Submitted:
21 December 2023
Posted:
21 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Isolates Collection
2.2. Identification of Strains and Antimicrobial Susceptibility Testing
2.3. Detection of Extended-Spectrum Beta-Lactamases and Carbapenemases
2.4. MIC Determination
3. Results
3.1. Isolates Collection
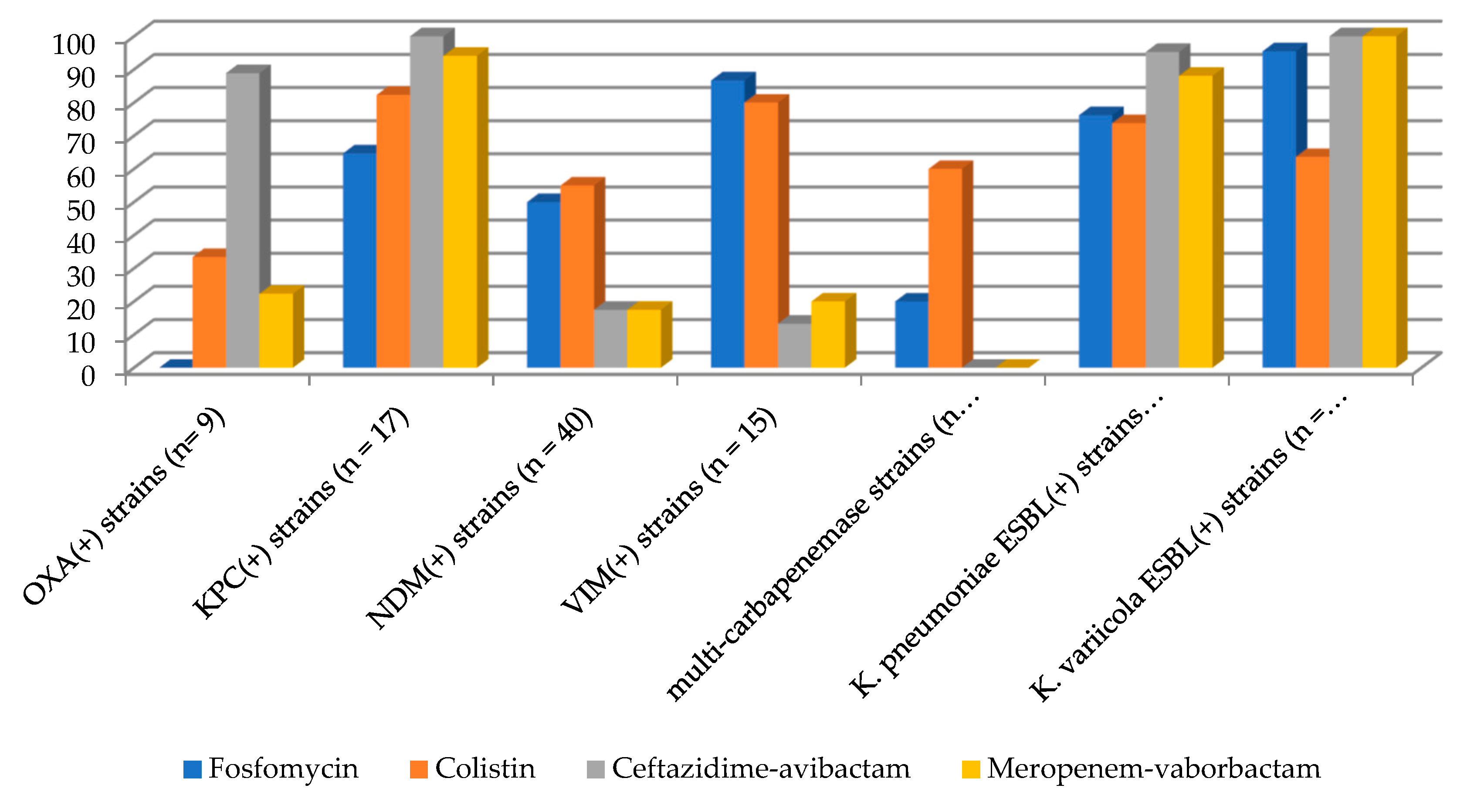
3.2. Identification of Strains and Antimicrobial Susceptibility Testing
3.3. Detection of Extended-Spectrum Beta-Lactamases and Carbapenemases
3.4. MIC Determination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karampatakis, T.; Tsergouli, K.; Behzadi, P. Carbapenem-Resistant Klebsiella Pneumoniae: Virulence Factors, Molecular Epidemiology and Latest Updates in Treatment Options. Antibiotics (Basel) 2023, 12, 234. [Google Scholar] [CrossRef]
- Rodríguez-Medina, N.; Barrios-Camacho, H.; Duran-Bedolla, J.; Garza-Ramos, U. Klebsiella Variicola : An Emerging Pathogen in Humans. Emerging Microbes & Infections 2019, 8, 973–988. [Google Scholar] [CrossRef]
- European Antimicrobial Resistance Surveillance Network (EARS-Net). Available online: https://www.ecdc.europa.eu/en/about-us/partnerships-and-networks/disease-and-laboratory-networks/ears-net (accessed on 9 October 2022).
