Submitted:
04 January 2024
Posted:
04 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Rehabilitation program
2.3. Physical therapy for the control group
2.4. GBE
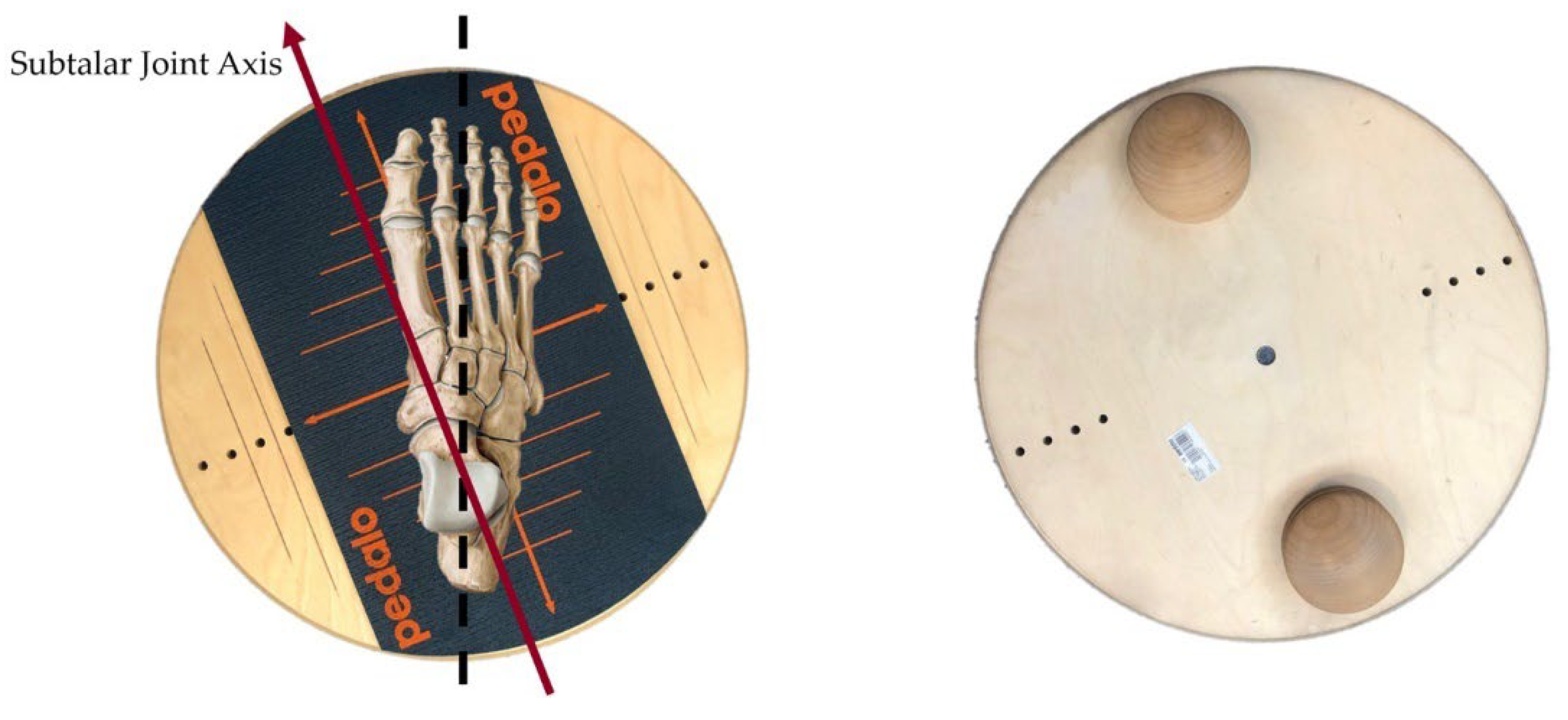
2.5. SBE
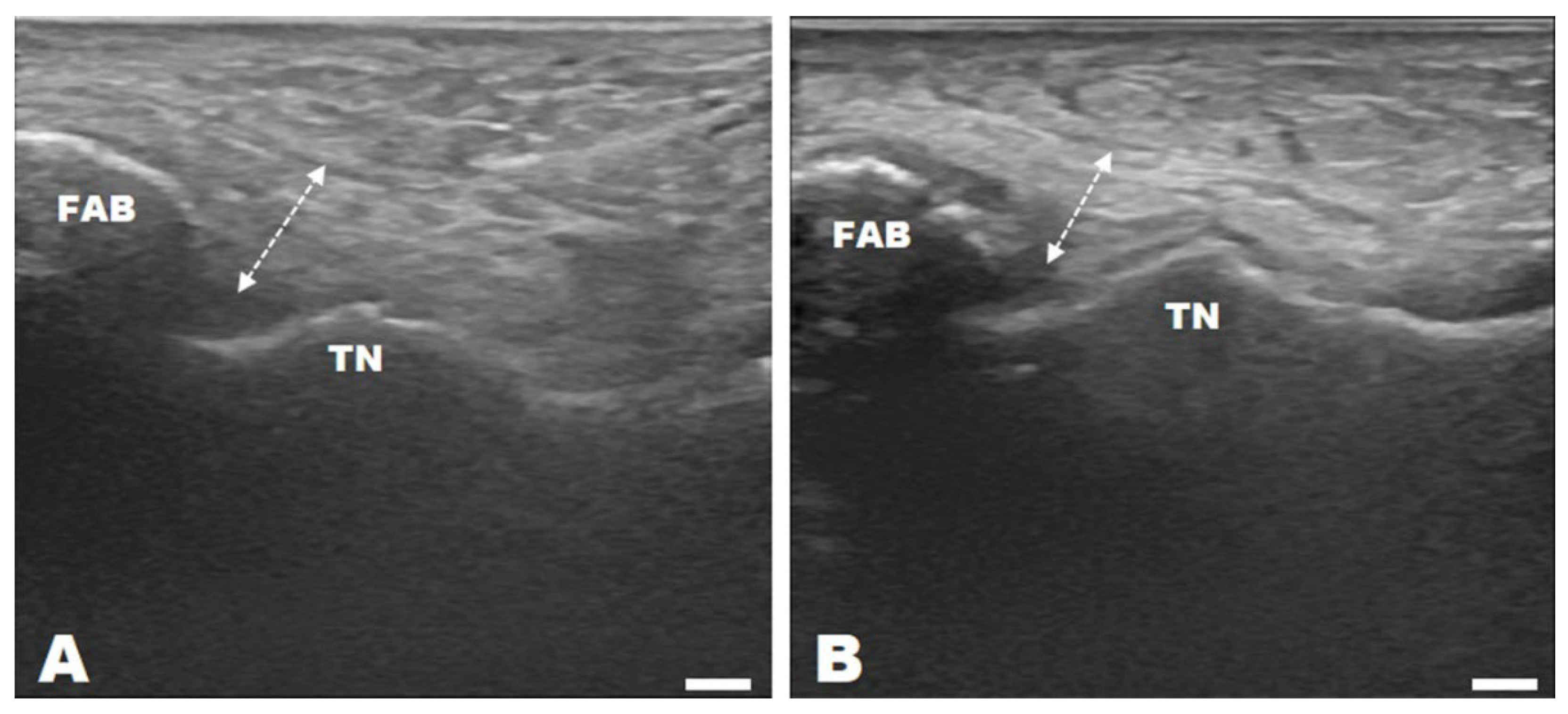
2.6. Ultrasonography
2.7. Isokinetic muscle functions
2.8. Dynamic stability
2.9. Statistical analysis
3. Results
3.1. Change in ultrasonography results of ATFL thickness
3.2. Changes in isokinetic muscle strength power
3.3. Changes in dynamic stability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Michell, T.B.; Ross, S.E.; Blackburn, J.T.; Hirth, C.J.; Guskiewicz, K.M. Functional balance training, with or without exercise sandals, for subjects with stable or unstable ankles. J. Athl Train. 2006, 41, 393–398. [Google Scholar]
- Feng, Y.; Ma, J.H.; Xiao, H.J.; Ao, R.G.; Zhang, F.G.; Li, W.C.; Wang, W.; Zeng, P.; Lu, T.; Revel, F.B.; et al. Randomized, double-blind, noninferiority study of diclofenac diethylamine 2.32% gel applied twice daily versus diclofenac diethylamine 1.16% gel applied four times daily in patients with acute ankle sprain. BMC. Musculoskeletal Disorders. 2022, 23, 1125–1135. [Google Scholar]
- Croy, T.; Saliba, S.; Saliba, E.; Anderson, M.W.; Hertel, J. Talofibular interval changes after acute ankle sprain: a stress ultrasonography study of ankle laxity. J. Sport Rehabil. 2013, 22, 257–263. [Google Scholar] [CrossRef]
- Renstrom, P.A.; Konradsen, L. Ankle ligament injuries. Br. J. Sports Med. 1997, 31, 11–20. [Google Scholar] [CrossRef]
- Kudo, S.; Aoyagi, T.; Kobayashi, T.; Koshino, Y.; Edama, M. Ultrasound imaging of subtalar joint instability for chronic ankle instability. Healthcare (Basel). 2023, 11, 2227–2237. [Google Scholar] [CrossRef]
- Fong, D.T.; Ha, S.C.; Mok, K.M.; Chan, C.W.; Chan, K.M. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: Five cases from televised tennis competitions. Am. J. Sports Med. 2012, 40, 2627–2632. [Google Scholar] [CrossRef]
- Michell, T.B.; Ross, S.E.; Blackburn, J.T.; Hirth, C.J.; Guskiewicz, K.M. Functional balance training, with or without exercise sandals, for subjects with stable or unstable ankles. J. Athl Train. 2006, 41, 393–398. [Google Scholar]
- Health insurance review & assessment service. HIRA bigdata open portal. The number of patients who visited the hospital for ankle sprains. Available online: https://opendata.hira.or.kr/op/opc/olap3thDsInfoTab3.do (accessed on 16 January 2023).
