1. Introduction
Aerosol particles are convenient carriers of therapeutic agents targeted to the respiratory system (RS). This method of drug delivery has been known since ancient times, where inhaling smoke from burning plant leaves was considered to relieve respiratory ailments [1,2]. In modern times, the dedicated medical devices for aerosol generation for inhalation purposes (nebulizers and inhalers) have been developed. Also, the beneficial effects of inhaling saline aerosols/salt particles from the environment have contributed to the development of halotherapy as a method of pulmonary rehabilitation [3], which can be also carried out under specific conditions of underground treatment in caves and salt mines (subterranean therapy) [4,5]. In addition to treating respiratory diseases, aerosols can also carry pharmaceuticals absorbed into the circulation and acting in other organs (systemic drugs). This can include insulin [6,7], painkillers [8], neuroactive substances [9,10], and even cardiovascular drugs [11], confirming that inhalation has the potential for applications in new therapeutic areas.
Despite the apparently easy (natural) way to introduce aerosol into the lungs via inhalation, obtaining particles with optimal properties and their application to maximize their delivery to specific areas of the RS is challenging. This is due both to the complex geometric structure of the RS in which the aerosol must be transported and distributed, and to the physics of aerosols during their actual airflow in the body. This paper highlights the most important, albeit often overlooked, factors responsible for successful aerosol drug targeting in RS, and attempts to identify and indicate new opportunities to improve this therapeutic method.
2. Major factors influencing the efficiency of drug delivery using aerosols
2.1. Basic concepts of inhalation therapy
Aerosol is a thermodynamically unstable system, so it cannot be prepared in advance and stored until use, but it must be generated just before inhalation. This is done with the help of special, sometimes complicated technical devices (inhalers or nebulizers). Since neither aerosol generation nor aerosol deposition is fully effective (efficiency below 100%), the amount of drug delivered to the target area that should induce the expected therapeutic effects is always lower than the initial dose loaded into the aerosolizing device.
Different physical mechanisms act on inhaled particles of various properties (e.g., shape, density) and sizes (micro- and nanoparticles), influencing the efficiency of their delivery to different parts of RS [12]. These mechanisms also depend on the actual flow in the system, and it is important to note that respiration is inherently associated with unstable (oscillatory) aerodynamic conditions, which strongly affect the behavior of aerosol particles. In addition, aerosol particles also can change their size during their lifetime, e.g., due to coagulation, condensation, or evaporation.
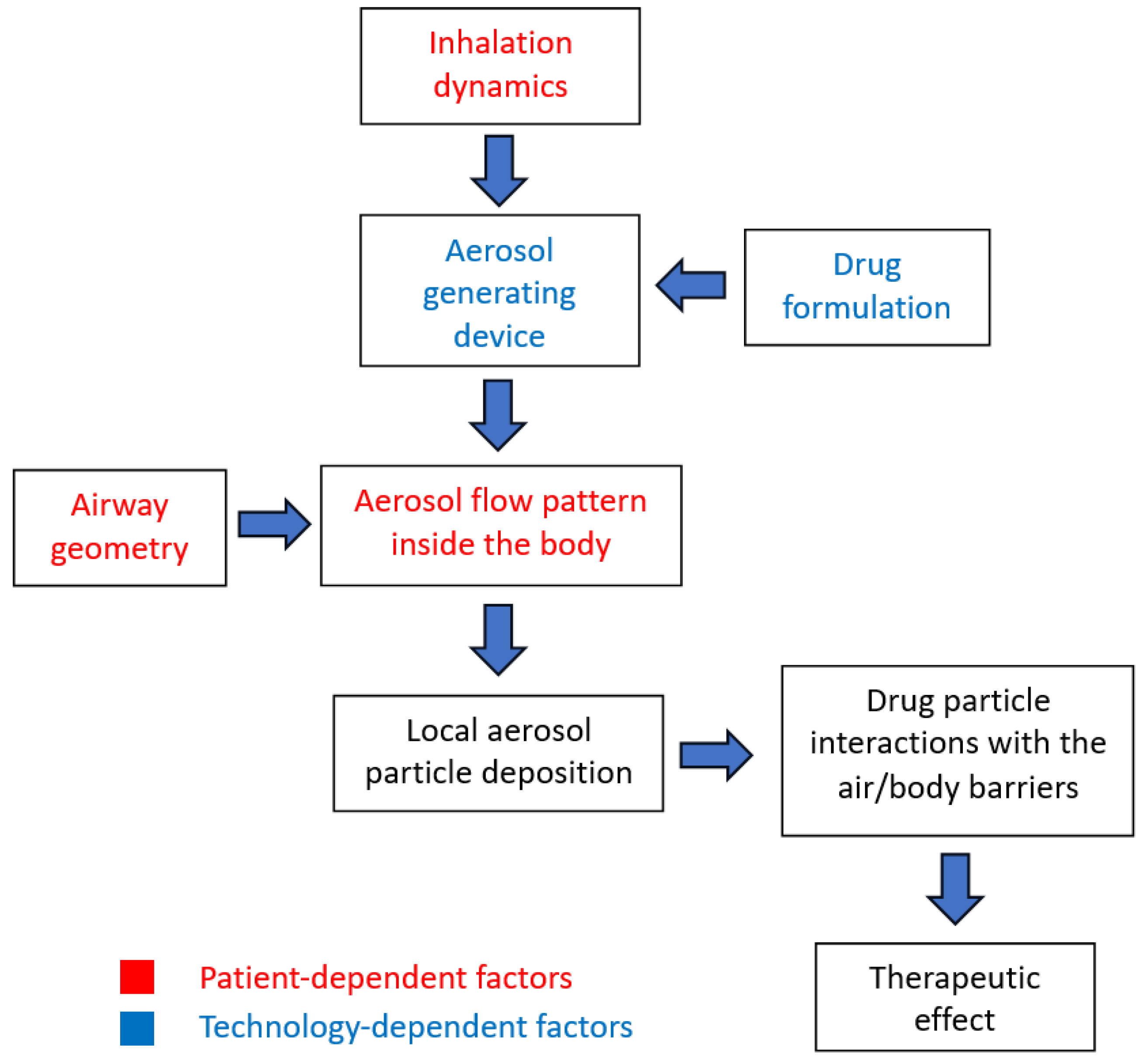
According to the above, it is clear that - unlike many other drug delivery systems (injections, capsules and tablets, suppositories) - the dose of inhaled aerosol drug delivered to the target areas cannot be precisely known, at it depends on many patient- and technology-dependent factors, which are indicated in
Figure 1.
2.2. Inhalation dynamics and particle deposition mechanisms
A considerable number of studies on experimental and numerical modeling of aerosol flow and deposition in the human respiratory tract are available in the literature [13–15], so only selected, sometimes underestimated or less frequently discussed issues will be highlighted here.
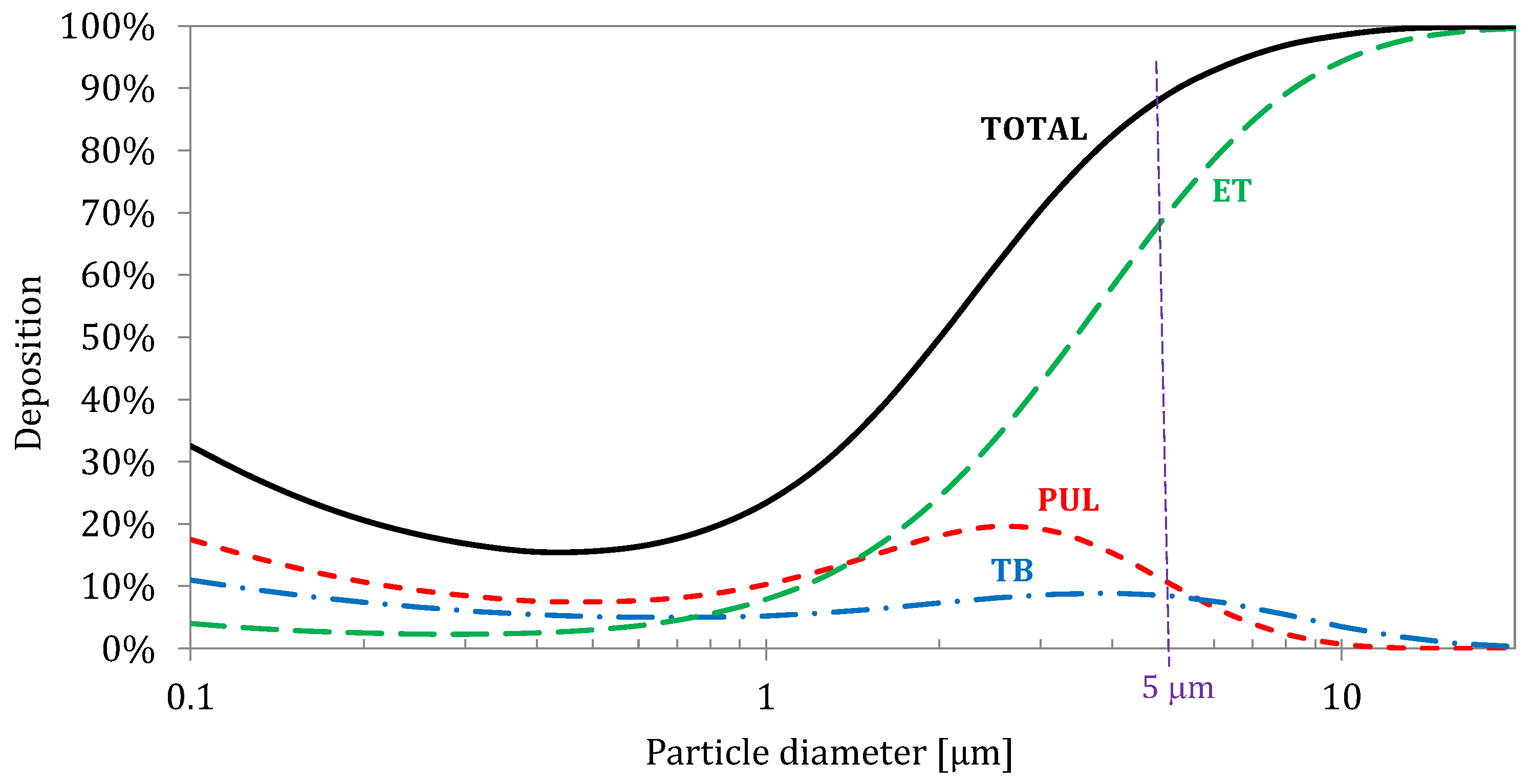
Upon inhalation, aerosol passes the airways of the head region (nasal or oral cavity, throat) and then it penetrates through the geometrically complex tracheobronchial tree. Inhaled particles undergo selective separation (deposition) in subsequent areas of RS through which they flow. This explains why large particles cannot be used to effectively target the pulmonary region. The schematic deposition efficiency curve for inhaled aerosol particles in the size range of 0.1-15 μm, which are typically used in the treatments of the lower RS is presented in
Figure 2. These data also show that always (for any particle size) fraction of inhaled drug is deposited in the regions outside this target, which can raise some concerns regarding the safety of the inhalation therapy, i.e., side-effects [16]. It should be also noted that some particles (mainly in the size range of 0.2-0.5 μm) are not deposited and are exhaled, since all deposition mechanisms for this size are ineffective.
