1. Introduction
Preterm birth, defined as a birth before 37 weeks of gestation, is a significant public health concern, affecting approximately 11% of all live births globally and accounting for more than 1 million infant deaths annually [
1,
2]. Spontaneous preterm delivery (sPTB) not only has immediate consequences such as neonatal mortality and morbidity but also has long-term implications including cognitive, behavioral, and neurological deficits in the surviving infants [
3,
4]. Consequently, early and accurate prediction of sPTB is of paramount importance to improve neonatal outcomes and reduce healthcare costs [
5].
Despite the substantial progress in understanding the pathophysiology of preterm birth, predicting and preventing it remains a significant challenge [
6,
7,
8]. Several conventional methods have been employed to identify women at risk of sPTB, including maternal history, clinical examination, biochemical markers, and ultrasound-based cervical length measurement [
9,
10]. However, these methods have their limitations, such as low sensitivity and specificity, invasive nature, or the need for skilled personnel [
10,
11]. Thus, there is an increasing demand for an accurate, inexpensive, and easy-to-use technique for the early prediction of preterm delivery.
Cervical elastography has emerged as a diagnostic tool for the assessment of the cervix's biomechanical properties during pregnancy [
12,
13]. The rationale behind using cervical elastography for predicting preterm delivery lies in the fact that the cervix undergoes significant structural and functional changes throughout pregnancy, including softening, shortening, and dilation, which can be detected by elastographic techniques [
14]. Several studies have reported association between cervical stiffness and the risk of preterm delivery [
15,
16]. Reduced cervical stiffness, as assessed by elastography, has been found to correlate with a higher likelihood of preterm birth [
17,
18]. Furthermore, some researchers have demonstrated that cervical elastography may outperform conventional cervical length measurement in predicting preterm delivery [
19,
20]. However, the optimal elastographic parameters for predicting preterm birth remain uncertain, and the results are often inconsistent and inconclusive [
21,
22,
23]. Additionally, this method requires high-end ultrasound imaging equipment, which can be expensive.
To investigate a novel elastographic approach for cervical measurements, a cost-effective Cervix Monitor (CM) device was designed featuring a tactile ultrasound probe with four tactile sensors and a single ultrasound transducer. A pilot clinical study with the CM probe involving 10 non-pregnant and 10 pregnant women demonstrated clinically acceptable measurement performance and reproducibility. The availability of stress-strain data enabled assessment of cervical elasticity and length [
24].
The objective of this study is to evaluate the efficacy of the tactile ultrasound approach in predicting preterm delivery at 24-28 weeks of gestation in women with singleton pregnancies.
2. Materials and Methods
2.1. Study Design
A prospective observational study was conducted at Rutgers Robert Wood Johnson Medical School (New Brunswick, NJ) and The Cooper Health System (Camden, NJ) between January 2020 and April 2022. Women with singleton pregnancy, between 24-28 weeks of gestation, were enrolled. Women with ruptured membranes, dilated cervices, planned cerclage, planned indicated preterm delivery, active cancer of lower urogenital tract, active viral or ulcerative lesions in the lower urogenital tract were excluded. The Informed Consent Form and Clinical Protocol were reviewed and approved centrally by the Western Institutional Review Board before the study's initiation. Demographic data including maternal age, race/ethnicity (NIH requirement), height, recorded weight at time of examination, parity, and prior obstetrical history was recorded at time of informed consent. Maternal comfort level of the CM examination was recorded on a 3-point scale (1- more comfortable than bimanual examination, 2-same, 3- less comfortable). Mode of delivery and gestational age at delivery was extracted from the electronic database at a later date.
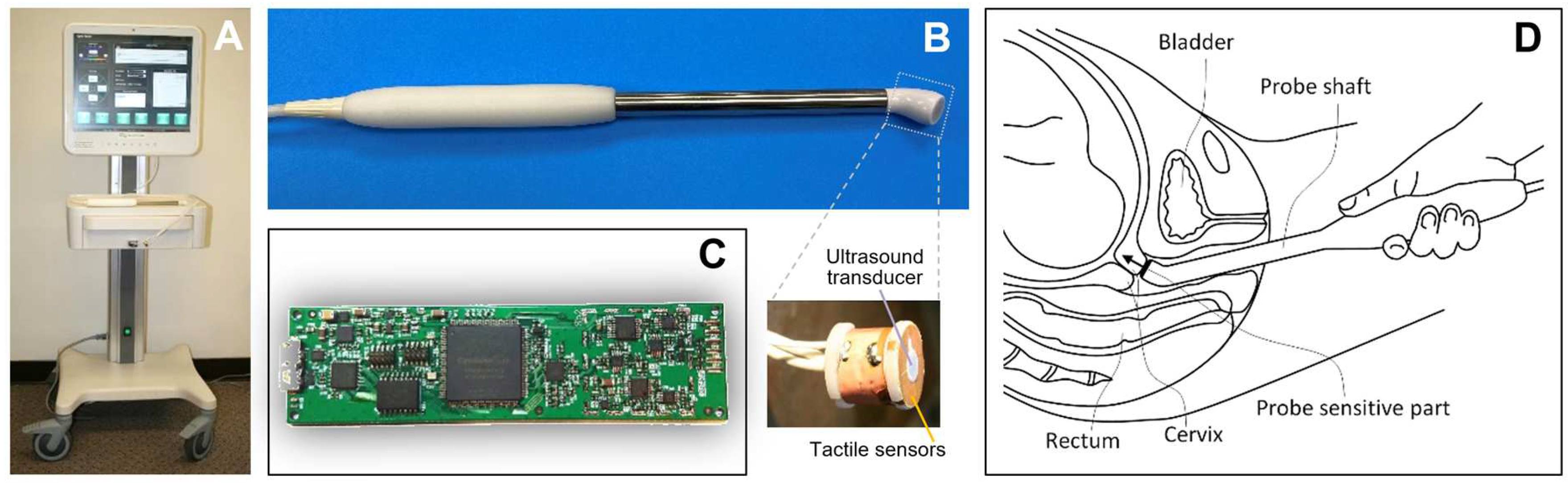
This study was conducted in two phases: development and validation. In the development phase, the CM examination procedure was optimized and ultrasound B-mode images with the CM probe were recorded for the cervix during the CM probe application to verify anatomical locations of the probe during measurements. The device, shown in
Figure 1, was used in the validation study. The approximate duration of the CM examination procedure on two cervical sectors is two minutes.