- Cantón, R.; Akóva, M.; Carmeli, Y.; Giske, C.G.; Glupczynski, Y.; Gniadkowski, M.; Livermore, D.M.; Miriagou, V.; Naas, T.; Rossolini, G.M.; et al. Rapid Evolution and Spread of Carbapenemases among Enterobacteriaceae in Europe. Clinical Microbiology and Infection 2012, 18, 413–431. [Google Scholar] [CrossRef]
- Oelschlaeger, P.; Ai, N.; DuPrez, K.T.; Welsh, W.J.; Toney, J.H. Evolving Carbapenemases: Can Medicinal Chemists Advance One Step Ahead Of The Coming Storm? (Perspective). J Med Chem 2010, 53, 3013–3027. [Google Scholar] [CrossRef]
- Baraniak, A.; Izdebski, R.; Herda, M.; Fiett, J.; Hryniewicz, W.; Gniadkowski, M.; Kern-Zdanowicz, I.; Filczak, K.; Łopaciuk, U. Emergence of Klebsiella Pneumoniae ST258 with KPC-2 in Poland. Antimicrob Agents Chemother 2009, 53, 4565–4567. [Google Scholar] [CrossRef] [PubMed]
- Rekomendacje: Pałeczki Enterobacterales wytwarzające karbapenemazy (CPE) – Epidemiologia, diagnostyka, leczenie i profilaktyka zakażeń, 2022 – Narodowy program ochrony antybiotyków.
- Sekowska, A.; Gospodarek, E.; Kruszyńska, E.; Hryniewicz, W.; Gniadkowski, M.; Duljasz, W.; Kusza, K.; Wawrzyniak, K. [First isolation of metallo-beta-lactamase producing Klebsiella pneumoniae strain in Poland]. Anestezjol Intens Ter 2010, 42, 27–30. [Google Scholar] [PubMed]
- Pitout, J.D.D.; Peirano, G.; Kock, M.M.; Strydom, K.-A.; Matsumura, Y. The Global Ascendency of OXA-48-Type Carbapenemases. Clin Microbiol Rev 2019, 33, e00102-19. [Google Scholar] [CrossRef] [PubMed]
- Eucast: EUCAST. Available online: https://www.eucast.org/ (accessed on 3 October 2023).
