1. Introduction
The COVID-19 pandemic had a diverse range of effects on the self-management of diabetes. Many aspects of diabetes management were disturbed during the pandemic. The interruption of healthcare services due to the implementation of lockdown measures, the burden on healthcare systems due to the high mortality and mortality of the COVID-19, and the fear of contracting during the outbreak of the COVID-19 infection significantly affected the provision of diabetes care [
1,
2]. As a result, there was a decline not only in routine ambulatory visits but also non-COVID related preventive, and emergency care [
3,
4,
5]. The restriction on the various lifestyle routines and daily activities such as dietary and physical activity as well as self-monitoring, timely access to medications and supplies and healthcare utilization-seeking behaviors were directly affected by the pandemic [
6]. In addition, stress, anxiety, and depression were highly prevalent during the pandemic and may have indirectly influenced the mental well-being of individuals and coping patterns [
6,
7,
8,
9].
In the Kingdom of Saudi Arabia (KSA), several studies explored the impact of the COVID pandemic on lifestyle behavior of diabetes patients with variable results. A study by Fatani et al. found that the lockdown had a negative effect on physical activity and sleeping hours, but minimal effect on eating habits which may have mitigated the negative effect on glycemic control parameters compared to the pre-COVID period [
10]. Aldaghri et al. also reported that dietary habits significantly changed in content, number, and times compared to a control group [
11]. A cross-sectional study on 394 individuals with diabetes in Jeddah Province showed that compliance with diet and physical activity was reduced in the post-lockdown period compared to the pre-lockdown period (25.1% vs.27.7% and 31% vs 35%, respectively) [
12]. However, among the same population, compliance with medications and regularly self-testing blood glucose were reported in 88.3% and 46.2% of the sample studied.
The Diabetes Self-Management Questionnaire, (DSMQ), is a reliable and validated instrument that enables the assessment of self-care activities determined to be associated with diabetes control [
13]. The questionnaire
’s domains cover five main aspects related to medication intake, diet, physical activity, self-monitoring of blood glucose, and an overall individual judgement of the adequacy of self-care. The questionnaire is available in Arabic and has been used in the Saudi population with diabetes predating the COVID pandemic time [
14]. A revised version of the questionnaire (DSMQ-R) was published in 2021 and it showed good properties for use in research and daily clinical practice to identify and improve patients self-management behaviors [
15].
The objective of this study was to assess the self-management behaviors of Saudi patients with diabetes during and post the COVID pandemic period using the Arabic version of the DSMQ.
2. Materials and Methods
2.1. Study Design and Setting
This was a cross-sectional study conducted at King Saud University Medical City in Riyadh, KSA from December 2021 to August 2023.
2.2. Study Population and Sample Size
This study included all medical records of people aged ≥ 18 years diagnosed with type 2 diabetes mellitus who had at least one KSUMC ambulatory clinic visit in each of the specified time frames (Pre-COVID-19: January 1, 2019 – March 21, 2020; COVID-19 Time frame: March 22, 2020 to April 30, 2021) were included in the study. Patients were randomly selected and contacted via telephone and/or Whatsapp®. Patients were excluded if there was any missing data in their questionnaire. The calculated sample size was 341 participants.
2.3. Ethical Considerations
This study was approved by the King Saud University College of Medicine Institutional Review Board (No. E-21-5883). Participants were informed that their participation was voluntary, and they had the right to decline completing the questionnaire at any point of time.
2.4. Diabetes Self-Management Questionnaire (DSMQ)
The DSMQ is a 16-item scale developed by Schmitt et al. in 2013 with the aim of investigating the relationship between diabetic self-management in patients with type 1 and type 2 diabetes and glycemic control [
13]. It contains four domains covering aspects related to dietary control, blood glucose management and medication adherence, physical activity, and physician contact/appointments. It has been validated, translated into many languages including Arabic, and used in the Gulf region (Saudi Arabia, Kuwait, and Oman) [
14,
16,
17,
18]. Permission to use the questionnaire was obtained through Mapi Research Trust (
https://eprovide.mapi-trust.org). In the current study, the DSMQ was modified to include 3 extra items on Overall COVID-19 Impact to end up with a total of 19 items (
Table 1). Item 16 is not included in any subscales. The scale includes five sub-scales: glucose management (1, 4, 6, 10, 12), diet control (2, 5, 9,13), physical activity (8, 11, 15), and use of health services (3, 7, 14) and Overall COVID-19 Impact (17,18,19). The scale was of 4-items Likert type, and each item on the scale was scored from 0 to 3 (0 does not apply to me, 1 applies to me a little, 2 apples considerably to me, 3 very much applies to me). Items 5, 7, 10, 11, 12, 13, 14, 15 ,16, 17, 18 and 19 on the scale were scored in reverse. For calculating the total DSMQ score and subscales, the relevant item scores were summed then transformed to a scale ranging from 0 to 10 (summed actual score/ summed theoretical score *10); for example, the subscale “Dietary Control” involves 4 items, so the sum theoretical score = 12; therefore, a summed score of 9 equals to a transformed score of (9/12 *10 = 7.5). A score approaching 10 indicated greater diabetic self-management.
2.5. Participant Demographics
The survey involved 508 responses from surveyed patients at KSUMC. However, some responses were excluded from the score analysis study for the following reasons:
129 responses had missing/incomplete values on important questionnaire items.
36 patients gave their responses twice or three times. Upon examining these duplicates, some responses had discrepancies in demographic information such as gender, age, nationality, how long they had diabetes, and the type of medications they are currently taking for diabetes. Accordingly, these duplicates were filtered by selecting the earliest response and correcting the demographic information according to the hospital system and physician/patient notes.
Accordingly, the unique responses of 341 patients were included in the subsequent score analysis.
