1. Introduction
The global presbyopic population has been estimated to have grown to one billion, and thus the demand for presbyopic correction has steadily grown over time [
1]. Since multifocal contact lenses (CLs) have shown to be beneficial for obtaining good near to far visual outcomes without using spectacles for presbyopic subjects, they have been widely acknowledged as one of the non-surgical viable options for presbyopic correction [
2,
3,
4]. In fact, a wide variety of multifocal CL designs have become available in daily practice, but these multifocal CLs are dependent on effective optical diameter, illuminance environment, as well as lens centration and movement, and thus susceptible for the effect of pupil variations, illumination levels, and lens fitting, resulting in a deterioration of visual quality. Actually, it has been shown that the multifocal CL design directly influences the discontinuation of CL wear [
5].
Extended depth of focus (EDOF) CLs have been developed by the Brien Holden Vision Institute and have become commercially available in Japan in recent years. EDOF CLs may theoretically have several advantages over other conventional multifocal CLs, in terms of less dependency on pupil size, less dependency on CL movement, and less decrease of contrast sensitivity. Indeed, it has been reported that EDOF CLs were helpful to provide good near to intermediate vision without compromising far vision, suggesting their viability for presbyopic correction [
6,
7,
8,
9,
10,
11]. However, these previous studies were rather limited and mostly conducted by the same research group using prototype CLs, and thus it should be evaluated by many research groups using commercially available CLs for the further prevalence of this novel CL in a clinical setting. Moreover, detailed all-distance visual acuities have not so far been investigated for presbyopic healthy subjects. It may give us intrinsic insights into understanding the patient-derived characteristics of EDOF CLs in such a population. The goal of the present study is to prospectively evaluate the detailed visual performance and satisfaction of EDOF CLs in presbyopic subjects.
2. Materials and Methods
2.1. Study Population
This prospective observational study comprised a total of 42 eyes of 21 consecutive presbyopic subjects (1 men and 20 women, mean age ± standard deviation: 50.6 ± 7.5 years). Eyes with best corrected visual acuity of less than 0 logMAR, eyes with manifest astigmatism of ≥ 1.25 diopter (D), and eyes with any history of ocular surgery, ocular trauma, or other concomitant eye diseases, were excluded from the study. This study was approved by the Institutional Review Board at Miyata Eye Hospital (identifier; CS-394) and followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients after explanation of the nature and possible consequences of the study.
2.2. Extended Depth of Focus Contact Lens Prescription
We used a commercially available EDOF CL (1dayPure EDOF
TM, SEED Co., Ltd., Tokyo, Japan) in the current study. This CL has a non-monotonic, aperiodic, non-diffractive, non-aspheric, refractive power profile across the optic zone, and increases the depth of focus by deliberate manipulation of multiple modes of spherical aberration terms [
12,
13], with 3 different depth of focus profiles (+0.75 D, +1.50 D, and +2.25 D) for near vision in the center region, a base curve of 8.4 mm, and a lens diameter of 14.2 mm. During an initial trial, the lens power was targeted at emmetropia with the lowest depth of focus (+0.75 D), based on the manufacturer’s instructions. According to the manufacturer’s instructions, the spherical power and the depth of focus were adjusted after preliminary evaluation and determined based on patient preferences of far to near binocular vision. Contact lens fitting was confirmed by experienced ophthalmologists (TK and EK). The subjects were instructed to use these CLs daily for 2 to 4 weeks.
2.3. Assessment of Visual Performance
We quantitatively assessed visual acuity at all distances (0.3, 0.5, 0.7, 1, 2, 3, and 5 m) using an all-distance vision tester (AS-15, Kowa, Japan), higher-order aberrations (HOAs), contrast sensitivity, and patient satisfaction, before and during the EDOF CL wear in the study population. Ocular HOAs for 4- and 6-mm pupils were measured with a Hartmann-Shack aberrometer (KR-1W, Topcon, Tokyo, Japan). Total ocular HOAs were calculated as the root-mean-square of the third- and fourth-order coefficients. The contrast sensitivity function was obtained with a functional vision analyzer, (Optec 6500, Stereo Optical, Chicago, USA) under photopic (85 cd/m
2) and mesopic (3 cd/m
2) light conditions. The area under the log contrast sensitivity function (AULCSF) was calculated from the obtained data of contrast sensitivity, as described previously [
13]. In brief, the log of contrast sensitivity was plotted as a function of log spatial frequency, and third-order polynomials were fitted to the data. The fitted function was integrated, and the resultant value was expressed as the AULCSF. Overall satisfaction was assessed using visual analogue scale (VAS) symptom intensity scores on a scale of 0 (no satisfaction) to 100 (maximum satisfaction). All examinations were performed by experienced ophthalmic technicians.
