1. Introduction
Malnutrition is one of the most feared long-term complications of bariatric surgery. It has been historically related to malabsorptive operations, as jejunoileal bypass (JIB), biliopancreatic diversion (BPD) and duodenal switch (DS), although patients submitted to less aggressive techniques can also present some degrees of malnutrition. Single-Anastomosis Duodeno-Ileal bypass with Sleeve Gastrectomy (SADI-S) was introduced as a simpler alternative to the Duodenal Switch (DS) in which malabsorption was supposed to be milder because of the increase in the length of the common channel (1). However, a high rate of nutritional problems presented in the first series of patients in which the common limb measured 200 cm. This led us to elongate the absorptive channel (250 to 300 cm) to ameliorate the malabsorptive effect of the operation (2). The new longer common channel still showed good weight loss results in the long-term, whereas there was a reduction in the nutritional issues (3, 4). Despite this greater absorption, some patients still present with hypoalbuminemia and other deficiencies (5), perhaps secondarily to a wrong selection, errors in the limb measurement or poor adherence to diet and supplementation. The management of malnourished patients can be difficult, and many times involves the revision of the technique. This seems to be easier in a one-limb operation when compared to Roux en Y configuration, but still the handling of a duodeno-intestinal anastomosis can be a concern for many surgeons.
In the present study, we review our experience on malnutrition after SADI-S and analyze the possible causes for this malnutrition, the markers that permit an early detection of these patients to avoid dreadful consequences, the current surgical solutions to improve their nutritional status and the outcomes after revisional surgery.
2. Materials and Methods
From May 2007 to September 2017, 258 consecutive patients were submitted to SADI-S, either as a one step surgery (213 cases) or as a second surgery after a previous sleeve gastrectomy (45 patients). The study was limited to patients operated before 2018 to warrant at least a 5 year follow up. The common limb was 200 cm in 50 cases, 250 cm in 156 cases and 300 cm in 52. Indications for SADI-S, surgical technique, supplementation and follow up have been reported previously (5). Thirty patients (11,6%) were admitted for severe malnutrition. This was defined as low albumin levels plus edema, in the absence of an inflammation status, and not amenable for ambulatory management. Sixteen patients were submitted to revisional surgery (6,2%), and constitute the series of our study (
Figure 1, Flow Chart).
Two surgeons (ASP and AJT) performed all the operations, both primary and revisional.Interventionary studies involving animals or humans, and other studies that require ethical approval, must list the authority that provided approval and the corresponding ethical approval code.
Statistics
Data are expressed by mean, range and standard error of the mean. Comparisons between the study series and the total SADI-S series are done with the t-test and chi-square test for numerical and categorical variables respectively.
3. Results
Follow up for the whole series was 85% at 5 years. Sixteen patients (6,2%) were reoperated. The incidence density was 0,6 cases per 100 patients-year. They were 6 men and 10 women, with a mean age at the index operation of 51 years (35 to 68), a mean initial weight of 118 kg (87 to 180), and a mean initial body mass index (BMI) of 44 kg/m2 (38 - 54). Type 2 diabetes was present in 10 patients (62%), 3 were under oral therapy and 7 under insulin treatment; 14 patients had hypertension (87%), 11 had dyslipidemia (69%), and 9 had sleep apnea (56%). One patient had been submitted to a previous bariatric operation, a sleeve gastrectomy. SADI-S had been performed with a 2 meter common limb in 8 cases (8/50, 16% malnutrition rate for SADI-S 200), and with a 250 cm common limb in the other 8 patients (8/156, 5,1% malnutrition rate for SADI-S 250). No one had undergone SADI-S with a 3 meter common limb.
3.1. Presentation
The mean time to first admission was 37 months, 2 months being the earliest one and 180 months the latest one. The mean number of hospital admissions before revision was 2,6 (0 - 5). Seven patients (43%) had the first episode requiring hospital admission in the first postoperative year, while 4 of them (25%) presented with malnutrition more than 5 years from surgery.
The mean time to reoperation was 56 months, from 16 to 186 months; 50% of the patients were reoperated in the first 3 postoperative years, and 37% of them beyond the 5th postoperative year.
Indication for reopeation was individualized, and different parameters influenced this decision, as were age, severity of the episode, psychiatric evaluation, social status, number of episodes, coexisting diseases, etc. The main cause for reoperation was severe malnutrition in most cases (11 patients), but also intractable diarrhea was present in some patients (4 cases); there was one patient with severe hypocalcemia and 3 had developed liver failure, two secondary to alcohol consumption and one to viral hepatitis and cirrhosis (
Table 1).
Mean age at reoperation was 55 years (32 - 71), mean weight 57 kg (46 - 74), mean BMI 21 kg/m2 (18,6 - 27) and mean total weight loss (TWL) 50,2% (32,7 - 68). All patients were nutritionally optimized to achieve normal albumin and total protein levels, in 7 cases with the need of total parenteral nutrition. The mean number of daily bowel movements was 5,6 (2 - 10).
