| Patient |
78 yo, male |
| Pathology |
Tongue base Angioleiomyoma |
| Treatment |
Surgery: Trans-Oral Robotic Surgery (TORS) |
| Novelty of this paper |
Trans-Oral Robotic Surgery to resect selected lesions of the oropharynx as an alternative to external approaches that lead to greater functional sequelae. |
1. Introduction
Non-epithelial tumours, in particular soft tissue tumours, are a varied group of pathologies less common but clinically relevant in the approach to the neoplastic pathology of the head and neck. Unfortunately, the much lower frequency compared to epithelial pathology and the absence of univocal treatment protocols translates into a limited availability of data in literature starting from epidemiological data up to clinical, radiological characteristics and therapeutic outcome 1.
Leiomyoma is a benign tumour arising from the smooth muscle. A hereditary etiology had already been described in the middle of the last century, lately a higher incidence in women has been described and could be attributed to hormonal variations. It is commonly observed in patients between the ages of 40 and 50 2.
A particular type of leiomyoma is the vascular leiomyoma or angioleiomyoma that arises from vascular smooth muscle (from the tunica media of veins and arteries). Morimoto in 1973 classified them into three types 3. It occurs more frequently in women between 30 and 60 years of age and normally like a painful solid mass in the skin of lower extremities and upper extremities. About 8.5% occurs in the head-neck region, mostly in the oral cavity, lips, ear, submandibular region, sinonasal cavities, larynx and masticatory space. In this location it usually presents as a small swelling of a few millimetres under a normotrophic mucosa.
It can also present, but with less frequency, with multiple swellings. It is usually asymptomatic, rarely it is associated with pain, and the consistency is soft 4.
Fibromas and lipomas, from a clinical point of view, may present similar findings to angioleiomyomas; hence a differential diagnosis must be established. Histological findings play a key role in the final diagnosis of leiomyoma. The differential diagnosis, moreover, must also include the malignant form of leiomyoma, i.e. leiomyosarcoma.
Imaging modalities may provide some limited diagnostic clues about the lesions. On MRI, angioleiomyoma appear hypo- to iso-intense on T1 and mixed hyper-intense signal on T2. CT scan density of the lesions can also vary from iso-hypo to iso-hyperdense. Therefore, the radiological differentiation can be difficult as they lack specific radiological features 5.
Surgical excision with section margins conducted on healthy tissue and confirmation of the diagnostic suspicion through a correct and careful histological examination, makes the possibility of recurrence scarce.
We here present the case of a tongue base angioleiomyoma with an emphasis on clinical data, pathologic findings and surgical approach.
2. Case report
A 78-year-old male patient presented to the ENT Department of our hospital complaining about a one-month history of globus sensation, dysphagia and a few episodes of hemoptysis. There was no fever or other systemic symptoms and the patient didn’t report any dyspnea, hoarseness, laryngeal pain, odynophagia or cough. The patient had a history of benign prostatic hyperplasia for which he was being treated with doxazosin. He did not have a smoking history.
