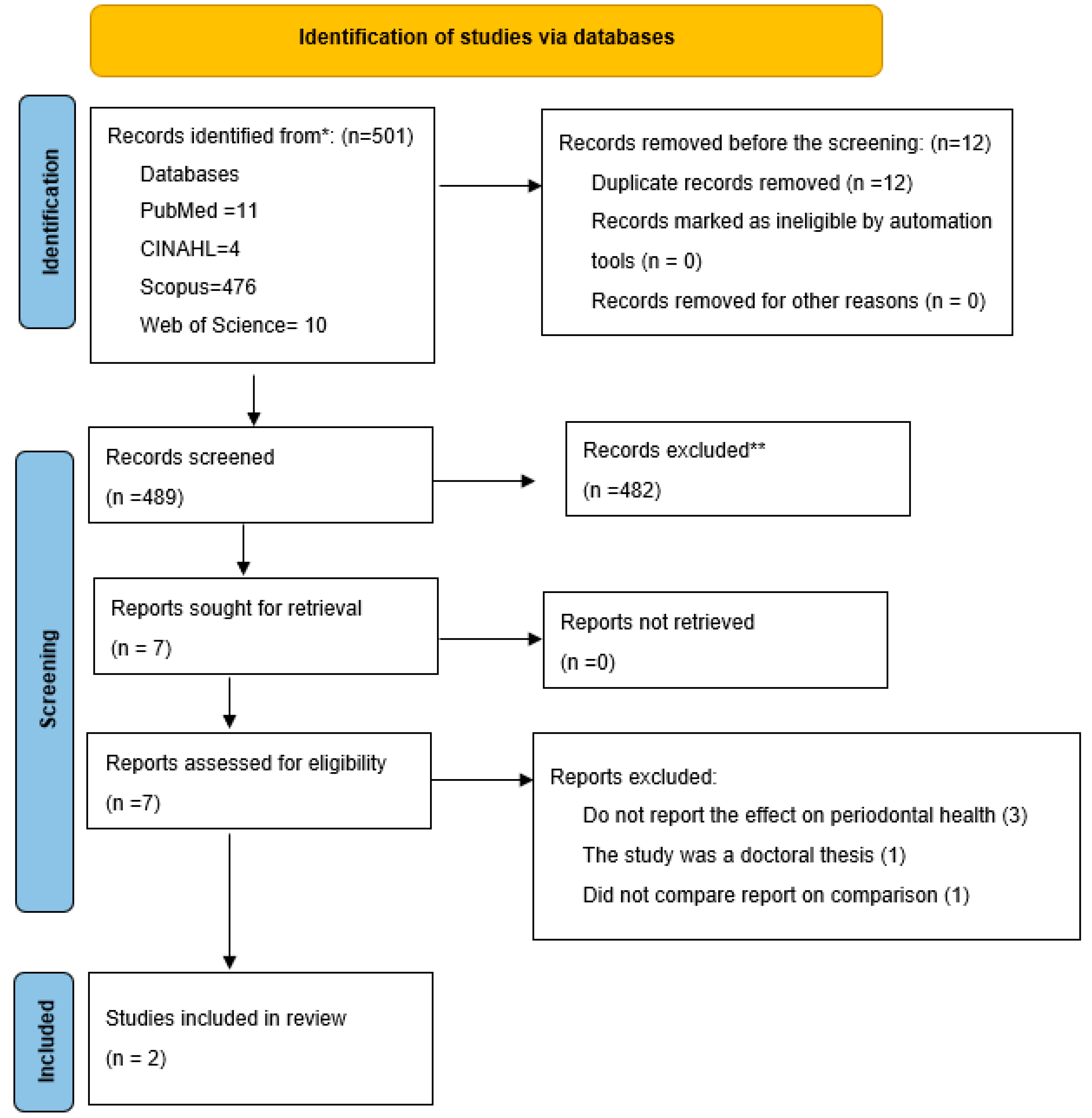
2. Materials and Methods
2.1. Research Question
2.2. Article Identification
2.3. Eligibility Criteria
2.4. Article Selection
2.5. Data Charting
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| S/N | Key words | Search trend |
| Smoking | (TS=(Cigar Smoking)) OR TS=(Cigarette Smoking) and Preprint Citation Index (Exclude – Database) | |
| Smokeless tobacco: | (((((((((((((((((((((TS=(Smokeless Tobacco)) OR TS=(Tobaccos, Smokeless)) OR TS=(Gutka)) OR TS=(Gutkas)) OR TS=(Gutka Tobacco)) OR TS=(Gutka Tobaccos)) OR TS=(Tobacco, Gutka)) OR TS=(Tobaccos, Gutka)) OR TS=(Snus)) OR TS=(Dipping Tobacco)) OR TS=(Dipping Tobaccos)) OR TS=(Tobacco, Dipping)) OR TS=(Tobaccos, Dipping)) OR TS=(Oral Tobacco)) OR TS=(Tobacco, Oral)) OR TS=(Chewing Tobacco)) OR TS=(Chewing Tobaccos)) OR TS=(Tobacco, Chewing)) OR TS=(Tobaccos, Chewing)) OR TS=(Snuff)) OR TS=(Mint Snuff)) OR TS=(Snuff, Mint) and Preprint Citation Index (Exclude – Database) | |
| Periodontium | ((((((((((TS=(Periodontiums)) OR TS=(Tooth Supporting Structures)) OR TS=(Structure, Tooth Supporting)) OR TS=(Structures, Tooth Supporting)) OR TS=(Supporting Structure, Tooth)) OR TS=(Supporting Structures, Tooth)) OR TS=(Tooth Supporting Structure)) OR TS=(Parodontium)) OR TS=(Parodontiums)) OR TS=(Paradentium)) OR TS=(Paradentiums) and Preprint Citation Index (Exclude – Database) | |
| Health | (((((TS=(Individual Health)) OR TS=(Health, Individual)) OR TS=(Normality)) OR TS=(Normalities)) OR TS=(Normalcy)) OR TS=(Normalcies) and Preprint Citation Index (Exclude – Database) |
| S/N | Keyword | Search terms |
| 1 | Smoking | TI smoking OR TI ( tobacco or smoking or nicotine or cigarettes ) OR TI tobacco smoking |
| 2 | Periodontium | TI periodontium OR TI ( parodontitis or periodontitis or tooth loss ) OR TI Tooth Supporting Structure OR TI Paradentium OR TI ( periodontitis or periodontal disease ) |
| 3 | Smokeless Tobacco | TI smokeless tobacco OR TI ( smokeless tobacco or gutka ) |
| 4 | Health | |
| S/N | Keyword | Search terms |
| 1 | Smoking | "Smoking"[Title/Abstract] OR "cigar smoking"[Title/Abstract] OR "cigarette smoking"[Title/Abstract] |
| 2 | Smokeless Tobacco | "smokeless tobacco"[Title/Abstract] OR (("Tobacco"[MeSH Terms] OR "Tobacco"[All Fields] OR "tobacco products"[MeSH Terms] OR ("Tobacco"[All Fields] AND "products"[All Fields]) OR "tobacco products"[All Fields] OR "Tobaccos"[All Fields] OR "tobacco s"[All Fields]) AND "Smokeless"[Title/Abstract]) OR "Gutka"[Title/Abstract] OR "Gutkas"[Title/Abstract] OR "gutka tobacco"[Title/Abstract] OR (("tobacco, smokeless"[MeSH Terms] OR ("Tobacco"[All Fields] AND "Smokeless"[All Fields]) OR "smokeless tobacco"[All Fields] OR "Gutka"[All Fields]) AND "Tobaccos"[Title/Abstract]) OR "tobacco gutka"[Title/Abstract] OR (("Tobacco"[MeSH Terms] OR "Tobacco"[All Fields] OR "tobacco products"[MeSH Terms] OR ("Tobacco"[All Fields] AND "products"[All Fields]) OR "tobacco products"[All Fields] OR "Tobaccos"[All Fields] OR "tobacco s"[All Fields]) AND "Gutka"[Title/Abstract]) OR "Snus"[Title/Abstract] OR "dipping tobacco"[Title/Abstract] OR (("dipped"[All Fields] OR "Dipping"[All Fields] OR "dippings"[All Fields]) AND "Tobaccos"[Title/Abstract]) OR "tobacco dipping"[Title/Abstract] OR (("Tobacco"[MeSH Terms] OR "Tobacco"[All Fields] OR "tobacco products"[MeSH Terms] OR ("Tobacco"[All Fields] AND "products"[All Fields]) OR "tobacco products"[All Fields] OR "Tobaccos"[All Fields] OR "tobacco s"[All Fields]) AND "Dipping"[Title/Abstract]) OR "oral tobacco"[Title/Abstract] OR "tobacco oral"[Title/Abstract] OR "chewing tobacco"[Title/Abstract] OR "chewing tobaccos"[Title/Abstract] OR "tobacco chewing"[Title/Abstract] OR "tobaccos chewing"[Title/Abstract] OR "Snuff"[Title/Abstract] OR "mint snuff"[Title/Abstract] OR (("tobacco, smokeless"[MeSH Terms] OR ("Tobacco"[All Fields] AND "Smokeless"[All Fields]) OR "smokeless tobacco"[All Fields] OR "Snuff"[All Fields] OR "snuffs"[All Fields]) AND "Mint"[Title/Abstract]) |
| 3 | Periodontium | "Periodontium"[Title/Abstract] OR "Periodontiums"[Title/Abstract] OR "tooth supporting structures"[Title/Abstract] OR (("structural"[All Fields] OR "structurally"[All Fields] OR "structurals"[All Fields] OR "structuration"[All Fields] OR "structurations"[All Fields] OR "Structure"[All Fields] OR "structure s"[All Fields] OR "structured"[All Fields] OR "Structures"[All Fields] OR "structuring"[All Fields]) AND "tooth supporting"[Title/Abstract]) OR (("structural"[All Fields] OR "structurally"[All Fields] OR "structurals"[All Fields] OR "structuration"[All Fields] OR "structurations"[All Fields] OR "Structure"[All Fields] OR "structure s"[All Fields] OR "structured"[All Fields] OR "Structures"[All Fields] OR "structuring"[All Fields]) AND "tooth supporting"[Title/Abstract]) OR (("support"[All Fields] OR "support s"[All Fields] OR "supported"[All Fields] OR "supporter"[All Fields] OR "supporter s"[All Fields] OR "supporters"[All Fields] OR "Supporting"[All Fields] OR "supportive"[All Fields] OR "supportiveness"[All Fields] OR "supports"[All Fields]) AND "structure tooth"[Title/Abstract]) OR "supporting structures tooth"[Title/Abstract] OR "tooth supporting structure"[Title/Abstract] OR "Parodontium"[Title/Abstract] OR "Paradentium"[Title/Abstract] OR "Paradentiums"[Title/Abstract] |