3.2. Surgical findings
The common limb was measured in all cases. In patients with an initial SADI-S 200, in 6 cases, the measured length was 2 meters; in 1 patient the limb was shorter, 170 cm, and in another one it was longer, 250 cm. In patients submitted to SADI-S 250, we found a correct common limb length in 4 cases, and a shorter one in the other 4 (220, 200, 190 and 150 cm) (
Table 1).
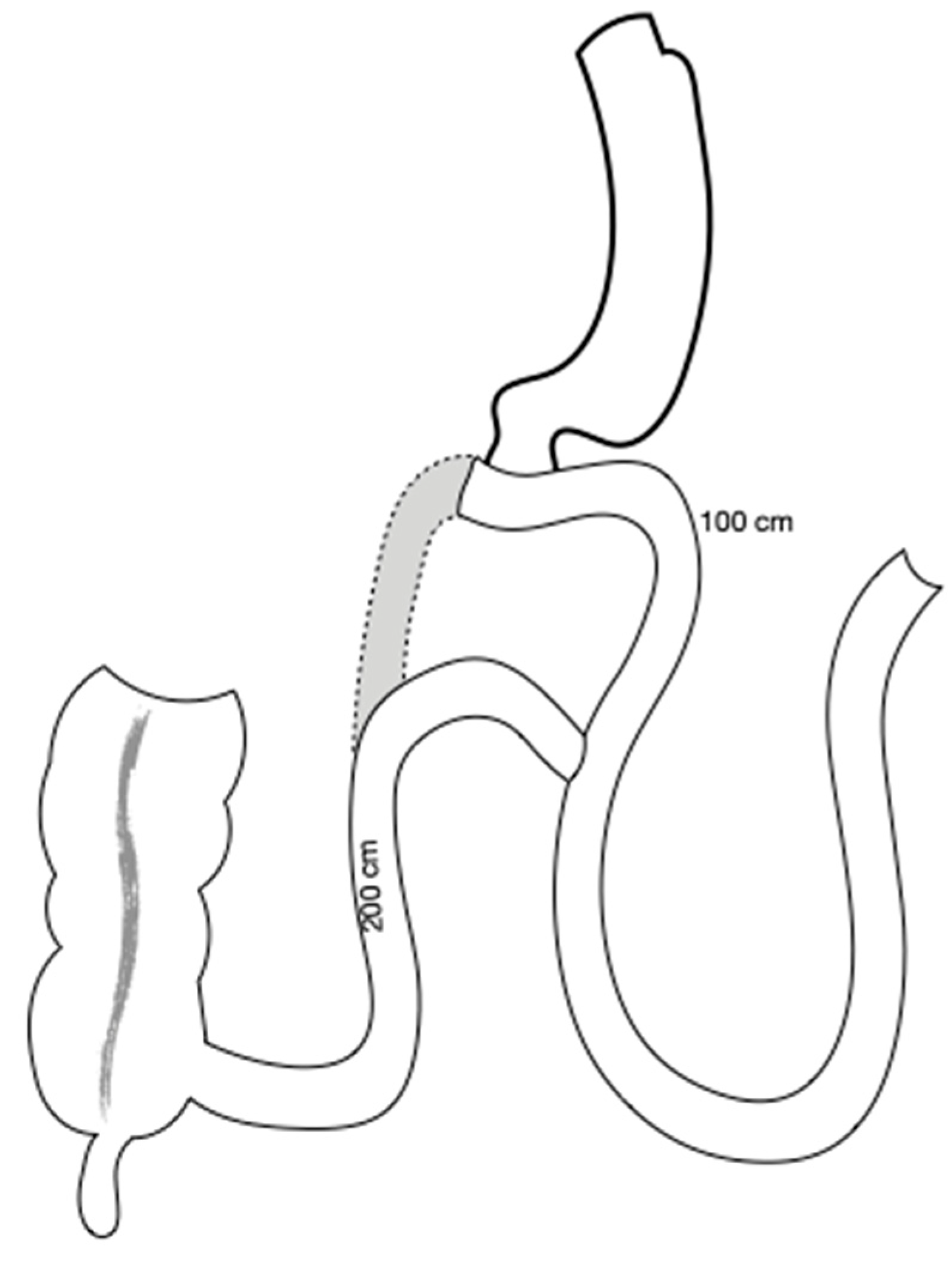
3.3. Surgical technique
The first 3 patients had a conversion into a Roux en Y DS through a division of the efferent limb just beyond the anastomosis, and the creation of a new anastomosis between this and the afferent one one meter proximal to the duodeno-ileostomy (
Figure 2). In this way the three patients had a DS with an antiperistaltic alimentary limb (1 meter) and a 2 meter common limb. Three patients were submitted to a “total” reversal (1 case, end to end duodeno-duodenostomy) or an “almost-total” reversal, a duodeno-jejunostomy in the first jejunal loop (2 cases). The other ten patients were submitted to an elongation of the common limb through the division of the previous anastomosis and the creation of a new one more proximally, leaving a final common channel of 270 in one case, 300 cm in 3 and 350 cm in 7 cases. A resizing of the sleeve gastrectomy over a 54 French bougie was performed along with the proximalization of the SADI-S in 3 cases; all three were suffering from severe diarrhea with no or mild hypoalbuminemia and had a very enlarged stomach (
Table 1).
