1. Introduction
Anomalous coronary artery (ACA) is a congenital cardiovascular malformation, with an incidence ranging from 0,24% to 1,3% population.[
1,
2,
3] This malformation can present in a variety of ways, including anomalies in origin, course, clinical manifestation and complication. However, there is no universal classification for ACA.[
3] Single coronary artery (SCA) is a rare variation of ACA, there was only an isolated ostium coronary artery originating from the aortic trunk. SCA has been linked with life-threatening symptoms and sudden cardiac death.[
4] Myocardial infarction is a rare manifestation in patients with ACA. Myocardial infarction is a rare manifestation in patients with ACA. As usual, the electrocardiogram (ECG) was used to detection for ischaemia heart disease. Unfortunately, the ECG’s pattern could not revealed the ACA’s condition. Due to the relatively few patients of ACA, the typical ECG pattern in anomalous coronary arteries is not yet found. Another prior study of ACA’s condition with myocardial infarction revealed Brugada ECG’s pattern. The Brugada’s sign is associated with the right bundle branch block (RBBB) and ST-elevations in anterior precordial leads (V1 to V3).[13] In our cases, we are also presenting the anomalous RCA originated from the left coronary artery in the setting of ischemic heart disease, but there were no Brugada ECG’s patterns as already reported.
2. Case 1
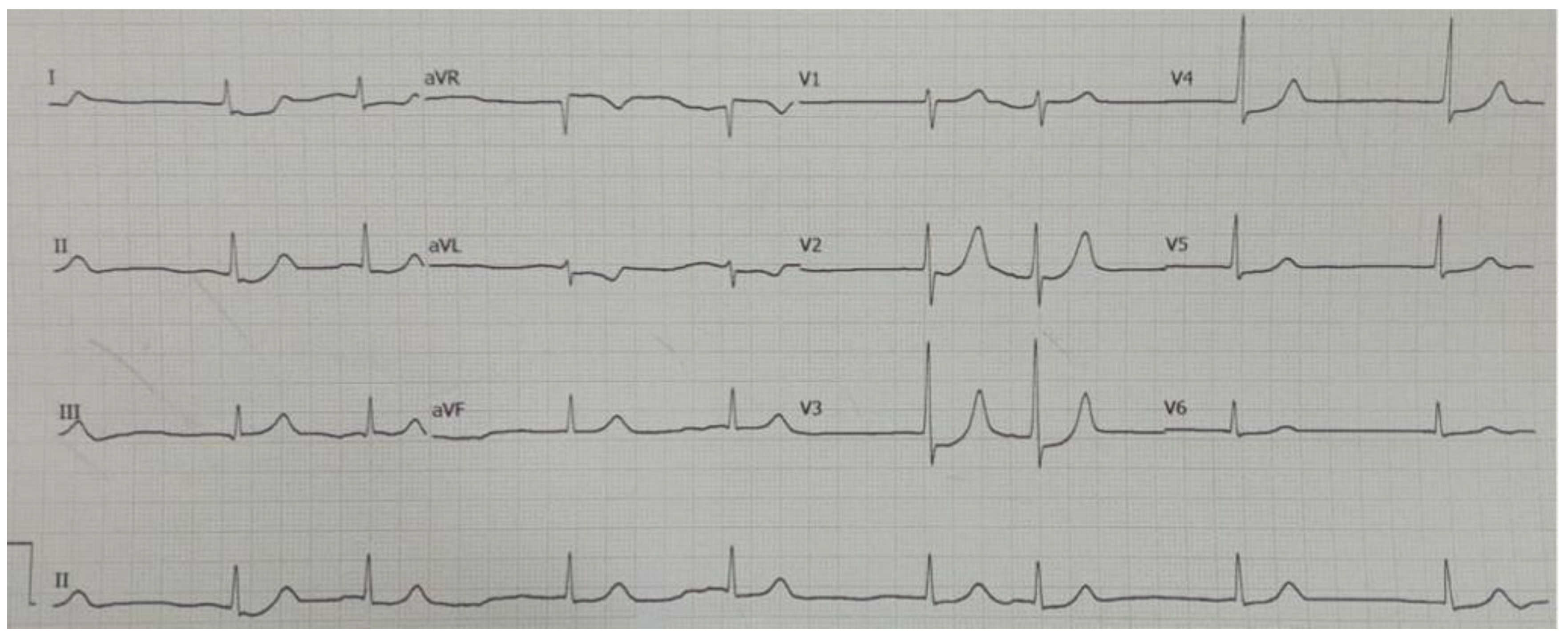
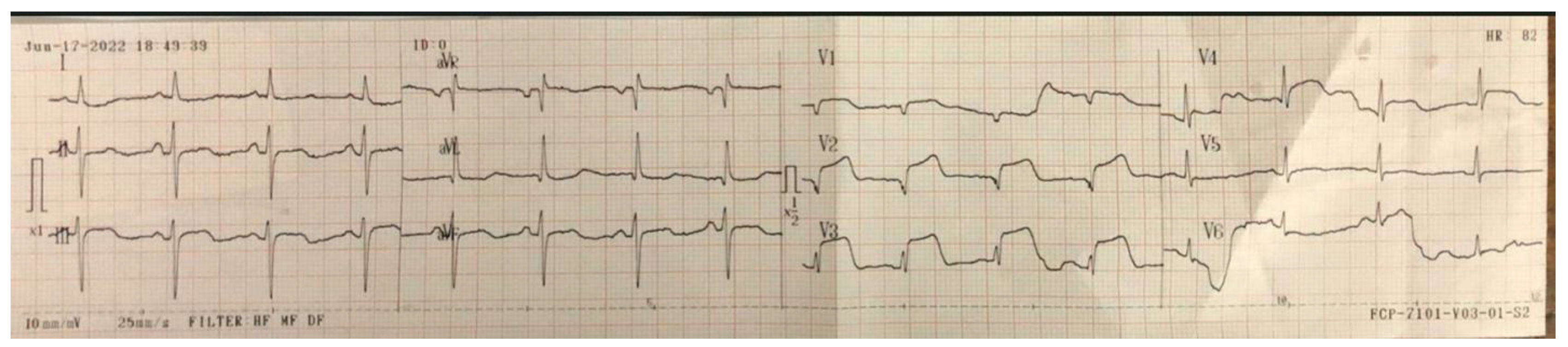
A 53-year-old male was referred from a local tertiary hospital with a chief complaint of sudden, typical chest pain with a 6-hour onset, accompanied by complaints of nausea and vomiting numerous times. The patient's medical history was lacking. Physical examination revealed he was hemodynamically unstable, with a blood pressure of 90/60 mmHg, 60 beat per minute with irregular pulse and mild tachypnea of 22 breaths per minute. Electrocardiogram (ECG) examination revealed a paroxysmal slow atrial fibrillation rhythm of 40–75 beats per minute (
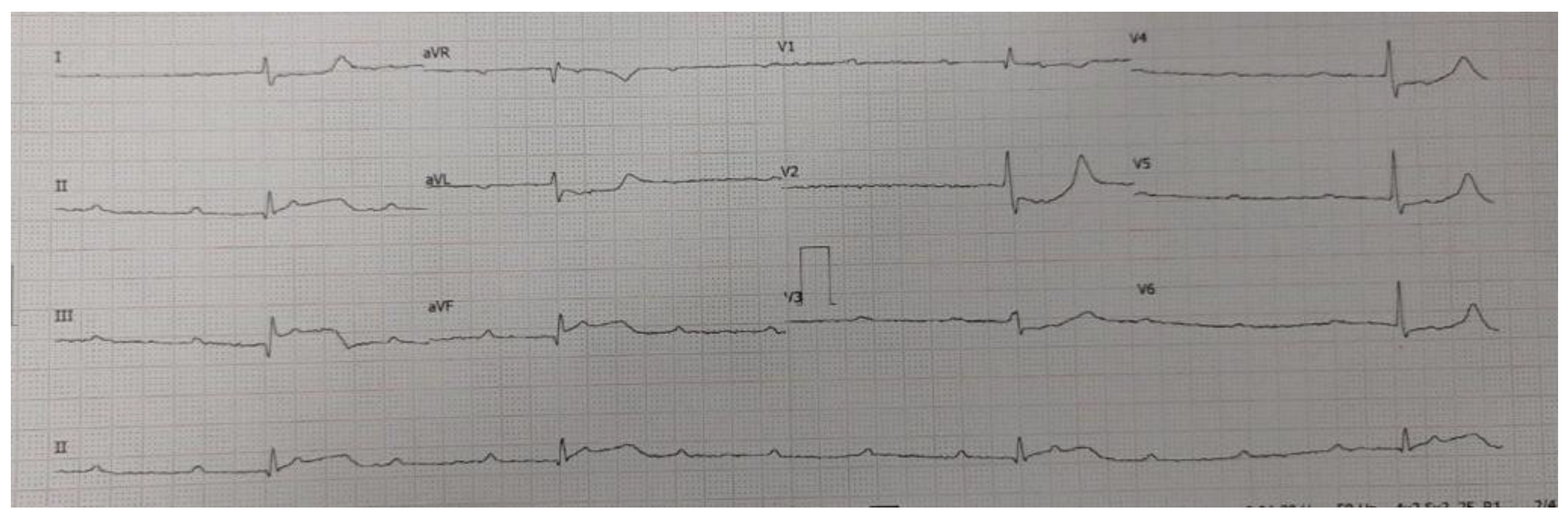
