1. Introduction
The postpartum period entails significant physical, psychosocial and social changes for women as they adapt to a new situation. Therefore, it is known as a period of special vulnerability related to maternal mental health [
1]. Approximately 9.6% to 19.2% of mothers experience a major or minor depressive episode during the first 12 months after childbirth [
2]. Thus, one of the main complications during the postpartum period is postpartum depression (PPD) [
3,
4].
Globally, it is estimated that 1 in 5 women will develop PPD. However, the prevalence of PPD varies significantly across geographic areas and cultures. Southern Africa has the highest reported prevalence (39.96%), eastern Europe (16.62%) and southern Europe (16.34%) show intermediate prevalence and Oceania (11.11%) has some of the lowest reported figures [
5,
6,
7]. Additionally, countries with higher income or developed countries have significantly lower prevalence than lower-income or developing countries [
5]. However, these figures may underestimate the true extent of the problem due to barriers to detection and the stigma associated with mental illnesses in the perinatal context. Some estimates suggest that greater than 50% of women with PPD are not diagnosed [
6]. PPD generally occurs within 4 weeks after childbirth and can last 6 months or longer after childbirth, although some authors indicate that it could last up to 2 years after childbirth [
4,
8,
9,
10].
Breastfeeding provides multiple demonstrated benefits at the physical, cognitive and social levels for both the mother and the newborn [
11,
12,
13]. However, the psychological benefits, especially those concerning PPD, are still largely unknown. Some studies indicate that depression during pregnancy and postpartum is one of the factors that can contribute to breastfeeding failure. Other studies also suggest an association between breastfeeding and PPD, suggesting that PPD may reduce rates of breastfeeding and that breastfeeding may decrease the risk of PPD. Additionally, there is evidence that breastfeeding can prevent PPD or help symptoms to recede more quickly. However, the direction of this association is still uncertain [
14,
15].
Due to all these reasons, PPD has become a significant health issue that affects not only women’s health by increasing maternal morbidity and mortality but also a newborn’s feeding patterns and, consequently, behavioural, emotional and cognitive development during early childhood [
5,
16].
Group interventions during the postpartum period, during which women share a safe space of mutual acceptance and understanding, have proven effective in improving depressive symptoms and empowering women to cope with their situation [
17]. Additionally, there are also encouraging results demonstrating that group interventions are effective at maintaining breastfeeding during the postpartum period, especially when this peer support is combined with the leadership of a healthcare professional or an International Board Certified Lactation Consultant (IBCLC) [
18]. Likewise, there is evidence of the positive impact that breastfeeding has on women’s mental health by enhancing their well-being, increasing perceived self-efficacy and promoting interaction with the newborn [
19,
20].
At the individual level, affective characteristics, or the “qualities that represent the typical ways of feeling of individuals”, are particularly important determinants of breastfeeding practices [
21]. One of these key affective characteristics is self-efficacy, defined by Bandura [
22] as “the belief in one’s capabilities to organize and execute the courses of action required to produce certain achievements or results”. In contrast, low levels of self-efficacy have been shown in previous studies to be a risk factor for the development of PPD [
23].
Thus, the mental health of the mother constitutes a significant underlying factor linked to barriers and reduced rates of intention, initiation and maintenance of breastfeeding. Given the evidence of a bidirectional association between maternal mental health and breastfeeding, it is essential to consider both aspects when evaluating the effectiveness of interventions aimed at improving these outcomes [
24,
25,
26].
The principal aim of this study was to assess the effectiveness of a midwife-led breastfeeding support group intervention on the maintenance of breastfeeding, the prevention of PPD and on general self-efficacy. Additionally, the study aimed to explore the relationship between maternal depression and breastfeeding success.
2. Materials and Methods
2.1. Study Design
This was a multicentric cluster randomized controlled trial with a control group (CG) and an intervention group (IG) and was not blinded. This study was conducted according to the latest Consolidated Standards of Reporting Trials 2010 guidelines for reporting randomized controlled trials [
27] and was completed as described in our published protocol [
28]. Prior to the start of the trial, it was registered in the International Standard Registered Clinical/Social Study Number registry (Trial ID: ISRCTN17263529; date recorded: 17 June 2020).
2.2. Participants and Study Area
Women who met the eligibility criteria were enrolled as participants from primary health centres in Andalusia, Spain. Andalusia is an autonomous community divided into eight provinces with a total of 8,472,407 inhabitants (data available in 2021) [
29], a birth rate of 7.72 per 1,000 inhabitants (2021) [
30] and 4,328,407 women of reproductive age [
31]. The study involved populations from the provinces of Seville, Cadiz, Huelva, Granada and Jaen.
2.3. Inclusion and Exclusion Criteria
Inclusion criteria included the following:
Healthy women performing exclusive or partial breastfeeding 10 days after birth and who attended antenatal lessons at the primary health centre;
Women over 18 years of age;
Women who accepted and signed the informed consent form.
Exclusion criteria included the following:
Human immunodeficiency virus positive;
Cancer;
Tuberculosis infection;
No intention to breastfeed;
Impossibility or contraindication to breastfeed due to medical conditions;
Premature and/or complicated labour or newborn in a neonatal intensive care unit during the first month of life;
Communication difficulties due to language barriers.
