Introduction
Computed tomography (CT) has become a popular imaging modality for examining a wide range of disease processes, offering extensive clinical uses for both children and adults in emergency and routine diagnostic settings. Its widespread accessibility, affordability, speed, and relatively non-invasive nature make it popular over other sophisticated investigations like magnetic resonance imaging (MRI). Over the past few decades, advancements in image quality and the reliability and versatility of CT have led to its increased utilisation in clinical practice. Based on the findings of the United Nations Scientific Committee on Effects of Atomic Radiation (UNSCEAR), about 500,000 patients receive some form of CT examination daily (1). Despite the development of alternative imaging methods that abstain from ionising radiation, CT scans have displayed persistent growth globally. This leads to a significantly more effective radiation dose for the patient than other ionising radiation modalities.
Table I shows a comparison of estimated effective doses for commonly performed various types of CT examinations (2).
Table 1.
Comparison of estimated effective doses for commonly performed radiological examinations2.
Table 1.
Comparison of estimated effective doses for commonly performed radiological examinations2.
| Radiologic Examination |
Effective Dose (mSv) |
Range (mSv) |
| Chest radiography |
0.1 |
0.05–0.24 |
| Mammography |
0.4 |
0.1-0.7 |
| Head CT |
2 |
0.9–4.0 |
| Neck CT |
4 |
0.7–9.0 |
| Standard chest CT |
8 |
4.0–18.0 |
| Low-dose chest CT |
1.5 |
Variable |
| Coronary CT angiography |
15 |
7–39 |
| Abdominal CT |
10 |
3.5–25 |
| Pelvic CT |
8 |
3.3–10 |
| Multiphase abdominopelvic CT |
31 |
6–90 |
| Spine CT |
8 |
1.5–10 |
| CT colonography |
10 |
4.0–13.2 |
| Whole-body CT |
12 |
7–13.5 |
Ionising radiation is associated with risks to humans due to deterministic effects, which result in direct effects of high radiation, whereas stochastic effects occur by chance. In stochastic effects, there is no threshold point of radiation, and the cancer risk increases proportionate to the radiation dose. Exposure to >100 mSv of radiation over a lifetime is linked to a 1 in 200 chance of developing radiation-associated cancer (3). CT-related radiation is responsible for about 42% of the total collective effective dose arising from diagnostic radiology (1). A recent meta-analysis demonstrated a disproportionate increase in cancer risks from CT scans for adults, based on 111.6 million adult subjects from Asia, Europe, and America. It also showed the direct relationship between radiation dosage, body site where CT exposure was applied, and the likelihood of cancer risks (4). Therefore, numerous published scientific papers have discussed methods to reduce the lifetime total effective dose while preserving the diagnostic ability of the examination. One such strategy is to utilise low-dose CT (LD-CT) and ultralow-dose CT (ULD-CT) protocols, maintaining reasonably good diagnostic performances in many acute and non-acute medical and surgical conditions
Low-dose CT and ultralow-dose CT.
The fundamental principles of radiation protection in medical imaging include justification and optimisation. Justification involves ensuring that an examination is medically necessary. At the same time, optimisation emphasises the importance of minimising radiation doses in medical imaging while maintaining diagnostic accuracy, in alignment with the principle of “As Low As Reasonably Achievable” (ALARA). Behavioural and technical factors are important in reducing effective doses for the patient. Behavioural factors involve actions and practices undertaken by healthcare professionals and technologists to reduce ration doses. Technological factors are actions to reduce the tube current (mA, milliampere) and voltage (kVp, kilovolt peak), tube rotation speed (s, seconds), the extent of coverage, employing automatic tube current modulation, optimising the pitch and slice thickness, iterative reconstructions (IR) and newer artificial intelligence-based deep learning techniques.
The goal of LD-CT is to minimise radiation to the patient while achieving maximum image resolution and diagnostic capabilities. To obtain LD-CT, various kVp and mAs settings have been utilised in multidetector computed tomography (MDCT) across different anatomical regions and protocols. Initially, the LD-CT protocols aimed to reduce kVp and/or mAs and image reconstruction was performed with raw data using conventional filtered back projection techniques. Reducing slice thickness has been demonstrated to enhance the ability to detect small objects, such as small renal/ureteric calculi or lung nodules. However, image resolution is significantly impacted due to an increase in image noise (5). There are no specific cutoff levels for kVp and mAs in applying LD-CT and ULD-CT. Studies have shown that the average effective dose in LD-CT is approximately 2 mSv for chest CT in lung cancer screening and less than 3.5 mSv for CT kidney, ureter, and bladder (CT- KUB) (6,7). If the average CT abdomen and pelvis dose falls within the 10-12 mSv range, LD-CT reduces the overall dose by more than 75%. This reduction in radiation dose is highly significant for the patient.