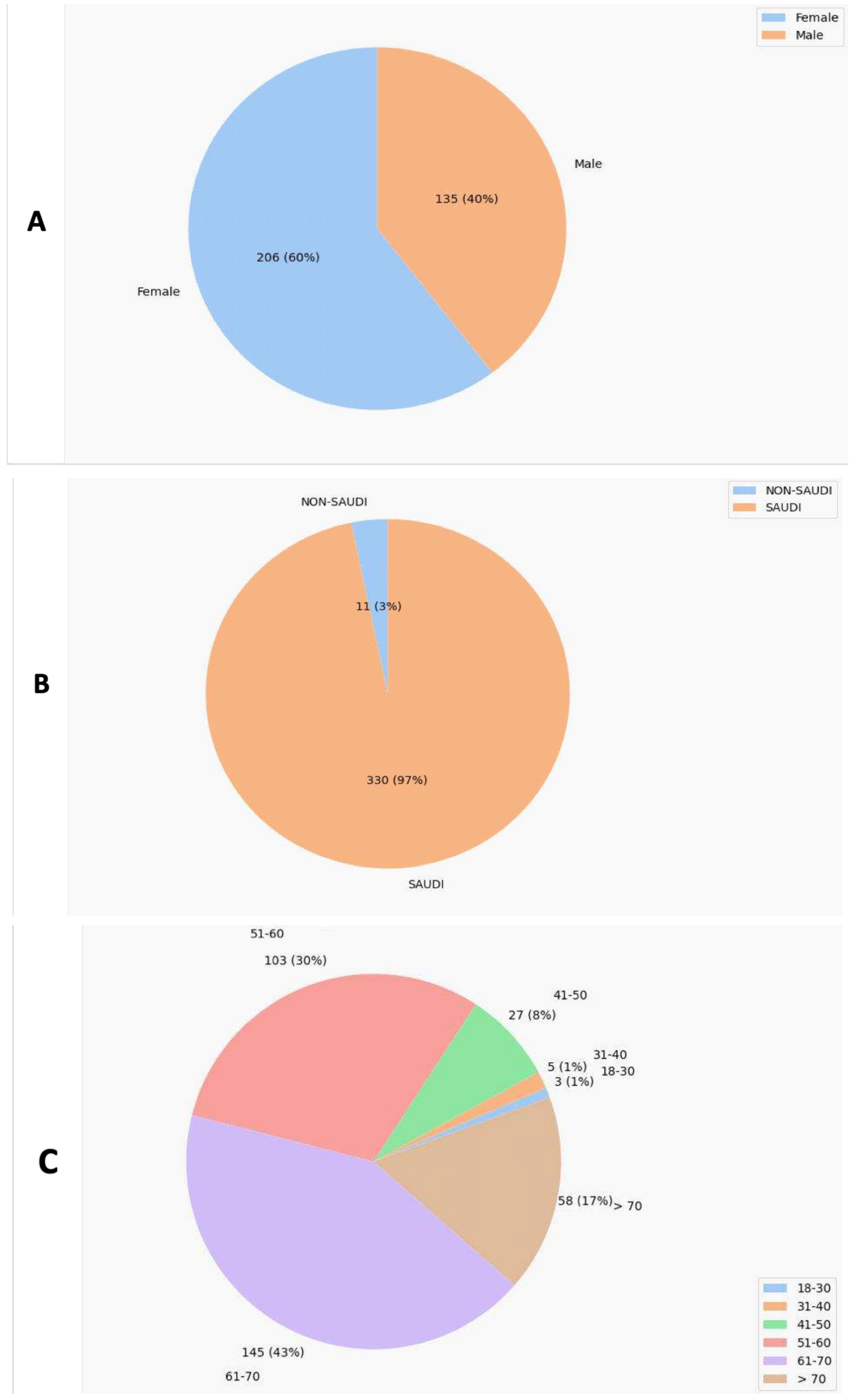
The demographic data indicates that the study showed a balanced distribution of gender where 60% of patients were female (
Figure 1A). On the other hand, the majority of patients (97%) were Saudi, (43%) were 61-70 years old, and (49%) were taking oral medications only (
Figure 1B–D).
2.7. Software
The analysis of the data in this study was primarily conducted using the Python programming language (version 3.9.13) within a Jupyter Notebook environment (jupyter_core: 4.11.1, notebook server: 6.4.12). A variety of packages, including pandas, numpy, seaborn, matplotlib, itertools, and statannotations were employed for tasks such as presenting data, organizing it into groups, validating it, manipulating data frames, and generating visualizations. Parts of this manuscript were crafted with the assistance of automated writing programs like Claude, Copy.ai, as well as Microsoft's AI chatbot. Some Python code scripts used for associated data processing benefited to some extent from guidance provided by those artificial intelligence tools. Notwithstanding, the authors held accountability for the concepts explored, the substance covered, and the final form of the manuscript.
2.8. Statistical Analysis
The normality of the data was determined using Shapiro-Wilk test from the Scipy.stats Python package [
19]. For dependent variables that were binary (e.g. pass/fail), the data were analyzed statistically using a chi-square test for independence in a contingency table to evaluate two independent samples. When there were more than two samples, a Bonferroni post-hoc adjustment following chi-square was utilized. These analyses were conducted using functions in the Scipy Python package [
20,
21].
Other dependent variables that were discrete or continuous were assessed using the Mann-Whitney U test for two independent samples (statannotations python package) or the Wilcoxon signed-rank test for two paired samples (Scipy.stats python package). For more than two samples, a Kruskal-Wallis H test followed by post-hoc Dunn's test with Bonferroni correction was applied, drawing on functions from the Pingouin and Scikit-Posthocs packages [
22].
Correlational analysis involved Spearman's correlation test using Scipy functions [
23]. For all statistical tests, a p-value of ≤ 0.05 was considered statistically significant.
3. Results
3.1. Study Overview
The study involved 341 participants who were enrolled in the DSMQ study. The average for each item ranged from 1.76 to 2.83 (out of 3) which indicates good diabetes self-management during COVID-19 (
Table 2). The survey consistency study showed that most of the survey dimensions showed acceptable (> 0.5) Cronbach`s alfa values. However, only the dimension of health care use involved 3 items and showed a low Cronbach`s alfa value which might be somehow agreeing with what Schmitt reported on healthcare use that showed a marginal consistency value [
13]. However, the DSMQ sum scale based on 16 or 19 items showed high Cronbach`s alfa values (> 0.7) which reflects good overall internal consistency of survey items together (
Table 3).
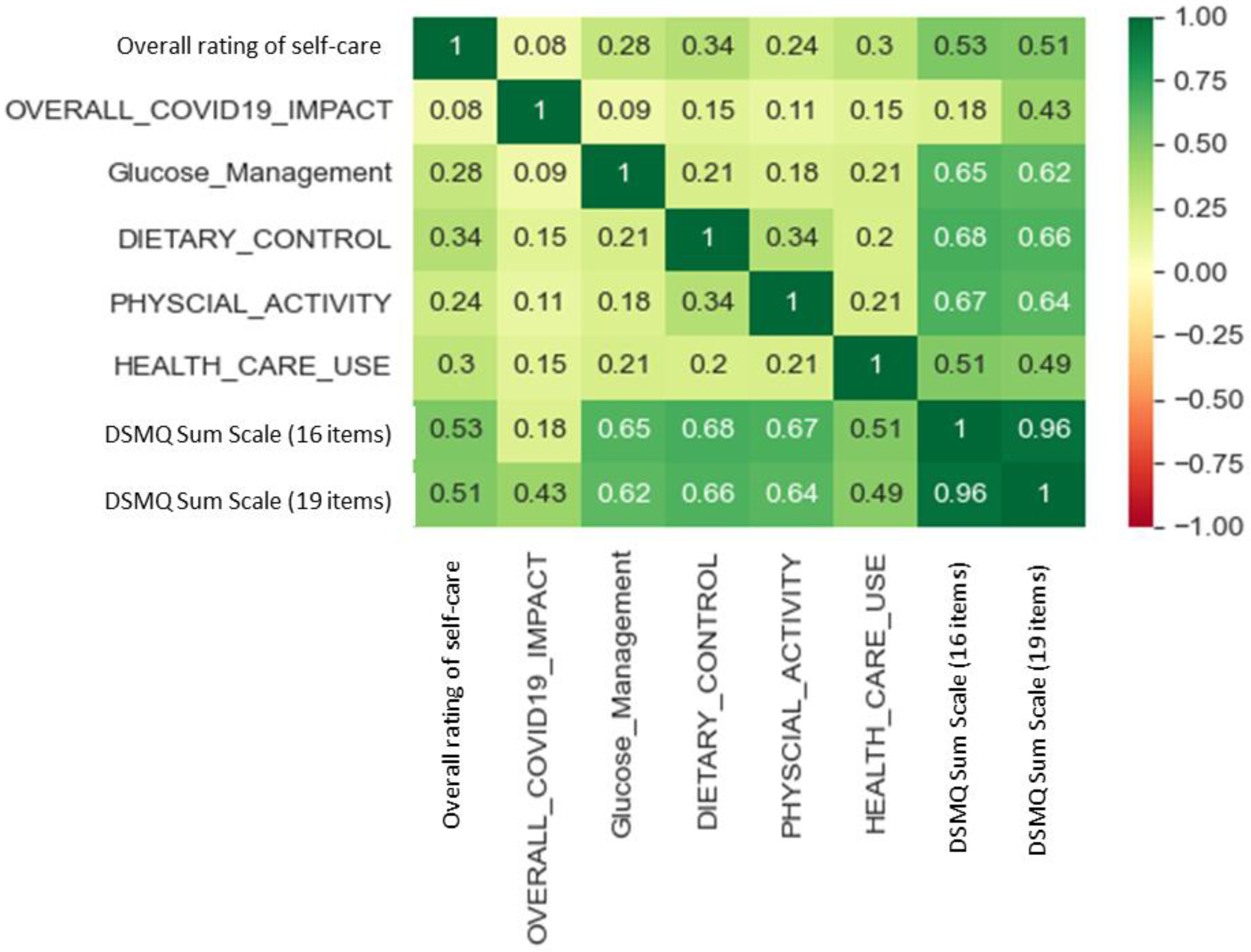
All the DSMQ subscales showed negligible to weak positive correlations with each other (
Figure 2). However, the total DSMQ score (19 items) showed moderate positive correlations with DSMQ sum scale, healthcare use, and overall COVID-19 impact and showed strong positive correlations with Glucose management, diet control and physical activity (
Figure 2). A similar observation was observed with total DSMQ score (16 items) except for "overall COVID-19 impact" which showed a weak positive correlation (
Figure 2).
