Submitted:
18 December 2023
Posted:
19 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
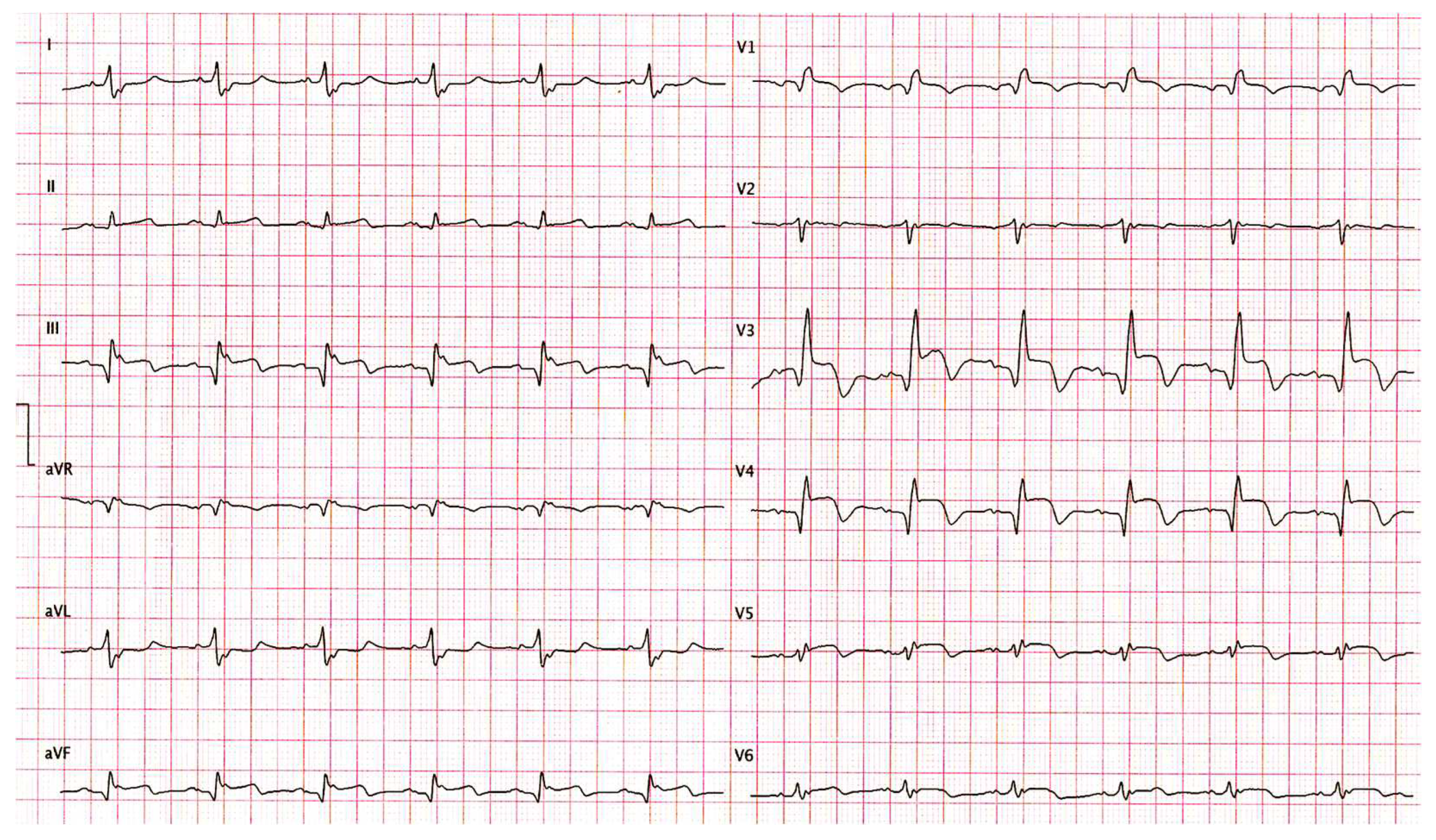
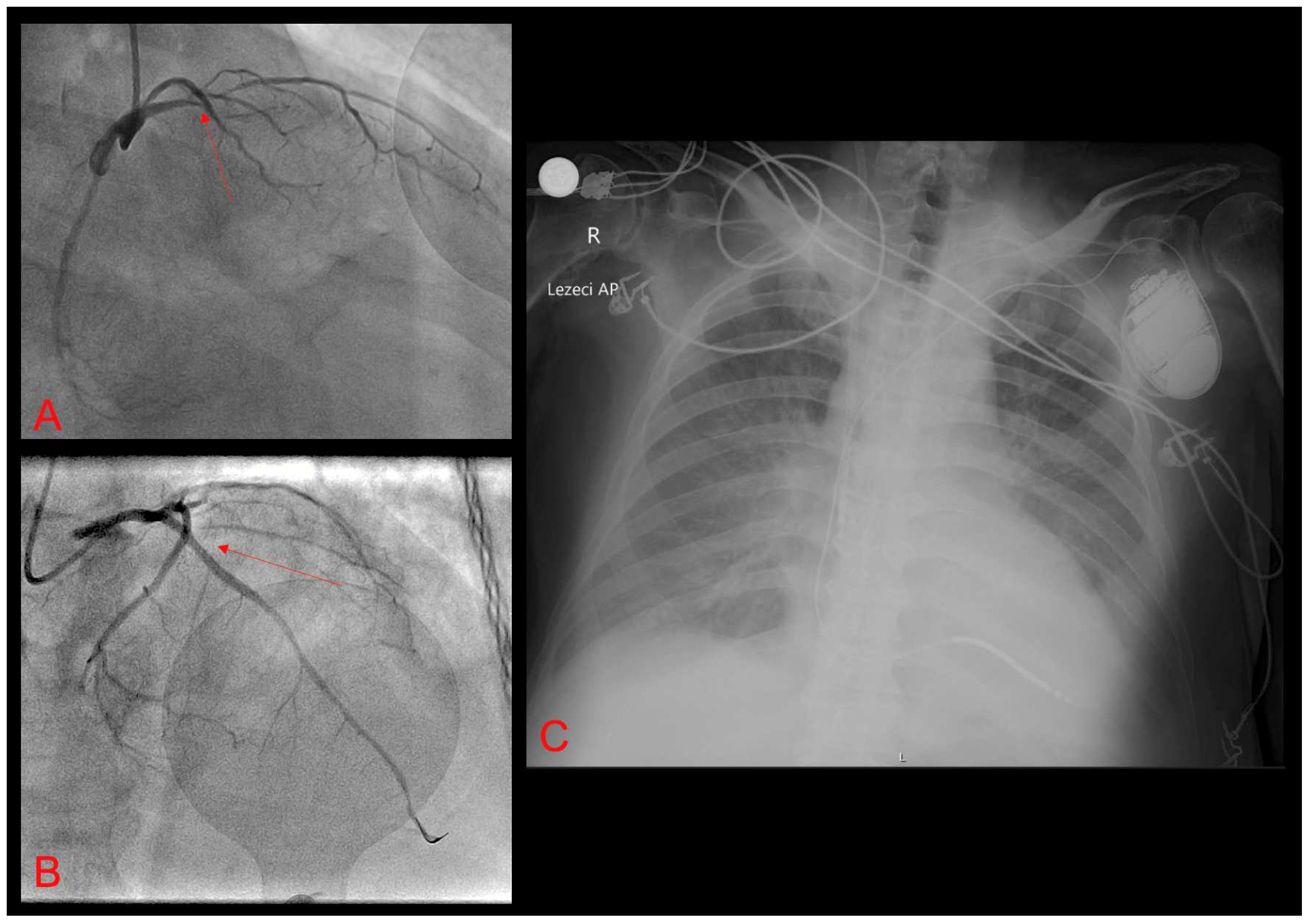
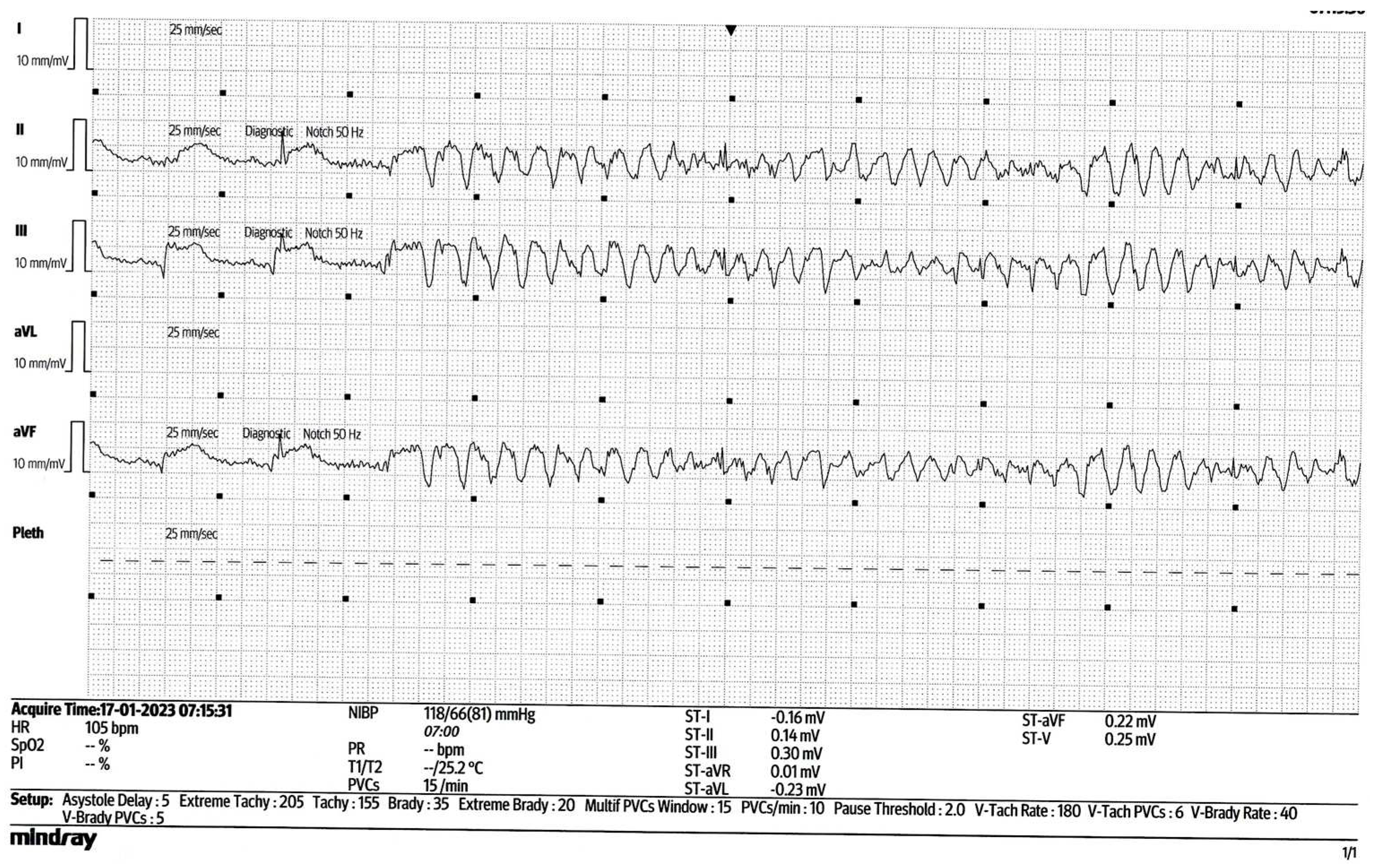
2. Case Report
3. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hohnloser SH, Al-Khalidi HR, Pratt CM, Brum JM, Tatla DS, Tchou P, Dorian P; SHock Inhibition Evaluation with AzimiLiDe (SHIELD) Investigators. Electrical storm in patients with an implantable defibrillator: incidence, features, and preventive therapy: insights from a randomized trial. Eur Heart J. 2006 Dec;27(24):3027-32. [CrossRef]
- Piccini JP, Berger JS, Brown DL. Early sustained ventricular arrhythmias complicating acute myocardial infarction. Am J Med. 2008 Sep;121(9):797-804. [CrossRef]
- Gorenek B, Blomström Lundqvist C, Brugada Terradellas J, Camm AJ, Hindricks G, Huber K, Kirchhof P, Kuck KH, Kudaiberdieva G, Lin T, Raviele A, Santini M, Tilz RR, Valgimigli M, Vos MA, Vrints C, Zeymer U, Lip GY, Potpara T, Fauchier L, Sticherling C, Roffi M, Widimsky P, Mehilli J, Lettino M, Schiele F, Sinnaeve P, Boriani G, Lane D, Savelieva I. Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. Europace. 2014 Nov;16(11):1655-73. [CrossRef]
- Pedersen CT, Kay GN, Kalman J, Borggrefe M, Della-Bella P, Dickfeld T, Dorian P, Huikuri H, Kim YH, Knight B, Marchlinski F, Ross D, Sacher F, Sapp J, Shivkumar K, Soejima K, Tada H, Alexander ME, Triedman JK, Yamada T, Kirchhof P, Lip GY, Kuck KH, Mont L, Haines D, Indik J, Dimarco J, Exner D, Iesaka Y, Savelieva I. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Europace. 2014 Sep;16(9):1257-83. [CrossRef]