2.4. Statistical Analysis
We conducted statistical analyses by using a commercially available statistical software (Bellcurve for Excel, Social Survey Research Information Co, Ltd., Tokyo, Japan). Since all data did not fulfill the criteria for normal distribution by the Kolmogorov-Smirnov test, the Wilcoxon signed-rank test was applied to compare the two groups before and during CL wear. The results are expressed as mean ± standard deviation, and a value of p<0.05 was considered statistically significant.
3. Results
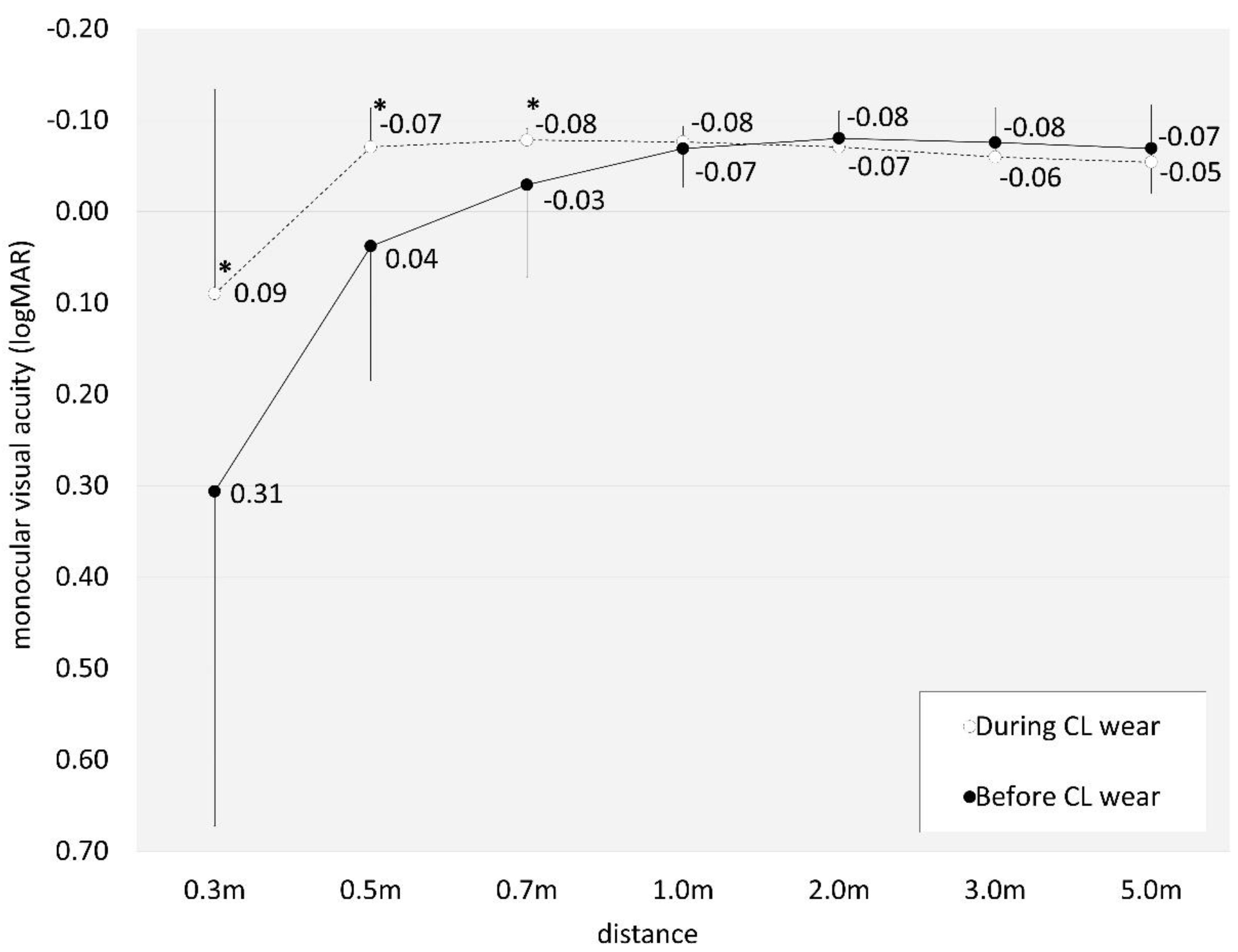
Table 1 shows the demographics of the study population. Eyes fitted with a depth of focus designation of +0.75, +1.50, and +2.25 D were 30 (71%), 12 (29%), and 0 (0%) eyes, respectively. Neither CL-related nor non-related complications occurred in any case throughout the observation period. Monocular visual acuity at 0.3, 0.5, 0.7, 1, 2, 3, and 5 m during EDOF CL wear