Introduction
Rhombencephalosynapsis (RES) is a congenital disorder characterized by cerebellar maldevelopment resulting in the fusion of cerebellar hemispheres and hypogenesis or agenesis of the cerebellar vermis (1). It is also associated with other CNS abnormalities and aqueductal stenosis causing hydrocephalus. Though rhombencephalosynapsis commonly occurs in combination with syndromes, it rarely can be seen as an isolated case. This disorder with unknown etiology and pathogenesis, presents with varied symptoms ranging from no symptoms to ataxia, body incoordination, dysarthria, hypotonia, epilepsy, head shaking, and in severe cases death in early adulthood. With recent advances, it can be diagnosed prenatally by fetal MRI. The presence of ventriculomegaly on fetal sonography should raise the suspicion of rhombencephalosynapsis (2). If not diagnosed prenatally, then brain MRI is done in symptomatic patients. There is no specific treatment available for RES, only supportive treatment, and surgical management for associated congenital anomalies like hydrocephalus are done (3).
Case Presentation
A 60-year-old Indian female patient was admitted to SVP Hospital with the chief complaint of repeating words and irrelevant talking for 3 days, headache and giddiness for 2 days, and vomiting for 1 day. The patient was relatively asymptomatic for 3 days, following which she started repeating words and speaking non-sensible words. This was associated with occasional difficulty in recognizing relatives. During this time, the patient consulted another doctor and the blood pressure was 196/100 mm Hg for which injection Labetalol was administered. After the blood pressure was stabilized, the patient was admitted to our institute.
Negative history of fever, diarrhea, abdominal pain, loss of consciousness, seizures, palpitations, chest pain, pedal edema, and decreased urine output.
Past History
The patient has a history of hypertension for 30 years and is on medication for the same. She has a history of brain tumor and hysterectomy done 27 years ago.
Physical Examination
On examination, the patient's general condition was good. She was conscious and well-oriented to time, place, and person. A nervous system examination revealed a normal Glass Glow Coma Scale (GCS) score. Her pupils were bilaterally equal in size and diameter and reactive to light. Extraocular Movements (EOM) were normal. Muscle tone was normal in all four limbs and strength of the limbs was level 5. Deep Tendon reflexes were present in all the limbs with +5/+5. The patient had no facial weakness, no stiff neck, and no other biological pathological signs.
Lab Examination
Table 1.
Blood Examination.
Table 1.
Blood Examination.
| Test |
Observed Value |
Reference Range |
| Haemoglobin |
8.1 g/dl |
(12-18) |
| WBC |
7.69 kU/L |
(5.2-12.4) |
| RBC |
4.17*106/ul |
(4.5-5.5) |
| Haematocrit |
27.8% |
(40-50) |
| Platelet counts |
393 kU/L |
(130-400) |
| Neutrophiles |
76% |
(49-74) |
| Lymphocyte |
15% |
(26-46) |
| Monocyte |
07% |
(2-12) |
| Eosinophil |
02% |
(0-5) |
| Basophil |
00% |
(0-2) |
Table 2.
Liver Function Tests.
Table 2.
Liver Function Tests.
| Test |
Observed Value |
Reference Range |
| SGPT serum |
18 U/L |
(10-49) |
| SGOT serum |
38 U/L |
(0-34) |
| Alkaline Phosphatase Serum |
94 U/L |
(45-129) |
| Total Bilirubin |
0.70 mg/dl |
(0.3-1.2) |
| Direct Bilirubin |
0.29 mg/dl |
(0-0.3) |
| Indirect Bilirubin |
0.41 mg/dl |
- |
Table 3.
Renal Function Tests.
Table 3.
Renal Function Tests.
| Test |
Observed Value |
Reference Range |
| Blood Urea |
24.7 mg/dl |
(15-45) |
| Creatinine serum |
0.85 mg/dl |
(0.5-1.1) |
| Sodium serum |
127 mmol/L |
(132-146) |
| Potassium serum |
4.01 mmol/L |
(3.5-5.5) |
| Chlorine serum |
82 mmol/L |
(99-109) |
Table 4.