- Greene M, Newman D, Geist M, Paquette M, Heng D, Dorian P. Is electrical storm in ICD patients the sign of a dying heart? Outcome of patients with clusters of ventricular tachyarrhythmias. Europace. 2000 Jul;2(3):263-9. [CrossRef]
- Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA, Charron P, Corrado D, Dagres N, de Chillou C, Eckardt L, Friede T, Haugaa KH, Hocini M, Lambiase PD, Marijon E, Merino JL, Peichl P, Priori SG, Reichlin T, Schulz-Menger J, Sticherling C, Tzeis S, Verstrael A, Volterrani M; ESC Scientific Document Group. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126. [CrossRef]
- Magdi M, Mubasher M, Alzaeem H, Hamid T. Resistant Ventricular Arrhythmia and the Role of Overdrive Pacing in the Suppression of the Electrical Storm. Case Rep Cardiol. 2019 May 22;2019:6592927. [CrossRef]
- European Heart Rhythm Association; Heart Rhythm Society; Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ, Priori SG, Quinones MA, Roden DM, Silka MJ, Tracy C, Smith SC Jr, Jacobs AK, Adams CD, Antman EM, Anderson JL, Hunt SA, Halperin JL, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL; American College of Cardiology; American Heart Association Task Force; European Society of Cardiology Committee for Practice Guidelines. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006 Sep 5;48(5):e247-346. [CrossRef]
- Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, Blom N, Brugada J, Chiang CE, Huikuri H, Kannankeril P, Krahn A, Leenhardt A, Moss A, Schwartz PJ, Shimizu W, Tomaselli G, Tracy C; Document Reviewers; Ackerman M, Belhassen B, Estes NA 3rd, Fatkin D, Kalman J, Kaufman E, Kirchhof P, Schulze-Bahr E, Wolpert C, Vohra J, Refaat M, Etheridge SP, Campbell RM, Martin ET, Quek SC; Heart Rhythm Society; European Heart Rhythm Association; Asia Pacific Heart Rhythm Society. Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Europace. 2013 Oct;15(10):1389-406. [CrossRef]
- Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, Deal BJ, Dickfeld T, Field ME, Fonarow GC, Gillis AM, Granger CB, Hammill SC, Hlatky MA, Joglar JA, Kay GN, Matlock DD, Myerburg RJ, Page RL. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018 Sep 25;138(13):e210-e271. [CrossRef]
- Kowlgi GN, Cha YM. Management of ventricular electrical storm: a contemporary appraisal. Europace. 2020 Dec 23;22(12):1768-1780. [CrossRef]
- Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, Deal BJ, Dickfeld T, Field ME, Fonarow GC, Gillis AM, Granger CB, Hammill SC, Hlatky MA, Joglar JA, Kay GN, Matlock DD, Myerburg RJ, Page RL. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2018 Oct;15(10):e190-e252. [CrossRef]
- Meng L, Tseng CH, Shivkumar K, Ajijola O. Efficacy of Stellate Ganglion Blockade in Managing Electrical Storm: A Systematic Review. JACC Clin Electrophysiol. 2017 Sep;3(9):942-949. [CrossRef]
- Nayyar S, Ganesan AN, Brooks AG, Sullivan T, Roberts-Thomson KC, Sanders P. Venturing into ventricular arrhythmia storm: a systematic review and meta-analysis. Eur Heart J. 2013 Feb;34(8):560-71. [CrossRef]
- Komatsu Y, Hocini M, Nogami A, Maury P, Peichl P, Iwasaki Y, et al. Catheter ablation of refractory ventricular fibrillation storm after myocardial infarction: a multicenter study. Circulation 2019;139:2315–2325. [CrossRef]
