Submitted:
04 December 2023
Posted:
05 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Materials
- -
- age between 20 and 25 years old,
- -
- good general health.
- -
- chronic systemic diseases
- -
- past injury or surgery in the head or face area,
- -
- good oral health - no presence of any ongoing dental pain.
2.2. Method
2.2.1. Emotional state assessment
2.2.2. Pain Pressure Threshold Assessment
2.3. Statistical analysis
3. Results
3.1. Results
3.2. Figures, Tables and Schemes
3.2.1. Figures:
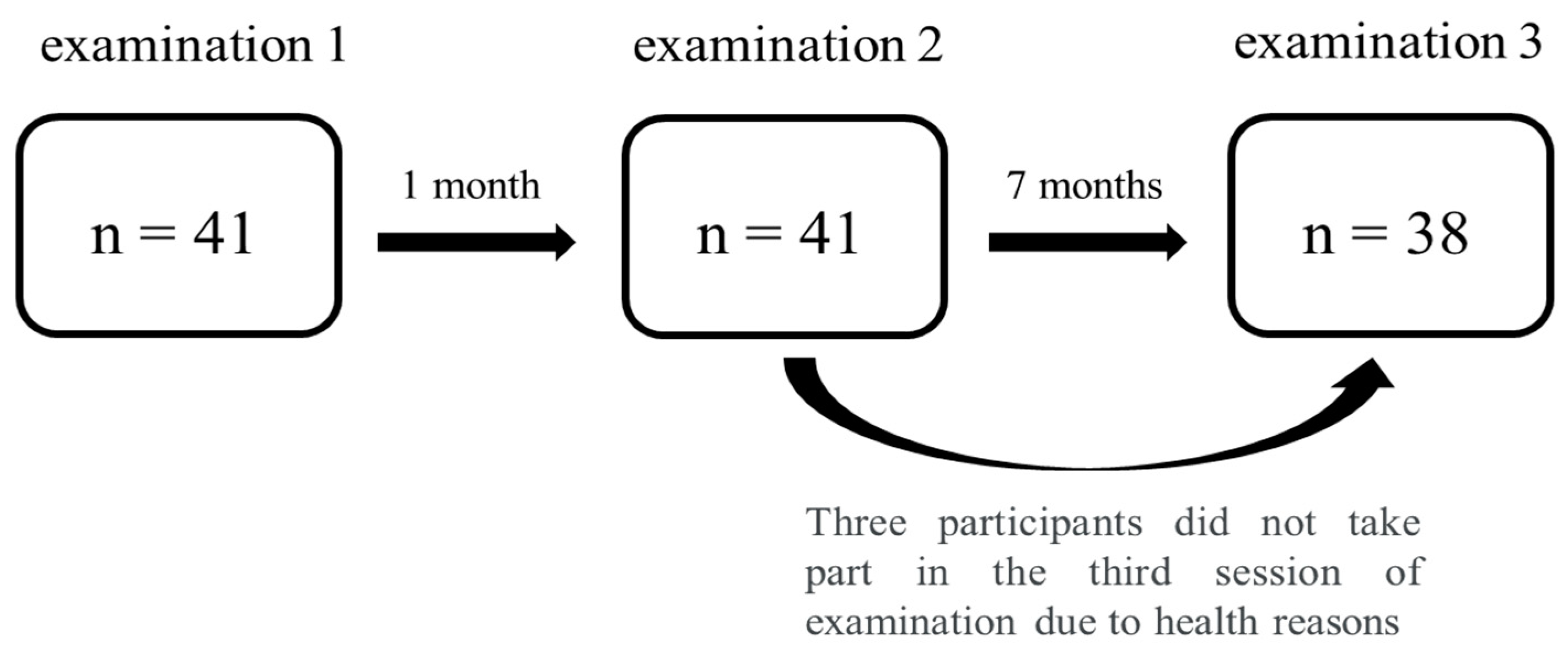
- Group size and time schedule of the examination sessions. [source: own project]……………….3
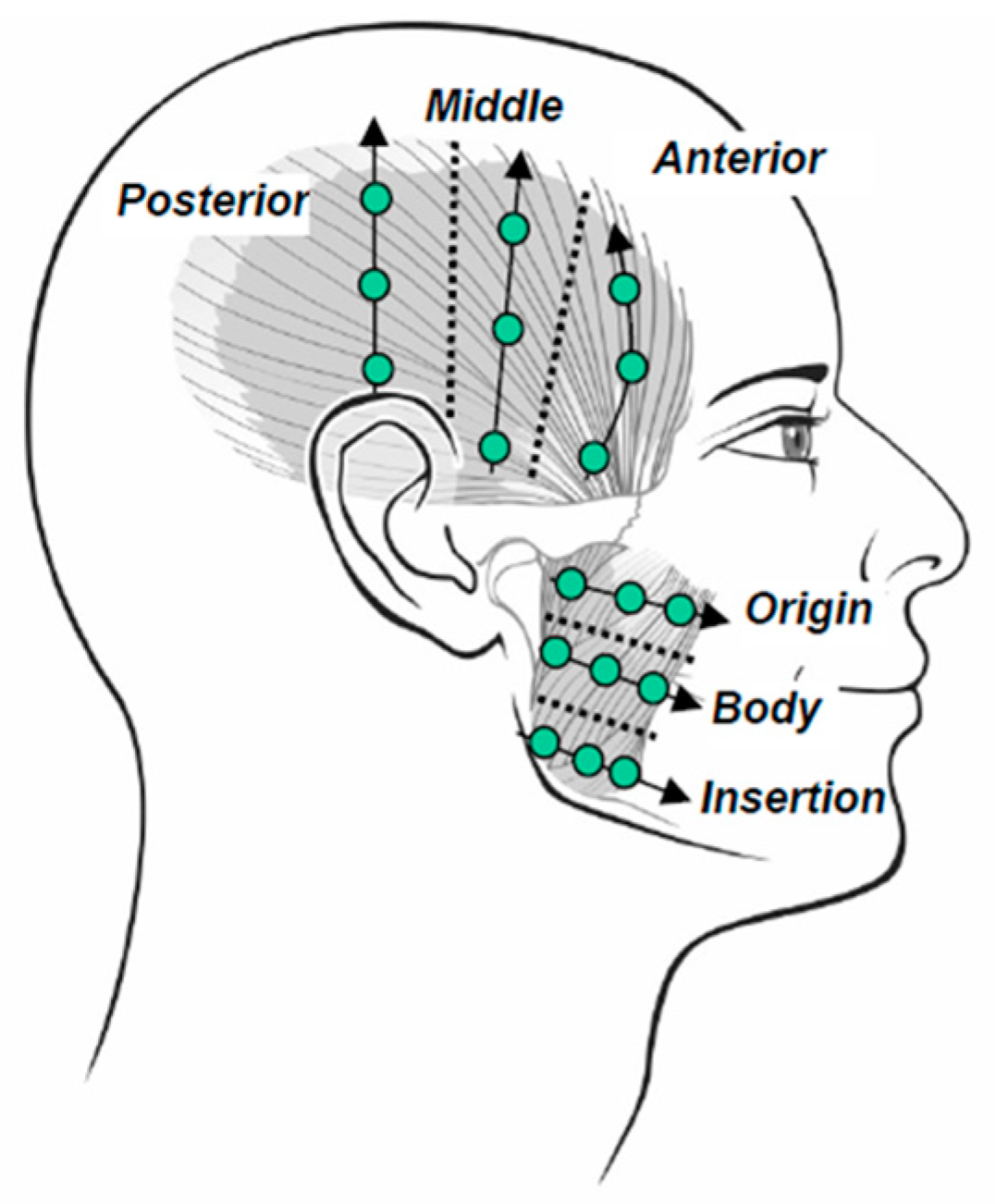
- Localization of the points on the masseter muscle for PPT examination. [source: Schiffman et al., 2014]..………………………………………………………….…………….………………………...4
3.2.2. Tables:
- Number of participants in TMD and control groups during each examination session…………5
- Results of chronic pain (GCPS) and the emotional state (PHQ-9 and GAD-7) questionnaires in the TMD and control groups in all three examination sessions…..……………….………………..5
- Dimorphic differences between the results of chronic pain (GCPS) and the emotional state (PHQ-9 and GAD-7) questionnaires…………………..……………………………………………….6
- Pressure pain threshold (PPT) changes between the sessions (1, 2 or 3) for the right (MR) and the left masseter muscle (ML)…………………………………………………………………………..7
- Correlation between chronic orofacial pain questionnaire (GCPS) and pressure pain threshold (PPT) between the three examination sessions. Right (MR) and left (ML) masseter muscles…...7
4. Discussion
5. Conclusions
- The orofacial pain scores were higher in the TMD group compared with the control subjects.
