Introduction
A brain injury sustained during fetal or early childhood development is typically the cause of atrophy or hypoplasia of one cerebral hemisphere (hemiatrophy), which is known as Dyke-Davidoff-Masson syndrome (DDMS). Dyke, Davidoff, and Masson first reported it in a group of nine patients who had simple skull X-ray abnormalities along with hemiplegia [1,8]. The degree of brain damage affects the clinical features, which can vary. Cerebral hemiatrophy, facial asymmetry, contralateral hemiplegia or hemiparesis, seizures, speech and language impairments, mental retardation, and, on occasion, behavioural abnormalities and psychiatric symptoms are among the clinical features of DDMS. Cerebral hemiatrophy with ipsilateral compensatory enlargement of the skull and sinuses are characteristic radiological findings. Most of the reported cases of the syndrome were in adults and adolescents [1–3].
Case Presentation
Presenting the case of a 26-year-old male who came to Medicine OPD with chief complaints of generalized weakness, dizziness, vomiting, difficulty walking and frequent episodes of seizures for a week. He also had an episode of generalized tonic-clonic seizure. So, he was hospitalized for management and to identify the cause behind paresis and seizures despite being on antiepileptics. The patient had a normal antenatal course and was born full-term. The patient had a complicated perinatal period with no spontaneous induction of labour and a failed attempt at forceps delivery followed by emergency LSCS. The patient developed left-handed grip and spasticity at 9 months of age along with delayed milestones