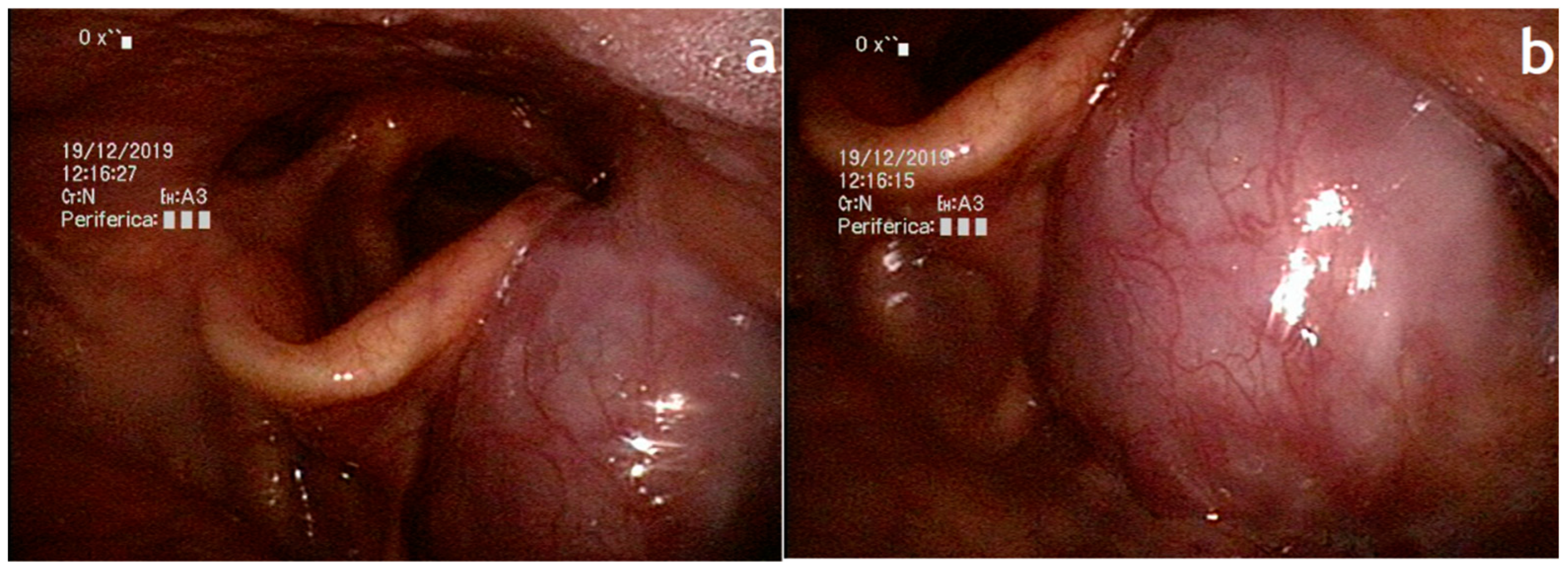
The patient underwent an ENT examination with laryngoscopy that revealed the presence of a 2 cm solitary submucosal mass located on the left tongue base covered with normal mucosa, with no signs of ulceration or active bleeding. The pharynx and larynx were mobile, and no other abnormalities were found in the remaining head and neck examination
(Figure 1).
Figure 1.
Preoperative appearance of the lesion (endoscopic view). a Laryngoscopy before the operation showing a 2 cm oval mass located on the left tongue base. b Epiglottis appears slightly dislocated by the mass, normal breathing space, no signs of active bleeding.
Figure 1.
Preoperative appearance of the lesion (endoscopic view). a Laryngoscopy before the operation showing a 2 cm oval mass located on the left tongue base. b Epiglottis appears slightly dislocated by the mass, normal breathing space, no signs of active bleeding.
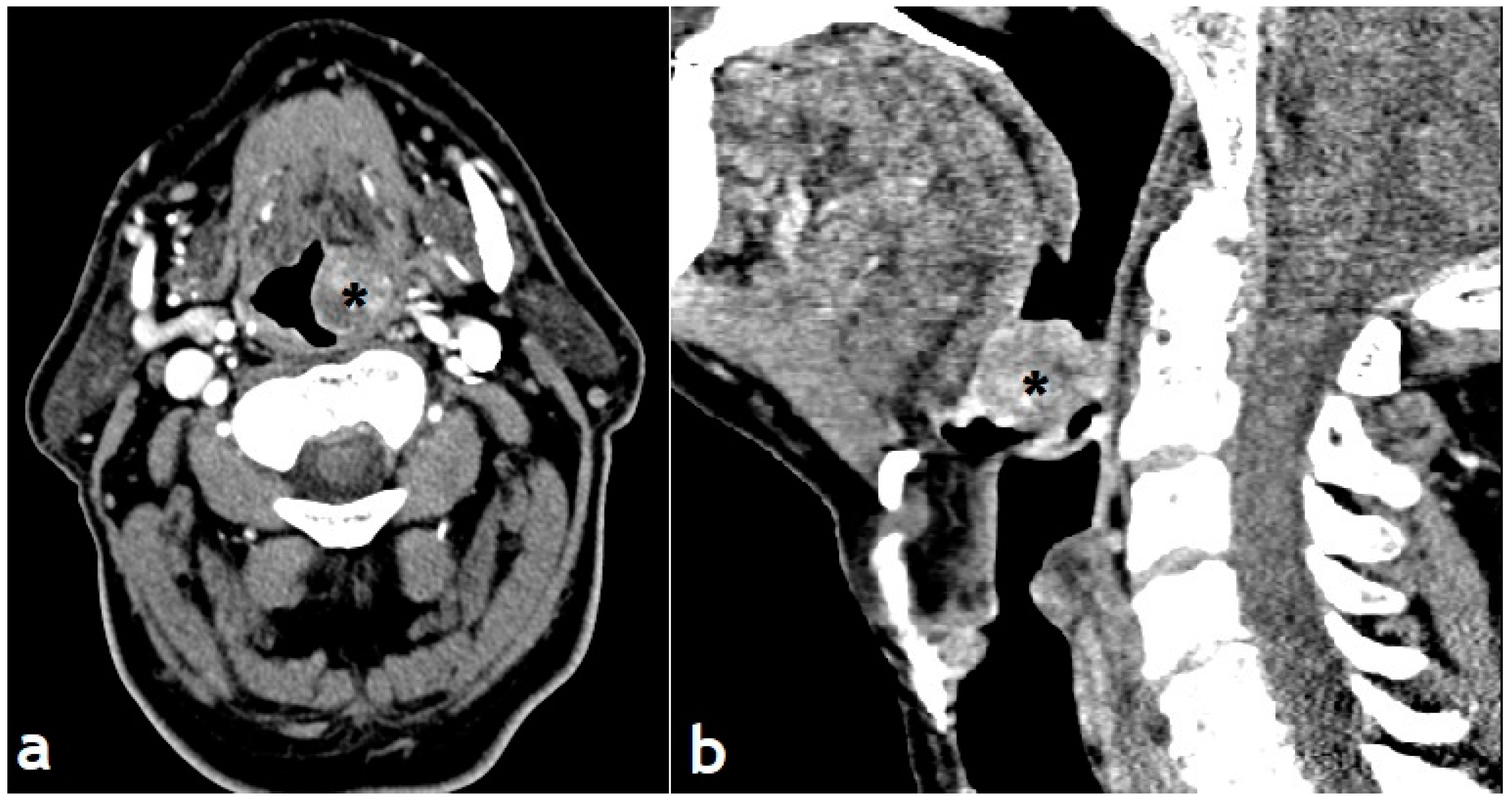