- The prevalence of pain, depression and anxiety was higher in female subjects, but only some were significant.
- The PPT (only of the right masseter) correlates with the incidence and intensity of chronic orofacial pain assessed by the GCPS questionnaire results, but not in all cases.
- The PPT tested with an algometer on the masseter muscles does not correlate with the emotional state measured with PHQ-9 and GAD-7 in the study population.
Study Advantages
Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kessler, R. C., de Jonge, P., Shahly, V., van Loo, H. M., Wang, P. S. E., & Wilcox, M. A. Epidemiology of depression. Annu Rev Public Health. 2014; 34:119–138. [CrossRef]
- Athanas, A., McCorrison, J., Campistron, J., Bender, N., Price, J., Smalley, S., & Schork, N. J. Characterizing Emotional State Transitions During Prolonged Use of a Mindfulness and Meditation App: Observational Study, JMIR Mental Health, 2021; 8(3). [CrossRef]
- Yang, Y., Ligthart, L., Terwindt, G. M., Boomsma, D. I., Rodriguez-Acevedo, A. J., & Nyholt, D. R. Genetic epidemiology of migraine and depression, Cephalalgia, 2016; 36(7), 679-691. [CrossRef]
- Farnik, M., & Pierzchała, W., Stan emocjonalny, funkcje poznawcze i jakość życia u chorych na OBPS, Pneumonologia i Alergologia Polska, 2007, 75 (supl 1), 77-79. Polish. [CrossRef]
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P, List T, Svensson P, Gonzales Y. Diagnostic criteria for Temporomandibular Disorders (DC-TMD) for clinical and research applications: Recommendations of the International RDC-TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain headache; 2014; 28(1):6-27. [CrossRef]
- Simoen, L., Van den Berghe, L., Jacquet, W., & Marks, L. Depression and anxiety levels in patients with temporomandibular disorders: Comparison with the general population, Clinical oral investigations, 2020; 24(11), 3939-3945. [CrossRef]
- Morley S., Psychologiczne koncepcje bólu Dobrogowski J. Wardliczek J. (red) Terapie uzupełniające w leczeniu bólu, Elsevier Urban & Partner Wrocław, 2010.
- Strachan, E., Poeschla, B., Dansie, E., Succop, A., Chopko, L., & Afari, N. Clinical and evoked pain, personality traits, and emotional states: Can familial confounding explain the associations?, Journal of psychosomatic research, 2015; 78(1), 58-63. [CrossRef]
- Khedr, M. A., El Sayed, H. G., & El Wakil, A. Perceived stress in multiple sclerosis patients: Relationship with mood states and pain experience. Multiple sclerosis and related disorders, 2022; 59,103650. Advance online publication. [CrossRef]
- Von Korff, M. (2011). Assessment of chronic pain in epidemiological and health services research: Empirical bases and new directions. In D. C. Turk & R. Melzack (Eds.), Handbook of pain assessment (pp. 455–473). The Guilford Press.