Figure 1), which changed 2 hours later to total AV-Block (TAVB) dan show ST-segment elevation (STEMI) in the inferior lead and horizontal ST depression in leads V1–V4 (
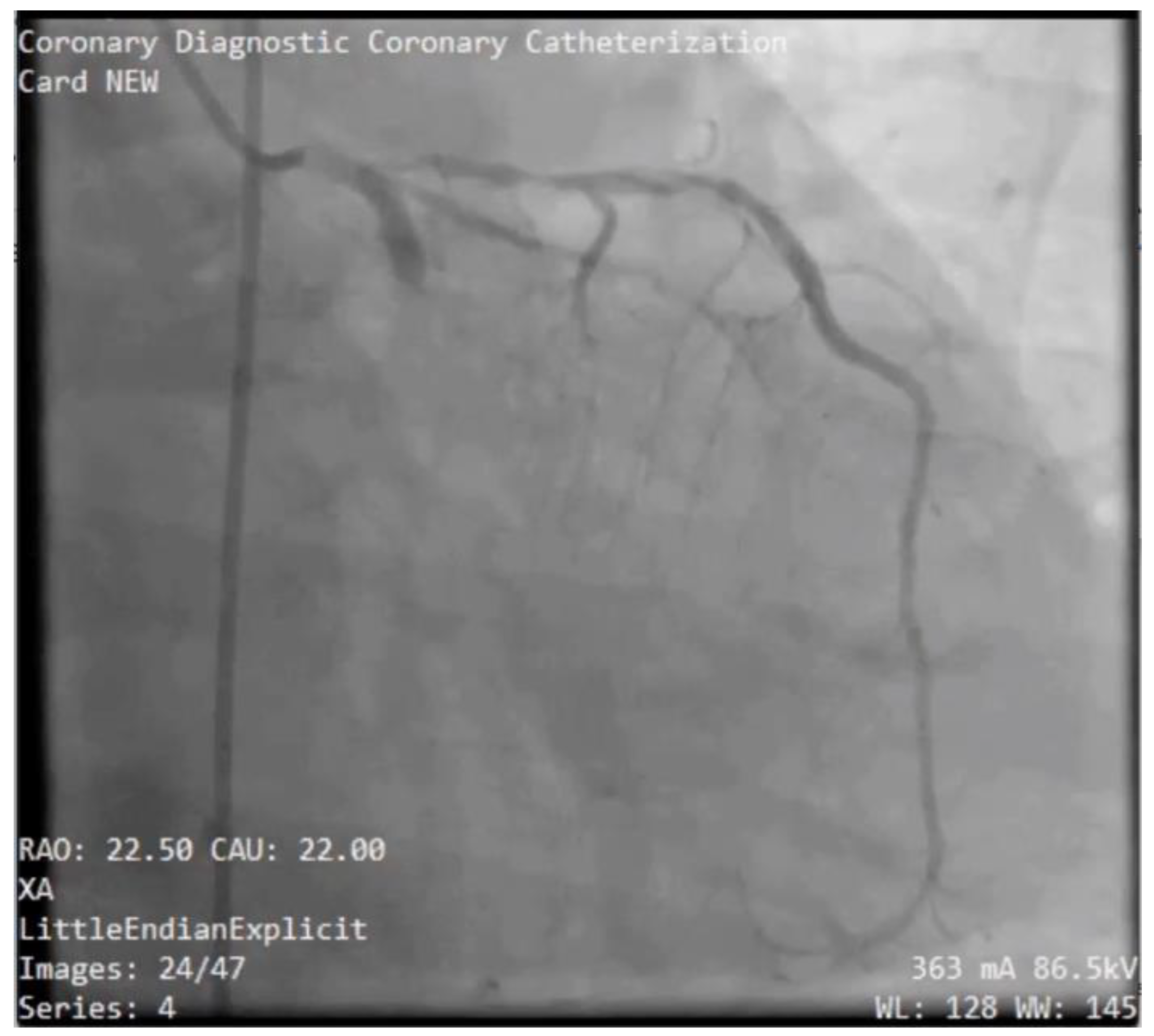
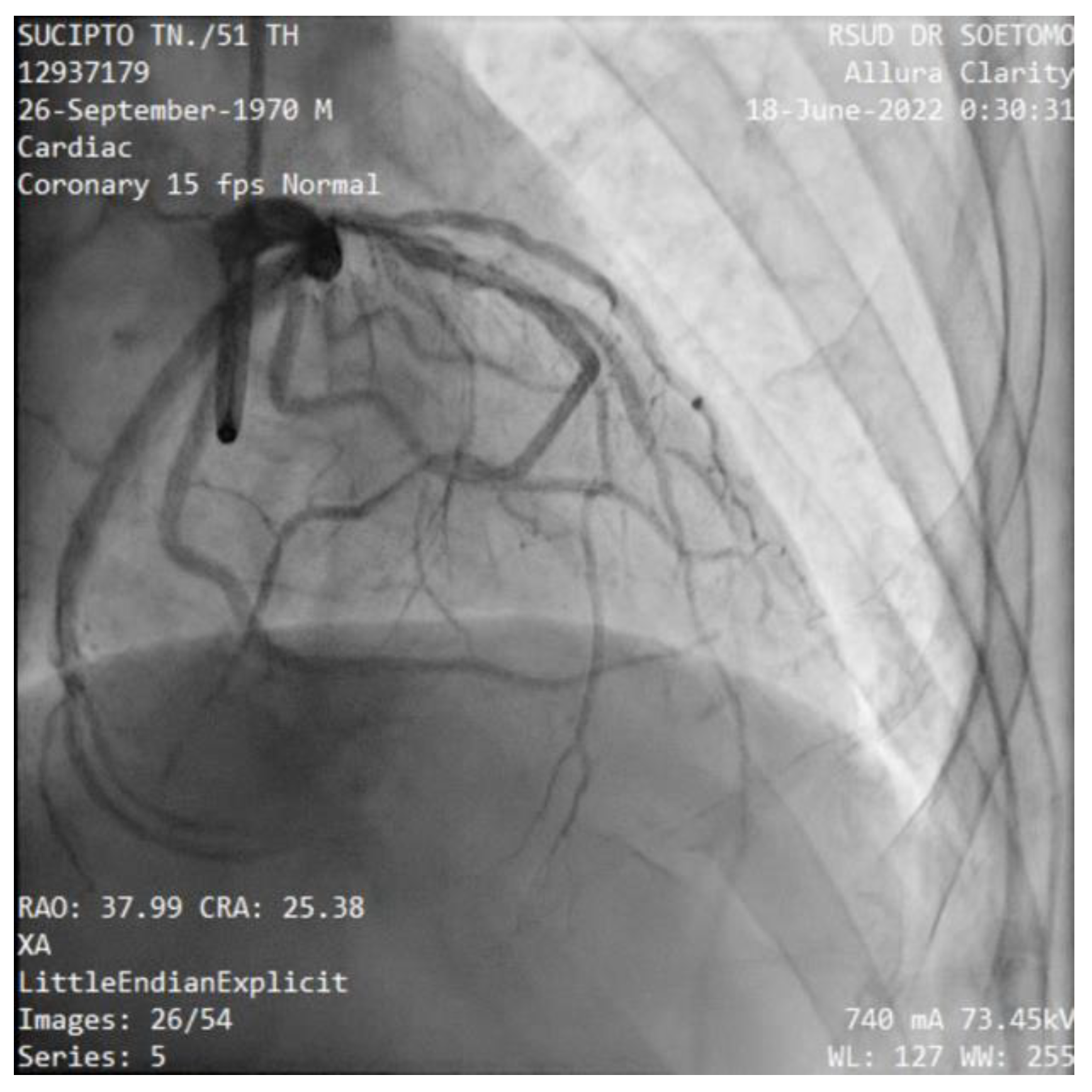
Figure 2). The patient then underwent primary PCI in the cath-lab and temporary pacemaker implantation. At the time of angiography, the attempt to engage in the right coronary artery (RCA) ostium failed, which suspected an RCA anomaly (
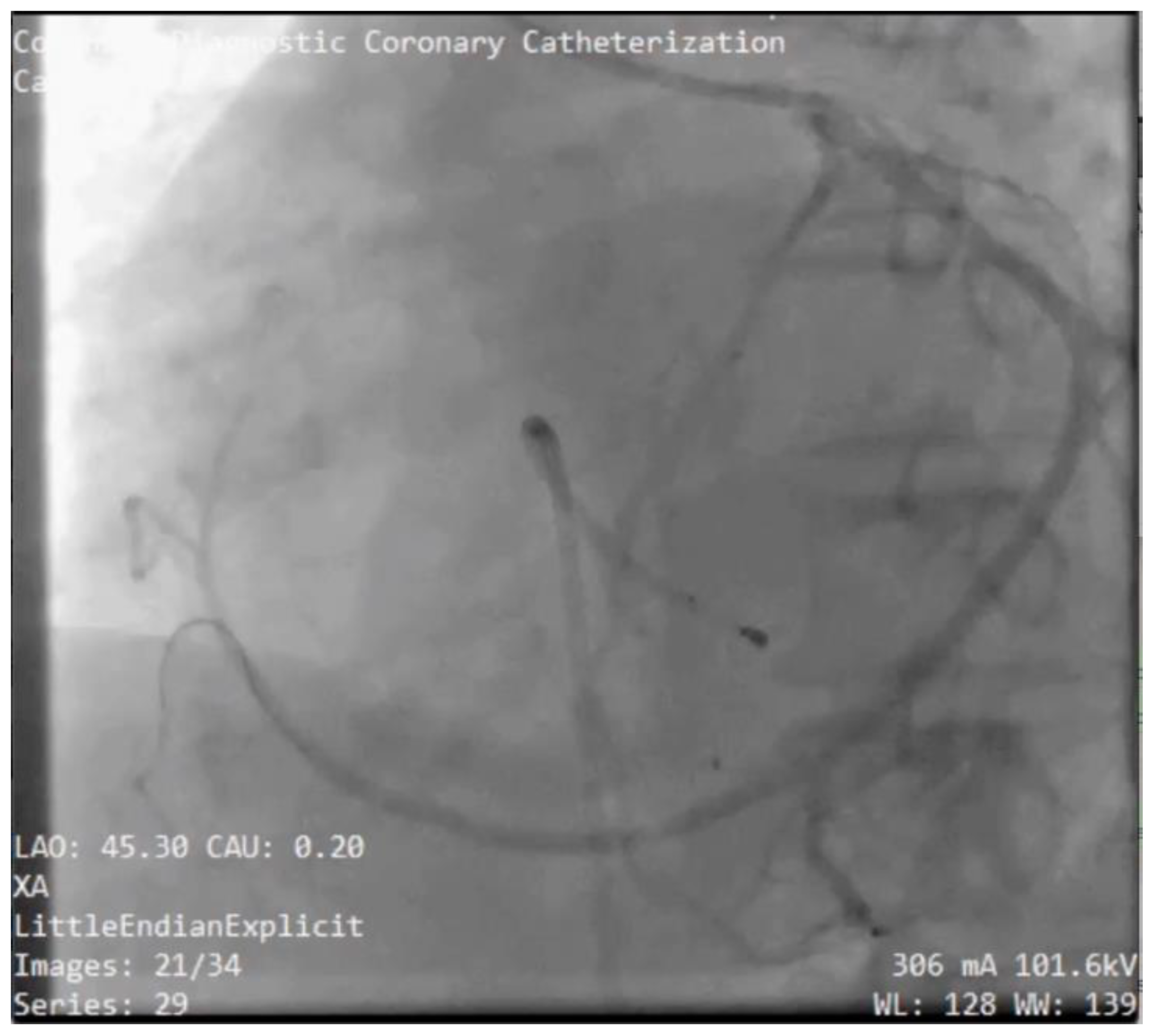
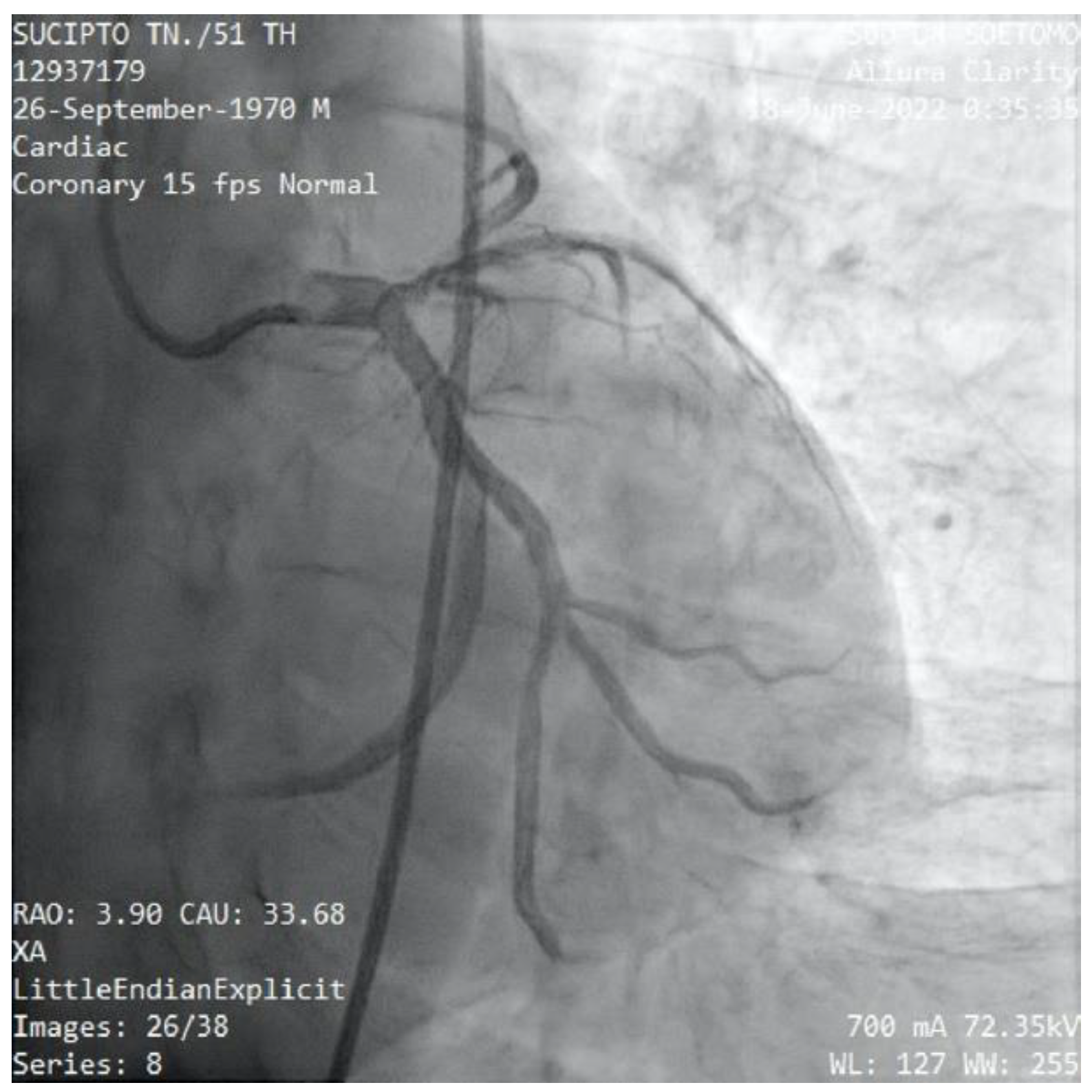
Figure 3). Then we tried guiding through the left main coronary artery (LMCA) to the left circumflex artery (LCx), found total occlusion in the mid-left circumflex, and long lesions in the ostium to the proximal left anterior descending artery (LAD). We decided to open the total occlusion that occurred in the LCx, as soon as the LCx was opened there was ostium of the RCA (