| 4 | Health | "Health"[Title/Abstract] OR "individual health"[Title/Abstract] OR "health individual"[Title/Abstract] OR "Normality"[Title/Abstract] OR "Normalities"[Title/Abstract] OR "Normalcy"[Title/Abstract] OR "Normalcies"[Title/Abstract] |
| S/N | Keyword | Search terms |
| #1 | Smoking | smoking OR cigar AND smoking OR cigarette AND smoking |
| #2 | Smokeless tobacco | smokeless AND tobacco OR chewing AND tobacco OR snuff OR oral AND tobacco |
| #3 | #1 OR #2 | |
| #4 | periodontal health | periodontal AND health |
| #5 | #3 AND #5 |
References
- Lang NP, Bartold PM. Periodontal health. J. Periodontol. 2018, 89, S9–S16. [Google Scholar] [CrossRef]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef]
- Wulandari, P.; Masulili, S.L.C.; Soeroso, Y. Quality of Life and Its Relationship with Periodontal Disease. Dentika Dent. J. 2022, 25, 97–102. [Google Scholar] [CrossRef]
- Laxman, V.K.; Annaji, S. Tobacco Use and Its Effects on the Periodontium and Periodontal Therapy. J. Contemp. Dent. Pr. 2008, 9, 97–107. [Google Scholar] [CrossRef]
- Yap, A. Oral Health Equals Total Health: A Brief Review. J. Dent. Indones. 2017, 24. [Google Scholar] [CrossRef]
- Singh B, Singh R. Gingivitis–A silent disease. J. Dent. Med. Sci. 2013, 6, 30–33. [Google Scholar] [CrossRef]
- Herrera, D.; Sanz, M.; Shapira, L.; Brotons, C.; Chapple, I.; Frese, T.; Graziani, F.; Hobbs, F.D.R.; Huck, O.; Hummers, E.; et al. Association between periodontal diseases and cardiovascular diseases, diabetes and respiratory diseases: Consensus report of the Joint Workshop by the European Federation of Periodontology (EFP) and the European arm of the World Organization of Family Doctors (WONCA Europe). J. Clin. Periodontol. 2023, 50, 819–841. [Google Scholar] [CrossRef]
- Liccardo, D.; Cannavo, A.; Spagnuolo, G.; Ferrara, N.; Cittadini, A.; Rengo, C.; Rengo, G. Periodontal Disease: A Risk Factor for Diabetes and Cardiovascular Disease. Int. J. Mol. Sci. 2019, 20, 1414. [Google Scholar] [CrossRef]
- Ong, M.M.; Wang, H.-L. Periodontic and orthodontic treatment in adults. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 420–428. [Google Scholar] [CrossRef]
- Bergstrom, J.; Keilani, H.; Lundholm, C.; Radestad, U. Smokeless tobacco (snuff) use and periodontal bone loss. J. Clin. Periodontol. 2006, 33, 549–554. [Google Scholar] [CrossRef]
