1. Introduction
In-stent restenosis (ISR) is a common complication that can occur following the placement of a coronary stent [
1,
2]. In recent years, the use of drug-eluting stents (DESs) reduces ISR and major adverse cardiac events [
3,
4]. However, ISR after DES implantation still occurs [
5,
6]. The black hole (BH) phenomenon is an intraluminal restenotic lesion image obtained by intravascular ultrasound (IVUS) and optical coherence tomography (OCT) [
7,
8,
9,
10,
11,
12]. The development of ISR involves multiple factors, including biological, mechanical, patient, and operator-related factors [
13,
14,
15]. Intracoronary imaging is crucial for determining the specific mechanism of ISR, enabling tailored treatment strategies based on the identified cause. Therefore, we present a case of an ISR lesion with a suspected BH phenomenon on IVUS confirmed by OCT.
2. Case Description
A 72-year-old male presented to our outpatient department with incremental exertional dyspnea and chest pain for the past 2 weeks. He had ischemic heart disease and underwent percutaneous coronary intervention (PCI) on June 21, 2022, with sirolimus-eluting stents (SES) placed at the proximal portion of the left anterior descending (LAD) artery and the proximal to middle portion of the left circumflex artery. His ongoing medications included aspirin, clopidogrel, bisoprolol, atorvastatin, ezetimibe, furosemide, and hypoglycemic agents (pioglitazone, glimepiride, and dulaglutide).
During the cardiovascular outpatient department visit, his symptoms had subsided, and the ECG displayed sinus rhythm without significant ST/T wave changes for 9 months. According to the history and positive findings of the treadmill exercise test, he was admitted for coronary angiography. On admission, his laboratory data revealed poor diabetic control (hemoglobin A1C of 8.3%) and controlled hyperlipidemia (total cholesterol, 132 mg/dL; triglycerides, 54 mg/dL; low-density lipoprotein, 55 mg/dL, and high-density lipoprotein, 59 mg/dL). Blood counts, serum electrolytes, and renal and liver function tests were within normal limits.
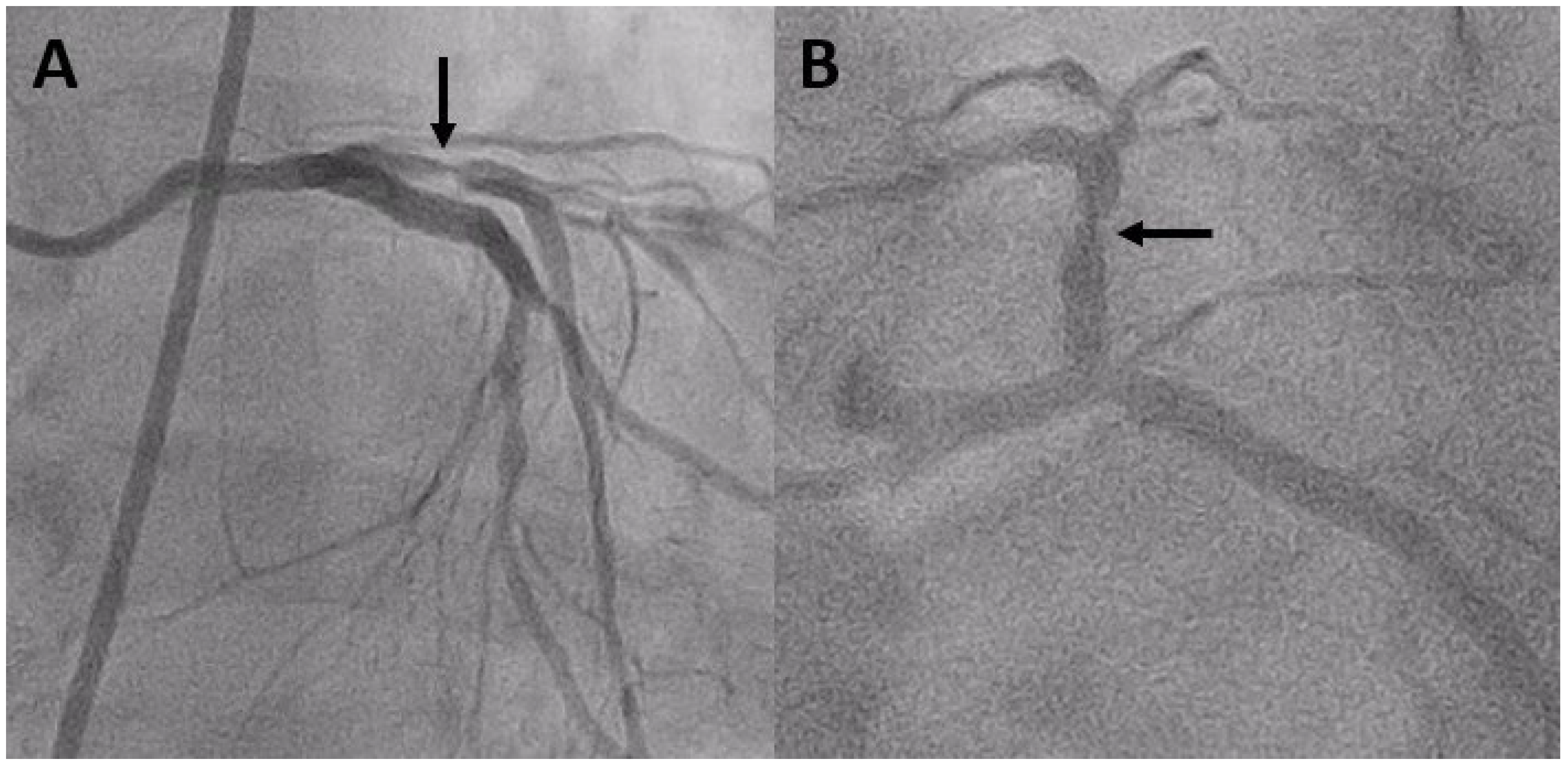
Coronary angiography on April 27, 2023, revealed severe ISR of the proximal LAD (
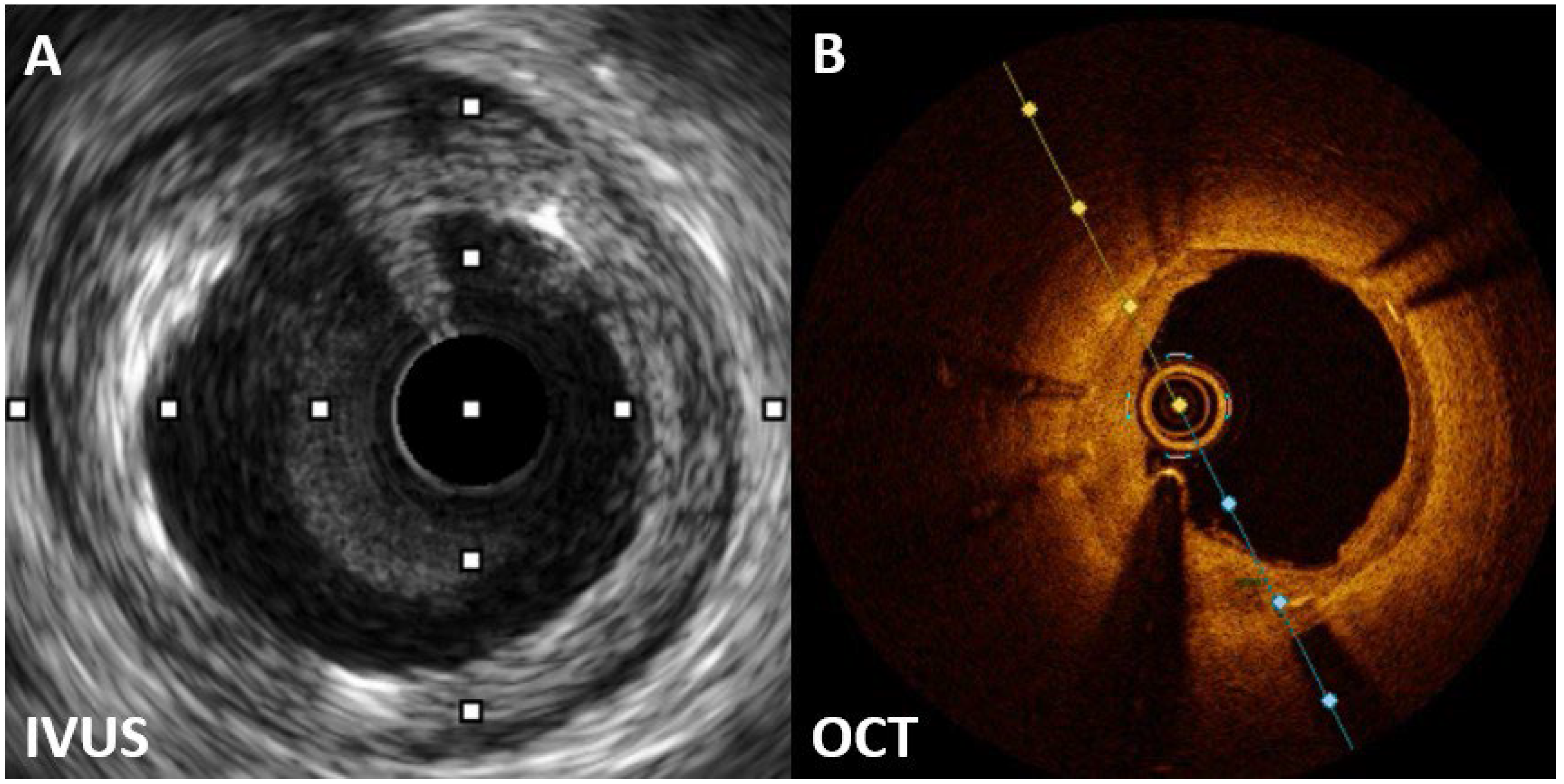
Figure 1). A 60-MHz high-definition IVUS was performed, which revealed a homogenous echolucent appearance at an ISR of the SES (
Figure 2A) and a suspected BH phenomenon.
