Submitted:
27 December 2023
Posted:
28 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
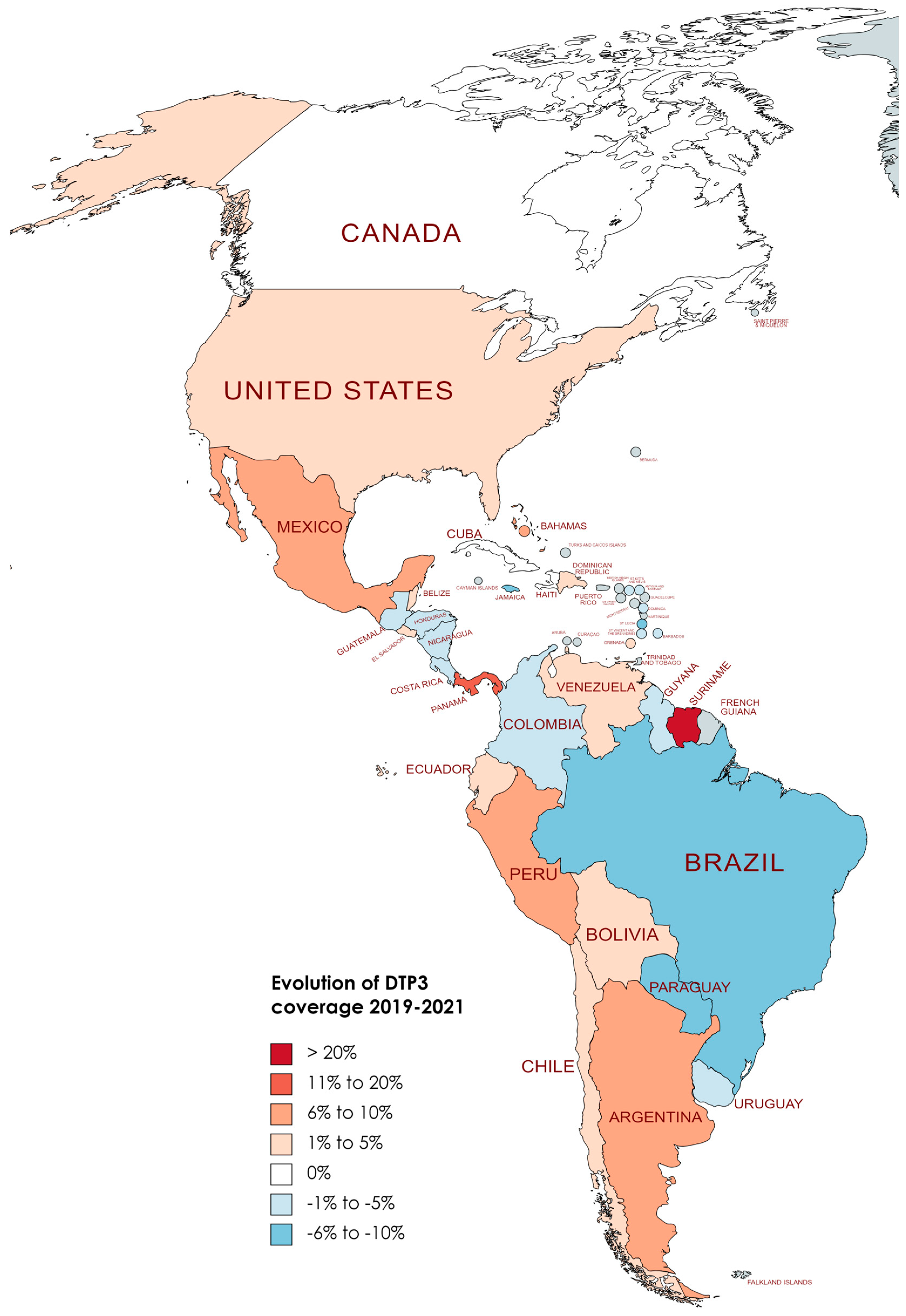
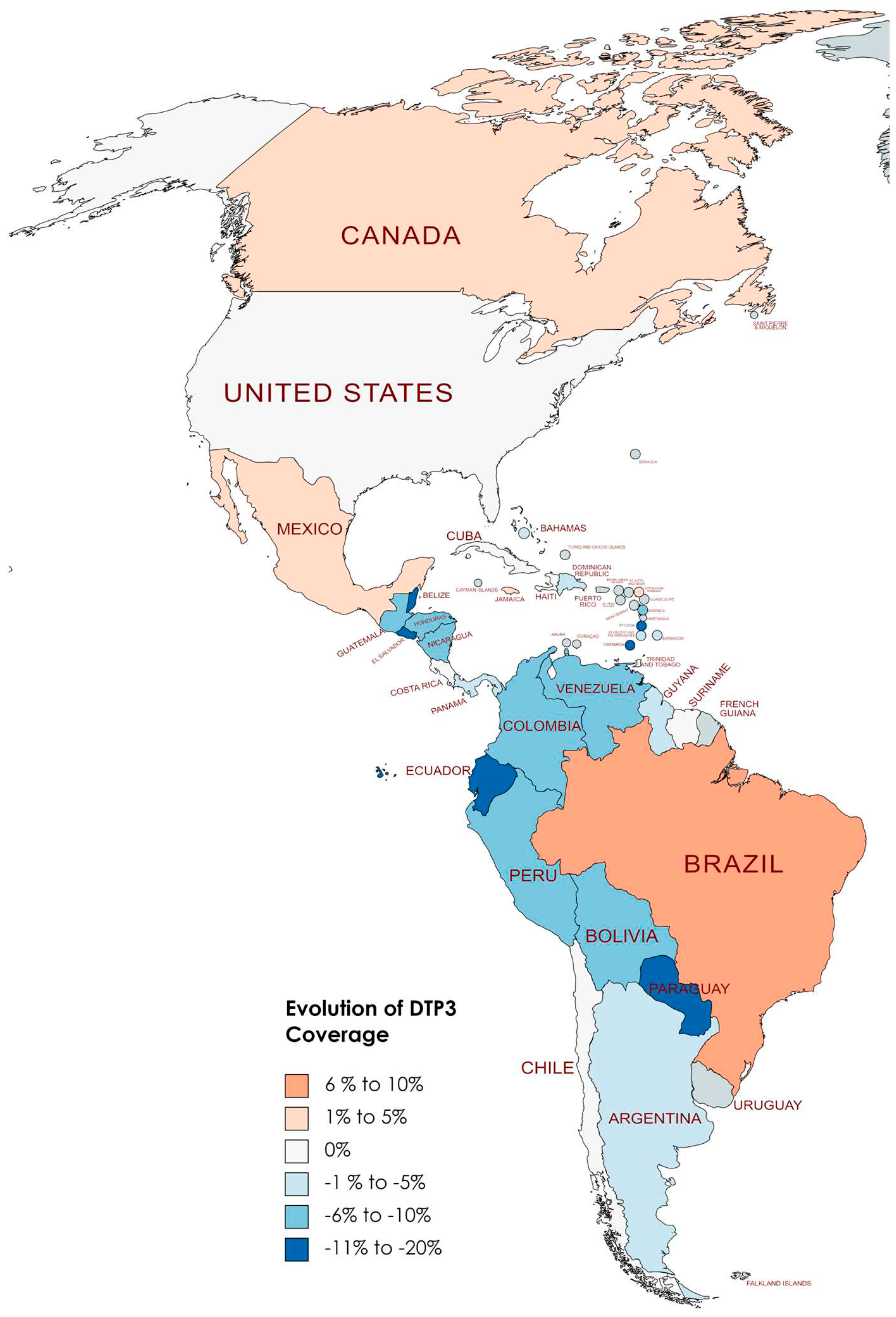
2.1. Regional Analysis
2.2. Statistical Analysis
2.3. Software
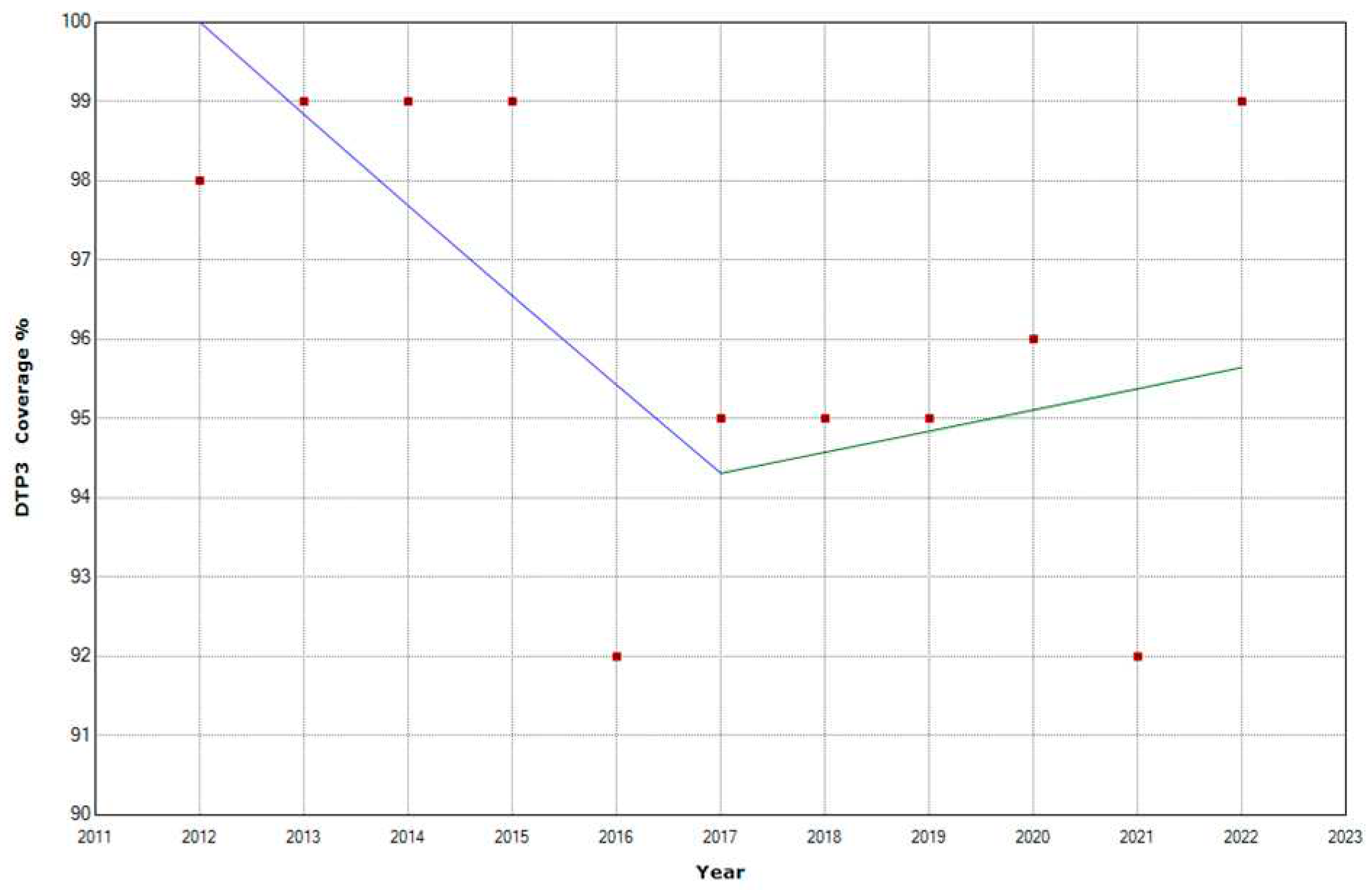
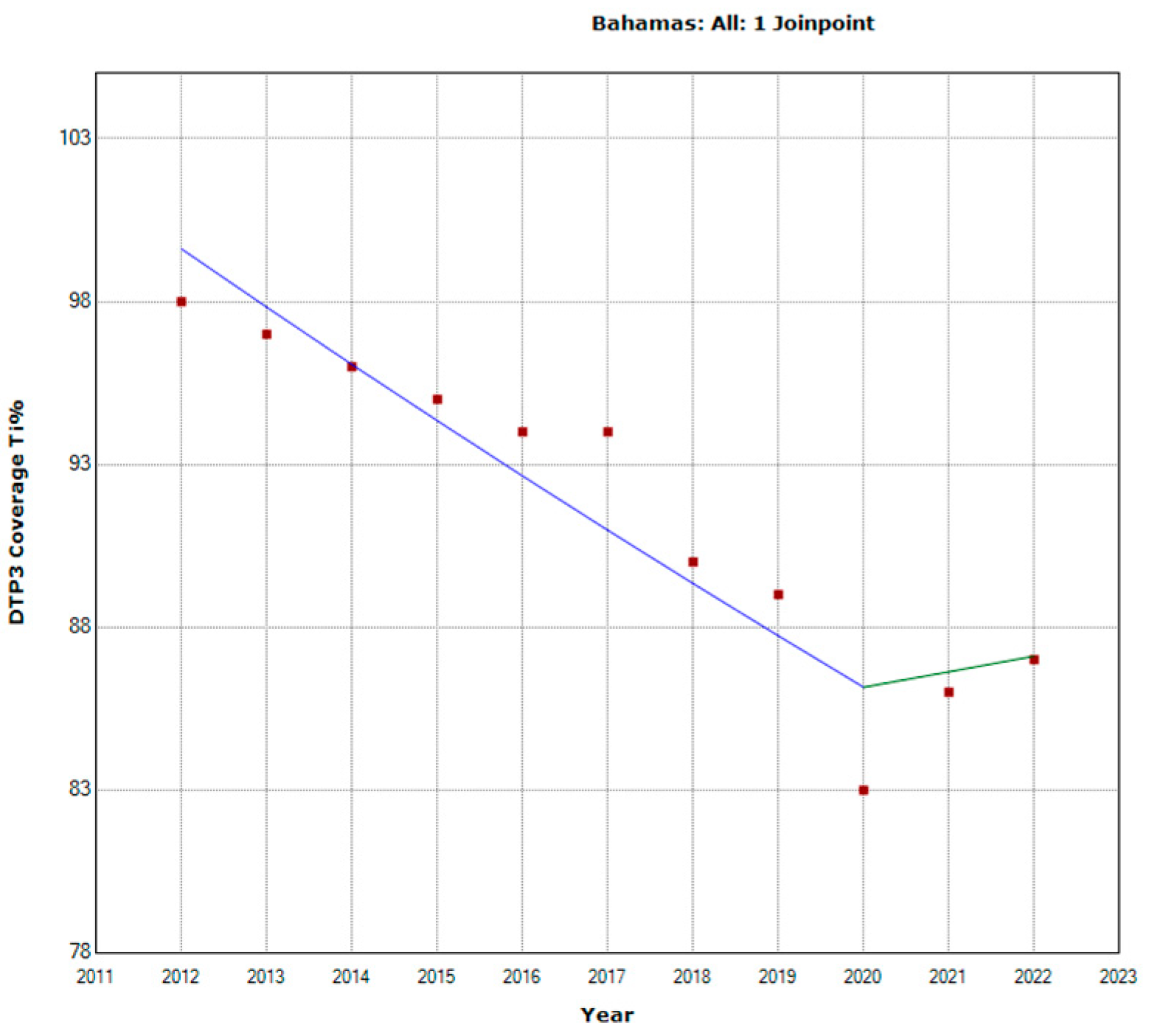
3. Results
4. Discussion
4.1. Overview of the Study and Its Context
4.1.1. Methodological Considerations and Data Limitations
4.1.2. Discrepancies in Vaccine Coverage Data and Trend Analysis.
4.2. Analysis of DTP3 Vaccination Trends
4.3. Comparative Global and Regional Perspectives
4.4. Influential Factors and Challenges
4.5. Strategies and Interventions for Enhancing Vaccine Coverage
4.6. The Role of Healthcare Systems and Planning
4.7. Looking to the Future
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ota, M. O. C.; de Moraes, J. C.; Vojtek, I.; Constenla, D.; Doherty, T. M.; Cintra, O.; Kirigia, J. M. Unveiling the Contributions of Immunization for Progressing towards Universal Health Coverage. Hum Vaccin Immunother 2022, 18 (1). [CrossRef]
- Suffel, A. M.; Ojo-Aromokudu, O.; Carreira, H.; Mounier-Jack, S.; Osborn, D.; Warren-Gash, C.; McDonald, H. I. Exploring the Impact of Mental Health Conditions on Vaccine Uptake in High-Income Countries: A Sys-tematic Review. BMC Psychiatry 2023, 23 (1), 15. [CrossRef]
- Hassan, M. N. A Survey on Hygienic Practices and Immunization Coverage among 12-59 Months Old Chil-dren in Urban Slum, Barishal, Bangladesh. Asian Journal of Medical and Biological Research 2022, 8 (4), 277–285. [CrossRef]
- Evans, A.; Mahar, A. L.; Deb, B.; Boblitz, A.; Brownell, M.; Guttmann, A.; Stukel, T. A.; Cohen, E.; Sarkar, J.; Eze, N.; Katz, A.; Raveendran, T.; Saunders, N. Gaps in Childhood Immunizations and Preventive Care Visits during the COVID-19 Pandemic: A Population-Based Cohort Study of Children in Ontario and Manitoba, Canada, 2016–2021. Canadian Journal of Public Health 2023, 114 (5), 774–786. [CrossRef]
- Stein, R. A. Vaccination: A Public Health Intervention That Changed History & Is Changing with His-tory. Am Biol Teach 2011, 73 (9), 513–519. [CrossRef]
- Pan, J.; Wang, Y.; Cao, L.; Wang, Y.; Zhao, Q.; Tang, S.; Gong, W.; Guo, L.; Liu, Z.; Wen, Z.; Zheng, B.; Wang, W. Impact of Immunization Programs on 11 Childhood Vaccine-Preventable Diseases in China: 1950–2018. The Innovation 2021, 2 (2), 100113. [CrossRef]
- Espinal, M. A. The Pan American Health Organization: 120 Years in the Americas Hemisphere. The Lancet Regional Health - Americas 2023, 21, 100488. [CrossRef]
- Zulfan, G. P.; Sihombing, J. A.; Amin, D. M.; Widiantari, A. D.; Berti, M. P. E.; Murtiani, F. Clinical Manifesta-tion of Childhood Diphtheria. Jurnal Ilmiah Kedokteran Wijaya Kusuma 2023, 12 (1), 1. [CrossRef]
- WHO. Global Vaccine Action Plan 2011-2020.; WHO Press: Geneva, 2013.
- Shahid, A. S. M. S. Bin; Rahman, A. E.; Shahunja, K. M.; Afroze, F.; Sarmin, M.; Nuzhat, S.; Alam, T.; Chow-dhury, F.; Sultana, M. S.; Ackhter, M. M.; Parvin, I.; Saha, H.; Islam, S. Bin; Shahrin, L.; Ahmed, T.; Chisti, M. J. Vaccination Following the Expanded Programme on Immunization Schedule Could Help to Reduce Deaths in Children under Five Hospitalized for Pneumonia and Severe Pneumonia in a Developing Country. Front Pediatr 2023, 11. [CrossRef]
- Atteraya, M. S.; Song, I. H.; Ebrahim, N. B.; Gnawali, S.; Kim, E.; Dhakal, T. Inequalities in Childhood Im-munisation in South Asia. Int J Environ Res Public Health 2023, 20 (3), 1755. [CrossRef]
- Basu, S.; Ashok, G.; Debroy, R.; Ramaiah, S.; Livingstone, P.; Anbarasu, A. Impact of the COVID-19 Pandemic on Routine Vaccine Landscape: A Global Perspective. Hum Vaccin Immunother 2023, 19 (1). [CrossRef]
- Budu, E.; Ahinkorah, B. O.; Guets, W.; Ameyaw, E. K.; Essuman, M. A.; Yaya, S. Socioeconomic and Resi-dence-based Related Inequality in Childhood Vaccination in Sub-Saharan Africa: Evidence from Benin. Health Sci Rep 2023, 6 (4). [CrossRef]
- Albers, A. N.; Wright, E.; Thaker, J.; Conway, K.; Daley, M. F.; Newcomer, S. R. Childhood Vaccination Prac-tices and Parental Hesitancy Barriers in Rural and Urban Primary Care Settings. J Community Health 2023, 48 (5), 798–809. [CrossRef]
- Santoli, J. M.; Lindley, M. C.; DeSilva, M. B.; Kharbanda, E. O.; Daley, M. F.; Galloway, L.; Gee, J.; Glover, M.; Herring, B.; Kang, Y.; Lucas, P.; Noblit, C.; Tropper, J.; Vogt, T.; Weintraub, E. Effects of the COVID-19 Pan-demic on Routine Pediatric Vaccine Ordering and Administration — United States, 2020. MMWR Morb Mortal Wkly Rep 2020, 69 (19), 591–593. [CrossRef]
- Zhong, Y.; Clapham, H. E.; Aishworiya, R.; Chua, Y. X.; Mathews, J.; Ong, M.; Wang, J.; Murugasu, B.; Chiang, W. C.; Lee, B. W.; Chin, H.-L. Childhood Vaccinations: Hidden Impact of COVID-19 on Children in Singapore. Vaccine 2021, 39 (5), 780–785. [CrossRef]
- Tolera, S. T., Kaweti, G., & Aboma, L. M. Article Review on Potential Impact of COVID-19 Pandemic on So-cioeconomic of Ethiopia, Africa. Health Sciences 2022, 11 (8), 19–30.
- Yang, J.; Vaghela, S.; Yarnoff, B.; De Boisvilliers, S.; Di Fusco, M.; Wiemken, T. L.; Kyaw, M. H.; McLaughlin, J. M.; Nguyen, J. L. Estimated Global Public Health and Economic Impact of COVID-19 Vaccines in the Pre-Omicron Era Using Real-World Empirical Data. Expert Rev Vaccines 2023, 22 (1), 54–65. [CrossRef]
- Chen, X.; Huang, H.; Ju, J.; Sun, R.; Zhang, J. Impact of Vaccination on the COVID-19 Pandemic in US States. Sci Rep 2022, 12 (1), 1554. [CrossRef]
- Heffernan, C. The ‘New Normal’: Delivering Childhood Immunisations during the COVID-19 Pandemic. Practice Nursing 2020, 31 (9). [CrossRef]
- Athiyaman, A.; Ajayi, T.; Mutuku, F.; Luwaga, F.; Bryer, S.; Giwa, O.; Mngemane, S.; Edwige, N. N.; Berman, L. Recovering from the Unprecedented Backsliding in Immunization Coverage: Learnings from Country Pro-gramming in Five Countries through the Past Two Years of COVID-19 Pandemic Disruptions. Vaccines (Basel) 2023, 11 (2), 375. [CrossRef]
- Naor, M.; Pinto, G. D.; Davidov, P.; Abdrbo, L. Rapidly Establishing an Ultra-Cold Supply Chain of Vaccines in Israel: Evidence for the Efficacy of Inoculation to Mitigate the COVID-19 Pandemic. Vaccines (Basel) 2023, 11 (2), 349. [CrossRef]
- He, K.; Mack, W. J.; Neely, M.; Lewis, L.; Anand, V. Parental Perspectives on Immunizations: Impact of the COVID-19 Pandemic on Childhood Vaccine Hesitancy. J Community Health 2022, 47 (1), 39–52. [CrossRef]
- McDonald, H. I.; Tessier, E.; White, J. M.; Woodruff, M.; Knowles, C.; Bates, C.; Parry, J.; Walker, J. L.; Scott, J. A.; Smeeth, L.; Yarwood, J.; Ramsay, M.; Edelstein, M. Early Impact of the Coronavirus Disease (COVID-19) Pandemic and Physical Distancing Measures on Routine Childhood Vaccinations in England, January to April 2020. Euro Surveill 2020, 25 (19). [CrossRef]
- Lassi, Z. S.; Naseem, R.; Salam, R. A.; Siddiqui, F.; Das, J. K. The Impact of the COVID-19 Pandemic on Im-munization Campaigns and Programs: A Systematic Review. Int J Environ Res Public Health 2021, 18 (3), 988. [CrossRef]
- Alsuhaibani, M.; Alaqeel, A. Impact of the COVID-19 Pandemic on Routine Childhood Immunization in Saudi Arabia. Vaccines (Basel) 2020, 8 (4), 581. [CrossRef]
- Palo, S. K.; Dubey, S.; Negi, S.; Sahay, M. R.; Patel, K.; Swain, S.; Mishra, B. K.; Bhuyan, D.; Kanungo, S.; Som, M.; Merta, B. R.; Bhattacharya, D.; Kshatri, J. S.; Pati, S. Effective Interventions to Ensure MCH (Maternal and Child Health) Services during Pandemic Related Health Emergencies (Zika, Ebola, and COVID-19): A Sys-tematic Review. PLoS One 2022, 17 (5), e0268106. [CrossRef]
- Kiely, M.; Mansour, T.; Brousseau, N.; Rafferty, E.; Paudel, Y. R.; Sadarangani, M.; Svenson, L. W.; Robinson, J. L.; Gagneur, A.; Driedger, S. M.; MacDonald, S. E. COVID-19 Pandemic Impact on Childhood Vaccination Coverage in Quebec, Canada. Hum Vaccin Immunother 2022, 18 (1). [CrossRef]
- Verrier, F.; de Lauzanne, A.; Diouf, J.-B. N.; Zo, A. Z.; Ramblière, L.; Herindrainy, P.; Sarr, F. D.; Sok, T.; Vray, M.; Collard, J.-M.; Borand, L.; Kermorvant-Duchemin, E.; Delarocque-Astagneau, E.; Guillemot, D.; Huynh, B.-T.; Randriamamonjiarison, A. N.; Volahasina, T. A.; Rasoanaivo, F.; Rakotoarimanana, F. M. J.; Raheliari-vao, T. B.; Randrianirina, F.; Chon, T.; Goyet, S.; Kerleguer, A.; Ngo, V.; Lach, S.; Long, P.; Tarantola, A.; Diatta, M.; Faye, J.; Seck, A.; Padget, M.; Abdou, A. Y.; Garin, B. Vaccination Coverage and Risk Factors Associated With Incomplete Vaccination Among Children in Cambodia, Madagascar, and Senegal. Open Forum Infect Dis 2023, 10 (4). [CrossRef]
- Hogan, D.; Gupta, A. Why Reaching Zero-Dose Children Holds the Key to Achieving the Sustainable Devel-opment Goals. Vaccines (Basel) 2023, 11 (4), 781. [CrossRef]
- Alexander, C.; Cabrera, M.; Moore, M.; Lomazzi, M. Driving Paediatric Vaccine Recovery in Europe. Vaccines (Basel) 2023, 11 (1), 184. [CrossRef]
- Causey, K.; Fullman, N.; Sorensen, R. J. D.; Galles, N. C.; Zheng, P.; Aravkin, A.; Danovaro-Holliday, M. C.; Martinez-Piedra, R.; Sodha, S. V; Velandia-González, M. P.; Gacic-Dobo, M.; Castro, E.; He, J.; Schipp, M.; Deen, A.; Hay, S. I.; Lim, S. S.; Mosser, J. F. Estimating Global and Regional Disruptions to Routine Childhood Vaccine Coverage during the COVID-19 Pandemic in 2020: A Modelling Study. The Lancet 2021, 398 (10299), 522–534. [CrossRef]
- Wiysonge, C. S.; Uthman, O. A.; Ndumbe, P. M.; Hussey, G. D. Individual and Contextual Factors Associated with Low Childhood Immunisation Coverage in Sub-Saharan Africa: A Multilevel Analysis. PLoS One 2012, 7 (5), e37905. [CrossRef]
- WHO. GLOBAL ROUTINE IMMUNIZATION STRATEGIES AND PRACTICES (GRISP) A Companion Document to the Global Vaccine Action Plan (GVAP); WHO: Geneva, 2016.
