Introduction
Diastematomyelia (split cord syndrome) is a type of spinal dysraphism that occurs when there is a longitudinal split in the spinal cord (1). The split can be due to a bony spur or fibrous septum, which causes both neurological and orthopaedic complaints in the patient. It is also associated with cutaneous symptoms such as a dimple, hair patch, etc. which further aids in the diagnosis of diastematomyelia (2). Most cases are diagnosed in early childhood when the child starts to complain of lower back pain, scoliosis, lower limb weakness and paresthesia. This slowly progresses to complete motor and sensory loss with loss of bowel and bladder control. Radiological imaging like X-rays, MRI, and CT scans along with clinical presentation diagnoses diastematomyelia accurately. The treatment of choice for this condition is the surgical removal of the bony spur along with resection and repair of the deformity (3).
Case Presentation:
A 54-year-old Indian female patient was admitted to Hospital with a clinical complaint of lower back pain for 5 months. The patient was relatively asymptomatic before 5 months following which she developed lower back pain which was not relieved with medications. This was associated with a burning sensation in both feet and difficulty in standing up. During this time, the patient consulted many doctors and an MRI of the spine was suggested. After this, she came to our institute for further care.
Negative history of trauma, fall, bowel and bladder dysfunction, and altered gait.
Past History
The patient has no significant past history.
Physical Examination
On examination, the patient's general condition was good. She was conscious and well-oriented to time, place and person. A nervous system examination revealed a Glass Glow Coma Scale (GCS) score of E4 M6 V5. Her pupils were bilaterally equal in size and diameter and reactive to light. Extraocular Movements (EOM) were normal. Muscle tone was normal in the upper limbs but there was hypertonia in the lower limbs, and strength of the limbs was level 4. There was bilateral lower limb hyperreflexia and bilateral plantar upgoing with normal reflexes in the upper limbs. Also, there was hypoesthesia below the level of the umbilicus.
Lab Examination
Table 1.
Blood Examination.
Table 1.
Blood Examination.
| Test |
Observed value |
Reference Range |
| Haemoglobin |
12.6 g/dl |
(12-18) |
| WBC |
7.79 kU/L |
(5.2-12.4) |
| RBC |
4.61*106/ul |
(4.5-5.5) |
| Haematocrit |
41% |
(40-50) |
| Platelet counts |
392 kU/L |
(130-400) |
| Neutrophiles |
76% |
(49-74) |
| Lymphocyte |
15% |
(26-46) |
| Monocyte |
07% |
(2-12) |
| Eosinophil |
02% |
(0-5) |
| Basophil |
00% |
(0-2) |
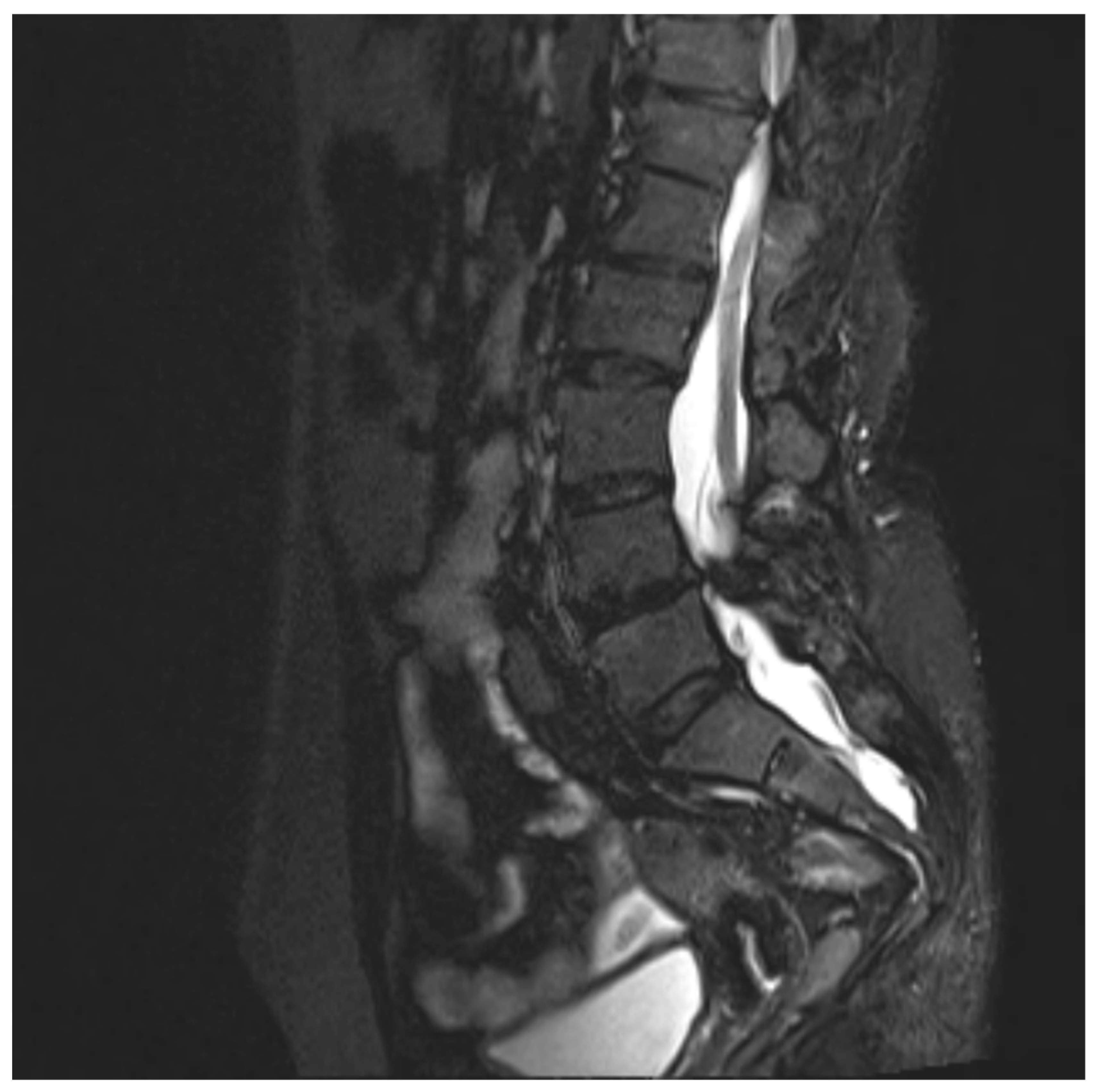
Radiological Imaging (MRI Spine)
Observation:
Diastematomyelia (type 1) from D11-L4 vertebral level with tethered cord syndrome and spina bifida occulta present.
Dural ectasia from D12 to S3 vertebral levels are seen.
D10-D11 level: Diffuse disc bulge with ligamentum flavum hypertrophy causing effacement over anterior and posterior thecal sac, central canal stenosis and right neural foraminal narrowing with resultant mild compression over right exiting nerve root with evidence of intramedullary T2WI/STIR hyperintensity in the spinal cord, suggestive of compressive myelomalacia.