was 0.09 ± 0.22, -0.07 ± 0.04, -0.08 ± 0.01, -0.08 ± 0.02, -0.07 ± 0.04, -0.06 ± 0.05, and -0.05 ± 0.06, respectively. We found a significant improvement at near to intermediate distances (0.3, 0.5, and 0.7m)(Wilcoxon signed-rank test, p⋖0.001, p⋖0.001, and p=0.003), but no significant change at intermediate to far distances (1, 2, 3, and 5 m)(p=0.480, p=0.180, p=0.070, and p=0.393) between before and during CL wear (
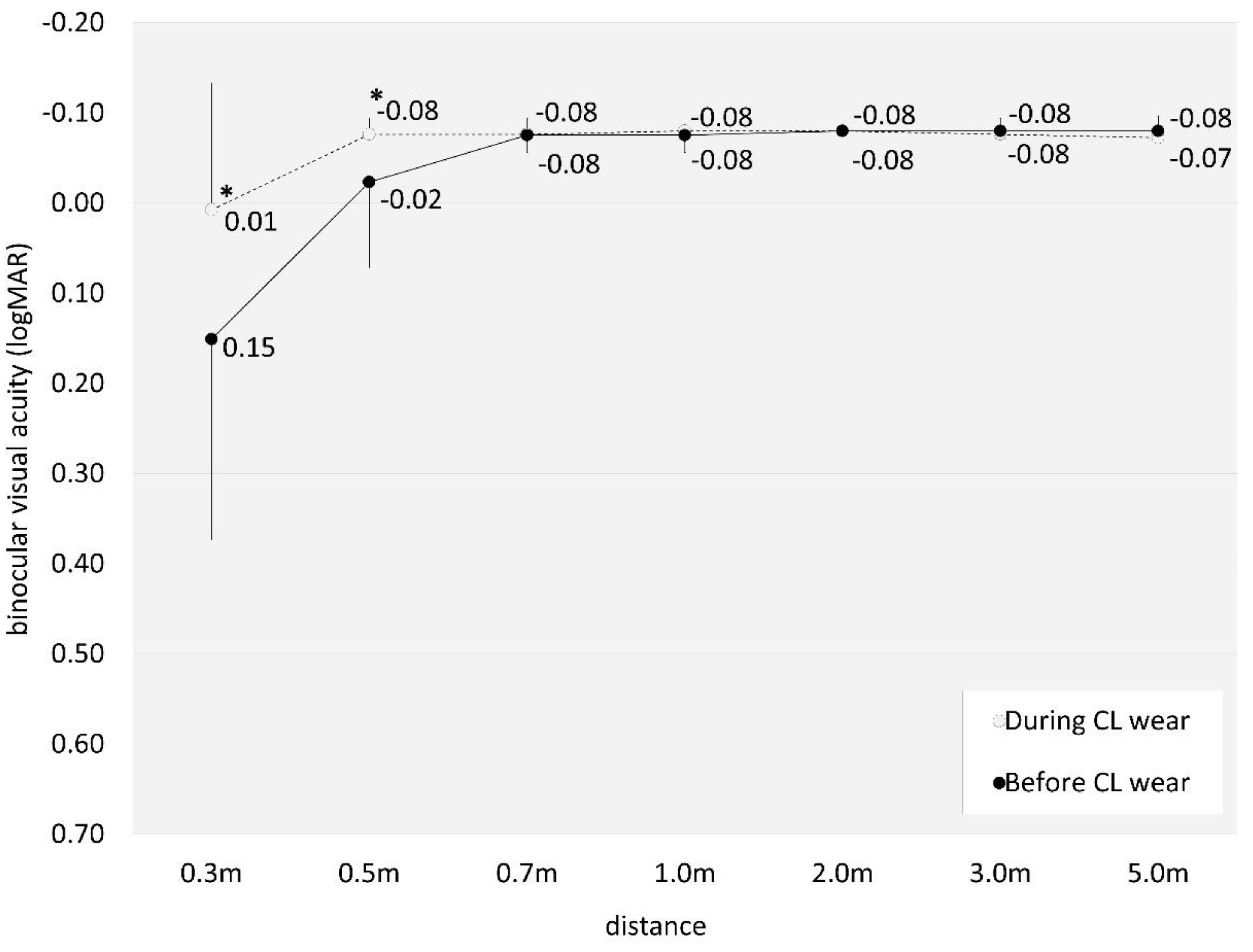
Figure 1). Binocular visual acuity at 0.3, 0.5, 0.7, 1, 2, 3, and 5 m during EDOF CL wear was 0.01 ± 0.14, -0.08 ± 0.02, -0.08 ± 0.02, -0.08 ± 0.00, -0.08 ± 0.00, -0.08 ± 0.02, and -0.07 ± 0.02, respectively. We found a significant improvement at near to intermediate distances (0.3, and 0.5m)(p=0.011, and p=0.026), but no significant change at intermediate to far distances (0.7, 1, 2, 3, and 5m)(p=1.000, p=0.317, p=1.000, p=0.317, and p=0.157) by EDOF wear (
Figure 2).