like inability to sit following which a diagnosis of cerebral palsy was made. He had his first seizure at the age of 2.5 years and has been on antiepileptics since. There is no significant family history of similar or any other neurological presentation.
Physical Examination
On general physical examination, hypertonia on the right with hypotonia on the left side of the body was noted. Decreased knee and ankle reflexes were seen on the right side with normal deep tendon reflexes on the left. Abnormal plantar reflex with extension of toes was noted on the right side with normal flexion of toes on left. Bilateral nystagmus was present. Power was normal in both the right and left halves. Vitals were within range and examination of other organ systems revealed nothing significant.
Laboratory Investigation
After admission, all the baseline investigations and thorough lab work for young stroke were done which included CBC with differential count, serum electrolytes, liver, thyroid and renal function tests, serum protein and albumin levels, and blood clotting tests ( PT, APTT, INR ). All laboratory investigations were within the reference range.
Radiological Examination
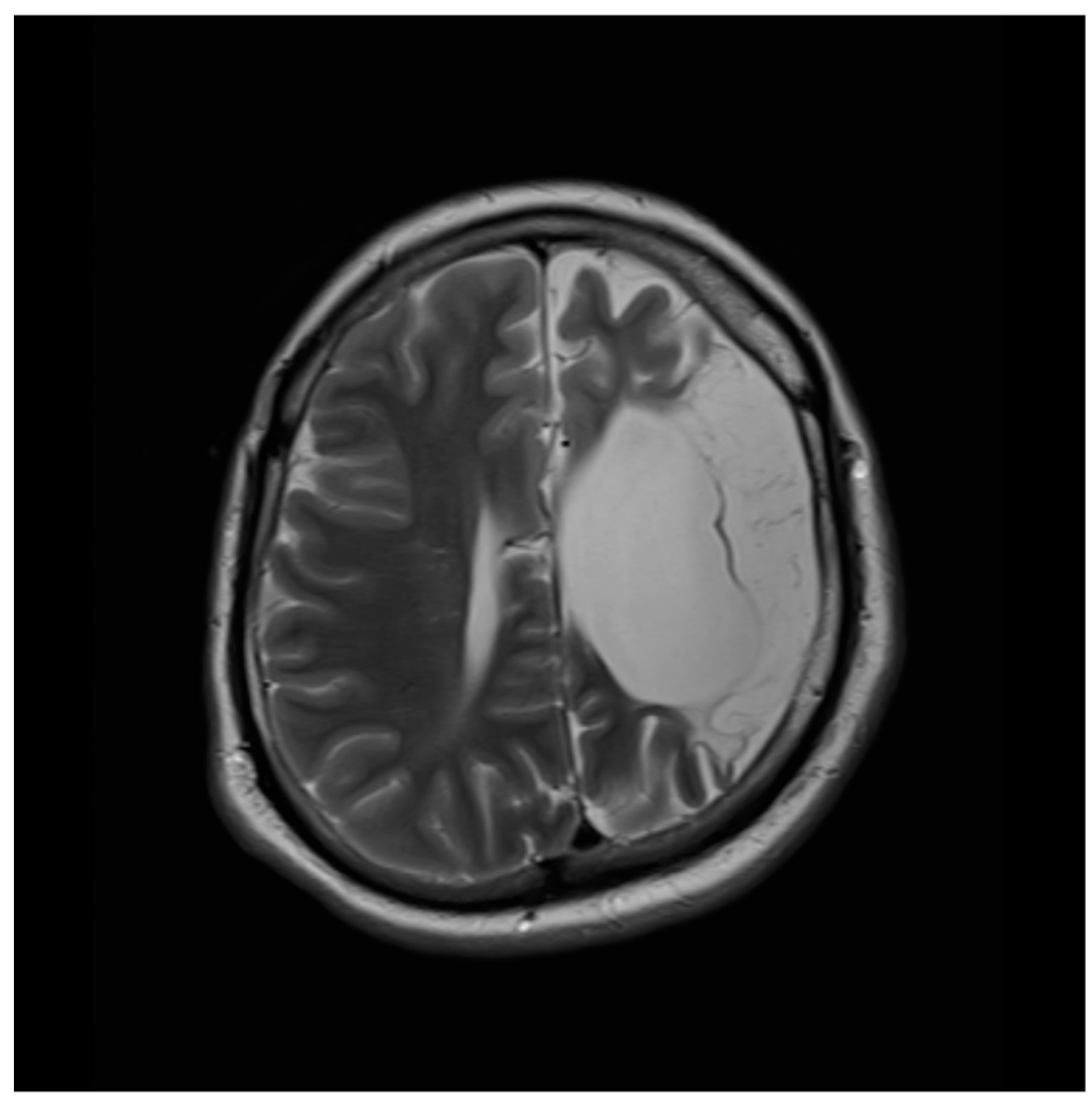
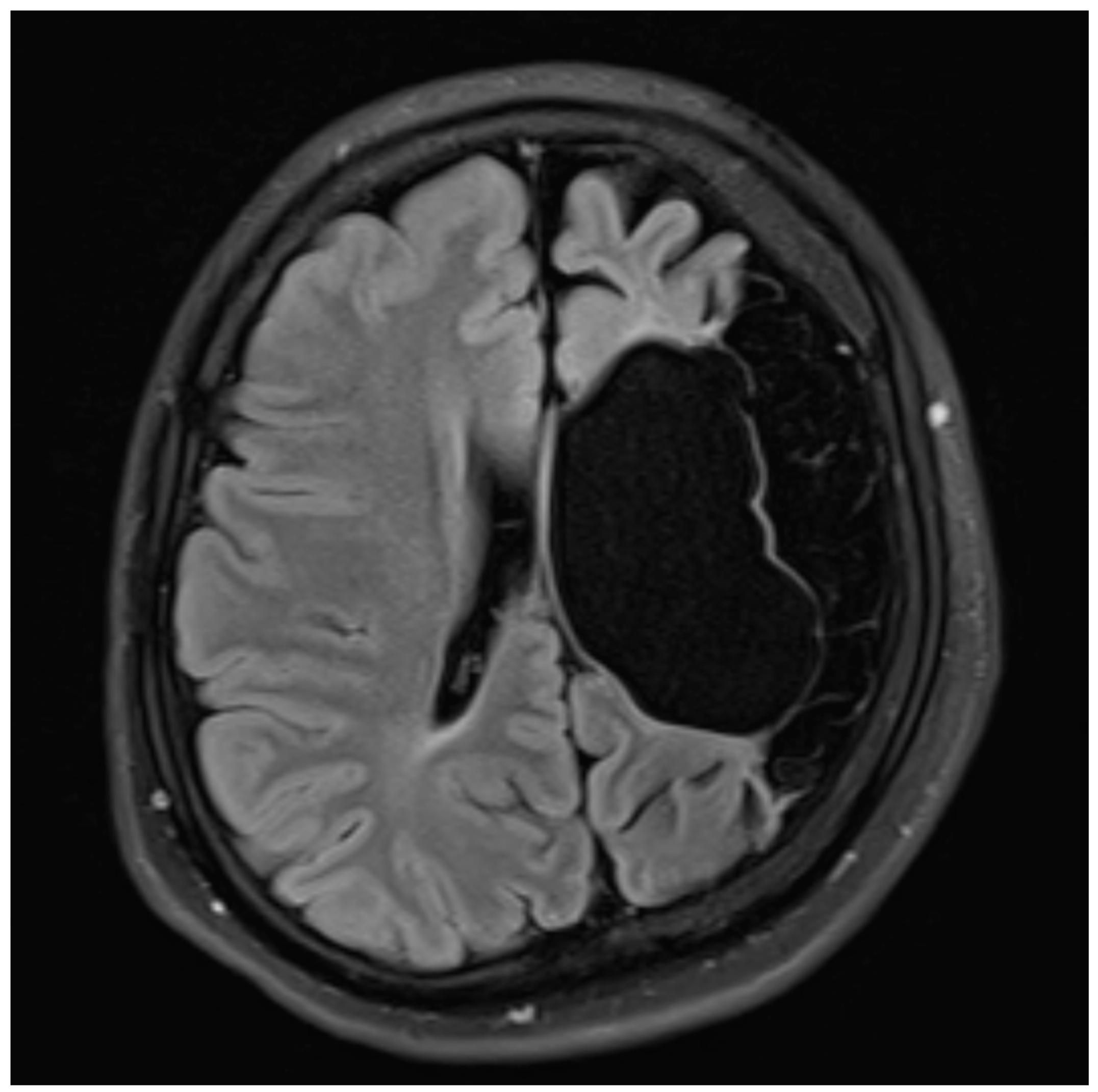
Chest X-ray and abdominal USG were done which came out to be normal. Later, an MRI was done to find out the cause as the patient had an episode of generalized tonic-clonic seizures, recurrent convulsions and motor impairment. MRI revealed hemiatrophy of the left cerebral hemisphere. An area of gliosis with cystic encephalomalacia in the left front-parietal-temporal lobe