- van der Zwaluw, K.; de Haan, A.; Pluister, G.N.; Bootsma, H.J.; de Neeling, A.J.; Schouls, L.M. The Carbapenem Inactivation Method (CIM), a Simple and Low-Cost Alternative for the Carba NP Test to Assess Phenotypic Carbapenemase Activity in Gram-Negative Rods. PLoS One 2015, 10, e0123690. [Google Scholar] [CrossRef] [PubMed]
- Kowalska-Krochmal, B.; Mączyńska, B.; Rurańska-Smutnicka, D.; Secewicz, A.; Krochmal, G.; Bartelak, M.; Górzyńska, A.; Laufer, K.; Woronowicz, K.; Łubniewska, J.; et al. Assessment of the Susceptibility of Clinical Gram-Negative and Gram-Positive Bacterial Strains to Fosfomycin and Significance of This Antibiotic in Infection Treatment. Pathogens 2022, 11, 1441. [Google Scholar] [CrossRef]
- Demirci-Duarte, S.; Unalan-Altintop, T.; Gulay, Z.; Sari Kaygisiz, A.N.; Cakar, A.; Gur, D. In Vitro Susceptibility of OXA-48, NDM, VIM and IMP Enzyme- Producing Klebsiella Spp. and Escherichia Coli to Fosfomycin. J Infect Dev Ctries 2020, 14, 394–397. [Google Scholar] [CrossRef]
- Aprile, A.; Scalia, G.; Stefani, S.; Mezzatesta, M.L. In Vitro Fosfomycin Study on Concordance of Susceptibility Testing Methods against ESBL and Carbapenem-Resistant Enterobacteriaceae. J Glob Antimicrob Resist 2020, 23, 286–289. [Google Scholar] [CrossRef]
- Appel, T.M.; Mojica, M.F.; De La Cadena, E.; Pallares, C.J.; Radice, M.A.; Castañeda-Méndez, P.; Jaime-Villalón, D.A.; Gales, A.C.; Munita, J.M.; Villegas, M.V. In Vitro Susceptibility to Ceftazidime/Avibactam and Comparators in Clinical Isolates of Enterobacterales from Five Latin American Countries. Antibiotics (Basel) 2020, 9, 62. [Google Scholar] [CrossRef] [PubMed]
- Zarakolu, P.; Eser, Ö.K.; Otlu, B.; Gürpınar, Ö.; Özakın, C.; Akalın, H.; Köksal, İ.; Ünal, S. In-Vitro Activity of Fosfomycin against Escherichia Coli and Klebsiella Pneumoniae Bloodstream Isolates and Frequency of OXA-48, NDM, KPC, VIM, IMP Types of Carbapenemases in the Carbapenem-Resistant Groups. J Chemother 2022, 34, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Galani, I.; Adamou, P.; Karaiskos, I.; Giamarellou, H.; Souli, M. Evaluation of ComASPTM Colistin (Formerly SensiTestTM Colistin), a Commercial Broth Microdilution-Based Method to Evaluate the Colistin Minimum Inhibitory Concentration for Carbapenem-Resistant Klebsiella Pneumoniae Isolates. J Glob Antimicrob Resist 2018, 15, 123–126. [Google Scholar] [CrossRef]
- Pruss, A.; Kwiatkowski, P.; Masiuk, H.; Jursa-Kulesza, J.; Bilska, I.; Lubecka, A.; Cettler, M.; Roszkowska, P.; Dołęgowska, B. Analysis of the Prevalence of Colistin Resistance among Clinical Strains of Klebsiella Pneumoniae. Ann Agric Environ Med. 2022, 29, 518–522. [Google Scholar] [CrossRef]
- Kazmierczak, K.M.; de Jonge, B.L.M.; Stone, G.G.; Sahm, D.F. In Vitro Activity of Ceftazidime/Avibactam against Isolates of Enterobacteriaceae Collected in European Countries: INFORM Global Surveillance 2012–15. Journal of Antimicrobial Chemotherapy 2018, 73, 2782–2788. [Google Scholar] [CrossRef]