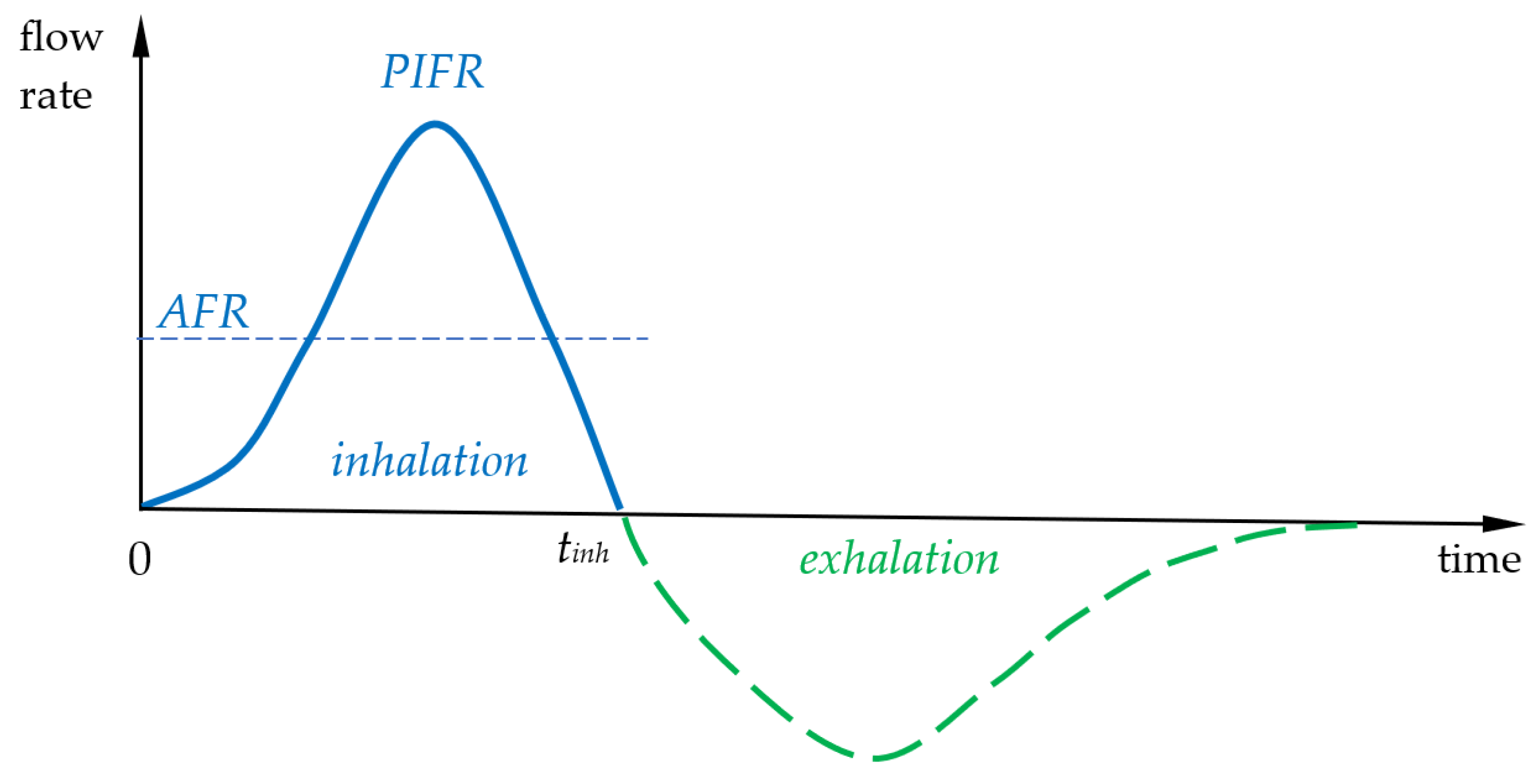
Most inhaled particles are deposited during aerosol entry into the lungs (inhalation), but some are also deposited during breath-holding [18,19] (which is often recommended as a good practice for patients using inhalers) as well as exhalation. Typical airflow during unforced inhalation, which is typical, e.g., for nebulization, is characterized by the frequency (breathing rate,
BR) of 12-15 min
-1 and total inhaled volume (tidal volume,
TV) of 500 ml. Taking
BR=15 min
-1, the average inhalation flow rate (
AFR) is equal to 250 L/s, i.e., 15 L/min, whereas the peak inspiratory flow rate (
PIFR) is at the level of 30-40 L/min,
Figure 3. From any type of inhalation curve, the
AFR can be calculated according to:
where
tinh is the inhalation time and
Q(t) – the instantaneous airflow rate. As seen in
Figure 3 the shape of exhalation curve is slightly different, especially in obstructive lung diseases when the duration of air outflow is extended, but, of course, all previously inhaled volume is forced out.
As already mentioned, particles are deposited due to several mechanisms (mainly: impaction, gravitational sedimentation, interception, Brownian diffusion), which are influenced by the time-varying local flow velocity in the given airways and the properties of the particles (mainly size/mass and shape). This hinders the precise determination of a direct relationship between particle size and location of deposition. The common misunderstanding is assuming that particles of a given size can be deposited only in a certain region or even a single bronchial generation. Even particles with one size (monodisperse aerosol) show spatial distribution of deposition in the RS. It can be easily seen in
Figure 2, which shows that deposition of 5 μm takes place mainly in the extrathoracic region (approx. 70% of the inhaled amount), but also in the tracheobronchial (approx. 9%) and the pulmonary regions (approx. 11%).
Theoretically, the behavior of aerosol particles in the RS can be analyzed using dimensionless numbers which are typically applied in characterization of the airflow and aerodynamic forces acting on aerosol particles in other (mainly technical) applications. However, it is important to be aware of some limitations of using common criteria such as Reynolds numbers (Re) and Stokes numbers (Stk), since the air velocity in the system is variable and, at the same time, the airways of a certain diameter are short, leading to a strong influence of inlet effects on the airflow field. For instance, the airflow through trachea during breathing is changing from laminar at the start of inhalation to turbulent at
PIFR, and then it becomes laminar again when the flow decreases down to zero (see
Figure 3).
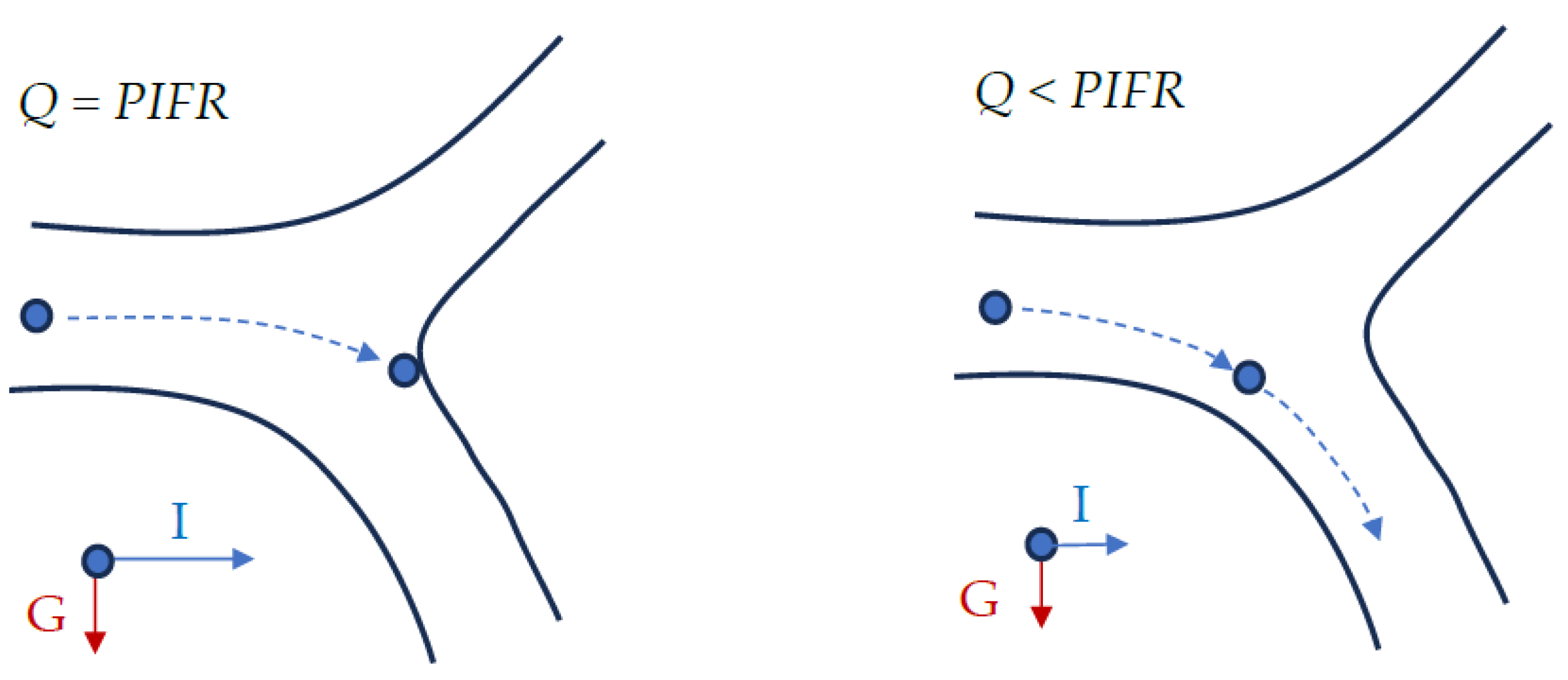
The variations in airflow structure influence particle fate in the airways. For example, if 5 μm particles are deposited by impaction in a certain generation at
PIFR, it may be expected that such particles can avoid inertial deposition in the same generation when the flow is slower, i.e., at all other moments of inhalation, because the inertial force acting on such particles will be weaker (
Figure 4). On the other hand, slower flows increase the probability of deposition by sedimentation (for large particles) and diffusion (for particles smaller than 0.1 μm). It is due to a longer residence time of the aerosol in a given element of RS, i.e., longer time available to particle landing on the airway wall due to gravitation. This analysis shows that there is an interplay between particle size, and its local and temporal velocity in the airways.