- WHO. Immunization and vaccine-preventable communicable diseases https://www.who.int/data/gho/data/themes/immunization (accessed 2023 -11 -12).
- Immunization and vaccine-preventable communicable diseases https://data.unicef.org/resources/immunization-coverage-are-we-losing-ground/ (accessed 2023 -04 -29).
- Cutts, F. T.; Izurieta, H. S.; Rhoda, D. A. Measuring Coverage in MNCH: Design, Implementation, and Inter-pretation Challenges Associated with Tracking Vaccination Coverage Using Household Surveys. PLoS Med 2013, 10 (5), e1001404. [CrossRef]
- Barbosa, J. Vaccination Week in the Americas Press Conference - Dr. Jarbas Barbosa, PAHO’s Director Re-marks - 20 April 2023 - PAHO/WHO | Pan American Health Organization https://www.paho.org/en/documents/vaccination-week-americas-press-conference-dr-jarbas-barbosa-pahos-director-remarks-20 (accessed 2023 -12 -15).
- PAHO. Fact Sheet - Vaccination Week in the Americas 2023 - PAHO/WHO | Pan American Health Organi-zation https://www.paho.org/en/documents/fact-sheet-vaccination-week-americas-2023 (accessed 2023 -12 -15).
- PAHO. Risk of vaccine-preventable disease outbreaks at 30-year high, PAHO Director says https://www.paho.org/en/news/20-4-2023-risk-vaccine-preventable-disease-outbreaks-30-year-high-paho-director-says (accessed 2023 -12 -15).
- WHO/UNICEF. Progress and Challenges with Achieving Universal Immunization Coverage. 2022 WHO/UNICEF Estimates of National Immunization Coverage (WUENIC); Geneva, 2023.
- Brown, C. L.; Montez, K.; Amati, J. B.; Simeonsson, K.; Townsend, J. D.; Orr, C. J.; Palakshappa, D. Impact of COVID-19 on Pediatric Primary Care Visits at Four Academic Institutions in the Carolinas. Int J Environ Res Public Health 2021, 18 (11), 5734. [CrossRef]
- Shet, A.; Carr, K.; Danovaro-Holliday, M. C.; Sodha, S. V; Prosperi, C.; Wunderlich, J.; Wonodi, C.; Reynolds, H. W.; Mirza, I.; Gacic-Dobo, M.; O’Brien, K. L.; Lindstrand, A. Impact of the SARS-CoV-2 Pandemic on Rou-tine Immunisation Services: Evidence of Disruption and Recovery from 170 Countries and Territories. Lancet Glob Health 2022, 10 (2), e186–e194. [CrossRef]
- Aguinaga-Ontoso, I.; Guillen-Aguinaga, S.; Guillen-Aguinaga, L.; Alas-Brun, R.; Onambele, L.; Aguina-ga-Ontoso, E.; Guillen-Grima, F. COVID-19 Impact on DTP Vaccination Trends in Africa: A Joinpoint Re-gression Analysis. Vaccines (Basel) 2023, 11 (6), 1103. [CrossRef]
- Castrejon, M. M.; Leal, I.; de Jesus Pereira Pinto, T.; Guzmán-Holst, A. The Impact of COVID-19 and Catch-up Strategies on Routine Childhood Vaccine Coverage Trends in Latin America: A Systematic Litera-ture Review and Database Analysis. Hum Vaccin Immunother 2022, 18 (6). [CrossRef]
- Munyangaju, I.; López-Varela, E.; Bassat, Q. Closing the Gap in Childhood Immunisation after the Pandemic. BMJ 2023, p627. [CrossRef]
- THE GLOBAL HEALTH OBSERVATORY. Immunization and vaccine-preventable communicable diseases Immunization and vaccine-preventable communicable diseases (accessed 2023 -11 -29).
- Kaur, G.; Danovaro-Holliday, M. C.; Mwinnyaa, G.; Gacic-Dobo, M.; Francis, L.; Grevendonk, J.; Sodha, S. V; Sugerman, C.; Wallace, A. Routine Vaccination Coverage — Worldwide, 2022. MMWR Morb Mortal Wkly Rep 2023, 72 (43), 1155–1161. [CrossRef]
- World Health Assembly. Immunization Agenda 2030: A Global Strategy to Leave No One Behind.; WHO: Geneva, 2020.
- UNICEF. COVID-19 pandemic fuels largest continued backslide in vaccinations in three decades https://www.unicef.org/press-releases/WUENIC2022release (accessed 2023 -05 -16).
- Data Warehouse - UNICEF DATA https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=IMMUNISATION&ver=1.0&dq=.IM_DTP3..&startPeriod=2000&endPeriod=2022 (accessed 2023 -04 -18).
- UNICEF. Number of Births. Data Warehouse - UNICEF DATA https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=GLOBAL_DATAFLOW&ver=1.0&dq=.DM_BRTS..&startPeriod=2019&endPeriod=2021 (accessed 2023 -05 -21).
- World Bank. Population, total | Data https://data.worldbank.org/indicator/SP.POP.TOTL (accessed 2023 -05 -21).
- White, K. J. The Durbin-Watson Test for Autocorrelation in Nonlinear Models. Rev Econ Stat 1992, 74 (2), 370. [CrossRef]
- Wagner, A. K.; Soumerai, S. B.; Zhang, F.; Ross-Degnan, D. Segmented Regression Analysis of Interrupted Time Series Studies in Medication Use Research. J Clin Pharm Ther 2002, 27 (4), 299–309. [CrossRef]
- Lopez Bernal, J.; Cummins, S.; Gasparrini, A. Interrupted Time Series Regression for the Evaluation of Public Health Interventions: A Tutorial. Int J Epidemiol 2016, dyw098. [CrossRef]
- Slavova, S.; Rock, P.; Bush, H. M.; Quesinberry, D.; Walsh, S. L. Signal of Increased Opioid Overdose during COVID-19 from Emergency Medical Services Data. Drug Alcohol Depend 2020, 214, 108176. [CrossRef]
- Joinpoint Regression Program. Version 4.3.1.0. April, 2016; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute.
- Kim, H. J.; Fay, M. P.; Feuer, E. J.; Midthune, D. N. Permutation Tests for Joinpoint Regression with Applica-tions to Cancer Rates. Stat Med 2000, 19 (3), 335–351. [CrossRef]
- Muggeo, V. M.; Atkins, D. C.; Gallop, R. J.; Dimidjian, S. Segmented Mixed Models with Random Change-points: A Maximum Likelihood Approach with Application to Treatment for Depression Study. Stat Model-ling 2014, 14 (4), 293–313. [CrossRef]
- Muggeo, V. M. R. Interval Estimation for the Breakpoint in Segmented Regression: A Smoothed Score-based Approach. Aust N Z J Stat 2017, 59 (3), 311–322. [CrossRef]
- Muggeo, V. M. R. Testing with a Nuisance Parameter Present Only under the Alternative: A Score-Based Approach with Application to Segmented Modelling. J Stat Comput Simul 2016, 86 (15), 3059–3067. [CrossRef]
- Fasola, S.; Muggeo, V. M. R.; Küchenhoff, H. A Heuristic, Iterative Algorithm for Change-Point Detection in Abrupt Change Models. Comput Stat 2018, 33 (2), 997–1015. [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria. 2023.
- RStudio Team. RStudio: Integrated Development for R. RStudio, PBC,: Boston, MA. 2023.
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer-Verlag: New York, 2016.
- Wickham, H.; Bryan, J. Readxl: Read Excel Files_. R Package Version 1.4.3. 2023.
- Mapchart Version 4.3.2. Mapchart. November 30, 2023.
- Brewer, C. A.; Hatchard, G. W.; Harrower, M. A. ColorBrewer in Print: A Catalog of Color Schemes for Maps. Cartogr Geogr Inf Sci 2003, 30 (1), 5–32. [CrossRef]
- Brewer, C. A.; Hatchard, G. W.; Harrower, M. A. COLORBREWER 2.0 Color Advice for Cartograph. 2013.
- Rau, C.; Lüdecke, D.; Dumolard, L. B.; Grevendonk, J.; Wiernik, B. M.; Kobbe, R.; Gacic-Dobo, M.; Danova-ro-Holliday, M. C. Data Quality of Reported Child Immunization Coverage in 194 Countries between 2000 and 2019. PLOS Global Public Health 2022, 2 (2), e0000140. [CrossRef]
- Maciak, M.; Mizera, I. Regularization Techniques in Joinpoint Regression. Statistical Papers 2016, 57 (4), 939–955. [CrossRef]
- Kontopantelis, E.; Doran, T.; Springate, D. A.; Buchan, I.; Reeves, D. Regression Based Quasi-Experimental Approach When Randomisation Is Not an Option: Interrupted Time Series Analysis. BMJ 2015, 350 (jun09 5), h2750–h2750. [CrossRef]
- Taljaard, M.; McKenzie, J. E.; Ramsay, C. R.; Grimshaw, J. M. The Use of Segmented Regression in Analysing Interrupted Time Series Studies: An Example in Pre-Hospital Ambulance Care. Implementation Science 2014, 9 (1), 77. [CrossRef]
- Bower, M.; Kothari, U.; Akerman, M.; Krilov, L. R.; Fiorito, T. M. Impact of COVID-19 on HPV Vaccination Rates in New York City and Long Island. Pediatric Infectious Disease Journal 2023. [CrossRef]
- Urueña, A.; Machado, R.; Cunha, J.; López Colmano, C.; Rancaño, C.; Kfouri, R.; Pírez, C.; Bonvehí, P.; Calvo, M.; Cuadros, R.; Muñoz, G.; Rodríguez, M.; Torres, J.; Cahn, F.; Ballalai, I. Opinions, Attitudes and Factors Related to SARS-CoV-2 Vaccine Uptake in Eight South American Countries. Vaccines (Basel) 2023, 11 (11), 1660. [CrossRef]
- Mwinnyaa, G.; Peters, M. A.; Shapira, G.; Neill, R.; Sadat, H.; Yuma, S.; Akilimali, P.; Hossain, S.; Wendrad, N.; Atiwoto, W. K.; Ofosu, A. A.; Alfred, J. P.; Kiarie, H.; Wesseh, C. S.; Isokpunwu, C.; Kangbai, D. M.; Mohamed, A. A.; Sidibe, K.; Drouard, S.; Fernandez, P. A.; Azais, V.; Hashemi, T.; Hansen, P. M.; Ahmed, T. Vaccination Utilization and Subnational Inequities during the COVID-19 Pandemic: An Interrupted Time-Series Analysis of Administrative Data across 12 Low- and Middle-Income Countries. Vaccines (Basel) 2023, 11 (9), 1415. [CrossRef]
- United Nations. Global disparity in access to essential vaccines, says WHO report | UN News https://news.un.org/en/story/2022/11/1130402 (accessed 2023 -12 -17).
- WHO. Vaccine inequity undermining global economic recovery https://www.who.int/news/item/22-07-2021-vaccine-inequity-undermining-global-economic-recovery (ac-cessed 2023 -12 -17).
- WHO. Global Vaccine Market Report 2022 https://www.who.int/publications/m/item/global-vaccine-market-report-2022 (accessed 2023 -12 -17).
- Guglielmi, G. Pandemic Drives Largest Drop in Childhood Vaccinations in 30 Years. Nature 2022, 608 (7922), 253. [CrossRef]
- OECD. Access to COVID-19 vaccines: Global approaches in a global crisis - OECD https://read.oecd-ilibrary.org/view/?ref=1069_1069384-ewmqrw9sx2&title=Access-to-COVID-19-vaccines-Global-approaches-in-a-global-crisis (accessed 2023 -12 -17).
- Handfield R. Challenges and Opportunities to Expand the COVID-19 Vaccine Supply Chain: A Global Sum-mit | Supply Chain Resource Cooperative https://scm.ncsu.edu/scm-articles/article/challenges-and-opportunities-to-expand-the-covid19-vaccine-supply-chain-a-global-summit (accessed 2023 -12 -17).
- Muhoza, P.; Danovaro-Holliday, M. C.; Diallo, M. S.; Murphy, P.; Sodha, S. V.; Requejo, J. H.; Wallace, A. S. Routine Vaccination Coverage — Worldwide, 2020. MMWR Morb Mortal Wkly Rep 2021, 70 (43), 1495–1500. [CrossRef]
- Evans, B.; Keiser, O.; Kaiser, L.; Jombart, T. Analysis of Global Routine Immunisation Coverage Shows Dis-ruption and Stagnation during the First Two-Years of the COVID-19 Pandemic with Tentative Recovery in 2022. Vaccine X 2023, 15, 100383. [CrossRef]
- Rachlin, A.; Carolina Danovaro-Holliday, M; Murphy, P.; Samir, Sodha, V.; Wallace, A. S. Report Routine Vaccination Coverage-Worldwide, 2021. Morbidity and Mortality Weekly 2021, 71 (44), 1396–1400.
- LaMori, J.; Feng, X.; Pericone, C. D.; Mesa-Frias, M.; Sogbetun, O.; Kulczycki, A. Hepatitis Vaccination Ad-herence and Completion Rates and Factors Associated with Low Compliance: A Claims-Based Analysis of US Adults. PLoS One 2022, 17 (2), e0264062. [CrossRef]
- Périères, L.; Séror, V.; Boyer, S.; Sokhna, C.; Peretti-Watel, P. Reasons given for Non-Vaccination and un-der-Vaccination of Children and Adolescents in Sub-Saharan Africa: A Systematic Review. Hum Vaccin Im-munother 2022, 18 (5). [CrossRef]
- Atnafu Gebeyehu, N.; Abebe Gelaw, K.; Asmare Adella, G.; Dagnaw Tegegne, K.; Adie Admass, B.; Mesele Gesese, M. Incomplete Immunization and Its Determinants among Children in Africa: Systematic Review and Meta-Analysis. Hum Vaccin Immunother 2023. [CrossRef]
- Cdc. CDC Strategy for Global Response to COVID-19 (2020-2023). 2022.
- Dayaratna K; Tyrrell P; Vanderplas A. A Comparative Analysis of Policy Approaches to COVID-19 Around the World, with Recommendations for US Lawmakers | The Heritage Foundation https://www.heritage.org/public-health/report/comparative-analysis-policy-approaches-covid-19-around-the-world (accessed 2023 -12 -17).
- Bliss, K. E. Strengthening Routine Immunizations and Responding to Covid-19. Center at the Center for Strategic and International Studies: Washington, DC 2020.
- de Albuquerque Veloso Machado, M.; Roberts, B.; Wong, B. L. H.; van Kessel, R.; Mossialos, E. The Relation-ship Between the COVID-19 Pandemic and Vaccine Hesitancy: A Scoping Review of Literature Until August 2021. Front Public Health 2021, 9. [CrossRef]
- Tan, L. (L. J.; Safadi, M. A. P.; Horn, M.; Regojo Balboa, C.; Moya, E.; Schanbaum, J.; Pimenta, P.; Lambert, E.; Soumahoro, L.; Sohn, W.-Y.; Bruce, T.; Ruiz García, Y. Pandemic’s Influence on Parents’ Attitudes and Be-haviors toward Meningococcal Vaccination. Hum Vaccin Immunother 2023, 19 (1). [CrossRef]
- Bonanni, P.; Steffen, R.; Schelling, J.; Balaisyte-Jazone, L.; Posiuniene, I.; Zatoński, M.; Van Damme, P. Vaccine Co-Administration in Adults: An Effective Way to Improve Vaccination Coverage. Hum Vaccin Immunother 2023, 19 (1). [CrossRef]
- Spencer, N.; Markham, W.; Johnson, S.; Arpin, E.; Nathawad, R.; Gunnlaugsson, G.; Homaira, N.; Rubio, M. L. M.; Trujillo, C. J. The Impact of COVID-19 Pandemic on Inequity in Routine Childhood Vaccination Cover-age: A Systematic Review. Vaccines (Basel) 2022, 10 (7), 1013. [CrossRef]
- Ning, C.; Wang, H.; Wu, J.; Chen, Q.; Pei, H.; Gao, H. The COVID-19 Vaccination and Vaccine Inequity Worldwide: An Empirical Study Based on Global Data. Int J Environ Res Public Health 2022, 19 (9), 5267. [CrossRef]
- Sabbatucci, M.; Odone, A.; Signorelli, C.; Siddu, A.; Silenzi, A.; Maraglino, F. P.; Rezza, G. Childhood Immun-isation Coverage during the COVID-19 Epidemic in Italy. Vaccines (Basel) 2022, 10 (1), 120. [CrossRef]
- Olusanya, O. A.; Bednarczyk, R. A.; Davis, R. L.; Shaban-Nejad, A. Addressing Parental Vaccine Hesitancy and Other Barriers to Childhood/Adolescent Vaccination Uptake During the Coronavirus (COVID-19) Pan-demic. Front Immunol 2021, 12. [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (Basel) 2021, 9 (2), 160. [CrossRef]
- Evans, W. D.; Bingenheimer, J. B.; Long, M.; Ndiaye, K.; Donati, D.; Rao, N. M.; Akaba, S.; Nsofor, I.; Agha, S. Outcomes of a Social Media Campaign to Promote COVID-19 Vaccination in Nigeria. PLoS One 2023, 18 (9), e0290757. [CrossRef]
- Diedrich, D., Northcote, N., Röder, T., & Sauer-Sidor, K. Strategic resilience during the COVID-19 crisis | McKinsey https://www.mckinsey.com/capabilities/strategy-and-corporate-finance/our-insights/strategic-resilience-during-the-covid-19-crisis (accessed 2023 -04 -29).
- Soorapanth, S.; Cheung, R.; Zhang, X.; Mokdad, A. H.; Mensah, G. A. Rural–Urban Differences in Vaccination and Hesitancy Rates and Trust: US COVID-19 Trends and Impact Survey on a Social Media Platform, May 2021–April 2022. Am J Public Health 2023, 113 (6), 680–688. [CrossRef]
- Olstad, D. L.; McIntyre, L. Reconceptualising Precision Public Health. BMJ Open 2019, 9 (9), e030279. [CrossRef]
- WHO and UNICEF warn of a decline in vaccinations during COVID-19 https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19 (accessed 2023 -04 -29).
- Watts, E.; Mak, J.; Patenaude, B. Benefit-Cost Ratios of Continuing Routine Immunization During the COVID-19 Pandemic in Africa. J Benefit Cost Anal 2022, 13 (1), 91–106. [CrossRef]
- de Oliveira Roque e Lima, J.; Pagotto, V.; Rocha, B. S.; Scalize, P. S.; Guimarães, R. A.; de Lima, M. D.; da Silva, L. N.; da Silva Oliveira, M. D.; Moura, W. É. A.; Teles, S. A.; Rosso, C. F. W.; Caetano, K. A. A. Low Vaccine Coverage and Factors Associated with Incomplete Childhood Immunization in Racial/Ethnic Minorities and Rural Groups, Central Brazil. Vaccines (Basel) 2023, 11 (4), 838. [CrossRef]
- Tan, N. C.; Pang, J.; Koh, E. The Impact of a Revised National Childhood Immunization Schedule on Vac-cination Defaulters. Vaccines (Basel) 2023, 11 (4), 859. [CrossRef]
- Saxena, K.; Marden, J. R.; Carias, C.; Bhatti, A.; Patterson-Lomba, O.; Gomez-Lievano, A.; Yao, L.; Chen, Y.-T. Impact of the COVID-19 Pandemic on Adolescent Vaccinations: Projected Time to Reverse Deficits in Rou-tine Adolescent Vaccination in the United States. Curr Med Res Opin 2021, 37 (12), 2077–2087. [CrossRef]
- Patel Murthy, B.; Zell, E.; Kirtland, K.; Jones-Jack, N.; Harris, L.; Sprague, C.; Schultz, J.; Le, Q.; Bramer, C. A.; Kuramoto, S.; Cheng, I.; Woinarowicz, M.; Robison, S.; McHugh, A.; Schauer, S.; Gibbs-Scharf, L. Impact of the COVID-19 Pandemic on Administration of Selected Routine Childhood and Adolescent Vaccinations — 10 US Jurisdictions, March–September 2020. MMWR Morb Mortal Wkly Rep 2021, 70 (23), 840–845. [CrossRef]
- Moraga-Llop, F. A.; Fernández-Prada, M.; Grande-Tejada, A. M.; Martínez-Alcorta, L. I.; Moreno-Pérez, D.; Pérez-Martín, J. J. Recovering Vaccine Coverage Lost Due to the COVID-19 Pandemic. Vacunas (English Edi-tion) 2020, 21 (2), 129–135. [CrossRef]
- WHO. Scale-up routine immunization along with COVID-19 vaccination: WHO https://www.who.int/southeastasia/news/detail/08-09-2021-scale-up-routine-immunization-along-with-covid-19-vaccination-who (accessed 2023 -04 -29).