- Pena, I.; Picazo, J.J.; Rodríguez-Avial, C.; Rodríguez-Avial, I. Carbapenemase-Producing Enterobacteriaceae in a Tertiary Hospital in Madrid, Spain: High Percentage of Colistin Resistance among VIM-1-Producing Klebsiella Pneumoniae ST11 Isolates. Int J Antimicrob Agents 2014, 43, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Feng, Y.; McNally, A.; Zong, Z. Occurrence of Colistin-Resistant Hypervirulent Klebsiella Variicola. J Antimicrob Chemother 2018, 73, 3001–3004. [Google Scholar] [CrossRef]
- Kim, S.J.; Jo, J.; Ko, K.S. Lipid A Modification-Induced Colistin-Resistant Klebsiella Variicola from Healthy Adults. J Med Microbiol 2023, 72. [Google Scholar] [CrossRef]
- Sękowska, A. Wrażliwość wielolekoopornych szczepów Klebsiella pneumoniae na połączenie ceftazydymu z awibaktamem. Forum Zakażeń 2019, 10, 269–273. [Google Scholar] [CrossRef]
- Wilson, W.R.; Kline, E.G.; Jones, C.E.; Morder, K.T.; Mettus, R.T.; Doi, Y.; Nguyen, M.H.; Clancy, C.J.; Shields, R.K. Effects of KPC Variant and Porin Genotype on the In Vitro Activity of Meropenem-Vaborbactam against Carbapenem-Resistant Enterobacteriaceae. Antimicrob Agents Chemother 2019, 63, e02048-18. [Google Scholar] [CrossRef]
- Bianco, G.; Boattini, M.; Comini, S.; Casale, R.; Iannaccone, M.; Cavallo, R.; Costa, C. Occurrence of Multi-Carbapenemases Producers among Carbapenemase-Producing Enterobacterales and in Vitro Activity of Combinations Including Cefiderocol, Ceftazidime-Avibactam, Meropenem-Vaborbactam, and Aztreonam in the COVID-19 Era. Eur J Clin Microbiol Infect Dis 2022, 41, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Sader, H.S.; Mendes, R.E.; Duncan, L.; Kimbrough, J.H.; Carvalhaes, C.G.; Castanheira, M. Ceftazidime-Avibactam, Meropenem-Vaborbactam, and Imipenem-Relebactam Activities against Multidrug-Resistant Enterobacterales from United States Medical Centers (2018-2022). Diagn Microbiol Infect Dis 2023, 106, 115945. [Google Scholar] [CrossRef]
- Gaibani, P.; Lombardo, D.; Bussini, L.; Bovo, F.; Munari, B.; Giannella, M.; Bartoletti, M.; Viale, P.; Lazzarotto, T.; Ambretti, S. Epidemiology of Meropenem/Vaborbactam Resistance in KPC-Producing Klebsiella Pneumoniae Causing Bloodstream Infections in Northern Italy, 2018. Antibiotics (Basel) 2021, 10, 536. [Google Scholar] [CrossRef] [PubMed]
- Camargo, C.H.; Yamada, A.Y.; de Souza, A.R.; Reis, A.D.; Santos, M.B.N.; de Assis, D.B.; de Carvalho, E.; Takagi, E.H.; Cunha, M.P.V.; Tiba-Casas, M.R. Genomic Diversity of NDM-Producing Klebsiella Species from Brazil, 2013–2022. Antibiotics (Basel) 2022, 11, 1395. [Google Scholar] [CrossRef]
- Ge, H.; Qiao, J.; Xu, H.; Liu, R.; Zhao, J.; Chen, R.; Li, C.; Chen, M.; Guo, X. Emergence of OXA-484-Producing <em>Klebsiella Variicola</Em> in China. IDR 2023, 16, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Fu, L.; Hu, X.; Liang, X.; Gong, G.; Xie, C.; Zhang, F.; Wang, Y.; Zhou, Y. Co-Occurrence of Klebsiella Variicola and Klebsiella Pneumoniae Both Carrying Bla KPC from a Respiratory Intensive Care Unit Patient. Infect Drug Resist 2021, 14, 4503–4510. [Google Scholar] [CrossRef]
- Zurfluh, K.; Poirel, L.; Nordmann, P.; Klumpp, J.; Stephan, R. First Detection of Klebsiella Variicola Producing OXA-181 Carbapenemase in Fresh Vegetable Imported from Asia to Switzerland. Antimicrob Resist Infect Control 2015, 4, 38. [Google Scholar] [CrossRef]