- Karlsson, J.; Lansinger, O. Lateral instability of the ankles joint. Clin Orthop. Relat Res. 1992, 276, 253–261. [Google Scholar] [CrossRef]
- Peter, J.W.; Trevvino, S.G.; Renstrom, P.A. Chronic lateral ankle instability. Foot Ankle. 1991, 12, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Wenning, M.; Gehring, D.; Mauch, M.; Schmal, H.; Ritzmann, R.; Paul, J. Functional deficits in chronic mechanical ankle instability. J. Orthop Surg. Res. 2020, 15, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Takao, M.; Matsui, K.; Stone, J.W.; Glazebrook, M.A.; Kennedy, J.G.; Guillo, S.; Calder, J.D.; Katlsson, J. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1003–1006. [Google Scholar] [CrossRef]
- Odak, S.; Ahluwalia, R.; Shivarathre, D.G.; Mahmood, A.; Blucher, N.; Hennessy, M.; Platt, S. Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot Ankle Int. 2015, 36, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.S.; Kirby, K.A.; Piazza, S.J. Determination of subtalar joint axis location by restriction of talocrural joint motion. Gait Posture. 2007, 25, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Baumhauer, J.F.; O’Brien, T. Surgical considerations in the treatment of ankle Instability. J. Athl Train. 2002, 37, 458–462. [Google Scholar] [PubMed]
- Vega, J.; Guelfi, M.; Malagelada, F.; 0Peña, F.; Dalmau-Pastor, M. Arthroscopic all-inside anterior talofibular ligament repair through a three-portal and no-ankle-distraction technique. JBJS. Essent Surg Tech. 2018, 8, e25–36. [Google Scholar] [CrossRef] [PubMed]
- Akinobu, N.; Shigeto, N.; Yoshiyuki, S.; Yukie, K.; Aki, F.; Ko, K.; Akihiro, S. Arthroscopic internal brace augmentation with arthroscopic modified Broström operation for chronic ankle instability. Arthrosc. Tech. 2021, 10, 995–1000. [Google Scholar]
- Kim, E.S.; Lee, K.T.; Park, J.S.; Lee, Y.K. Arthroscopic anterior talofibular ligament repair for chronic ankle instability with a suture anchor technique. Orthopedics. 2011, 34, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Moritz, M.; Ulf, K.H.; Ingmar, I. Arthroscopic modified Broström operation versus open reconstruction with local periosteal flap in chronic ankle instability. Arch. Orthop. Trauma Surg. 2022, 142, 3581–3588. [Google Scholar]
- Lee, K.T.; Kim, E.S.; Kim, Y.H.; Ryu, J.S.; Rhyu, I.J.; Lee, Y.K. All-inside arthroscopic modified Broström operation for chronic ankle instability: a biomechanical study. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1096–1100. [Google Scholar] [CrossRef]