Computed tomography (CT) revealed a 2.0-cm-sized well-circumscribed inhomogeneous left tongue base mass with no evidence of involvement or destruction of adjacent structures. These findings indicated a tumor with potentially rich vascularisation
(Figure 2).
Figure 2.
Preoperative CT scan showing a 2 cm well-defined mass originating from the left tonsillar pillar and extends to the supraglottic plane causing deviation of the oropharyngeal lumen.
Figure 2.
Preoperative CT scan showing a 2 cm well-defined mass originating from the left tonsillar pillar and extends to the supraglottic plane causing deviation of the oropharyngeal lumen.
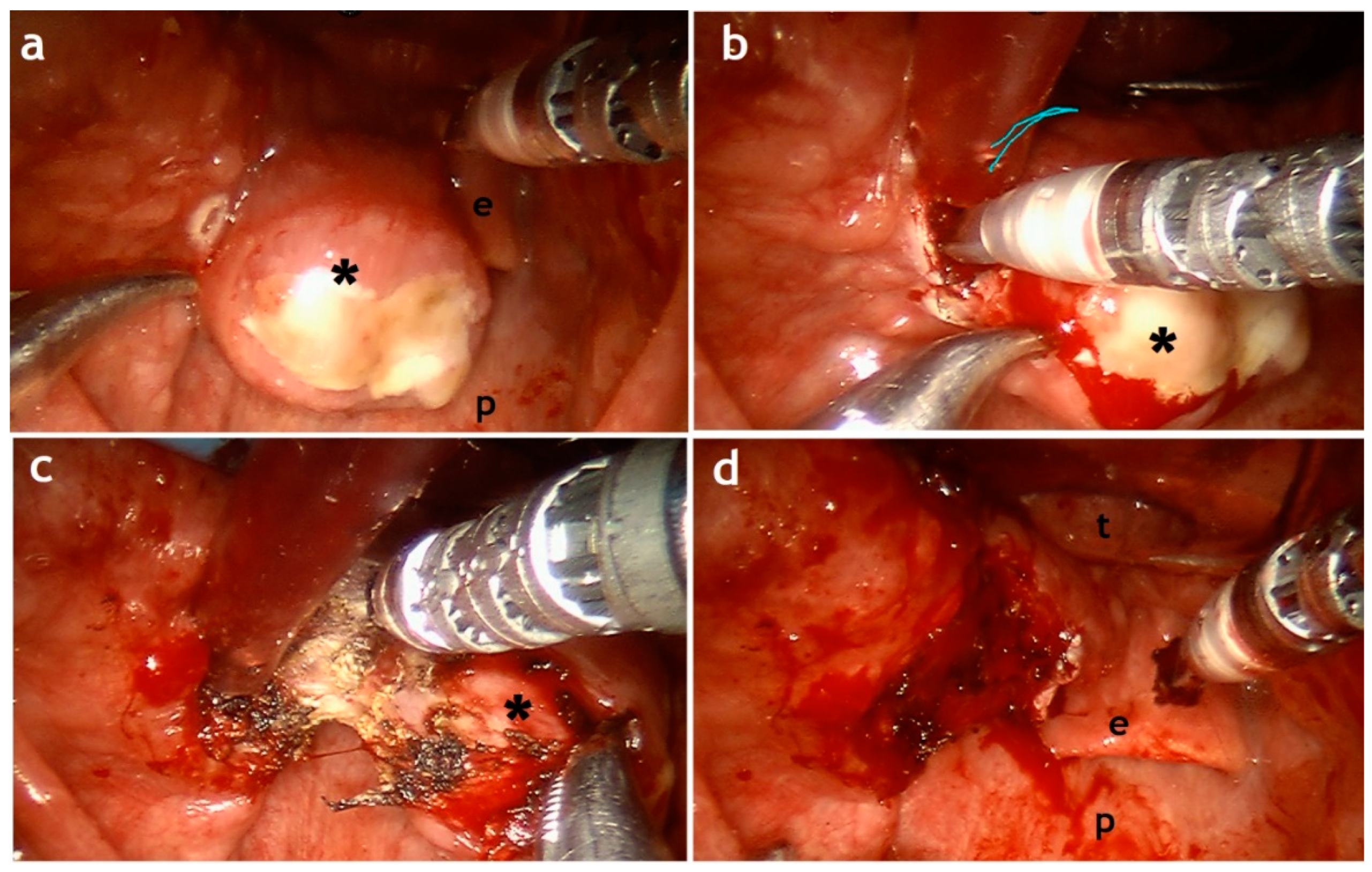
The patient underwent a direct laryngoscopy under general anaesthesia and a biopsy was performed. During biopsy no major bleeding was encountered. Histopathological analysis was suggestive for angioleiomyoma and a diagnosis of a tongue base angioleiomyoma was made. Treatment options were discussed. Surgical resection was proposed, and the patient accepted a transoral robot-assisted resection. After a standard tracheotomy, the da Vinci system was set up as for transoral procedures and the patient was treated according to our standardized technique by two experienced surgeons.
67(
Figure 3).
Figure 3.
Intraoperative appearance with a transoral robotic-assisted procedure. a Intraoperative aspect of the lesion before excision with signs of previous biopsy. b-c Robotic phases of the procedure. d Complete resection of the lesion. Epiglottis (e); posteriorpharyngeal wall (p); lesion(*); tongue (t).
Figure 3.
Intraoperative appearance with a transoral robotic-assisted procedure. a Intraoperative aspect of the lesion before excision with signs of previous biopsy. b-c Robotic phases of the procedure. d Complete resection of the lesion. Epiglottis (e); posteriorpharyngeal wall (p); lesion(*); tongue (t).