2.4. Sample Size
According to 2021 data from the National Statistical Institute of Spain, there were a total of 65,650 births in Andalusia. Specifically, the provinces of Seville (15,655 births), Granada (7,083), Huelva (4,227), Jaen (4,499) and Cadiz (8,904) accounted for 40,368 births, constituting 61.79% of the total births in the region [
32]. The rate of exclusive breastfeeding (EBF) at 6 months in Andalusia is 39% [
33], which was considered the baseline value in the CG. An anticipated increase of 10%, as suggested by previous research [
34,
35], in the rate of EBF at 6 months was established. To achieve this difference between the two groups, a two-tailed hypothesis was posed, with a power of 80% and allowing for a type I error of 5%. The necessary sample size amounted to 371 women distributed between the two study groups.
2.5. Randomization and Recruitment
Primary health centres were randomly assigned to either the IG or the CG (receiving usual care), considering whether any form of group breastfeeding support intervention was already available. The allocation of health centres into these groups was performed by a research technician, who was independent of the researchers responsible for participant recruitment, using a random sequence [
36]. The technician provided random unique identifiers to the health centres, distinguishing between those belonging to the CG and IG.
Subsequently, the women were again randomized following a simple strategy (1:1) at 35–37 weeks of gestation by the collaborating primary health centre midwives. Finally, each participant received an identification code based on the group to which she was assigned.
2.6. Intervention
Participants in the CG received standard care in terms of maternal education and postpartum visits, following the guidelines outlined in the Protocol for Care during Pregnancy, Childbirth and Puerperium by the Andalusian Health and Social Welfare Council [
37], similarly to the women in the IG. Within the initial 10 days after giving birth, they underwent a one-on-one visit with the midwife to address individual concerns. Additionally, women had the opportunity to request individual postpartum consultations with the designated midwife at their health centre as needed.
Women in the IG received the usual prenatal and postpartum care, just like those in the CG. Subsequently, they engaged in monthly 2-hour in-person and/or virtual group sessions known as breastfeeding support groups, during which the midwife assumed the roles of leader and moderator. These sessions encompassed an educational element, featuring theoretical and practical presentations related to breastfeeding and aligned with the recommendations of the Baby-Friendly Hospital Initiative [
38]. They also included motivational and social or peer support components established within the group. Consequently, on a monthly basis, women received support from an organized and proactive professional. In addition to these monthly gatherings, participants had the opportunity to interact with each other, connect with other breastfeeding women and communicate with the designated midwife through a Facebook™ and/or WhatsApp™ group specifically created for this purpose. This strengthened peer support, and queries regarding the topic were addressed using information and communication technologies [
39]. Similarly, participating women retained the option to request individual consultations with the designated midwife on demand, similarly to those receiving standard care.
2.7. Assessment
Sociodemographic and obstetric clinical data were collected by a questionnaire designed for this purpose via a web application. Incorrect or incomplete data were corrected via direct consultation with participants or were collected from their medical records with their consent. The data collected including the following:
Sociodemographic variables: maternal age, country of origin, civil status (single, married, separated, widow), educational level (none, primary school, secondary school, university), employment status (self-employed, employed, unemployed);
Obstetric variables: parity (primiparous, multiparous), gestational age, labour onset (induction, spontaneous), type of birth (eutocic, instrumental, elective caesarean section, emergent caesarean section), newborn sex, birth weight.
The type of breastfeeding was recorded at hospital discharge, as well as at three established follow-up time points: 10 days postpartum (T1), 2 months postpartum (T2) and 4 months postpartum (T3). Distinctions were made between EBF, breastfeeding with occasional supplementation of formula, mixed feeding and formula feeding.
PPD was measured using the Edinburgh Postnatal Depression Scale (EPDS) designed by Cox et al. [
40] in 1987 and validated for the Spanish population by García-Esteve et al. [
41] in 2003. This is a 10-item self-reported scale in which women indicate how they felt in the last 7 days. The scale is structured into three factors: anhedonia (items 1, 2 and 10), anxiety (items 3–6) and depressive symptomatology (items 7–9) [
42]. The minimum possible score is 0, and the maximum is 30. The best cut-off of the Spanish validation of the EPDS was 10/11 for combined major and minor depression, the sensitivity was 79% and the specificity was 95.5%, with a positive predictive value of 63.2% and a negative predictive value of 97.7%. At this cut-off, all cases of major depression were detected. The area under the receiver operating characteristic curve was 0.976 (
p = 0.001) with an asymptotic 95% confidence interval between 0.968 and 0.984 [
41].
General self-efficacy was measured using the General Self-efficacy Scale (GSE) designed by Baessler and Schwarcer [
43] in 1996. It was validated for the Spanish population by Sanjuán et al. [
44]. This scale assesses the enduring sense of personal competence to effectively handle a wide variety of stressful situations. It is a unidimensional scale with 10 Likert-type questions [
43]. A change in the original response form (10-point Likert-type scale instead of a 4-point scale) was introduced in order to adapt the scale to other research instruments. The reliability of the Spanish version of the GSE, as measured by the Cronbach alpha coefficient, was 0.87 [
44].
The main control and outcome variables were measured before the start of the intervention (baseline) and at 2- and 4-month follow-ups.