2.2. Cervix Monitor
The CM was designed as a cart-based device (
Figure 1A) featuring a medical-grade touchscreen computer and a detachable cervical probe (
Figure 1B). The CM probe comprises a tactile array with four capacitive pressure sensors surrounding an ultrasound transducer, as illustrated in
Figure 1B. The probe sensitive plane was angled by 40 degrees from the basic probe axis (see
Figure 1D).
The ultrasound 5.0 MHz transducer, operating in pulse-echo mode with a data acquisition resolution of 20 ns (50 MHz sample rate), has a diameter of 3.0 mm. Biocompatible, two-component silicones were used to ensure sensor assembly functionality, durability, stability, and mechanical protection. The pressure measurement noise level was below 30 Pa within the operational range of 30 kPa. The ultrasound transmitting pulses had a peak amplitude below 50 V and a length less than 1 µs, providing acoustic power significantly below the FDA-established limits for ultrasound emission in obstetrics: spatial-peak temporal-average (I
spta) of 13 mW/cm
2, spatial-peak pulse-average intensity (I
sppa) of 86 W/cm
2, and mechanical index (MI) of 1.0. Medical-grade 316 stainless steel, commonly used in the production of surgical instruments, was employed to fabricate the probe body (see
Figure 1B). A proprietary printed circuit board (see
Figure 1C) was designed to perform the dual functions of tactile signal acquisition and generation/acquisition of synchronized ultrasound signals. Its key features include serving four tactile/pressure sensors and one ultrasound transducer at 100 data frames per second. Important that no expensive components were used in the CM probe and electronics shown in
Figure 1.
A custom-designed linear array of 32 ultrasound transducers (Vermon, France) was used in the same cervical probe to image the cervical tissue around the probe in B-mode with ArtUs electronics (Telemed, Vilnius, Lithuania) in the development study.
The CM software interface enabled real-time observation of the cervical ultrasound signal as well as the applied pressure. The cervical length was calculated from the time-of-flight of an ultrasound pulse reflected from the internal cervical surface; similar to used technique in the feasibility study [
24]. The ultrasound peak position for the cervical internal surface was detected using a signal envelope after Gaussian complex wavelet filtering [27] in C++. The cervical elasticity was calculated as a ratio of the applied load (stress) on the cervix surface from the CM probe to the resultant changes in cervical length (strain). This approach was optimized with soft silicone tissue models with known parameters in bench testing and verification.
2.3. Examination Procedure