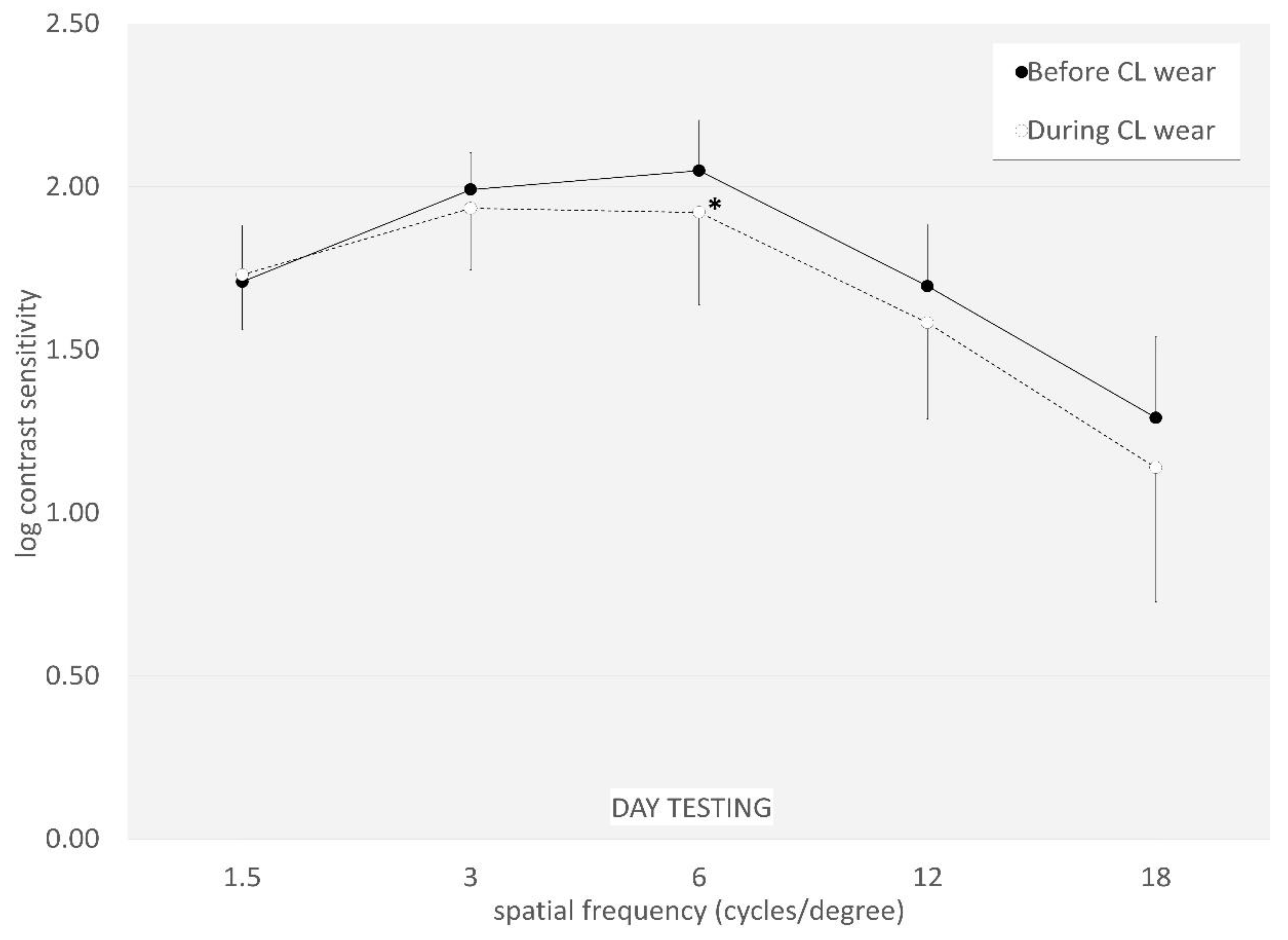
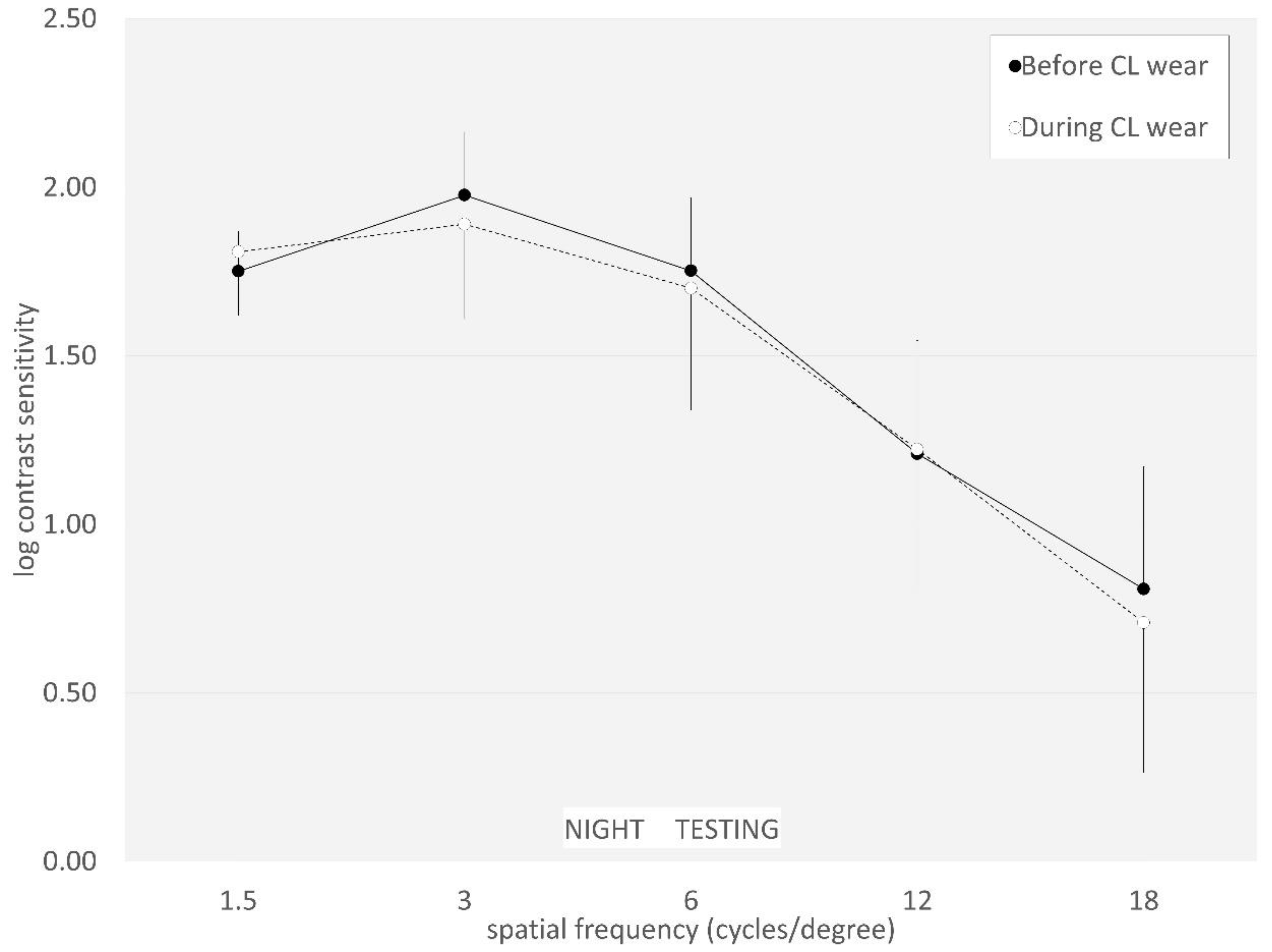
The AULCSF did not significantly change from 2.00 ± 0.12 to 1.91 ± 0.22 under photopic conditions (p=0.099). It also did not significantly change from 1.76 ± 0.20 to 1.72 ± 0.31 under mesopic conditions (p=0.689). Log contrast sensitivity did not significantly change at any spatial frequencies, except for at 6 cycles/degrees (p=0.042) under photopic conditions (
Figure 3 and
Figure 4).