- Lövgren, A., Parvaneh, H., Lobbezoo, F., Häggman-Henrikson, B., Wänman, A., & Visscher, C. M. Diagnostic accuracy of three screening questions (3Q/TMD) in relation to the DC/TMD in a specialized orofacial pain clinic, Acta Odontologica Scandinavica, 2018; 76(6), 380-386. [CrossRef]
- Ramalho, D., Macedo, L., Goffredo Filho, G., Goes, C., & Tesch, R. Correlation between the levels of non-specific physical symptoms and pressure pain thresholds measured by algometry in patients with temporomandibular disorders, Journal of oral rehabilitation, 2015; 42(2), 120-126. [CrossRef]
- Herpich CM, Gomes CAFP, Dibai-Filho AV, Politti F, Souza CDS, Biasotto-Gonzalez DA, Correlation Between Severity of Temporomandibular Disorder, Pain Intensity, and Pressure Pain Threshold, J Manipulative Physiol Ther, 2017; Jan;41(1):47-51. [CrossRef]
- Tesch, R. D. S., Fernandes, F. S., Favilla, E. E., De Goffredo Filho, G. S., & Goes Differences in non-specific physical symptom levels and pressure pain thresholds between patients with masticatory myofascial pain and arthralgia, Cranio : the journal of craniomandibular practice, 2018; 38(6), 389–395. [CrossRef]
- Argoff, C. E., Dubin, A., Pilitsis, J., & McCleane, G., Pain management secrets E-Book. Elsevier Health Sciences; 2009.
- Jerez-Mayorga, D., Dos Anjos, C. F., Macedo, M. C., Fernandes, I. G., Aedo-Muñoz, E., Intelangelo, L., & Barbosa, A. C. Instrumental validity and intra/inter-rater reliability of a novel low-cost digital pressure algometer. PeerJ, 2020; 8, e10162. [CrossRef]
- Suchocka L. Psychologia Bólu, Warszawa, Wydawnictwo Difin; 2008.
- Sibille, K. T., Kindler, L. L., Glover, T. L., Staud, R., Riley III, J. L., & Fillingim, R. B. Affect balance style, experimental pain sensitivity, and pain-related responses, The Clinical journal of pain, 2012; 28(5), 410. [CrossRef]
- De la Torre Canales, G., Bonjardim, L. R., Poluha, R. L., Soares, F. F. C., Guarda-Nardini, L., Conti, P. R., & Manfredini, D. Correlation between physical and psychosocial findings in a population of temporomandibular disorder patients, Int J Prosthodont, 2020; 33(2), 155-9. [CrossRef]
- Bitiniene D, Zamaliauskiene R, Kubilius R, Leketas M, Gailius T, Smirnovaite K. Quality of life in patients with temporomandibular disorders. A systematic review. Stomatologija. 2018;20(1):3-9.
- Baldacci, F., Lucchesi, C., Cafalli, M., Poletti, M., Ulivi, M., Vedovello, M. & Gori, S. Migraine features in migraineurs with and without anxiety–depression symptoms: A hospital-based study, Clinical neurology and neurosurgery, 2015; 132, 74-78. [CrossRef]
- Crofford, L. J. Psychological aspects of chronic musculoskeletal pain. Best practice & research Clinical rheumatology, 2015; 29(1), 147-155. [CrossRef]
- Goesling, J., Clauw, D. J., & Hassett, A. L. Pain and depression: an integrative review of neurobiological and psychological factors, Current psychiatry reports, 2013, 15(12), 421. [CrossRef]
- Rodriguez-Blanco, C., Cocera-Morata, F. M., Heredia-Rizo, A. M., Ricard, F., Almazán-Campos, G., & Oliva-Pascual-Vaca, Á. Immediate effects of combining local techniques in the craniomandibular area and hamstring muscle stretching in subjects with temporomandibular disorders: a randomized controlled study, The journal of alternative and complementary medicine, 2015; 21(8), 451-459. [CrossRef]