3.2. Study Findings in Comparison with Relevant Previous Studies
The DSMQ was conducted in the same hospital system involving a similar patient population prior to COVID-19 by Almiqbal et al. [
14]. The authors were contacted; however, the full data set was no longer accessible. Interestingly, the current study showed a relatively lower glucose management score compared to the Saudi population before COVID-19. However, the current study showed higher subscale scores for diet control, physical activity, and particularly healthcare use that showed about 1.8-fold increment compared to DSMQ of the Saudi population before COVID-19 (
Table 4) [
14]. On the other hand, the current study showed higher DSMQ total scores as well as all DSMQ subscales compared to post_covid-19 DSMQ findings in the Turkish population (
Table 4) [
24].
3.3. Influence of Patient Demographics on DSMQ Findings
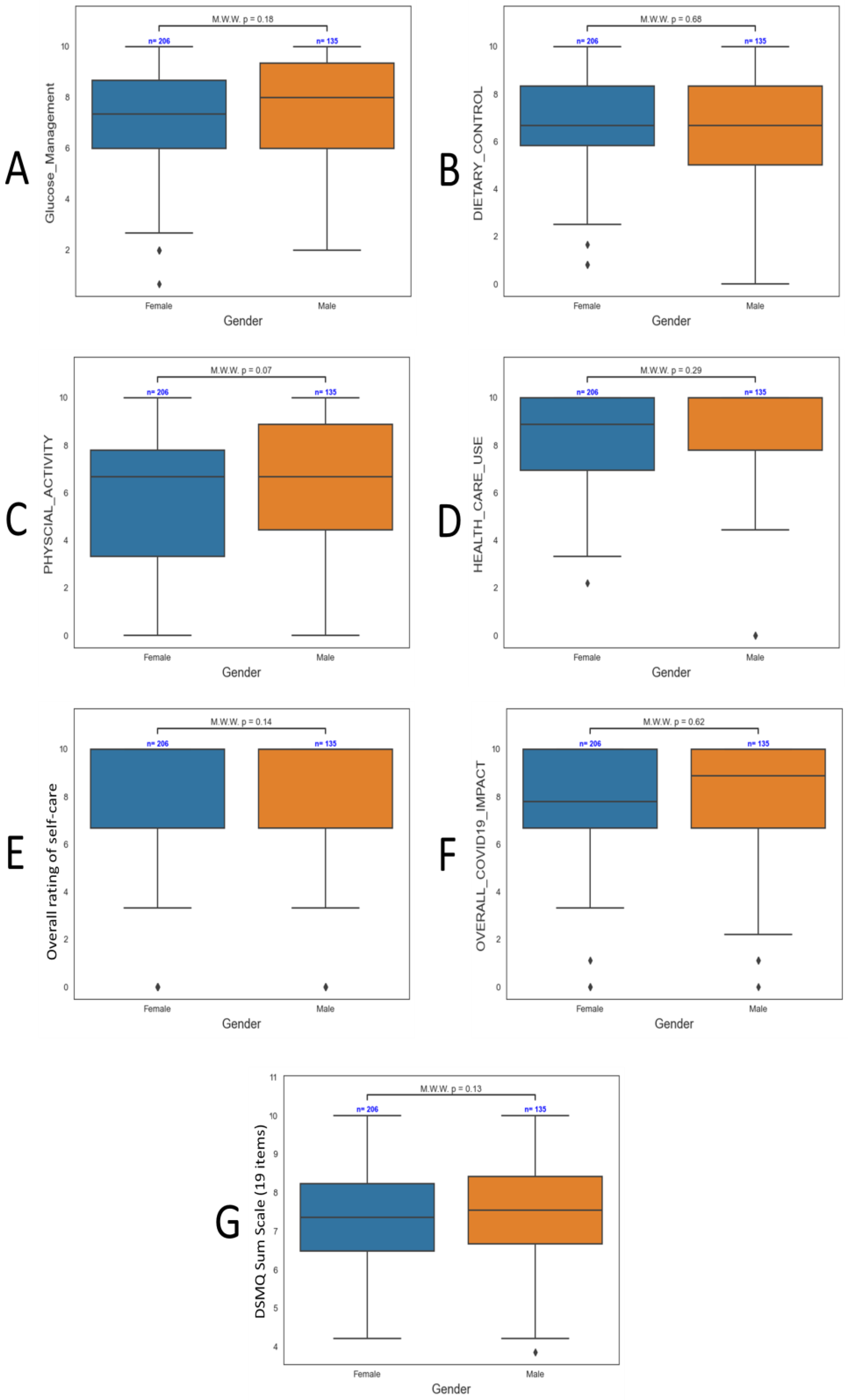
The gender showed no significant effect on all DSMQ subscales as well as the sum scale (
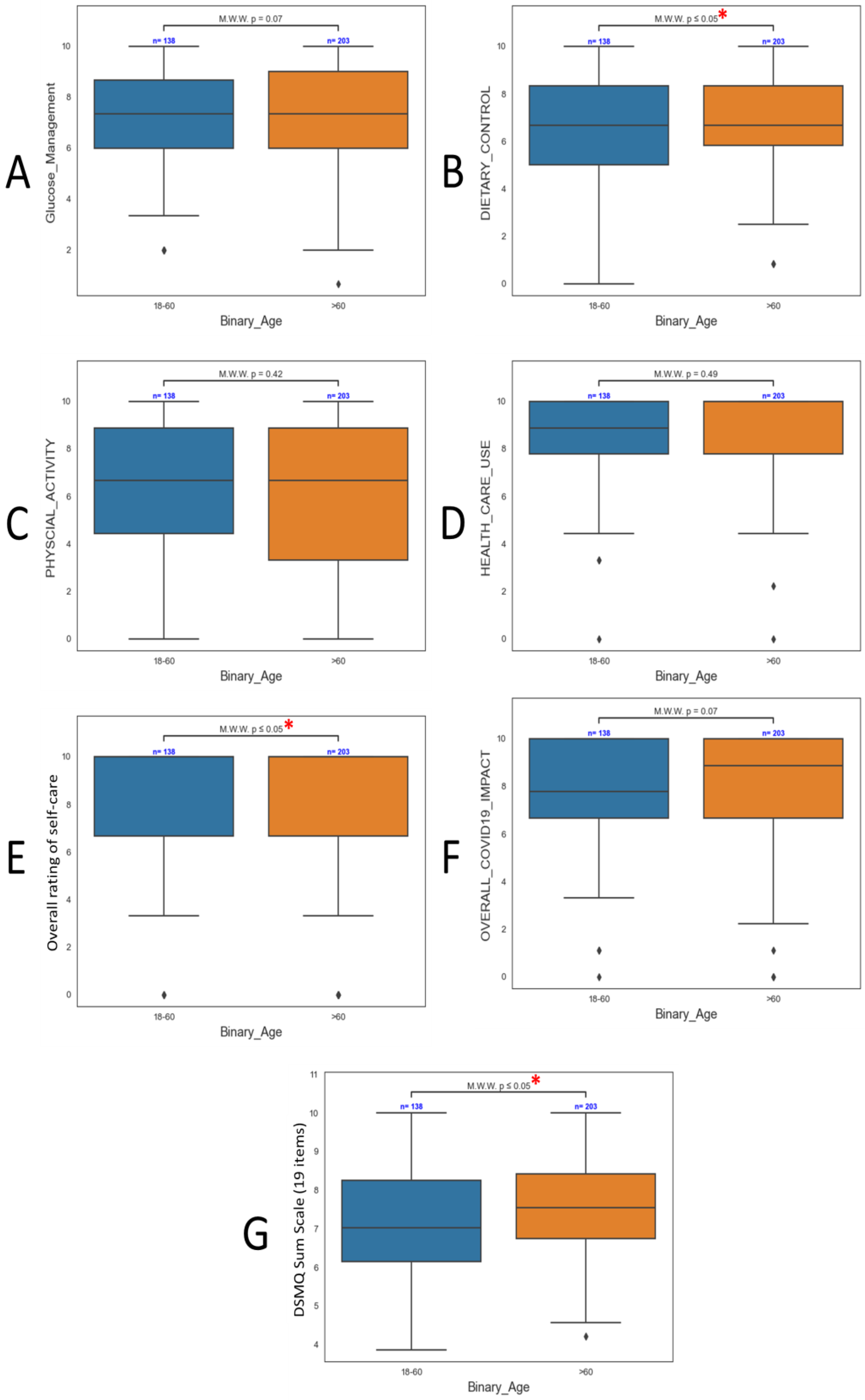
Figure 3). On the other hand, patient age had a significant (p < 0.05) effects on diet control, overall rating of self-care, and DSMQ sum scale (
Figure 4B, E, G). In particular, patients aged > 60 years old showed significantly higher (p < 0.05) ratings of diet control and overall self-care. Although all other subscales showed no significant difference, the DSMQ sum scale showed significantly higher scores in those elderly patients (
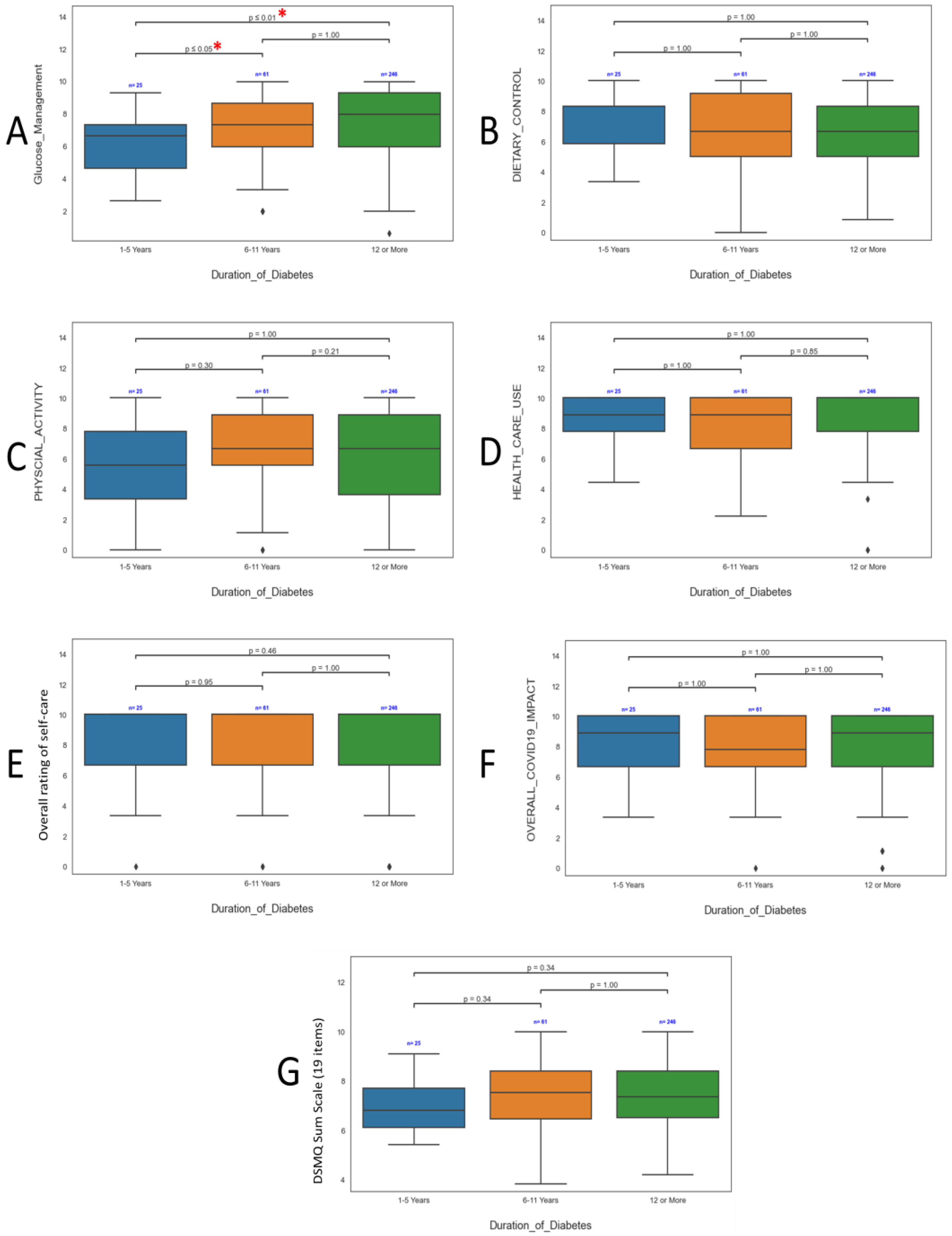
Figure 4). Regarding the time since diagnosis of diabetes, patients that were diagnosed with diabetes 1-5 years ago showed significantly (p < 0.05) lower glucose management scores compared to corresponding patient groups with longer diabetes history (
Figure 5A). However, diabetes duration showed no significant effect on all other subscales as well as the sum scale (
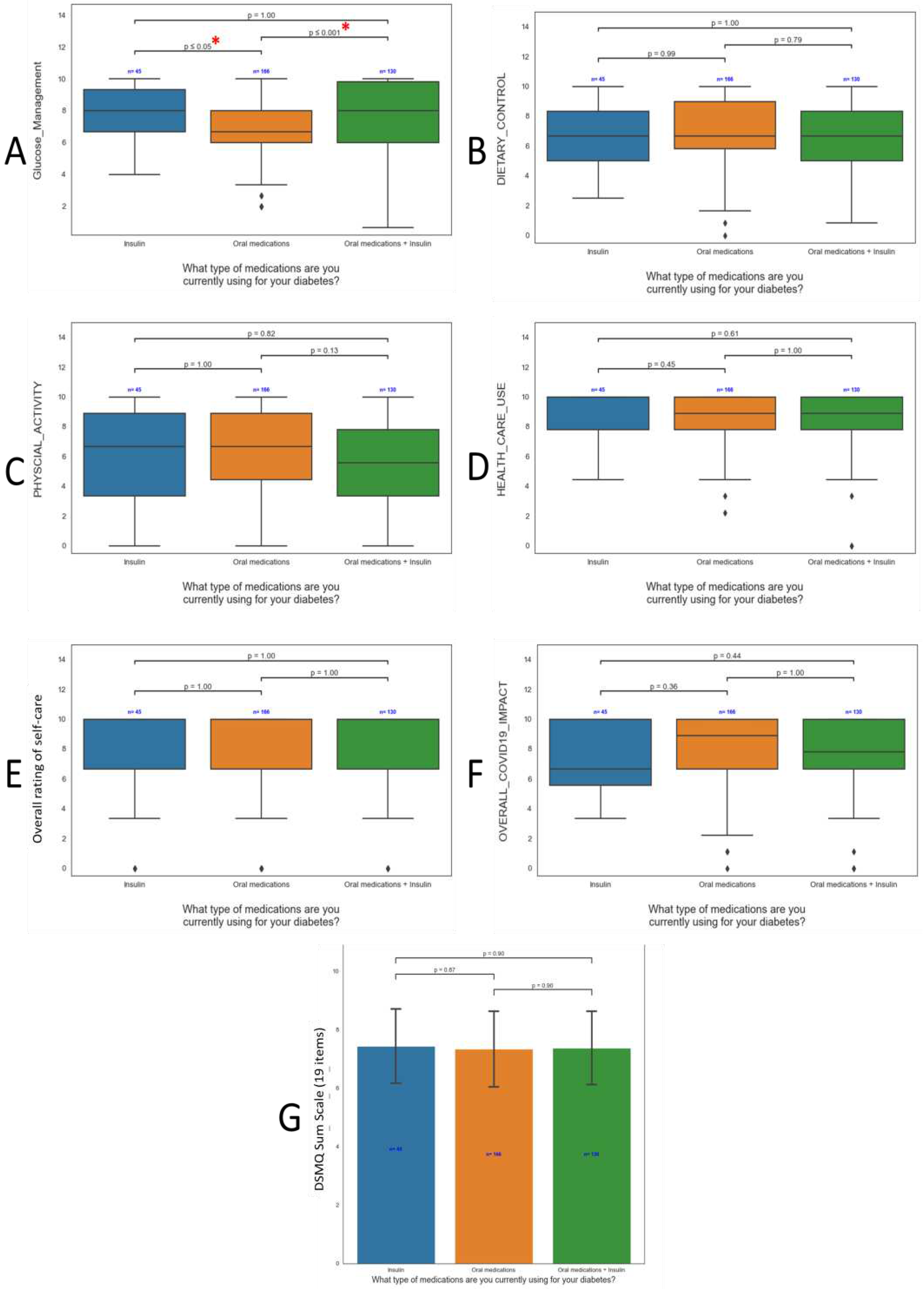
Figure 5B-G). Similar findings were observed for the effect of medication type where patients who are on insulin therapy (either alone or in combination) showed significantly (p < 0.05) higher glucose management scores compared to corresponding patients who used oral medications only (
Figure 6A). No other significant effects were observed for medication types in all other subscales as well as the sum scale (