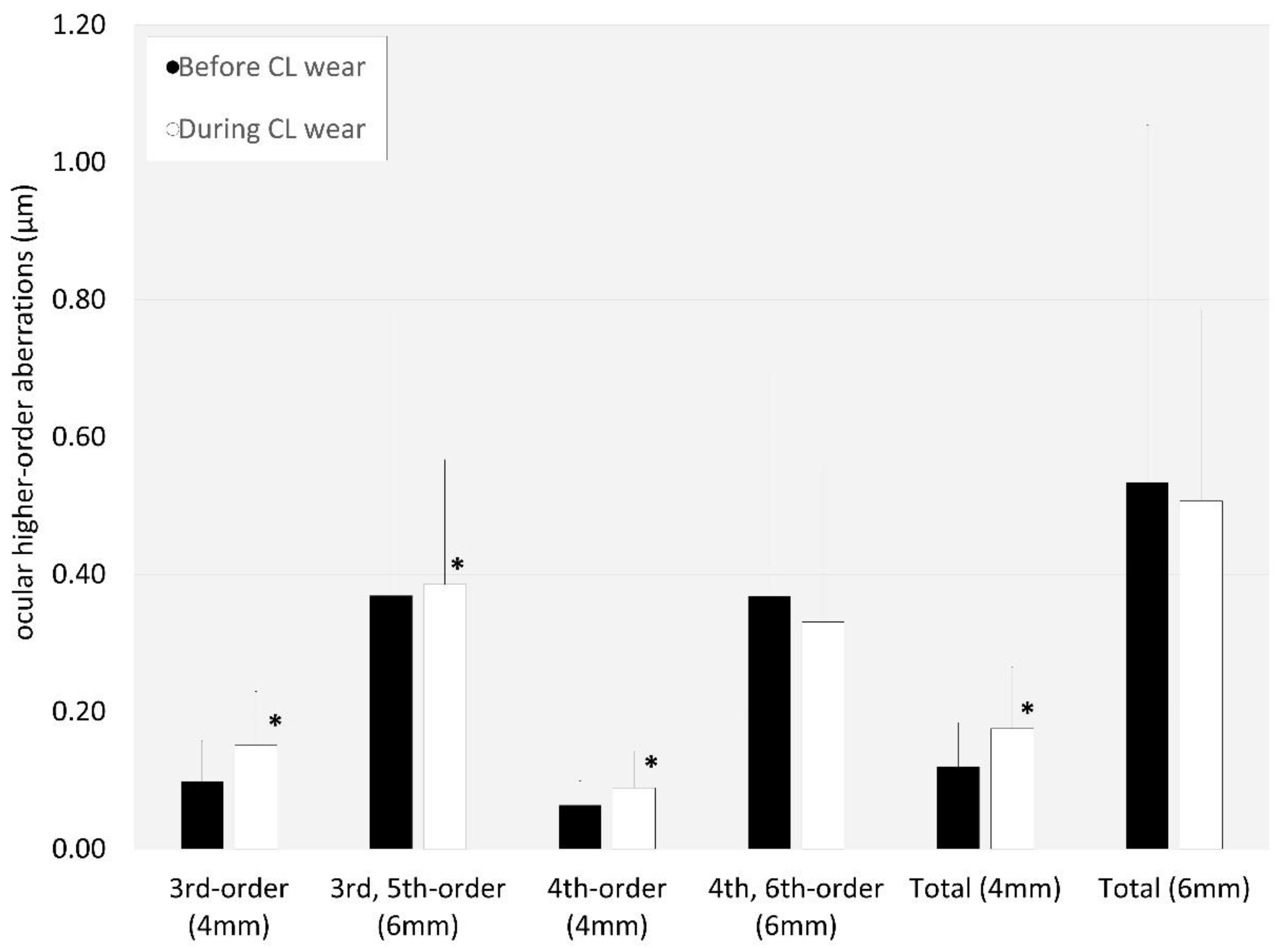
Ocular higher-order aberrations significantly increased during CL wear, except for fourth-order and sixth-order or total HOAs for a 6-mm pupil (p=0.563, or p=0.615)(
Figure 5). The overall satisfaction score significantly improved from 37.9 ± 31.3 to 65.7 ± 23.0 during EDOF CL wear (p=0.008).
Table 1.
Demographics of the study population.
Table 1.
Demographics of the study population.
| Patient demographics |
| Age |
50.6 ± 7.5 years (range, 40 to 64 years) |
| Gender |
Male : Female = 1 : 20 |
| Corrected visual acuity (logMAR) |
-0.17 ± 0.03 (range, -0.08 to -0.18) |
| Manifest spherical equivalent |
-1.99 ± 2.49 D (range, -7.00 to 0.88 D) |
| Mean astigmatism |
0.52 ± 0.35 D (range, 0 to 1.00 D) |
Figure 1.
Graph showing monocular visual acuity at all distances (0.3, 0.5, 0.7, 1, 2, 3, and 5 m) before and during extended depth of focus contact lens wear.
Figure 1.