- Berhane, H. Y.; Worku, A.; Fawzi, W. Effect of COVID-19 on Routine Childhood Vaccination in Bahir Dar City, Northwestern, Ethiopia. Vaccines (Basel) 2023, 11 (10), 1569. [CrossRef]
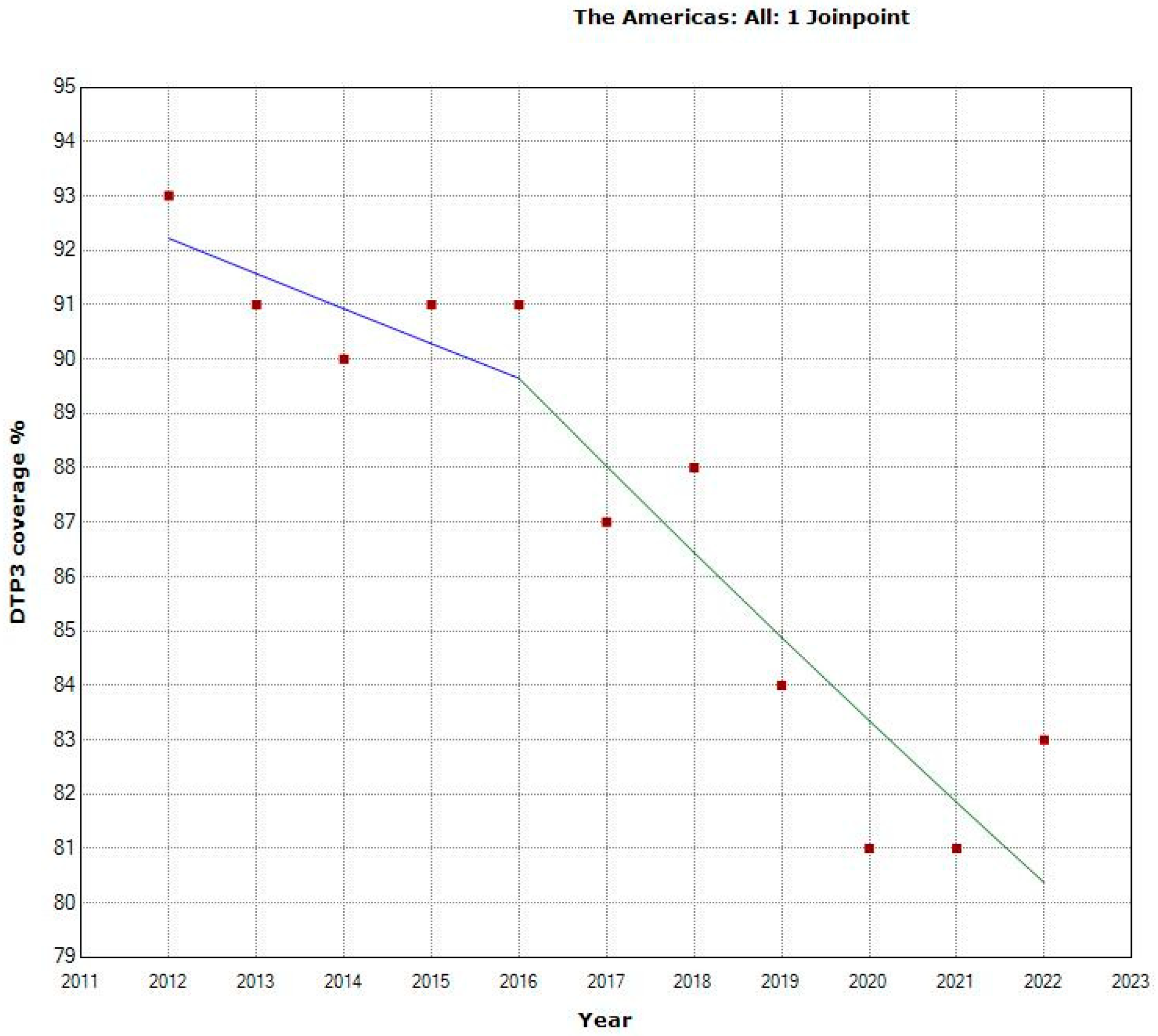



| Periods | Years | APC (95% CI) | P |
|---|---|---|---|
| Total Period | 2012-2021 | -1.4 (-1.8.; -1.0) | < 0.001 |
| Period 1 | 2012-2016 | -0.7 (-2.9; 1.5) | 0.464 |
| Period 2 | 2016-2022 | -1.8 (-2.9; -0.7) | 0.008 |
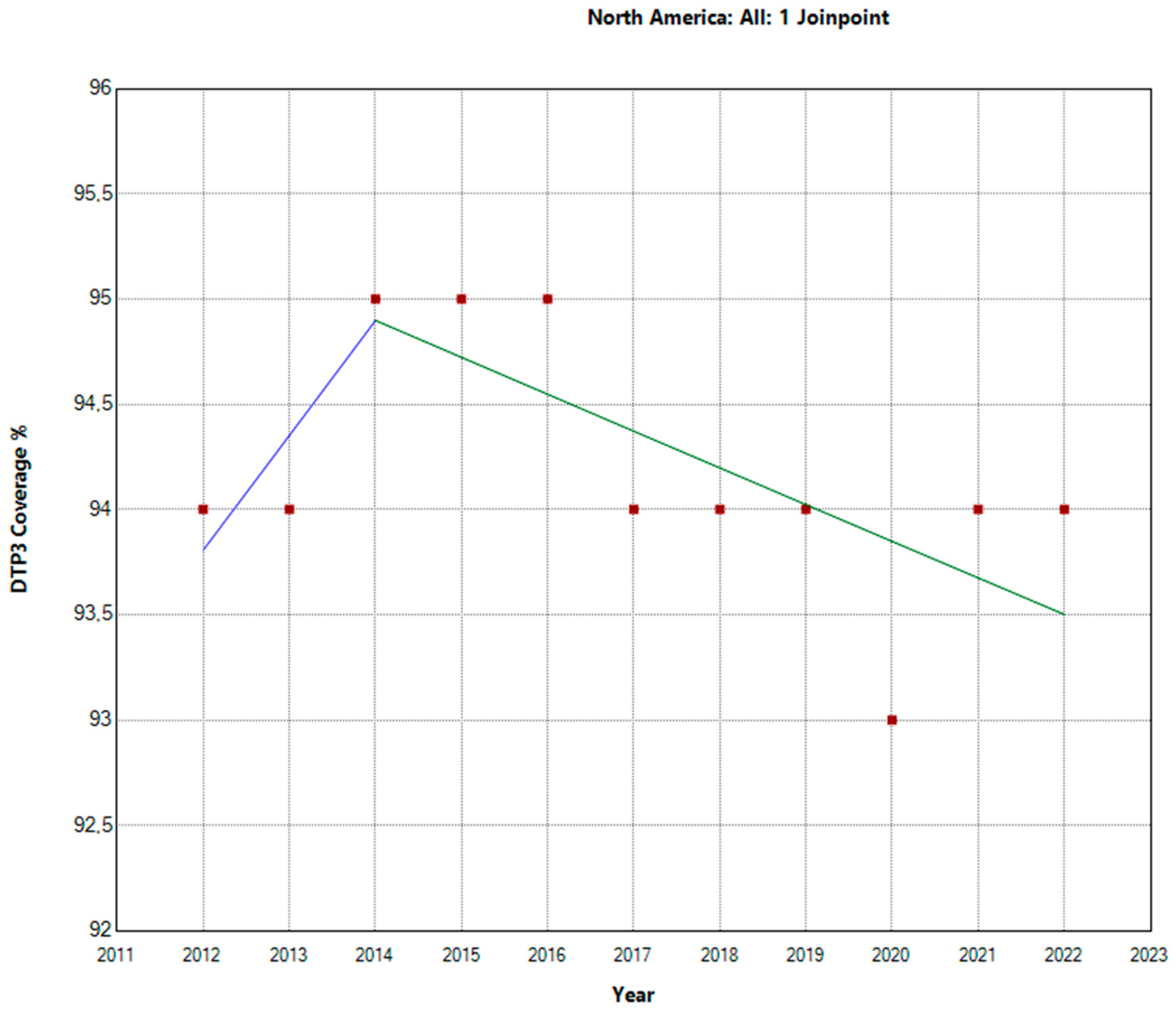
| Periods | Years | APC | 95% LCI | 95% UCI | P |
|---|---|---|---|---|---|
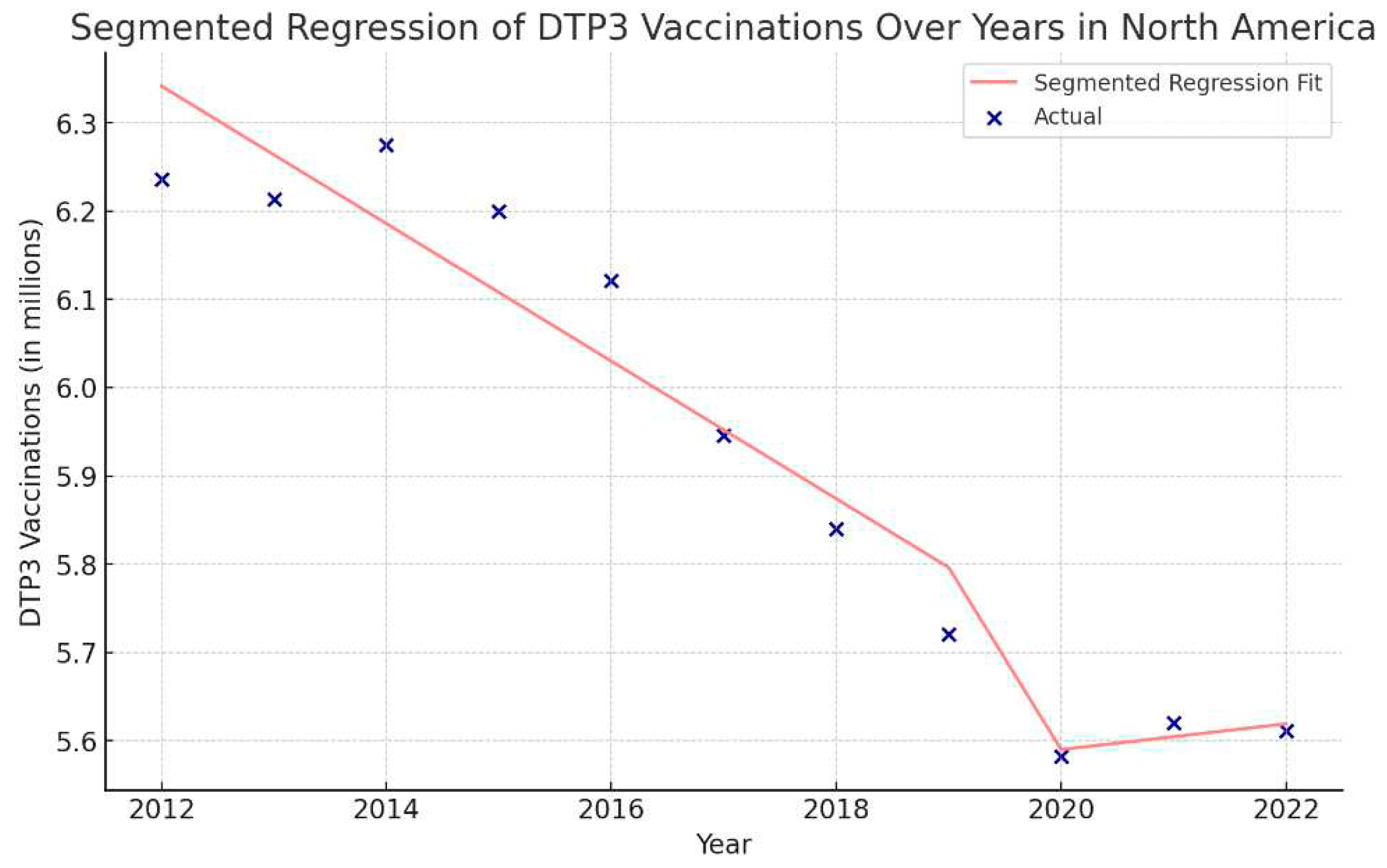
| North America | |||||
| Total Period | 2012-2022 | -0.1 | 0.2 | 0 | 0.136 |
| Period 1 | 2012-2014 | 0.6 | -0.2 | 1.4 | 0.494 |
| Period 2 | 2014-2022 | -0.2 | -0.9 | 0.1 | 0.057 |
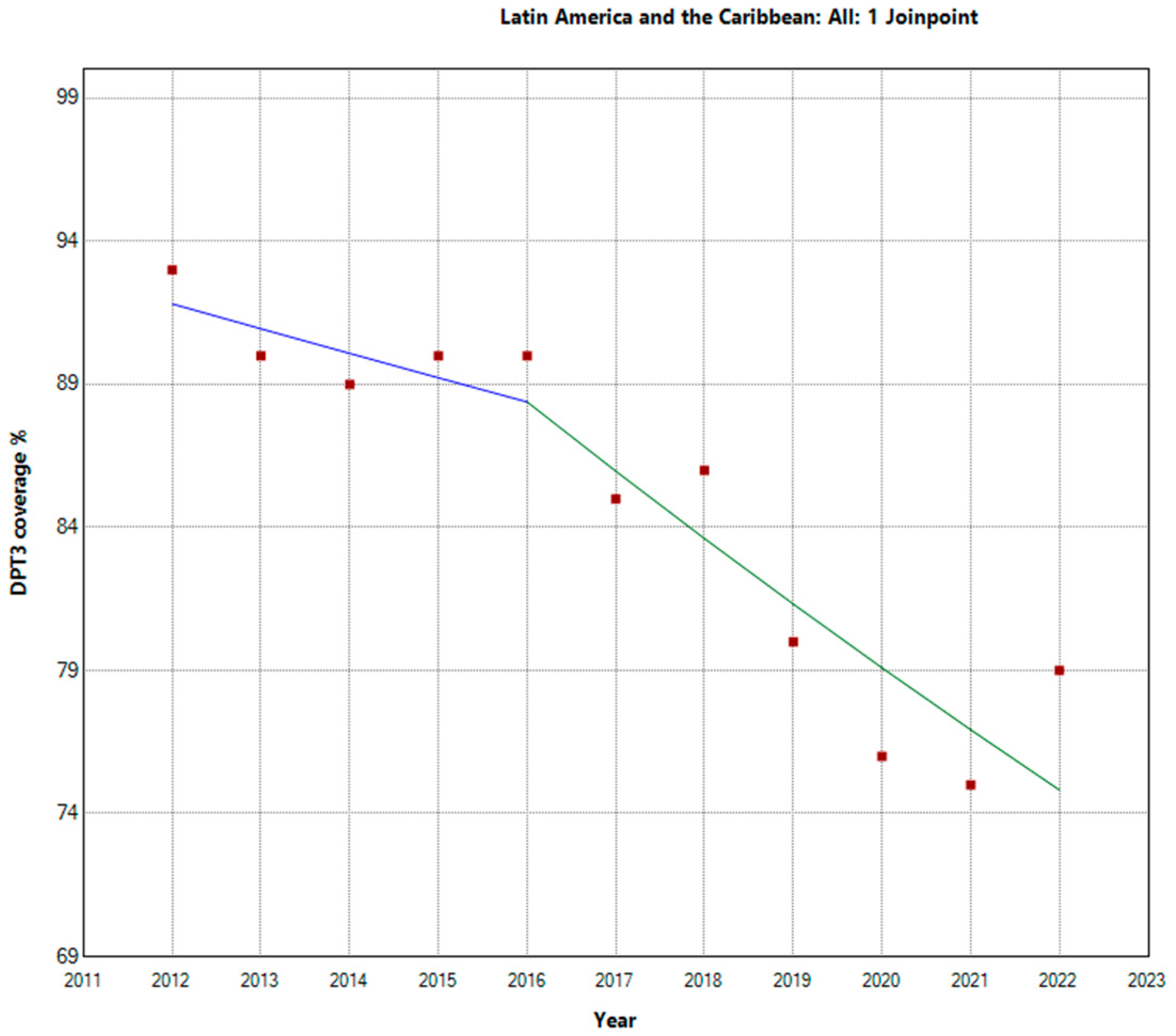
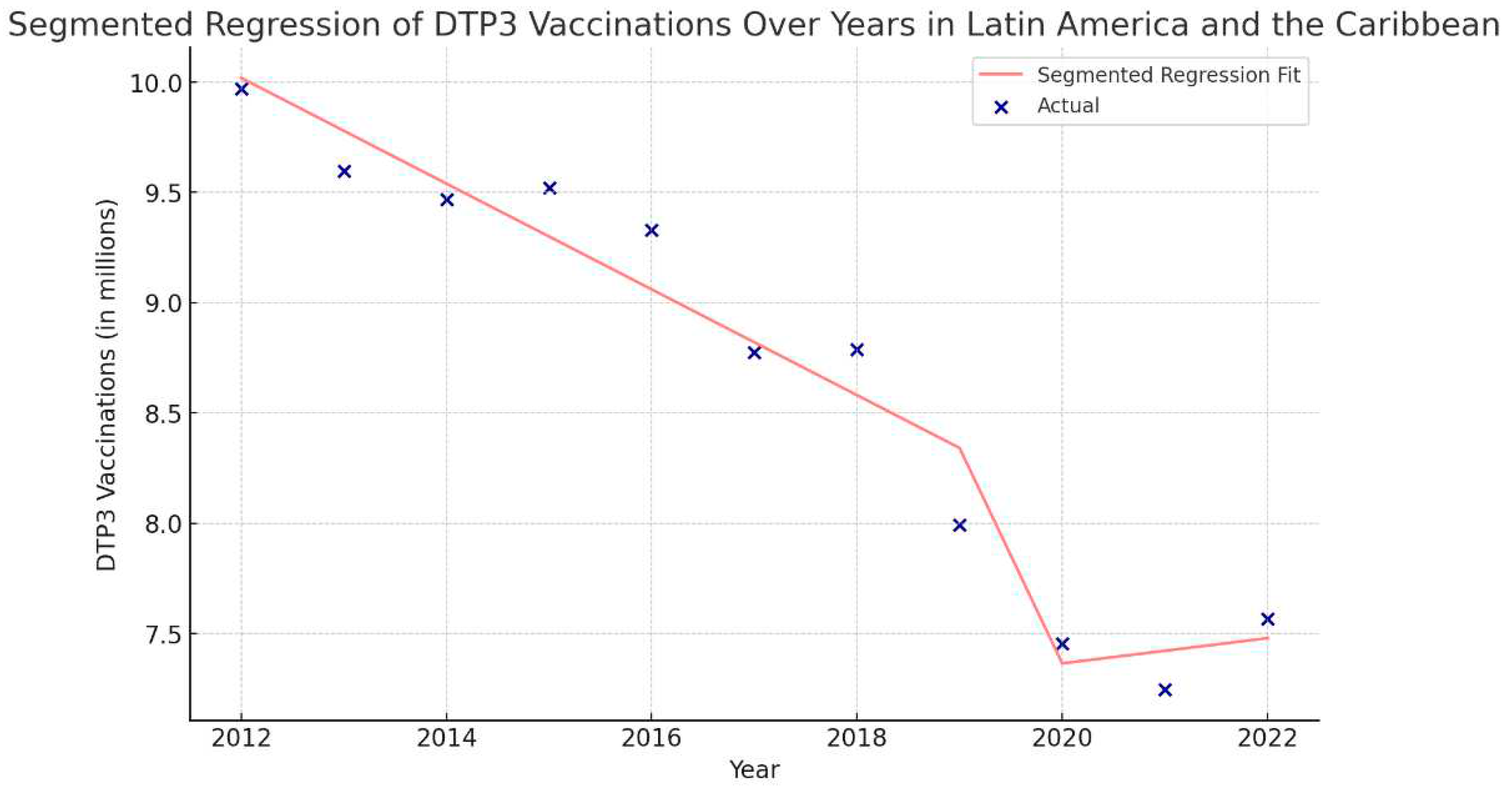
| Latin America and the Caribbean | |||||
| Total Period | 2012-2022 | -2.1 | -2.7 | -1.5 | < 0.001 |
| Period 1 | 2012-2016 | -0.9 | -4.4 | 2.6 | 0.531 |
| Period 2 | 2016-2022 | -2.7 | -4.5 | -0.9 | 0.010 |
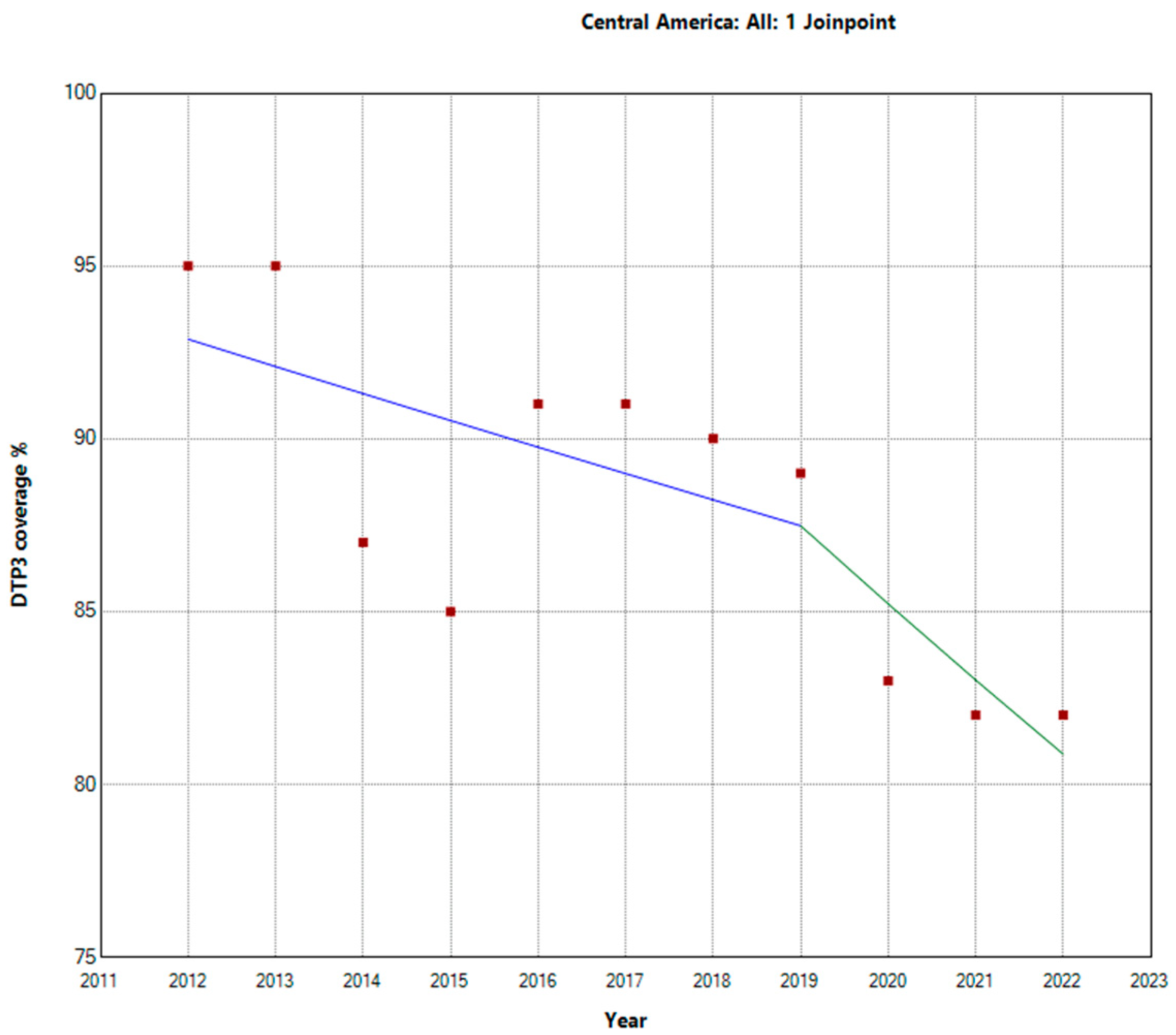
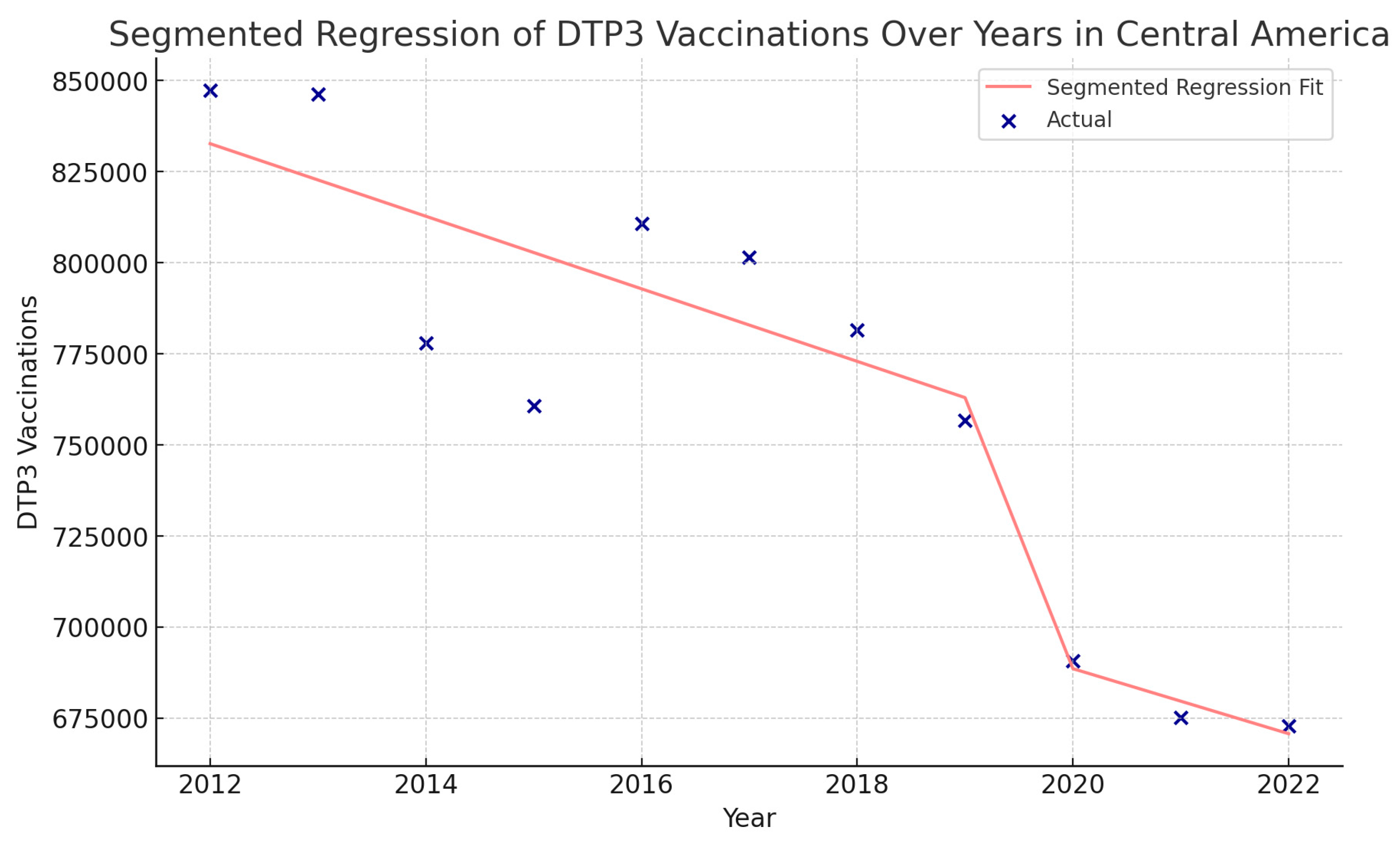
| Central America | |||||
| Total Period | 2012-2022 | -1.3 | -2.1 | -0.4 | 0.009 |
| Period 1 | 2012-2019 | -0.9 | -2.8 | 1.1 | 0.321 |
| Period 2 | 2019-2022 | -2.6 | -8.6 | 3.8 | 0.354 |
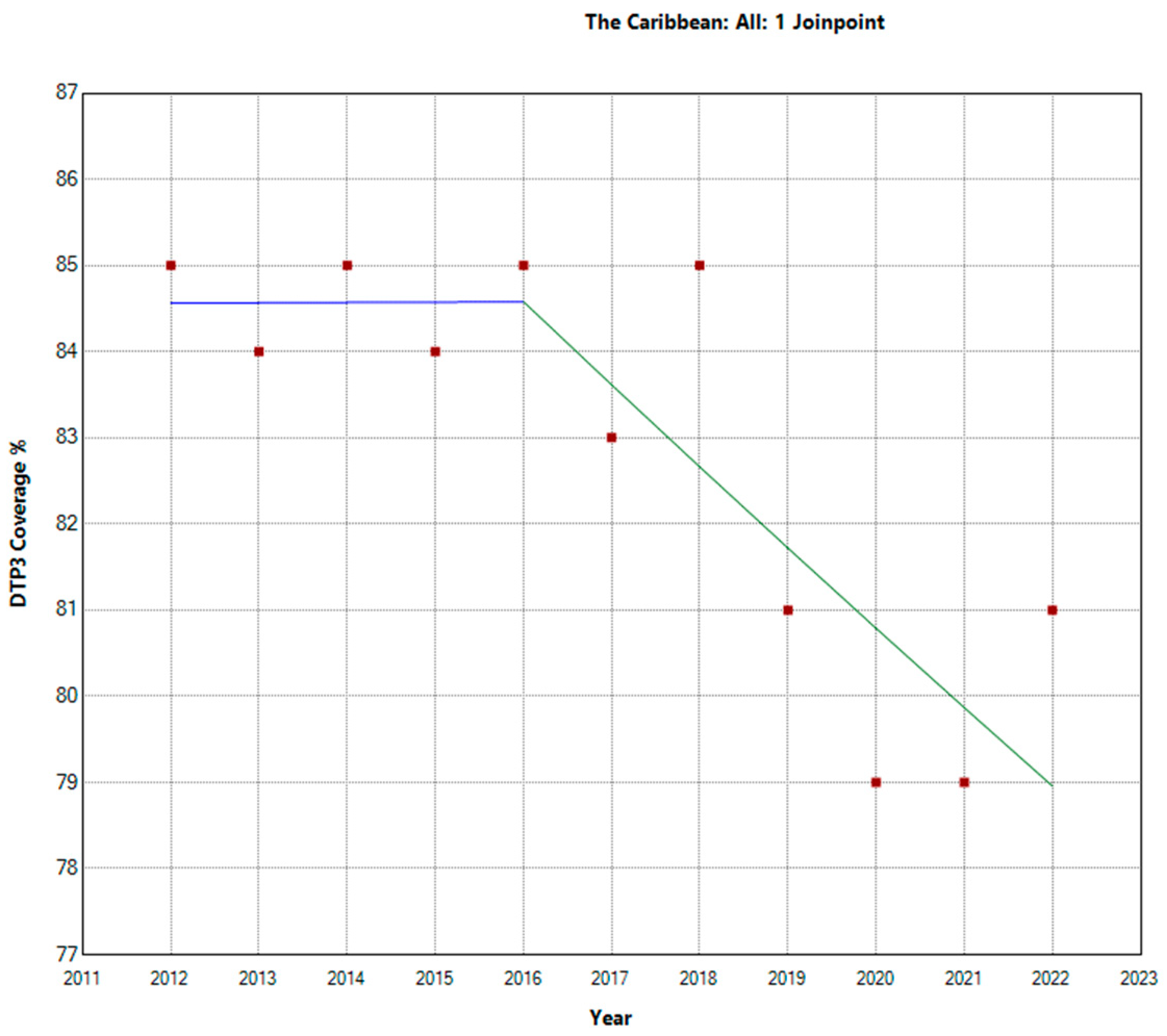
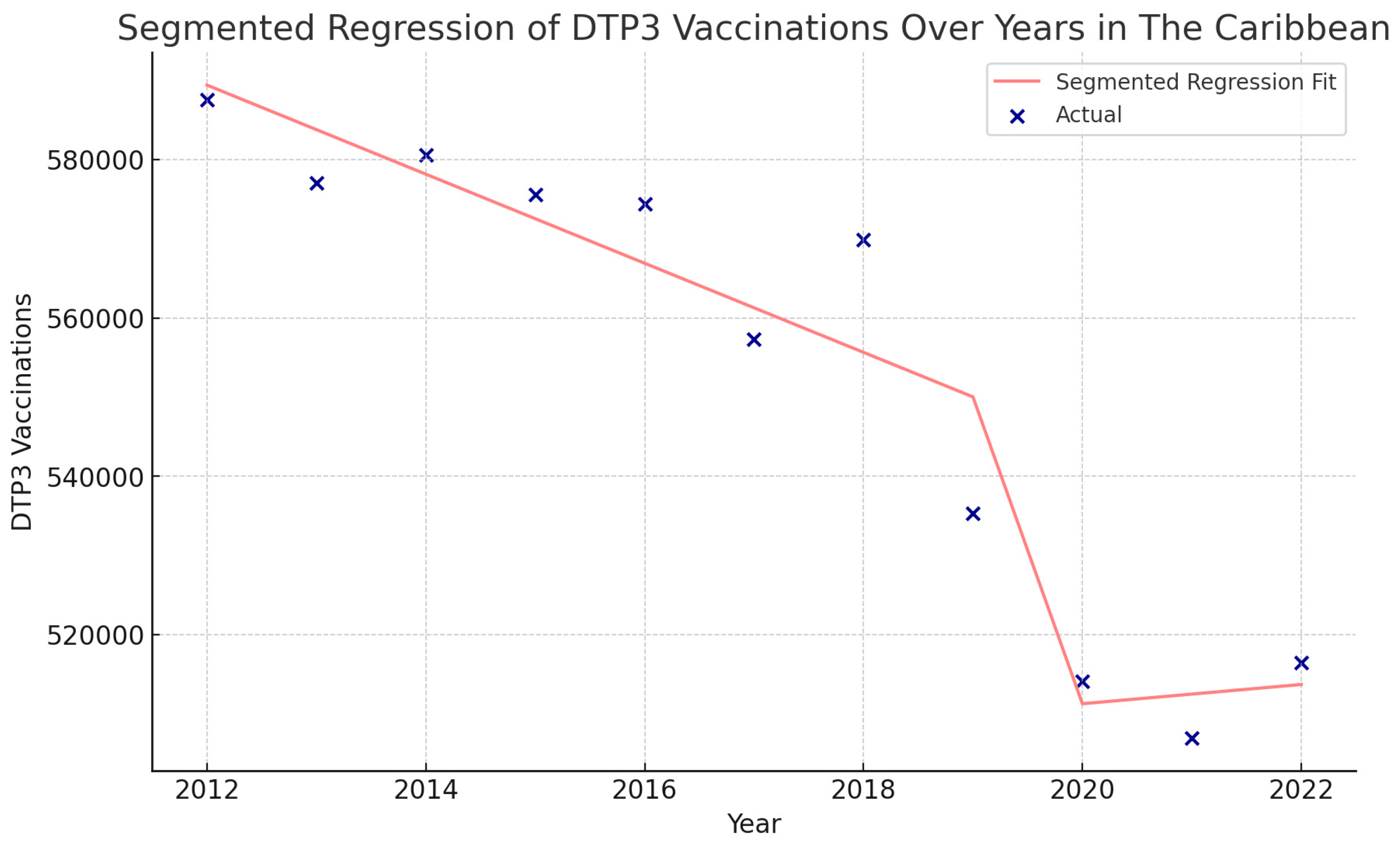
| Caribbean | |||||
| Total Period | 2012-2022 | -0.7 | -1.1 | -0.4 | 0.001 |
| Period 1 | 2012-2016 | 0.0 | -1.9 | 2.0 | 0.996 |
| Period 2 | 2016-2022 | -1.1 | -2.1 | -0.1 | 0.031 |
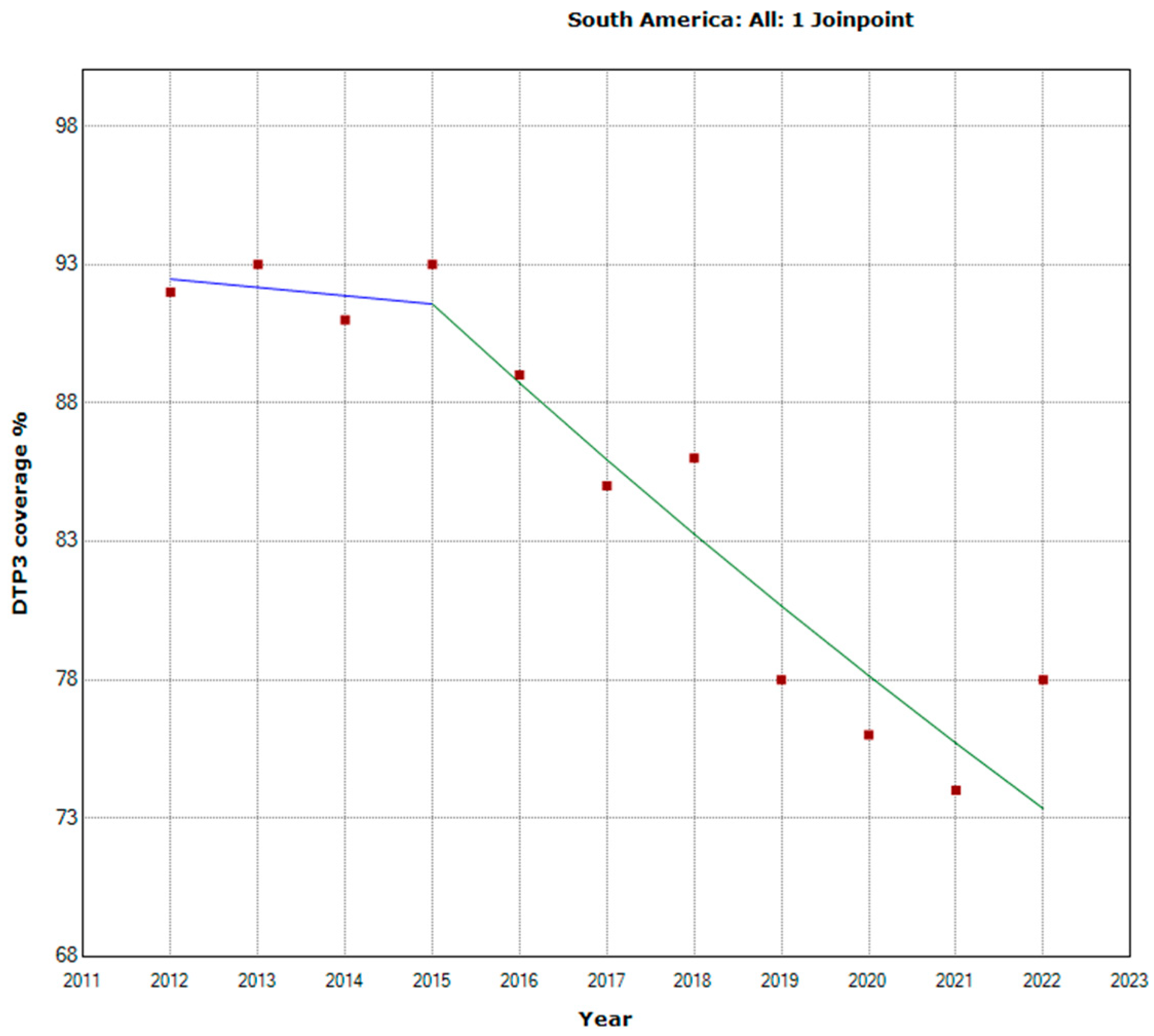
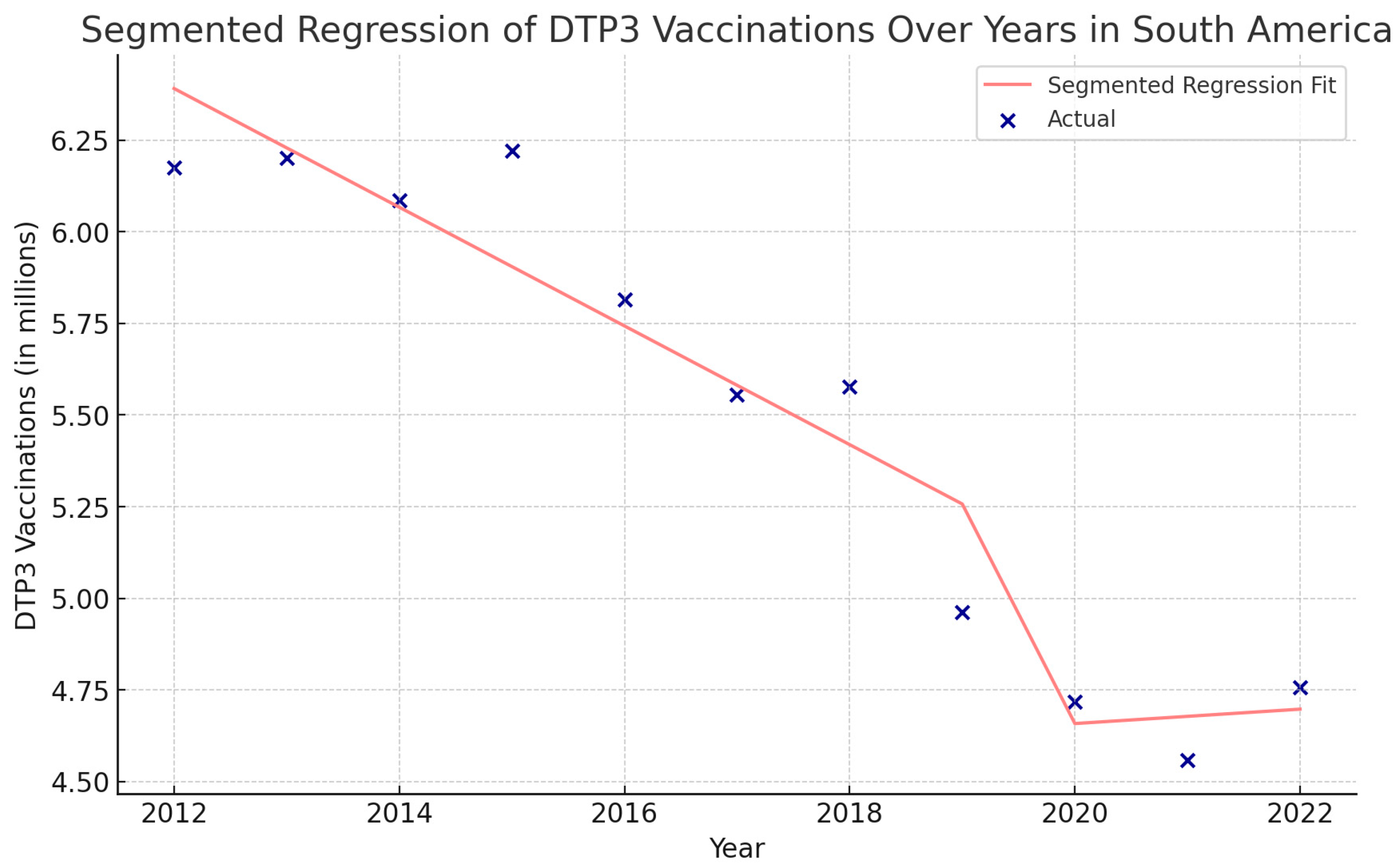
| South America | |||||
| Total Period | 2012-2022 | -2.5 | -3.1 | -1.8 | < 0.001 |
| Period 1 | 2012-2015 | -0.3 | -5.9 | 5.6 | 0.895 |
| Period 2 | 2015-2022 | -3.1 | -4.4 | -1.8 | 0.001 |
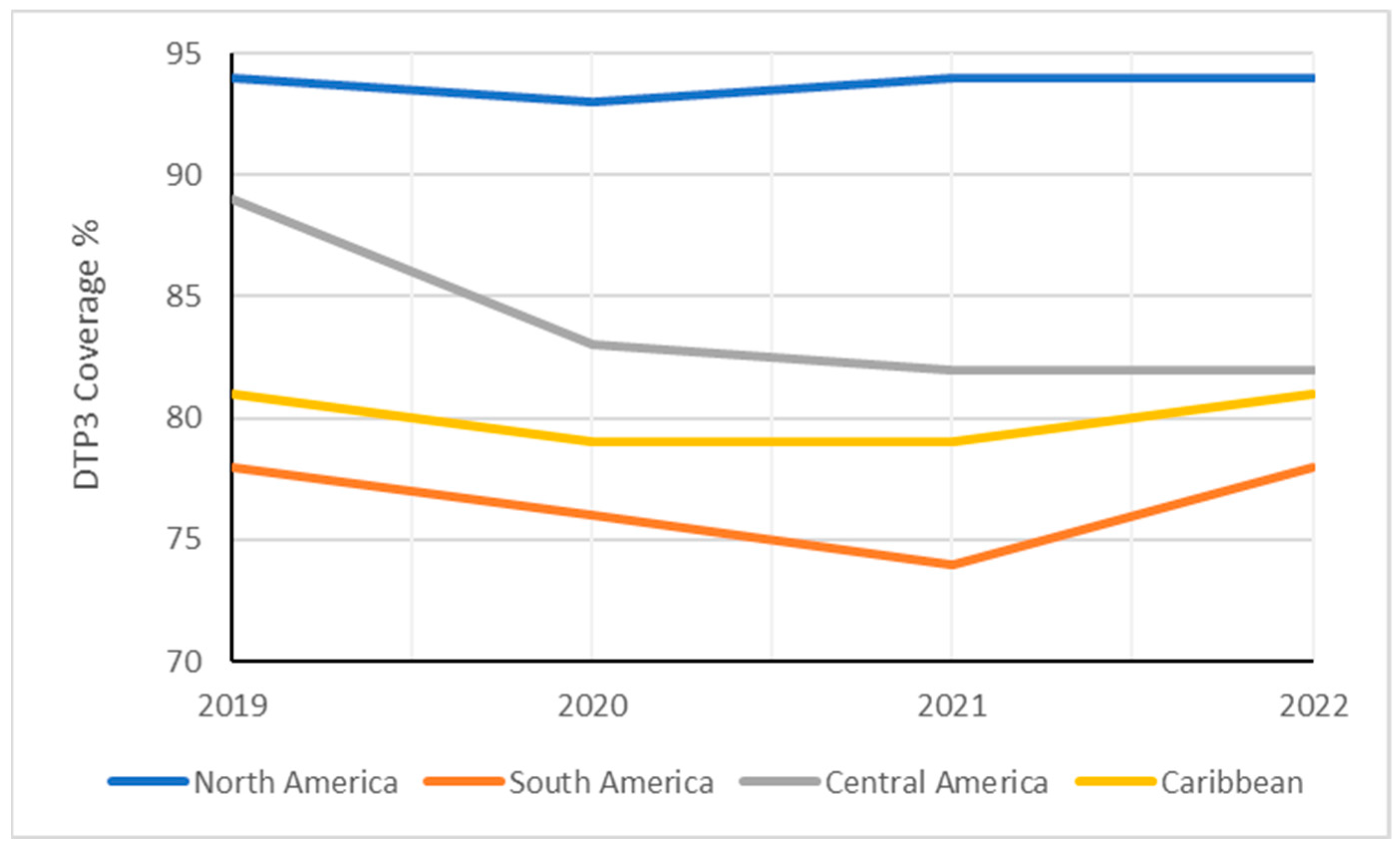
| Region | 2019 | 2020 | 2021 | 2022 | Absolute Changes 2019–2022 |
Relative Changes 2019–2022 |
|---|---|---|---|---|---|---|
| Americas | 84 | 81 | 81 | 83 | -1% | -1,19% |