Figure 6B-G). It worth mentioning that study involved a very low % of non-Saudi population (3%) and the statistical analysis showed that no significant different were found between Saudi and non-Saudi population within the DSMQ sum scale as well as all subscales.
4. Discussion
This study focused on the impact of the COVID-19 pandemic on diabetes self-management in the Saudi Arabian population using the DSMQ. Our study was unique due to the specific questions regarding the impact of the COVID-19 pandemic on diabetes control. When compared to DSMQ results prior to COVID-19 as well as the results in the Turkish population, patients in this study generally had better DSMQ sum scale scores [
9,
14,
16,
24,
25,
26,
27]. Previous studies suggest that the COVID-19 pandemic has had a significant impact on diabetes self-management in the Saudi Arabian population. The challenges faced by individuals with diabetes include reduced compliance with medical treatment, lifestyle changes, increased psychological distress, and limited access to healthcare services; however, the findings of this study have several important implications related to diabetes care in the post-COVID-19 era [
9,
10,
11,
12,
28,
29].
In the current study, participants reported high glucose management scores. Two studies in similar patient populations to this study had slightly higher scores in this domain and one had lower scores, but it appears as the COVID-19 pandemic did not lead to significant changes in glycemic management [
14,
26,
27]. This was directly expressed by the study participants in their answers to the three COVID-19 questions. It is interesting to note that the glucose management scores in this study were substantially higher than those reported in the southern region of Saudi Arabia, the scores of Saudi Arabian health care professionals, and post-COVID scores in Turkey [
16,
24,
25]. Difficulties in glucose management may be due to common barriers reported in both local and international studies which have mentioned that adherence and access to healthcare services was decreased during the pandemic. A cross-sectional study conducted in Jazan, Saudi Arabia, involving 394 patients found that the COVID-19 lockdown significantly reduced the levels of compliance, medical treatment, and lifestyle habits among Saudi patients with diabetes [