Moreover, employing advanced techniques like IR algorithms and DLT reduces the radiation dose to as low as 1 mSv, thereby minimising image noise in ULD-CT. This reduction is approximately equivalent to the radiation dose used in abdominal radiographs (0.7 mSv) (7). The clinical application and value of LD-CT and ULD-CT for diagnosing various medical and surgical issues in many body systems are summarised in the following.
Respiratory system.
Lung cancer is the primary contributor to cancer-related deaths globally (8). Early identification of lung cancers could significantly reduce mortality and morbidity. Therefore, regular screening of high-risk populations with LD-CT has significantly reduced lung cancer mortality (9). The value of LD-CT has been explained in various trials with promising results. The US National Lung Screening Trial (NLST) reported a 20% decrease in lung cancer mortality through LD-CT screening. The more recent Nederlands-Leuvens Longkanker Screenings Onderzoek (NELSON) trial reported a 24% reduction compared to not using LD-CT screening. Similarly, the Multicentric Italian Lung Detection (MILD) trial demonstrated a 39% reduction in cumulative cancer mortality over ten years (9). Artificial intelligence (AI) has been incorporated into LD-CT screening programs to reduce false positive rates and screening costs (10). While undergoing LD-CT screening for lung cancer, multiple additional non-cancer-related incidental pulmonary pathologies, such as pleural effusion, emphysema, reticular opacities, and fibrosis, can be detected(11). In one study, emphysema was detected in 23.8% of subjects who underwent LD-CT for lung cancer screening, and more than 75% of emphysema cases were diagnosed for the first time with LD-CT (12).Kubo et al. demonstrated that LD-CT with 50 mAs does not differ significantly from standard dose CT (150 mAs) when diagnosing lung parenchymal, pleural, and mediastinal abnormalities (13). A recent systematic review revealed that standard-dose CT could be replaced with LD-CT for evaluating COVID-19 pneumonia with acceptable image quality (14).
Cardiovascular system
Cardiovascular diseases (CVDs) are responsible for nearly one-third of all deaths worldwide and significantly contribute to healthcare costs (15). These diseases include coronary artery disease, stroke, heart failure, hypertension, peripheral arterial disease, and other vascular and cardiac diseases. Cancer patients have a ten times greater risk of CVD mortality than the general population (16). Therefore, screening and diagnosing these conditions are important to reduce morbidity and mortality, especially during cancer screening.
Coronary artery calcification (CAC) scoring is a recognised predictor of CVD risk and mortality (17). Recent studies have shown that CAC can reliably be quantified during lung cancer screening using LD-CT (18,19). However, inherited drawbacks of LD-CT, such as signal-to-noise ratio and image artefacts, are significantly eliminated by recent LD-CT coupled with AI-based deep learning methods (19).
Aortic valve calcifications (AVC) significantly predict future CVD-associated deaths. LD-CT is a valuable tool for screening individuals at risk and grading the severity of AVC (20). Furthermore, a recent study has assessed the effects of mitral annular calcification (MAC) and CVD mortality using LD-CT in COVID-19 infection (21).
Pulmonary hypertension (PHT) is associated with increased morbidity and mortality and is often difficult to diagnose early due to non-specific patient symptoms. One way to predict PHT is to measure the diameter of the main pulmonary artery (MPA) and evaluate the MPA: ascending aorta ratio. In this context, LD-CT has been used to evaluate vascular diameter in patients undergoing lung cancer screening (20).
Genitourinary system.