| North America | 94 | 93 | 94 | 94 | 0% | 0,00% |
| Latin America and the Caribbean | 80 | 76 | 75 | 79 | -1% | -1,25% |
| South America | 78 | 76 | 74 | 78 | 0% | 0,00% |
| Central America | 89 | 83 | 82 | 82 | -7% | -7,87% |
| Caribbean | 81 | 79 | 79 | 81 | 0% | 0,00% |
| 2019 | 2022 | ||||
|---|---|---|---|---|---|
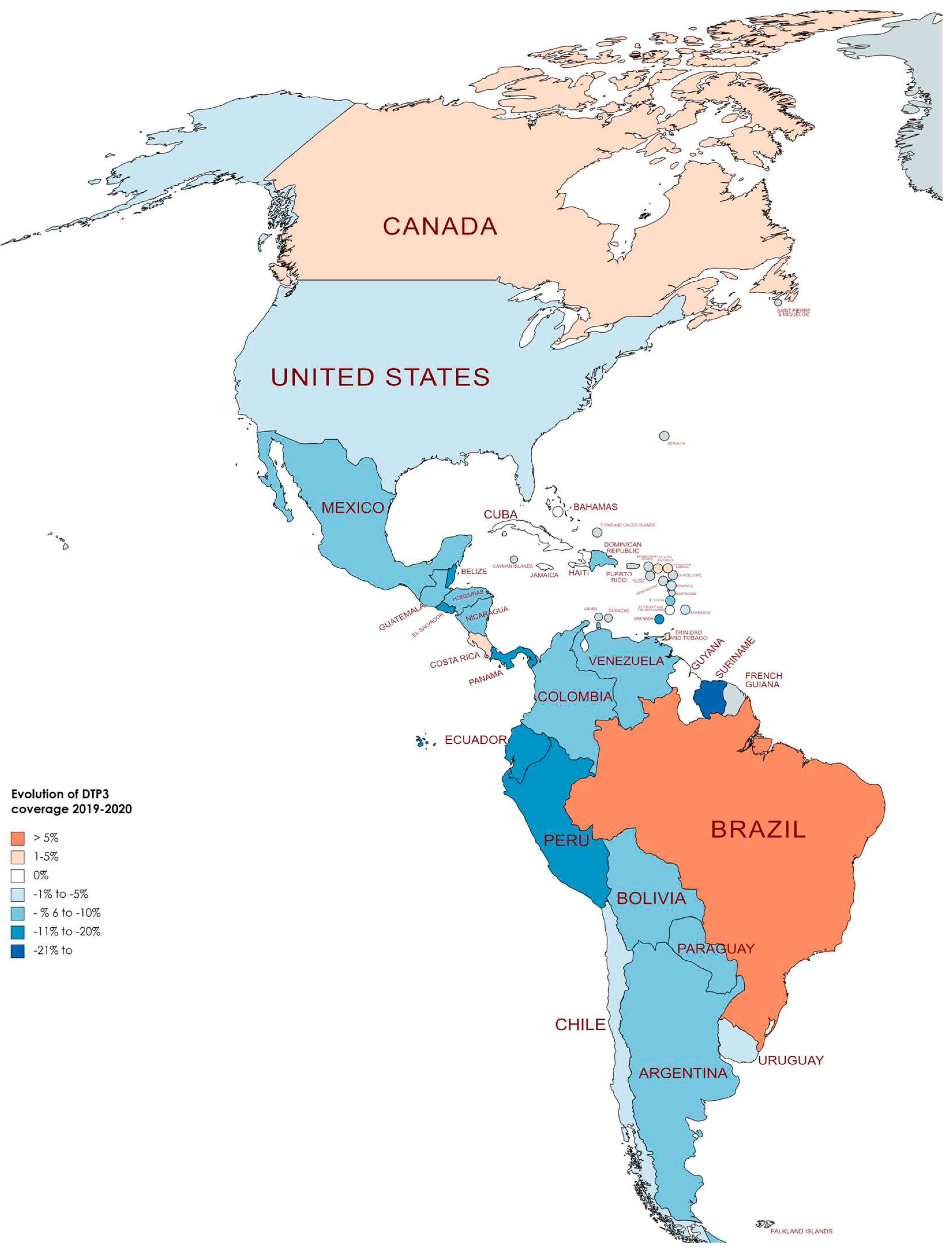
| Country | DTP3 (%) | Births (n) | DTP3 (%) | Births (n) | p † |
| Antigua and Barbuda | 95 | 1058 | 99 | 1124 | <0.001 |
| Argentina | 83 | 661385 | 81 | 627741 | <0.001 |
| Bahamas | 89 | 4641 | 87 | 4659 | ns |
| Barbados | 90 | 3050 | 86 | 3037 | ns |
| Belize | 98 | 7333 | 84 | 7193 | 0.003 |
| Bolivia | 75 | 263006 | 69 | 264070 | <0.001 |
| Brazil | 70 | 2886359 | 77 | 2723266 | <0.001 |
| Canada | 91 | 363393 | 92 | 376188 | ns |
| Chile | 96 | 224350 | 96 | 230824 | ns |
| Colombia | 94 | 733940 | 87 | 723264 | <0.001 |
| Costa Rica | 95 | 65282 | 95 | 60517 | ns |
| Cuba | 99 | 110404 | 99 | 99693 | ns |
| Dominica | 99 | 946 | 92 | 966 | ns |
| Dominican Republic | 89 | 210196 | 88 | 203625 | ns |
| Ecuador | 85 | 300075 | 70 | 298666 | <0.001 |
| El Salvador | 90 | 103547 | 75 | 100313 | <0.001 |
| Grenada | 94 | 2041 | 77 | 1960 | 0.054 |
| Guatemala | 85 | 391582 | 79 | 372335 | <0.001 |
| Guyana | 99 | 16898 | 98 | 16129 | ns |
| Haiti | 51 | 271669 | 51 | 268523 | ns |
| Honduras | 88 | 215469 | 78 | 217590 | <0.001 |
| Jamaica | 96 | 33815 | 98 | 32663 | ns |
| Mexico | 82 | 1965139 | 83 | 1866399 | <0.001 |
| Nicaragua | 98 | 142181 | 92 | 139164 | <0.001 |
| Panama | 88 | 77044 | 87 | 76637 | ns |
| Paraguay | 86 | 139138 | 69 | 137960 | <0.001 |
| Peru | 88 | 591025 | 82 | 592156 | <0.001 |
| Saint Kitts and Nevis | 97 | 607 | 96 | 563 | ns |
| Saint Lucia | 92 | 2113 | 81 | 2035 | ns |
| Saint Vincent and the Grenadines | 97 | 1405 | 92 | 1324 | ns |
| Suriname | 77 | 11049 | 77 | 11123 | ns |
| Trinidad and Tobago | 93 | 18904 | 93 | 17429 | ns |
| Uruguay | 94 | 3756830 | 94 | 3726867 | ns |
| United States | 94 | 37107 | 94 | 35668 | ns |
| Venezuela | 64 | 497361 | 56 | 438384 | <0.001 |