The CM examination procedure included: (1) placing the patient in the lithotomy position, (2) inserting the speculum into the vagina to ensure proper visualization and access to the cervix, and (3) performing CM measurements at 12 and 6 o'clock with real-time observation of applied pressure level and capturing the reflected ultrasound signal. The applied cervix pressure was limited to 30 kPa (<2.5 N to the probe tip) during CM measurements.
2.4. Statistical Analysis
General descriptive statistics (mean values, standard deviations, boxplots) and p-values for two-sample t-tests were calculated with MATLAB version R2022b (MathWorks, MA). Receiver operating characteristic (ROC) analysis was performed with MedCalc 2023 software (MedCalc Software Ltd, Belgium). Method of DeLong et al. [28] was employed for calculation of the 95% confidence intervals for ROC analysis.
3. Results
Overall, this study enrolled 166 women. Five subjects did not attend the CM examination, seven were lost to follow-up, and two cases were lost due to an operator error in CM data recording. The development study included 34 patients, while the validation study involved 132 patients. Among these 132 cases, spontaneous preterm birth occurred in eight cases and five preterm births happened in 5 women due to clinically indicated maternal or fetal conditions.
In the following data analysis, the CM examination data for 127 women at 24
0/7 - 28
6/7 gestational weeks were used.
Table 1 presents basic characteristics for the spontaneous preterm group of 8 subjects and the term group of 119 subjects. The mean maternal age, subject's height, weight, and gestational age at CM examination showed no statistically significant differences between both groups (
Table 1).
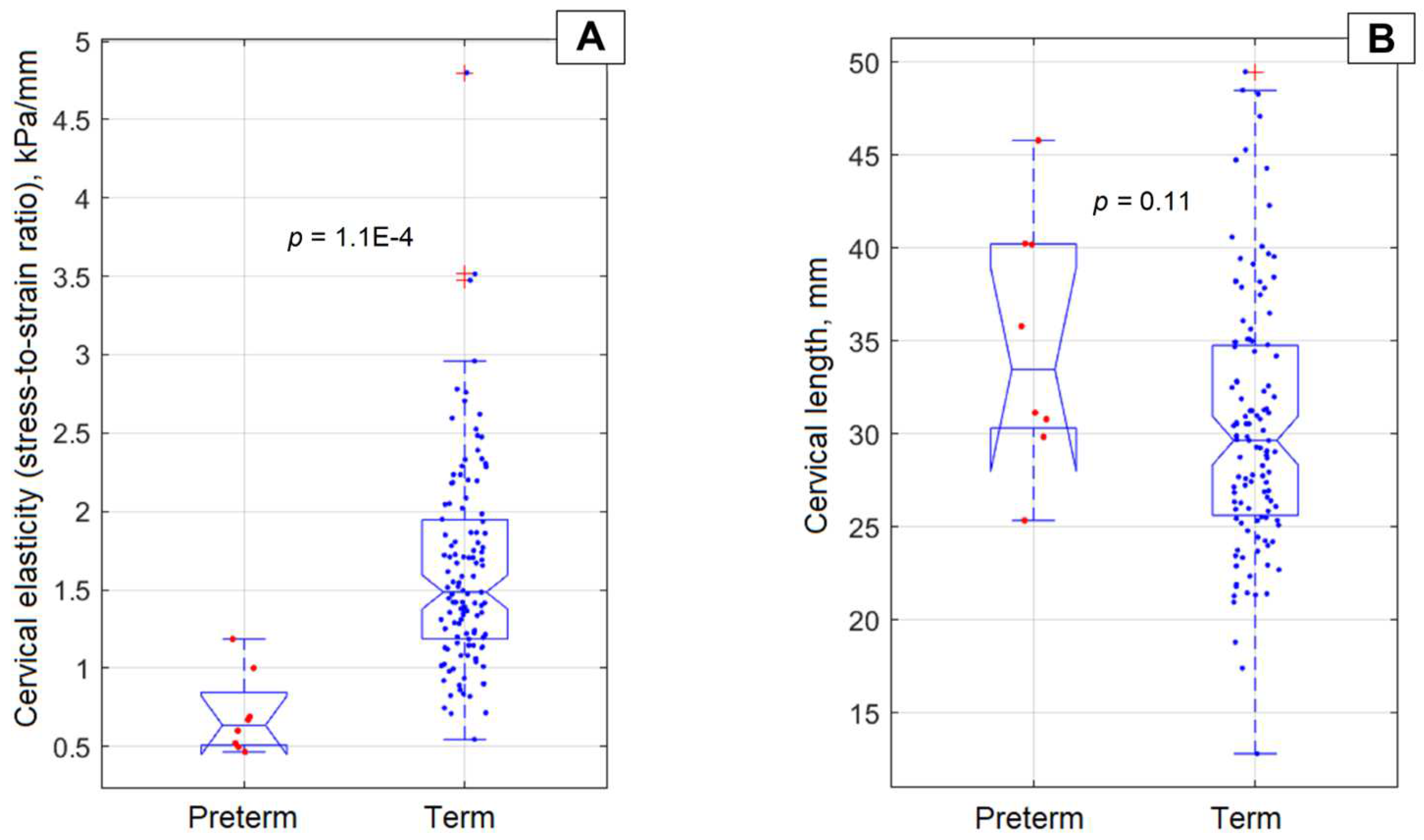
The mean gestational age for the preterm group was 34 weeks and five days, while for the term group it was 39 weeks and one day. There was no statistically significant difference between these groups regarding cervical length (p-value = 0.11). The preterm group demonstrated lower cervical stress-to-strain ratio (elasticity) values in both the anterior and posterior cervical compartments, with average values across these compartments being 0.70±0.26 kPa/mm, compared to 1.63±0.65 kPa/mm for the term group; this difference was statistically significant with a p-value of 1.1×10-4.
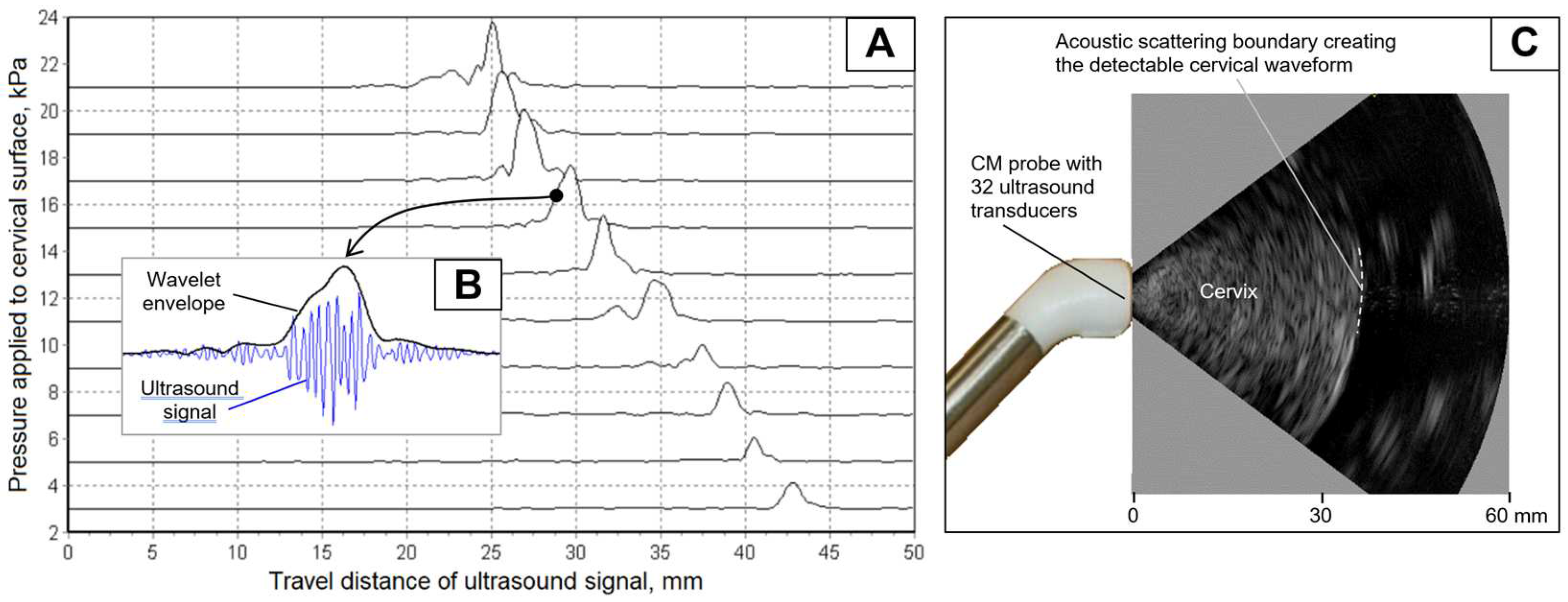
Figure 2 illustrates the acquisition of return acoustic signals from the internal cervical surface during the application of measured pressure (see vertical axis in
Figure 2A) from the probe to the cervical external surface. As shown, the cervix has been compressed from 43 mm to 25 mm at an applied pressure of 21 kPa.
Figure 2B presents the original ultrasound waveform with an envelope calculated with a complex Gauss wavelet at 5.0 MHz. To ensure that we capture the signal from the internal cervical surface, we incorporated an ultrasound array in the same probe, which provided B-mode imaging (see
Figure 2C).