3.4. Outcome
After surgery, one patient with an advanced respiratory disease rejected ventilatory support and died. One patient with a Roux-en-Y DS was readmitted with an intestinal obstruction for an internal hernia, and was reoperated; intestinal resection was necessary, and she finally was converted into a Roux-en-Y Gastric Bypass. One patient with a Roux-en-Y DS with an antipersitaltic alimentary limb was reoperated 10 years later for gastro-ileal stasis with postprandial fullness and frequent regurgitation and vomiting. She was converted into a SADI-S with a 300 cm common limb.
3.5. Long term results
In the long term the mean weight was 71 kg (44 - 89) with a mean weight regain of 14 kg from revisional surgery; the mean BMI was 26 kg/m2 (17 - 37), and the stool frequency was normalized, with mean number of bowel movements of 1,3 (0,5 - 4).
3.6. Factors related to malnutrition
Clinical and laboratory data of patients needing surgery for malnutrition were crossed with data from the complete series of patients submitted to SADI-S to find out which parameters could be related to the development of malnutrition. Patients in which the common limb was found to be too short at reoperation (shorter than 15% than expected) were excluded, as we considered that the main reason for malnutrition in this subset was the technical error. Results are presented in
Table 2. Older age, lower BMI, higher glycemia, higher glycated hemoglobin (HbA1c), lower alkaline phosphatase, hypertension and a shorter common limb in the initial SADI-S (2 meter) were all significantly related to the possibility of reoperation for malnutrition.
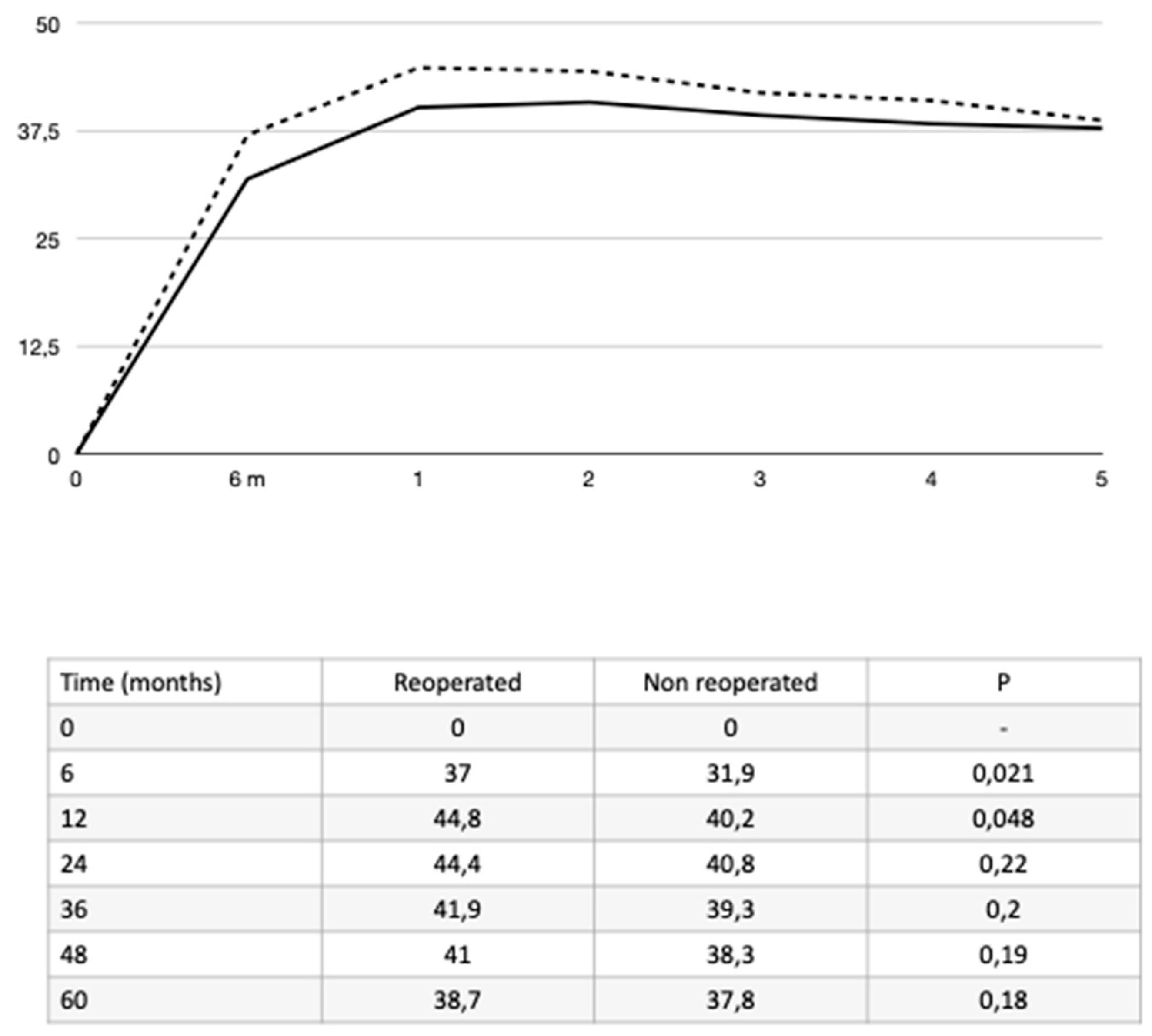
Patients submitted to reoperation had, after the index surgery, a greater weight loss (
Figure 3), a higher number of daily bowel movements as well as many laboratory test alterations as shown in
Table 3.