30]. A one-year follow-up study examined the impact of the COVID-19 pandemic on diabetes self-management globally. While not specific to the Saudi Arabian population, the study highlighted the challenges faced by individuals with diabetes during the pandemic, including disruptions in healthcare access, changes in lifestyle habits, and increased psychological distress [
29]. Difficulties accessing medications, a vital component of therapy, due to lockdown restrictions in movement or medication shortages may have been the primary cause as opposed to patient negligence.
There were several positive results that show promise in the future care of patients with diabetes in Saudi Arabia. When compared to pre-COVID-19 results by Almigbal et al., participants reported higher scores for dietary control and physical activity [
14]. Furthermore, healthcare use approximately doubled post-COVID. Dietary control, physical activity, and healthcare system utilization are highly emphasized core components of Diabetes Self-Management Education and Support (DSMES) [
31]. Furthermore, lifestyle changes including diet and exercise can lead to a decrease in hemoglobin A1C of up to 2% [
32,
33]. The dietary control scores reported in this study were the highest reported in Saudi Arabia and higher than post-COVID scores in Turkey [
14,
16,
24,
26,
27]. The only exception were the dietary scores reported in healthcare providers; however, this population was different than our study and it is expected that healthcare professional dealing with patients with diabetes would have better dietary control due to more knowledge about the dietary recommendations and having access to healthier food choices [
25]. Likewise, physical activity scores were amongst the highest reported in Saudi Arabia to date. During the pandemic, patients also may have dedicated more time towards exercise and been more conscious of their dietary habits especially with the reduced opportunities for gathering with family and friends who may have made adherence to dietary changes more difficult due to societal or peer pressure. It is also possible that patients were more encouraged to make lifestyle modifications due to the increased risk of poor COVID-19 outcomes and mortality in patients with diabetes.