| Enzymes Producing by Klebsiella pneumoniae Complex Strains (n = 160) |
|---|
| OXA-48-, CTX-M1-positive K. pneumoniae strains (n = 2) |
| OXA-181-, CTX-M1-positive K. pneumoniae strains (n = 7) |
| KPC-, CTX-M1-positive K. pneumoniae strains (n = 12) |
| KPC-positive K. pneumoniae strains (n = 5) |
| NDM-, CTX-M1-positive K. pneumoniae strains (n = 33) |
| NDM-positive K. pneumoniae strains (n = 7) |
| VIM-, CTX-M1 positive K. pneumoniae strains (n = 7) |
| VIM-positive K. pneumoniae strains (n = 8) |
| NDM-, OXA-181-, CTX-M1-positive K. pneumoniae strains (n = 13) |
| NDM-, OXA-181-, CTX-M1-, CTX-M9-positive K. pneumoniae strains (n = 1) |
| VIM-, NDM-, CTX-M1-positive K. pneumoniae strains (n = 1) |
| ESBL-positive K. pneumoniae strains (n = 42) |
| ESBL-positive K. variicola strains (n = 22) |
| Antimicrobial | K. pneumoniae Carbapenemase-Positive Strains (n = 96) | K. pneumoniae ESBL-Positive Strains (n = 42) | K. variicola ESBL-Positive Strains (n = 22) | |||
|---|---|---|---|---|---|---|
| MIC50 | MIC90 | MIC50 | MIC90 | MIC50 | MIC90 | |
| Fosfomycin | 24 | 48 | 12 | 32 | 4 | 16 |
| Colistin | 0.75 | 8 | 0.5 | 4 | 1.5 | 4 |
| Ceftazidime-avibactam | 16 | 128 | 0.75 | 2 | 0.5 | 0.5 |
| Meropenem-vaborbactam | 24 | 128 | 0.25 | 1.5 | 0.25 | 0.5 |
| MIC Value (mg/L) |
K. pneumoniae Carbapenemase-Positive strains (n = 96) | K. pneumoniae ESBL-Positive Strains (n = 42) | K. variicola ESBL-Positive Strains (n = 22) |
|---|---|---|---|
| 4 | 3 | 4 | 5 |
| 8 | 5 | 6 | 4 |
| 16 | 16 | 12 | 6 |
| 32 | 24 | 10 | 6 |
| 48 | 1 | 0 | 0 |
| 64 | 17 | 2 | 0 |
| 128 | 18 | 4 | 1 |
| 256 | 7 | 1 | 0 |
| >256 | 5 | 3 | 0 |
| MIC Value (mg/L) |
K. pneumoniae Carbapenemase-Positive Strains (n = 96) | K. pneumoniae ESBL-Positive Strains (n = 42) | K. variicola ESBL-Positive Strains (n = 22) |
|---|---|---|---|
| 0.25 | 2 | 1 | 4 |
| 0.5 | 29 | 20 | 5 |
| 1 | 25 | 8 | 2 |
| 2 | 3 | 2 | 3 |
| 8 | 11 | 6 | 8 |
| 16 | 13 | 5 | 0 |
| >16 | 12 | 0 | 0 |
| MIC Value(mg/L) | K. pneumoniae Carbapenemase-Positive Strains (n = 96) | K. pneumoniae ESBL-positive Strains (n = 42) | K. variicola ESBL-Positive Strains (n = 22) | |||
|---|---|---|---|---|---|---|
| CZA | MV | CZA | MV | CZA | MV | |
| 0.032 | 0 | 1 | 0 | 1 | 0 | 1 |
| 0.047 | 0 | 1 | 1 | 2 | 2 | 0 |
| 0.064 | 0 | 1 | 0 | 1 | 1 | 2 |
| 0.094 | 0 | 1 | 0 | 1 | 0 | 3 |
| 0.125 | 0 | 0 | 0 | 6 | 0 | 0 |
| 0.19 | 0 | 0 | 0 | 2 | 0 | 0 |
| 0.25 | 0 | 1 | 5 | 0 | 0 | 4 |
| 0.38 | 1 | 0 | 1 | 3 | 4 | 2 |
| 0.5 | 2 | 1 | 3 | 6 | 5 | 4 |
| 0.75 | 3 | 1 | 3 | 1 | 4 | 3 |
| 1 | 4 | 4 | 12 | 3 | 3 | 1 |
| 1.5 | 11 | 6 | 7 | 0 | 0 | 1 |
| 2 | 8 | 6 | 6 | 6 | 3 | 1 |
| 3 | 1 | 1 | 0 | 2 | 0 | 0 |
| 4 | 4 | 2 | 2 | 3 | 0 | 0 |
| 8 | 1 | 3 | 1 | 2 | 0 | 0 |
| 12 | 0 | 0 | 0 | 1 | 0 | 0 |
| 16 | 2 | 2 | 0 | 0 | 0 | 0 |
| 32 | 4 | 2 | 0 | 0 | 0 | 0 |
| 48 | 1 | 8 | 0 | 0 | 0 | 0 |
| 64 | 3 | 5 | 1 | 0 | 0 | 0 |
| 96 | 1 | 2 | 0 | 0 | 0 | 0 |
| 128 | 6 | 3 | 0 | 0 | 0 | 0 |
| 256 | 16 | 18 | ||||
| >256 | 28 | 27 | 0 | 2 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