- Moimaz, S.; Zina, L.; Saliba, O.; Garbin, C. Smoking and periodontal disease: Clinical evidence for an association. Prim. Dent. Care 2010, 7, 84–84. [Google Scholar] [CrossRef]
- Hagh, L.G.; Zakavi, F.; Ansarifar, S.; Ghasemzadeh, O.; Solgi, G. Association of dental caries and salivary sIgA with tobacco smoking. Aust. Dent. J. 2013, 58, 219–223. [Google Scholar] [CrossRef]
- Huang, X.-Z.; Zhu, L.-B.; Li, Z.-R.; Lin, J. Bacterial colonization and intestinal mucosal barrier development. World J. Clin. Pediatr. 2013, 2, 46–53. [Google Scholar] [CrossRef]
- Wu, Y.; Dong, G.; Xiao, W.; Xiao, E.; Miao, F.; Syverson, A.; Missaghian, N.; Vafa, R.; Cabrera-Ortega, A.; Rossa, C.; et al. Effect of Aging on Periodontal Inflammation, Microbial Colonization, and Disease Susceptibility. J. Dent. Res. 2016, 95, 460–466. [Google Scholar] [CrossRef]
- Martu M-A, Maftei G-A, Luchian I, Popa C, Filioreanu A-M, Tatarciuc D, et al. Wound healing of periodontal and oral tissues: Part II—Patho-phisiological conditions and metabolic diseases. Rom. J. Oral. Rehabil. 2020, 12, 30–40. [Google Scholar]
- Burrows, S. Root Caries Part 1: an Overview of the Challenges. Dent. Updat. 2020, 47, 103–114. [Google Scholar] [CrossRef]
- Sheiham, A. Dietary effects on dental diseases. . Public. Health Nutr. 2001, 4, 569–591. [Google Scholar] [CrossRef]
- Yu, C.; Abbott, P. An overview of the dental pulp: its functions and responses to injury. Aust. Dent. J. 2007, 52, S4–S6. [Google Scholar] [CrossRef]
- Javed, F.; Rahman, I.; Romanos, G.E. Tobacco-product usage as a risk factor for dental implants. Periodontology 2000 2019, 81, 48–56. [Google Scholar] [CrossRef]
- Yu, B.; Wang, C. Osteoporosis and periodontal diseases – An update on their association and mechanistic links. Periodontology 2000 2022, 89, 99–113. [Google Scholar] [CrossRef]
- 21. World Health Organization. Guidance on COVID-19 for the care of older people and people living in long-term care facilities, other non-acute care facilities and home care. WHO Regional Office for the Western Pacific;
- Bates, C.; Fagerström, K.; Jarvis, M.J.; Kunze, M.; McNeill, A.; Ramström, L. European Union policy on smokeless tobacco: a statement in favour of evidence based regulation for public health. Tob. Control. 2003, 12, 360–367. [Google Scholar] [CrossRef]
- Polosa, R.; Rodu, B.; Caponnetto, P.; Maglia, M.; Raciti, C. A fresh look at tobacco harm reduction: the case for the electronic cigarette. Harm Reduct. J. 2013, 10, 19–19. [Google Scholar] [CrossRef]
- Mathur V, Gupta T, Mathur MR, Murti PR. Oral Health Consequences of Smokeless Tobacco Use. Manu Raj Mathur n.d.:195.