- Gould, N.; Seligson, D.; Gassman, J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980, 1, 84–89. [Google Scholar] [CrossRef]
- Braun, B.L. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch. Fam Med. 1999, 8, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Mangwani, J.; Hakmi, M.A.; Smith, T.W.D. Chronic lateral ankle instability: Review of anatomy, biomechanics, pathology, diagnosis and treatment. Foot. 2001, 11, 76–84. [Google Scholar] [CrossRef]
- O’Sullivan, S.B.; Schmitz, T.J.; Fulk, G.D. Physical rehabilitation: Assessment and treatment, 7rd ed.; F.A. Davis Company: Philadelphia, PA, USA, 2019; pp. 147–149. [Google Scholar]
- Kirby, K.A. Lecithin in mania: A preliminary report. Am. J. Psychiatry. 2006, 96, 212–219. [Google Scholar]
- Nairn, B.C.; Sutherland, C.A.; Drake, J.D. Motion and muscle activity are affected by instability location during a squat exercise. J. Strength. Cond. Res. 2017, 31, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Brotzman, S.B.; Wilk, k. E. Clinical or thopaedic rehabilitation, 2nd ed.; Mosby: Philadelphia, PA, USA, 2003; pp. 391–392. [Google Scholar]
- Zhu, Y.; Feng, Y.; Peng, L. Effect of transcutaneous electrical nerve stimulation for pain control after total knee arthroplasty: A systematic review and meta-analysis. J. Rehabil Med. 2017, 49, 700–704. [Google Scholar] [CrossRef] [PubMed]
- Kathy, L.; Geoff, G.; Todd, R.; Erik, A.W.; Joseph, G.; Thomas, W.K. Increased ligament thickness in previously sprained ankles as measured by musculoskeletal ultrasound. J. Athl Train. 2015, 50, 193–198. [Google Scholar]
- Park, J.H.; Rhyu, H.S.; Rhi, S.Y. The effects of instrument-assisted soft tissue mobilization rehabilitation exercise on range of motion, isokinetic strength, and balance in chronic ankle instability taekwondo players. J. Exerc Rehabil. 2020, 16, 516–521. [Google Scholar] [CrossRef]
- Plisky, P.J.; Grman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The reliability of an instrumented device for measuring components of the star excursion balance test. N. Am. J. Sports Phys. Ther. 2009, 4, 92–99. [Google Scholar]
- Linek, P.; Sikora, D.; Wolny, T.; Saulicz, E. Reliability and number of trials of Y balance test in adolescent athletes. Musculoskelet Sci. Pract. 2017, 31, 72–75. [Google Scholar] [CrossRef]