Other tests.
| Test |
Observed Value |
Reference Range |
| Cortisol serum |
33.46 ug/dl |
(3-16) |
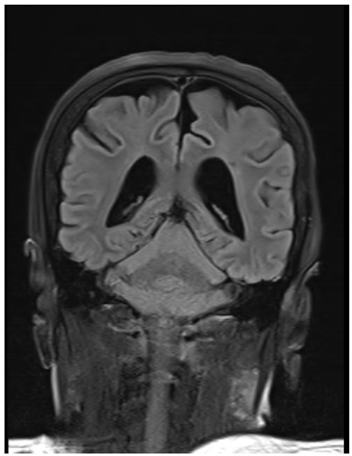
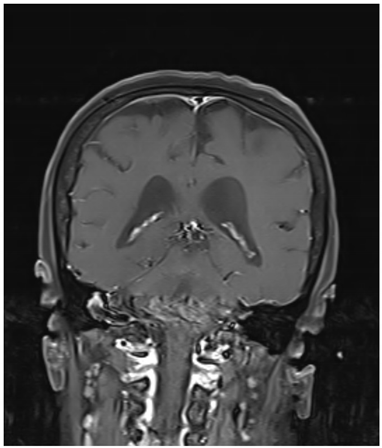
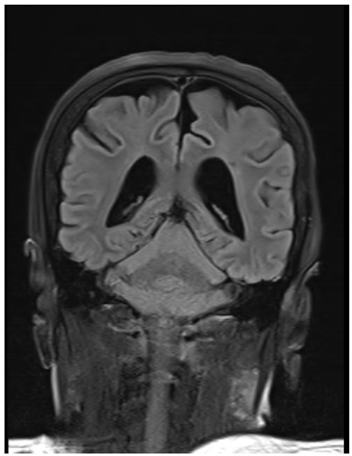
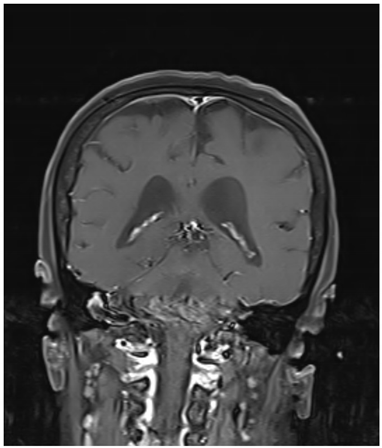
Radiological Imaging: (MRI Brain Plain)
Observation:
Absence of cerebellar vermis with the fusion of both cerebellar hemispheres and dentate nuclei along with dilated left lateral and third ventricle, suggestive of Rhombencephalosynapsis. (Donald-Duck Sign)
Age-related cerebral and cerebellar cortical atrophy with chronic ischemic changes is also seen.
Treatment
The patient was given tablet telmisartan 40 mg and tablet cilnidipine 10 mg both twice a day for 10 days. She was also given a tablet of tolvaptan 15 mg once a day for 10 days. Along with this, folic acid, vitamin B complex, and ferrous sulfate tablets were given once a day for 10 days. The patient was discharged once her condition was stabilized and symptoms improved.
Follow-Up Case
The patient was followed up for around 6 months and there has been no recurrence or aggravation.
Diagnosis
The patient was given appropriate treatment for 10 days and there was significant improvement in her condition. Based on the clinical presentation, imaging findings, and response to antibiotic therapy, the patient was diagnosed with Rhombencephalosynapsis.
Discussion and Literature
Rhombencephalosynapsis (RES) is a rare, congenital malformation of the posterior fossa characterized by hypogenesis or agenesis of the vermis, a dorsal fusion of cerebellar hemispheres, and fusion of dentate nuclei and superior cerebellar peduncles. The degree of disease severity depends on the degree of maldevelopment of the cerebellar vermis. The first case of rhomboencephalosynapsis was described in the autopsy report of a 28-year-old male by Henrich Obersteiner in 1914 (4).