It follows that the common assumption of steady flow which is used in many CFD and experimental
in vitro studies is unrealistic and may result in unprecise understanding and predictions of drug delivery to different regions of RS. For example, an analysis by Sosnowski et al. [20] showed that the actual airflow structure inside the oral cavity and pharynx at any phase of inspiration is never equal to the structure representing the average flow. This was confirmed also for bronchial airways [21]. The results of particle deposition in a given location inside the airways which are obtained assuming
Q =
AFR also differs from the values obtained from summing the instantaneous deposition during the cycle, and this can be easily explained by the fact that local deposition efficiency of particles with a certain size is not a linear function of the flow rate. Therefore, the cumulative number (or mass) of drug particles deposited in each RS region during inhalation cannot be assessed by evaluating the flux for the
AFR and extrapolating it over the entire time
tinh [22,23]. The assumption of the steady-state flow also neglects all transient effects, which influence particle deposition. Secondary flows, which are formed during realistic breathing in the regions of bronchial bifurcation, were shown to increase the deposition of inhaled particles [22–25]. These flows can be characterized by Womersley number, Wo:
where R is radius of the tube (bronchus), ω – angular frequency of breathing, ν - kinematic viscosity of air.
Another common simplification in many studies is the assumption of a parabolic profile at the inlet the trachea, which neglects airflow disturbances generated before the air enters in bronchial tree (laryngeal jet) [26,27].
It should be also remembered that particles which have entered the respiratory system during inhalation but were not deposited during this period, can be deposited during other phases of breathing. Particularly, the instant of stopping and the reversal of flow direction from inhalation to exhalation can contribute to enhanced deposition of extrafine particles [20,28].
2.3. The influence of airway geometry
Almost all quantitative deposition data available in the literature, obtained with
in vivo,
in vitro, and
in silico (CFD – computational fluid dynamics) studies, are obtained for healthy subjects. This is partly because many results were obtained in the field of inhalation toxicology and then adapted to inhalation therapy. However, inhalation drugs are administered to patients suffering from lung diseases such as asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis, pulmonary hypertension, etc. In all these cases, the airways are locally narrowed or obstructed due to excessive mucus secretion and inflammation. This changes the geometry of bronchial airways, result in different airflow and the distribution of particle deposition. Kadota et al. [29] compared the results of CFD calculations for three actual geometries of COPD patients, showing the dependence of drug delivery effectiveness on disease severity. Results obtained in our laboratory show the variable distribution of aerosol flow through the bronchi of reconstructed 3D bronchial geometry of a patient with COPD according to data from [29],
Figure 5. The observed flow structure will affect the mass of aerosol that penetrates to different areas of the lungs, as predicted by CFD computations.
3. The role of the aerosol generating device and the form of the precursor
It was already highlighted that aerosol must be generated directly before inhalation due its intrinsic instability. Even if the time scale required for the use of freshly produced aerosol is short, rapid changes in the aerosol properties may lead to its inapplicability to a given therapeutic purpose. The method of aerosol generation is dictated by the form of the precursor, which can be either liquid (solution or suspension) or solid (powder).
Medicinal liquids are atomized into fine droplets by several methods: by applying pressure to the liquid forced through the nozzle, pneumatically (using compressed air), by ultrasounds [30], by collision of liquid streams [31], electro-hydrodynamically [32], using surface acoustic waves [33], etc. The size distribution of generated liquid droplets can be adjusted to certain therapeutic application by the design of the atomizing device, process parameters, and liquid properties.
Aerosol generation from powders must combine powder fluidization (transfer to the gas phase) with particle deagglomeration (break-up of particle clusters) [34]. This requires turbulent flow through the inhaler, and usually is related with a high pressure drop which must be overcome by patient during inhalation. This is why, a special inspiration maneuver is always required when using dry powder inhalers (DPIs) to assure a forceful flow with a defined duration. It should be noted that the required flow pattern is not always achievable with certain DPIs, since patients are of different ages and health conditions (e.g., children, elderly, patients with COPD), therefore different inhalation force and capability to inhale according to the requirements. The emitted dose and particle size distribution of the aerosol particles can be flow-dependent, and it is a function on the DPI design and drug formulation [35].
Preparation of powders with the properties required to obtain aerosols using DPIs suitable for targeted drug delivery in another challenge. Of course, the powder grains must be smaller than the expected aerosol particle size, but this does not guarantee that all aerosol particles will be small enough, since micrometer-sized particles easily form permanent agglomerates. This is why inhalable powders are typically prepared as a mixture of fine grains of a drug with larger particles of an excipient (usually lactose). Such blends are more easily fluidized and deagglomerated than fine grains without the excipient, however the preparation of blends is also demanding, especially for drugs which contain more than one therapeutic substance [36]. Some powders can be engineered in a way to allow them to be aerosolized without lactose [37–39].
In contrast to liquid droplets, engineered powder particles can be of different shape and can also be porous, which can be used to maximize their local delivery to different regions of the RS. Programmed non-sphericity of particles can be used to obtain a better penetration, deposition, and functionality of inhaled drugs [40–42].
The above discussion shows that the optimal aerosol properties are defined by the target of drug delivery which, therefore, also influences the choice of method/device for generating particles of a given size range. Below two targets and the corresponding drug delivery devices will be presented.
3.1. Drug targeting to the lower respiratory system
Several types of inhalation devices are typically used to generate and target medical aerosol to the lower RS. The three most used are: pressurized metered dose inhalers (pMDIs), dry powder inhalers (DPIs), and nebulizers, but other designs of inhalers are also present in the market (
Table 1). Each class of these devices can be subdivided in additional subtypes.
Medical aerosols targeted to RS should be inhaled through the mouth to reduce deposition of the drug in the upper airways (extrathoracic region). However, aerosolized therapeutics are also delivered to the lungs through the nose using inhalation masks, which are useful when aerosol administration through the mouthpiece is not possible or ineffective (e.g., small children, disabled or uncooperative patients). Transnasal administration can also be performed during oxygen supplementation using a high-flow nasal cannula (HFNC), when oxygen-enriched air is used to carry the aerosol which is preferably delivered from a nebulizer with a low internal flow, such as VMN [43,44].
Table 1.
Types of inhaling devices and systems for aerosol drug delivery to the lower airways.
Table 1.
Types of inhaling devices and systems for aerosol drug delivery to the lower airways.
Pressurized metered
dose inhalers (pMDIs) |
Dry powder inhalers (DPIs) |
Nebulizers |
Other (examples) |
| 1. Hand-actuated |
1. Single dose (capsule) |
1. Pneumatic (jet) |
Soft mist inhaler
(Respimat® SMI) [31] |
| 2. Breath-actuated (mechanical) [45,46] |
2. Containing pre-metered doses (on blister) |
2. Ultrasonic
|
Thermal vaporization
(sublimation/resublimation) breath actuated inhaler
(Staccato®) [47] |
| Cab be used both with or without holding chamber (or spacer) |
3. Metering the dose from powder reservoir |
|
|
Only nebulizers and HFNC systems allow patients to inhale aerosol with spontaneous (i.e., not forced) breathing, which makes these inhaling devices the most versatile. In other cases, i.e., when the inhalation is restricted by external resistance of the inhaler and requires the additional inspiratory effort of a patient, the flow function
Q(t) (also:
PIFR and
AFR – see
Figure 2) will be different. During inhalation the lungs must adapt to the inhaling device. This process can be understood as the achieving the duty point of the pump, where the actual flow rate
Q and the corresponding pressure drop in the system, Δ
P, depend both on the pump capacity (here: lungs capacity) and the external resistance (here: the inhaler). In other words, the actual airflow rate depends on the internal aerodynamic resistance of the inhaler, as the mechanical capacity of the lungs is only partly adjustable to the flow restrictions. This shows that the frequently used PIFR value, which is measured under arbitrary conditions, can be misleading because it is not obtained with all inhalers with different resistance. It is especially important in DPIs, where the air must be drawn forcefully through the device to assure the required powder aerosolization.
DPIs are classified to low-, medium-, and high-resistant devices based on the value of intrinsic aerodynamic resistance
RD, defined as:
and some high-resistant DPIs are not appropriate for patients with a compromised lung mechanics. Also, in pMDIs patients should adapt to the special breathing maneuver, i.e., slow and deep inhalation followed by breath-hold [48]. Therefore, the inhalation curve shown schematically in
Figure 3 is applicable only to nebulizers, which have low resistance and can be used with spontaneous breathing.
3.2. Drug targetting to the nasal cavity.
Topical delivery of medicines to the surface of the nasal cavity is important since almost a quarter of the population suffers from allergic rhinitis [49], requiring the use of the locally acting decongestants and anti-inflammatory drugs. These medicines in the form of nasal drops are not comfortable to use and often run down the throat, causing irritation. Aerosols appear more convenient and effective in the homogeneous delivering drugs to the nasal cavity, however due to the narrow and tortuous nasal air passages, delivering medication to this region is difficult.