In addition, the healthcare use scores were by far the most impressive scores reported in both Saudi Arabia and Turkey post-pandemic [
9,
14,
16,
24,
25,
26,
27]. Improved healthcare utilization is an essential component of diabetes care in general, and a crucial component of the Saudi Vision [
34]. One of the national health care transformation objectives includes facilitating access to healthcare services and an important related initiative is the development of a health care model that places more emphasis on the prevention of diseases rather than treatment [
35]. Telehealth is a means of expanding patient access and many of the participants in this study increased their healthcare utilization via virtual medical encounters. The Ambulatory Care Practice Research Network writing task force of the Saudi Society of Clinical Pharmacy has called for an expansion of virtual clinics and Telehealth to achieve this objective [
36].
While overall self-care was upheld, some disparities emerged across demographic subgroups of Saudis with diabetes. Newly diagnosed patients reported lower DSMQ scores compared to those with longer diabetes duration, highlighting the need for more intensive education and skills training early in the disease course. This is especially important during crises when usual health services are interrupted. The higher scores among elderly Saudis may reflect greater health consciousness with age or concerns about diabetes complications. Although not reaching a level of statistical significance, Alkhormi et al. also reported that patients ≥ 65 accounted for a greater percentage of participants with appropriate self-management of diabetes during COVID-19 as opposed to their younger counterparts [
9]. This differs however from the post-COVID results in Turkey and pre-COVID results from Najran which indicated that patients with who had diabetes for a longer duration or were elderly had poorer self-management [
16,
24]. This may indicate that the patients in this study were better educated regarding diabetes care. Finally, those using insulin had better glucose monitoring skills than oral medication users, likely due to the need for frequent self-injections.
The authors of this study would like to mention some limitations. First, the study included a small sample size from one hospital system; however, the sample size and patient population is similar to previous studies conducted in Saudi Arabia and the study sample sized fulfilled the calculated minimum sample size required. Second, bias due to over- or under reporting cannot be ruled out when utilizing a self-reported questionnaire such as the DSMQ. Third, recall bias may have occurred in some participants especially those who participated in the later stages of the survey. Finally, this manuscript did not include clinical data such as the hemoglobin A1C or other related patient vitals.
5. Conclusions
In conclusion, this cross-sectional study provides valuable insights into the maintenance of diabetes self-management among Saudis during the significant lifestyle and healthcare disruptions imposed by COVID-19. The DSMQ results suggest effective adaptation by Saudi patients, but also reveal target groups that require more self-care support, especially during public health emergencies. Further research should elucidate specific barriers to optimal diabetes control during pandemics and develop appropriate management strategies tailored to the Saudi context.
Author Contributions
Conceptualization, I.S. and G.B.; Methodology, I.S., G.B., and H.K.; Software, A.S.; Validation, G.B.; Formal Analysis, A.S.; Investigation, I.S. and G.B..; Resources, I.S and G.B.; Data Curation, A.S., G.B. and H.K.; Writing–Original Draft Preparation, I.S., G.B., and A.S.; Writing – Review & Editing, I.S., A.S., G.B., and H.K.; Visualization, I.S. and G.B.; Supervision, I.S.; Project Administration, I.S.; Funding Acquisition, A.S. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to extend their appreciation to King Saud University, Riyadh, Saudi Arabia for supporting this work through the Researcher Supporting Project (RSPD-2023R747).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the King Saud University College of Medicine Institutional Review Board No. E-21-5883 on 22 April 2021.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to extend their appreciation to King Saud University, Riyadh, Saudi Arabia for supporting this work through the Researcher Supporting Project (RSPD-2023R747).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mohseni, M., et al., Challenges of routine diabetes care during COVID-19 era: A systematic search and narrative review. Prim Care Diabetes, 2021. 15(6): p. 918-922. https://doi.org/10.1016/j.pcd.2021.07.017. [CrossRef]
- Vamos, E.P. and K. Khunti, Indirect effects of the COVID-19 pandemic on people with type 2 diabetes: time to urgently move into a recovery phase. BMJ Qual Saf, 2022. 31(7): p. 483-485. https://doi.org/10.1136/bmjqs-2021-014079. [CrossRef]
- Mafi, J.N., et al., Trends in US Ambulatory Care Patterns During the COVID-19 Pandemic, 2019-2021. JAMA, 2022. 327(3): p. 237-247. https://doi.org/10.1001/jama.2021.24294. [CrossRef]
- Molina, M., et al., Analysis of Emergency Department Encounters Among High Users of Health Care and Social Service Systems Before and During the COVID-19 Pandemic. JAMA Netw Open, 2022. 5(10): p. e2239076. https://doi.org/10.1001/jamanetworkopen.2022.39076. [CrossRef]
- Zachrison, K.S., Z. Yan, and L.H. Schwamm, Changes in Virtual and In-Person Health Care Utilization in a Large Health System During the COVID-19 Pandemic. JAMA Netw Open, 2021. 4(10): p. e2129973. https://doi.org/10.1001/jamanetworkopen.2021.29973. [CrossRef]
- Khunti, K., et al., The impact of the COVID-19 pandemic on diabetes services: planning for a global recovery. Lancet Diabetes Endocrinol, 2022. 10(12): p. 890-900. https://doi.org/10.1016/S2213-8587(22)00278-9. [CrossRef]
- Distaso, W., et al., Diabetes self-management during the COVID-19 pandemic and its associations with COVID-19 anxiety syndrome, depression and health anxiety. Diabet Med, 2022. 39(10): p. e14911. doi: 10.1111/dme.14911. [CrossRef]
- Zupa, M.F., et al., Changes in Self-management During the COVID-19 Pandemic Among Adults with Type 2 Diabetes at a Federally Qualified Health Center. J Immigr Minor Health, 2022. 24(5): p. 1375-1378. https://doi.org/10.1007/s10903-022-01351-7. [CrossRef]
- Alkhormi, A.H., et al., Psychological Health and Diabetes Self-Management among Patients with Type 2 Diabetes during COVID-19 in the Southwest of Saudi Arabia. Medicina (Kaunas), 2022. 58(5). https://doi.org/10.3390/medicina58050675. [CrossRef]
- Fatani, B., et al., Behavioral Changes in Patients With Diabetes During the COVID-19 Pandemic in Saudi Arabia: A Cross-Sectional Study. Cureus, 2023. 15(2): p. e34956. https://doi.org/10.7759/cureus.34956. [CrossRef]