- Fritz, C. O., Morris, P. E., & Richler, J. J. Effect size estimates: Current use, calculations, and interpretation. Journal of Experimental Psychology: General, 2012; 141(1), 2–18. [CrossRef]
- Sójka, A., Stelcer, B., Roy, M., Mojs, E., & Pryliński, M. Is there a relationship between psychological factors and TMD?. Brain and behavior, 2019; 9(9), e01360. [CrossRef]
- Kotiranta, U., Forssell, H., & Kauppila, T. Painful temporomandibular disorders (TMD) and comorbidities in primary care: associations with pain-related disability. Acta odontologica Scandinavica, 2019, 77(1), 22–27. [CrossRef]
- Stålnacke C, Ganzer N, Liv P, Wänman A, Lövgren A. Prevalence of temporomandibular disorder in adult patients with chronic pain. Scand J Pain. 2020 Sep 24;21(1):41-47. [CrossRef]
- Osiewicz, M., Lobbezoo, F., Ciapała, B., Pytko-Polończyk, J., & Manfredini, D. Pain Predictors in a Population of Temporomandibular Disorders Patients. Journal of clinical medicine, 2020; 9(2), 452. [CrossRef]
- Chantaracherd, P., John, M. T., Hodges, J. S., & Schiffman, E. L. Temporomandibular joint disorders' impact on pain, function, and disability. Journal of dental research, 2015; 94(3 Suppl), 79S–86S. [CrossRef]
- Knuutila, J., Kivipuro, J., Näpänkangas, R., Auvinen, J., Pesonen, P., Karppinen, J., Paananen, M., Pirttiniemi, P., Raustia, A., & Sipilä, K. Association of temporomandibular disorders with pain sensitivity: A cohort study. European journal of pain (London, England), 2022; 26(1), 143–153. [CrossRef]
- Mohn, C., Vassend, O., & Knardahl, S. Experimental pain sensitivity in women with temporomandibular disorders and pain-free controls: the relationship to orofacial muscular contraction and cardiovascular responses. The Clinical journal of pain, 2008; 24(4), 343–352. [CrossRef]
- Miettinen, O., Lahti, S., & Sipilä, K. Psychosocial aspects of temporomandibular disorders and oral health-related quality-of-life. Acta odontologica Scandinavica, 2012; 70(4), 331–336. [CrossRef]
- Nozaki-Taguchi, N., Hayashida, T., & Isono, S. Qualitative measurement of opioid effects on pain and dyspnea: gender difference in the sensitivity. JA clinical reports, 2020; 6(1), 85. [CrossRef]
- Moutinho, I. L., Maddalena, N. C., Roland, R. K., Lucchetti, A. L., Tibiriçá, S. H., Ezequiel, O. D., & Lucchetti, G. Depression, stress and anxiety in medical students: A cross-sectional comparison between students from different semesters. Revista da Associacao Medica Brasileira (1992), 2017; 63(1), 21–28. [CrossRef]
- Tysiąc-Miśta, M. K., Pudlo, R., Nitsze-Wierzba, M., & Fischer, P. Badanie poziomu lęku i depresji wśród lekarzy dentystów z terenu województwa śląskiego na podstawie skali HADS. Psychiatria, 2022. [CrossRef]
- de Araújo Vitor, C. A., de Oliveira Lira Ortega, A., Ferreira, A. C. F. M., Da Silva, C. A., Gallottini, M. H. C., & Santos, M. T. B. R. Pressure pain threshold of masticatory muscles in children and adolescents with and without intellectual disability: A pilot study, European Archives of Paediatric Dentistry, 2021; 22(4), 587-593. [CrossRef]