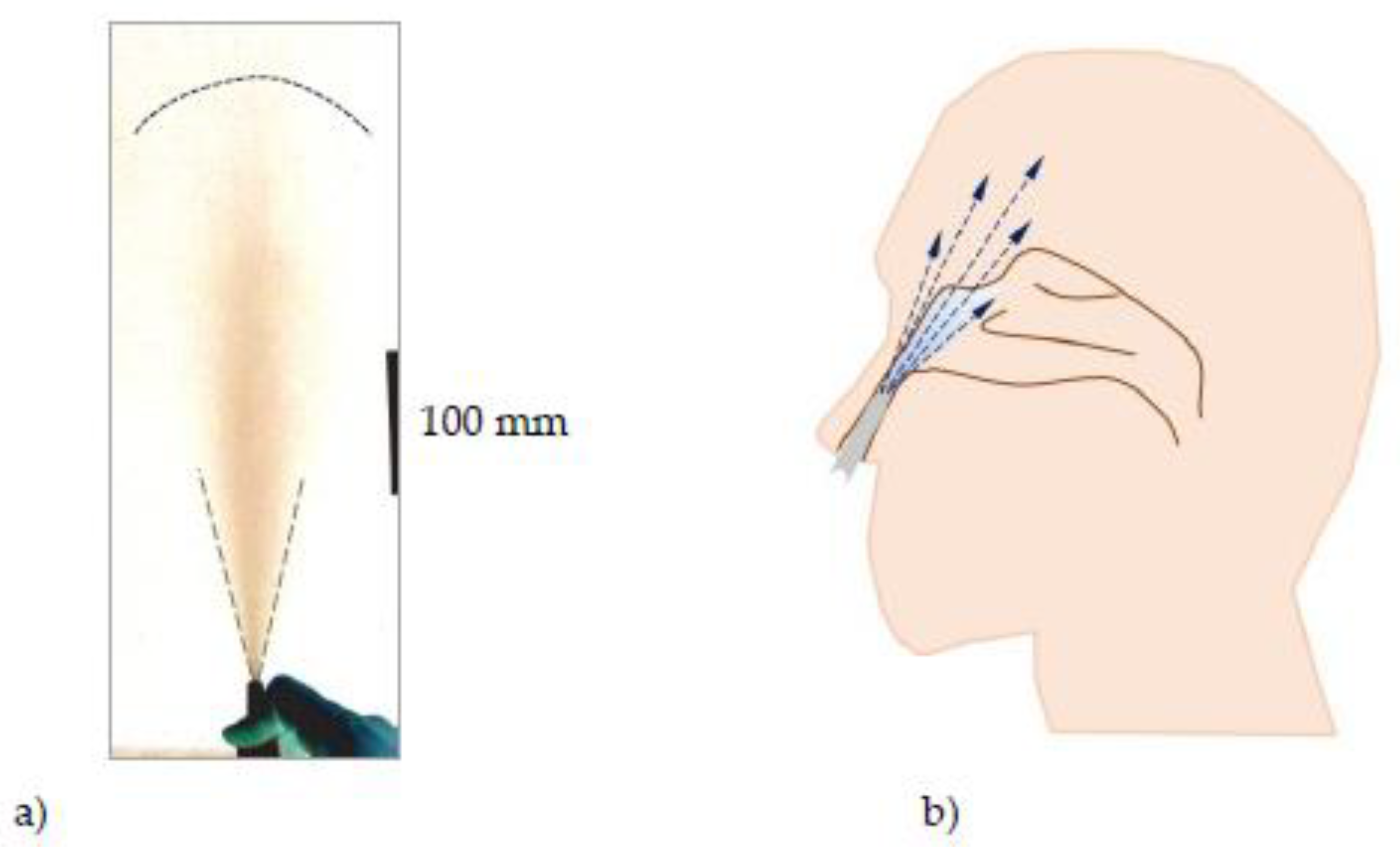
Drug delivery to the surface of the nasal cavity requires relatively large aerosol particles (30-80 μm) to avoid their penetration to the throat and lower RS. Generation of such aerosol can be easily done from liquids by atomization in hand-operated nasal pumps. The pressure applied on the liquid is low, but enough to produce droplets of the required size. However, as in all atomization processes, a small volume of liquid is converted to a large volume of gas-liquid system, i.e., aerosol. A well-dispersed aerosol plume of droplets ejected from the atomizer nozzle is up to hundreds of millimeters in length and up to 100 mm in width, depending on liquid properties and nozzle design [50,51], which makes if incompatible with nasal geometry,
Figure 6. Therefore, after placing the atomizer tip inside the nostril, the plume cannot evolve, and the ejected liquid is deposited on the nearby surfaces of the nasal sidewall and nasal septum [50]. Under such conditions, an even drug distribution in the whole nasal cavity is not possible. This situation is different compared to the free penetration through the nasal geometry of aerosol inhaled from nebulizers.
Since drugs aerosolized in nasal pumps cannot be direct delivered to all parts of the nasal cavity, the pharmaceutical effects observed after drug application needs additional explanation. It can be provided by the gravitational runoff of deposited liquid, as well as liquid spreading to deeper parts of the nose caused by the aerodynamic interactions between the inhaled air and the liquid layer of drug deposited in the front of the nose [50,52]. The kinetics of such translocation of the liquid drug depends on its rheological properties [53], the deposited volume, and probably also on the other factors such as wetting/adhesion forces. It was also confirmed that high velocity of airflow caused by intense drawing the air through the nose in a natural reflex to prevent drug drainage, significantly improves the spread of the drug into the deeper regions of the nasal cavity [50].
Intranasal administration of drugs as aerosols becomes more difficult in cases of airway obstruction caused by anatomical abnormalities (obturation, deviated nasal septum, polyps). In such situations, aerosols administered as relatively large droplets sprayed from a nasal pump are even less effective. Some concepts of using acoustic vibrations have been proposed to enhance aerosol penetration in congested or partly blocked nasal airways [54]. In this application, the aerosol droplets are finer, which allows them to be carried with the air along the nasal air passages. Due to the additional pressure wave, they are deposited on the walls of the nose and do not penetrate to the deeper structures of RS [55,56].
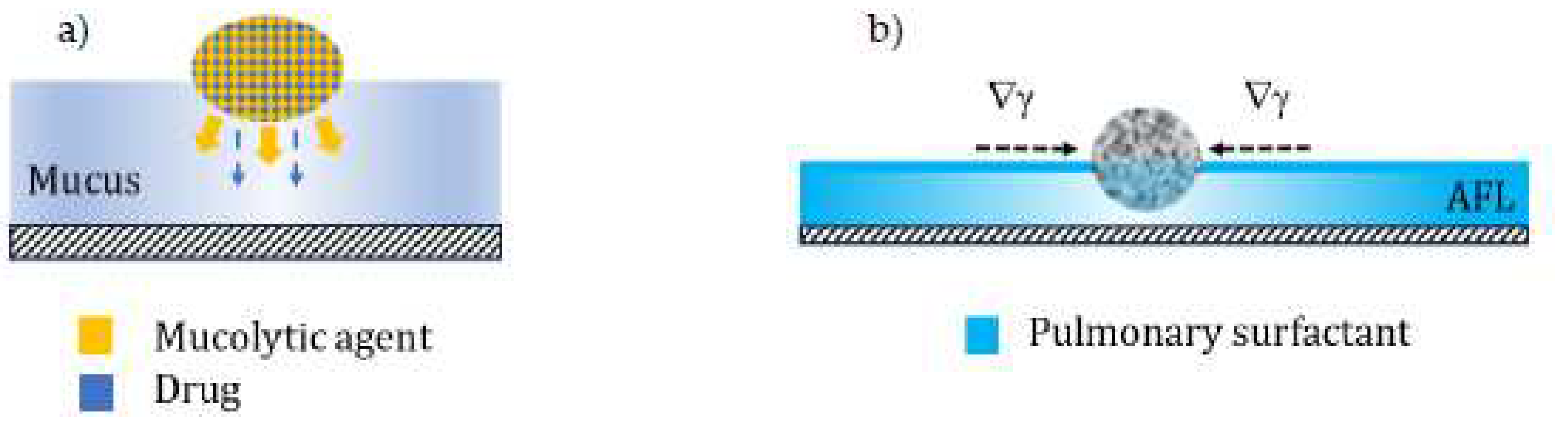
4. Particle-lung interaction and the mass transfer after drug deposition
The process of delivering an aerosol drug involves its deposition on the surface of the respiratory system and subsequent interaction with this surface. The surface of RS is covered by fluids that act as a protective barrier function, and these are mucus in the bronchial tree or pulmonary surfactant in the alveolar region. The composition and physicochemical properties of these fluids very often determine the bioavailability or safety of a given drug, but also help to develop the most favorable formulation. These may include, for instance, multicomponent composite particles, where one component (mucolytic agent, e.g., N-acetylcysteine) interracts with viscous mucus, causing its local thinning and facilitating diffusion of the second (therapeutic) component [57,58], or particles with mucoadhesive properties that extend the residence time of the drug on the bronchial surface [59]. Many drug particles are soluble in the liquid covering the lung surface, however, the use of poorly soluble engineered particles (e.g., porous, nanostructured) can also be considered attractive. The porosity of the particles allows to obtain effects of a controlled reduction of the natural defense mechanisms on the alveolar level, prolonging the residence time of particles deposited in this area. This action is related to the presence of the pulmonary surfactant (PS) in the alveolar fluid layer (AFL), which contributes to the local clearance both through hydrodynamic processes associated with Marangoni effects [60,61], and by direct stimulation of alveolar macrophages [62,63].
It was proposed that decrease of the surfactant concentration and its surface activity observed due to PS adsorption on porous particles (with a large surface area) can slowdown these natural defense mechanisms [64]. Both concepts, which can be adapted to increase the rate of drug delivery from aerosol drug carriers deposited in the RS, are schematically shown in
Figure 7.
5. Selected concepts and methods of improvement of targeted aerosol delivery to different regions in the respiratory system
When analyzing aerosol generation methods, it is clear that the ability to tailor particle size distribution is one of the most important ways to maximize the amount of drug targeted to different regions of the RS. This factor also decides on possible side effects and drug loses. Therefore, this section discusses options for controlling particle size and maximizing inhalation dose, focusing mainly on nebulizers as aerosol delivery devices.
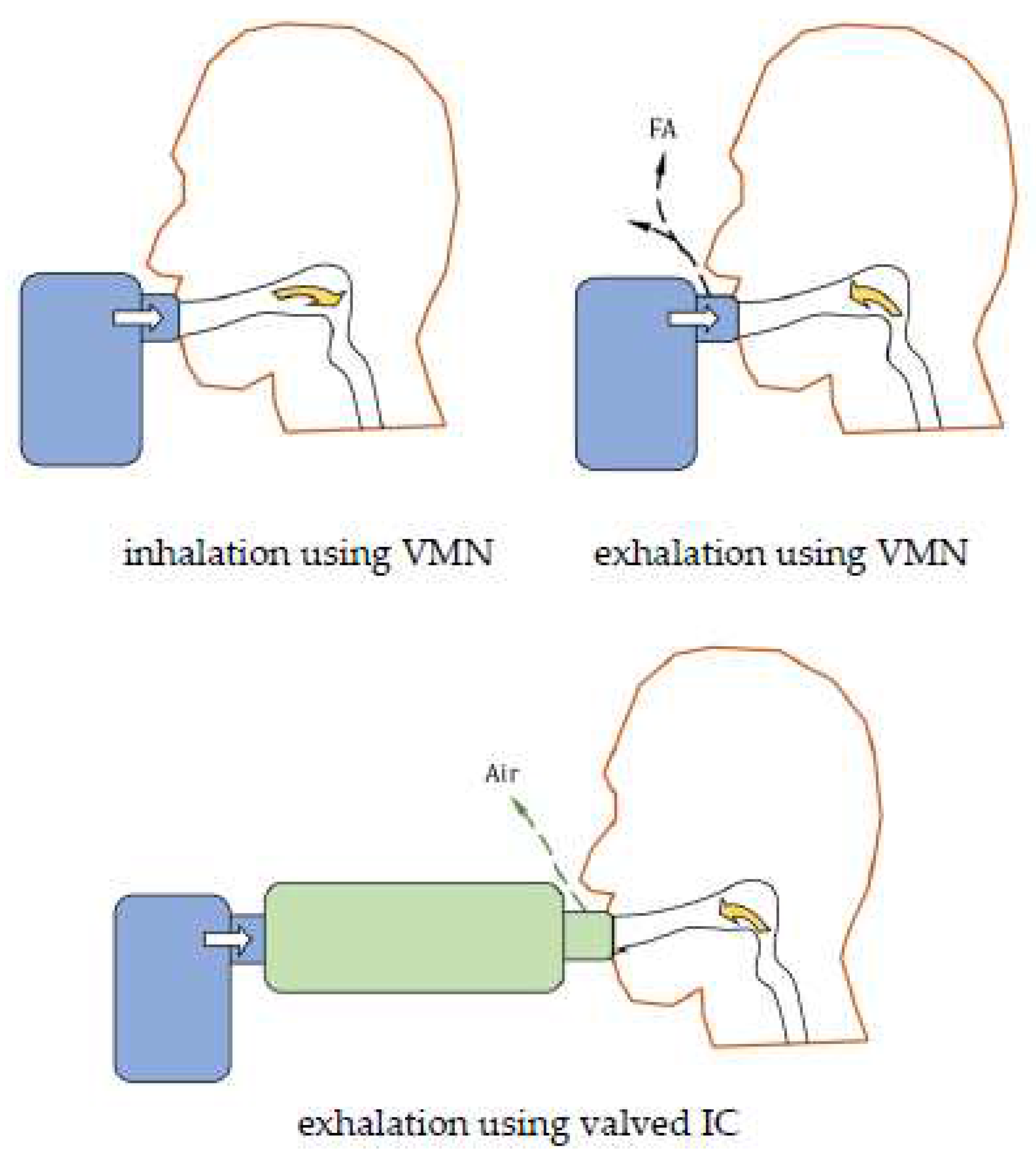
5.1. Nebulizer with a valved inhalation chamber
In continuously operating (constant output) nebulizers, a part of the drug is lost as, so-called, fugitive aerosol, emitted during the exhalation phase, i.e., when it cannot be taken up by the patient [65]. To prevent this, the use of an inhalation chamber (IC), a simple device widely used with pMDI inhalers, has been proposed [66]. The IC connected to the nebulizer provides a holding space for the aerosol produced during exhalation and breath-hold, allowing it to be absorbed by patient in the consecutive inhalation,
Figure 8. Despite a loss of aerosol due to inertial and gravitational deposition in the IC, the effective availability of the drug to the patient is greater compared to the nebulizer without the chamber. This concept is particularly applicable to VMNs, which are typically not equipped with any valves which can minimize the fugitive emission.