2.8. Data Collection
The enrolment of participants commenced in October 2021 and concluded in May 2023. This process was performed by the midwives overseeing each health centre. These midwives underwent prior training for the project and received guidance from a research technician midwife associated with the project but not directly involved in the intervention. The designated midwife at the health centre, during consultations with eligible women, provided information about the study’s nature and objectives, as well as details regarding the follow-up procedures. Once participants provided information via the project’s web application, they agreed to participate and signed the informed consent form in duplicate. The web application automatically sent them reminder messages and emails at the three evaluation time points established in the study.
The data relating to electronic follow-up were coded and safeguarded by the research team. All data were stored in an electronic database accessible only to members of the research team.
2.9. Data Analysis
Descriptive data analyses were conducted to characterize the variables. Baseline characteristics were compared between the group experiencing potential losses during follow-up and the group completing follow-up using cross-tabulation analysis. Means were compared using Fisher’s exact or t-tests, as appropriate. Associations between baseline and childbirth variables and EBF maintenance at 10 days, 2 months and 4 months postpartum were examined using cross-tabulation analysis.
Per-protocol analysis was performed. Chi-square or Fisher’s exact tests and ANOVA or t-tests, as appropriate, were employed for mean comparisons. To assess the effect of the intervention on EBF maintenance at various postpartum time points, cross-tabulation analysis and chi-square tests were utilized. Additionally, a multivariate logistic model was employed to calculate adjusted odds ratios and their 95% confidence intervals for each time point.
The assumption that variables were normally distributed was checked using the Kolmogorov–Smirnov test. Group homogeneity analyses based on baseline and childbirth variables were conducted using cross-tabulation analysis, utilizing chi-square or Fisher’s exact tests as needed. ANOVA and t-tests were employed for mean comparisons.
Data analysis was conducted using SPSS v. 28.1 for Windows (IBM Corp. 2018, Armonk, NY, USA) and R (R Project 2019, version 4.0.2). The threshold for statistical significance was set at p < 0.05.
2.10. Ethical Considerations
Before beginning the study, it was approved by the Research Ethics Committees of the Virgen Macarena and Virgen del Rocío hospitals (Seville, Spain) on 13 March 2021 (Code 2722-N-20).
Participation in the project was voluntary, as was the participation request. Verbal and written informed consent information was provided to every participant in the study. The study was designed according to Spanish Law No. 14/2007 of 3 July regarding biomedical research and complied with the study suitability requirements and with the procedure regarding the study objectives. The data were anonymously handled according to the Spanish Organic Law on Protection of Personal Data and Guarantee of Digital Rights (Spanish Organic Law 3/2018).
3. Results
3.1. Characteristics of the Sample
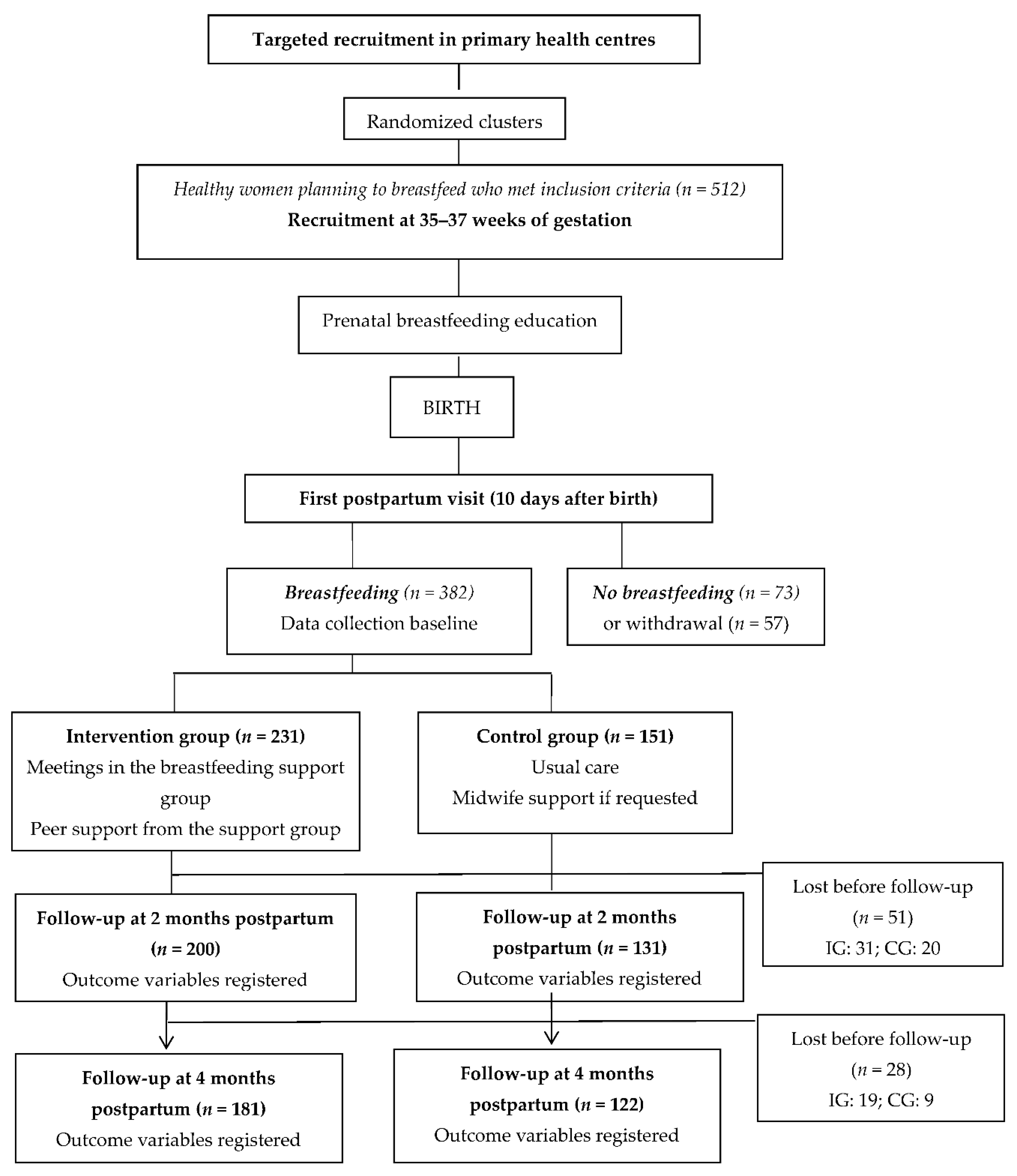
A total of 512 participants were initially selected, with 130 (25.4%) excluded from randomization for the following reasons: 73 (56.2%) were not breastfeeding their newborns, and 57 (43.8%) declined follow-up in the first 10 days postpartum.