Degenerative disc disease was noted at multiple lower dorsal and lumbar levels with compression of nerve roots at various levels as described above.
Figure 1.
Sagittal MRI T2WI-STir image showing low lying tethered cord.
Figure 1.
Sagittal MRI T2WI-STir image showing low lying tethered cord.
Figure 2.
Axial T2WI image showing Dual hemi cord within two dural sac separated by intervening bony septum(Type i diastematomyelia).
Figure 2.
Axial T2WI image showing Dual hemi cord within two dural sac separated by intervening bony septum(Type i diastematomyelia).
Following surgery, there has been improvement in the MRI scans.
Treatment
The patient was given Pregabalin 75 mg once a day, Diclofenac gel to be applied twice a day on the affected part, and Paracetamol 500 mg as and when needed for pain all for 10 days. The patient was advised surgery and she underwent decompressive laminectomy from the D11-L4 vertebra. She had no post-surgery complications and was discharged once her condition improved.
Follow up Case
The patient was followed up for around 6 months and there has been no recurrence or aggravation.
Diagnosis
The patient was given appropriate treatment and there was significant improvement in her condition. Based on the clinical presentation, imaging findings, and response to treatment, the patient was diagnosed with Diastematomyelia.
Discussion and Literature
Diastematomyelia, also known as diastomyelia or split cord malformation, is a congenital disorder that most commonly affects females (4). It occurs due to the presence of a connection between the neural tube and the amniotic cavity or primitive bowel (5). It is often associated with other vertebral anomalies like spina bifida, butterfly vertebra, etc.
There is a formation of osseous, cartilaginous, or fibrous septum in the central portion of the spinal canal anchoring the cord to vertebrae. This in turn results in partial or complete splitting of the spinal cord into two. Each hemicord has its own anterior spinal artery supply. The division usually reunites at the distal point, if it doesn’t unite, then it is called diplomyelia. Diastematomyelia acts as a barrier that slows down the normal growth of the spinal cord, resulting in neurocutaneous symptoms.
Diastematomyelia can be classified into two, depending upon the separation of dura (6):
- I.
Double dural sacs with common midline spur- symptomatic and more severe
- II.
Single dural sac containing both hemicords with the presence of a septum- can be asymptomatic and is less severe.
The clinical features of this condition can present at any age, although most commonly it occurs during childhood. The most common site that is affected is the lower thoracic and upper lumbar vertebra. The symptoms begin with stigmata of cutaneous manifestation like a dimple, hairy patch, lipoma, hemangioma, etc. which is followed by neurological symptoms: lower back pain, leg weakness, lower limb deformities, and scoliosis (7). With increasing age, due to tethered cord syndrome, neurological impairment progresses to bowel/bladder dysfunction along with gradual motor and sensory loss. The presence of spur further results in neurological deterioration. The clinical presentation is related to the degree of strain placed on the spinal cord with time. The patient also has associated foot abnormalities such as club foot. In some cases, the condition remains silent until the occurrence of acute trauma.