The idea of using valved IC as a universal add-on device to any VMN was inspired by the Aerogen® Ultra nebulizing system, in which the Aerogen® Solo VMN was connected to an accessory that allowed this small VMN to be conveniently used as a handheld nebulizer [67,68]. Studies of the operation of the Intec Twister Mesh VMN nebulizer [67] (the nebulizer on Polish market with a design analogous to Aura Portable Nebulizer available in the US [70]) connected to the valved IC showed that the amount of aerosol taken by the patient increases almost 1.75-fold. In addition, the aerosol leaving the IC has a more favorable particle size distribution, because mainly largest droplets are deposited inside the chamber, allowing to increase the fine particle fraction (FPF). The increase in the amount of aerosol delivered with droplets smaller in the 5 μm is 2.8-fold as compared to aerosol delivered without the valved IC [66]. A recent study with another VMN nebulizer (Intec Turbo Mesh [71]) for many drugs (glucocorticosteroids, anticholinergics, short- and long-acting β2-mimetics: SABA and LABA, mucolytics) showed that the increase in the availability of fine droplets is between 16% (SABA) through 130-170% (glucocorticosteroids) to 190% (anticholinergics) [72]. Decreasing the mass of large droplets in inhaled aerosol should bring additional benefits to the patient, i.e., the reduction of local (oropharyngeal) side effects. Overall, it seems that the proposed concept is likely to improve the effectiveness of inhalation treatment and drug targeting to the lower RS using constant-output nebulizers, particularly VMNs.
5.2. Adjusting aerosol droplet size by physicochemical and process parameters of nebulization.
In general, the size of aerosol droplets formed in the nebulizer can be altered by the proper designing the atomizing system and adjusting process conditions. The pressure of air used to atomize drugs in a particular model of nebulizing system (compressor + dedicated nebulizing vessel) is constant. However, even for the constant pressure there is a possibility to adjust the droplet size by tuning the inner geometry of the nebulizing vessel. A few commercially available jet nebulizers can produce droplets of different sizes after changing the internal geometry of the atomization system, e.g., by replacing a plastic element, which alters the distance between the nozzle and impaction baffle [73,74]. Increasing the diameter of the droplets allows to increase the dose delivered to the upper parts of RS, e.g., in the case of throat infections or croup (laryngotracheitis) [75].
Droplet size can also be modified by changing the physicochemical properties of the liquid, including the viscosity (or more generally: rheological properties), surface tension, and, sometimes, ionic strength [76–79]. In the case of inhalation drugs, this can potentially be achieved by using proper (e.g., classified as GRAS – generally recognized as safe) drug additives, such as biosurfactants or viscosity modifiers of natural origin [80]. It is worth noting some of that these substances (biosurfactants) can also be candidates for replacing synthetic adjuvants of inhalation drugs, such as Polysorbat 80 [81].
Several studies have reported that after thickening the aqueous solution, smaller aerosol droplets are generated in a pneumatic nebulizer [76,77]. Despite a reduced emission efficiency, increasing the liquid viscosity by additives should allow the drug to be better targeted to the periphery of the lungs. Since droplets can penetrate to the alveoli, it was also important to see that several proposed natural thickeners (sodium hyaluronate, xanthan gum, and agar) do not compromise PS function (in vitro studies [82]). The decrease in the mass median aerodynamic diameter (MMAD) of aerosol nebulized from liquids with higher viscosity may seem surprising but is easily explained based on analysis of the aerosol formation process in a pneumatic nebulizer. The increase in droplet size during primary atomization in the two-fluid (pneumatic) nozzle leads to their stronger impaction on the baffles and secondary atomization, associated with the formation of smaller droplets. This is more intense for viscous liquids (larger primary droplets) than for liquids with lower viscosity, hence a shift in the droplet size distribution toward smaller diameters is observed after increasing the viscosity.
The situation is different in the ultrasonic nebulizers, both classical and VMN. In the case of Newtonian liquids, the mass of very fine droplets decreases when viscosity increases, which, however, does not necessarily imply a decrease in the value of the volumetric median diameter Dv50, since a simultaneous decrease of the mode of the distribution is observed [83]. On the other hand, in the case of non-Newtonian fluids, additional submicron droplets appear in the aerosol, formed as satellites from the breakdown of droplets generated from the ultrasonic fountain, which results in the decrease in Dv50. Very viscous liquids are not atomized at all in ultrasonic nebulizers [77], which requires to use only pneumatic devices for their nebulization. It has been also shown that in addition to shear (dynamic) viscosity, dilatational (second) viscosity of the liquid also plays a role in the droplet formation in ultrasonic devices [83].
Biosurfactants, by reducing the surface tension, cause a decrease in the size of droplets emitted from pneumatic nebulizers due to the generation of a greater number of small droplets during the primary atomization. These droplets are small enough to avoid inertial collisions with the baffles of the nebulizing vessel and directly pass into the emitted aerosol. Increase in the FPF in the aerosol allow a better targeting of lower RS. However, an undesirable effect of the presence of surface-active compounds is foaming of the liquid in the nebulizing vessel. It reduces the aerosol emission rate, since the nozzle is fed with a mixture of liquid and gas (i.e., foam) instead of liquid. Foaming also increases the so-called residual volume (the amount of liquid remaining inside the nebulizer at the end of nebulization), since the liquid is embedded in the foam that sticks to the walls of the vessel.
The ionic strength of the solution, which can be adjusted by adding electrolytes, also affects the size of aerosol droplets, but only in VMN nebulizers with a metal membrane. The effect is attributed to ionic interactions near the vibrating membrane [78], and may be important e.g., during nebulization of hypertonic saline.
Physicochemical properties of the liquid also depend on temperature, which is, therefore, another parameter influencing the droplet size distribution and possibility of drug targeting in RS. In all nebulizers, the change in liquid temperature can be caused by thermal effects related to the operation of the nebulizer itself. The liquid is typically cooled in pneumatic devices due to adiabatic evaporation and is heated in classical ultrasonic nebulizers due to the energy provided from the vibrating piezoelectric crystal. It means that droplet size hence the efficiency of drug delivery, will be different in the beginning of inhalation and after several minutes of the treatment [84]. The smallest changes in temperature, and thus the minor effect on droplet size, are observed in VMN nebulizers.
Evaporation of water (solvent) also increases the concentration of the sprayed solution in the systems where the liquid drains to the vessel (pneumatic and classic ultrasonic nebulizers). Both changes in temperature and concentration in time alter the size distribution of aerosol droplets released during a nebulization process, and this factor should also be taken into account when discussing the possibilities of targeting of inhaled drugs using nebulizers. The temperature can also be intentionally set to a higher level by thermostatting the nebulizer to obtain a desired droplet size distribution. For instance, it was shown that Dv50 of nebulized saline in a selected nebulizer can be reduced from 5.23 μm at 20 °C to 4.23 μm by heating the liquid to 35 °C (thermo-aerosol) [85].
There is also another option for adjusting droplet size of inhaled wet aerosol based on thermodynamic effects in the aerosol phase. The mist released from nebulizer can be diluted in the mouthpiece or mask, i.e., before entering the mouth, with intentionally added dry and warm air This leads to a reduction in droplet size due to water evaporation and allows to obtain a higher dose potentially delivered to the lower RS. As confirmed both by CFD computations and experiments [86], the effect can be adjusted by air humidity and temperature, but also by the mixing ratio between the wet aerosol and the auxiliary air. This concept was also confirmed in invasive ventilation where dry air allowed to reduce the MMAD of inhaled droplets from above 4 μm to below 2 μm, improving drug deposition in lung periphery [87].
5.3. Targetted drug delivery by functionalized particles and non-conventional therapeutics
In addition to the common techniques for delivering drugs by aerosol inhalation, several innovative concepts need to be noted. An interesting possibility for targeted drug delivery is the use of magnetic particles that can be attracted to disease areas in the lungs under the influence of an external magnetic field [88,89]. Despite a more complicated preparation of suitable drug carriers, the method offers a novel and attractive way of effective targeting tumors in lung cancer [90,91].
Aerosol therapy can be used not only with pharmaceuticals, but also other agents that show the therapeutic effects in the lungs. For example, aerosol gene therapy has been proposed for several pulmonary diseases [92], including cystic fibrosis [93,94] and lung cancer [95,96]. Inhalation of aerosolized immunotherapeutics and monoclonal antibodies was also proposed in anticancer therapy of the RS [97,98]. Inhaled bacteriophage aerosol has been considered as an alternative to inhaled antibiotics in pulmonary infections [92]. Some attempts have been also done in the field of inhalation of living cells [99], including the aerosol delivery of stem cells in COVID-19 treatment [100]. All these innovative concepts still require optimization of the aerosolization technique to ensure that sensitive biomolecules are not damaged due to the high stresses encountered during atomization.