| Country | Years | APC | 95% LCI | 95% UCI | P |
|---|---|---|---|---|---|
| Antigua and Barbuda | |||||
| Total Period | 2012-2022 | -0.4 | -0.9 | 0 | 0.04 |
| Period 1 | 2012-2017 | -1.2 | -2.7 | 0.4 | 0.118 |
| Period 2 | 2017-2022 | 0.3 | -1.3 | 1.9 | 0.677 |
| Bahamas | |||||
| Total Period | 2012-2022 | -1.5 | -2 | -0.9 | < 0.001 |
| Period 1 | 2012-2020 | -1.8 | -2.2 | -1.4 | < 0.001 |
| Period 2 | 2020-2022 | 0.6 | -2.7 | 3.9 | 0.697 |
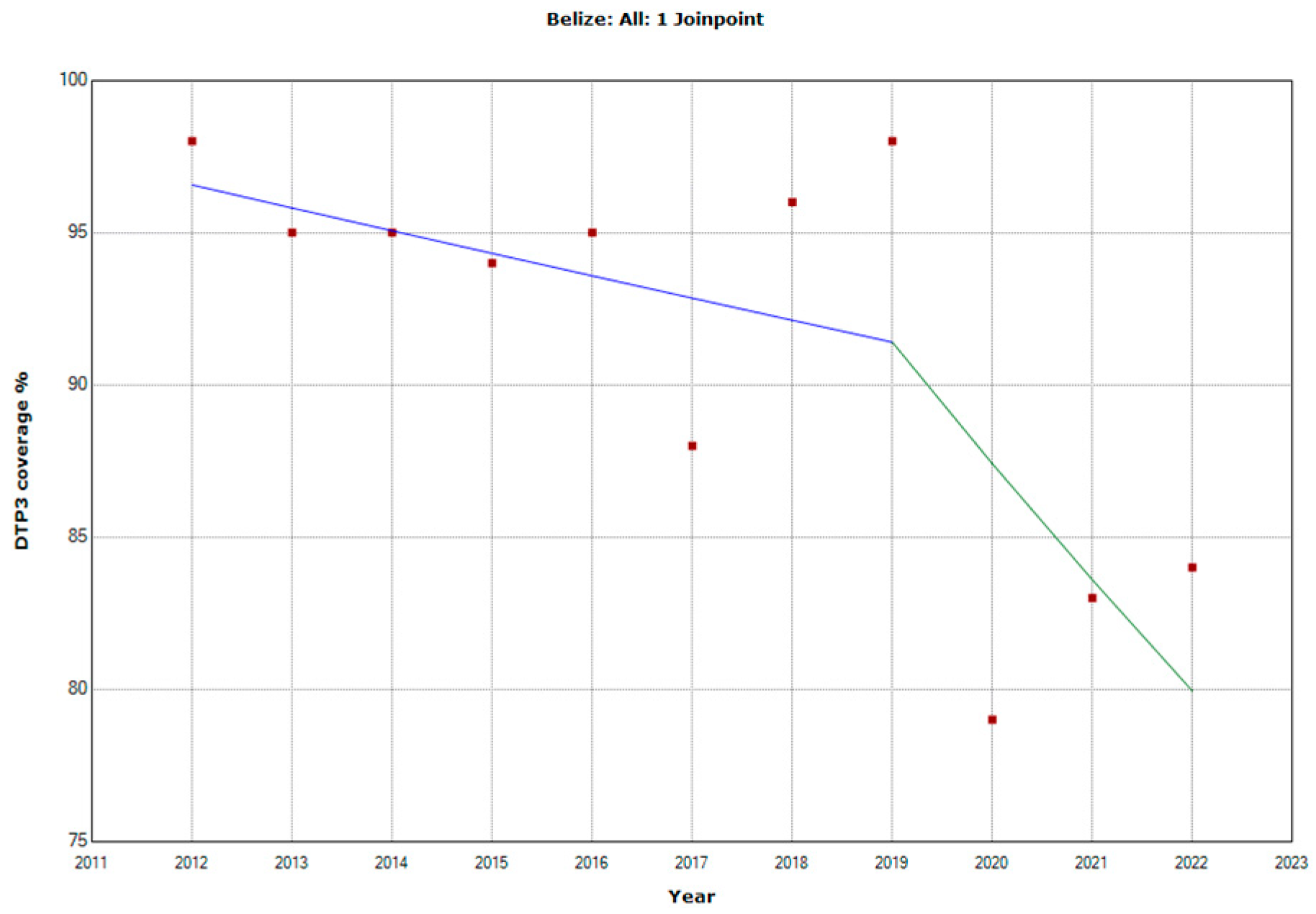
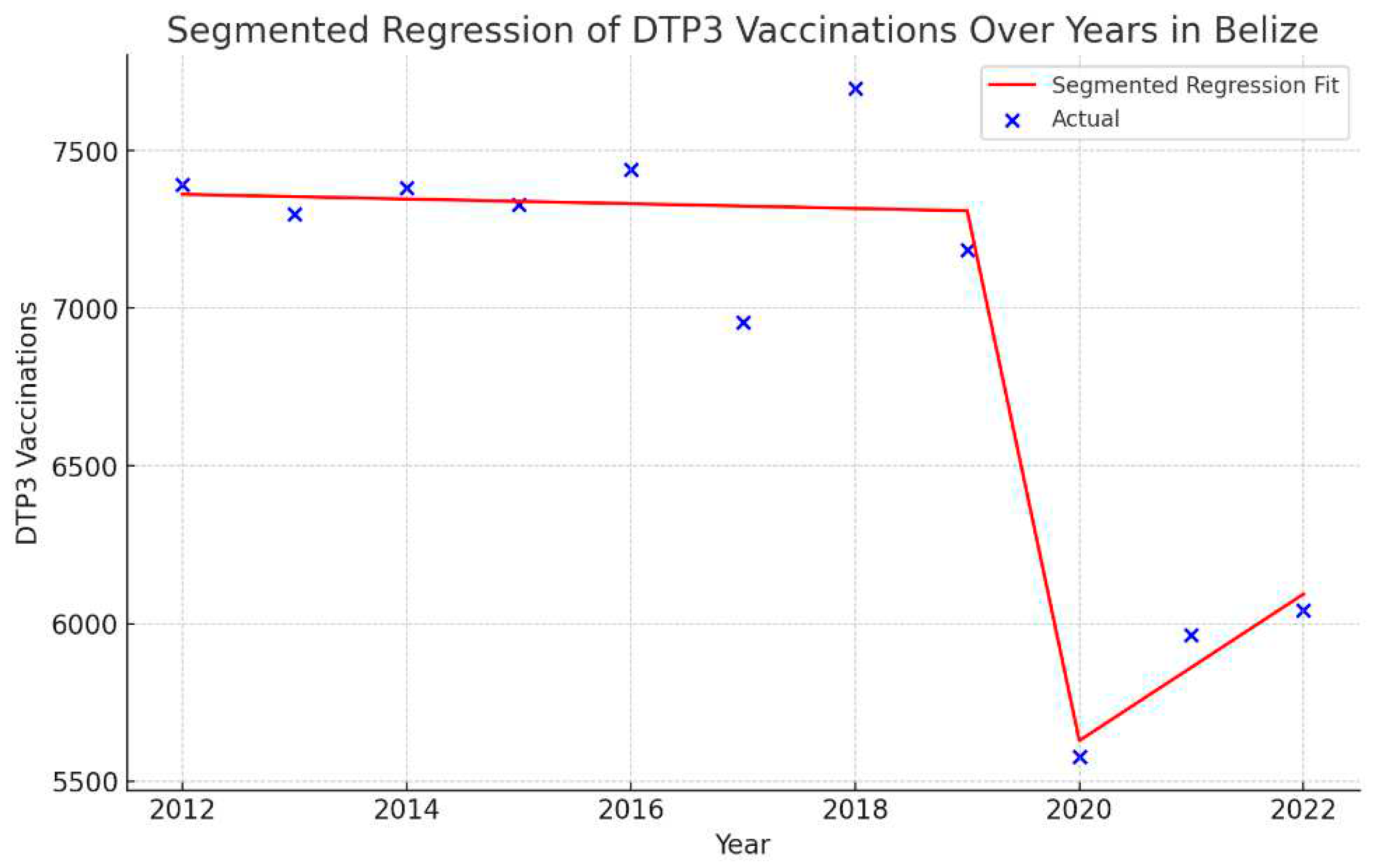
| Belize | |||||
| Total Period | 2012-2022 | -1.6 | -2.6 | -0.6 | 0.005 |
| Period 1 | 2012-2019 | -0.8 | -1.7 | 0.2 | 0.09 |
| Period 2 | 2019-2022 | -4.4 | -8.3 | -0.3 | 0.04 |
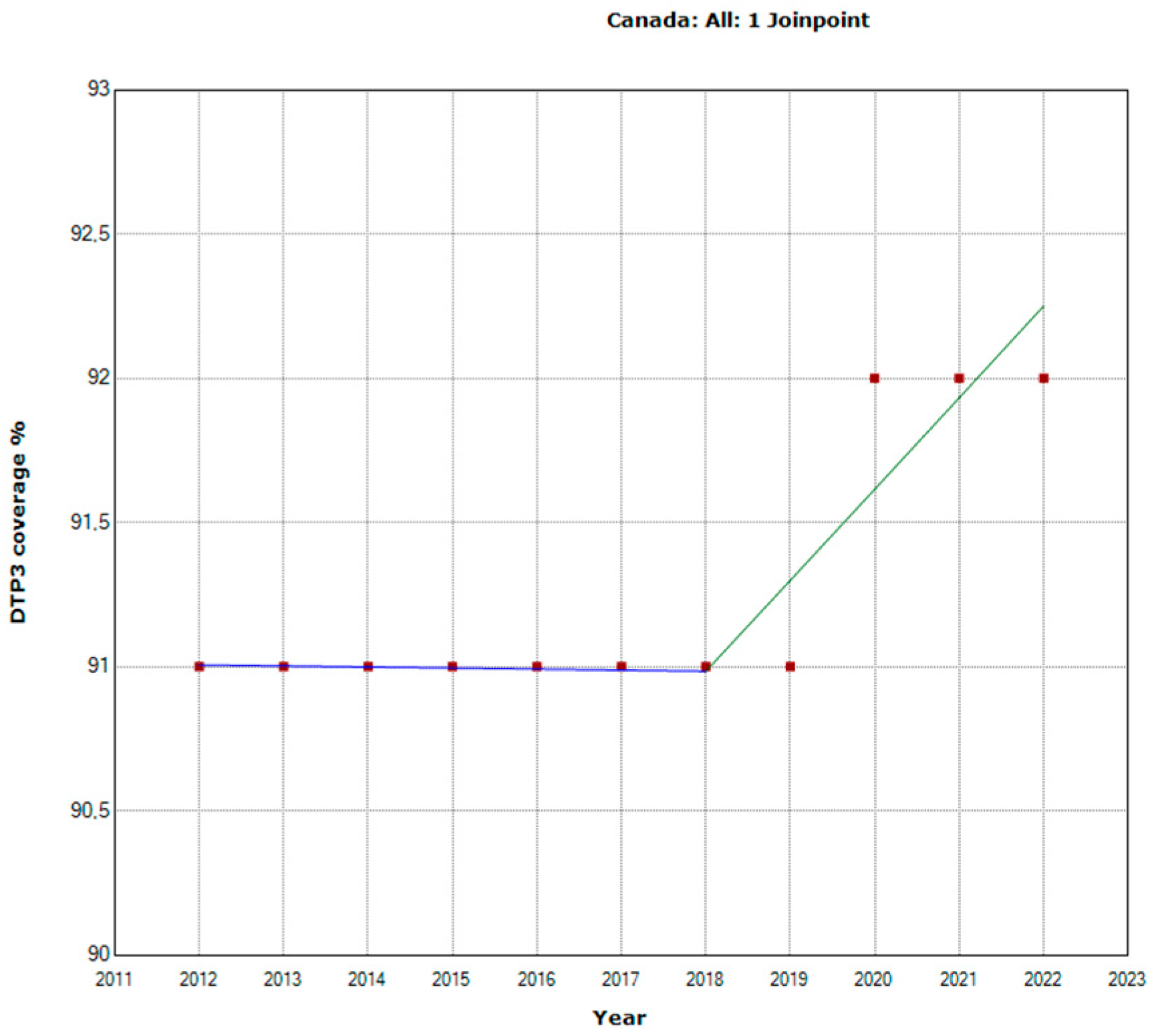
| Canada | |||||
| Total Period | 2012-2022 | 0.1 | 0.1 | 0.2 | 0.003 |
| Period 1 | 2012-2018 | 0 | -0.1 | 0.1 | 0.931 |
| Period 2 | 2018-2022 | 0.3 | 0.1 | 0.6 | 0.008 |
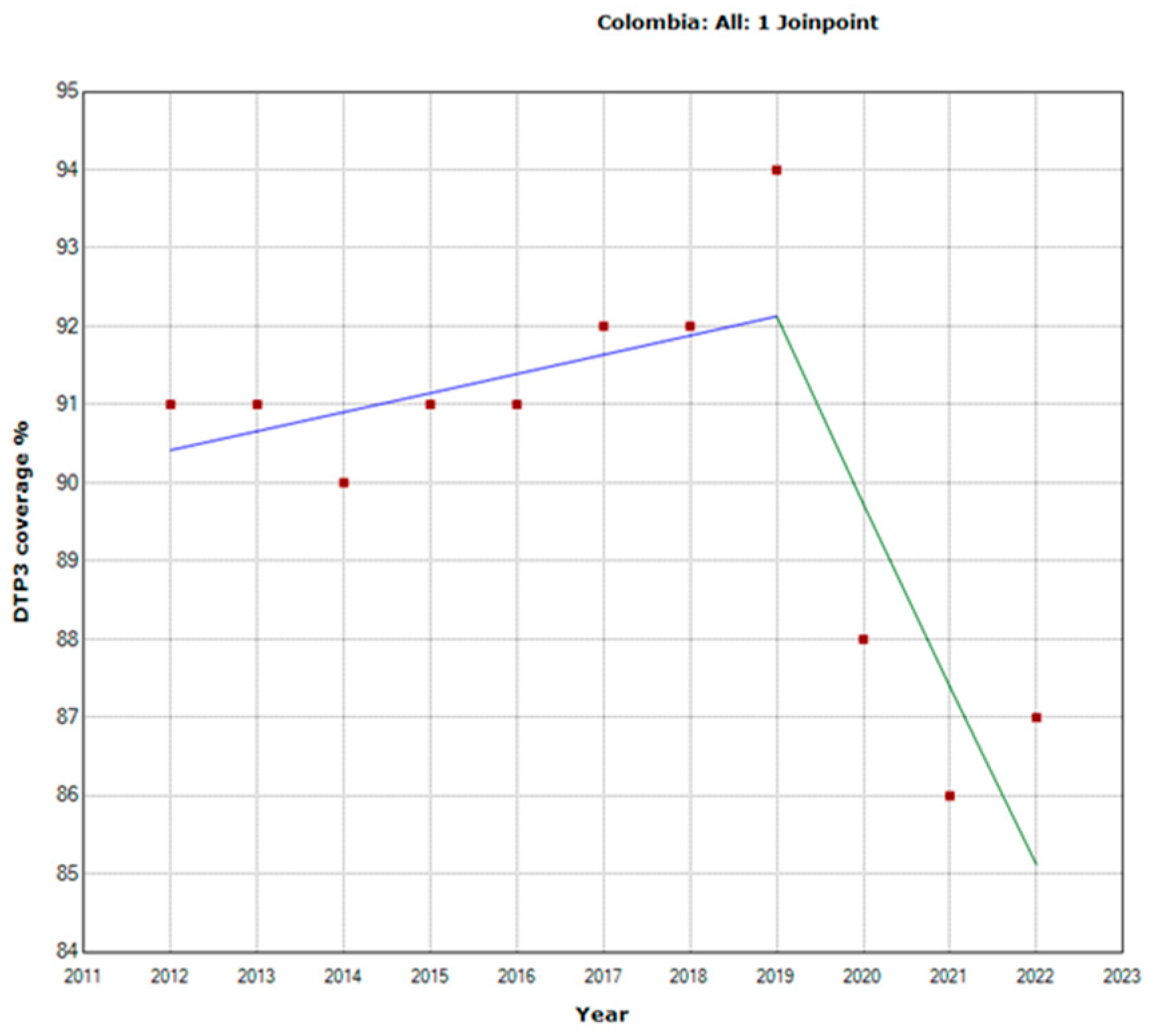
| Colombia | |||||
| Total Period | 2012-2022 | -0.4 | -0.9 | 0.1 | 0.102 |
| Period 1 | 2012-2019 | 0.3 | 0 | 0.6 | 0.071 |
| Period 2 | 2019-2022 | -2.6 | -3.8 | -1.4 | 0.002 |
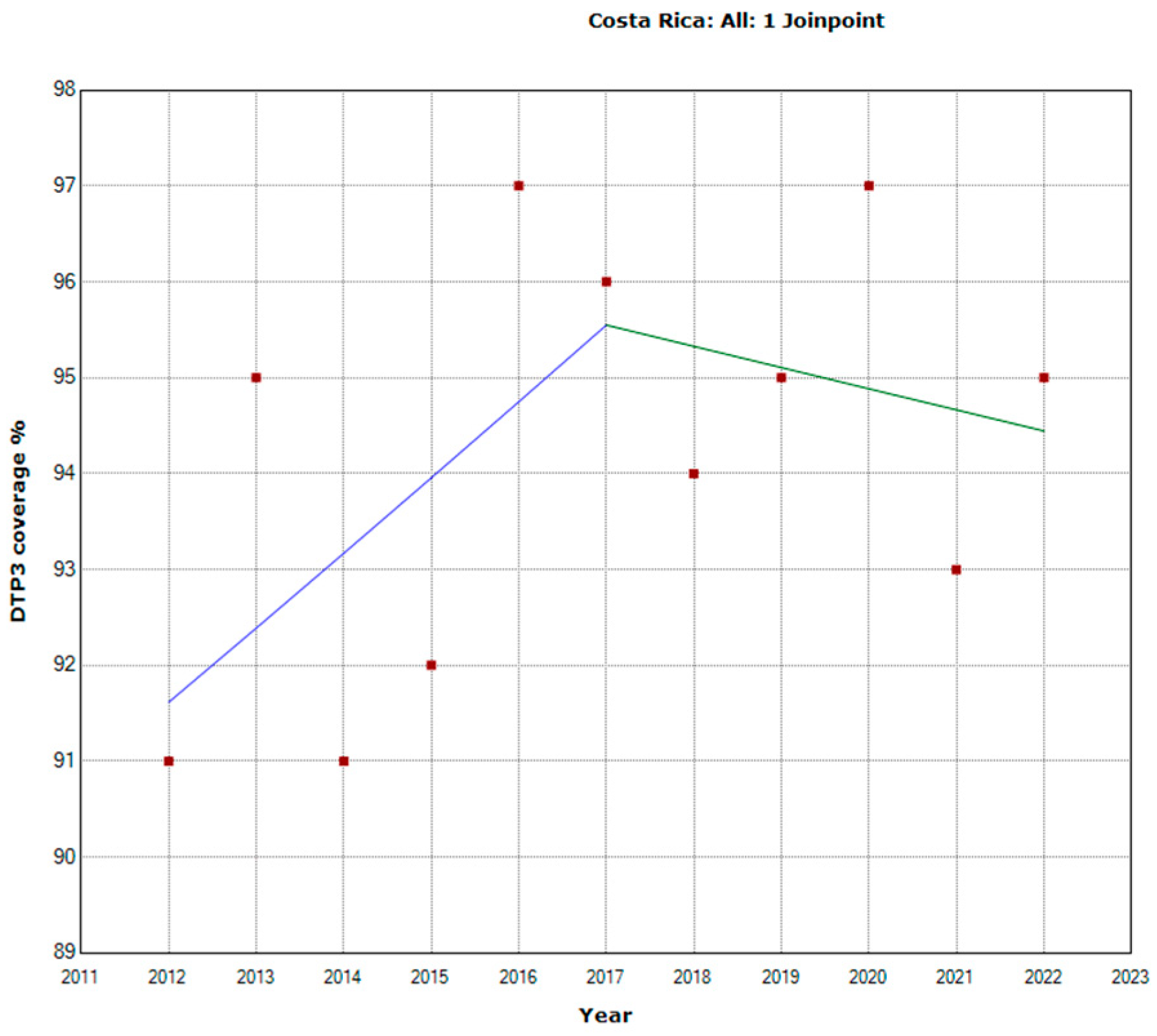
| Costa Rica | |||||
| Total Period | 2012-2022 | -0.4 | -0.9 | 0.1 | 0.102 |
| Period 1 | 2012-2017 | 0.8 | -0.6 | 2.3 | 0.198 |
| Period 2 | 2017-2022 | -0.2 | -1.6 | 1.2 | 0.702 |
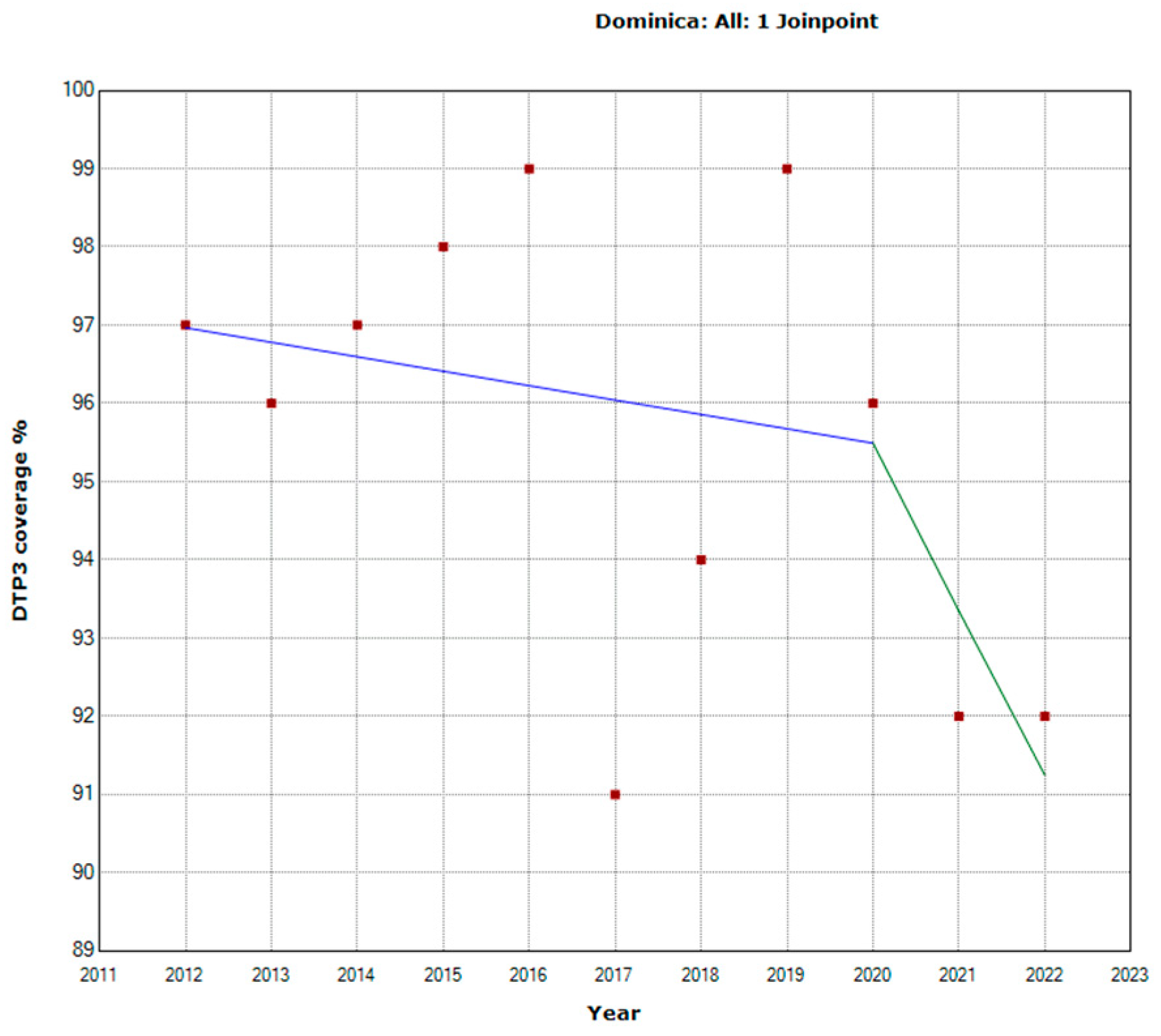
| Dominica | |||||
| Total Period | 2012-2022 | -0.4 | -1 | 0.1 | 0.101 |
| Period 1 | 2012-2020 | -0.2 | -1.3 | 0.9 | 0.677 |
| Period 2 | 2020-2022 | -2.2 | -12.5 | 9.3 | 0.635 |
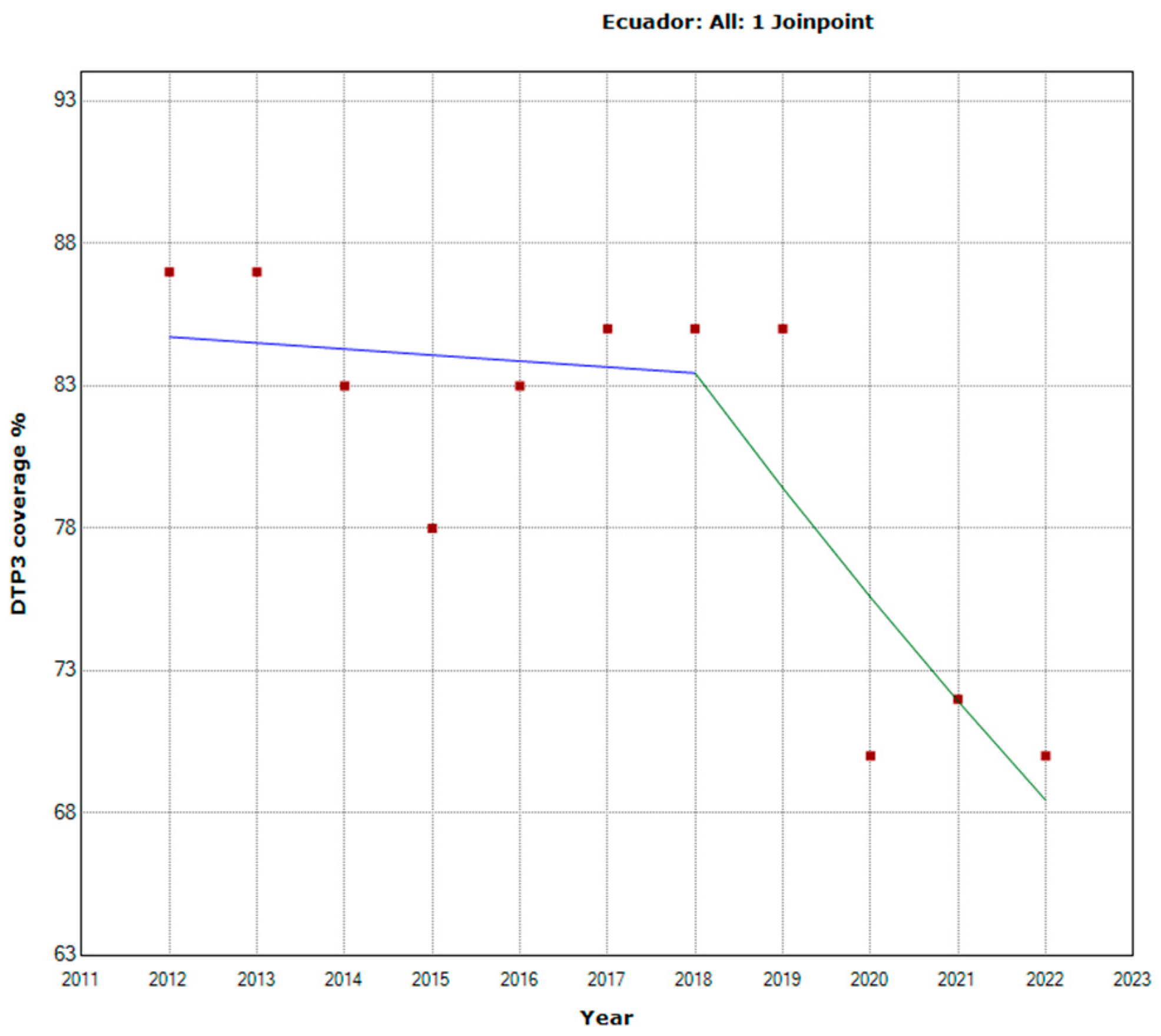
| Ecuador | |||||
| Total Period | 2012-2022 | -1.9 | -3.2 | -0.7 | 0.007 |
| Period 1 | 2012-2018 | -0.3 | -3.2 | 2.8 | 0.843 |
| Period 2 | 2018-2022 | -4.8 | -10.1 | 0.8 | 0.078 |
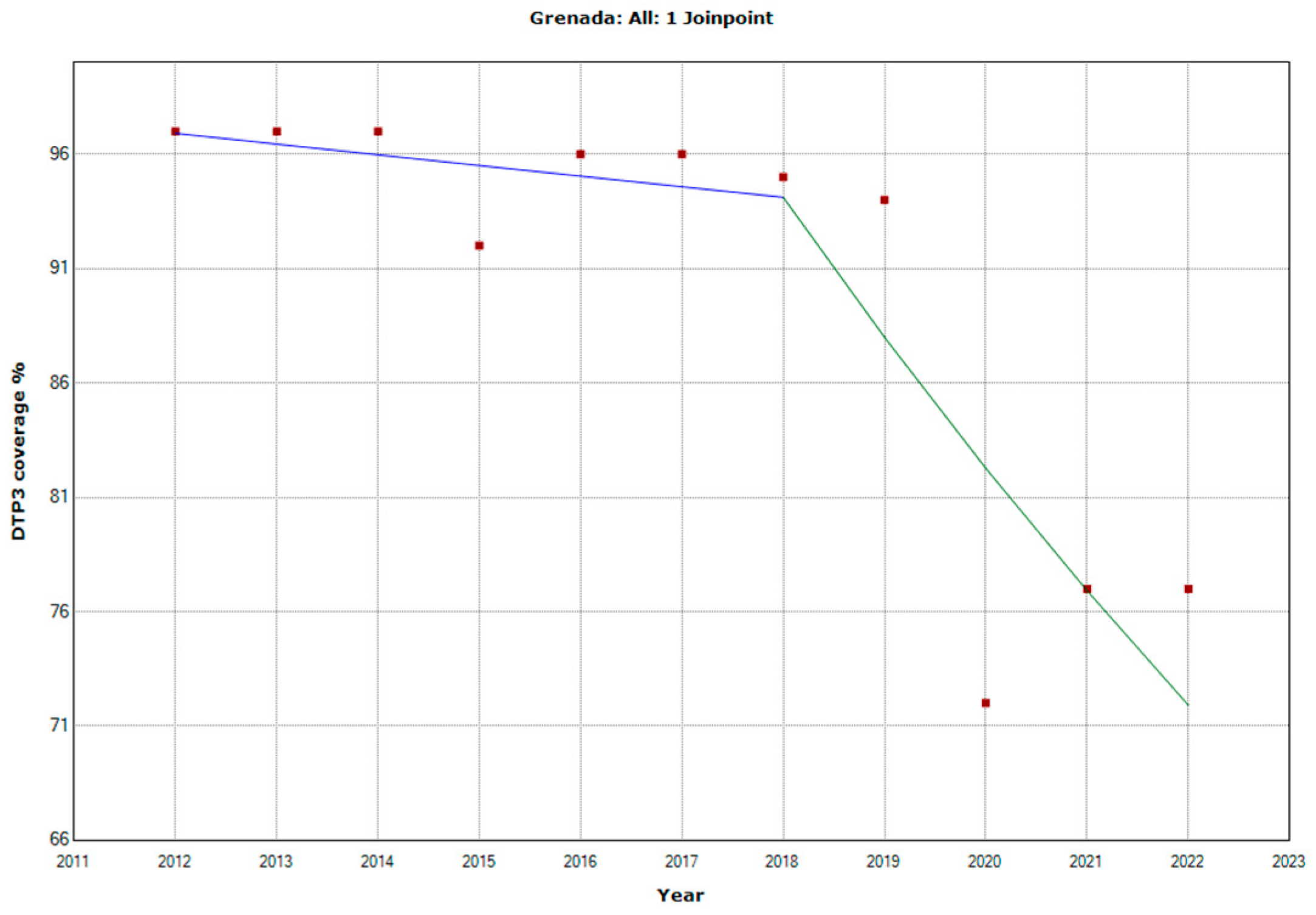
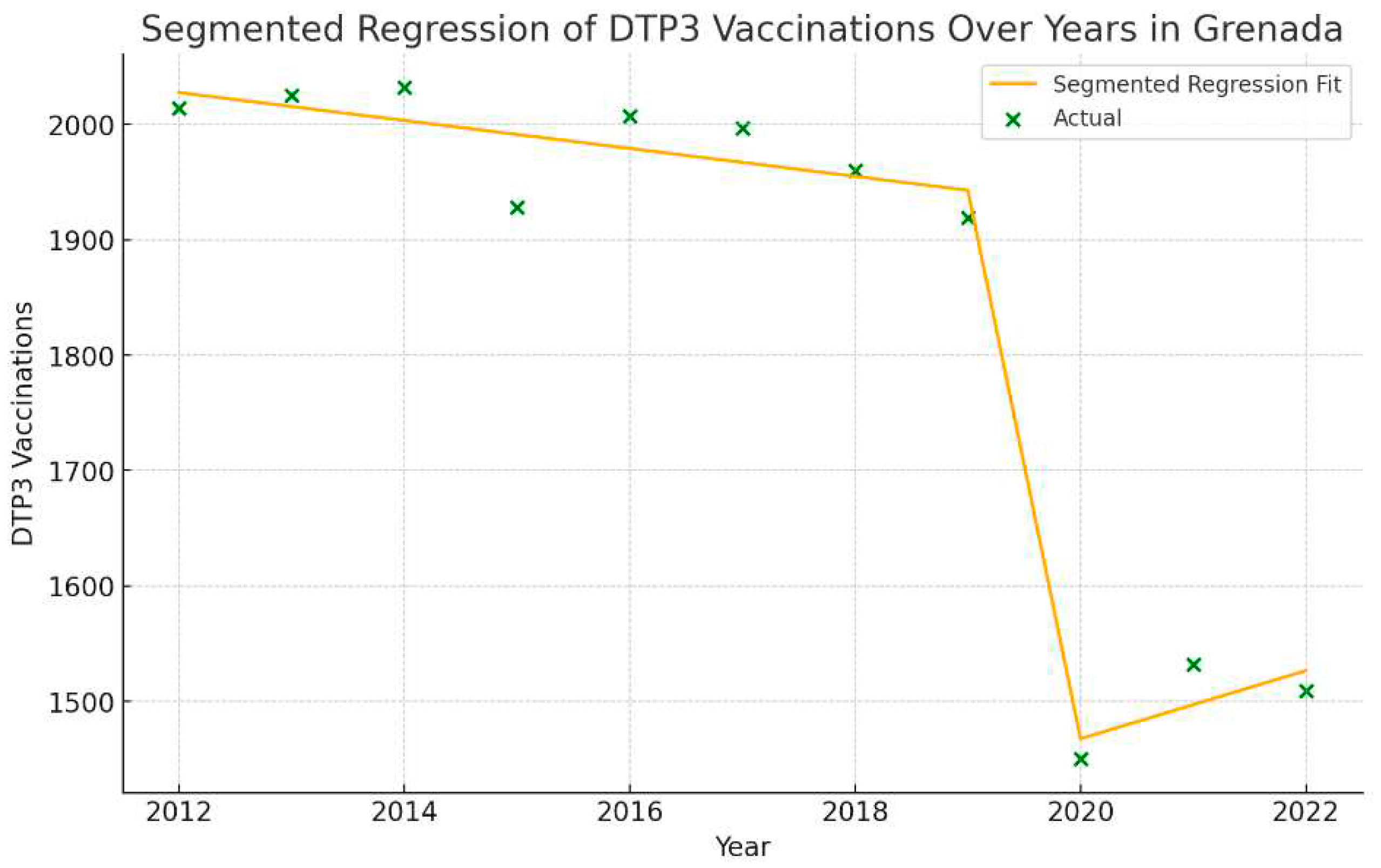
| Grenada | |||||
| Total Period | 2012-2022 | -2.7 | -4.1 | -1.3 | 0.002 |
| Period 1 | 2012-2018 | -0.5 | -3.5 | 2.6 | 0.71 |
| Period 2 | 2018-2022 | -6.5 | -12.1 | -0.6 | 0.036 |