Graph showing monocular visual acuity at all distances (0.3, 0.5, 0.7, 1, 2, 3, and 5 m) before and during extended depth of focus contact lens wear.
Figure 2.
Graph showing binocular visual acuity at all distances (0.3, 0.5, 0.7, 1, 2, 3, and 5 m) before and during extended depth of focus contact lens wear.
Figure 2.
Graph showing binocular visual acuity at all distances (0.3, 0.5, 0.7, 1, 2, 3, and 5 m) before and during extended depth of focus contact lens wear.
Figure 3.
Graph showing contrast sensitivity function before and during extended depth of focus contact lens wear under photopic conditions.
Figure 3.
Graph showing contrast sensitivity function before and during extended depth of focus contact lens wear under photopic conditions.
Figure 4.
Graph showing contrast sensitivity function before and during extended depth of focus contact lens wear under mesopic conditions.
Figure 4.
Graph showing contrast sensitivity function before and during extended depth of focus contact lens wear under mesopic conditions.
Figure 5.
Graph showing ocular higher-order aberrations before and during extended depth of focus contact lens wear.
Figure 5.
Graph showing ocular higher-order aberrations before and during extended depth of focus contact lens wear.
4. Discussion
In the current study, In the current study, our results showed that EDOF CLs provided a significantly better visual performance at near to intermediate distances, and subsequent higher patient satisfaction, but that it induced a slight deterioration of contrast sensitivity function in this presbyopic population. There has so far been only one clinical study on the visual performance of this commercially available EDOF CL, but it has only focused on a pseudophakic population [
10]. With regard to the prototype of the EDOF CL, Tilla et al.[
5,
6] and Bakaraju et al.[
7] showed, in a prospective, randomized, clinical trial, that it provided better intermediate and near vision than other commercially available multifocal CLs without compromising far vision. Sha et al.[
8] showed that EDOF CLs provided significant improvements over commonly used aspheric, center-near design multifocal CLs in vision clarity at near to intermediate, overall lack of ghosting, vision stability, and overall vision satisfaction. Martínez-Alberquilla et al.[
9] demonstrated that both EDOF and other multifocal CLs offered good visual quality without compromising the ocular surface integrity and provided similar symptomatology levels for presbyopic patients. Their previous findings were in agreement with our current findings of EDOF CLs. Hiraoka et al.[
10] showed that the EDOF CL exhibited a substantially improved vision at near to intermediate distances even in patients undergoing monofocal intraocular lens implantation. Coupled with their findings, it is indicated that this novel EDOF CL can be widely applied not only for presbyopic phakic, but also pseudophakic patients in a clinical setting.
We observed that there were no significant decreases in contrast sensitivity function, except for at 6 cycles/degrees under photopic conditions, and that contrast sensitivity function was within the normal range during the EDOF CL wear. Interestingly, the decline in contrast sensitivity function under mesopic light conditions was lower than that under photopic light conditions in this study population, as evidenced by the corresponding AULCSF values. It might be somewhat attributed to less dependency in pupil diameter and illumination levels of the EDOF CL in comparison with other multifocal CLs. Hiraoka et al.[
10] also stated that contrast sensitivity slightly declined at the middle to high spatial frequencies in eyes that underwent cataract surgery. We assume that this discrepancy was possibly due to the differences in the additional powers of the EDOF CL (low to middle vs. middle to high). We also found that the change in distance visual acuity was minimal and non-significant during EDOF CL wear. It may be useful for presbyopic patients who wish to obtain good visual outcomes especially at a far distance. We assume that this EDOF CL can be applied for presbyopic patients who wish to usually drive a car at night. Novillo-Díaz et al.[
5] demonstrated that poor far vision was the most common cause for multifocal CL discontinuation. Based on our findings that the effect on far vision was essentially minimal among multifocal CLs, this EDOF CL may also work well for continuous use in daily life.
There are some limitations to this study. First, we did not use other CLs as a control group, since our primally goal is not to compare the visual performance of two different CLs, but to assess the changes in visual performance before and during EDOF CL wear, which may be helpful for grasping the real-world experience of this promising CL. Second, the sample size was relatively small, and gender was biased in this study population. Third, we did not assess long-term visual outcomes of EDOF CL wearers. A further long-term study in a large cohort of patients is still necessary to confirm the authenticity of our results.
5. Conclusions
In summary, our results may support the view that EDOF CLs are effective for obtaining good near to far vision and subsequent high overall satisfaction, even though contrast sensitivity function slightly decreases. Based on our findings, we believe that EDOF CLs are one of the feasible options for presbyopic correction, particularly when patients prioritize far vision even when wearing presbyopic CLs.