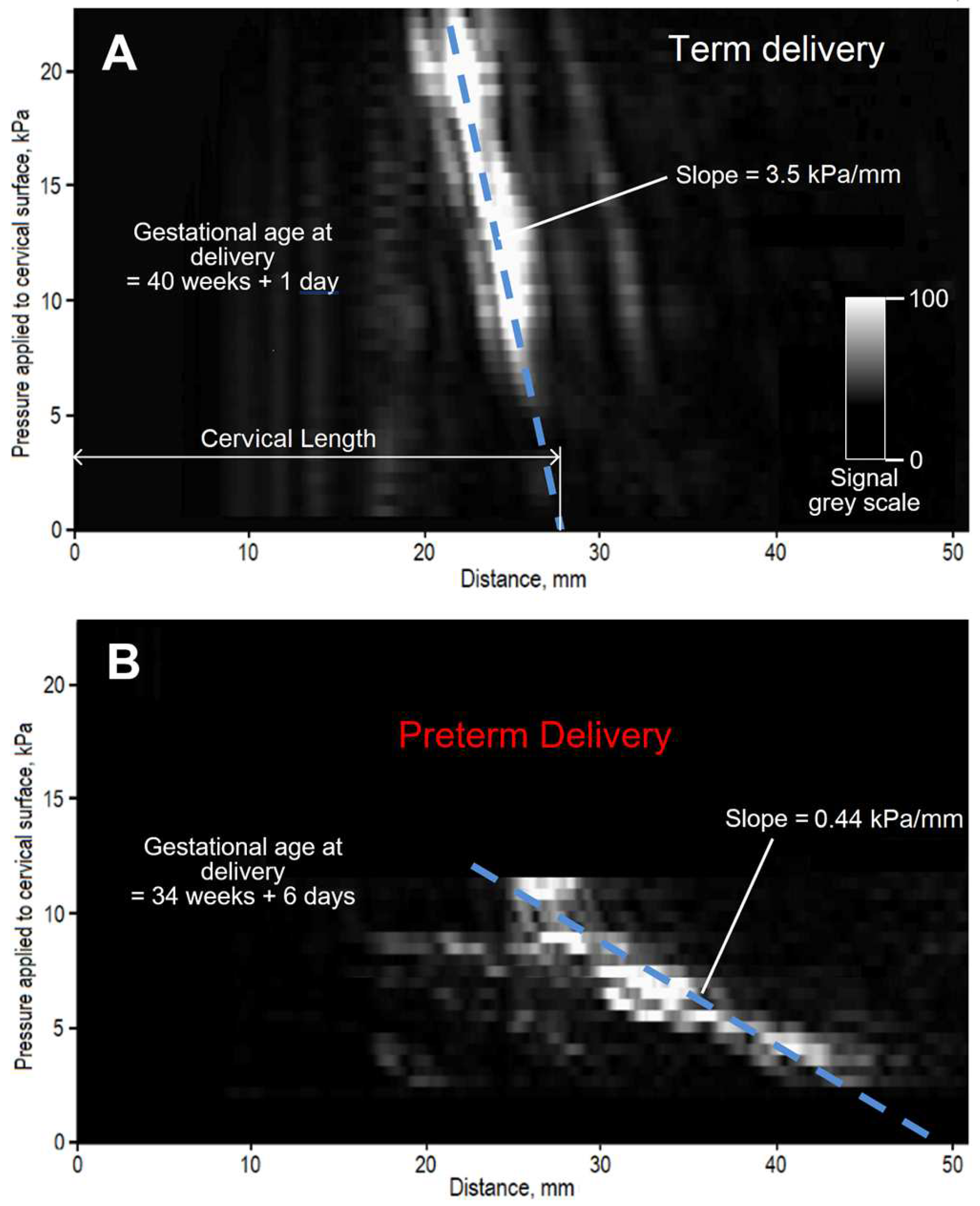
Figure 3 presents two stress-strain cervical maps for two subjects to illustrate the method for calculating the stress-to-strain ratio as a slope. The horizontal axis represents a distance for travel of an ultrasound signals reflected from cervical tissue. The vertical axis displays the pressure value applied to the cervical surface by the CM probe. The amplitude of the reflected ultrasound signals in these maps is presented by a linear grayscale shown in
Figure 3A. The white color in this map corresponds to higher amplitude of the reflected ultrasound signal from internal cervical surface. The slope, marked by the dashed blue line in these cases, is changing from 3.5 kPa/mm in
Figure 3A (term delivery) to 0.44 kPa/mm in
Figure 3B (preterm delivery). Prolongation of the slope line to intersection with the horizontal axis (see
Figure 3A) was used for calculating cervical length in this study.