- Dinov B, Arya A, Bertagnolli L, Schirripa V, Schoene K, Sommer P, Bollmann A, Rolf S, Hindricks G. Early referral for ablation of scar-related ventricular tachycardia is associated with improved acute and long-term outcomes: results from the Heart Center of Leipzig ventricular tachycardia registry. Circ Arrhythm Electrophysiol. 2014 Dec;7(6):1144-51. [CrossRef]
- Wang S, Luo H, Mao T, Xiang C, Hu H, Zhao J, Wang X, Wang J, Liu H, Yu L, Jiang H. Stereotactic arrhythmia radioablation: A novel therapy for cardiac arrhythmia. Heart Rhythm. 2023 Sep;20(9):1327-1336. [CrossRef]
- Le Pennec-Prigent S, Flecher E, Auffret V, Leurent G, Daubert JC, Leclercq C, Mabo P, Verhoye JP, Martins RP. Effectiveness of Extracorporeal Life Support for Patients With Cardiogenic Shock Due To Intractable Arrhythmic Storm. Crit Care Med. 2017 Mar;45(3):e281-e289. [CrossRef]
- Vergara P, Tung R, Vaseghi M, Brombin C, Frankel DS, Di Biase L, Nagashima K, Tedrow U, Tzou WS, Sauer WH, Mathuria N, Nakahara S, Vakil K, Tholakanahalli V, Bunch TJ, Weiss JP, Dickfeld T, Vunnam R, Lakireddy D, Burkhardt JD, Correra A, Santangeli P, Callans D, Natale A, Marchlinski F, Stevenson WG, Shivkumar K, Della Bella P. Successful ventricular tachycardia ablation in patients with electrical storm reduces recurrences and improves survival. Heart Rhythm. 2018 Jan;15(1):48-55. [CrossRef]
- Do DH, Bradfield J, Ajijola OA, Vaseghi M, Le J, Rahman S, Mahajan A, Nogami A, Boyle NG, Shivkumar K. Thoracic Epidural Anesthesia Can Be Effective for the Short-Term Management of Ventricular Tachycardia Storm. J Am Heart Assoc. 2017 Oct 27;6(11):e007080. [CrossRef]