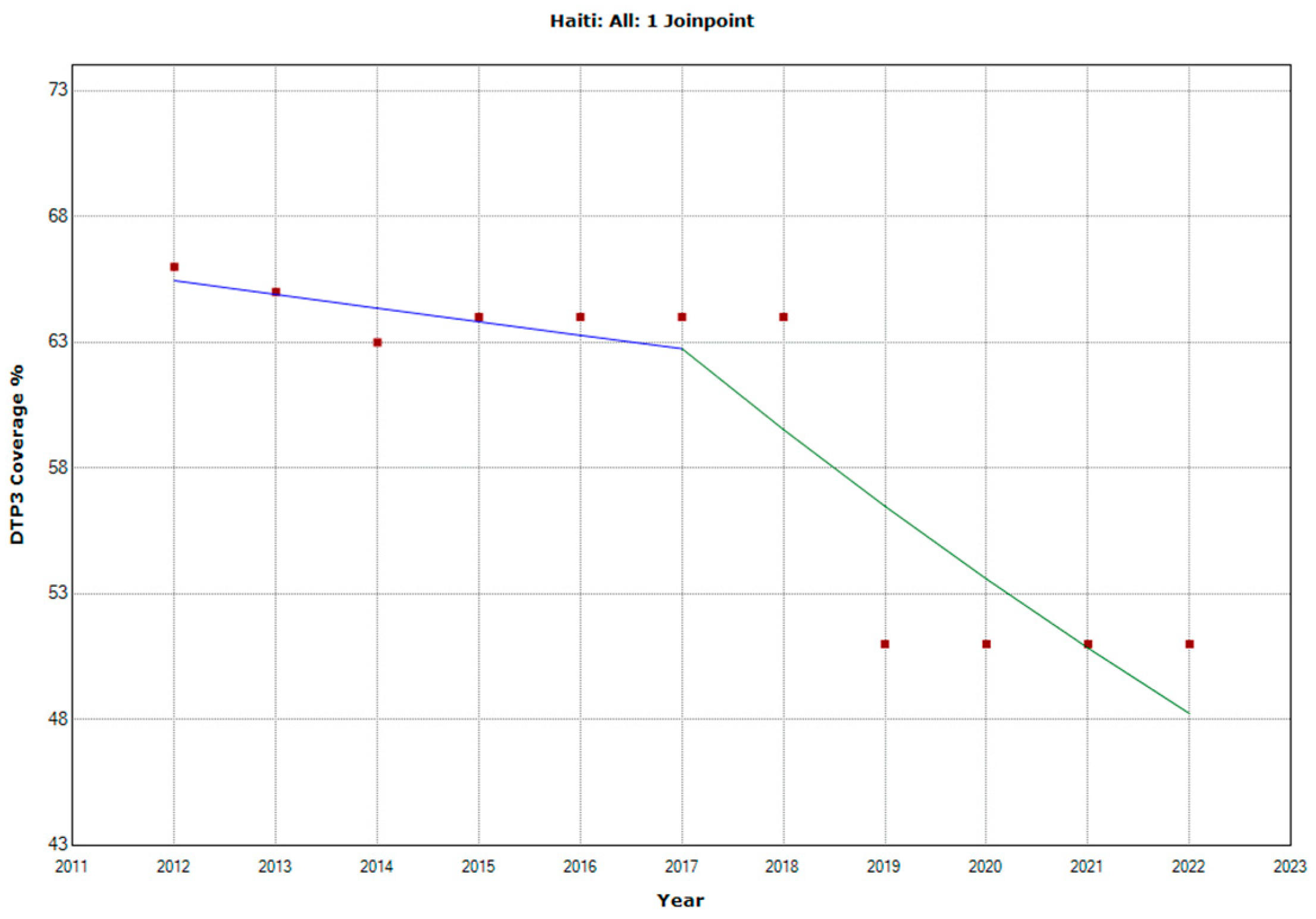
| Haiti | |||||
| Total Period | 2012-2022 | -3.0 | -4.3 | -1.7 | 0.001 |
| Period 1 | 2012-2017 | -0.8 | -5.2 | 3.7 | 0.663 |
| Period 2 | 2017-2022 | -5.1 | -9.3 | -0.7 | 0.029 |
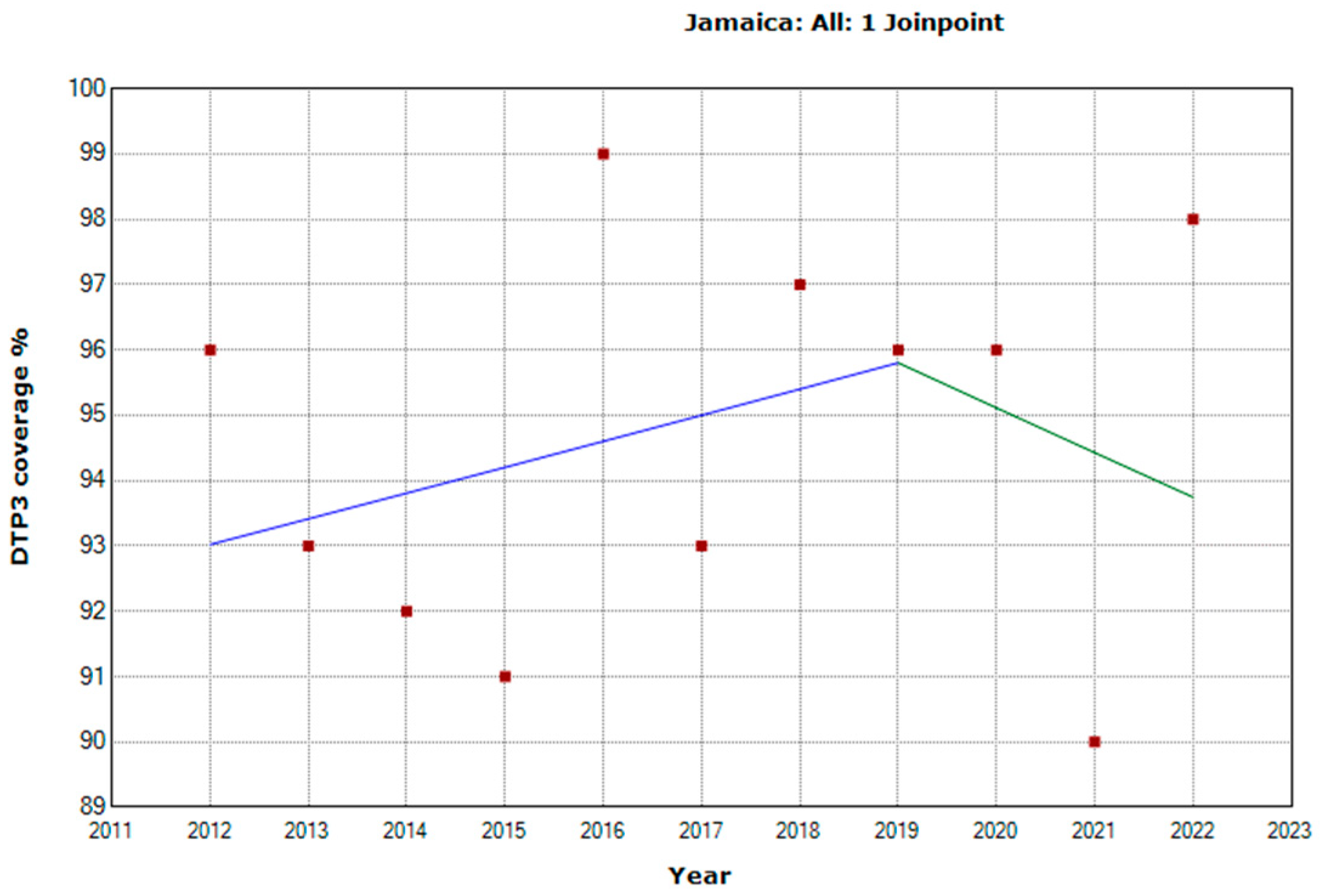
| Jamaica | |||||
| Total Period | 2012-2022 | 0.2 | -0.3 | 0.7 | 0.476 |
| Period 1 | 2012-2018 | 0.4 | -0.8 | 1.6 | 0.427 |
| Period 2 | 2018-2022 | -0.7 | -6 | 4.8 | 0.756 |
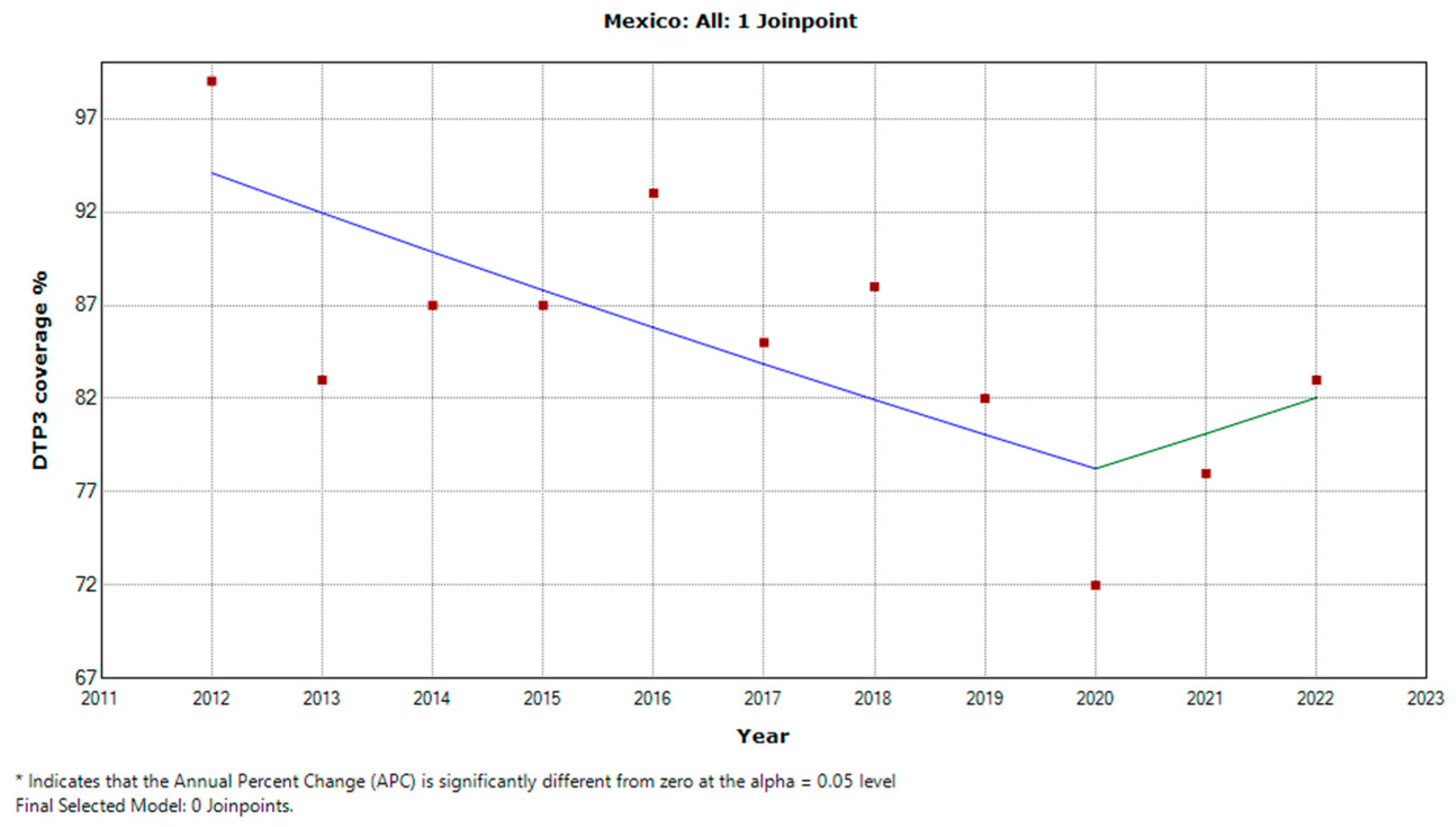
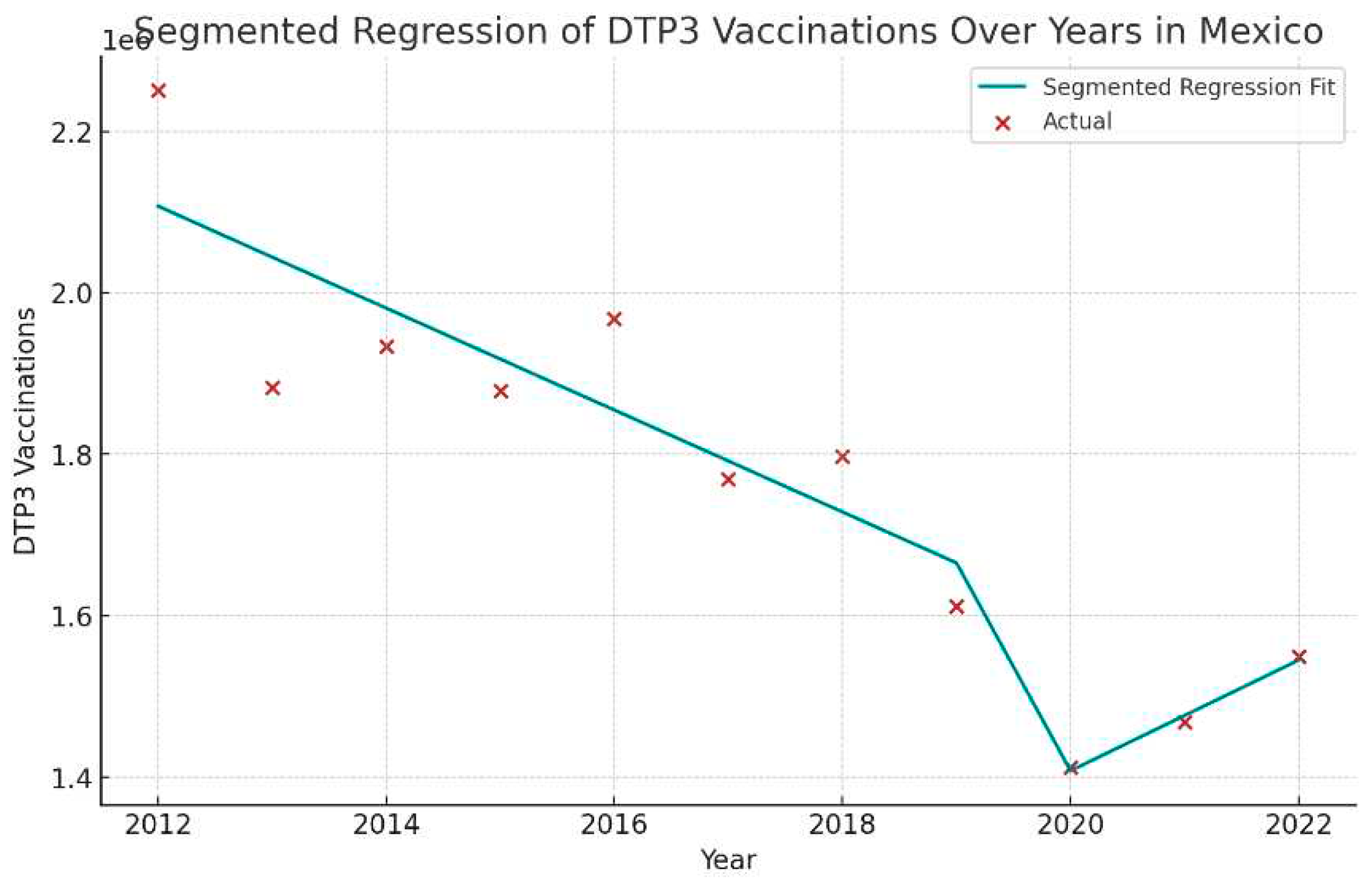
| Mexico | |||||
| Total Period | 2012-2022 | -1.7 | -3.1 | -0.2 | 0.027 |
| Period 1 | 2012-2020 | -2.3 | -4.5 | 0 | 0.048 |
| Period 2 | 2020-2022 | 2.4 | -16.3 | 25.2 | 0.783 |
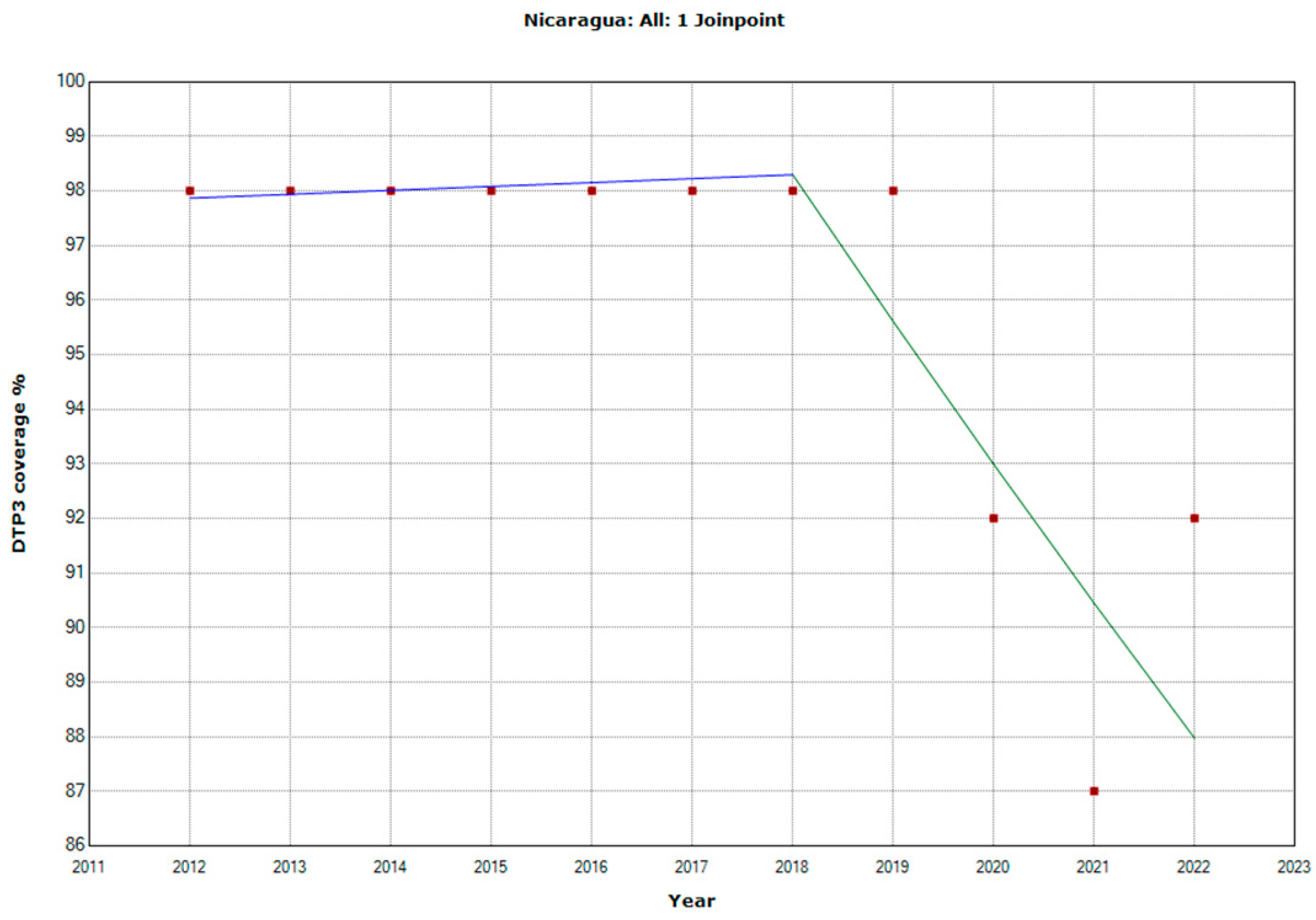
| Nicaragua | |||||
| Total Period | 2012-2022 | -0.9 | -1.5 | -0.4 | 0.006 |
| Period 1 | 2012-2018 | 0.1 | -1 | 1.2 | 0.875 |
| Period 2 | 2018-2022 | -2.7 | -4.9 | -0.6 | 0.022 |
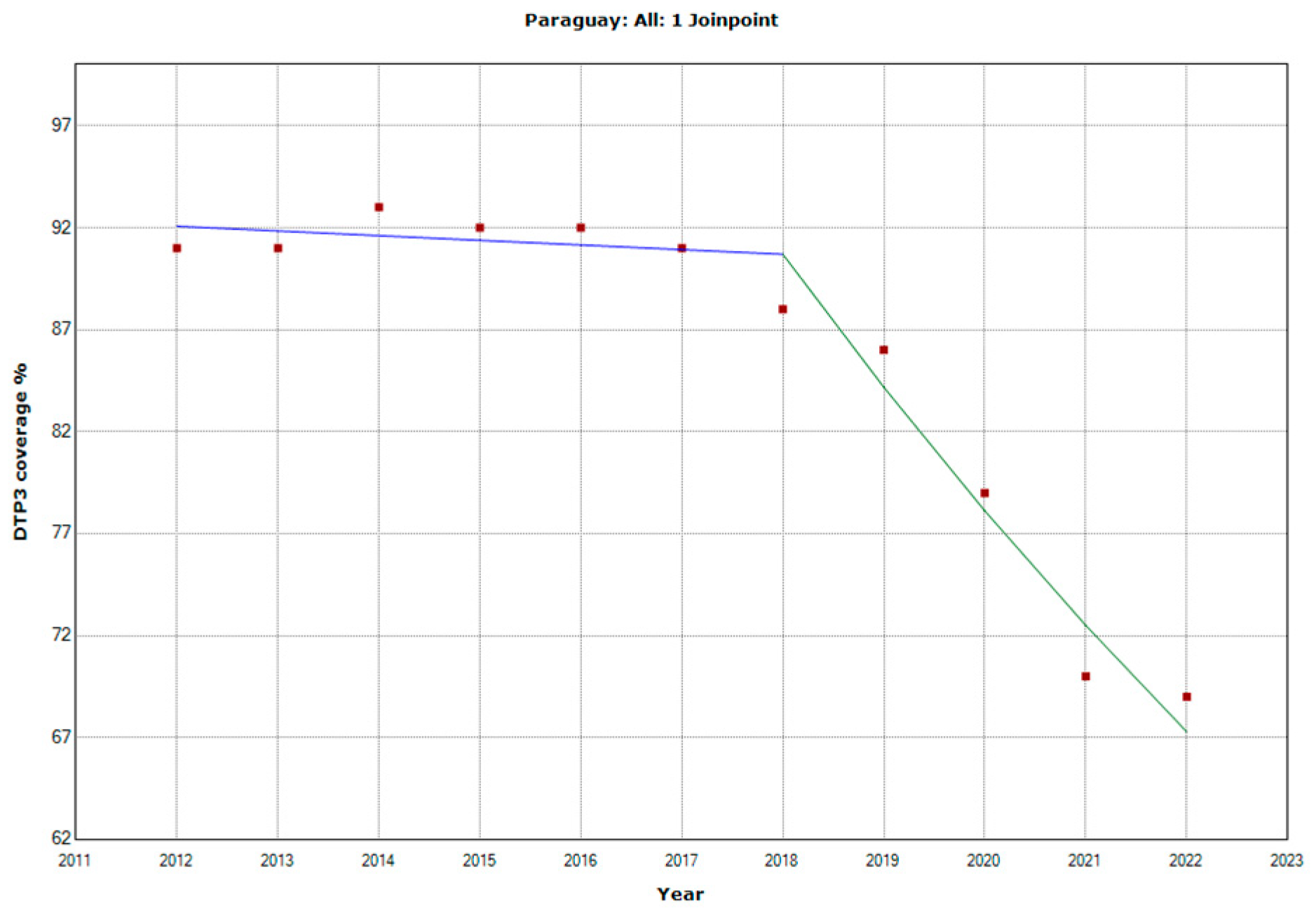
| Paraguay | |||||
| Total Period | 2012-2022 | -2.8 | -4.1 | -1.5 | 0.001 |
| Period 1 | 2012-2018 | -0.3 | -1.1 | 0.6 | 0.506 |
| Period 2 | 2018-2022 | -7.2 | -8.8 | -5.6 | < 0.001 |
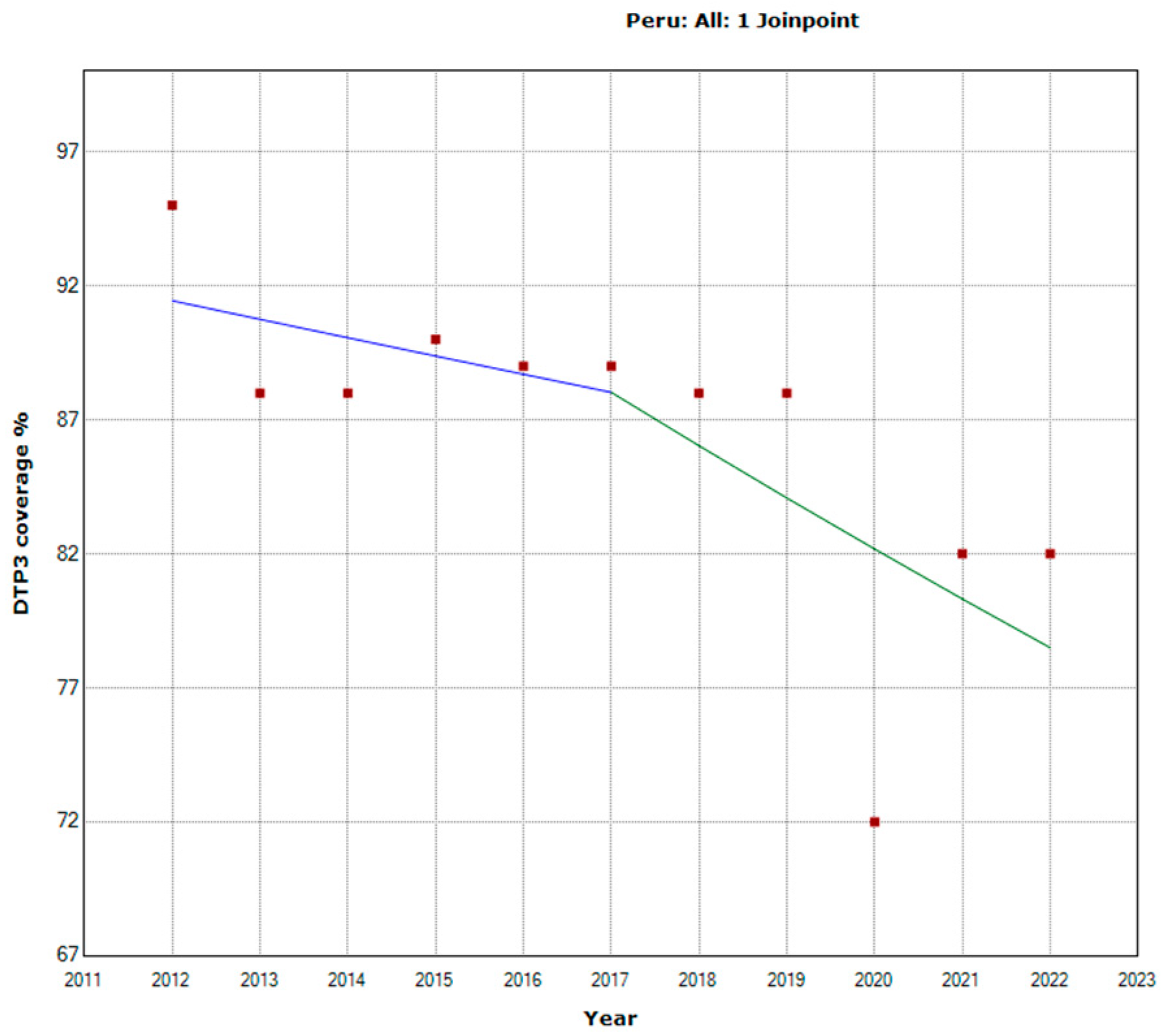
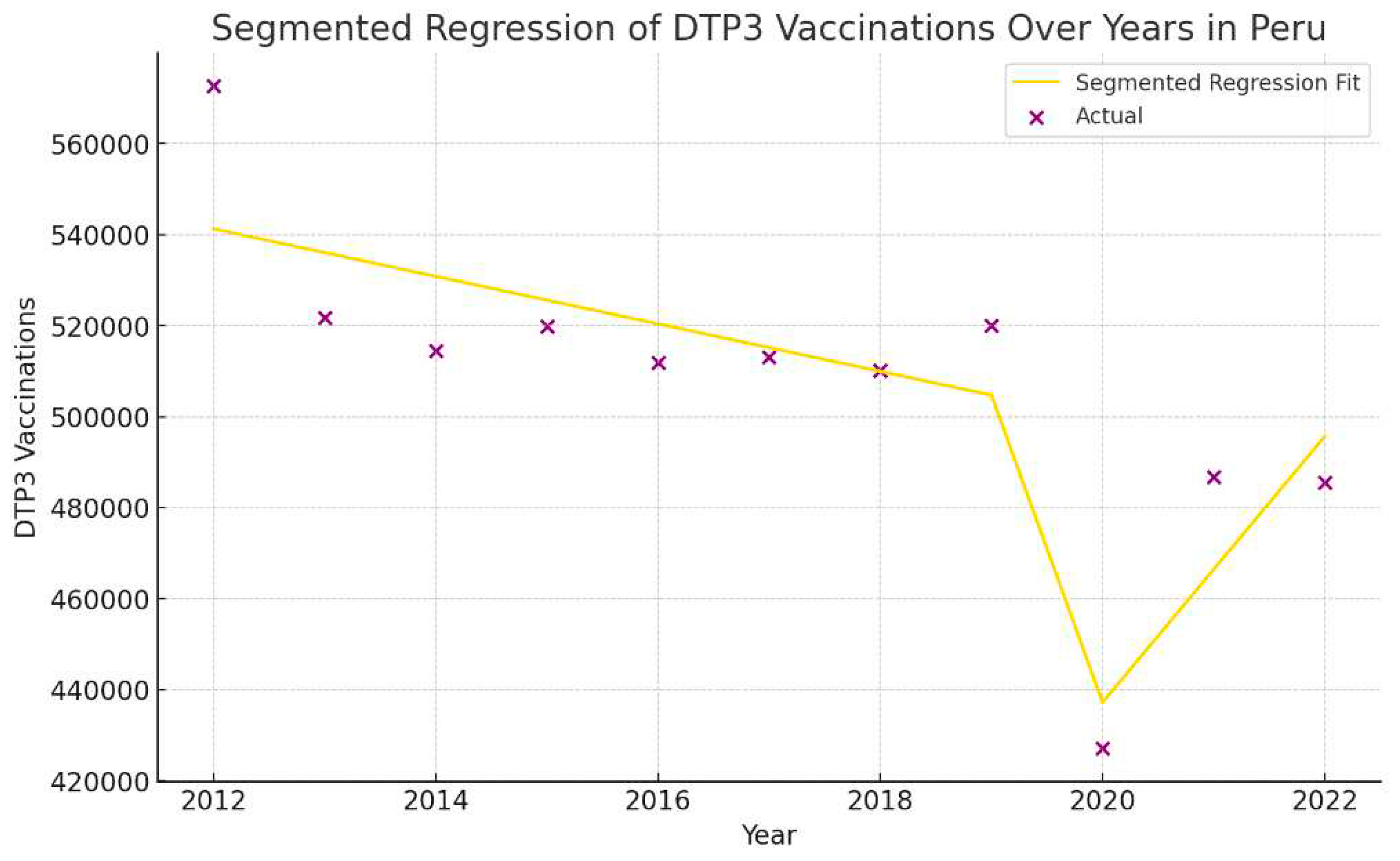
| Peru | |||||
| Total Period | 2012-2022 | -1.5 | -2.6 | -0.4 | 0.012 |
| Period 1 | 2012-2017 | -0.8 | -5.4 | 4.1 | 0.709 |
| Period 2 | 2017-2022 | -2.3 | -6.8 | 2.5 | 0.284 |
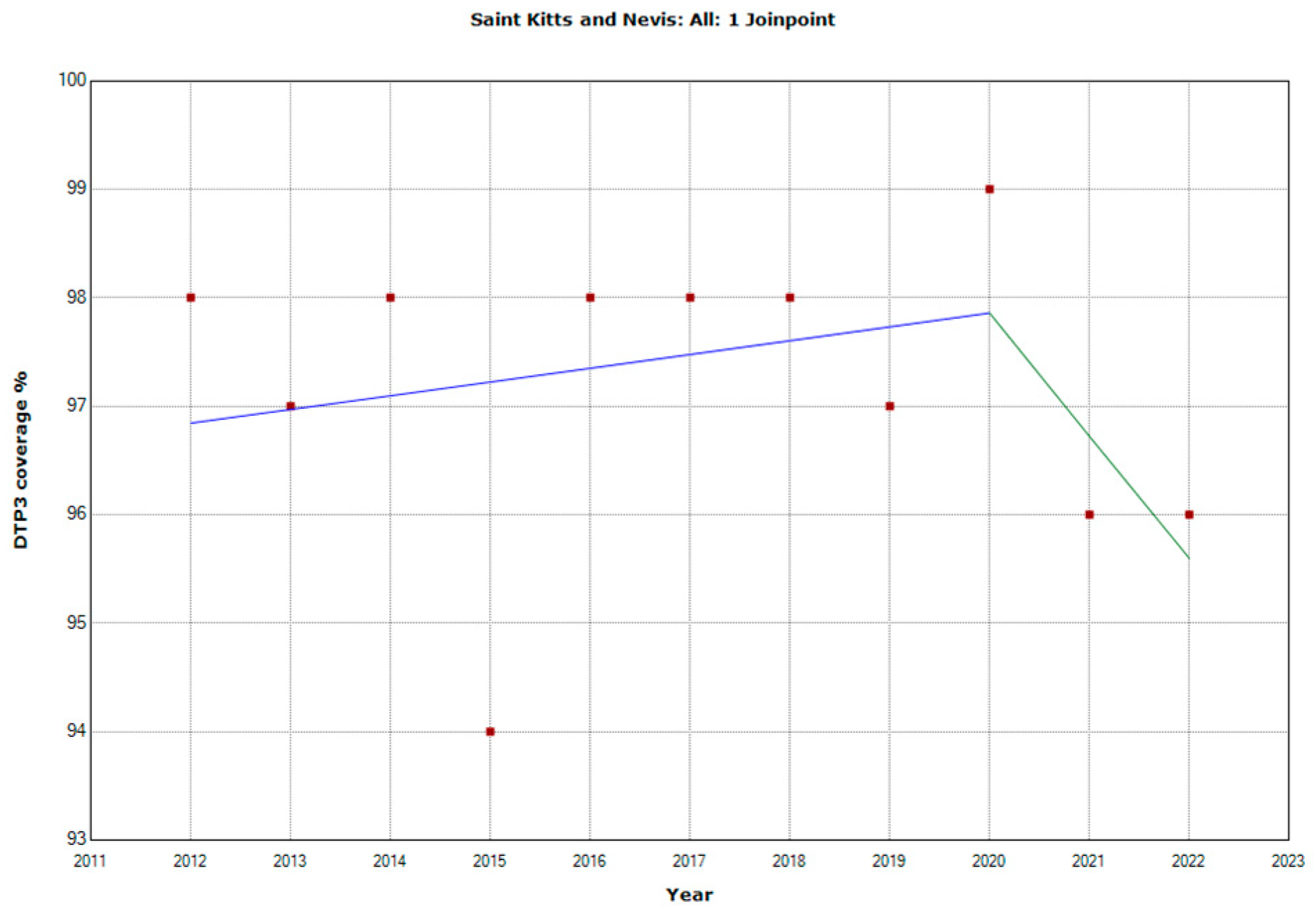
| Saint Kitts and Nevis | |||||
| Total Period | 2012-2022 | 0 | -0.3 | 0.2 | 0.87 |
| Period 1 | 2012-2020 | 0.1 | -0.3 | 0.6 | 0.489 |
| Period 2 | 2020-2022 | -1.2 | -7.1 | 5.2 | 0.661 |
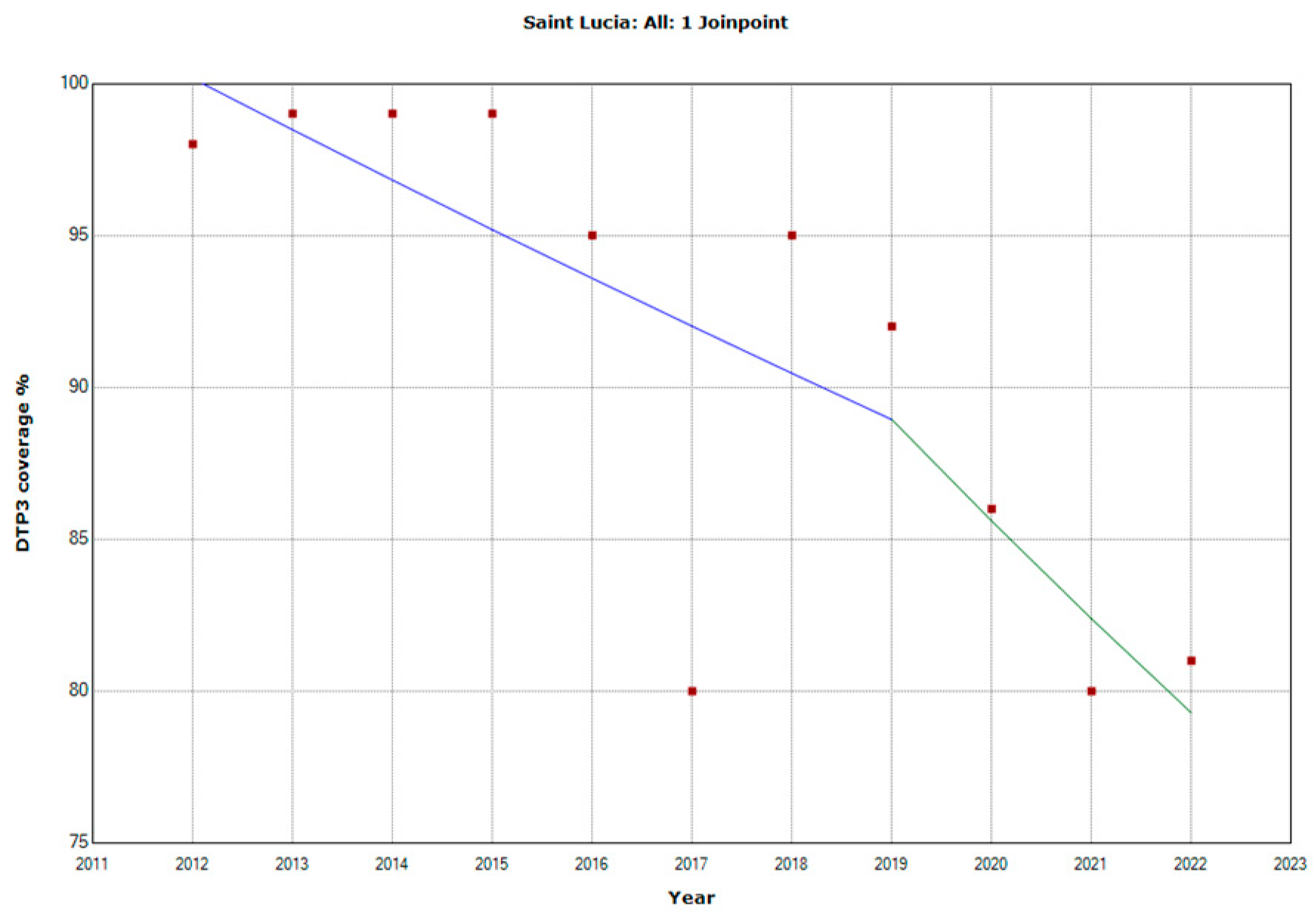
| Saint Lucia | |||||
| Total Period | 2012-2022 | -2.2 | -3.2 | -1.1 | 0.001 |
| Period 1 | 2012-2019 | -1.7 | -4.1 | 0.8 | 0.141 |
| Period 2 | 2019-2022 | -3.8 | -13.2 | 6.7 | 0.4 |
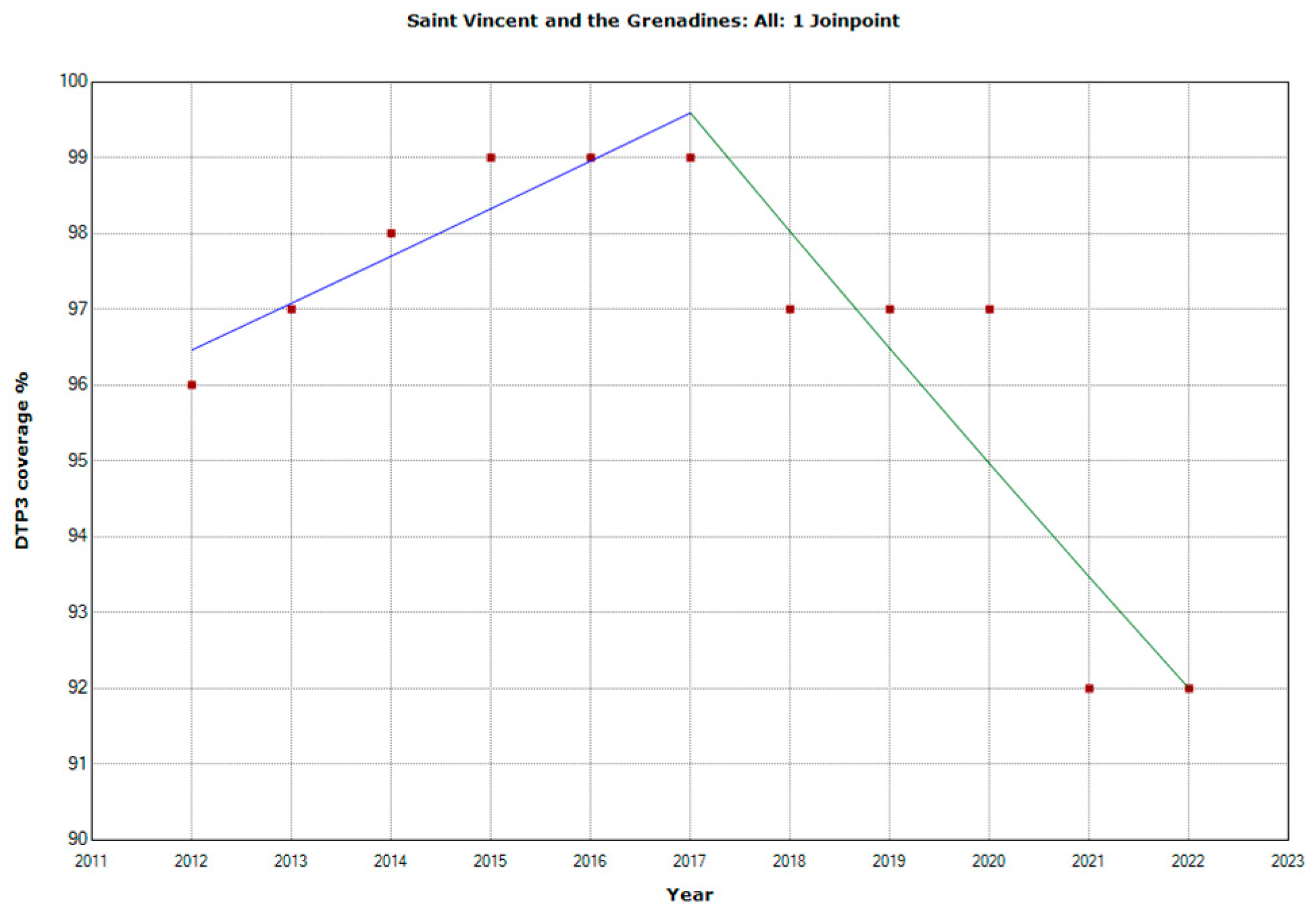
| Saint Vincent and the Grenadines | |||||
| Total Period | 2012-2022 | -0.5 | -0.9 | 0 | 0.045 |
| Period 1 | 2012-2017 | 0.6 | -0.2 | 1.5 | 0.105 |
| Period 2 | 2017-2022 | -1.6 | -2.4 | -0.8 | 0.003 |