Once there is suspicion of diastematomyelia, a plain X-ray is done to identify bony malformations. The characteristic finding on the X-ray is the presence of a bony spur and the widening of interpedicular distance at the level of the affected vertebra (8). X-ray being non-specific, other radiological modalities are used. MRI is the first choice for screening, diagnosing, and planning the treatment of diastematomyelia. The laminar fusion along with neural arch defect is a good predictor of diastematomyelia. To get detailed bone anatomy, intradural and extradural pathology, a CT scan is preferred. It can also be diagnosed prenatally by fetal USG, which shows an extra posterior echogenic focus between fetal spinal laminae with splaying of posterior elements (9). Early prenatal diagnosis results in early intervention and thus better prognosis.
The treatment of diastematomyelia depends upon symptom severity, classification, and MRI findings. In asymptomatic individuals, there is no need for treatment. Regular follow-up with proper neurological examination should be done. The ones with symptoms require surgery, however, the role of surgery remains controversial. Spur or septum removal surgery is done first and this is usually followed by surgical correction of the spine (10). Merely, removing the spur or septum doesn’t guarantee a regain of neurological function but it prevents further neurological impairment. Spinal surgery includes laminoplasty which is preferred over laminectomy. It may be done with or without dural sac resection and repair. It is better to correct dural abnormality as well to avoid cord tethering. Overall, the spinal surgery decompresses the neural structures thus improving neurological symptoms. A post-surgery CT scan is done to ensure proper resection of the defect.
Conclusion
Diastematomyelia, a congenital disorder of the spinal cord can present with a wide spectrum of clinical symptoms ranging from cutaneous to orthopaedic to neurological features. Various diagnostic modalities ranging from X-rays to advanced imaging like MRI, and CT scans play an important role in knowing the anatomy, diagnosing, and treating this condition. Even though it can be diagnosed prenatally via fetal sonography, the efficacy of surgical interventions remains debatable. Nevertheless, spine and dural sac resection following the bony spur removal have resulted in significant improvement in neurological symptoms, especially in type 1 diastematomyelia.
Ethical Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mamo G, Batra R, Steinig J. A Case of Diastematomyelia Presenting With Minimal Neurologic Deficits in a Middle-Aged Patient. Cureus [Internet]. 2021 Jan 11 [cited 2023 Dec 22];13(1). Available from: /pmc/articles/PMC7872494/. [CrossRef]
- Zaleska-Dorobisz U, Bladowska J, Biel A, Pałka LW, Hołownia D. MRI diagnosis of diastematomyelia in a 78-year-old woman: Case report and literature review. Pol J Radiol [Internet]. 2010 [cited 2023 Dec 22];75(2):82. Available from: /pmc/articles/PMC3389875/.
- Sergeenko (Pavlova) OM, Savin DM, Ryabykh SO. Treatment of spinal deformity with diastematomyelia type I: one-stage, two-stage surgery and new technique (vertebral column resection through wide bony septum). Childs Nerv Syst [Internet]. 2022 Jan 1 [cited 2023 Dec 22];38(1):163–72. Available from: https://pubmed.ncbi.nlm.nih.gov/34626222/. [CrossRef]
- Doherty D, Walker WO. Neural Tube Defects. Encyclopedia of the Neurological Sciences. 2014 Jan 1;360–5. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/diastematomyelia.
- Vissarionov S V., Krutelev NA, Snischuk VP, Alam M, Kravchenko AP, Zheng YP, et al. Diagnosis and treatment of diastematomyelia in children: a perspective cohort study. Spinal Cord Ser Cases [Internet]. 2018 [cited 2023 Dec 22];4:109. Available from: /pmc/articles/PMC6300541/. [CrossRef]
- El-Feky M, Salam H. Diastematomyelia. Radiopaedia.org [Internet]. 2009 Nov 1 [cited 2023 Dec 22]; Available from: http://radiopaedia.org/articles/7419.
- Morrow MJ. Encyclopedia of the Neurological Sciences (Second Edition). Encyclopedia of the Neurological Sciences (Second Edition) [Internet]. 2014 [cited 2023 Dec 22];892–3. Available from: http://www.sciencedirect.com:5070/referencework/9780123851581/encyclopedia-of-the-neurological-sciences.
- Bell D, Weerakkody Y. Widening of interpedicular distance. Radiopaedia.org. 2010 Mar 18; Available from: https://radiopaedia.org/articles/widening-of-interpedicular-distance.
- Has R, Yuksel A, Buyukkurt S, Kalelioglu I, Tatli B. Prenatal diagnosis of diastematomyelia: presentation of eight cases and review of the literature. Ultrasound in Obstetrics and Gynecology [Internet]. 2007 Nov 1 [cited 2023 Dec 22];30(6):845–9. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/uog.4066. [CrossRef]
- Vissarionov S V., Krutelev NA, Snischuk VP, Alam M, Kravchenko AP, Zheng YP, et al. Diagnosis and treatment of diastematomyelia in children: a perspective cohort study. Spinal Cord Ser Cases [Internet]. 2018 [cited 2023 Dec 22];4:109. Available from: /pmc/articles/PMC6300541/. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).