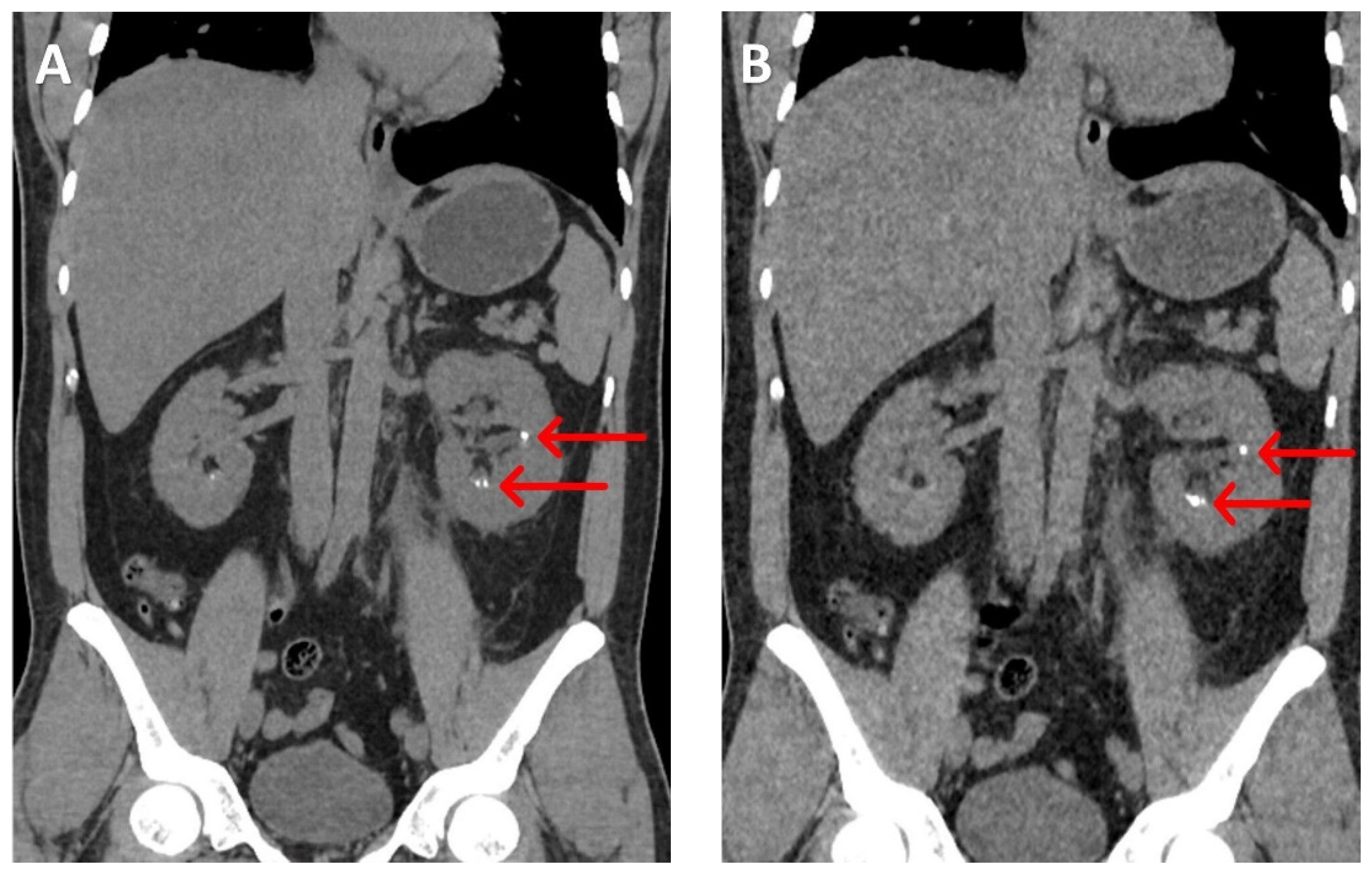
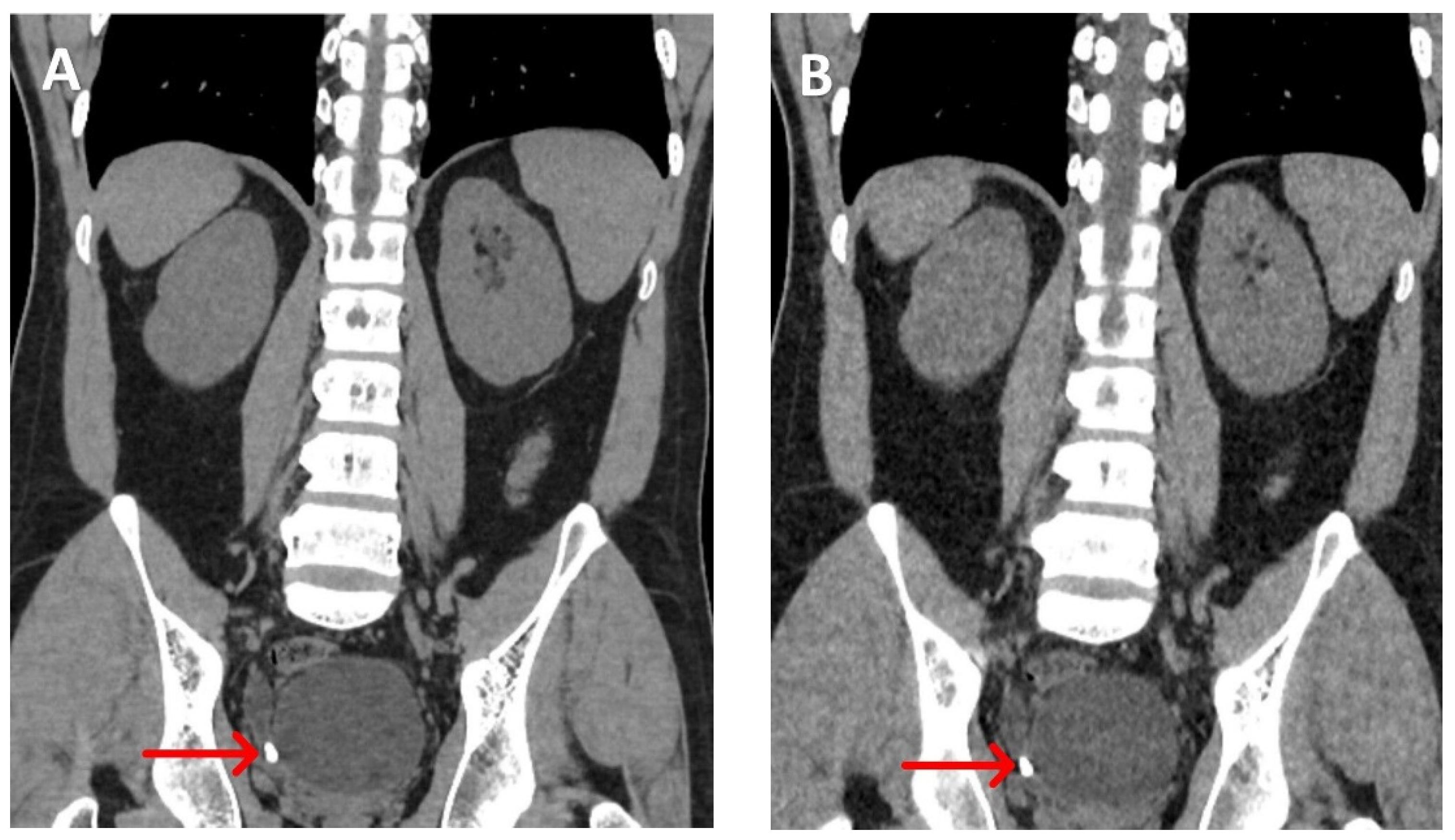
The prevalence of urolithiasis ranges from 1% to 20%, resulting in annual healthcare costs amounting to billions of dollars. Nearly one-third of these patients experience recurrence over 10 years. Standard-dose non-contrast CT imposes an additional radiation burden on the patient during diagnostic workups and monitoring. Therefore, the value of LD-CT of the kidneys, ureters, and bladder (LDCT-KUB) has been emphasised in numerous studies over the last two decades.
A meta-analysis has shown that LDCT-KUB can detect renal calculi > 3 mm with a sensitivity of 93% and specificity of 97%, using an average radiation dose of 1.4 mSv. This represents an approximately 85% reduction in radiation compared to the standard-dose CT-KUB (22)
(Figure 1 and Figure 2).
Recent studies have further highlighted the potential for reducing radiation doses to sub-millisievert levels using ultralow dose CT techniques.
In a recent publication, Zhang et al. utilised an ultra-low dose CT protocol combined with deep learning reconstruction methods. The study demonstrated a significant reduction in radiation dose (0.64 ± 0.17 mSv) while preserving image resolution and sensitivity for detecting calculi. This radiation dose is comparable to the 0.7 mSv typically associated with a standard abdominal X-ray and represents a 77% dose reduction compared to LD-CT (23).
Furthermore, whole-body LD-CT could accurately determine the presence or absence of bone metastasis in prostatic carcinoma, guiding clinical decision-making during management (24).