Figure 4). A total occlusion was successfully opened, and a stent was placed on the coronary culprit (mid-LCx), with the final result being good to distal flow (TIMI flow III). The patient was then sent to the critical care unit for close hemodynamic observation and received optimal medical treatment, including antiplatelet therapy (aspirin and ticagrelor), high-intensity statin (atorvastatin 40 mg/d). The patient was discharged two days later after undergoing general treatment and it has been confirmed that there are no acute complications of right heart failure.
Figure 1.
Case #1: ECG patient shows a paroxysmal slow atrial fibrillation rhythm of 40–75 beats per minute.
Figure 1.
Case #1: ECG patient shows a paroxysmal slow atrial fibrillation rhythm of 40–75 beats per minute.
Figure 2.
Case #1: The ECG changed to Total AV-Block (TAVB) and showed ST-segment elevation in the inferior lead and horizontal ST depression in leads V1–V4 after 2 hours.
Figure 2.
Case #1: The ECG changed to Total AV-Block (TAVB) and showed ST-segment elevation in the inferior lead and horizontal ST depression in leads V1–V4 after 2 hours.
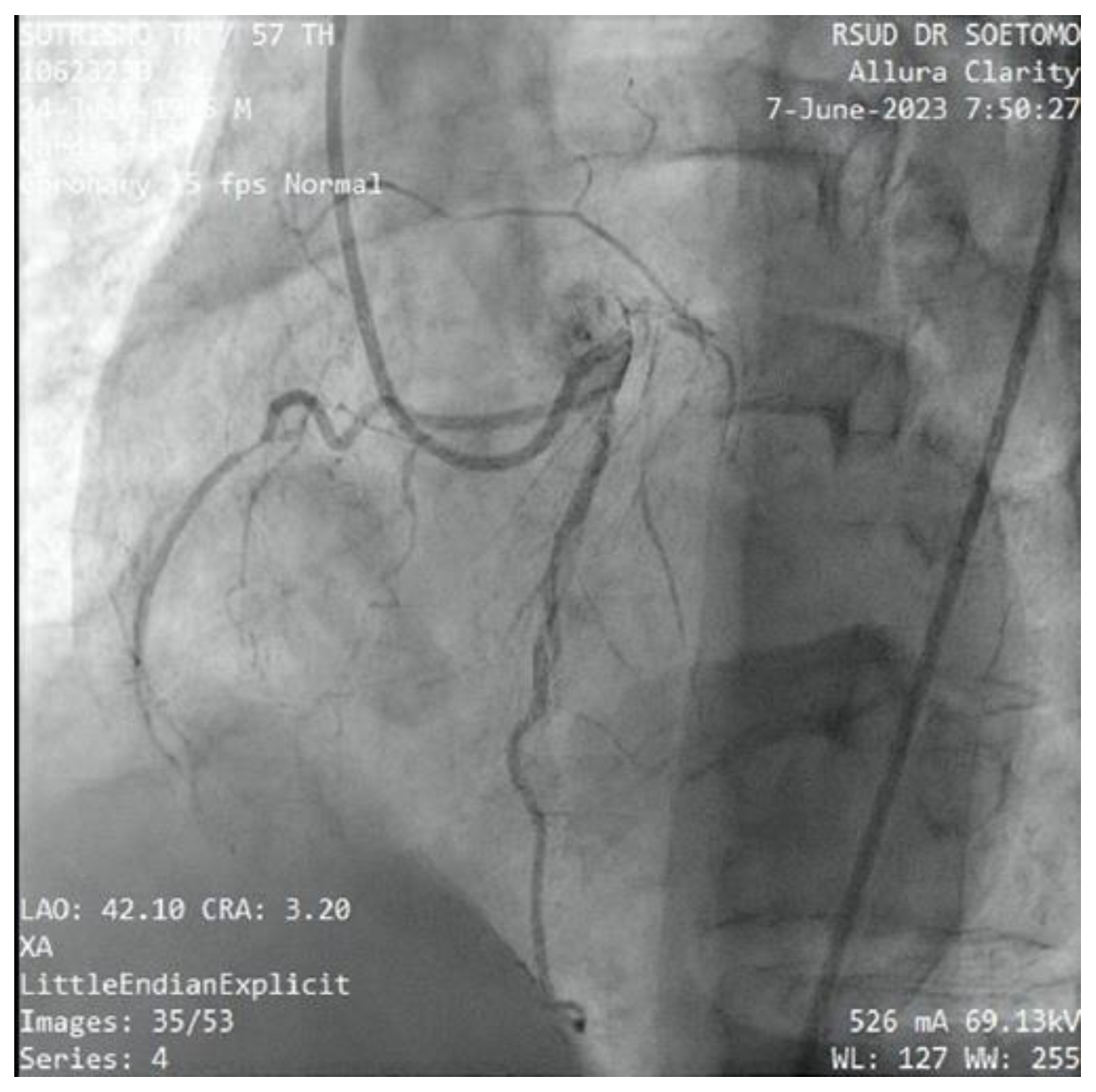
Figure 3.