The analysis focused on a total sample of 382 mother–child dyads, randomly distributed, with 151 (39.5%) in the CG and 231 (60.5%) in the IG. There were 51 (13.35%) dropouts between T1 and T2 (
n = 331), 27 (7.06%) of them due to discontinuation of breastfeeding. In additional, 28 participants (7.32%) dropped out between T2 and T3 (
n = 303), motivated by discontinuation of breastfeeding, resulting in a total of 79 participants who did not continue responding to surveys (
Figure 1).
We compared baseline characteristics between the dropout group (n = 79 [CG: 29; IG: 50]) and the final analysed group (n = 303). Fisher’s exact and t-tests were used, as appropriate for variable types, to compare the groups. We observed that only those women in the IG dropout group had a lower rate of university education compared to the follow-up group (52.0% vs 66.9%); this difference was statistically significant (p = 0.038). Thus, despite these losses, group homogeneity was maintained, indicating their random origin.
3.2. Sociodemographic and Obstetric–Neonatal Variables
The participants had a mean age of 33.4 ± 4.7 years, with 93.5% (357/382) born in Spain. The majority had university education (64.4%), were married (55.0%) and had gainful employment (61.5%). The mean gestational age at birth was 39.5 ± 1.2 weeks, and 53.9% (206/382) of participants were primiparous, with 60.7% (232/382) experiencing spontaneous onset of labour culminating in vaginal delivery (61.8%). The average birth weight was 3,271 ± 434.3 g.
The relative rate of breastfeeding experience was 38.4% (58/151) in the CG and 44.6% (103/231) in the IG. We did not find statistically significant differences between the sociodemographic or obstetric–neonatal characteristics of the two groups, except for early skin-to-skin contact (
p = 0.028), gestational age (
p = 0.028) and feeding type at 4 months (
p < 0.001;
Table 1).
During the follow-up period, we observed a gradual reduction in the breastfeeding rate from 78.0% (298/382) at 10 days to 69.5% (230/331) at 2 months and 61.7% (187/305) at 4 months postpartum. Statistically significant differences were found between the rates of breastfeeding in the CG (50.0%) and the IG (69.6%) at 4 months postpartum (
p < 0.001;
Table 2).
Statistically significant differences between the groups were observed in PPD at 4 months postpartum, with a lower mean score on the EPDS in the IG than the CG (12.49 ± 3.6 vs 13.39 ± 4.0;
p = 0.044;
Table 3).
We examined the relationships between the maintenance of EBF and both EPDS and GSE scores during the study period. We observed statistically significant differences in the GSE scores of women who did and did not perform EBF only at T2 and T3, with women performing EBF obtaining higher scores (78.1 ± 14.3 vs 74.3 ± 15.2 at T2 [
p = 0.014]; 78.3 ± 14.4 vs 72.4 ± 15.9 at T3 [
p < 0.001];
Table 4). Statistically significant differences were observed in the EPDS scores of women who did and did not perform EBF only at T2 and T3, with lower mean scores in women performing EBF (12.2 ± 3.5 vs 13.5 ± 3.9 at T2 [
p = 0.002]; 12.1 ± 3.6 vs 14.1 ± 3.8 at T3 [
p < 0.001];
Table 4).
Table 5 presents the factors associated with the maintenance of EBF across the three distinct postpartum periods. Logistic regression analysis results revealed significant associations between various variables and the likelihood of sustaining EBF during each period. At T1, the absence of early skin-to-skin contact was significantly associated with a decrease in the likelihood of maintaining EBF (OR = 0.432,
p = 0.014). At T2, EPDS scores were significantly associated with the likelihood of maintaining EBF. Specifically, an increase in EPDS T2 scores was linked to a significant decrease in the likelihood of sustaining EBF (OR = 0.915,
p = 0.012). This finding suggests that higher levels of depressive symptoms during the second postpartum period were associated with a reduction in the likelihood of maintaining EBF. Similarly, at T3, EPDS scores were significantly associated with the probability of maintaining EBF, with an increase in score linked to a significant decrease in the likelihood of sustaining EBF (OR = 0.887,
p = 0.002). Finally, the absence of intervention was related to a significant decrease in the probability of maintaining EBF at T3 (OR = 0.474,
p = 0.003).