5.4. Better aerosol targetting using electronic technologies, smart inhalers, and artificial intelligence solutions
A significant change in the effectiveness of aerosol therapy is expected from new electronically assisted solutions implemented in ‘smart inhalers’ [101,102]. Many of these devices are designed to help patients take their medications regularly and keep the patient and doctor informed about medication intake, which is essential for proper control of the therapy. Most noteworthy, however, are solutions that improve the handling and operation of the inhaler for optimal aerosol generation and inhalation, hence a better controlled regional delivery of inhaled drugs. Some of these systems benefit from machine learning algorithms, resulting in the application of artificial intelligence (AI), which is expected to significantly improve the outcome of the therapy [103].
Even before the era of smart inhalers, mechanical systems were developed which were able to activate a pMDI only when the minimal inspiratory flow required to trigger a dose was achieved. For example, Easi-Breathe
® or Autohaler
® systems helped eliminate coordination errors in pMDI inhalers [45,46]. Nowadays, the use of electronic sensors along with digital analysis of the measured signals (pressure, airflow changes) has allowed further advances in this field. As an example, the Adaptive Aerosol Delivery (ADD
®) system is based on analysis of the patient's breathing pattern during nebulizer use and then adjusting the aerosol release only during the first phase of inspiration, eliminating the problem of drug waste and fugitive emission [104]. By proper timing of aerosol release it also allows to better target lower RS. Analogous sensor systems along with software were developed for DPI inhalers [105], where inhalation dynamics is known to be crucial for generating an aerosol dose with the desired PSD [86]. The number of smart devices and sensors currently available on the market is substantial (refer, e.g., to [106,107] for a more comprehensive data), so only a few most popular systems are listed in
Table 2. Most of them have a module enabling a wireless communication with mobile phone applications which makes them even more convenient to use by patients. Some systems focus on improving aerosol delivery to the lower part of the RS (e.g., Group 1), while others mainly serve to monitor proper use of the device without analyzing factors affecting actual aerosol delivery (e.g., sensors in Group 2). It can be expected that new capabilities of smart inhalers will be linked to the use of artificial intelligence (AI) algorithms for faster and better adjustment of optimal inhalation conditions based on the large amount of data collected from the population.
6. Conclusions and future directions
The targeted delivery of drugs through the inhalation of aerosols is challenging. Its effectiveness is influenced by (i) the method of generation of aerosol with suitable properties for penetration to a specific level of the respiratory system, (ii) individual patient characteristics (respiratory tract geometry, inhalation technique), and (iii) the patient’s ability to operate a given aerosol delivery device. It means that even when aerosol with the desired properties is potentially available, its deposition in the areas requiring treatment is not assured due to patient-related factors.
This paper discussed the key factors responsible for the targeted delivery of inhaled aerosol drugs, emphasizing both the importance of non-steadiness of airflow through the inhaler and respiratory airways, and the limitations in the prediction of deposition resulting from common simplifications in in silico and in vitro modeling. It was shown that other factors, such as the choice of drug delivery device and appropriate development of the properties/composition of the drug carrier particles, can affect the fate of inhaled therapeutic agents.
Both physicochemical and physiological constraints do not allow to obtain perfect targeting of inhaled aerosols without drug losses, however the regional delivery can be optimized. Several possible strategies to improve the effectiveness of drug delivery to specific areas, such as the lower respiratory tract or nasal cavity, were highlighted. Some possible solutions are based on controlling aerosol droplet size generated in nebulizers by altering the physicochemical properties of liquid drugs, using the inhalation chamber as an add-on device, or diluting the aerosol with external air before its entrance to the RS. For aerosol directed into the nasal cavity, an attractive option is to use pulsed mist delivered from a nebulizer instead of using rather ineffective delivery of large aerosol droplets sprayed from a nasal pump. Much is also expected from modern electronic systems implemented in smart inhalers, which are increasingly based on the use of artificial intelligence. The concepts presented in the paper indicate only some possible approaches to improved targeted delivery of inhaled aerosol drugs, which still requires further intensive research and effective development of practical solutions.
Funding
This research was funded by National Science Center (Poland), grant number 2018/29/B/ST8/00273.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in this article.
Acknowledgments
The author thanks Kazunori Kadota, PhD from Osaka Medical and Pharmaceutical University (Japan) for sharing the data of tracheobronchial geometry.
Conflicts of Interest
The author declares no conflict of interest.
References
- Sanders, M. Inhalation therapy: an historical review. Prim. Care Respir. J. 2007, 16, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Stein, S.W.; Thiel, C.G. The history of therapeutic aerosols: a chronological review. J. Aerosol Med. Pulm. Drug Deliv. 2017, 30, 20–41. [Google Scholar] [CrossRef] [PubMed]
- Maccarone, C.; Masiero, S. Spa therapy interventions for post respiratory rehabilitation in COVID-19 subjects: does the review of recent evidence suggest a role? Environ. Sci. Pollut. Res. 2021, 28, 46063–46066. [Google Scholar] [CrossRef] [PubMed]
- Kostrzon, M.; Sliwka, A.; Wloch, T.; Szpunar, M.; Ankowska, D.; Nowobilski, R. Subterranean pulmonary rehabilitation in chronic obstructive pulmonary disease. Adv. Exp. Med. Biol. 2019, 1176, 35–46. [Google Scholar] [CrossRef]
- Zając, D.; Russjan, E.; Kostrzon, M.; Kaczyńska, K. Inhalations with brine solution from the 'Wieliczka' salt mine diminish airway hyperreactivity and inflammation in a murine model of non-atopic asthma. Int. J. Mol. Sci. 2020, 21(13), 4798. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, R.R.; Das, S. Inhaled insulin - current direction of insulin research. J. Clin. Diagn. Res. 2017, 11, OE01–OE02. [Google Scholar] [CrossRef] [PubMed]
- Klonoff, D.C. Afrezza inhaled insulin: the fastest-acting FDA-approved insulin on the market has favorable properties. J. Diabetes Sci. Technol. 2014, 8, 1071–1073. [Google Scholar] [CrossRef] [PubMed]
- Osowicka, M.; Janowiak, P.; Gorzewska, A.; Lichodziejewska-Niemierko, M. Inhaled opioids for cancer pain relief: A narrative review. Medicine 2022, 101, e28921. [Google Scholar] [CrossRef] [PubMed]
- de Berardis, D.; Fornaro, M.; Orsolini, L.; et al. The role of inhaled loxapine in the treatment of acute agitation in patients with psychiatric disorders: a clinical review. Int. J. Mol. Sci. 2017, 18, 349. [Google Scholar] [CrossRef]
- Glenardi, G.; Handayani, T.; Barus, J.; Mangkuliguna, G. Inhaled levodopa (CVT-301) for the treatment of Parkinson disease. A systematic review and meta-analysis of randomized controlled trials. Neurol. Clin. Pract. 2022, 12, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Miragoli M, Ceriotti P, Iafisco M; et al. Inhalation of peptide-loaded nanoparticles improves heart failure. Sci. Transl. Med. 2018, 10, eaan6205. [Google Scholar] [CrossRef]
- Cheng, Y.S. Mechanisms of pharmaceutical aerosol deposition in the respiratory tract. AAPS PharmSciTech. 2014, 15, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, W. Modelling inhaled particle deposition in the human lung—a review. J. Aerosol Sci. 2011, 42, 693–724. [Google Scholar] [CrossRef]
- Longest, P.W.; Holbrook, L.T. In silico models of aerosol delivery to the respiratory tract - Development and applications. Adv. Drug Del. Rev. 2012, 64, 296–311. [Google Scholar] [CrossRef]
- Mutuku, J.K.; Hou, W.-C.; Chen, W.-H. An overview of experiments and numerical simulations on airflow and aerosols deposition in human airways and the role of bioaerosol motion in COVID-19 transmission. Aerosol Air Quality Res. 2020, 20, 1172–1196. [Google Scholar] [CrossRef]
- Miravitlles, K.; Auladell-Rispau, A.; Monteagudo, M.; Vázquez-Niebla, J.C.; Mohammed, J.; Nuñez, A.; Urrútia, G. Systematic review on long-term adverse effects of inhaled corticosteroids in the treatment of COPD. Eur. Respir. Rev. 2021, 30, 210075. [Google Scholar] [CrossRef]
- MPPD: Multiple-Path Particle Dosimetry Model (MPPD v 3.04), Applied Research Associates, Inc. Available online: https://www.ara.com/mppd/ (accessed on 28.11.2023).