Case #1: The angiography shows a suspected RCA anomaly.
Figure 3.
Case #1: The angiography shows a suspected RCA anomaly.
Figure 4.
Case 1#: The ostium of RCA originates from the LCx.
Figure 4.
Case 1#: The ostium of RCA originates from the LCx.
3. Case 2
A 51 year old male presented to our hospital with a history of chest pain for 7 hours. He was a heavy smoker and hypertensive. His family history was unremarkable. At admission, his heart rate was 90 beats per minute and blood pressure was 130/80 mmHg. ECG showed ST-elevation in lead V1-V4 (Figure 5). Laboratory revealed elevated WBCs count (19,600), SGOT (210), and hsTnI (1,670).
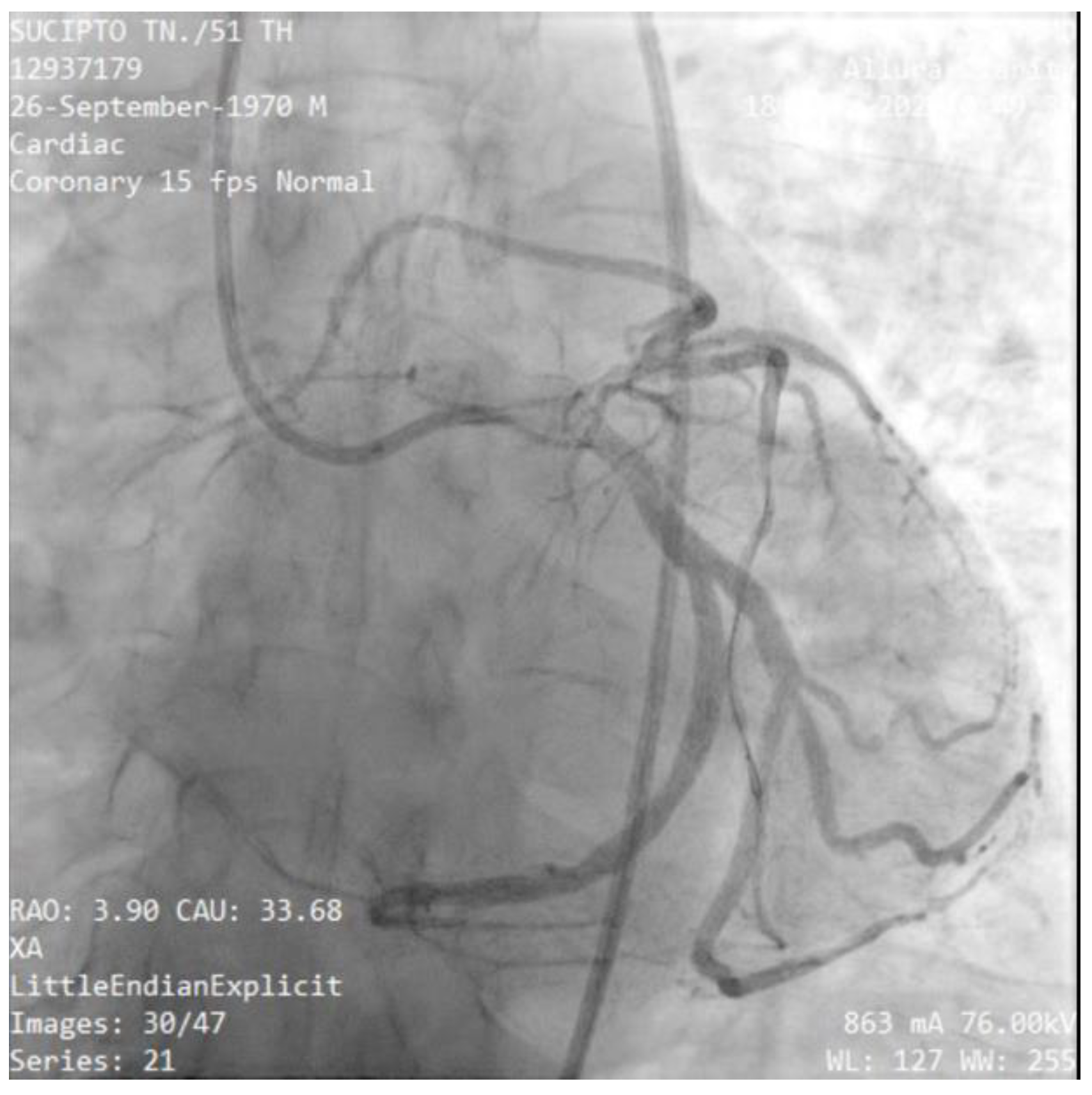
The patient was scheduled for primary percutaneous coronary intervention. Coronary angiography was performed angiography of the left coronary artery revealed a normal LMCA which divided into LAD and LCx (
Figure 6). The proximal LAD was giving branch to the RCA, whilst the mid portion of LAD was critically stenosis. The thrombus was aspirated stented in mid LAD with subsequent TIMI 3 flow distally (
Figure 8). The patient had an uneventful course after the intervention and was discharged in stable condition after 3 days.
Figure 5.
Case #2: ECG shows ST-elevation in lead V1-V4 .
Figure 5.
Case #2: ECG shows ST-elevation in lead V1-V4 .