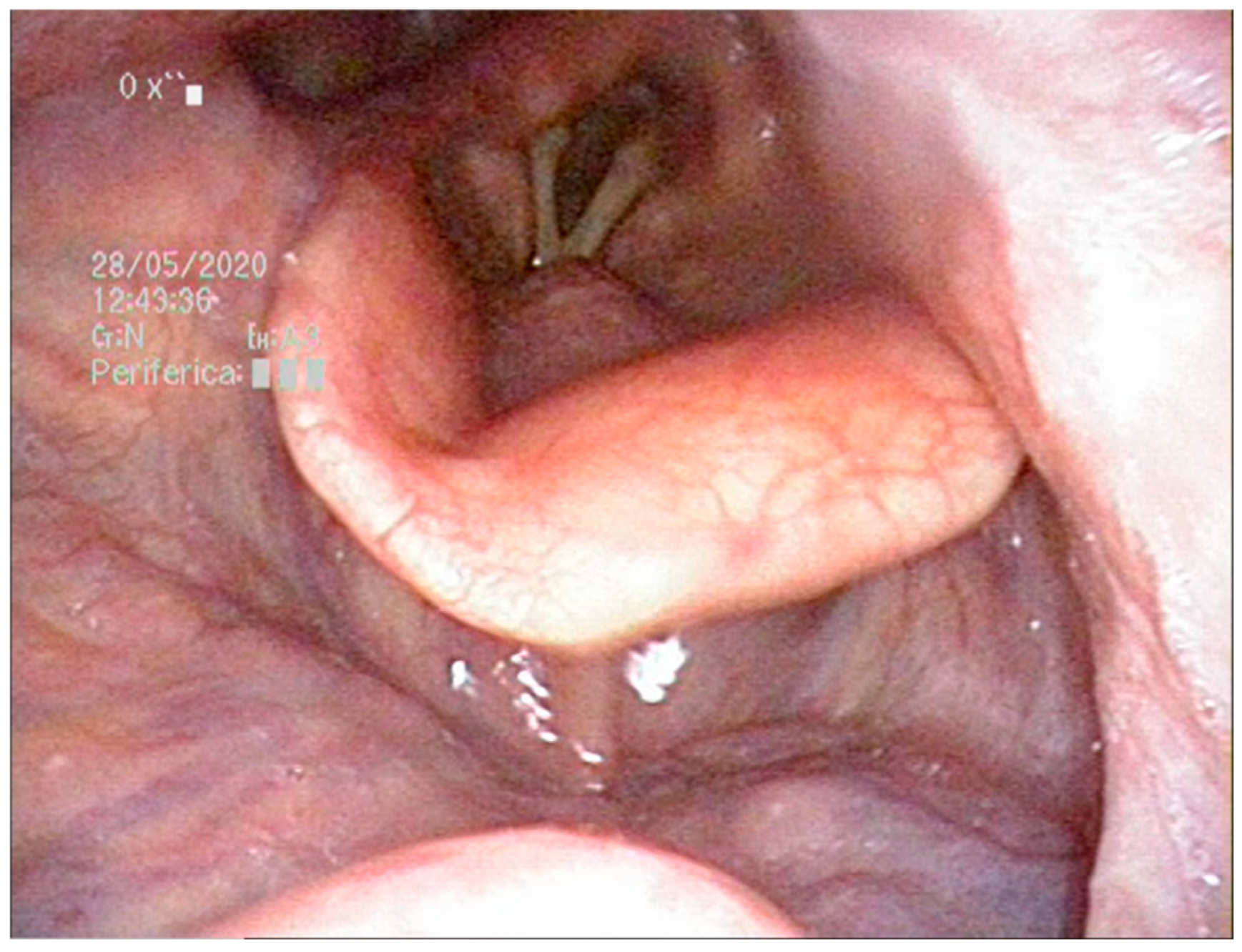
A nasogastric tube was placed. Surgical procedure was uneventful, and no major bleeding was encountered. Haemostasis was achieved with bipolar forceps and a suture point. The patient was allowed a soft postoperative diet on post-operative day 6 and the feeding tube was removed the day after. Tracheotomy was removed on post-operative day 9. No post-operative bleeding was observed. The patient was discharged on day 10. Histological examination confirmed the presence of a 2 cm angioleiomyoma of the tongue base. Follow-up showed perfect healing of the tongue base mucosa and the patient reported no swallowing problems
(Figure 4). The patient refused to perform a post-op imaging.Written informed consent has been obtained from the patient to publish this paper.
Figure 4.
A 6-months follow-up endoscopic examination showing perfect healing of the tongue base mucosa.
Figure 4.
A 6-months follow-up endoscopic examination showing perfect healing of the tongue base mucosa.