- Sonnenberg, A.H.; Taylor, E.; Mondoñedo, J.R. , et al. Breath hold facilitates targeted deposition of aerosolized droplets in a 3D printed bifurcating airway tree. Ann. Biomed. Eng. 2021, 49, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Khajeh-Hosseini-Dalasm, N.; Longest, P.W. Deposition of particles in the alveolar airways: inhalation and breath-hold with pharmaceutical aerosols. J. Aerosol Sci. 2015, 79, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, T.R.; Moskal, A.; Gradoń, L. Dynamics of oro-pharyngeal aerosol transport and deposition with the realistic flow pattern. Inhalation Toxicol. 2006, 18, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Kleinstreuer, C.; Zhang, Z. Particle deposition in the human tracheobronchial airways due to transient inspiratory flow patterns. J. Aerosol. Sci. 2007, 38, 625–644. [Google Scholar] [CrossRef]
- Se, C.M.K.; Inthavong, K.; Tu, J. Unsteady particle deposition in a human nasal cavity during inhalation. J. Comput. Multiphase Flows 2010, 2, 207–218. [Google Scholar] [CrossRef]
- Naseri, A.; Shaghaghian, S. , Abouali, O.; Ahmadi, G. Numerical investigation of transient transport and deposition of microparticles under unsteady inspiratory flow in human upper airways. Respir. Physiol. Neurobiol. 2017, 244, 56–72. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Moskal, A.; Gradoń, L. Mechanims of aerosol particle deposition in the oro-pharynx under non-steady airflow. Ann. Occup. Hyg. 2007, 51, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Moskal, A; Gradoń, L. Temporary and spatial deposition of aerosol particles in the upper human airways during breathing cycle. J. Aerosol Sci. 2002, 33, 1525–1539. [Google Scholar] [CrossRef]
- Lin, C.L.; Tawhai, M.H.; McLennan, G.; Hoffman, E.A. Characteristics of the turbulent laryngeal jet and its effect on airflow in the human intra-thoracic airways. Respir. Physiol. Neurobiol. 2007, 157, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Xi, J.; Longest, P.W; Martonen, T.B. Effects of the laryngeal jet on nano- and microparticle transport and deposition in an approximate model of the upper tracheobronchial airways. J. Appl. Physiol. 2008, 104, 1761–1777. [Google Scholar] [CrossRef] [PubMed]
- Gaddam, M.G.; Santhanakrishnan, A. Effects of varying inhalation duration and respiratory rate on human airway flow. Fluids 2021, 6, 221. [Google Scholar] [CrossRef]
- Kadota, K.; Matsumoto, K.; Uchiyama, H. , et al. In silico evaluation of particle transport and deposition in the airways of individual patients with chronic obstructive pulmonary disease. Eur. J. Pharm. Biopharm. 2022, 174, 10–19. [Google Scholar] [CrossRef]
- Wiedmann, T.S.; Ravichandran, A. Ultrasonic nebulization system for respiratory drug delivery. Pharm. Dev. Technol. 2001, 6, 83–89. [Google Scholar] [CrossRef]
- Dalby, R.; Spallek, M.; Voshaar, T. A review of the development of Respimat Soft Mist Inhaler. Int. J. Pharm. 2004, 283, 1–9. [Google Scholar] [CrossRef]
- Ijsebaert, J.C.; Geerse, K.B.; Marijnissen, J.C.M.; Lammers, J.-W.J.; Zanen, P. Electro-hydrodynamic atomization of drug solutions for inhalation purposes. J. Appl. Physiol. 2001, 91, 2735–2741. [Google Scholar] [CrossRef]
- Qi, A.; Friend, J.R.; Yeo, L.Y.; et al. Miniature inhalation therapy platform using surface acoustic wave microfuidic atomization. Lab. Chip 2009, 9, 2184–2193. [Google Scholar] [CrossRef]
- Gac, J.; Sosnowski, T.R.; Gradoń, L. Turbulent flow energy for aerosolization of powder particles. J. Aerosol Sci. 2008, 39, 113–126. [Google Scholar] [CrossRef]
- Kamin, W.E.S.; Genz, T.; Roeder, S.; Scheuch, G.; Trammer, T.; Juenemann, R.; Cloes, R.M. Mass output and particle size distribution of glucocorticosteroids emitted from different inhalation devices depending on various inspiratory parameters. J. Aerosol Med. 2002, 15, 65–73. [Google Scholar] [CrossRef]
- Hejduk, A.; Urbańska, A.; Osiński, A.; Łukaszewicz, P.; Domański, M.; Sosnowski, T.R. Technical challenges in obtaining an optimized powder/DPI combination for inhalation delivery of a bi-component generic drug. J. Drug Deliv. Sci. Technol. 2018, 44, 406–414. [Google Scholar] [CrossRef]
- Cassidy, J.P.; Amin, N.; Marino, M.; et al. Insulin lung deposition and clearance following Technosphere® insulin inhalation powder administration. Pharm. Res. 2011, 28, 2157–2164. [Google Scholar] [CrossRef] [PubMed]
- Gradoń, L.; Sosnowski, T.R. Formation of particles for dry powder inhalers. Adv. Powder Technol. 2014, 25, 43–55. [Google Scholar] [CrossRef]
- Xia, Y.; Su, Y.; Wang, Q.; et al. Preparation, characterization, and pharmacodynamics of insulin-loaded fumaryl diketopiperazine microparticle dry powder inhalation. Drug Deliv. 2019, 26, 650–660. [Google Scholar] [CrossRef]
- Sturm, R. A computer model for the simulation of nonspherical particle dynamics in the human respiratory tract. Phys. Res. Int. 2012, 2012, e142756. [Google Scholar] [CrossRef]
- Shachar-Berman, L; Ostrovski, Y.; De Rosis, A.; Kassinos, S.; Sznitman, J. Transport of ellipsoid fibers in oscillatory shear flows: Implications for aerosol deposition in deep airways. Eur. J. Pharm. Sci. 2018, 113, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Shukla, S.K.; Sarode, A.; Kanabar, D.D.; Muth, A.; Kunda, N.K.; Mitragotri, S.; Gupta, V. Bioinspired particle engineering for non-invasive inhaled drug delivery to the lungs. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 128, 112324. [Google Scholar] [CrossRef]
- Li, J.; Fink, J.B.; MacLoughlin, R.; Dhand, R. A narrative review on trans-nasal pulmonary aerosol delivery. Crit. Care 2020, 24, 506. [Google Scholar] [CrossRef]
- Mac Giolla Eain, M.; MacLoughlin, R. In-Line Aerosol therapy via nasal cannula during adult and paediatric normal, obstructive, and restrictive breathing. Pharmaceutics 2023, 15, 2679. [Google Scholar] [CrossRef]
- Price, D.B.; Pearce, L.; Powell, S.R.; Shirley, J.; Sayers, M.K. Handling and acceptability of the Easi-Breathe device compared with a conventional metered dose inhaler by patients and practice nurses. Int. J. Clin. Pract. 1999, 53, 31–36. [Google Scholar] [CrossRef]
- Worth, H. A comparison of HFA-BDP Autohaler with budesonide Turbuhaler in asthma control of adult patients with mild to moderately severe disease. Respir Med. 2000, 94 Suppl D, S27–S30. [Google Scholar] [CrossRef]
- Dinh, K.; Myers, D.J.; Glazer, M.; et al. In vitro aerosol characterization of Staccato® Loxapine. Int. J. Pharm. 2011, 403, 101–108. [Google Scholar] [CrossRef]
- Laube, B.L.; Janssens, H.M.; de Jongh, F.H.C.; et al. What the pulmonary specialist should know about the new inhalation therapies. Eur. Resp. J. 2011, 37, 1308–1417. [Google Scholar] [CrossRef]
- Dykewicz, M.S.; Hamilos, D.L. Rhinitis and sinusitis. J. Allergy Clin. Immunol. 2010, 125 (2 Suppl 2), S103–S115. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Rapiejko, P.; Sova, J.; Dobrowolska, K. Impact of physicochemical properties of nasal spray products on drug deposition and transport in the pediatric nasal cavity model. Int. J. Pharm. 2020, 574, 118911. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, K.; Van Strien, J.; Singh, N.; Inthavong, K. Primary break-up and atomization characteristics of a nasal spray. PLoS One 2020, 15, e0236063. [Google Scholar] [CrossRef]
- Kolanjiyil, A.V.; Alfaifi, A.; Aladwani, G.; Golshahi, L.; Longest, W. Importance of spray-wall interaction and post-deposition liquid motion in the transport and delivery of pharmaceutical nasal sprays. Pharmaceutics 2022, 14, 956. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, T.R.; Dobrowolska, K. Aerodynamically driven translocation of non-Newtonian fluids: the relevance for intranasal drug delivery. Chem. Eng. Transact. 2021, 86, 1207–1212. [Google Scholar] [CrossRef]
- Möller, W.; Schuschnig, U.; Meyer, G.; Häussinger, K.; Keller, M.; Junge-Hülsing, B.; Mentzel, H. Ventilation and aerosolized drug delivery to the paranasal sinuses using pulsating airflow - a preliminary study. Rhinology 2009, 46, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Pari Sinus 2. Available online: https://www.pari.com/int/products/nose-and-nasal-sinuses/pari-sinus2-int/ (accessed on 19.11.2023).
- Florkiewicz, E.; Taff, J.; Taff, M.; Sosnowski, T.R. 2023. Process intensification in medical applications – use of vibroaerosols for enhanced drug delivery into the paranasal sinuses. In Abstracts of 8th European Conference of Process Intensification, Warsaw, Poland, 31.05-2.06.2023, page 38.
- Odziomek, M.; Sosnowski, T.R.; Gradoń, L. Conception, preparation and properties of functional carrier particles for pulmonary drug delivery. Int. J. Pharm. 2012, 433, 51–59. [Google Scholar] [CrossRef]
- Odziomek, M.; Sosnowski, T.R.; Gradoń, L. The influence of Functional Carrier Particles (FCPs) on the molecular transport rate through the reconstructed bronchial mucus - in vitro studies. Transp. Porous Media 2015, 106, 439–454. [Google Scholar] [CrossRef]
- Thakur, A.J.; Kaundle, B.; Singh, I. Mucoadhesive drug delivery systems in respiratory diseases. Targeting Chronic Inflammatory Lung Diseases Using Advanced Drug Delivery Systems, Dua, K.; Hansbro, P.N.; Wadhwa, R.; Haghi, L.; Pont, L.G.; Wiliams, K.A.,Eds., Academic Press, 2020, pp. 475-491. [CrossRef]
- Gradoń, L.; Podgórski, A. Hydrodynamical model of pulmonary clearance. Chem. Eng. Sci. 1989, 44, 741–749. [Google Scholar] [CrossRef]
- Sosnowski, T.R. Particles on the lung surface – physicochemical and hydrodynamic effects. Curr. Opin. Coll. Interf. Sci. 2018, 36, 1–9. [Google Scholar] [CrossRef]
- Agudelo, C.W.; Samaha, G.; Garcia-Arcos, I. Alveolar lipids in pulmonary disease. A review. Lipids Health Dis. 2020, 19, 122. [Google Scholar] [CrossRef] [PubMed]
- Gradoń, L.; Podgórski, A. Displacement of alveolar macrophages in air space of human lung. Med. Biol. Eng. Comput. 1995, 33, 575–581. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Gradoń, L.; Iskandar, F.; Okuyama, K. Interaction of deposited aerosol particles with the alveolar liquid layer. Optimization of Aerosol Drug Delivery, Gradoń, L.; Marijnissen, J., Eds., Kluwer Academic Publishers, Dordrecht, The Netherlands, 2003, pp. 205-216.
- Sosnowski, T.R.; Janeczek, K.; Grzywna, K.; Emeryk, A. Mass and volume balances of nebulization process for the determination of the expected dose of liquid medicines delivered by inhalation. Chem. Process. Eng. 2021, 47, 253–261. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Vilkotsky, A.I.; Emeryk, A. Vibrating mesh nebulizers with a valved inhalation chamber for increased drug delivery to the lower airways. Respiratory Drug Delivery 2022, Dalby, R.N., Peart, J.; Suman, J.D.; Young, P.M.; Traini, D.; Watts, A., Eds.; RDD Online, Richmond, VA, USA, 2022; Volume 1, pp. 551-554.
- Sarhan, R.M.; Elberry, A.A.; Abdelwahab, N.S.; Rabea, H.; Salem, M.N.; Abdelrahim, ME. Effect of a nebulizer holding chamber on aerosol delivery. Respir. Care 2018, 63, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Aerogen Ultra. Available online: https://www.aerogen.com/products/aerogen-ultra (accessed on 19.11.2023).
- IntecMedical. Available online: https://www.intecmedical.pl/inhalator-membranowy-siateczkowy-intec-twister-mesh.html (accessed on 19.11.2023).
- Auramedical. Available online: https://www.aura-medical.com/product/aura-portable-nebulizer/ (accessed on 19.11.2023).
- Intec Medical. Available online: https://www.intecmedical.pl/inhalator-membranowo-siateczkowy-turbo-mesh.html (accessed on 19.11.2023).
- Sosnowski, T.R. Mesh nebulizer with an inhalation chamber. Presented at 24th Conference of Allergologists, Pulmonologists and Clinical Immunologists, Lublin, Poland 8-10.09.2023 (unpublished).
- Pari. Available online: https://www.pari.com/int/inhalation-therapy/background-on-inhalation/ (accessed on 19.11.2023).
- Flaem. Available online: https://www.flaem.eu/en/products/aerosol-therapy-lower-airways/4neb (accessed on 19.11.2023).