Given the significant constriction of the lumen area of the ISR lesion, obtaining a high-quality OCT image without balloon predilatation is challenging. Hence, we chose the 2.0-mm balloon to minimize the effect on the original lesion. OCT revealed a layered pattern with a superficial high-signal intensity band adjacent to the luminal surface and a signal-poor region near the stent (
Figure 2B). According to the above imaging findings, the patient was diagnosed with BH phenomenon through OCT.
A DES was implanted and subsequently postdilated using a noncompliant balloon. After PCI, the lumen surface appeared smooth, with no evidence of tissue prolapse or residual intraluminal thrombus, with a well-deployed stent. Thrombolysis in myocardial infarction III distal blood flow was achieved using angiography.
3. Discussion
Following the placement of a coronary stent, ISR can commonly emerge as a complication [
1,
2]. Despite advances in technology, the occurrence rate of ISR has remained relatively consistent, affecting approximately 10% after DES implantation [
5,
6].
The cause of ISR is multifactorial and can be attributed to various biological, mechanical, and procedural factors [
13,
14,
15]. Mechanical factors primarily include stent expansion or fracture, whereas biological factors involve localized inflammation leading to excessive neointimal growth and late neoatherosclerosis.
The “BH” phenomenon, which has been characterized as an intraluminal restenotic lesion with a homogeneous black appearance (echolucent) on IVUS, was initially observed in patients following brachytherapy [
7]. This phenomenon has also been identified in patients who have received SES implants [
8].
DES improved BMS limitations but raised concerns about complications such as late restenosis and thrombosis. Late DES thrombosis is marked by delayed healing with impaired reendothelialization and persistent fibrin deposition. The exact cause of late restenosis remains unclear but may involve a delayed healing response to stent polymers and drugs.
Although the BH phenomenon is unusual in DES restenosis, establishing a universal mechanism is challenging. Tissue analysis of the BH revealed a primarily hypocellular matrix with areas rich in proteoglycans, possibly due to delayed vascular wound healing following SES implantation. The echolucent appearance is likely attributed to this hypocellular matrix and its high water content [
9,
10].
OCT revealed a layered structure with an inner layer with high-signal intensity and outer layers with low signal intensity. The low OCT signal intensity is a result of restenotic tissue rich in proteoglycan and poor in collagen matrix or fibrin-rich thrombus formation. Although various restenotic tissues can exhibit low OCT signal intensity, the consistent border and structure in this case suggest that the BH phenomenon in OCT may be due to the lack of organized mature connective tissue elements in the restenotic tissue [
11,
12].
Assessments by IVUS or OCT before DES restenosis treatment can help identify restenotic tissue characteristics and guide the development of an optimal strategy to prevent recurrent ISR. However, OCT is superior to IVUS for the diagnosis of the BH phenomenon after DES implantation.
4. Conclusions
A BH phenomenon can occur after SES implantation. The diagnosis of the BH phenomenon after DES implantation favors OCT over IVUS.
Author Contributions
Conceptualization, C.C.K. and G.P.J.; methodology, C.C.K.; software, W.C.T. and C.C.C.; validation, C.C.K. and G.P.J.; formal analysis, C.C.K. and G.P.J.; investigation, C.C.K.; resources, W.C.T.; data curation, C.C.K. and G.P.J.; writing—original draft preparation, C.C.K. and G.P.J.; writing—review and editing, G.P.J.; visualization, W.C.T., C.C.C., and G.P.J.; supervision, G.P.J.; project administration, C.C.K.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study as per institution protocol.