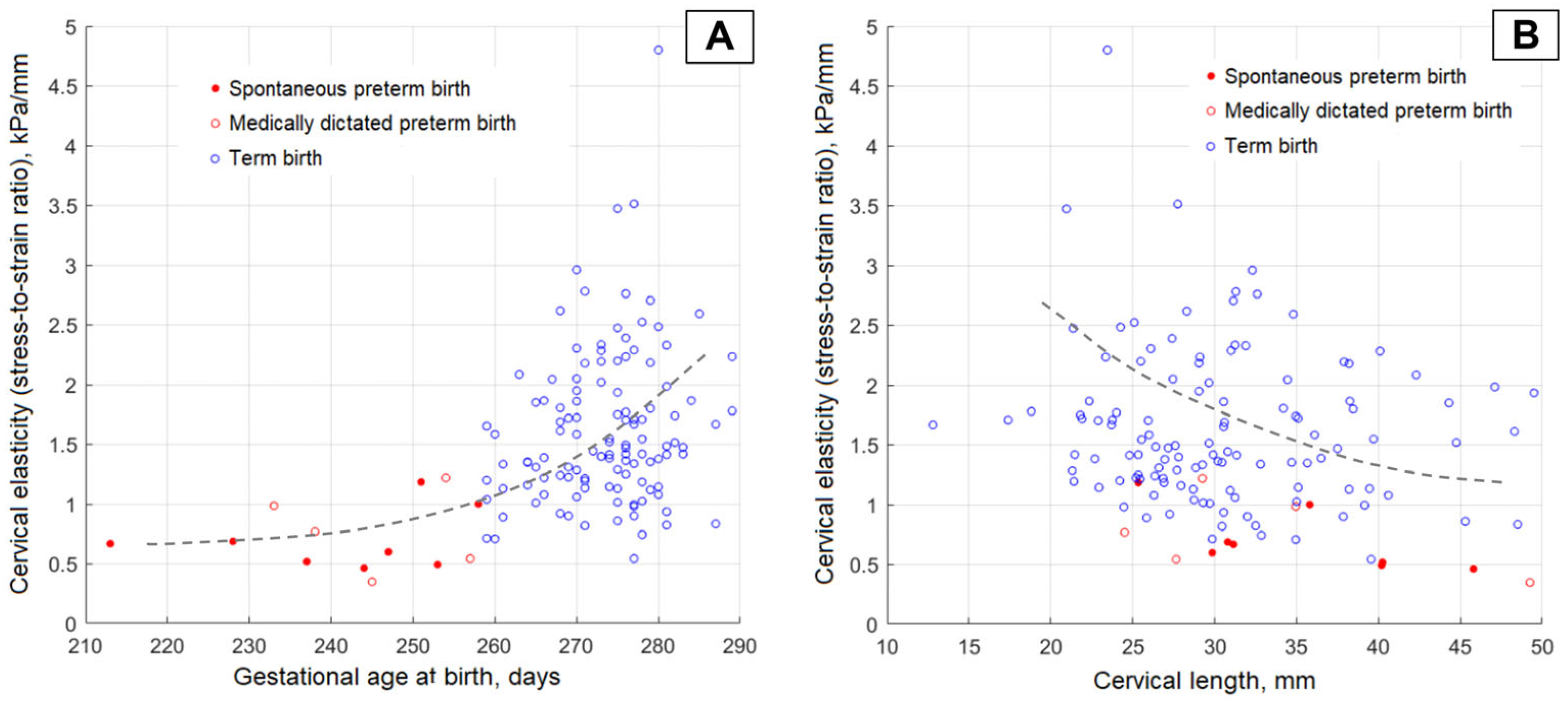
Figure 4A displays the CM-measured cervical elasticity at 24-28 gestational weeks versus gestational age at birth.
Figure 4B shows the CM-measured cervical elasticity versus CM-measured cervical length. The data presentation in
Figure 4B is provided because the tendency of cervical elasticity decrease is observed with an increase in cervical length (see dashed line).
Figure 5 presents the boxplots to compare average cervical elasticity and length for the preterm and term groups. The boxplot in
Figure 5A demonstrates a significant decrease in the preterm group with p = 1.1×10
-4. However, for the cervical length, no statistically significant difference was found (see
Figure 5B) with p = 0.11.
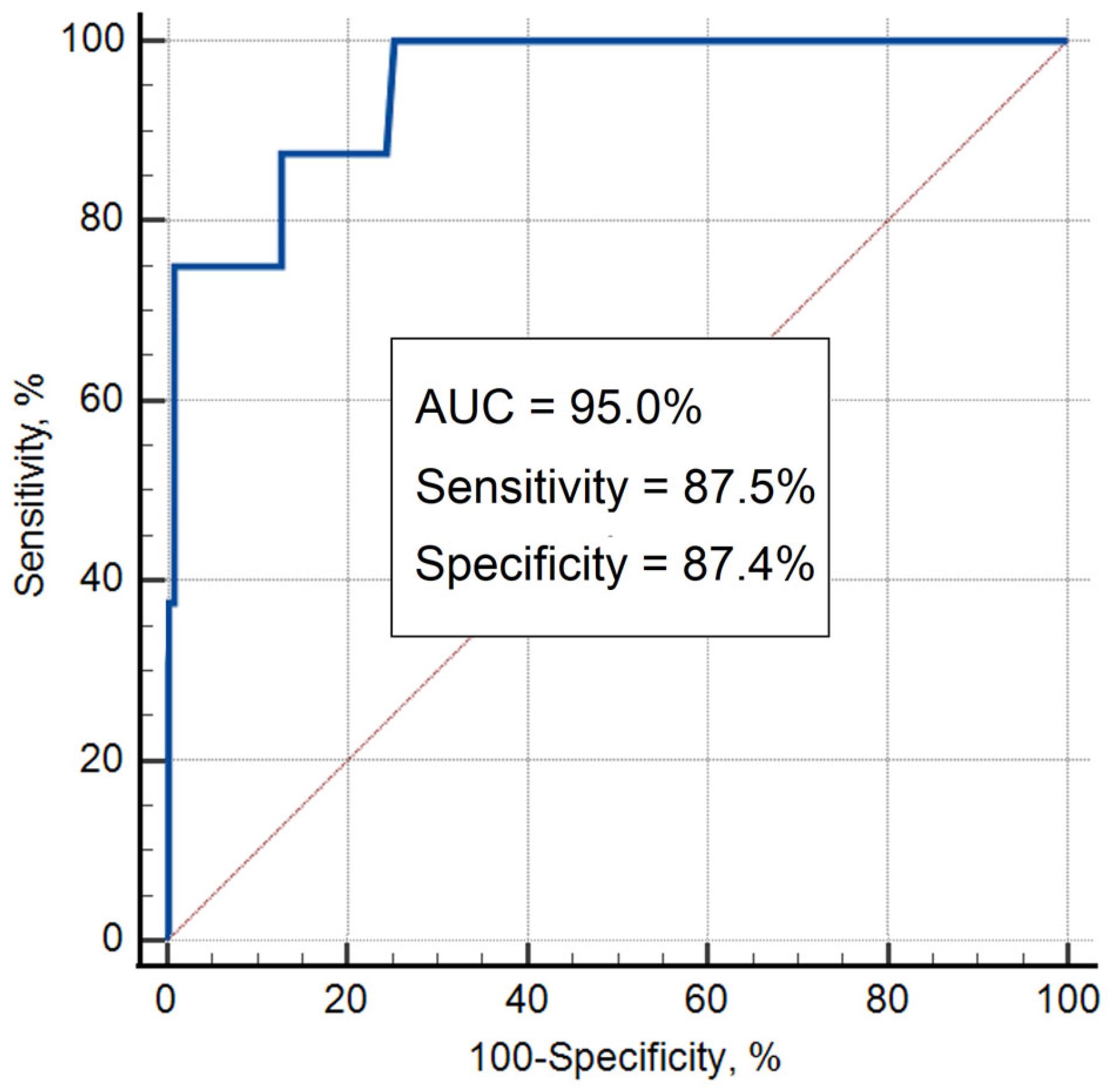
Receiver operating characteristic (ROC) analysis revealed that average cervical elasticity had a sensitivity of 87.5% (95% CI, 47.3–97.7) and a specificity of 87.4% (95% CI, 80.1–92.8) for predicting sPTB at a cutoff value of 1.0 kPa/mm for the cervical stress-to-strain ratio (average for anterior and posterior). The area under the ROC curve (AUC) was 95.0% (95% CI, 88.5–100.0;
p = 1.1×10
-4) for predicting sPTB based solely on cervical elasticity data (stress-to-strain ratio) (
Figure 6).