- Muthukrishnan, A.; Warnakulasuriya, S. Oral health consequences of smokeless tobacco use. Indian. J. Med. Res. 2018, 148, 35–40. [Google Scholar] [CrossRef]
- Tolle, SL. Periodontal and risk assessment. Dent. Hyg. -E-Book: Theory Pract. 2014, 6, 313. [Google Scholar]
- Helal, O.; Göstemeyer, G.; Krois, J.; El Sayed, K.F.; Graetz, C.; Schwendicke, F. Predictors for tooth loss in periodontitis patients: Systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 699–712. [Google Scholar] [CrossRef]
- Kamath, K.P.; Mishra, S.; Anand, P.S. Smokeless Tobacco Use as a Risk Factor for Periodontal Disease. Front. Public. Heal. 2014, 2, 195. [Google Scholar] [CrossRef]
- Leite, F.R.; Nascimento, G.G.; Scheutz, F.; López, R. Effect of Smoking on Periodontitis: A Systematic Review and Meta-regression. Am. J. Prev. Med. 2018, 54, 831–841. [Google Scholar] [CrossRef]
- Mehta, A.; Ramanarayanan, V.; Karuveettil, V.; Janakiram, C. Association between Smokeless Tobacco Use and Risk of Periodontitis in Asian Countries: A Systematic Review and Meta-Analysis. Asian Pac. J. Cancer Prev. 2021, 22, 3061–3074. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S173–S182. [Google Scholar] [CrossRef]
- Haque, MF. Haque MF. Oral pain after stopping tobacco use: a prospective study on the relationship of predictors of oral pain with paan tobacco chewing and cessation in UK resident Bangladeshi adult women. PhD Thesis. 2010.
- Millar, W.J.; Locker, D. Smoking and oral health status. J. Can. Dent. Assoc. 2007, 73, 155. [Google Scholar]
- Vellappally, S.; Jacob, V.; Šmejkalová, J.; Shriharsha, P.; Kumar, V.; Fiala, Z. Tobacco Habits and Oral Health Status in Selected Indian Population. Central Eur. J. Public. Heal. 2008, 16, 77–84. [Google Scholar] [CrossRef]
- Alade, O.; Folayan, M.O.; Adeniyi, A.; Adeyemo, Y.I.; Oyapero, A.; Olatosi, O.O.; Nzomiwu, C.; Popoola, B.O.; Eigbobo, J.; Oziegbe, E.; et al. Differences in Oral Lesions Associated with Tobacco Smoking, E-Cigarette Use and COVID-19 Infection among Adolescents and Young People in Nigeria. Int. J. Environ. Res. Public. Heal. 2022, 19, 10509. [Google Scholar] [CrossRef]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018, 169, 467–73. [Google Scholar] [CrossRef]
- Cambala AD, Kumar RA, Murugan T. Comparative study on the severity of periodontal destruction in chronic periodontitis patients with habits of smoking tobacco versus chewing smokeless tobacco. CAL 2019, 4, 4–2. [Google Scholar]
- Kulkarni, V.; Uttamani, J.R.; Bhatavadekar, N.B. Comparison of clinical periodontal status among habitual smokeless-tobacco users and cigarette smokers. Int. Dent. J. 2016, 66, 29–35. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Évid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Petersen, P.E.; Bourgeois, D.; Ogawa, H.; Estupinan-Day, S.; Ndiaye, C. The global burden of oral diseases and risks to oral health. Bull. World Health Organ. 2005, 83, 661–669. [Google Scholar]
- Agbor, M.; Azodo, C.; Tefouet, T. Smokeless tobacco use, tooth loss and oral health issues among adults in Cameroon. Afr. Heal. Sci. 2013, 13, 785–790. [Google Scholar] [CrossRef]
- Chu, Y.H.; Tatakis, D.N.; Wee, A.G. Smokeless Tobacco Use and Periodontal Health in a Rural Male Population. J. Periodontol. 2010, 81, 848–854. [Google Scholar] [CrossRef]
- Montén, U.; Wennström, J.L.; Ramberg, P. Periodontal conditions in male adolescents using smokeless tobacco (moist snuff). J. Clin. Periodontol. 2006, 33, 863–868. [Google Scholar] [CrossRef]
- Bergström, J. Tobacco smoking and chronic destructive periodontal disease. Odontology 2004, 92, 1–8. [Google Scholar] [CrossRef]