4. Discussion
The purpose of this study was to assess the effect of midwife-led breastfeeding support groups on the maintenance of breastfeeding, the prevalence of PPD and the perceived general self-efficacy of the participants.
In our study, one of the most important factors related to the initiation of breastfeeding was early skin-to-skin contact after delivery. This result aligns with findings from a Cochrane review indicating that this intimate contact between the newborn and the mother provides a unique environment that meets basic biological needs, according to mammalian neuroscience, and programs future behaviours that aid in the maintenance of EBF [
45]. Breastfeeding is considered a protective factor against PPD because it causes the release of oxytocin, which contributes to the well-being of the woman [
46].
Another factor in our study related to the initiation of breastfeeding was greater gestational age at birth, indicating that these newborns had greater biological maturity that allowed for a more satisfactory initiation of breastfeeding and better adaptation to extrauterine life. Conversely, early-term infants (born between weeks 37 + 0 and 38 + 6) are more likely to experience adverse neonatal outcomes that necessitate medical interventions, thereby complicating the initiation of breastfeeding [
47,
48]. This could not be analysed in our study, as participants with preterm pregnancies were not included.
The maintenance of breastfeeding during the first 6 months plays a crucial role in the health and well-being of the mother–infant dyad. According to our data on postpartum depressive symptoms, as measured by the EPDS, higher levels of depressive symptoms were associated with a reduction in the maintenance of EBF at 2 months (T2) and 4 months (T3). However, we must clarify that the direction of the association is unknown, as we do not know whether women who report fewer signs and symptoms of PPD have better breastfeeding experiences or whether those who continue breastfeeding for a longer period adapt more effectively postpartum and therefore have lower PPD scores. This challenge has already been identified by other authors who reported that women who breastfed for a longer duration had a statistically significantly lower EPDS risk score for PPD [
49]. A study by Bascom et al. [
50] suggested that, when depressive symptoms appear in postpartum women prematurely, difficulties with breastfeeding often lead to its early cessation.
Another key factor for the maintenance of breastfeeding is education and support through breastfeeding support groups. Our findings align with those of other studies, which have shown that interventions for promoting breastfeeding based on a combination of social support from peers and leadership by IBCLCs yield better results in maintaining breastfeeding during the first 6 months postpartum [
28]. In our study, we did not observe differences at 2 months postpartum, when the first breastfeeding challenge occurs [
51], but we did observe differences at 4 months postpartum, when women return to work, as indicated by other studies in which interventions were effective at 4 and 6 months postpartum [
52].
General self-efficacy in breastfeeding, which is based on confidence, helps to improve breastfeeding rates [
53]. In our study, it was linked to breastfeeding and PPD. Women who demonstrated higher general self-efficacy showed higher levels of breastfeeding [
54] and lower levels of PPD. Additionally, those who participated in breastfeeding support groups had better outcomes for the aforementioned parameters. This aligns with the findings of Tsen et al. [
55] in their randomized controlled trial, which indicate that previous breastfeeding experiences (performance accomplishments), along with observing successful breastfeeding in peers (vicarious experience) and verbal encouragement from a leader promoting breastfeeding (verbal persuasion), lead to breastfeeding success. The stress and anxiety reduction provided by these support groups increases self-efficacy and, consequently, breastfeeding [
55]. Additionally, our study showed that women who were part of midwife-led breastfeeding support groups maintained breastfeeding for a longer duration and experienced less PPD. Hence, multiple findings suggest that support groups have numerous benefits as a health promotion strategy and coping mechanism for illnesses through informative support, shared experiences and opportunities to learn from others [
56,
57].
We must acknowledge some limitations of our study. For example, only healthy women and newborns were included, thereby limiting the variability of observed physiological parameters and potentially simplifying their interpretation. Data related to breastfeeding type were self-reported, which could introduce a memory bias, even though data collection was conducted chronologically over time. Additionally, pregnant women might have misclassified types of breastfeeding (EBF, breastfeeding with other foods, etc.), which could also be related to memory bias. However, maternal recall for reporting these data has been shown to be a valid and reliable estimate of breastfeeding [
58]. Furthermore, we lacked a baseline assessment prior to pregnancy of women’s rates of depression. We cannot determine if women who experienced PPD had previously suffered from depression or showed signs of being at risk. Finally, another limitation was the withdrawal of patients from both the CG and the IG throughout the period of data collection.
We would like to highlight several strengths of our study, such as the prospective, consecutive and randomized inclusion of patients in five provinces of Andalusia, a southern region of Spain, allowing the findings to be applicable in routine clinical practice. The training provided by the research team to the midwives recruiting pregnant women ensured that the CG and IG samples were as homogeneous as possible. Another significant strength of this study was the use of multivariate logistic regression to determine the factors favouring breastfeeding at different data collection time points (from T1 to T3), a statistical approach not implemented in previous studies.