There are no specific genetic or environmental causes of the disease identified. The disease pathogenesis is also unknown, but several studies show that both genetic and environmental factors play an important role in its etiopathogenesis. Several genetic changes like interstitial deletion of the long arm of chromosome 2q, tetrasomy 9p, etc. may have caused cerebellar maldevelopment (5). It commonly occurs with supratentorial abnormalities like ventriculomegaly due to aqueductal stenosis and other CNS abnormalities like hydrocephalus, Chiari I malformation, etc. The disease can rarely manifest alone or it may be seen in combination with other syndromes like VACTERL defects (Vertebral anomalies, Anal atresia, Cardiovascular anomalies, tracheoesophageal fistula, Esophageal atresia, Renal anomalies, and Limb defects), Gomez Lopez Hernandez syndrome (GLHS), etc. therefore, patients can be classified into 4 categories (6):
The clinical spectrum of the disease varies from being asymptomatic to loss of cognition. When rhomboencephalosynapsis presents as an isolated defect, the patient usually has no symptoms. The disease usually presents in early childhood, however, when severe, it can manifest in early infancy. The most common clinical manifestations include ataxia, hypotonia, epilepsy, spasticity, abnormal eye movements, impaired or normal cognitive function depending on severity, dysarthria, and the characteristic figure of eight and side-to-side head shaking (7). The patient usually also has atypical craniofacial features like hypertelorism, flat midface, prominent forehead, and low set posteriorly placed ears. The neurocognitive development varies ranging from normal IQ to intellectual deficits. Asymptomatic patients have a normal life with mild issues of balance and coordination but the ones with symptoms have a shorter life expectancy and death by childhood.
The diagnosis of rhombencephalosynapsis is done with imaging or neuropathological finding of a hypoplastic single-lobed cerebellum (8). It can be diagnosed prenatally via fetal MRI if there is ventriculomegaly and cerebellar hypoplasia on fetal ultrasonography. If the diagnosis is done prenatally, then the prognosis is usually worse. The diagnostic modality of choice is Brain MRI. It usually shows abnormal posterior fossa and fourth ventricle which gives a diamond or keyhole shape, which is also known as the Donald duck sign (9). If an MRI is not available or is contraindicated, then a Brain CT scan can also be done to diagnose rhomboencephalosynapsis. The most common differentials for this disorder include the Dandy-Walker spectrum and Joubert syndrome (10) and these are easily separated from RES by brain MRI.
There is no definitive treatment for rhombencephalosynapsis. No medical management is required for isolated cases of rhombencephalosynapsis. The affected infant is given supportive treatment along with ventriculostomy or ventricular shunting for obstructive hydrocephalus. For the patients diagnosed after birth, symptomatic treatment along with physical, social, and psychological care is given. Their symptoms gradually improve with rehabilitation and physiotherapy. Surgical management is done for associated anomalies.
Being a rare disorder, rhombencephalosynapsis is often missed on clinical diagnosis, which results in the birth of the affected child. Thus, prenatal counselling for this disorder should be encouraged to prevent future struggles for both the child and parents (11).
Conclusions
Rhombencephalosynapsis is a congenital disorder with many possible etiopathogenesis hypotheses. The diagnosis is often missed due to association with other syndromes. Brain MRI stays the mainstay modality for diagnosis of RES. Since it’s a cerebellar maldevelopment disorder, medications cannot help much. Surgical management is done for other associated abnormalities. Though recent advances in research have put into light its clinical features and imaging findings, we need more gene investigations to overcome the limitations of current genetic study approaches. Detailed prenatal history information is needed to know the disease etiopathogenesis better.
Ethical Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Paprocka, J.; Jamroz, E.; Ścieszka, E.; Kluczewska, E. Isolated rhomboencephalosynapsis-a rare cerebellar anomaly. Available online: http://www.polradiol.com/fulltxt.php?ICID=882587 (accessed on 15 December 2023).