- Al-Daghri, N.M., et al., COVID-19 Lockdown and Lifestyle Changes in Saudi Adults With Types 1 and 2 Diabetes. Front Public Health, 2022. 10: p. 912816. https://doi.org/10.3389/fpubh.2022.912816. [CrossRef]
- Alshareef, R., et al., Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab Syndr, 2020. 14(5): p. 1583-1587. https://doi.org/10.1016/j.dsx.2020.07.051. [CrossRef]
- Schmitt, A., et al., The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes, 2013. 11: p. 138. https://doi.org/10.1186/1477-7525-11-138. [CrossRef]
- Almigbal, T.H., et al., Association of health literacy and self-management practices and psychological factor among patients with type 2 diabetes mellitus in Saudi Arabia. Saudi Med J, 2019. 40(11): p. 1158-1166. https://doi.org/10.15537/smj.2019.11.24585. [CrossRef]
- Schmitt, A., et al., A Self-Report Measure of Diabetes Self-Management for Type 1 and Type 2 Diabetes: The Diabetes Self-Management Questionnaire-Revised (DSMQ-R) - Clinimetric Evidence From Five Studies. Front Clin Diabetes Healthc, 2021. 2: p. 823046. https://doi.org/10.3389/fcdhc.2021.823046. [CrossRef]
- Al-Qahtani, A.M., Frequency and factors associated with inadequate self-care behaviors in patients with type 2 diabetes mellitus in Najran, Saudi Arabia. Based on diabetes self-management questionnaire. Saudi Med J, 2020. 41(9): p. 955-964. doi: 10.15537/smj.2020.9.25339. [CrossRef]
- Al-Khaledi, M., et al., Diabetes Self-Management: A Key to Better Health-Related Quality of Life in Patients with Diabetes. Med Princ Pract, 2018. 27(4): p. 323-331. https://doi.org/10.1159/000489310. [CrossRef]
- Al-Hadhrami, R., O. Al-Rawajfah, and J. Muliira, Diabetes Self-Management and the Associated Factors Among Adult Omanis with Type 1 Diabetes. Sultan Qaboos Univ Med J, 2020. 20(4): p. e339-e345. https://doi.org/10.18295/squmj.2020.20.04.010. [CrossRef]
- Mishra, P., et al., Descriptive statistics and normality tests for statistical data. Ann Card Anaesth, 2019. 22(1): p. 67-72. doi: 10.4103/aca.ACA_157_18. [CrossRef]
- McHugh, M.L., The chi-square test of independence. Biochem Med (Zagreb), 2013. 23(2): p. 143-9. doi:10.11613/bm.2013.018. [CrossRef]
- Anderson, M.R., et al., Determining Success or Failure After Foot and Ankle Surgery Using Patient Acceptable Symptom State (PASS) and Patient Reported Outcome Information System (PROMIS). Foot Ankle Int, 2018. 39(8): p. 894-902. https://doi.org/10.1177/1071100718769666. [CrossRef]
- Nahm, F.S., Nonparametric statistical tests for the continuous data: the basic concept and the practical use. Korean J Anesthesiol, 2016. 69(1): p. 8-14. https://doi.org/10.4097/kjae.2016.69.1.8. [CrossRef]
- Schober, P., C. Boer, and L.A. Schwarte, Correlation Coefficients: Appropriate Use and Interpretation. Anesth Analg, 2018. 126(5): p. 1763-1768. doi:10.1213/ane.0000000000002864. [CrossRef]
- Utli, H. and B. Vural Doğru, The effect of the COVID-19 pandemic on self-management in patients with type 2 diabetics. Prim Care Diabetes, 2021. 15(5): p. 799-805. https://doi.org/10.1016/j.pcd.2021.07.009. [CrossRef]
- Alhussein, N.A., et al., Diabetes Self-Management Among Healthcare Providers in King Abdulaziz Medical City, Riyadh: A Cross-Sectional Pilot Study. Cureus, 2021. 13(9): p. e18155. https://doi.org/10.7759/cureus.18155. [CrossRef]
- Alodhayani, A., et al., Association between self-care management practices and glycemic control of patients with type 2 diabetes mellitus in Saud Arabia: A cross -sectional study. Saudi J Biol Sci, 2021. 28(4): p. 2460-2465. https://doi.org/10.1016/j.sjbs.2021.01.047. [CrossRef]
- Alruhaim, H.Y., et al., The association between diabetes numeracy and diabetes self-management among Saudi adults with insulin-treated diabetes. Saudi Med J, 2021. 42(5): p. 517-525. https://doi.org/10.15537/smj.2021.42.5.20200422. [CrossRef]
- Shi, C., et al., Barriers to Self-Management of Type 2 Diabetes During COVID-19 Medical Isolation: A Qualitative Study. Diabetes Metab Syndr Obes, 2020. 13: p. 3713-3725. https://doi.org/10.2147/dmso.s268481. [CrossRef]
- Olesen, K., et al., How has the COVID-19 Pandemic Affected Diabetes Self-Management in People With Diabetes? - A One-Year Follow-Up Study. Front Clin Diabetes Healthc, 2022. 3: p. 867025. https://doi.org/10.3389/fcdhc.2022.867025. [CrossRef]
- Oraibi, O., et al., Impact of COVID-19 on Patients with Diabetes Standard of Care in the Jazan Region, Saudi Arabia. Mater Sociomed, 2022. 34(4): p. 272-277. https://doi.org/10.5455/msm.2022.34.272-277. [CrossRef]
- ElSayed, N.A., et al., 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2023. Diabetes Care, 2022. 46(Supplement_1): p. S68-S96. https://doi.org/10.2337/dc24-s005. [CrossRef]
- Boulé, N.G., et al., Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. Jama, 2001. 286(10): p. 1218-27. https://doi.org/10.1034/j.1600-0838.2002.120111_3.x. [CrossRef]
- Franz, M.J., et al., Academy of Nutrition and Dietetics Nutrition Practice Guideline for Type 1 and Type 2 Diabetes in Adults: Systematic Review of Evidence for Medical Nutrition Therapy Effectiveness and Recommendations for Integration into the Nutrition Care Process. J Acad Nutr Diet, 2017. 117(10): p. 1659-1679. https://doi.org/10.1016/j.jand.2017.03.022. [CrossRef]
- Vision, K., 2030 Strategic Objectives and Vision Realization Programs. 2021.
- Chowdhury, S., D. Mok, and L. Leenen, Transformation of health care and the new model of care in Saudi Arabia: Kingdom's Vision 2030. J Med Life, 2021. 14(3): p. 347-354. https://doi.org/10.25122/jml-2021-0070. [CrossRef]
- Alshaya, O.A., et al., Ambulatory care pharmacy in Saudi Arabia; definition, history, present, future potentials, and expected challenges. JACCP: JOURNAL OF THE AMERICAN COLLEGE OF CLINICAL PHARMACY, 2022. 5(3): p. 332-341. https://doi.org/10.1002/jac5.1577. [CrossRef]
Figure 1.
The distribution of patients according to (A) Gender, (B) Nationality, (C) Age, and (D) Type of diabetes medications.
Figure 1.
The distribution of patients according to (A) Gender, (B) Nationality, (C) Age, and (D) Type of diabetes medications.
Figure 2.
Inter-correlation between DSMQ total and subscale scores, n = 341.
Figure 2.
Inter-correlation between DSMQ total and subscale scores, n = 341.
Figure 3.
Influence of Gender on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Over all COVID-19 impact and (G) total DSMQ score (19 items), n = 341.
Figure 3.
Influence of Gender on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Over all COVID-19 impact and (G) total DSMQ score (19 items), n = 341.
Figure 4.
Influence of Age on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Overall COVID-19 impact, and (G) total DSMQ score (19 items), n = 341. A significant difference (p ≤ 0.05) was denoted with a red asterisk (*).