Gastrointestinal system
Acute appendicitis is a leading cause of acute abdomen in childhood and adolescence. Medical imaging plays a vital role in diagnosing appendicitis, both to confirm the diagnosis and to rule out other conditions that mimic appendicitis. Ultrasound is considered the first-line imaging method for diagnosing acute appendicitis in children, with a sensitivity ranging from 71% to 94% and specificity from 81% to 98% (25). However, CT abdomen is primarily used in certain countries and particularly in obese individuals, despite concerns about radiation dose.
As a result, the diagnostic capability of LD-CT has been emphasised in numerous studies. In a meta-analysis by Yun et al., the pooled sensitivity and specificity of low-dose CT were found to be 96.25% and 93.22%, respectively. There was no statistically significant difference between LD-CT and standard-dose CT (p = 0.71). This study included a combination of non-contrast and CT studies with IV contrast, and the majority demonstrated radiation doses of less than 2 mSv (26).
Furthermore, during the initial evaluation of the acute abdomen, LD-CT demonstrates a significant diagnostic yield compared to plain radiography and prevents unnecessary additional radiation exposure in standard-dose CT. Acute abdominal conditions benefiting from LD-CT assessment include complete or partial intestinal obstruction, strangulated abdominal wall hernia, internal hernia, colitis, constipation, pancreatitis, acute urinary retention, ascites, hemoperitoneum, and pneumoperitoneum (27).
In assessing hepatic steatosis, LD-CT serves as a more objective evaluation of fatty changes than ultrasonography, which is a more subjective assessment method. Moderate hepatic steatosis, indicated by a pathological liver fat content of 30%, is objectively assessed when the liver attenuation value is < 40 HU in unenhanced LD-CT. Therefore, fatty liver assessment is more readily obtained from LD-CT as an additional finding when performed to achieve another objective, such as renal calculi assessment (28).
Musculoskeletal system.
In acute major trauma, it is essential to rapidly identify life-threatening injuries and those that lead to permanent disabilities. Whole-body CT (WBCT) is considered the standard for managing adult major trauma in many settings, aiding in determining the Injury Severity Score (ISS). The use of WBCT in pediatric trauma patients is debatable due to the associated high radiation doses. Nevertheless, some centres have implemented low-dose WBCT protocols, featuring a mean radiation dosage of 4.8 mSv, in contrast to normal dose protocols with an average radiation dosage of about 20.6 mSv. Therefore, low-dose WBCT significantly reduces the radiation dose by approximately 77% (29).
In acute minor trauma, up to 80% of missed diagnoses in an emergency department are due to missed fractures. Using ultralow dose CT in suspected peripheral skeleton trauma detects more fractures and associated other injuries with relatively similar radiation compared to plain radiography (30).
Further, low-dose lumbar spine CT demonstrates superior image quality with better anatomical and pathological details than X-ray lumbar spine, with a nearly similar radiation dose (31). Low-dose WBCT can be used in multiple myeloma to monitor disease and detect incidental findings, ultimately improving overall management (32).
Head and Neck
Sinusitis is a common upper respiratory disease in pediatric subjects. Though CT is the gold standard for sinus imaging in adults, in children, CT sinuses cannot be used freely due to radiation burden. Therefore, the value of LD-CT sinuses has been studied in many centres, with a significantly low radiation dose, having a mean effective dose of about 0.0531 mSv compared to plain radiography (mean effective dose of about 0.0528 mSv) (33). LD-CT of the head is valuable in diagnosing intracranial haemorrhage, especially during follow-up, with a 45% reduction of effective dose compared to conventional CT (34).
Conclusion.
This narrative review emphasises the clinical applications and diagnostic value of LD-CT and ULD-CT across various body systems. These protocols have facilitated significant reductions of up to 80% in patient radiation exposure compared to standard doses while maintaining maximum image resolution and diagnostic capabilities. Future research studies are necessary to enhance image quality using AI-based technologies while reducing radiation doses.
Author contributions
SRS formulated the concept, designed the review, conducted the literature review, and wrote the manuscript.
Funding
This review received no external funding.
Availability of data and materials
Acquired DICOM medical images during the current review are available from the corresponding author upon reasonable request. The subject's identifying information was removed in radiology images.
Acknowledgements
The author acknowledges the management and Radiographers of Leesons Hospital, Ragama, Sri Lanka.