3. Discussion
The World Health Organization defines leiomyoma as a “circumscribed benign, often cutaneous tumour composed of intersecting bundles of mature smooth muscle cells.” It also classifies leiomyomas into three groups: solid leiomyoma, vascular leiomyoma (angioleiomyoma) and epithelioid leiomyoma (leiomyoblastoma). Our patient presented an angioleiomyoma of the tongue base. Morimoto further classified angioleiomyomas into three histologic subtypes: (1) capillary or solid: The most common type, which shows closely compacted smooth muscle and many small, slit-like vascular channels. (2) Venous: vascular channels with thick, easily identifiable muscular walls. (3) Cavernous: the vascular channels are dilated with less smooth muscle.
Head and neck angioleiomyomas are really uncommon. More often they occur in the subcutis of lower and upper extremities. In the head and neck, they have been found more frequently in the nasal cavity, paranasal sinus and oral cavity. The tongue base is an even more uncommon location. Up to date there are only 17 cases of tongue base angioleiomyoma published in literature 8.
Many studies report a female preponderance; by contrast the patient of our case is a male patient. Zhu et al. suggest that sex hormones are possibly associated with the growth of angioleiomyoma 9.
Clinically speaking angioleiomyomas of the upper and lower limbs present as solitary or multiple extremely painful lesions. Tongue base angioleiomyomas usually present as painless, slow growth, solitary lesions. Symptoms are mostly due to mass effect and clinical presentation is strongly influenced by the size of the lesion. Our patient complaint mainly about globus sensation, dysphagia and a few episodes of haemoptysis. This unspecific clinical presentation could mimic different other lesions, such as inflammatory disease, benign mesenchymal tumours, soft tissue cystic lesions and vascular lesions 10.
Given the non-specific clinical presentation it is mandatory to require an imaging exam and a biopsy with patohistological and immunohistochemical analysis of the tumour tissue that will give a definite diagnosis. It is very important to distinguish these tumours from their malignant forms, leiomyosarcomas. No case of malignant transformation of oral angioleiomyoma was reported to date 7.
In cases where imaging shows severe signs of hypervascularization, a preoperative angiography could be advisable 11. In our case MRI did not show signs of hypervascularization; it was therefore not considered appropriate to perform a preoperative angiography. Given the position of the lesion and the experience of our team with transoral robotic-assisted surgery, it was decided, in agreement with the patient, to proceed with transoral robotic-assisted surgery (TORS). Surgery started by positioning a temporary tracheostomy before the TORS time, useful for preventing difficulty during intubation and allowing better tumour exposure12.Although different surgical approaches have been described, the transoral approach provides good exposure and is less traumatic with better post-operative recovery. Visualization of the surgical field was excellent. The patient was operated on without any significant problem; the angled vision offered by the machine allows dissection under direct control. The robotic phase of our surgery lasted less than 45 minutes and was performed as follows: resection of the lesion on the left tongue base, check for clean margins, careful haemostasis with bipolar forceps and suture points. The transcervical suprahyoid approach and lateral pharyngotomy are equally effective but at the same time associated with significant morbidity. Laser-assisted procedure have good advantages, but they need a high level of surgical skill 13. Hemorrhage is one of the most common complications following TORS and is the cause of 30% of readmissions. The severity of post-TORS hemorrhage can range from minor bleeding treated with observation to catastrophic hemorrhage leading to emergent tracheotomy for airway management and even death. No consensus on risk factors for post-TORS hemorrhage or its management currently exists in the literature 14. In our case we decided for a safety tracheotomy that was removed on post-operative day 9. No major bleeding was encountered during surgery and postoperative. Clearly the description of our case does not want to have a purpose in terms of indications but wants to describe the possibility of considering TORS in the case of benign tumours of the tongue base, such as angioleiomyomas. Especially in rare cases like this where a standard technique can difficulty be achieved.