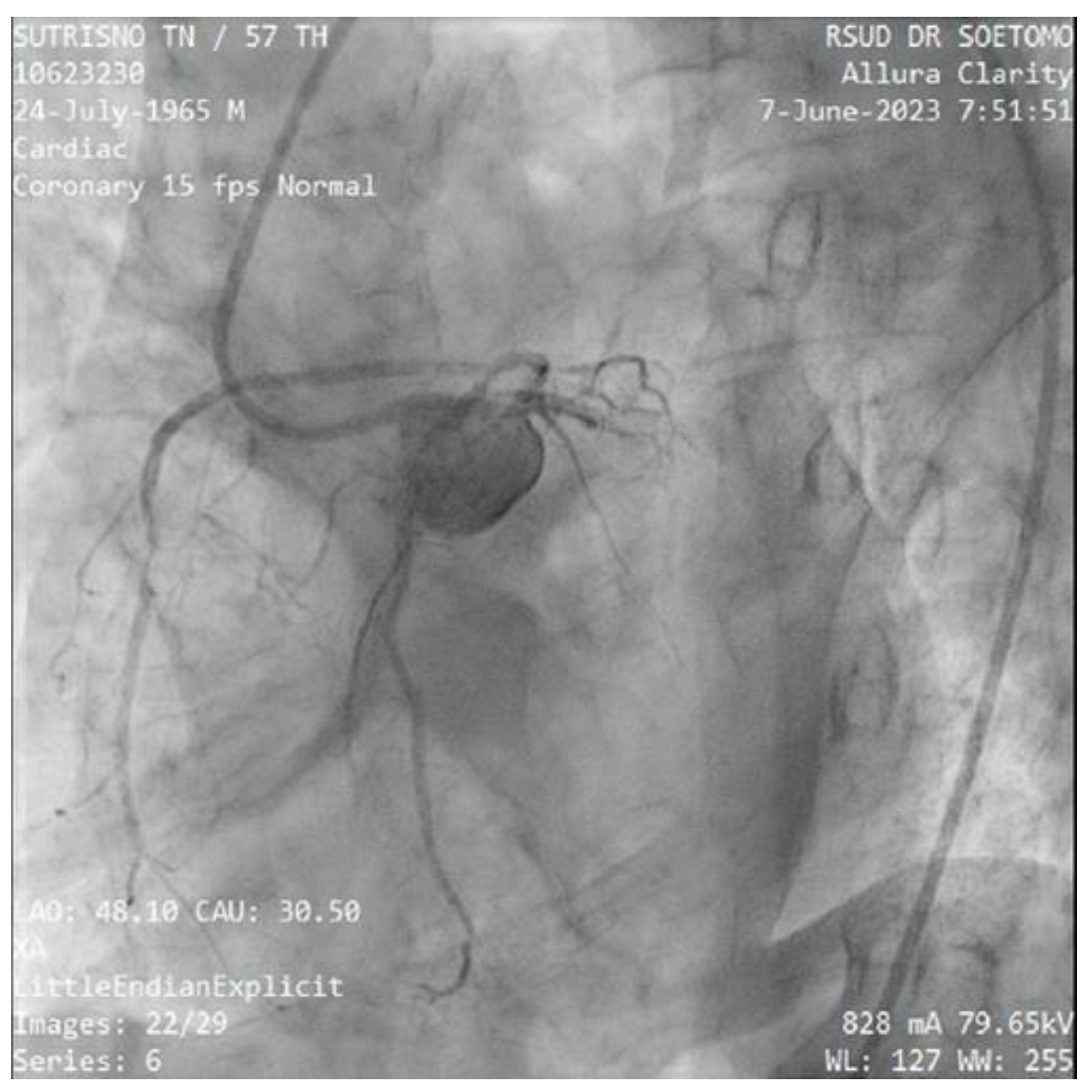
Figure 6.
Case #2: The angiography shows a normal LMCA which divided into LAD and LCx. There are a 99% stenosis of mid-LAD and the RCA originates from proximal-LAD.
Figure 6.
Case #2: The angiography shows a normal LMCA which divided into LAD and LCx. There are a 99% stenosis of mid-LAD and the RCA originates from proximal-LAD.
Figure 7.
Case #2: The RCA originates from the proximal-LAD.
Figure 7.
Case #2: The RCA originates from the proximal-LAD.
Figure 8.
Case #2: We dilate with balloon and stent in mid-LAD and TIMI flow grade of 3 was restored.
Figure 8.
Case #2: We dilate with balloon and stent in mid-LAD and TIMI flow grade of 3 was restored.
4. Case 3
A 57-year-old male with a history of being a smoker was admitted to our emergency department due to chest pain for 11-hours. He described the pain as 8 of 10 in severity. He also reported associated sweating, blurred vision and the syncope sensation. His family history was unremarkable. His vital signs were as follows: blood pressure 85/61 mmHg and heart rate 45 beats/min. Sulfa atropine 1 vial and dopamine pump 5 gamma was administered due to hypotension and bradycardia. Initial workup revealed hyperlipidaemia and high sensitivity troponin I. ECG showed sinus rhythm, TAVB and upsloping ST depression and peak T wave in V2-V5 leads (
de Winter sign) which refers to anterior STEMI
(Figure 9). He received a loading dose of aspirin 300 mg and clopidogrel 300 mg for STEMI. We decided to perform percutaneous coronary intervention (PCI). Coronary angiography found triple-vessel disease (TVD) coronary artery disease (CAD), which occluded at the LAD, LCx and RCA, and there was anomalous evidence that the RCA originates from diagonal branches of the LAD
(Figure 12).
Figure 9.
Case #3: ECG showed sinus rhythm, TAVB and upsloping ST depression and peak T wave in V2-V5 leads (de Winter sign) which refers to anterior STEMI.
Figure 9.
Case #3: ECG showed sinus rhythm, TAVB and upsloping ST depression and peak T wave in V2-V5 leads (de Winter sign) which refers to anterior STEMI.
Figure 10.
Case #3: Coronary angiography shows a single ostial left main coronary artery (LMC), located short and normally. It also revealed a 50% stenosis of the proximal-mid left anterior descending coronary artery (LAD).
Figure 10.
Case #3: Coronary angiography shows a single ostial left main coronary artery (LMC), located short and normally. It also revealed a 50% stenosis of the proximal-mid left anterior descending coronary artery (LAD).