- Harrel, S.K.; Cobb, C.M.; Sheldon, L.N.; Rethman, M.P.; Sottosanti, J.S. Calculus as a Risk Factor for Periodontal Disease: Narrative Review on Treatment Indications When the Response to Scaling and Root Planing Is Inadequate. Dent. J. 2022, 10, 195. [Google Scholar] [CrossRef]
- Allen, D.L.; Kerr, D.A. Tissue Response in the Guinea Pig to Sterile and Non-Sterile Calculus. J. Periodontol. 1965, 36, 121–126. [Google Scholar] [CrossRef]
- Wilson Jr TG, Harrel SK, Nunn ME, Francis B, Webb K. The relationship between the presence of tooth-borne subgingival deposits and inflammation found with a dental endoscope. J. Periodontol. 2008, 79, 2029–35. [Google Scholar] [CrossRef]
- Montenegro Raudales JL, Yoshimura A, Sm Z, Kaneko T, Ozaki Y, Ukai T, et al. Dental calculus stimulates interleukin-1β secretion by activating NLRP3 inflammasome in human and mouse phagocytes. PLoS One 2016, 11, e0162865. [Google Scholar] [CrossRef]
- Ziauddin, S.M.; Yoshimura, A.; Raudales, J.L.M.; Ozaki, Y.; Higuchi, K.; Ukai, T.; Kaneko, T.; Miyazaki, T.; Latz, E.; Hara, Y. Crystalline structure of pulverized dental calculus induces cell death in oral epithelial cells. J. Periodontal Res. 2017, 53, 353–361. [Google Scholar] [CrossRef]
- Ziauddin, S.; Alam, M.I.; Mae, M.; Oohira, M.; Higuchi, K.; Yamashita, Y.; Ozaki, Y.; Yoshimura, A. Cytotoxic effects of dental calculus particles and freeze-dried Aggregatibacter actinomycetemcomitans and Fusobacterium nucleatum on HSC-2 oral epithelial cells and THP-1 macrophages. J. Periodontol. 2021, 93, E92–E103. [Google Scholar] [CrossRef]
- Deng, Z.-L.; Szafrański, S.P.; Jarek, M.; Bhuju, S.; Wagner-Döbler, I. Dysbiosis in chronic periodontitis: Key microbial players and interactions with the human host. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef]
- Velidandla, S.; Bodduru, R.; Birra, V.; Jain, Y.; Valluri, R.; Ealla, K.K.R. Distribution of Periodontal Pockets Among Smokers and Nonsmokers in Patients with Chronic Periodontitis: A Cross-sectional Study. Cureus 2019, 11, e5586. [Google Scholar] [CrossRef]
- Guinet, E.; Nouri-Shirazi, M. Evidence for the immunosuppressive role of nicotine on human dendritic cell functions. Immunology 2003, 109, 365–373. [Google Scholar] [CrossRef]
- Yusko, D.A.; Buckman, J.F.; White, H.R.; Pandina, R.J. Alcohol, Tobacco, Illicit Drugs, and Performance Enhancers: A Comparison of Use by College Student Athletes and Nonathletes. J. Am. Coll. Heal. 2008, 57, 281–90. [Google Scholar] [CrossRef]
- Albandar, J.M.; Streckfus, C.F.; Adesanya, M.R.; Winn, D.M. Cigar, Pipe, and Cigarette Smoking as Risk Factors for Periodontal Disease and Tooth Loss. J. Periodontol. 2000, 71, 1874–1881. [Google Scholar] [CrossRef]
- Fisher, M.; Taylor, G.; Tilashalski, K. Smokeless Tobacco and Severe Active Periodontal Disease, NHANES III. J. Dent. Res. 2005, 84, 705–710. [Google Scholar] [CrossRef]
- Anand, P.S.; Kamath, K.P.; Bansal, A.; Dwivedi, S.; Anil, S. Comparison of periodontal destruction patterns among patients with and without the habit of smokeless tobacco use – a retrospective study. J. Periodontal Res. 2013, 48, 623–631. [Google Scholar] [CrossRef]
- Rathod, S.; Wanikar, I.; Raj, A.; Maske, S.; Harkare, V. Association between kharra chewing and periodontal health status in oral submucous fibrosis patients of Central India, Nagpur. J. Indian. Soc. Periodontol. 2018, 22, 345–347. [Google Scholar] [CrossRef]
- Shyagali, T.; Salama, M.H.; Bhayya, D. Prevalence of tobacco usage and its effect on the periodontal health parameters in the mining employees and the general population- A Comparative study. Braz. J. Oral. Sci. 2017, 16, 1–9. [Google Scholar] [CrossRef]