- Kim, J.G.; Lee, D.W.; Bae, K.C.; Choi, B.C.; Yang, S.J.; Cho, S.I.; Kim, D.H. Correlation of Y Balance with clinical scores and functional tests after anterior cruciate ligament reconstruction in young and middle-aged patients. Clin. Orthop. Surg. 2023, 15, 50–58. [Google Scholar] [CrossRef]
- Peng, L.; Yu, L.; Jia, J.; Gan, Y.; Ding, A.; Xiong, P.; Zhao, Y.; Yao, Y. The effect of thickness and elastic modulus of the anterior talofibular ligament on anterior ankle joint stiffness: A subject-specific finite element study. Front. Bioeng. Biotechnol. 2023, 11, 1175347. [Google Scholar] [CrossRef]
- Gulotta, L.V.; Rodeo, S.A. Growth factors for rotator cuff repair. Am. J, Sports Med. 2009, 28, 2126–2133. [Google Scholar] [CrossRef]
- Nikolaidou, O.; Migkou, S.; Karampalis, C. Rehabilitation after rotator cuff repair. Open. Orthop. J. 2017, 28, 154–162. [Google Scholar] [CrossRef]
- Liu, K.; Gustavsen, G.; Royer, T.; Wikstrom, E.A.; Glutting, J.; Kaminski, T.W. Increased ligament thickness in previously sprained ankles as measured by musculoskeletal ultrasound. J. Athl Train. 2015, 50, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Hua, Y.H.; Yang, Y.; Chen, S.Y.; Cai, Y.H. Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta. Radiol. 2012, 53, 1142–1145. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Kim, T.H.; Lee, M.G.; Park, Y.G. Absence of ATFL remnant does not affect the clinical outcomes of the modified broström operation for chronic ankle instability. Knee surg. Sports Traumatol. Artrosc. 2020, 28, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Tuecking, L.R.; Erdle, B.; Bernstein, A.; Ogon, P.; Jaeger, M.; Südkamp, N.P.; Izadpanah, K.; Maier, D. Ligamentous healing potential of the acromioclavicular ligament following acute anatomical reconstruction. Arch. Orthop. Trauma Surg. 2022, 142, 2225–2234. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.C.; Miao, X.; Ao, Y.F.; Hu, Y.L.; Jiao, C.; Guo, Q.W.; Xie, X.; Zhao, F.; Pi, Y.B.; Li, N.; et al. Characteristics and predictors of muscle strength deficit in mechanical ankle instability. BMC. Musculoskeletal Disorders. 2020, 21, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Terada, M.; Pietrosimone, B.G.; Gribble, P.A. Therapeutic interventions for increasing ankle dorsiflexion after ankle sprain: a systematic review. J. Athl Train. 2013, 48, 696–709. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A.; Delahunt, E. Treatment of common deficits associated with chronic ankle instability. Sports Med. 2009, 39, 207–224. [Google Scholar] [CrossRef] [PubMed]