Author Contributions
Conceptualization, K.K., T.K., and K.M.; Data curation, T.K. S.H. M.H. and E.K..; Investigation, K.K., and T.K.; Methodology, K.K., and T.K..; Supervision, K.M..; Visualization, K.K.; Writing—review & editing, K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board at Miyata Eye Hospital (identifier; CS-394).
Informed Consent Statement
Written informed consent was obtained from all patients after explanation of the nature and possible consequences of the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, KK, upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
CL; contact lens, EDOF; extended depth of focus, D; diopter, HOAs; higher-order aberrations, AULCSF; area under the log contrast sensitivity function, VAS; visual analogue system, logMAR; logarithm of the minimal angle of resolution.
References
- Holden, B.A.; Fricke, T.R.; Ho, S.M.; Wong, R.; Schlenther, G.; Cronjé, S.; Burnett, A.; Papas, E.; Naidoo, K.S.; Frick, K.D. Global Vision Impairment Due to Uncorrected Presbyopia. Arch. Ophthalmol. 2008, 126, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Davies, L.N. Presbyopia: Effectiveness of correction strategies. Prog. Retin. Eye Res. 2019, 68, 124–143. [Google Scholar] [CrossRef] [PubMed]
- Molina-Martín, A.; Piñero, D.P.; Martínez-Plaza, E.; Rodríguez-Vallejo, M.; Fernández, J.M. Efficacy of Presbyopia-Correcting Contact Lenses: A Systematic Review. Eye Contact Lens: Sci. Clin. Pr. 2023, 49, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.B.; Efron, N.; Woods, C.A. International contact lens prescribing in 2022. Contact Lens Spectr 2023, 38, 28–35. [Google Scholar]
- Novillo-Díaz, E.; Villa-Collar, C.; Narváez-Peña, M.; Martín, J.L.R. Fitting success for three multifocal designs: Multicentre randomised trial. Contact Lens Anterior Eye 2018, 41, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Tilia, D.; Bakaraju, R.C.; Chung, J.; Sha, J.; Delaney, S.; Munro, A.; Thomas, V.; Ehrmann, K.; Holden, B.A. Short-Term Visual Performance of Novel Extended Depth-of-Focus Contact Lenses. Optom. Vis. Sci. 2016, 93, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Tilia, D.; Munro, A.; Chung, J.; Sha, J.; Delaney, S.; Kho, D.; Thomas, V.; Ehrmann, K.; Bakaraju, R.C. Short-term comparison between extended depth-of-focus prototype contact lenses and a commercially-available center-near multifocal. J. Optom. 2016, 10, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Bakaraju, R.C.; Tilia, D.; Sha, J.; Diec, J.; Chung, J.; Kho, D.; Delaney, S.; Munro, A.; Thomas, V. Extended depth of focus contact lenses vs. two commercial multifocals: Part 2. Visual performance after 1 week of lens wear. J. Optom. 2018, 11, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Sha, J.; Tilia, D.; Kho, D.; Diec, J.; Thomas, V.; Bakaraju, R.C. Comparison of Extended Depth-of-Focus Prototype Contact Lenses With the 1-Day ACUVUE MOIST MULTIFOCAL After One Week of Wear. Eye Contact Lens: Sci. Clin. Pr. 2018, 44 Suppl 2, S157–S163. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Alberquilla, I.; García-Montero, M.; Ruiz-Alcocer, J.; Crooke, A.; Madrid-Costa, D. Visual function, ocular surface integrity and symptomatology of a new extended depth-of-focus and a conventional multifocal contact lens. Contact Lens Anterior Eye 2020, 44, 101384. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, T.; Kiuchi, G.; Hiraoka, R.; Kotsuka, J.; Kinoshita, Y.; Oshika, T. Comparison of visual performance between extended depth of focus contact lens and single-vision contact lens in eyes with monofocal intraocular lens. Jpn. J. Ophthalmol. 2021, 65, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Bakaraju, R.C.; Ehrmann, K.; Ho, A. Extended depth of focus contact lenses vs. two commercial multifocals: Part 1. Optical performance evaluation via computed through-focus retinal image quality metrics. J. Optom. 2018, 11, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Plainis, S.; Atchison, D.A.; Charman, W.N. Power Profiles of Multifocal Contact Lenses and Their Interpretation. Optom. Vis. Sci. 2013, 90, 1066–1077. [Google Scholar] [CrossRef] [PubMed]
- A Applegate, R.; Howland, H.C.; Sharp, R.P.; Cottingham, A.J.; Yee, R.W. Corneal Aberrations and Visual Performance After Radial Keratotomy. J. Refract. Surg. 1998, 14, 397–407. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).