Competing Interests
The author declares that he has no competing interests.
References
- United Nations Scientific Committee on the Effects of Atomic Radiation (2010) Sources and Effects of Ionizing Radiation. United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2008 Report. Volume I: Sources: Report to the General Assembly, Scientific Annexes A and B. New York.
- Albert, JM. Radiation risk from CT: implications for cancer screening. American Journal of Roentgenology. 2013 Jul;201(1):W81-7. [CrossRef]
- National Research Council: Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, The National Academies Press, 2006, p 422.
- Cao CF, Ma KL, Shan H, Liu TF, Zhao SQ, Wan Y, Wang HQ. CT scans and cancer risks: A systematic review and dose-response meta-analysis. BMC cancer. 2022 Nov 30;22(1):1238. [CrossRef]
- Ketelslegers E, Van Beers BE: Urinary calculi: improved detection and characterization with thin-slice multidetector CT. Eur Radiol 2006; 16: 161–165. [CrossRef]
- Rampinelli C, Origgi D, Bellomi M. Low-dose CT: technique, reading methods and image interpretation. Cancer imaging. 2012;12(3):548. [CrossRef]
- Rodger F, Roditi G, Aboumarzouk OM. Diagnostic accuracy of low and ultra-low dose CT for identification of urinary tract stones: a systematic review. Urologia internationalis. 2018 Apr 12;100(4):375-85. [CrossRef]
- The Global Cancer Observatory, 2023, Accessed on November 16, 2023.
- Amicizia D, Piazza MF, Marchini F, Astengo M, Grammatico F, Battaglini A, Schenone I, Sticchi C, Lavieri R, Di Silverio B, Andreoli GB. Systematic review of lung cancer screening: advancements and strategies for implementation. InHealthcare 2023 Jul 21 (Vol. 11, No. 14, p. 2085). MDPI. [CrossRef]
- Grenier PA, Brun AL, Mellot F. The potential role of artificial intelligence in lung cancer screening using low-dose computed tomography. Diagnostics. 2022 Oct 8;12(10):2435. [CrossRef]
- Pinsky PF, Lynch DA, Gierada DS. Incidental findings on low-dose CT scan lung cancer screenings and deaths from respiratory diseases. Chest. 2022 Apr 1;161(4):1092-100. [CrossRef]
- Steiger D, Siddiqi MF, Yip R, Yankelevitz DF, Henschke CI, Jirapatnakul A, Flores R, Wolf A, Libby DM, Smith JP, Pasmantier M. The importance of low-dose CT screening to identify emphysema in asymptomatic participants with and without a prior diagnosis of COPD. Clinical imaging. 2021 Oct 1;78:136-41. [CrossRef]
- Kubo T, Ohno Y, Nishino M, Lin PJ, Gautam S, Kauczor HU, Hatabu H, iLEAD Study Group. Low dose chest CT protocol (50 mAs) as a routine protocol for comprehensive assessment of intrathoracic abnormality. European Journal of Radiology Open. 2016 Jan 1;3:86-94. [CrossRef]
- Suliman II, Khouqeer GA, Ahmed NA, Abuzaid MM, Sulieman A. Low-Dose Chest CT Protocols for Imaging COVID-19 Pneumonia: Technique Parameters and Radiation Dose. Life. 2023 Apr 12;13(4):992. [CrossRef]
- Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021 Dec;21(1):1-2. [CrossRef]
- Sturgeon KM, Deng L, Bluethmann SM, Zhou S, Trifiletti DM, Jiang C, Kelly SP, Zaorsky NG. A population-based study of cardiovascular disease mortality risk in US cancer patients. European heart journal. 2019 Dec 21;40(48):3889-97. [CrossRef]
- Shemesh J, Henschke CI, Shaham D, Yip R, Farooqi AO, Cham MD, McCauley DI, Chen M, Smith JP, Libby DM, Pasmantier MW. Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology. 2010 Nov;257(2):541-8. [CrossRef]
- Waltz J, Kocher M, Kahn J, Dirr M, Burt JR. The future of concurrent automated coronary artery calcium scoring on screening low-dose computed tomography. Cureus. 2020 Jun 12;12(6). [CrossRef]