- Petrocheilou, A.; Tanou, K.; Kalampouka, E.; Malakasioti, G.; Giannios, C.; Kaditis, A.G. Viral croup: diagnosis and a treatment algorithm. Pediatr. Pulmonol. 2014, 49, 421–429. [Google Scholar] [CrossRef] [PubMed]
- McCallion, O.N.M.; Taylor, K.M.G.; Thomas, M.; Taylor, A.J. Nebulization of fluids of different physicochemical properties with air-jet and ultrasonic nebulizers. Pharm. Res. 1995, 12, 1682–1688. [Google Scholar] [CrossRef]
- McCallion, O.N.M.; Patel, M.J. Viscosity effects on nebulisation of aqueous solutions. Int. J. Pharm. 1996, 130, 245–249. [Google Scholar] [CrossRef]
- Beck-Broichsitter, M.; Oesterheld, N. Electrolyte type and nozzle composition affect the process of vibrating membrane nebulization. Eur. J. Pharm. Biopharm. 2017, 119, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, M.; Oesterheld, N.; Knuedeler, M.-C.; Seeger, W.; Schmeh, I.T. On the correlation of output rate and aerodynamic characteristics in vibrating-mesh-based aqueous aerosol delivery. Int. J. Pharm. 2014, 461, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Dobrowolska, K.E., Kinowska, M., Sosnowski, T.R. Nebulization of solutions containing guar gum as a viscosity modifier of natural origin. Respiratory Drug Delivery 2022, Dalby, R.N., Peart, J.; Suman, J.D.; Young, P.M.; Traini, D.; Watts, A., Eds.; RDD Online, Richmond, VA, USA, 2022; Volume 1, pp. 541-544.
- Pulmicort Respules 0.5 mg. Available online: https://www.medicines.org.uk/emc/product/880/smpc (accessed on 28.11.2023).
- Dobrowolska, K.; Miros, M.; Sosnowski, T.R. Impact of natural-based viscosity modifiers of inhalation drugs on the dynamic surface properties of the pulmonary surfactant. Materials 2023, 16, 1975. [Google Scholar] [CrossRef] [PubMed]
- Broniarz-Press, L.; Sosnowski, T.R.; Matuszak, M.; Ochowiak, M.; Jabłczyńska, K. The effect of shear and extensional viscosities on atomization of Newtonian and non-Newtonian fluids in ultrasonic inhaler. Int. J. Pharm. 2015, 485, 41–49. [Google Scholar] [CrossRef]
- Ochowiak, M.; Kasperkowiak, A.; Doligalski, M.; et al. The thermostated medical jet nebulizer: aerosol characteristics. Int. J. Pharm. 2019, 567, 118475. [Google Scholar] [CrossRef]
- Steckel, H.; Eskandar, F. Factors affecting aerosol performance during nebulization with jet and ultrasonic nebulizers. Eur. J. Pharm. Sci. 2003, 19, 443–455. [Google Scholar] [CrossRef]
- Dorosz, A.; Moskal, A.; Sosnowski, T.R. Dynamics of aerosol generation and flow during inhalation for improved in vitro-in vivo correlation (IVIVC) of pulmonary medicines. Chem. Proc. Eng.: New Front. 2023, 44, e39. [Google Scholar] [CrossRef]
- Montigaud, Y.; Georges, Q.; Leclerc, L.; et al. Impact of gas humidification and nebulizer position under invasive ventilation: preclinical comparative study of regional aerosol deposition. Sci. Rep. 2023, 13, 11056. [Google Scholar] [CrossRef]
- Ostrovski, Y.; Hofemeier, P.; Sznitman, J. Augmenting regional and targeted delivery in the pulmonary acinus using magnetic particles. Int. J. Nanomedicine 2016, 11, 3385–3395. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, S.; Shamloo, A.; Alishiri, M.; Mofrad, Y.M.; Akherati, F. Targeted pulmonary drug delivery in coronavirus disease (COVID-19) therapy: A patient-specific in silico study based on magnetic nanoparticles-coated microcarriers adhesion. Int. J. Pharm. 2021, 609, 121133. [Google Scholar] [CrossRef] [PubMed]
- Dames, P.; Gleich, B.; Flemmer, A.; et al. Targeted delivery of magnetic aerosol droplets to the lung. Nat. Nanotechnol. 2007, 2, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Saadat, M.; Manshadi, M.K.D.; Mohammadi, M.; Zare, M.J.; Zarei, M.; Kamali, R.; Sanati-Nezhad, A. Magnetic particle targeting for diagnosis and therapy of lung cancers. J. Control. Release 2020, 328, 776–791. [Google Scholar] [CrossRef]
- Wang, X; Xie, Z. ; Zhao, J.; Zhu, Z.; Yang, C.; Liu, Y. Prospects of inhaled phage therapy for combatting pulmonary infections. Front. Cell. Infect. Microbiol. 2021, 11, 758392. [Google Scholar] [CrossRef]
- Bisserier, M.; Sun, X.-Q.; Fazal, S.; Turnbull, I.C.; Bonnet, S.; Hadri, L. Novel insights into the therapeutic potential of lung-targeted gene transfer in the most common respiratory diseases. Cells 2022, 11, 984. [Google Scholar] [CrossRef] [PubMed]
- Agent, P.; Parrott, H. Inhaled therapy in cystic fibrosis: agents, devices and regimens. Breathe (Sheff). 2015, 11, 110–118. [Google Scholar] [CrossRef]
- Rowe, S.M.; Zuckerman, J.B.; Dorgan, D.; et al. Inhaled mRNA therapy for treatment of cystic fibrosis: Interim results of a randomized, double-blind, placebo-controlled phase 1/2 clinical study. J. Cystic Fibr. 2023, 22, 656–664. [Google Scholar] [CrossRef]
- Zarogoulidis, P.; Darwiche, K.; Hohenforst-Schmidt, W.; Huang, H.; Li, Q.; Freitag, L.; Zarogoulidis, K. Inhaled gene therapy in lung cancer: proof-of-concept for nano-oncology and nanobiotechnology in the management of lung cancer. Future Oncol. 2013, 9, 1171–1794. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, M.; Muramatsu, N.; Matsunaga, W.; et al. Effects of inhalable gene transfection as a novel gene therapy for non-small cell lung cancer and malignant pleural mesothelioma. Sci. Rep. 2022, 12, 8634. [Google Scholar] [CrossRef]
- Storti, C.; Le Noci, V.; Sommariva, M.; Tagliabue, E.; Balsari, A.; Sfondrini, L. Aerosol delivery in the treatment of lung cancer. Curr. Cancer Drug Targ. 2015, 15, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, T.R.; Kurowska, A.; Butruk, B.; Jabłczyńska, K. Spraying of cell colloids in medical atomizers. Chem. Eng. Transact. 2013, 32, 2257–2262. [Google Scholar] [CrossRef]
- Torres Zambrano, G.M.; Maher Ahmed, Y.; Ventura Carmenate, Y.; et al. Stem cell nebulization therapy for COVID-19 infection: radiological and clinical outcomes. Egypt J. Radiol. Nucl. Med. 2021, 52, 115. [Google Scholar] [CrossRef]
- Kikidis, D.; Konstantinos, V.; Tzovaras, D.; Usmani, O.S. The digital asthma patient: the history and future of inhaler based health monitoring devices. J Aerosol Med. Pulm. Drug Deliv. 2016, 29, 219–232. [Google Scholar] [CrossRef]
- Mosnaim, G.S.; Greiwe, J.; Jariwala, S.P.; Pleasants, R.; Merchant, R. Digital inhalers and remote patient monitoring for asthma. J. Allergy Clin. Immunol. Pract. 2022, 10, 2525–2533. [Google Scholar] [CrossRef]
- Zhao, M.; Hoti, K.; Wang, H.; et al. Assessment of medication self-administration using artificial intelligence. Nat. Med. 2021, 27, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Denyer, J.; Dyche, T. The Adaptive Aerosol Delivery (AAD) technology: Past, present, and future. J. Aerosol Med. Pulm. Drug Deliv. 2010, 23 (Suppl 1), S1–S10. [Google Scholar] [CrossRef]
- Roszczyk, P.; Śrutek, M.; Wiśniewski, W.; et al. Capsule inhaler, method for monitoring intake of a substance, computer program and computer program product. Patent LU501909B1, granted 01.12.2022.
- Xiroudaki, S.; Schoubben, A.; Giovagnoli, S.; Rekkas, D.M. Dry Powder Inhalers in the digitalization era: current status and future perspectives. Pharmaceutics 2021, 13, 1455. [Google Scholar] [CrossRef]
- Häußermann, S.; Arendsen, L.J.; Pritchard, J.N. Smart dry powder inhalers and intelligent adherence management. Adv. Drug Deliv. Rev. 2022, 191, 114580. [Google Scholar] [CrossRef]
- I-neb AAD System. Battery-powered drug delivery device. Available online: https://www.philips.co.uk/healthcare/product/HC85167/i-neb-battery-powered-drug-delivery-system (accessed on 28.11.2023).
- Breelib Inhalation System. Available online: https://www.vectura.com/wp-content/uploads/2023/03/DAW-00058-08.pdf (accessed on 28.11.2023).
- AKITA® JET Inhalation System. Instructions for use. Available online: https://www.vectura.com/wp-content/uploads/2022/06/daw-00025-06.pdf (accessed on 28.11.2023).
- Fischer, A.; Stegemann, J.; Scheuch, G.; Siekmeier, R. Novel devices for individualized controlled inhalation can optimize aerosol therapy in efficacy, patient care and power of clinical trials. Eur. J. Med. Res. 2009, 14 (Suppl 4), 71–77. [Google Scholar] [CrossRef] [PubMed]
- Cipolla, D.; Chan., H.-K.; Schuster, J.; Farina, D. Personalized medicine: development of inhalation systems tailored to the individual. Ther. Deliv. 2010, 1, 667–682. [Google Scholar] [CrossRef]
- Komalla, V.; Wong, C.Y.J.; Sibum, I.; et al. Advances in soft mist inhalers. Expert Opin. Drug Deliv. 2023, 20, 1055–1070. [Google Scholar] [CrossRef]
- Hailie smart inhaler. Available online: https://www.hailie.com/ (accessed on 28.11.2023).
- Findair One add-on devices. Available online: https://findair.eu/products/findair-one-addons.html (accessed on 28.11.2023).
- Propeller Health. Available online: https://propellerhealth.com/our-platform/ (accessed on 28.11.2023).
- CapMedic - simplifying respiratory care by correct and regular inhaler use. Available online: https://capmedicinhaler.com/ (accessed on 28.11.2023).
- Amiko. Upgrading respiratory care with digital medicines. Available online: https://www.amiko.io/ (accessed on 28.11.2023).
- Digihaler. Available online: https://www.digihaler.com/ (accessed on 28.11.2023).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).