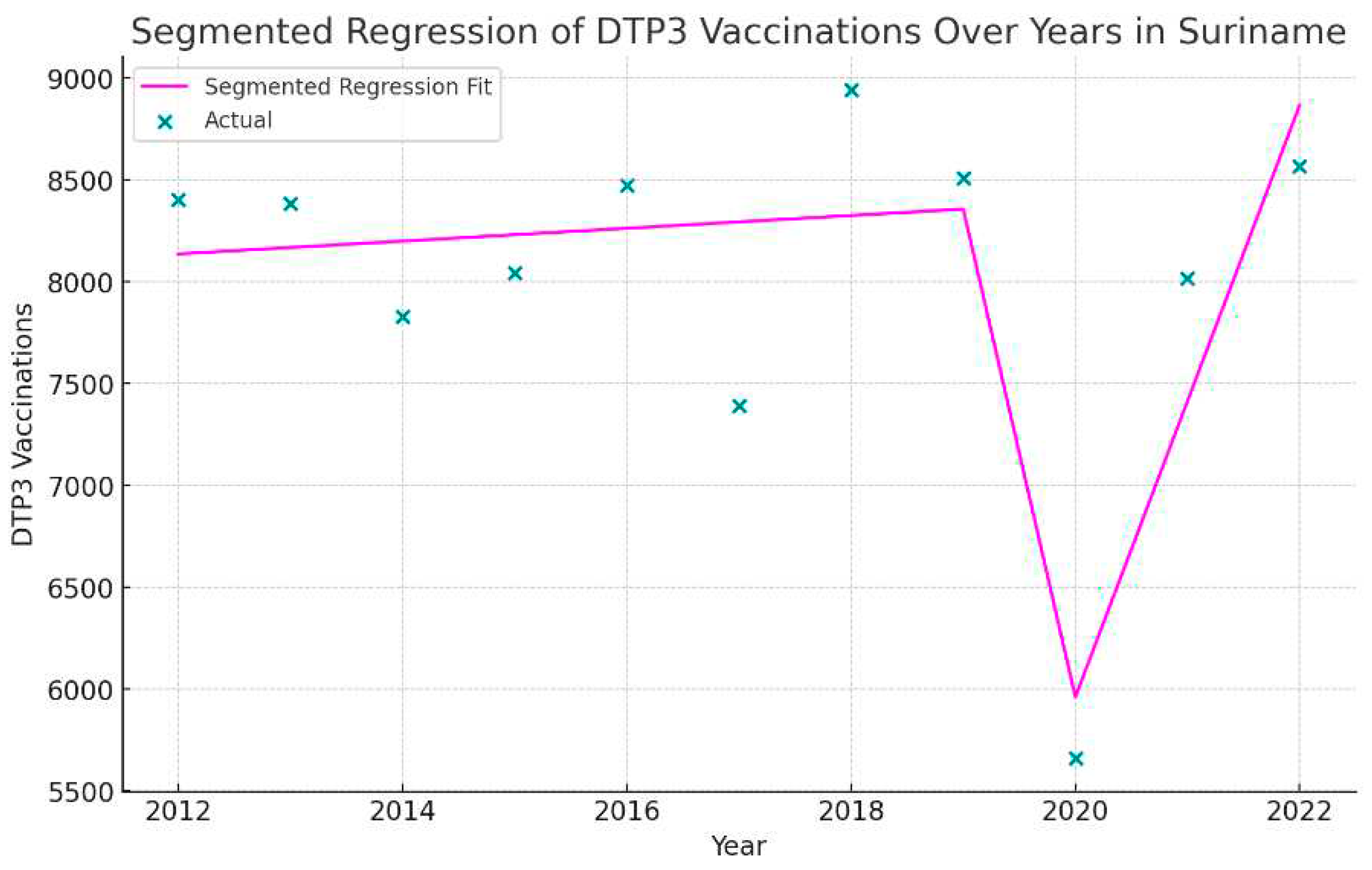
| Suriname | |||||
| Total Period | 2012-2022 | -1 | -3.3 | 1.4 | 0.361 |
| Period 1 | 2012-2020 | -2.1 | -4 | -0.2 | 0.038 |
| Period 2 | 2020-2022 | 7.3 | -14 | 33.9 | 0.466 |
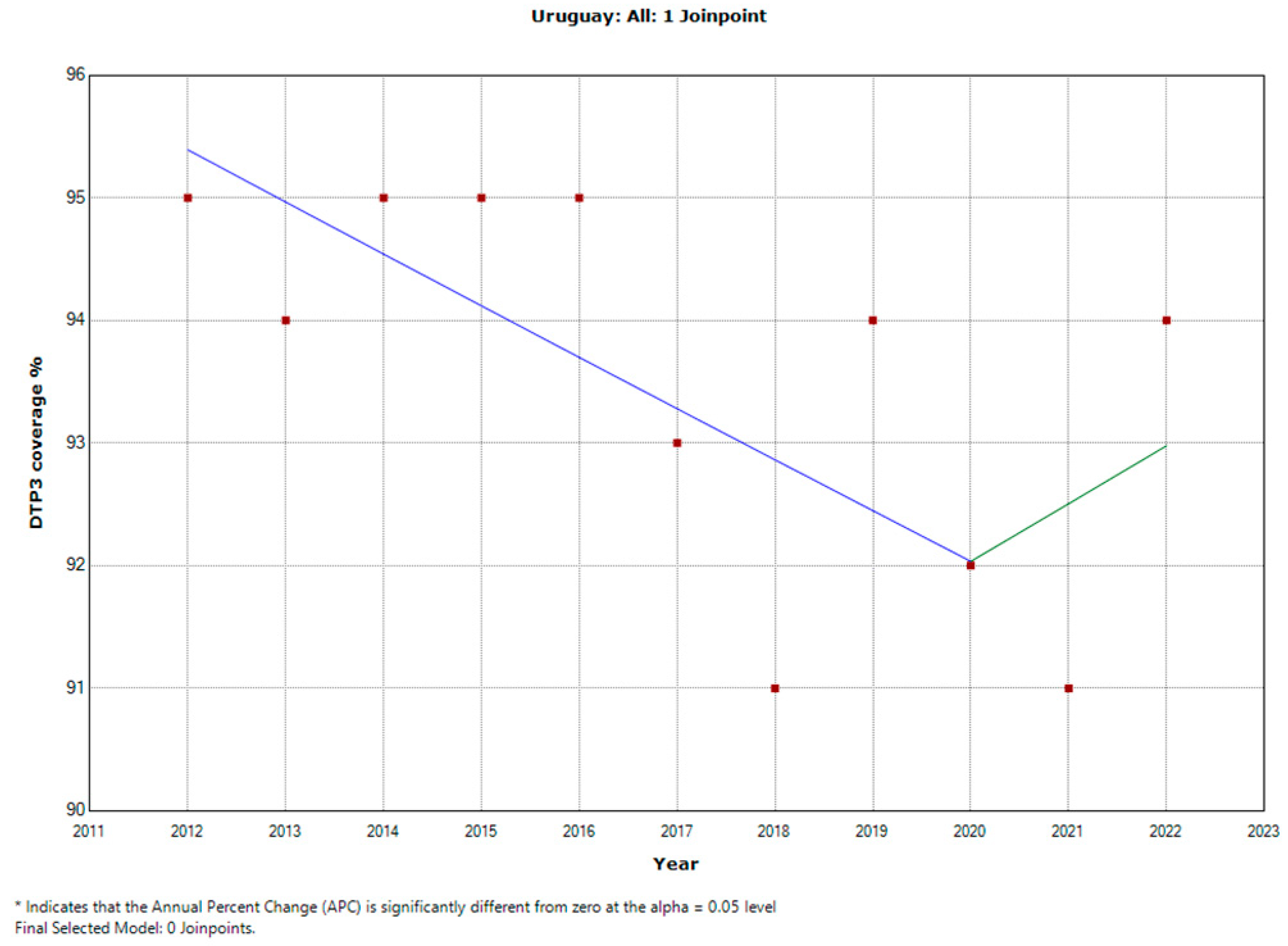
| Uruguay | 2012-2022 | -0.3 | -0.6 | -0.1 | 0.016 |
| Period 1 | 2012-2020 | -0.4 | -0.9 | 0 | 0.049 |
| Period 2 | 2020-2022 | 0.5 | -4.5 | 5.8 | 0.817 |
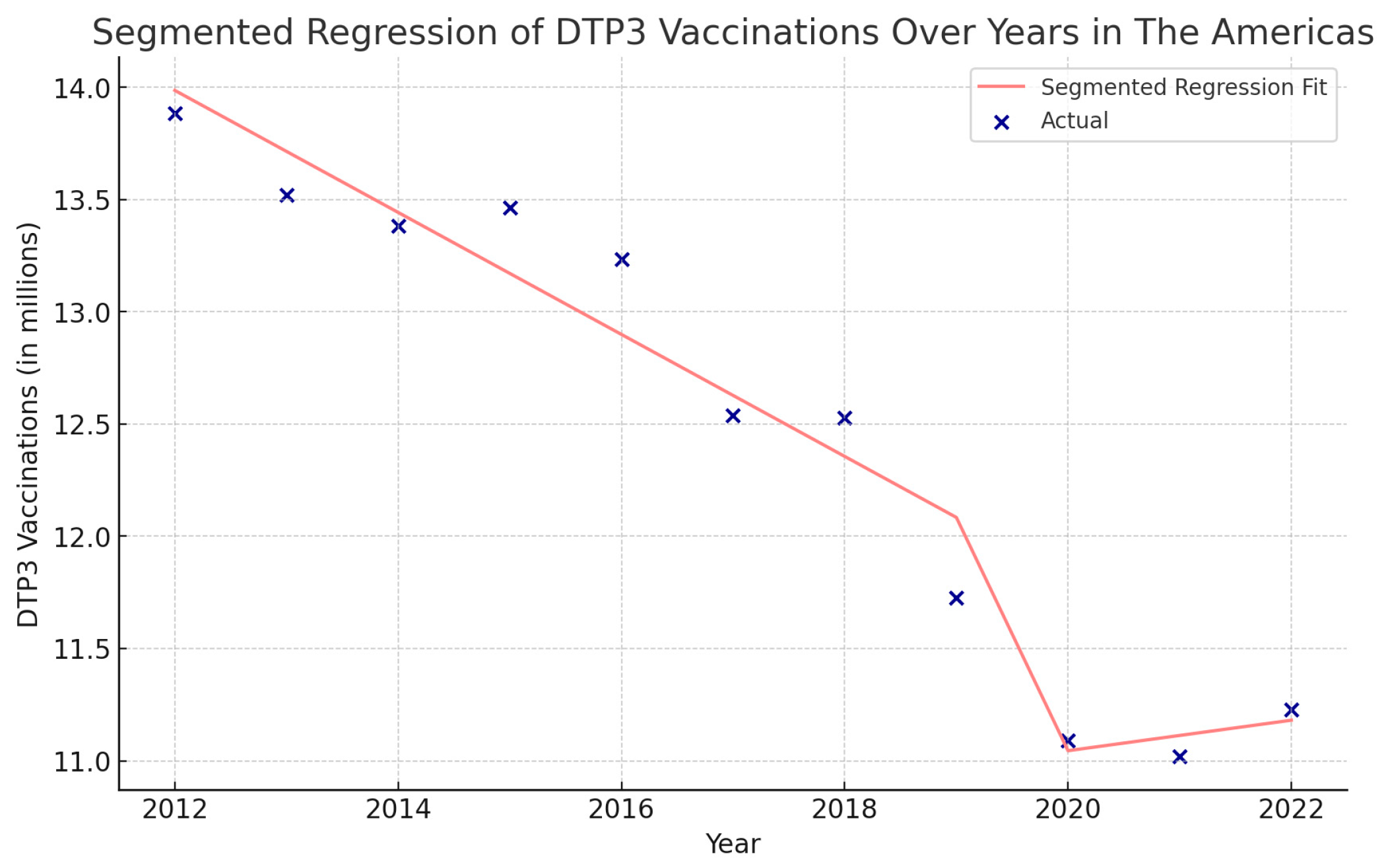
| Region | Intercept | Year | Covid-19 | Interaction |
|---|---|---|---|---|
| The Americas | 14,257,167. | -271,700*** | -3,824,000 † | 339,600† |
| North America | 6,419,470 | -77,900*** | -960,900 | 92,490, |
| Latin America and the Caribbean | 10,258,998. | -239,700 | -3,408,000† | 296,800 |
| Central America | 842,631 | -9,958* | -73,740 | 1,035 |
| The Caribbean | 595,044 | -5,629* | -94,750 | 6,845 |
| South America | 6,552,726 | -161,900** | -2,071,000, | 181,600, |
| Nation | Intercept | Year | Covid-19 | Interaction |
| Antigua and Barbuda | 1,166 | -25* | -242 | 41 |
| Argentina | 747,939 | -21,550* | -440,868 | 40,473 |
| Bahamas | 5,272 | -147* | -2,177 | 235 |
| Barbados | 2,906 | -8 | -444 | 19 |
| Belize | 73,689 | -7 | -3,833* | 240 |
| Bolivia | 246,668 | -4,856† | -80,433 | 6,430 |
| Brazil | 3,086,377 | -101,299* | -799,678 | 76,649 |
| Canada | 346,374 | -1,670 | -28,913 | 4,283* |
| Chile | 223,231 | -1,354 | -54,775 | 6,213 |
| Colombia | 671,882 | 277 | 43,507 | -8,393 |
| Costa Rica | 68482 | -580† | 4,127 | -856 |
| Cuba | 128,843 | -2,206* | 1,376 | -726 |
| Dominica | 889 | 1 | 160 | -16 |
| Dominican Republic | 183,881 | 170 | -58,735 | 4,679 |
| Ecuador | 273,474 | -3,456 | -59,827 | 3,220 |
| El Salvador | 116,148 | -2,777* | -27167 | 1,609 |
| Grenada | 2,040 | -12† | -838* | 42 |
| Guatemala | 366,586 | -4,476 | 36,154 | -5,709 |
| Guyana | 15,500 | 49 | 2,205 | -220 |
| Haiti | 183,283 | -3,133 | -39,333 | 2,490 |
| Honduras | 215,078 | -3,019 | -29,014 | 1,396 |
| Jamaica | 39,982 | -942* | -8,835 | 955 |
| Mexico | 2,170,515 | -63,127* | -1,379,021† | 131,627 |