Pratt et al. suggest that image guidance as applied to TORS procedures could be an exciting proposition, since the regions of interest (e.g., the tongue base, oropharynx) are typically adjacent to and enclosed by rigid anatomy and proximity to critical vasculature and other vitally important anatomical structures; additional studies are required.15
We therefore believe that in terms of efficacy and quality of life, robotic technology should be considered a more than valid alternative to conventional open procedures, as its minimally invasive approach results in significant benefits for the patient such as faster recovery times and better functional outcomes, less postoperative pain and morbidity, shorter operative times, and a reduction in the risk of infection15, additionally TORS allows access for oropharyngeal resection without pharyngotomy or mandibulotomy, maintaining the critical muscular framework of the laryngopharynx necessary to preserve swallowing function. 16
4. Conclusion
Tongue angioleiomyoma are extremely rare, benign, vascular tumours characterized with slow growth and nonspecific clinical presentation. Surgical treatment with transoral robotic surgery was proven to be safe and useful in reducing intraoperative and postoperative complications and recovery time.
References
- Razek, A. A. & Huang, B. Y. Soft Tissue Tumors of the Head and Neck: Imaging-based Review of the WHO Classification. RadioGraphics31, 1923–1954 (2011). [CrossRef]
- Ramesh, P., Annapureddy, S. R., Khan, F. & Sutaria, P. D. Angioleiomyoma: a clinical, pathological and radiological review: Angioleiomyoma: A Review. Int. J. Clin. Pract.58, 587–591 (2004). [CrossRef]
- Weiss, S. W., Goldblum, J. R. & Enzinger, F. M. Enzinger and Weiss’s soft tissue tumors. (Mosby, 2001).
-
Pathology and genetics of head and neck tumours: ... reflects the views of a working group that convened for an Editorial and Consensus Conference in Lyon, France, July 16 - 19, 2003. (IARC Press, 2007).
- Wong, S. W., Laybourne, J., Irion, L. & Cook, A. A rare case of orbital angioleiomyoma. Orbit40, 60–64 (2021). [CrossRef]
- Dallan, I. et al. Transoral robotic tongue base reduction and supraglottoplasty combined with maxillomandibular advancement: a new option for selected sleep apnea patients? Preliminary report. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. EUFOS Affil. Ger. Soc. Oto-Rhino-Laryngol. - Head Neck Surg.276, 3543–3548 (2019). [CrossRef]
- Fiacchini, G., Vianini, M., Dallan, I. & Bruschini, L. Is the Da Vinci Xi system a real improvement for oncologic transoral robotic surgery? A systematic review of the literature. J. Robot. Surg.15, 1–12 (2021). [CrossRef]
- Danić, D. et al. Harmonic scalpel surgical treatment of the tongue angioleomyoma--case report and review of the literature. Coll. Antropol.36 Suppl 2, 167–170 (2012).
- Zhu, G., Xiao, D. & Sun, P. Expression of estrogen and progesterone receptors in angioleiomyoma of the nasal cavity of six patients. Oncol. Lett.11, 2359–2364 (2016).. [CrossRef]
- Liu, Y. et al. Angioleiomyomas in the head and neck: A retrospective clinical and immunohistochemical analysis. Oncol. Lett.8, 241–247 (2014). [CrossRef]
- Sung, Y. E., Rhee, C. K. & Lee, K. Y. A Rare Case of Angioleiomyoma Arising in the Subglottic Area to Upper Trachea of a Patient with Underlying Asthma. J. Pathol. Transl. Med.51, 92–95 (2017). [CrossRef]
- Mercante, G., Ruscito, P., Pellini, R., Cristalli, G. & Spriano, G. Transoral robotic surgery (TORS) for tongue base tumours. Acta Otorhinolaryngol. Ital. Organo Uff. Della Soc. Ital. Otorinolaringol. E Chir. Cerv.-facc.33, 230–235 (2013).
- Dallan, I. et al. Transoral robotic resection of an ectopic tongue-base thyroid gland. J. Robot. Surg.7, 83–86 (2013). [CrossRef]
- Stokes, W. et al. Bleeding Complications After Transoral Robotic Surgery: A Meta-Analysis and Systematic Review. The Laryngoscope131, 95–105 (2021). [CrossRef]
- Pratt, P. & Arora, A. Transoral Robotic Surgery: Image Guidance and Augmented Reality. ORL80, 204–212 (2018).
- Hutcheson, K. A., Holsinger, F. C., Kupferman, M. E. & Lewin, J. S. Functional outcomes after TORS for oropharyngeal cancer: a systematic review. Eur. Arch. Otorhinolaryngol.272, 463–471 (2015). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).