- Bergström, J. Influence of tobacco smoking on periodontal bone height. Long-term observations and a hypothesis. J. Clin. Periodontol. 2004, 31, 260–266. [Google Scholar] [CrossRef]
- Julkunen-Iivari, A.; Heikkinen, A.M.; Räisänen, I.T.; Ruokonen, H.; Meurman, J.H.; Toppila-Salmi, S.; Söder, P.; Söder, B. Tobacco Products, Periodontal Health and Education Level: Cohort Study from Sweden. Dent. J. 2020, 8, 90. [Google Scholar] [CrossRef]
- Wickholm, S.; Söder, P.; Galanti, M.R.; Söder, B.; Klinge, B. Periodontal disease in a group of Swedish adult snuff and cigarette users. Acta Odontol. Scand. 2004, 62, 333–338. [Google Scholar] [CrossRef]
| S/N | Author year of publication) | Title | Study Design and study location | Study objective | Periodontal health in tobacco smokers | Periodontal health in smokeless tobacco users | Comparative outcome |
| 1 | Akanksha et al, 2020 [37] | Comparative study on the severity of periodontal destruction in chronic periodontitis patients with habits of smoking tobacco versus chewing smokeless tobacco | cross-sectional. No adjustment for confounders INDIA |
Evaluate and compare the severity of periodontal destruction in chronic periodontitis patients who were tobacco smokers and tobacco chewers in a South Indian population. | Periodontal probing depth: 3.4± 0.9 mm Clinical attachment level: 4.7± 1.1 mm Gingival Index: 1.1 ± 0.1mm Periodontal Index: 1.6 ± 0.3 mm |
Periodontal probing depth: 2.65 ± 0.5 mm Clinical attachment level: 4.2 mm ± 0.5 mm Gingival Index: 0.9 ± 0.2mm Periodontal Index: 1 ± 0.5 mm |
Periodontal probing depth (P = 0.03) and periodontal index (p=0.003) were significantly higher in tobacco smokers than smokeless tobacco users. No significant difference in the clinical attachment level and gingival index between the two groups. |
| 3 | Kulkarni et al., 2015 [38] | Comparison of clinical periodontal status among habitualsmokeless-tobacco users and cigarette smokers |
cross-sectional No adjustment for confounders INDIA |
Not defined | Plaque index score (%): Score 0: 4.95 Score 1: 26.44 Score 2: 41.34 Score 3: 27.47 Debris index score (%): Score 0: 5.20 Score 1: 27.70 Score 2: 42.21 Score 3: 25.30 Calculus index score(%): Score 0: 5.78 Score 1: 29.75 Score 2: 39.66 Score 3: 24.79 Gingival inflammation(%) No: 8.26 Mild/Moderate: 58.67 Severe: 33.05 Bleeding on probing (%) Present: 91.73 Absent: 8.26 Pocket depth (%) No pocket: 6.61 <4mm: 30.57 4-6-6mm: 34.71 >6mm: 28.09 |
Plaque index score (%): Score 0: 7.63 Score 1: 18.51 Score 2: 45.67 Score 3: 28.39 Debris index score (%): Score 0: 6.20 Score 1: 17.50 Score 2: 46.30 Score 3: 30.00 Calculus index score(%): Score 0: 6.17 Score 1: 22.22 Score 2: 44.44 Score 3: 27.16 Gingival inflammation(%) No: 13.58 Mild/Moderate: 62.96 Severe: 23.45 Bleeding on probing (%) Present: 85.18 Absent: 14.81 Pocket depth (%) No pocket: 9.87 <4mm: 22.16 4-6-6mm: 14.38 >6mm: 13.58 |
Plaque index score was not statistically significantly higher among smokeless tobacco users than among cigarette users. Debris index score was not statistically significant between groups. Calculus index score was significantly higher among cigarette smokers than in the smokeless tobacco users (P ≤ 0.01). Gingival inflammation scores between groups were not statistically significant, although it showed a tendency to be higher for the smokeless tobacco users. Smokeless tobacco users had higher percentage of sites with pocket depth > 6 mm compared with the cigarette smokers. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