- Krajden Haratz, K.; Oliveira Szejnfeld, P.; Govindaswamy, M.; Leibovitz, Z.; Gindes, L.; Severino, M.; et al. Prenatal diagnosis of rhombencephalosynapsis: Neuroimaging features and severity of vermian anomaly. Ultrasound in Obstetrics and Gynecology 2021, 58, 864–874. Available online: https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1002/uog.23660?src=getftr. [CrossRef]
- Weaver, J.; Manjila, S.; Bahuleyan, B.; Bangert, B.A.; Cohen, A.R. Rhombencephalosynapsis: Embryopathology and management strategies of associated neurosurgical conditions with a review of the literature. J Neurosurg Pediatr [Internet] 2013, 11, 320–326. Available online: https://pubmed.ncbi.nlm.nih.gov/23331215/ (accessed on 15 December 2023). [CrossRef] [PubMed]
- Aldinger, K.A.; Dempsey, J.C.; Tully, H.M.; Grout, M.E.; Mehaffey, M.G.; Dobyns, W.B.; et al. Rhombencephalosynapsis: Fused cerebellum, confused geneticists. Am J Med Genet C Semin Med Genet [Internet] 2018, 178, 432. Available online: https://PMC/articles/PMC6540982/. [CrossRef] [PubMed]
- Di Vera, E.; Liberati, M.; Celentano, C.; Calabrese, G.; Guanciali-Franchi, P.E.; Morizio, E.; et al. Rhombencephalosynapsis in a severely polymalformed fetus with non-mosaic tetrasomy 9p, in intracytoplasmic-sperm-injection pregnancy. J Assist Reprod Genet [Internet] 2008, 25, 577. Available online: https://PMC/articles/PMC2593768/. [CrossRef]
- Ishak, G.E.; Dempsey, J.C.; Shaw, D.W.W.; Tully, H.; Adam, M.P.; Sanchez-Lara, P.A.; et al. Rhombencephalosynapsis: A hindbrain malformation associated with incomplete separation of midbrain and forebrain, hydrocephalus, and a broad spectrum of severity. Brain [Internet] 2012, 135, 1370. Available online: https://PMC/articles/PMC3338925/. [CrossRef]
- Tully, H.M.; Dempsey, J.C.; Ishak, G.E.; Adam, M.P.; Mink, J.W.; Dobyns, W.B.; et al. Persistent figure-8 and side-to-side head shaking is a marker for rhombencephalosynapsis. Mov Disord [Internet] 2013, 28, 2019. Available online: https://PMC/articles/PMC5510988/. [CrossRef] [PubMed]
- McAuliffe, F.; Chitayat, D.; Halliday, W.; Keating, S.; Shah, V.; Fink, M.; et al. Rhombencephalosynapsis: Prenatal imaging and autopsy findings. Ultrasound in Obstetrics and Gynecology [Internet] 2008, 31, 542–548. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/uog.5318 (accessed on 15 December 2023). [CrossRef] [PubMed]
- Baba, Y.; Gaillard, F. Rhombencephalosynapsis. Radiopaedia.org. 2010 Jan 24. Available online: https://radiopaedia.org/articles/rhombencephalosynapsis.
- McAuliffe, F.; Chitayat, D.; Halliday, W.; Keating, S.; Shah, V.; Fink, M.; et al. Rhombencephalosynapsis: Prenatal imaging and autopsy findings. Ultrasound in Obstetrics and Gynecology [Internet] 2008, 31, 542–548. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/uog.5318 (accessed on 15 December 2023). [CrossRef] [PubMed]
- Gupta, A.; Tauqeer Fazal, S.; Kumar Anjali Mehta, S.; Saini, P. Prenatal Diagnosis of Rhombencephalosynapsis. Available online: https://www.thieme-connect.com/products/ejournals/pdf/10.1007/s40556-016-0110-2.pdf.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).