5. Conclusions
Women participating in midwife-led breastfeeding support groups exhibited higher levels of general self-efficacy, maintained breastfeeding for a longer duration and showed less PPD at 4 months after childbirth compared to women in the CG. These findings suggest the need for healthcare providers (midwives) to develop intervention strategies that address factors supporting the initiation and maintenance of breastfeeding, by enhancing self-efficacy to reduce the occurrence of PPD, as these have been identified as promising interventions, although further research is needed.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Figure S1: title; Table S1: title; Video S1: title.
Author Contributions
Conceptualization and methodology: F. L.-L & I. R.-G.; analysis of data: V-C. R; writing—original draft preparation, writing—review and editing: F. L.-L, I. R.-G., R.V-C; I. C.-G., & D. G.-B. All authors have read and agreed to the published version of the manuscript.
Funding
This is a project document that has received a public grant for its development in the call for Research, Development, and Innovation on Biomedicine and Health Sciences in Andalusia of the Health and Family Council (Consejería de Salud y Familias), Spain (Code PI-0008-2019). The funders had no role in the design of this study nor in its execution, analyses, data interpretation, or presentation of results.
Institutional Review Board Statement
“The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Committees of the Virgen Macarena and Virgen del Rocío hospitals (Seville, Spain) on 13 March 2021 (Code 2722-N-20), for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to confidentiality issues.
Acknowledgments
We would like to thank all the mothers who agreed to take part in the study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Trial registration
International Standard Registered Clinical/Social Study Number registry (Trial ID: ISRCTN17263529; date recorded: 17 June 2020).
References
- Zhao, X. H.; Zhang, Z. H. Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J. Psychiatr. 2020, 53, 102353. [Google Scholar] [CrossRef]
- Banti ,S.; Mauri,M.; Oppo,A.; Borri,C.; Rambelli, C.; Ramacciotti, D.; Montagnani, M.S.; Camilleri, V.; Cortopassi, S.; Rucci, P.; Cassano, G.B. From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the perinatal depression-research & screening unit study. Compr Psychiatry 2011, 52, 343-351. [CrossRef]
- Wang, J.; Wu, X.; Lai, W.; Long, E.; Zhang, X.; Li, W.; Zhu, Y.; Chen, C.; Zhong, X.; Liu, Z.; Wang, D.; Lin, H. Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open. 2017, 7, e017173. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. 2. Arlington: American Psychiatric Association 2014; pp 123-125.
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; Liu, Z.; Li, Z.; Yang, B.X. Mapping global prevalence of depression among postpartum women. Transl Psychiatry, 2021, 11,543. Erratum in: Transl Psychiatry. 2021 Dec 20;11(1):640. [CrossRef]
- Payn, J.L.; Maguire, J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol. 2019, 52, 165–180. [Google Scholar] [CrossRef]
- de la Fe Rodríguez-Muñoz, M.; Le, H.N.; de la Cruz, I.V.; Crespo, M.E.O.; Méndez, N.I. Feasibility of screening and prevalence of prenatal depression in an obstetric setting in Spain. Eur J Obstet Gynecol Reprod Biol. 2017, 215:101-105. [CrossRef]
- O'Hara, M.W.; Wisner, K.L. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014, 28, 3–12. [Google Scholar] [CrossRef]
- Bruist, A. Perinatal mental health: a guide to the Edinburgh Postnatal Depression Scale. Archives of Women’s Mental Health 2004, 7, 96.
- Mayberry, L.J.; Horowitz, J.A.; Declercq, E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J Obstet Gynecol Neonatal Nurs. 2007, 36, 542–549. [Google Scholar] [CrossRef]
- Department of Health and Human Service Office on Women's Health. Benefits of breastfeeding. Nutr Clin Care. 2003. 3:125-31. [Google Scholar]
- Binns, C.; Lee, M.; Low, W.Y. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac J Public Health. 2016, 1, 7–14. [Google Scholar] [CrossRef]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015, 467, 96–113. [Google Scholar] [CrossRef]
- Figueiredo,B.; Dias, C.C.; Brandão, S.; Canário, C.; Nunes-Costa, R. Breastfeeding and postpartum depression: state of the art review. J Pediatr (Rio J). 2013, 4,332-338. [CrossRef]
- Xia, M.; Luo, J.; Wang, J.; Liang, Y. Association between breastfeeding and postpartum depression: A meta-analysis. J Affect Disord. 2022, 308, 512–519. [Google Scholar] [CrossRef]
- Dennis, C.L.; Boyce, P. Further psychometric testing of a brief personality scale to measure vulnerability to postpartum depression. J Psychosom Obstet Gynaecol. 2004, 25, 305–311. [Google Scholar] [CrossRef]
- Gillis, B.D.; Parish, A.L. Group-based interventions for postpartum depression: An integrative review and conceptual model. Arch Psychiatr Nurs. 2019, 33, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Gallego, I.; Leon-Larios, F.; Corrales-Gutierrez, I.; González-Sanz, J.D. Impact and Effectiveness of Group Strategies for Supporting Breastfeeding after Birth: A Systematic Review. Int J Environ Res Public Health. 2021, 18, 2550. [Google Scholar] [CrossRef] [PubMed]
- Nishioka, E.; Haruna, M.; Ota, E.; Matsuzaki, M.; Murayama, R.; Yoshimura, K.; Murashima, S. A prospective study of the relationship between breastfeeding and postpartum depressive symptoms appearing at 1-5 months after delivery. J Affect Disord. 2011, 133, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.J.; Mazmanian, D. Breastfeeding and Postpartum Depression: An Overview and Methodological Recommendations for Future Research. Depress Res Treat, 2016, 2016, 4765310. [Google Scholar] [CrossRef] [PubMed]
- McCoach, D.B., Gable, R.K., Madura, J.P. Instrument Development in the Affective Domain. School and corporate applications. 3rd edition.; Springer,New York, 2013.