Figure 4.
Influence of Age on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Overall COVID-19 impact, and (G) total DSMQ score (19 items), n = 341. A significant difference (p ≤ 0.05) was denoted with a red asterisk (*).
Figure 5.
Influence of duration of diabetes on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Overall COVID-19 impact, and (G) total DSMQ score (19 items), n = 341. A significant difference (p ≤ 0.05) was denoted with a red asterisk (*).
Figure 5.
Influence of duration of diabetes on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Overall COVID-19 impact, and (G) total DSMQ score (19 items), n = 341. A significant difference (p ≤ 0.05) was denoted with a red asterisk (*).
Figure 6.
Influence of medications type on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Overall COVID-19 impact, and (G) total DSMQ score (19 items), n = 341. A significant difference (p ≤ 0.05) was denoted with a red asterisk (*).
Figure 6.
Influence of medications type on (A) Glucose management, (B) Dietary control, (C) Physical activity, (D) healthcare use, (E) DSMQ sum scale (F) Overall COVID-19 impact, and (G) total DSMQ score (19 items), n = 341. A significant difference (p ≤ 0.05) was denoted with a red asterisk (*).
Table 1.
Diabetes Self-Management Questionnaire (DSMQ).
Table 1.
Diabetes Self-Management Questionnaire (DSMQ).
| Item code* |
Item statement |
| Q1 |
I check my blood sugar levels with care and attention. |
| Q2 |
The food I choose to eat makes it easy to achieve optimal blood sugar levels. |
| Q3 |
I keep all doctors’ appointments recommended for my diabetes treatment. |
| Q4 |
I take my diabetes medication (e. g. insulin, tablets) as prescribed. |
| rQ5 |
Occasionally I eat lots of sweets or other foods rich in carbohydrates. |
| Q6 |
I record my blood sugar levels regularly (or analyze the value chart with my blood glucose meter). |
| rQ7 |
I tend to avoid diabetes-related doctors’ appointments. |
| Q8 |
I do regular physical activity to achieve optimal blood sugar levels. |
| Q9 |
I strictly follow the dietary recommendations given by my doctor or diabetes specialist. |
| rQ10 |
I do not check my blood sugar levels frequently enough as would be required for achieving good blood glucose control. |
| rQ11 |
I avoid physical activity, although it would improve my diabetes.', |
| rQ12 |
I tend to forget to take or skip my diabetes medication (e. g. insulin, tablets). |
| rQ13 |
Sometimes I have real ‘food binges’ (not triggered by low blood sugar)', |
| rQ14 |
Regarding my diabetes care, I should see my medical practitioner(s) more often. |
| rQ15 |
I tend to skip planned physical activity. |
| rQ16 |
My diabetes self-care is poor. |
| rQ17 |
The COVID-19 pandemic negatively affected my diabetes control. |
| rQ18 |
The COVID-19 pandemic negatively affected my exercise regimen. |
| rQ19 |
The COVID-19 pandemic negatively affected my ability to follow a diet (for my Diabetes). |
Table 2.
Descriptive analysis of DSMQ individual items (n = 341).
Table 2.
Descriptive analysis of DSMQ individual items (n = 341).
| parameters |
Q1 |
Q2 |
rQ3 |
Q4 |
Q5 |
Q6 |
rQ7 |
Q8 |
Q9 |
rQ10 |
rQ11 |
rQ12 |
rQ13 |
rQ14 |
rQ15 |
rQ16 |
rQ17 |
rQ18 |
rQ19 |
| mean |
1.98 |
1.76 |
2.68 |
2.77 |
2.24 |
1.30 |
2.83 |
1.33 |
1.77 |
2.36 |
2.13 |
2.61 |
2.40 |
2.23 |
2.04 |
2.53 |
2.40 |
2.21 |
2.42 |
| std |
1.08 |
1.00 |
0.74 |
0.59 |
0.91 |
1.26 |
0.61 |
1.12 |
1.06 |
0.90 |
1.04 |
0.81 |
0.93 |
1.08 |
1.06 |
0.79 |
0.89 |
0.96 |
0.83 |
| min |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
0.00 |
| 25% |
1.00 |
1.00 |
3.00 |
3.00 |
2.00 |
0.00 |
3.00 |
0.00 |
1.00 |
2.00 |
2.00 |
3.00 |
2.00 |
2.00 |
1.00 |
2.00 |
2.00 |
2.00 |
2.00 |
| 50% |
2.00 |
2.00 |
3.00 |
3.00 |
2.00 |
1.00 |
3.00 |
1.00 |
2.00 |
3.00 |
2.00 |
3.00 |
3.00 |
3.00 |
2.00 |
3.00 |
3.00 |
3.00 |
3.00 |
| 75% |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
2.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
| max |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
3.00 |
Table 3.
Internal Consistency of DMSO subscale and subscales.
Table 3.
Internal Consistency of DMSO subscale and subscales.
| Parameters |
Items* |
n |
Cronbach's alpha |
| Glucose Management |
Q1, Q4, Q6, rQ10, rQ12 |
5 |
0.577 |
| Dietary Control |
Q2, rQ5, Q9, rQ13 |
4 |
0.578 |
| Physical Activity |
Q8, rQ11, rQ15 |
3 |
0.758 |
| Health Care Use |
Q3, rQ7, rQ14 |
3 |
0.262 |
| Overall rating of self-care |
rQ16 |
1 |
NA |
| DSMQ Sum Scale (16 items) |
Q1, Q2, Q3, Q4, rQ5, Q6, rQ7, Q8, Q9, rQ10, rQ11, rQ12rQ13, rQ14, rQ15, rQ16 |
16 |
0.720 |
| Overall COVID-19 Impact |
rQ17,rQ18,rQ19 |
3 |
0.708 |
| DSMQ Sum Scale (19 items) |
Q1, Q2, Q3, Q4, rQ5, Q6, rQ7, Q8, Q9, rQ10, rQ11, rQ12, rQ13, rQ14, rQ15, rQ16,rQ17,rQ18,rQ19 |
19 |
0.719 |
Table 4.
Descriptive analysis of total score and subscales of DSMQ (n = 341).
Table 4.
Descriptive analysis of total score and subscales of DSMQ (n = 341).
| Parameters |
DMSQ score |
Turkish population
POST-COVID
(adapted from [8])
n = 378
|
Saudi population POST-COVID
(current study)
n = 341
|
Saudi population
BEFORE COVID
(adapted from [7])
n = 352
|
| Glucose Management |
5.18 ± 0.24 |
7.35 ± 1.94 |
7.8 ± 2.3 |
| Dietary Control |
5.20 ± 1.15 |
6.82 ± 2.17 |
6.5 ± 1.5 |
| Physical Activity |
5.10 ± 0.22 |
6.12 ± 2.95 |
5.8 ± 1.1 |
| Health Care Use |
5.24 ± 0.56 |
8.6 ± 1.77 |
4.8 ± 1.2 |
| Overall rating of self-care |
NA |
8.45 ± 2.65 |
NA |
| DSMQ Sum Scale (16 items) |
5.25 ± 1.04 |
7.29 ± 1.4 |
NA |
| Overall COVID-19 Impact |
NA |
7.81 ± 2.37 |
NA |
| DSMQ Sum Scale (19 items) |
NA |
7.37 ± 1.28 |
NA |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).