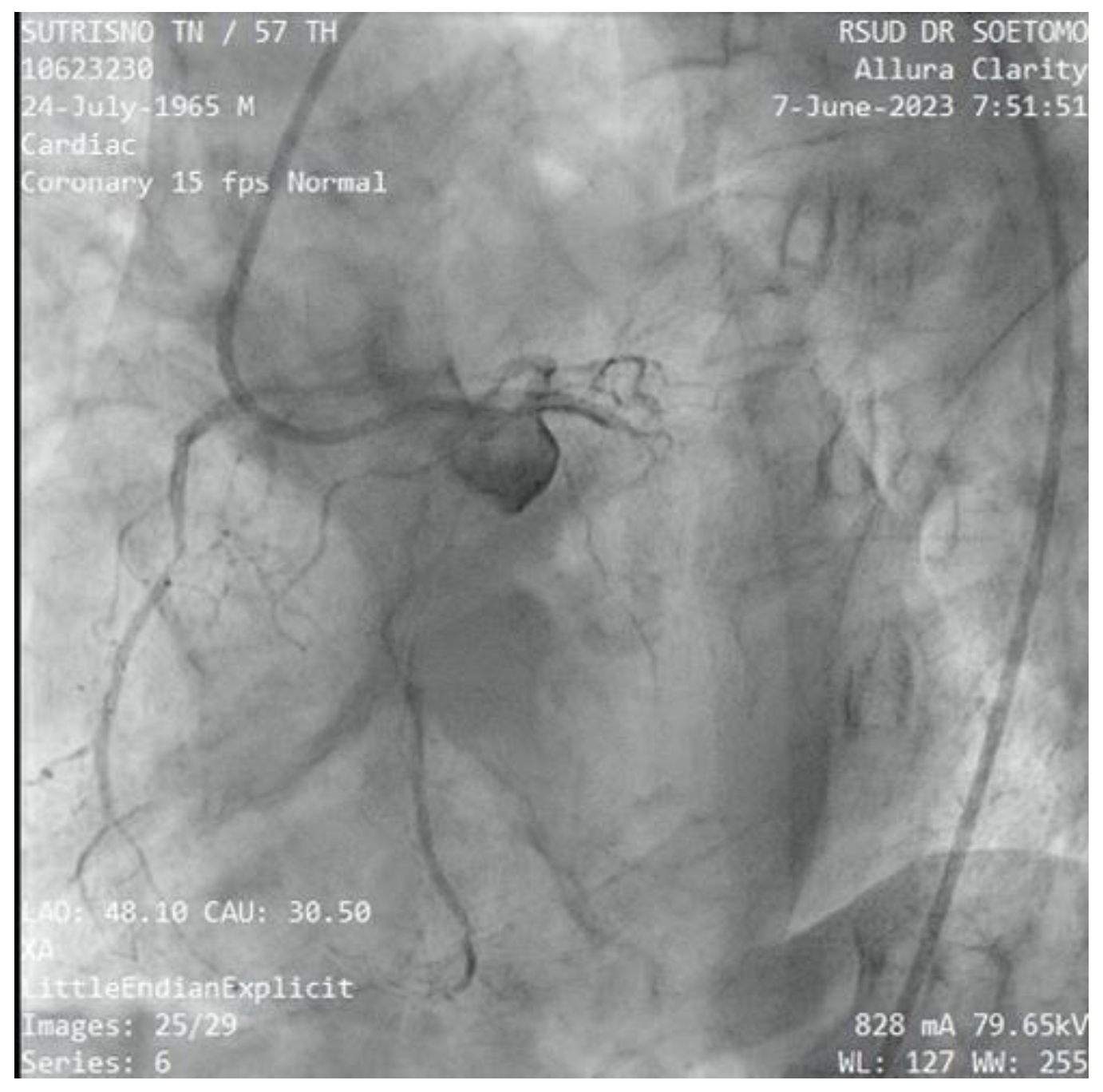
Figure 11.
Case #3: The angiography LAO; CAU view shows the LAD feeds collaterals from septal branches to the distal left circumflex coronary artery (LCx) and total occlusion of the ostial LCx.
Figure 11.
Case #3: The angiography LAO; CAU view shows the LAD feeds collaterals from septal branches to the distal left circumflex coronary artery (LCx) and total occlusion of the ostial LCx.
Figure 12.
Case #3: The RCA originates from the diagonal branches (D1) in which 90% of the proximal RCA was occluded. .
Figure 12.
Case #3: The RCA originates from the diagonal branches (D1) in which 90% of the proximal RCA was occluded. .
Following coronary angiography, we discussed the revascularization strategy. PCI was performed the LCX was stent, LAD and RCA occlusion was treated with balloons. During the action, the patient developed hypotension and bradycardia after the balloon implantation to proximal RCA occlusion. Epinephrine 400 nano/kgBW/minutes, vasopressin 300 nano/kgBW/minutes and dopamine 15 mcg/kgBW/minutes was given due to poor hemodynamic status, the patient intubated immediately. Suddenly, the ECG monitor showed asystole rhythm. He got cardiac-pulmonary resuscitation by the team for 30 minutes and was given epinephrine 1 mg for 8 times. Unfortunately, the patient did not survive from the cardiac arrest.
4. Discussion
The anomalous origin of coronary arteries is a rare finding, malformation that forms during fetal development. Their prevalence ranges from 0,24% to 1,3% in previously report.[
1,
2,
3] ACA can be divided as abnormalities in origin, course, clinical manifestation and complication. However, universal consensus on the ACA classification has not been exist.[
3] Consequently, there are numerous different types of ACA. This anomaly has been known as a second most common cause of sudden deaths among young athletes, after hypertrophic cardiomyopathy.[6]
SCA is a rare anomaly, ranging from 0,024% to 0,066% of individuals. It is defined as an isolated ostium coronary artery originating from the aortic trunk supplying the entire heart.[4,7] In majority, the previous SCA case report described an RCA originating from the proximal or middle portion of the LAD.[
2] The clinical manifestation varies from asymptomatic to symptomatic as a chest pain, ventricular fibrillation or myocardial infarction, which may lead to life-threatening conditions or sudden cardiac death.[8]
Here, we present three cases of the anomalous RCA originating from the LAD or LCx, associated with myocardial infarction event. As we know, myocardial inflation is one of the most mortality causes in the population, approximately 20% of these patients die within 1 year of the event.[9] Generally, myocardial infarct patients come to emergency settings with chest pain as a primary symptom, followed by breathing problems.[10] In these cases reported SCA patients complained of sudden chest pain with various time onset; 6 hours, 7 hours and 11 hours, consecutively. From the ECG examination, we revealed ST-elevation myocardial infarction (STEMI) in these three patients, where, first and third patients had sinus bradycardia which led to TAVB pattern, whilst the second patient had normal sinus rhythm.
The difference of the heart rate in ECG pattern may be due to the occlusion site of the myocardial infarction. In Case#1, There was a total occlusion in LCx, when we opened it, we found RCA’s ostium there as an anomalous coronary artery. Also, the Case#3 patient’s had RCA occlusion which it originated from LAD as an anomaly. As we know, occluded RCA that decreased the arterial blood flow may result in bradycardia rhythm and hypotension that the reflexes developed from ischemic right ventricle. The proximal RCA occlusion were more frequently to result in bradycardia-hypotension than the distal RCA occlusion.[11,12] The bradycardia rhythm is often used as a predictor of inferior myocardial infarction [12], that occurred in the first case. In Case#2, the patient had no RCA occlusion.
Another prior study of ACA’s condition with myocardial infarction revealed Brugada ECG’s pattern. The Brugada’s sign is associated with the right bundle branch block (RBBB) and ST-elevations in anterior precordial leads (V1 to V3).[13] The Pseudo-Brugada ECG’s pattern was found in a 36-year-old man presented with chest pain without cardiac history. After the cardiac catheterization, he surprisingly had an anomalous coronary artery of RCA originated from left coronary cusp, coursing between aorta and pulmonary artery without evidence of atherosclerotic coronary artery disease.[14] The similar report was also found in a 33-year-old man aborted from sudden cardiac death. The Brugada-like ECG was found after the cardiopulmonary resuscitation. The cardiac angiography of this patient also revealed the abnormal origin of RCA from the left coronary artery.[15] In our cases, we are also presenting the anomalous RCA originated from the left coronary artery in the setting of ischemic heart disease, but there were no Brugada ECG’s patterns as already reported. From Burch and Depaquales report in 1962, some investigators found the ECG’s pattern of the anomalous origin of left coronary artery from pulmonary artery (ALCAPA) in the infants, such as: deep & wide Q waves in Lead I, AVL, V4, V5, V6; T wave inversion in V5 and V6; ST-elevation or depression in Lead I, V5 and V6; tall R wave in V6 and deep S wave in V1; the electrical axis of the QRS complex lies between 60 and 90 degree in frontal plane.[16,17]
The ECG’s pattern of myocardial infarction in ACA’s patients compared with patients with normal coronary arteries has been lacking data. Due to the relatively few patients of ACA, the typical ECG pattern in anomalous coronary arteries is not yet found. To date, ECG examination could not be described as an diagnostic tool to identify the coronary anomalous or malformation. The prior ACA’s studies rarely displayed or mentioned the ECG’s typical characteristics of ACA.[16] Only a few congenital coronary anomalies have been reviewed.