Informed Consent Statement
Informed consent was obtained from the parents.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kyaw, H.; Johal, G.; Gedela, M.; Barman, N.; Kini, A.; Sharma, S.K. Is coronary brachytherapy staging a Comeback for the treatment of in-stent sestenosis? Curr. Cardiol. Rep. 2021, 23, 156. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.W.; Huang, M.S.; Su, P.F.; Chao, T.H.; Lee, C.H.; Liu, P.Y. Management of restenosis after stenting in left main coronary artery disease. Acta Cardiol. Sin. 2023, 39, 277–286. [Google Scholar] [PubMed]
- Liou, K.; Jepson, N.; Cao, C.; Luo, R.; Pala, S.; Ooi, S.Y. Drug-eluting balloon versus second generation drug eluting stents in the treatment of in-stent restenosis: A systematic review and meta-analysis. Heart Lung Circ. 2016, 25, 1184–1194. [Google Scholar] [CrossRef] [PubMed]
- Macovei, L.; Magopet, R.; Campo, G. Drug-eluting stents: new presumed effects over in-stent restenosis prevention. Minerva Cardiol. Angiol. 2021, 69, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Fu, G.; Yu, Z.; Chen, Y.; Chen, Y.; Tian, F.; Yang, X. Direct adsorption of anti-CD34 antibodies on the Nano-Porous stent surface to enhance endothelialization. Acta Cardiol. Sin. 2016, 32, 273–280. [Google Scholar] [PubMed]
- Parfrey, S.; Siu, V.; Graham, J.J.; Vijayaraghavan, R.; Li, C.; Pang, J.; Kalra, S.; Džavík, V.; Wijeysundera, H.C.; Bagai, A. from the University of Toronto CTO Collaborative. Evaluation and management of drug-eluting stent in-stent restenosis. Curr. Opin. Cardiol. 2023, 38, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Castagna, M.T.; Mintz, G.S.; Weissman, N.; Maehara, A.; Finet, G.; Waksman, R. "Black hole": echolucent restenotic tissue after brachytherapy. Circulation. 2001, 103, 778. [Google Scholar] [CrossRef] [PubMed]
- Hirose, M.; Kobayashi, Y.; Leon, M.B. Echolucent neointimal hyperplasia "dark wall" after sirolimus eluting stent implantation. Heart. 2004, 90, 1143. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Shiode, N.; Shirota, K.; Fukuda, Y.; Kitamura, F.; Tominaga, K.; Kato, Y.; Miura, H.; Inoue, K.; Nobuyoshi, M. Pathological finding of sirolimus-eluting stent (SES) restenosis lesion with black hole appearance on intravascular ultrasound. Circ. J. 2009, 73, 1969–1971. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Murata, T.; Kono, M.; Imoto, H.; Koyama, T.; Nakamura, K.; Kadama, S.; Noguchi, H.; Saito, T. Black hole restenosis after drug-eluting stent implantation for in-stent restenosis: potential mechanism and optimal strategy. Heart Vessels 2015, 30, 682–686. [Google Scholar] [CrossRef] [PubMed]
- Kurita, T.; Terashima, M.; Suzuki, T. Serial optical coherence tomography imaging of the "black-hole" phenomenon by intravascular ultrasound following sirolimus-eluting stent implantation. EuroIntervention 2012, 7, 1480–1481. [Google Scholar] [CrossRef] [PubMed]
- Landmesser, U. Optical coherence tomography (OCT) evaluation after coronary stenting: the "black hole" and other low OCT signal-intensity areas. EuroIntervention 2012, 7, 1367–1371. [Google Scholar] [CrossRef] [PubMed]
- Cai, W.; Chen, E.; Zeng, X.; Chen, C.; Wu, L.; Zheng, X.; Chen, L. Efficacy and biosafety of a new bioresorbable vascular scaffold covered with biodegradable film in rabbits: An in vivo study. Acta Cardiol. Sin. 2020, 36, 660–666. [Google Scholar] [PubMed]
- Aoki, J.; Tanabe, K. Mechanisms of drug-eluting stent restenosis. Cardiovasc. Interv. Ther. 2021, 36, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Clare, J.; Ganly, J.; Bursill, C.A.; Sumer, H.; Kingshott, P.; de Haan, J.B. The mechanisms of restenosis and relevance to next generation stent design. Biomolecules 2022, 12, 430. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).