| Nicaragua | 140,894 | -108 | -4,172 | -885 |
| Panama | 62938 | 493 | -48,279 | 4,392 |
| Paraguay | 123,679 | 129 | 48,857 | -7,328 |
| Peru | 546,498 | -5,221 | -372,338* | 34,451* |
| Saint Kitts and Nevis | 672 | -10* | 123 | -14 |
| Saint Lucia | 2,207 | -38† | 242 | -37 |
| Saint Vincent and the Grenadines | 1,843 | -57* | -25 | 1 |
| Suriname | 8105 | 31 | -15,211* | 1,421* |
| Trinidad and Tobago | 19,470 | -221* | 3238 | -372 |
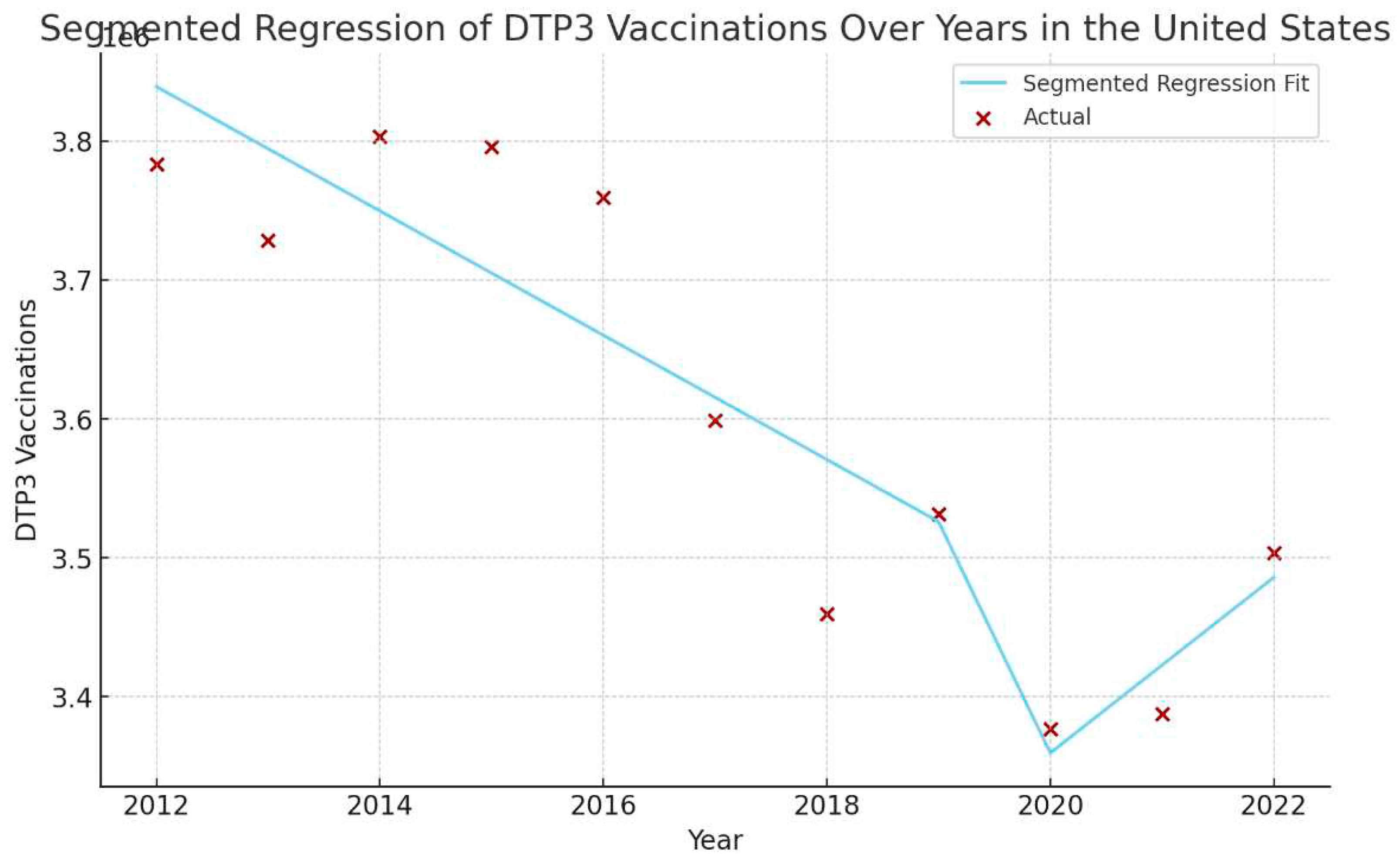
| United States | 3,884,049 | -44,760* | -1,093,444† | 107,962† |
| Uruguay | 49,522 | -1,632* | -21,125 | 2,086 |
| Venezuela | 549,286 | -26,220 | -268,317 | 23,130 |
| Joinpoint | X2 | Segmented regression | |||
|---|---|---|---|---|---|
| Country | Estimate | Lower 95%CI | Upper 95%CI |
2019-22 | 2002-22 |
| Antigua and Barbuda | 2017 | 2014 | 2020 | <0.001 | |
| Argentina | <0.001 | ||||
| Bahamas | 2020 | 2014 | 2020 | ||
| Barbados | |||||
| Belize | 2019 | 2014 | 2020 | 0.003 | <0.05 |
| Bolivia (Plurinational State of) | <0.001 | ||||
| Brazil | <0.001 | ||||
| Canada | 2018 | 2016 | 2020 | <0.05 | |
| Chile | |||||
| Colombia | 2019 | 2017 | 2020 | <0.001 | |
| Costa Rica | 2017 | 2014 | 2020 | ||
| Cuba | |||||
| Dominica | 2020 | 2014 | 2020 | ||
| Dominican Republic | |||||
| Ecuador | 2018 | 2014 | 2020 | <0.001 | |
| El Salvador | <0.001 | ||||
| Grenada | 2018 | 2014 | 2020 | <0.05 | |
| Guatemala | <0.001 | ||||
| Guyana | |||||
| Haiti | 2017 | 2014 | 2020 | ||
| Honduras | <0.001 | ||||
| Jamaica | 2019 | 2014 | 2020 | ||
| Mexico | 2020 | 2014 | 2020 | <0.001 | |
| Nicaragua | 2018 | 2016 | 2020 | <0.001 | |
| Panama | |||||
| Paraguay | 2018 | 2016 | 2019 | <0.001 | |
| Peru | 2017 | 2014 | 2020 | <0.001 | <0.05 |
| Saint Kitts and Nevis | 2020 | 2014 | 2020 | ||
| Saint Lucia | 2019 | 2014 | 2020 | ||
| Saint Vincent and the Grenadines | 2017 | 2014 | 2020 | ||
| Suriname | 2020 | 2014 | 2020 | <0.05 | |
| Trinidad andTobago | |||||
| Uruguay | 2020 | 2014 | 2020 | ||
| United States | |||||
| Venezuela | <0.001 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