The maternal comfort level of the CM examination was estimated by 54 women to be more comfortable than the bimanual examination, by 65 women to be the same, and by 8 women to be less comfortable.
4. Discussion
This study on 127 women (8 spontaneous preterm and 119 term births) demonstrated that the tactile ultrasound probe predicts preterm birth at 24-28 gestational weeks with accuracy of 95.0% (95% CI, 88.5–100.0). We found that in our analyzed data sample, the history of preterm birth (PTB) has no effect, as the diagnostic accuracy, calculated as the ROC curve area without cases with history of prior preterm birth, is 93.0% (95% CI, 83.9-100). Additionally, no significant differences were found between parous and nulliparous women, with diagnostic accuracies of 93.9% (95% CI, 81.7-100) and 95.8% (95% CI, 89.3-100), respectively. The fundamental outcome of this research hinges on measuring cervical elasticity, expressed as a stress-to-strain ratio.
Despite the Shapiro-Wilk and Kolmogorov-Smirnov tests for data normality rejected the null hypothesis that the data on cervical elasticity and length are normally distributed, ROC analysis remains acceptable for assessing diagnostic accuracy. This is because ROC analysis is a nonparametric method that does not make assumptions about the distribution of the data [42]. It evaluates the diagnostic performance of a test or a model by plotting the true positive rate (sensitivity) against the false positive rate (1-specificity) across various threshold settings.
No statistically significant difference was found between these preterm and term groups regarding cervical length (
p-value = 0.11). Moreover, a reverse tendency compared to that reported in the literature [
7] is observed. We found an increase in cervical length in the sPTB group as measured with the CM probe (see
Figure 5B). One possible explanation for this increase is that the CM probe's pressure measurement is overly sensitive to initial contact with the cervical surface, whereas the conventional ultrasound probe may easily deform the soft cervix, leading to errors in length measurement. Anyway, the cervical length measurement with this CM probe requires more exploration.
Another interesting finding in this study is that medically dictated birth cases demonstrated decreased cervical elasticity as well as spontaneous preterm birth cases (see five red hollow circles in
Figure 4A). It might be explained by the whole women reproductive system is adjusting to not favorable maternal and/or fetus conditions being prepared to possible preterm birth including cervical softening. No additional mitigating factors, such as age, BMI, or other similar variables, were found to correlate with the observed cervical elasticity in cases of preterm births within the studied group.
We identified 17 published studies with cervical ultrasound which aimed sPTB predictive capabilities. Among them, nine studies used strain elastography (SE) [
15,
17,
18,
19,27,28,31,32,37] and eight shear wave elastography (SWE) [
22,
23,29,30,33–36]. Sixteen of 17 studies showed that cervical elastography could predict preterm birth. One study with 10 preterm cases found no statistically significant differences in cervical elasticity for preterm versus term birth [
22]. Four studies presented results as Odds Ratio (OR) [
15,
23,28,30] ranging from 1.15 to 6.5. In the studies that characterized sensitivity, specificity, and accuracy, these values ranged from 59% to 96.7%, 57.9% to 96.3%, and 63.4% to 98%, respectively. The current study (1) adds to the growing body of data that cervical elasticity is a meaningful predictor of preterm birth, and in fact, may be superior to cervical length measurement by transvaginal ultrasound, which is currently in widespread clinical use, and (2) demonstrates applicability of the cervical stress-to-strain ratio directly measured by the simplified tactile ultrasound probe for predicting spontaneous preterm birth.
Assessments of the maternal serum proteome and transcriptome early in pregnancy have demonstrated that some cases of sPTB result from events that occur well before a woman manifests preterm labor symptoms [38,39]. In the current study, we have shown that changes in cervical elasticity represent another detectable change that occurs before the clinical syndrome of preterm labor manifests. This provides another opportunity to intervene early to prevent preterm birth.
Combining cervical elasticity, which has now been shown to predict preterm birth in multiple prospective studies, with other indicators of preterm birth, may allow for a better assessment of sPTB risk. Preterm labor can be caused by multiple pathological processes [40], yet most women at high risk for sPTB are treated similarly. By assessing a patient’s history, serum protein or RNA markers, and cervical secretions through tests such as fetal fibronectin [41], and considering cervical elasticity, we may develop a more personalized treatment approach to prevent sPTB. This may lead to better success against this important clinical syndrome.
In this study, the cervical stress-strain technique was developed and tested to assess its predictive capability for sPTB. It is evident that larger, multi-center studies are required to validate the CM examination procedures and establish cutoff values for cervical elasticity, preferably using absolute units. An unanswered question is the cervical elasticity distribution along the cervical canal, which has to be investigated in future research. Another question is the translation of the stress-to-strain ratio into the Young's modulus scale. This question is under investigation with finite element modeling and validation with cervical tissue models; it is beyond the scope of this article.
Study strength: Although the study has a relatively small sample size, its strength is demonstrated by the CM technique's capacity to yield a 95% confidence interval of 88.5% - 100.0% for detecting cervical conditions leading to preterm birth. A major advantage of the CM device is that the tactile ultrasound device can be designed as a cost-effective alternative to SE and SWE ultrasound devices, which require high-quality imaging capabilities. The probe could potentially have a disposable intravaginal measuring part costing below $100.
Study weakness: The CM technique allows for the reliable calculation of the cervical stress-to-strain ratio. However, the cervical length measurements with the CM probe may provide overestimated values due to initial cervical deformation with inconsistently low-amplitude ultrasound signals, especially for a softer cervix. The study sample size did not allow exploration of potential racial and ethnic differences in cervical elasticity cutoff for sPTB. Future studies, with larger and diverse populations, are needed to address this issue. Additionally, this reported study does not assess causes of preterm birth by clinical suspicion or placental pathology, which is another limitation and possible perspectives for future research.