left corona radiata and left basal ganglia with resultant ex vacuo dilatation of left ventricle suggestive of previous brain trauma was also noted. MRI also revealed Wallerian degeneration of the left cerebral peduncle and mild thickening of calvaria on the left side. There was a mildly prominent left frontal sinus indicating hyperpneumatization. A mild line shift of approximately 3.6 mm towards the left side and diffuse thinning of the corpus callosum was also noted.
Figure 1.
MRI T2WI of the patient with significant left cerebral hemisphere atrophy.
Figure 1.
MRI T2WI of the patient with significant left cerebral hemisphere atrophy.
Figure 2.
MRI Flair of the patient with significant left cerebral hemisphere atrophy.
Figure 2.
MRI Flair of the patient with significant left cerebral hemisphere atrophy.
Diagnosis
The clinical presentation and imaging results were correlated, and DDMS was ultimately diagnosed.
Management
Physiotherapy and anti-epileptic drugs made up his treatment plan. For focused intervention and care, he was referred to inpatient neurology services. At the time of discharge, vitals were normal, hypotonia on the left, decreased knee and ankle reflexes on the right, bilateral nystagmus as well as abnormal plantar reflex on the right side were normalized. There was still hypertonia on the right side. The rest of the systemic examination was also normal.
Follow Up
The patient was advised at the time of discharge to follow up after 10 days in both the medicine and neurology department. The patient was followed up regularly for the next 8 months with no recurrence of seizures or any other symptoms.