- Krähenbühl, N.; Horn-Lang, T.; Hintermann, B.; Knupp, M. The subtalar joint a complex mechanism. FORT. Open Rev. 2017, 2, 309–316. [Google Scholar] [CrossRef]
- Ferran, N.A.; Maffulli, N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle. Clin. 2006, 11, 659–662. [Google Scholar] [CrossRef]
- Jimenez-Reyes, P.; Samozino, P.; Morin, J.B. Optimized training for jumping performance using the force-velocity imbalance: Individual adaptation kinetics. PLoS. One 2019, 14, e0216681. [Google Scholar] [CrossRef]
- Triantafyllopoulos, I.K.; Economopoulos, D.G.; Panagopoulos, A.; Niekerk, L. Chronic lateral ankle instability in highly active patients: A treatment algorithm based on the arthroscopic assessment of the calcaneofibular Ligament. Cureus. 2021, 13, e14310. [Google Scholar] [CrossRef] [PubMed]
- Dekerle, J.; Barstow, T.J.; Regan, L.; Carter, H. The critical power concept in all-out isokinetic exercise. J. Sci. Med. Sport. 2014, 17, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P. Isokinetic evaluation of muscular performance: implications for muscle testing and rehabilitation. Int. J. Sports. Med. 1994, 15, S11–18. [Google Scholar] [CrossRef] [PubMed]
- Arnold, B.L.; Linens, S.W.; Motte, S.J.; Ross, S.E. Concentric evertor strength differences and functional ankle instability: a meta-analysis. J. Athl Train. 2009, 44, 653–662. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.D.; Woollacott, M.H.; Jensen, J.L. Age-related changes in rate and magnitude of ankle torque development: Implications for balance control. J. Gerontol. A. Biol. Sci. Med. Sci. 1999, 54, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Hess, J.A.; Woollacott, M.; Shivitz, N. Ankle force and rate of force production increase following high intensity strength training in frail older adults. Aging. Clin. Exp. Res. 2006, 18, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Lu, J.; Cai, B.; Fan, S.; Jiang, X. Quantitative assessments of static and dynamic balance performance in patients with chronic ankle instability. Medicine (Baltimore) 2020, 99, e19775. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, S.H.; Choi, G.W.; H., W.; Jung, H.W.; Jang, W.Y. Individuals with recurrent ankle sprain demonstrate postural instability and neuromuscular control deficits in unaffected side. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 184–192. [Google Scholar] [CrossRef]