5. Conclusions
The designed tactile ultrasound probe provides a novel and cost-effective means for the characterization of cervical elasticity and has the potential to predict preterm birth.
6. Patents
Egorov V. Tactile ultrasound method and probe for predicting spontaneous preterm birth. USA Patent Application No. 18,370,439; September 2023.
Author Contributions
Conceptualization, V.E..; Methodology, V.E.; Software, V.E. and V.K. Electronics, V.K. and V.E.; Clinical data collection/Investigation, T.R., J.H. and M.K.; Formal Analysis, V.E., N.S. and B.F..; Resources, V.E. and N.S.; Data Curation, V.E.; Writing – Original Draft Preparation, V.E.; Writing – Review & Editing, T.R., J.H., M.K., V.K., B.F. and N.S.; Visualization, V.E.; Supervision, V.E.; Project Administration, V.E.; Funding Acquisition, V.E. and N.S.
Funding
This research was funded by research grant HD090793 from Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD), USA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Western IRB (protocol code CM02, date of approval October 31, 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.
Acknowledgments
The authors wish to acknowledge Dr. Jorge E. Tolosa for discussion of the clinical protocol and completion of one CM case at St. Luke's University Health Network, Bethlehem, PA, USA; Shama P. Khan, Research Study Manager at Rutgers Robert Wood Johnson Medical School for effective study coordination; and Alexandr Povar for assembling and testing the CM devices;
Conflicts of Interest
V. Egorov is a minor shareholder of Advanced Tactile Imaging, Inc.; he has submitted a patent application related to the described method and device. N. Sarvazyan is a minor shareholder of Advanced Tactile Imaging, Inc. The other authors declare no conflicts of interest regarding the publication of this article.
References
- Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health 2019; 7: e37–e46. [CrossRef]
- WHO, 2018. Preterm birth. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed 16 March 2023).
- Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016; 388: 3027–35. [CrossRef]
- Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N. Engl. J. Med. 2008; 359(3): 262–73. [CrossRef]
- Conde-Agudelo A, Papageorghiou AT, Kennedy SH, Villar J. Novel biomarkers for the prediction of the spontaneous preterm birth phenotype: a systematic review and meta-analysis. BJOG 2011; 118(9): 1042–54. [CrossRef]
- Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008; 371(9606): 75–84. [CrossRef]
- Hughes K, Ford H, Thangaratinam S, Brennecke S, Mol BW, Wang R. Diagnosis or prognosis? An umbrella review of mid-trimester cervical length and spontaneous preterm birth. BJOG 2023. Epub ahead of print. [CrossRef]
- Yang Q, Fan X, Cao X, Hao W, Lu J, Wei J, Tian J, Yin M, Ge L. Reporting and risk of bias of prediction models based on machine learning methods in preterm birth: A systematic review. Acta Obstet Gynecol Scand. 2023; 102(1): 7-14. [CrossRef]
- Honest H, Forbes CA, Durée KH, et al. 2009. Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling. Health Technol. Assess. 2009; 13: 1–627. [CrossRef]
- American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. Prediction and Prevention of Spontaneous Preterm Birth: ACOG Practice Bulletin, Number 234. Obstet Gynecol. 2021; 138(2): e65-e90. [CrossRef]
- Leow SM, Di Quinzio MKW, Ng ZL, et al. Preterm birth prediction in asymptomatic women at mid-gestation using a panel of novel protein biomarkers: the Prediction of PreTerm Labor (PPeTaL) study. Am J Obstet Gynecol MFM 2020; 2(2): 100084. [CrossRef]
- Swiatkowska-Freund M, Preis K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound Obstet. Gynecol. 2011; 38(1): 52–6. [CrossRef]
- Ophir J, Céspedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason. Imaging 1991; 13(2): 111–34. [CrossRef]
- House M, Feltovich H, Hall TJ, Stack T, Patel A, Socrate S. Three-dimensional, extended field-of-view ultrasound method for estimating large strain mechanical properties of the cervix during pregnancy. Ultrason. Imaging 2012; 34(1): 1–14. [CrossRef]
- Hernandez-Andrade E, Garcia M, Ahn H, Korzeniewski SJ, Saker H, Yeo L, Chaiworapongsa T, Hassan SS, Romero R. Strain at the internal cervical os assessed with quasi-static elastography is associated with the risk of spontaneous preterm delivery at ≤34 weeks of gestation. J. Perinat. Med. 2015; 43(6): 657-66. [CrossRef]
- Wozniak S, Czuczwar P, Szkodziak P, Milart P, Wrona W, Paszkowski T. Elastography in predicting preterm delivery in asymptomatic, low-risk women: a prospective observational study. BMC Pregnancy Childbirth 2014; 14: 238. [CrossRef]
- Köbbing, K, Fruscalzo A, Hammer K, Möllers M, Falkenberg M, Kwiecien R, Klockenbusch W, Schmitz R. Quantitative elastography of the uterine cervix as a predictor of preterm delivery. J Perinatol. 2014; 34(10): 774-80. [CrossRef]
- Sabiani L, Haumonte JB, Loundou A, Caro AS, Brunet J, Cocallemen JF, D'ercole C, Bretelle F. Cervical HI-RTE elastography and pregnancy outcome: a prospective study. Eur J Obstet Gynecol Reprod Biol. 2015; 186: 80-4. [CrossRef]
- Gesthuysen A, Hammer K, Möllers M, Braun J, Oelmeier de Murcia K, Falkenberg MK, Köster HA, Möllmann U, Fruscalzo A, Bormann E, Klockenbusch W, Schmitz R. Evaluation of Cervical Elastography Strain Pattern to Predict Preterm Birth. Ultraschall Med. 2020; 41(4): 397-403. [CrossRef]