- Slade, G. D., Sanders, A. E., Ohrbach, R., Fillingim, R. B., Dubner, R., Gracely, R. H., & Greenspan, J. D., Pressure pain thresholds fluctuate with, but do not usefully predict, the clinical course of painful temporomandibular disorder, PAIN, 2014; 155(10), 2134-2143. [CrossRef]
- Shao, B., Teng, H., Dong, S., & Liu, Z. Finite element contact stress analysis of the temporomandibular joints of patients with temporomandibular disorders under mastication. Computer methods and programs in biomedicine, 2022; 213, 106526. [CrossRef]
- Rollman, G. B., & Lautenbacher, S. Sex differences in musculoskeletal pain. The Clinical journal of pain, 2001; 17(1), . [CrossRef]
| Group (n=38) | Examination 1 | Examination 2 | Examination 3 |
| TMD | 24 (f14, m10) | 22 (f12, m10) | 21 (f12, m9) |
| control | 14 (f9, m5) | 16 (f11, m5) | 17 (f11, m6) |
| Questionnaire | TMD group | Control group | p value | Effect Size (R) | ||||
| mean | median | Interquartile range |
mean | median | interquartile range | |||
| GCPS1 | 0,95±0,95 | 1,00 | 1,00 | 0,71±0,27 | 0,00 | 0,00 | <0,001* | 0,61 |
| GCPS2 | 1,18±1,01 | 1,00 | 2,00 | 0,00±0,00 | 0,00 | 0,00 | <0,001* | 0,73 |
| GCPS3 | 1,19±1,12 | 1,00 | 3,00 | 0,12±0,48 | 0,00 | 0,00 | <0,001* | 0,64 |
| PHQ-91 | 8,75±4,71 | 8,50 | 6,00 | 6,71±4,71 | 5,00 | 7,00 | 0,187 | 0,26 |
| PHQ-92 | 8,27±4,62 | 8,00 | 6,00 | 11,44±5,12 | 10,50 | 10,50 | 0,202 | -0,07 |
| PHQ-93 | 9,10±6,39 | 8,00 | 8,00 | 11,76±8,02 | 10,00 | 10,00 | 0,310 | -0,20 |
| GAD-71 | 9,00±4,94 | 7,00 | 6,00 | 7,07±5,20 | 5,00 | 8,00 | 0,202 | 0,25 |
| GAD-72 | 8,05±4,40 | 6,50 | 6,00 | 11,94±4,40 | 13,00 | 11,00 | 0,523 | -0,13 |
| GAD-73 | 8,57±5,32 | 7,00 | 8,00 | 11,47±7,37 | 13,00 | 14,00 | 0,257 | -0,22 |
| Questionnaire | TMD group | Control group | p value | Effect Size (R) | ||||
| mean | median | interquartile range | mean | median | interquartile range | |||
| GCPS1 | 0,87±1,01 | 1,00 | 1,00 | 0,27±0,46 | 0,00 | 1,00 | 0,048* | 0,35 |
| GCPS2 | 0,83±1,11 | 0,00 | 2,00 | 0,47±0,64 | 0,00 | 1,00 | 0,502 | 0,12 |
| GCPS3 | 0,91±1,24 | 0,00 | 2,00 | 0,40±0,51 | 0,00 | 1,00 | 0,429 | 0,14 |
| PHQ-91 | 8,74±4,47 | 8,00 | 7,00 | 6,87±5,10 | 5,00 | 7,00 | 0,178 | 0,26 |
| PHQ-92 | 9,96±5,80 | 9,00 | 9,00 | 7,20±5,06 | 6,00 | 9,00 | 0,198 | 0,25 |
| PHQ-93 | 12,22±7,60 | 10,00 | 10,00 | 7,33±5,51 | 7,00 | 10,00 | 0,047* | 0,39 |
| GAD-71 | 9,70±5,30 | 8,00 | 9,00 | 6,13±3,89 | 6,00 | 5,00 | 0,059 | 0,37 |
| GAD-72 | 10,48±5,43 | 10,00 | 10,00 | 6,27±4,27 | 5,00 | 8,00 | 0,016* | 0,47 |
| GAD-73 | 11,22±6,32 | 10,00 | 11,00 | 7,80±6,13 | 7,00 | 11,00 | 0,088 | 0,33 |
| PPT | p value | Effect Size (R) |
| MR1 − MR2 | 1,000 | 0,03 |
| MR1 − MR3 | 0,032* | 0,41 |
| MR2 − MR3 | 0,004* | 0,52 |
| ML1 − ML2 | 1,000 | 0,08 |
| ML1 − ML3 | 0,729 | 0,19 |
| ML2 − ML3 | 0,969 | 0,16 |
| MR/ML examination 1 |
MR/ML examination 2 |
MR/ML examination 2 |
|
| GCPS1 | -0,421*/-0,437* | - | - |
| GCPS2 | - | -0,484*/-0,455* | - |
| GCPS3 | - | - | -0,315/-0,185 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