- Cain, M.S.; Garceau, S.W.; Linens, S.W. Effects of a 4-week biomechanical ankle platform system protocol on balance in high school athletes with chronic ankle instability. J. Sport Rehabil. 2017, 26, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Park, S.H.; Kim, S.H.; Choi, G.W.; Kim, H.J. Relationship between isokinetic muscle strength and functional tests in chronic ankle instability. J. Foot. Ankle. Surg. 2019, 58, 1187–1191. [Google Scholar] [CrossRef] [PubMed]
- Choisne, J.; Ringleb, S.I.; Samaan, M.A.; Bawab, S.Y.; Naik, D.; Anderson, C.D. Influence of kinematic analysis methods on detecting ankle and subtalar joint instability. J. Biomech. 2012, 45, 46–52. [Google Scholar] [CrossRef]
- Plisky, P.; Schwartkopf-Phifer, K.; Huebner, B.; Garner, M.B.; Bullock, G. Systematic review and meta-analysis of the Y-Balance test lower quarter: Reliability, discriminant validity, and predictive validity. Int. J. Sports Phys Ther. 2021, 16, 1190–1209. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Iqbal, Z.A.; Iqbal, A.; Ahmed, H.; Ramteke, S.U. Effect of chronic ankle sprain on pain, range of motion, proprioception, and balance among athletes. Int. J. Environ Res. Public Health 2020, 17, 5318. [Google Scholar] [CrossRef] [PubMed]
- Mattacola, C.G.; Dwyer, M.K. Rehabilitation of the ankle after acute sprain or chronic instability. J. Athl Train. 2002, 37, 413–429. [Google Scholar] [PubMed]
- Linens, S.W.; Ross, S.E.; Arnold, B.L. Wobble board rehabilitation for improving balance in ankles with chronic instability. Clin. J. Sport Med. 2016, 26, 76–82. [Google Scholar] [CrossRef]
- Bernier, J.N.; Perrin, D.H. Effect of coordination training on proprioception of the functionally unstable ankle. J. Orthop. Sports Phys Ther. 1998, 27, 264–75. [Google Scholar] [CrossRef]
- Anguish, B.; Sandrey, M.A. Two 4-week balance-training programs for chronic ankle instability. J. Athl Train. 2018, 53, 662–671. [Google Scholar] [CrossRef]
| Sex | Involved | Age (years) | Height (cm) | Weight (kg) | BMI (kg/m2) | |||
|---|---|---|---|---|---|---|---|---|
| M | F | Rt | Lt | |||||
| CON (n=11) | 5 | 6 | 3 | 8 | 34 ± 14.76 | 169.55 ± 9.05 | 76.55 ± 21.76 | 26.34 ± 5.97 |
| GBE (n=17) | 8 | 9 | 5 | 12 | 28.53 ± 10.93 | 171 ± 10.20 | 67.82 ± 16.67 | 23.01 ± 4.44 |
| SBE (n=19) | 5 | 14 | 9 | 10 | 28.53 ± 9.75 | 165.16 ± 8.62 | 62.79 ± 12.78 | 22.83 ± 3 |
| Index | Exercise | Intensity | Side | |
|---|---|---|---|---|
| Warm up |
Flexibility | Begin gentle ROM exercises of the ankle (DF, PF, IV, EV) |
4–6 weeks (5 s x 10 reps) × 3 sets |
Involved |