- Wang B, Zhang Y, Chen S, Xiang X, Wen J, Yi M, He B, Hu B. Diagnostic accuracy of cervical elastography in predicting preterm delivery: A systematic review and meta-analysis. Medicine (Baltimore) 2019; 98(29): e16449. [CrossRef]
- Helmi H, Siddiqui A, Yan Y, Basij M, Hernandez-Andrade E, Gelovani J, Hsu CD, Hassan SS, Mehrmohammadi M. The role of noninvasive diagnostic imaging in monitoring pregnancy and detecting patients at risk for preterm birth: a review of quantitative approaches. J Matern Fetal Neonatal Med. 2022; 35(3): 568-91. [CrossRef]
- Suthasmalee S, Moungmaithong S. Cervical shear wave elastography as a predictor of preterm delivery during 18-24 weeks of pregnancy. J Obstet Gynaecol Res. 2019; 45(11): 2158-68. [CrossRef]
- Patberg ET, Wells M, Vahanian SA, Zavala J, Bhattacharya S, Richmond D, Akerman M, Demishev M, Kinzler WL, Chavez MR, Vintzileos AM. Use of cervical elastography at 18 to 22 weeks' gestation in the prediction of spontaneous preterm birth. Am J Obstet Gynecol. 2021; 225(5): 525.e1-525.e9. [CrossRef]
- Egorov V, Rosen T, van Raalte H, Kurtenoks V. Cervical characterization with tactile-ultrasound probe. Open Journal of Obstetrics and Gynecology 2020; 10: 85-99. [CrossRef]
- Gradolewski D, Redlarski G. Wavelet-Based Denoising Method for Real Phonocardiography Signal Recorded by Mobile Devices in Noisy Environment. Computers in Biology and Medicine 2014; 52: 119-29. [CrossRef]
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44(3): 837-45. [CrossRef]
- Woźniak, S, Czuczwar P, Szkodziak P, Wrona W, Paszkowski T. Elastography for predicting preterm delivery in patients with short cervical length at 18-22 weeks of gestation: a prospective observational study. Ginekol Pol. 2015; 86(6): 442-7. [CrossRef]
- Oturina V, Hammer K, Möllers M, Braun J, Falkenberg MK, de Murcia KO, Möllmann U, Eveslage M, Fruscalzo A, Klockenbusch W, Schmitz R. Assessment of cervical elastography strain pattern and its association with preterm birth. J Perinat Med. 2017; 45(8): 925-32. [CrossRef]
- Hernandez-Andrade E, Maymon E, Luewan S, Bhatti G, Mehrmohammadi M, Erez O, Pacora P, Done B, Hassan SS, Romero R. A soft cervix, categorized by shear-wave elastography, in women with short or with normal cervical length at 18-24 weeks is associated with a higher prevalence of spontaneous preterm delivery. J Perinat Med. 2018; 46(5): 489-501. [CrossRef]
- Agarwal S, Agarwal A, Joon P, Saraswat S, Chandak S. Fetal adrenal gland biometry and cervical elastography as predictors of preterm birth: A comparative study. Ultrasound 2018; 26(1): 54-62. [CrossRef]
- Jiang L, Peng L, Rong M, Liu X, Pang Q, Li H, Wang Y, Liu Z. Nomogram Incorporating Multimodal Transvaginal Ultrasound Assessment at 20 to 24 Weeks' Gestation for Predicting Spontaneous Preterm Delivery in Low-Risk Women. Int J Womens Health 2022; 14: 323-31. [CrossRef]
- Du L, Zhang LH, Zheng Q, Xie HN, Gu YJ, Lin MF, Wu LH. Evaluation of Cervical Elastography for Prediction of Spontaneous Preterm Birth in Low-Risk Women: A Prospective Study. J Ultrasound Med. 2020; 39(4): 705-13. [CrossRef]
- Jung YJ, Kwon H, Shin J, Park Y, Heo SJ, Park HS, Oh SY, Sung JH, Seol HJ, Kim HM, Seong WJ, Hwang HS, Jung I, Kwon JY. The Feasibility of Cervical Elastography in Predicting Preterm Delivery in Singleton Pregnancy with Short Cervix Following Progesterone Treatment. Int J Environ Res Public Health 2021; 18(): 2026. [CrossRef]
- Sun J, Li N, Jian W, Cao D, Yang J, Chen M. Clinical application of cervical shear wave elastography in predicting the risk of preterm delivery in DCDA twin pregnancy. BMC Pregnancy Childbirth 2022; 22(1): 202. [CrossRef]
- Feng Q, Chaemsaithong P, Duan H, Ju X, Appiah K, Shen L, Wang X, Tai Y, Leung TY, Poon LC. Screening for spontaneous preterm birth by cervical length and shear-wave elastography in the first trimester of pregnancy. Am J Obstet Gynecol. 2022; 227(3): 500.e1-500.e14. [CrossRef]
- Yang X, Ding Y, Mei J, Xiong W, Wang J, Huang Z, Li R. Second-trimester cervical shear wave elastography combined with cervical length for the prediction of spontaneous preterm birth. Ultrasound Med Biol. 2022; 48(5): 820-29. [CrossRef]
- Abdallah M, Mostafa A, Gaafar I, Hegazy A. Value of cervical strain in ultrasound elastography as a predictor of spontaneous preterm delivery. Egyptian Journal of Radiology and Nuclear Medicine 2023; 54: 39. [CrossRef]
- Saade GR, Boggess KA, Sullivan SA, et al. Development and validation of a spontaneous preterm delivery predictor in asymptomatic women. Am J Obstet Gynecol. May 2016; 214(5): 633 e1-633.e24. [CrossRef]
- Camunas-Soler J, Gee EPS, Reddy M, et al. Predictive RNA profiles for early and very early spontaneous preterm birth. Am J Obstet Gynecol. 2022; 227(1): 72 e1-72.e16. [CrossRef]
- Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science. Aug 15 2014; 345(6198): 760-5. [CrossRef]
- Lockwood CJ, Senyei AE, Dische MR, et al. Fetal fibronectin in cervical and vaginal secretions as a predictor of preterm delivery. N Engl J Med. 1991; 325(10): 669-74. [CrossRef]
- Hajian-Tilaki KO, Hanley JA, Joseph L, Collet JP. A comparison of parametric and nonparametric approaches to ROC analysis of quantitative diagnostic tests. Med Decis Making 1997; 17(1): 94-102. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).