Discussion
Named for the three physicians who first described it in 1933—C.G. Dyke, L.M. Davidoff, and C.B. Masson—Dyke-Davidoff-Masson syndrome (DDMS) is a rare neurological condition characterised by atrophy or hypoplasia of one cerebral hemisphere (hemiatrophy). They described it in a series of nine patients who presented with hemiparesis, facial asymmetry, seizures, intellectual disability, and findings of pneumato-encephalographic changes on skull radiography [4,8]. Although the precise cause of DDMS is still unknown, prior research has linked the disorder to either an in-utero brain injury (congenital subtype), which develops in infancy, or a perinatal, postnatal or early childhood brain insult that develops late in life( acquired subtype) [4]. Vascular injury, vascular malformations, in-utero infections, and congenital anomalies are examples of prenatal causes. The following are examples of perinatal and postnatal causes: perinatal/postnatal infections, perinatal hypoxia, tumours, trauma, intracranial haemorrhage, stroke and febrile seizures [5]. Numerous ischemia events brought on by these factors are thought to be the potential cause of cerebral atrophy and the corresponding increasing neuro deficit. These episodes are thought to limit the generation of brain-derived neurotrophic factors, which in turn cause cerebral atrophy [1]. In this case, complicated perinatal history can be a potential factor responsible.
Depending on the severity of the injury, DDMS can appear clinically with a wide range of features. Among the more notable characteristics include intellectual disability, facial asymmetry, contralateral hemiparesis, and seizures (both localized and generalized). There have also been descriptions of related psychiatric diseases and neuropsychiatric symptoms [4]. Any hemisphere and both sexes are susceptible, however, left-sided involvement and male gender are more prevalent [2]. In this case, a male patient presented with drug-resistant seizures, episodes of GTCS, motor weakness manifesting as difficulty in walking, and diminished DTRs on the right side. Right-sided symptoms indicative of left-side cerebral involvement are also consistent with previous research findings. In addition, the patient is a known case of cerebral palsy which is a rare finding.
The two gold standard imaging modalities that are most useful in the diagnosis of DDMS are CT and MRI. Prominent cortical sulci, dilated lateral ventricles, cerebral hemiatrophy, hyperpneumatization of the frontal sinus, and compensatory hypertrophy of the skull are characteristic imaging findings associated with DDMS. As the patient ages, these imaging results become increasingly apparent. Compensatory calvarial involvement is seen when a cerebral injury happens during the intrauterine period or before the age of three [1]. In this case, MRI findings suggestive of DDMS were: Hemiatrophy of the left cerebral hemisphere, area of gliosis and cystic encephalomalacia in the left fronto-parieto-temporal lobe, left corona radiata and left basal ganglia with mild thickening of left calvaria on left side and mildly prominent left frontal sinus.
The disorders with cerebral hemiatrophy or midline structural shift disorders, like hemimegalencephaly, Sturge-Weber syndrome, Rasmussen encephalitis, basal ganglia germinoma, Fishman syndrome, Silver-Russell syndrome, and linear nevus syndrome, are the main focus of the differential diagnosis of DDMS [6]. A detailed history, careful examination and neuroimaging help in making a clear diagnosis. The calvarial changes are absent in Rasmussen’s syndrome. Although the clinical characteristics of basal ganglia germinoma are comparable, brain imaging shows cystic regions, focal haemorrhages, mild surrounding oedema, and calvarial alterations [7]. A congenital anomaly of neural proliferation hemimegalencephaly is characterized by the affected hemisphere’s excessive growth and not cerebral atrophy [6]. The presence of cerebral tramtrack calcification, the absence of midline shift, and the port-wine facial nevus are the characteristics that set Sturge-Weber Syndrome apart. Poor growth, delayed bone age, clinodactyly, normal head circumference, normal IQ, the traditional facial phenotype (triangular face, broad forehead, short pointed chin, and narrow wide mouth), and hemihypertrophy are the characteristics of Silver-Russel syndrome [9]. Typical face nevus, mental impairment, recurrent seizures, and unilateral ventricular dilatation suggest cerebral hemiatrophy are the hallmarks of linear nevus syndrome [2]. Fishman syndrome patients typically experience seizures in addition to ocular lipodermoid, unilateral cranial lipoma, cortical calcification, and hemiatrophy [6]. All these were carefully considered in this patient before making a diagnosis of DDMS.
The prudent use of antiseizure medications is part of the medical treatment for DDMS. Hemispherectomy is a surgical treatment option for drug-resistant seizures that has an 85% success rate in cured patients. Speech, occupational, and physical therapy are other components of long-term care [7,10]. The prognosis of DDMS is uncertain and largely dependent on how early the disease is discovered due to its distinctive clinical features and broad spectrum of presentations. A better prognosis is achieved when the disease is identified early and treated appropriately [12]. The prognosis is poorer for patients who suffer protracted, recurring seizures and whose hemiparesis begins before the age of two [11]. Antiepileptics along with physiotherapy and regular follow up formed the basal management in this case.