| Intensive muscle exercise |
Isometric | Ankle towel isometric exercise (DF, PF, IV, EV) |
4–5 weeks (5 s x 10 reps) × 3 sets |
Involved |
| Isotonic | Towel pulling with toe Ankle tubing exercise (DF, PF, IV, EV) |
5–6 weeks (5 s x 10 reps) × 3 sets |
Involved | |
| Toe raise Calf raise |
5–6 weeks (5 s x 10 reps) × 3 sets |
Both | ||
| Functional | Squat Lunge Side lunge Single step up (box) |
6–12 weeks (5 s x 10 reps) × 3 sets |
Both | |
| Jump (jump: pain free jump in place) Hop (hop: one leg-jump hop) |
6–12 weeks 10 reps × 3 sets |
|||
| Running | 10–12 weeks 30 min | |||
| Static balance |
Single standing HF Single standing HF and SF (DB, BB) |
6–12 weeks (5 s x 10 reps) × 3 sets |
Both | |
| Dynamic balance | Single squat (DB, BB) Single Y-squat (DB, BB) |
8–12 weeks 10reps × 3 sets |
||
| Cool down |
Stretching | Foam roller | 10 min | Both |
| Pre | Post | Paired t-test | Two-way RM ANOVA | |||||
|---|---|---|---|---|---|---|---|---|
| t-value | p-value | F | p | |||||
| ATFL thickness via ultrasonography | CON (n=11) | 8.57 ± 1.99 a | 7.82 ± 2.11 a | 3.112 | 0.011* | G | 0.692 | 0.506 |
| GBE (n=17) | 8.77 ± 1.88 a | 7.26 ± 1.88 a | 8.239 | 0.000*** | T | 109.649 | 0.000*** | |
| SBE (n=19) | 8.99 ± 2.10 a | 5.94 ± 1.52 b | 8.877 | 0.000*** | G×T | 16.556 | 0.000*** | |
| Pre | Post | Paired t-test | Two-way RM ANOVA | |||||
|---|---|---|---|---|---|---|---|---|
| t-value | p-value | F | p | |||||
| EV | CON (n=11) | 12.31 ± 4.76 a | 13.92 ± 5.11 a | –1.431 | 0.183 | G | 0.445 | 0.644 |
| GBE (n=17) | 11.54 ± 5.75 a | 15.64 ± 6.87 a | –3.579 | 0.003** | T | 43.685 | 0.000*** | |
| SBE (n=19) | 9.99 ± 5.59 a | 19.44 ± 4.22 b | –6.867 | 0.000*** | G×T | 9.508 | 0.000*** | |
| IV | CON (n=11) | 11.81 ± 6.27 a | 15.65 ± 7.26 a | –1.882 | 0.089 | G | 0.873 | 0.425 |
| GBE (n=17) | 13.69 ± 8.34 a | 18.44 ± 9.43 a | –3.895 | 0.001** | T | 62.930 | 0.000*** | |
| SBE (n=19) | 10.69 ± 7.89 a | 24.51 ± 9.29 b | –8.652 | 0.000*** | G×T | 12.815 | 0.000*** | |
| Pre | Post | Paired t-test | Two-way RM ANOVA | |||||
|---|---|---|---|---|---|---|---|---|
| t-value | p-value | F | p | |||||
| Dynamic stability | CON (n=11) | 82.35 ± 6.9 a | 87.15 ± 7.43 a | –2.573 | 0.028* | G | 2.624 | 0.084 |
| GBE (n=17) | 77.79 ± 10.32 a | 89.25 ± 5.59 a | –5.922 | 0.000*** | T | 59.831 | 0.000*** | |
| SBE (n=19) | 79.92 ± 11.35 a | 96.95 ± 4.52 b | –6.146 | 0.000*** | G×T | 5.762 | 0.006** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