- Chao H, Shan H, Homayounieh F, Singh R, Khera RD, Guo H, Su T, Wang G, Kalra MK, Yan P. Deep learning predicts cardiovascular disease risks from lung cancer screening low dose computed tomography. Nature Communications. 2021 May 20;12(1):2963. [CrossRef]
- Yip R, Jirapatnakul A, Hu M, Chen X, Han D, Ma T, Zhu Y, Salvatore MM, Margolies LR, Yankelevitz DF, Henschke CI. Added benefits of early detection of other diseases on low-dose CT screening. Translational Lung Cancer Research. 2021 Feb;10(2):1141. [CrossRef]
- Savaş ÖZ, BULUT E, AYDIN E, KIRCI DC, ÖZYILDIZ AG, PEKER M, TURAN OE. The Relationship of Mitral Anular Calcification with Mortality and Myocardial Injury in COVID-19 Patients. Sakarya Tıp Dergisi.;12(3):544-51. [CrossRef]
- Xiang H, Chan M, Brown V, Huo YR, Chan L, Ridley L. Systematic review and meta-analysis of the diagnostic accuracy of low-dose computed tomography of the kidneys, ureters and bladder for urolithiasis. Journal of medical imaging and radiation oncology. 2017 Oct;61(5):582-90. [CrossRef]
- Zhang X, Zhang G, Xu L, Bai X, Zhang J, Xu M, Yan J, Zhang D, Jin Z, Sun H. Application of deep learning reconstruction of ultra-low-dose abdominal CT in the diagnosis of renal calculi. Insights into Imaging. 2022 Oct 8;13(1):163. [CrossRef]
- Chavoshi M, Mirshahvalad SA, Zamani S, Radmard AR, Fallahi B, Mousavi SA. Whole-body low-dose CT can be of value in prostate cancer decision-making: a retrospective study on 601 patients. Insights into Imaging. 2023 Jul 16;14(1):124. [CrossRef]
- Téoule P, de Laffolie J, Rolle U, Reissfelder C. Acute appendicitis in childhood and adulthood: an everyday clinical challenge. Deutsches Ärzteblatt international. 2020 Nov;117(45):764. [CrossRef]
- Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY, Yang DM. Comparison of low-and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. American Journal of Roentgenology. 2017 Jun;208(6):W198-207. [CrossRef]
- Alshamari M, Norrman E, Geijer M, Jansson K, Geijer H. Diagnostic accuracy of low-dose CT compared with abdominal radiography in non-traumatic acute abdominal pain: prospective study and systematic review. European radiology. 2016 Jun;26:1766-74. [CrossRef]
- Boyce CJ, Pickhardt PJ, Kim DH, Taylor AJ, Winter TC, Bruce RJ, Lindstrom MJ, Hinshaw JL. Hepatic steatosis (fatty liver disease) in asymptomatic adults identified by unenhanced low-dose CT. American Journal of Roentgenology. 2010 Mar;194(3):623-8. [CrossRef]
- Simma L, Fornaro J, Stahr N, Lehner M, Roos JE, Lima TV. Optimising whole body computed tomography doses for paediatric trauma patients: a Swiss retrospective analysis. Journal of Radiological Protection. 2022 Apr 13;42(2):021521. [CrossRef]
- Alagic Z, Bujila R, Enocson A, Srivastava S, Koskinen SK. Ultra-low-dose CT for extremities in an acute setting: initial experience with 203 subjects. Skeletal radiology. 2020 Apr;49:531-9. [CrossRef]
- Alshamari M, Geijer M, Norrman E, Lidén M, Krauss W, Wilamowski F, Geijer H. Low dose CT of the lumbar spine compared with radiography: a study on image quality with implications for clinical practice. Acta Radiologica. 2016 May;57(5):602-11. [CrossRef]
- Simeone FJ, Harvey JP, Yee AJ, O’Donnell EK, Raje NS, Torriani M, Bredella MA. Value of low-dose whole-body CT in the management of patients with multiple myeloma and precursor states. Skeletal radiology. 2019 May 1;48:773-9. [CrossRef]
- Mulkens TH, Broers C, Fieuws S, Termote JL, Bellnick P. Comparison of effective doses for low-dose MDCT and radiographic examination of sinuses in children. American Journal of Roentgenology. 2005 May;184(5):1611-8. [CrossRef]
- Wu D, Wang G, Bian B, Liu Z, Li D. Benefits of low-dose CT scan of head for patients with intracranial hemorrhage. Dose-Response. 2020 Mar 5;18(1):1559325820909778. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).