The finding of ACA more often incidental during the workup for ischaemic heart disease. Cardiologists should be aware that a young individual with ischemia-like symptoms suspected the presence of ACA.[18] The modality assessment recommendation suggested coronary computed tomography angiography (CCTA) as gold standard for ACA’s diagnostic tool, followed by cardiac magnetic resonance (CMR) as an alternative.[19]
5. Conclusions
Because there are a limited number of ACA patients, the usual ECG pattern in anomalous coronary arteries has not been identified. Discovering ACA typically occurs by chance while investigating ischemic heart disease. Cardiologists need to recognize that a young person showing symptoms similar to ischemia might have ACA. The suggested method for evaluating ACA is coronary computed tomography angiography (CCTA), considered the most reliable diagnostic tool, and cardiac magnetic resonance (CMR) can be considered as another option.
Supplementary Materials
Video 1. Angiography with angle of fluoroscopy: RAO 22.5 CAU 22.0. The results of PCI didn’t show any flow to RCA, indicating a single coronary artery and suspected anomaly RCA. Video 2. Angiography with angle of fluoroscopy: LAO 45.30 CAU 0.20. The results after opening the total occlusion that occurred in the LCx, as soon as the LCx was opened there was a picture of the RCA. Video 3. Non-selective aortography showed single ostium left main coronary.
Author Contributions
Conceptualization, M.Y.A.; methodology, T.S.P.; software, B.P.D.K..; validation, R.A.N.; formal analysis, T.S.P.; investigation, B.P.D.K.; resources, R.A.N.; data curation, T.S.P.; writing—original draft preparation, B.P.D.K.; writing—review and editing, R.A.N.; visualization, B.P.D.K.; supervision, M.Y.A.; project administration, T.S.P.; funding acquisition, M.Y.A. All authors have read and agreed to the published version of the manuscript.” Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the case series.
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the stud. Written informed consent has been obtained from the patient(s) to publish this paper” if applicable.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.
Acknowledgments
Authors would like to thank Dr. Budi Baktijasa Dharmadjati, Dr. I Gde Rurus Suryawan, and Prof. Yudi Her Oktaviono for their excellence contribution in maintaining high quality of image in the cardiac catheterization laboratory at our hospital. Authors would like to thank all staff, fellows, residents and nurses who bravery work to save every life in cath lab.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Tuncer, C., Batyraliev, T., Yilmaz, R., Gokce, M., Eryonucu, B. and Koroglu, S. Origin and distribution anomalies of the left anterior descending artery in 70,850 adult patients: Multicenter data collection. Cathet. Cardiovasc. Intervent. 2006;68: 574-585. [CrossRef]
- Adam, E.L., Generoso, G. & Bittencourt, M.S. Anomalous Coronary Arteries: When to Follow-up, Risk Stratify, and Plan Intervention. Curr Cardiol Rep 23, 102 (2021). [CrossRef]
- Yamanaka, O. and Hobbs, R.E. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet. Cardiovasc. Diagn. 1990;21: 28-40. [CrossRef]
- Al Umairi, R., & Al-Khouri, M. Prevalence, Spectrum, and Outcomes of Single Coronary Artery Detected on Coronary Computed Tomography Angiography (CCTA). Radiology research and practice, 2019, 2940148. [CrossRef]
- Marchesini J, Campo G, Righi R, Benea G, Ferrari R. Coronary artery anomalies presenting with ST-segment elevation myocardial infarction. Clin Pract. 2011;1(4):e107. Published 2011 Nov 8. [CrossRef]
- Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8):1085-1092. [CrossRef]
- Desmet W, Vanhaecke J, Vrolix M, et al. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J. 1992;13(12):1637-1640. [CrossRef]
- Elbadawi A, Baig B, Elgendy IY, et al. Single Coronary Artery Anomaly: A Case Report and Review of Literature. Cardiol Ther. 2018;7(1):119-123. [CrossRef]
- Ye Q, Zhang J, Ma L. Predictors of all-cause 1-year mortality in myocardial infarction patients. Medicine (Baltimore). 2020;99(29):e21288. [CrossRef]
- Møller AL, Mills EHA, Gnesin F, et al. Impact of myocardial infarction symptom presentation on emergency response and survival. Eur Heart J Acute Cardiovasc Care. 2021;10(10):1150-1159. [CrossRef]
- Goldstein, James A.; Lee, Daniel T.; Pica, Mark C.; Dixon, Simon R.; O'Neill, William W.. Patterns of coronary compromise leading to bradyarrhythmias and hypotension in inferior myocardial infarction. Coronary Artery Disease 16(5):p 265-274, August 2005.
- Serrano CV Jr, Bortolotto LA, César LA, et al. Sinus bradycardia as a predictor of right coronary artery occlusion in patients with inferior myocardial infarction. Int J Cardiol. 1999;68(1):75-82. [CrossRef]
- Sangwatanaroj S, Prechawat S, Sunsaneewitayakul B, Sitthisook S, Tosukhowong P, Tungsanga K. New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives. Eur Heart J. 2001;22(24):2290-2296. [CrossRef]
- Sharma AK, Agnihotri A, Schachne J, Heist EK. Cardiac Arrest with “Pseudo Brugada” ECG Pattern in the Setting of Coronary Artery Anomaly. J Card Surg. 2010;25:614-617.
- Chang WT, Tsai WC, Lin CC. Interarterial course of coronary artery anomaly presenting as Brugada-like ECG and aborted cardiac death-Multidisciplinary images facilitate the diagnosis. J Formos Med Assoc. 2013;112(9):580-582. [CrossRef]
- Burch GE & DePasquale NP. The electrocardiogram in certain anomalies of the coronary arteries. American heart Journal. 1962;64(1):38-43.
- Lardhi AA. Anomalous origin of the coronary artery from pulmonary artery: A rare cause of myocardial infarction in children. Journal of Family and Community Meidicine. 2009;17(3):113-116.
- Gentile F, Castiglione V, Caterina RD. Coronary Artery Anomalies. Circulation. 2021;144(12):983-996.
- Frommelt P, Lopez L, Dimas VV, Eidem B, Han BK, Ko HH, Lorber R, Nii M, Printz B, Srivastava S, Valente AM, Cohen MS. Recommendations for Multimodality Assessment of Congenital Coronary Anomalies: A Guide from the American Society of Echocardiography: Developed in Collaboration with the Society for Cardiovascular Angiography and Interventions, Japanese Society of Echocardiography, and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2020 Mar;33(3):259-294. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).