- Bandura, A.Self-efficacy: toward a unifying theory of behavioral change. Psychological review, 1977, 2, 191–215. https://doi.org/10.1037//0033-295x.84.2.191. [CrossRef]
- Han. L.; Zhang, J.; Yang, J.; Yang, X.; Bai, H. Between Personality Traits and Postpartum Depression: The Mediated Role of Maternal Self-Efficacy. Neuropsychiatr Dis Treat. 2022, 18, 597-609. [CrossRef]
- Figueiredo B, Dias CC, Brandão S, Canário C, Nunes-Costa R. Breastfeeding and postpartum depression: state of the art review. J Pediatr (Rio J). 2013, 89, 332-338. [CrossRef]
- Henshaw, E.J. Breastfeeding and Postpartum Depression: A Review of Relationships and Potential Mechanisms. Curr Psychiatry Rep. 2023, 31. [Google Scholar] [CrossRef] [PubMed]
- Pezley, L.; Cares, K.; Duffecy, J.; Koenig, M.D.; Maki, P.; Odoms-Young, A.; Clark Withington, M,H.; Lima Oliveira, M.; Loiacono, B.; Prough, J.; Tussing-Humphreys, L.; Buscemi, J. Efficacy of behavioral interventions to improve maternal mental health and breastfeeding outcomes: a systematic review. Int Breastfeed J. 2022, 17, 67. [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C; Devereaux, P.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010, 340, c869. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Gallego, I.; Leon-Larios, F.; Ruiz-Ferrón, C.; Lomas-Campos, M.D. Evaluation of the impact of breastfeeding support groups in primary health CENTRES in Andalusia, Spain: a study protocol for a cluster randomized controlled trial (GALMA project). BMC Public Health. 2020, 20, 1129, Erratum in: BMC Public Health. 2020 Sep 23;20(1):1445. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. Oficina Estadística Española. Registro INE 2021.Available online: https://www.ine.es/jaxiT3/Datos.htm?t=2915 (accessed on 20 july 2023).
- Instituto Nacional de Estadística. Oficina Estadística Española. Registro INE 2021. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=1433#!tabs-tabla (acessed on 20 july 2023).
- Instituto Nacional de Estadística (INE). Series detalladas desde 2002. Población residente por fecha, sexo, grupo de edad y nacionalidad (agrupación de países). Oficina Estadística Española. Registro INE 2022. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=9689 (accesed on 20 july 2023).
- Instituto Nacional de Estadística (INE). Movimiento natural de la población: nacimientos. Fenómenos demográficos por comunidades y ciudades autónomas y tipo de fenómeno demográfico. Oficina Estadística Española. Registro INE 2021. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=6567 (accesed on 20 july 2023).
- Ministerio de Sanidad. Encuesta Nacional de Salud de España 2017 (ENSE 2017).Determinantes de Salud. Tipo de lactancia. Tabla 3.078. según sexo y clase social basada en la ocupación de la persona de referencia. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_MOD3_REL.pdf (accesed on 20 july 2023).
- Nabulsi, M.; Hamadeh, H.; Tamim, H.; Kabakian, T.; Charafeddine, L.; Yehya, N.; Sinno, D.; Sidani, S. A complex breastfeeding promotion and support intervention in a developing country: study protocol for a randomized clinical trial. BMC Public Health, 2014; 14, 36, PMID: 24428951; PMCID: PMC3898488. [Google Scholar] [CrossRef]
- Rollins, N.C.; Bhandari, N.; Hajeebhoy, N.; Horton, S.; Lutter, C.K.; Martines, J.C.; Piwoz, E.G.; Richter, L,M.;Victora, C.G.; Lancet Breastfeeding Series Group. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016, 387,491-504. [CrossRef]
- Guillaumes, S.; O’Callaghan, C. Versión en español del software gratuito OxMaR para minimización y aleatorización de estudios clínicos. Gac Sanit. 2019; 33, 395–397. [CrossRef]
- Aceituno, L.; Maldonado, J.; Arribas. L.; Caño, A.; Corona, I., Martín, J.E.; Mora, M.A.; Morales, L.; Ras, J., Sánchez, T.; Sanz, R. Embarazo, parto y puerperio. Proceso Asistencial Integrado, 3rd ed.; Consejería De Igualdad, Salud y Políticas Sociales. Junta de Andalucía, España, 2014; 24-46.
- World Health Organization, UNICEF. Protecting, promoting, and supporting breastfeeding in facilities providing maternity and newborn services: the revised Baby-friendly Hospital Initiative 2018. Implementation guidance. Ginebra: WHO; 2018.