Conclusions
In conclusion, it should be noted that DDMS may present with a wide range of radiological and clinical symptoms. However, the majority of the time, the diagnosis was made easier by the characteristic radiological indicators, which include cerebral hemiatrophy and compensatory hypertrophy of the ipsilateral skull. Because it’s a rare syndrome, an unskilled eye could easily misdiagnose it. To adequately manage patients, doctors must be educated about the signs, symptoms, risk factors, and diagnostic aspects of DDMS. The results of this study offer guidance in diagnosing and treating DDMS.
Patient Consent:
The patient in the study was provided with detailed information about the purpose, procedures, risks, benefits, and confidentiality measures associated with the research. The patient was given ample time to review the informed consent, ask questions, and make an informed decision regarding their participation. Written informed consent was obtained from the patient prior to their involvement in the study.
Conflict of Interest
The authors of this report declare that they have no conflicts of interest to disclose.
References
- Younas A, Saim M, Maqsood H, Younus S, Hassan Raza M. Dyke-Davidoff-Masson Syndrome: A Case Report and Review of Literature. Cureus. 2020;12(12):e11919. Published 2020 Dec 5. [CrossRef]
- Behera MR, Patnaik S, Mohanty AK. Dyke-Davidoff-Masson syndrome. J Neurosci Rural Pract. 2012;3(3):411-413. [CrossRef]
- Aldhaleei WA, Bhagavathula AS, Alshehhi F. Dyke-Davidoff-Masson syndrome presenting as recurrent chronic headache in late adult life. Brain Circ. 2020;6(2):123-125. Published 2020 Jun 26. [CrossRef]
- Al-Smair A, Abdel Hafez S, Saadeh A, Al-Ali A. An Adult With Dyke-Davidoff-Masson Syndrome: A Case Report. Cureus. 2022;14(3):e23315. Published 2022 Mar 19. [CrossRef]
- Gupta R, Joshi S, Mittal A, Luthra I, Mittal P, Verma V. Magnetic resonance imaging depiction of acquired Dyke-Davidoff-Masson syndrome with crossed cerebro-cerebellar diaschisis: Report of two cases. J Pediatr Neurosci. 2015;10(3):294-296. [CrossRef]
- Wang B, Jiang W, Yan W, et al. Clinical characteristics and neuroimaging findings of seven patients with Dyke Davidoff Masson syndrome. BMC Neurol. 2021;21(1):213. Published 2021 May 31. 31 May. [CrossRef]
- Adebayo PB, Bakare A, Bello MM, Olaewe OD, Wahab KW. Dyke-Davidoff-Masson syndrome in a Nigerian. Epilepsy Behav Case Rep. 2016;7:10-12. Published 2016 Sep 15. [CrossRef]
- Dyke CG, Davidoff LM, Masson CB. Cerebral hemiatrophy and homolateral hypertrophy of the skull and sinuses. Surg Gynecol Obstet. 1933;57:588–600.
- Uduma FU, Emejulu JK, Motah M, Okere PC, Ongolo PC, Muna W. Differential diagnoses of cerebral hemiatrophy in childhood: a review of literature with illustrative report of two cases. Glob J Health Sci. 2013;5(3):195-207. Published 2013 Mar 20. [CrossRef]
- Kumar NV, Gugapriya TS, Guru AT, Kumari SN. Dyke-Davidoff-Masson syndrome. Int J Appl Basic Med Res. 2016;6(1):57-59. [CrossRef]
- Acharya S, Andhale A, Shukla S, Bhansali PJ, Kabra R, Kumar S. Dyke-Davidoff-Masson Syndrome as a Predecessor of Recurrent Seizures in an Adult Male: A Report of a Rare Case. Cureus. 2022;14(9):e28838. Published 2022 Sep 6. [CrossRef]
- Khan MZ, Mahapatra SS, Patel T, Razzaq W, Khawaja UA. Presentation of Dyke-Davidoff-Masson Syndrome in a 32-Year-Old Female: Report of a Rare Case With a Literature Review. Cureus. 2023;15(6):e41101. Published 2023 Jun 28. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).