| Drug | Dose | Administration |
|---|---|---|
| Amiodarone | 150 mg bolus + 1200 mg continuous infusion during 24 hours | intravenous |
| Lidocaine | Bolus dose of 1mg/kg, with repeat bolus dose of 0.5mg/kg, followed by the continuous infusion of 20 mcg/kg/min. during 24 hours | intravenous |
| Metoprolol | 5 mg intravenous every 5 minutes; up to 3 doses | intravenous |
| Magnesium-sulphate | 2 g bolus dose | intravenous |
| Propofol | 50 mg bolus dose + continuous infusion of 100 mcg/kg/min. | intravenous |
| Propranolol | 40 mg twice a day after acute stabilization | oral |
| Drug | Dose |
|---|---|
| Amiodarone | IV: bolus 150 mg for stable VT; maintenance: 1 mg/min × 6 h, then 0.5 mg/min × 18 h; PO: 400 mg × q 8–12 h for 7–14 days, then 200–400 mg daily |
| Lidocaine | IV: bolus 1–1.5 mg/kg, can repeat up to total of 3 mg/kg, maintenance: 1–4 mg/min |
| Propranolol | IV: 1–3 mg q5 min to a maximum of 5 mg; PO: 10–40 mg q6 h immediate release; 60–160 mg q12 h extended release |
| Mexiletin | 150–300 mg PO q8–12 h |
| Procainamide | IV: bolus 10 mg/kg over 20 min, maintenance 2–3 g/24 h; oral: 500–1250 mg q6 h |
| Quinidine | Quinidine sulfate: 200–600 mg PO q6–12 h; quinidine gluconate 324–648 mg PO q8 h; IV loading dose 800 mg/50 mL, maintenance 50 mg/min |
| Sotalol | IV: 7 5 mg q12 h; PO: 80–160 mg q12 h |
| Metoprolol | IV: 5 mg q5 min up to 3 doses; PO: metoprolol tartarate 25–100 mg q12 h |
| Esmolol | IV: bolus: 0.5 mg/kg, maintenance: 0.05 mg/kg/min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