- Robinson, A.; Lauckner, C.; Davis, M.; Hall, J. ,Anderson, A.K. Facebook support for breastfeeding mothers: a comparison to offline support and associations with breastfeeding outcomes. Digit Health 2019, 5:2055207619853397. [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry, 1987; 150, 782–786. [Google Scholar] [CrossRef]
- Garcia-Esteve, L.; Ascaso, C.; Ojuel, J.; Navarro, P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003, 75, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Zotes, A.; Gallardo-Pujol, D.; Labad, J.; Martín-Santos, R.; García-Esteve, L.; Gelabert, E.; Jover, M.; Guillamat, R.; Mayoral, F.; Gornemann, I.; Canellas, F.; Gratacós, M.; Guitart, M.; Roca, M.; Costas, J.; Ivorra, J.L.; Navinés, R.; de Diego, Y.; Vilella, E.; Sanjuan, J. Factor Structure of the Spanish Version of the Edinburgh Postnatal Depression Scale. Actas Esp Psiquiatr. 2018, 46, 174–82. [Google Scholar]
- Baessler, J.; Schwarcer, R. Evaluación de la autoeficacia: Adaptación española de la escala de Autoeficacia General. Ansiedad y Estrés, 1996, 2, 1–8. [Google Scholar]
- Sanjuán, P.; Pérez, A.M.; Bermúdez, J. Escala de autoeficacia general: datos psicométricos de la adaptación para población española. Psicothema 2000, 12, 509–513. [Google Scholar]
- Moore, E.R.; Bergman, N.; Anderson, G.C.; Medley, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016, 11, CD003519.2016. [CrossRef]
- Niwayama, R.; Nishitani, S.; Takamura, T.; Shinohara, K.; Honda, S.; Miyamura, T.; Nakao, Y.; Oishi, K.; Araki-Nagahashi, M. . Oxytocin Mediates a Calming Effect on Postpartum Mood in Primiparous Mothers. Breastfeed Med. 2017, 12, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Nejsum, F.M.; Måstrup, R.; Torp-Pedersen, C.; Løkkegaard, E.C.L.; Wiingreen, R.; Hansen, B.M. Exclusive breastfeeding: Relation to gestational age, birth weight, and early neonatal ward admission. A nationwide cohort study of children born after 35 weeks of gestation. PLoS One. 2023, 18, e0285476. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.S.L.; Wong, J.Y.H.; Fong, D.Y.T.; Lok, K.Y.W.; Tarrant, M. Association between early-term birth and breastfeeding initiation, duration, and exclusivity: A systematic review. Birth. 2019, 46, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Toledo, C.; Cianelli, R.; Villegas Rodriguez, N.; De Oliveira, G.; Gattamorta, K.; Wojnar, D.; Ojukwu, E. The significance of breastfeeding practices on postpartum depression risk. Public Health Nurs. 2022, 39, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Bascom, E.M.E.; Napolitano, M.A. Breastfeeding Duration and Primary Reasons for Breastfeeding Cessation among Women with Postpartum Depressive Symptoms. J Hum Lact. 2016, 32, 282–91. [Google Scholar] [CrossRef] [PubMed]
- Franco-Antonio, C.; Santano-Mogena, E.; Sánchez-García, P.; Chimento-Díaz, S.; Cordovilla-Guardia, S. Effect of a brief motivational intervention in the immediate postpartum period on breastfeeding self-efficacy: Randomized controlled trial. Res Nurs Health, 2021 , 44, 295-307. [CrossRef]
- Franco-Antonio, C.; Calderón-García, J.F.; Santano-Mogena, E.; Rico-Martín, S.; Cordovilla-Guardia, S. Effectiveness of a brief motivational intervention to increase the breastfeeding duration in the first 6 months postpartum: Randomized controlled trial. J Adv Nurs., 2020, 76, 888–902. [Google Scholar] [CrossRef]
- Oliver-Roig, A.; d'Anglade-González, M.L.; García-García, B., Silva-Tubio, J.R.; Richart-Martínez, M.; Dennis, C.L. The Spanish version of the Breastfeeding Self-Efficacy Scale-Short Form: reliability and validity assessment. Int J Nurs Stud., 2012, 49(2):169-173. [CrossRef]
- Nilsson, I.M.S.; Kronborg, H.; Rahbek, K.; Strandberg-Larsen, K. The significance of early breastfeeding experiences on breastfeeding self-efficacy one week postpartum. Matern Child Nutr., 2020, 16, e12986. [Google Scholar] [CrossRef]
- Tseng, J.F.; Chen, S.R.; Au, H.K., Chipojola, R.; Lee, G.T.; Lee, P.H.; Shyu, M.L.; Kuo, S.Y. Effectiveness of an integrated breastfeeding education program to improve self-efficacy and exclusive breastfeeding rate: A single-blind, randomised controlled study. Int J Nurs Stud., 2020, 111, 103770. [CrossRef]
- Jablotschkin, M.; Binkowski, L.; Markovits Hoopii, R.; Weis, J. Benefits and challenges of cancer peer support groups: A systematic review of qualitative studies. Eur J Cancer Care (Engl)., 2022 , 31, e13700. [CrossRef]
- Grubesic, T.H.; Durbin, K.M. Geodemographies of Breastfeeding Support. J Hum Lact., 2021, 37, 301-313. [CrossRef]
- Li, R.; Scanlon, K.S.; Serdula, M.K. The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev., 2005, 63, 103–110. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).