4. Discussion
SADI-S is a safe operation for selected patients with adequate follow up and life-long supplementation (4). However, despite being apparently safer than prior malabsorptive operations as BPD and DS, some patients can experience malnutrition, a life-threatening condition that must be avoided or early detected and treated (5).
The main findings of this review of our experience are that a short common channel (200 cm) is followed by a high rate of severe malnutrition; that errors in the measurement of the small bowel may also lead to malnutrition; and that there are some patients who can be especially vulnerable, as those older than 55 years, those with hypertension and poor controlled type-2 diabetes and patients with low liver reserve due to preexisting liver disease. Clinicians have to be aware when patients lose weight too rapidly, have more severe diarrhea, or their laboratory tests are significantly altered in the first postoperative year, as they are all markers of malnutrition.
The initial operation with a common channel of 2 meters was abandoned in 2009 because of the high incidence of malnutrition (2). The simple increase in 50 cm did not affect the good results on weight loss, and, on the other hand, increased the safety of the operation (5). To achieve a secure technique, the measurement of the ileum has to be accurate enough, either if it is done with marked graspers or if it is performed with a tape of known length (6, 7). We recommend measuring the bowel after relaxing the smooth muscle with intravenous Buscopan®, as the stretching of the small bowel has demonstrate to obtain more accurate measurements (8).
We found an association between older age and malnutrition. Cossu et al (9) reviewed the importance of age on malnutrition in patients submitted to BPD, finding that the group of patients older than 55 years had a 16% rate of malnutrition and an 8% rate of revisional surgery. The authors outlined the difficulty of aged patients in changing alimentary habits after surgery and the clinical importance of some disorders related to aging, as it is loss of appetite, the impaired sense of taste, the lack of teeth and therefore good mastication and sometimes even depression.
We also found that hypertension was more prevalent between reoperated patients, as well as higher preoperative values of glycemia and HbA1c. Hypertension and poor control of diabetes, defined by HbA1c above 7% or high glycemia are both related to atherosclerosis, which along with age could be the cause of an impaired intestinal absorption and a decreased adaption capacity of the small bowel. Although there are no studies on microvascularization of the small bowel and nutrition, atherosclerosis has been previously related to malnutrition in patients with peripheral arterial disease (10).
Aged patients and patients with glycemic alteration would preferable undergo a SADI-S with a longer common limb or perhaps another safer operation, as proximal Roux en Y gastric bypass or sleeve gastrectomy.
We find no explanation to the relationship between a low preoperative alkaline phosphatase (AP) and malnutrition; low AP levels are related to low zinc and magnesium levels, what is seen in malnutrition. Unfortunately, we do not routinely analyze them preoperatively, so we cannot establish a connection between them.
Liver disease, obesity, weight loss and malnutrition are intimately related. Non-alcoholic fatty liver disease (NAFL) improves after a successful weight loss operation. However, when weight loss happens too fast, the loss of adipose tissue leads to a massive mobilization of free fatty acids that reach the liver and provoke hepatotoxicity. This is compensated by the reduction of liver fat caused by the weight loss (11). But when other mechanisms are present, as protein malnutrition or deficiency of specific amino acids, or bacterial overgrowth, this toxicity can lead to a liver failure. Bacterial overgrowth is not supposed to happen after SADI-S, because there is not a real blind loop, as it was in old malabsorptive operations. Nevertheless, the mere absence of nutrients in an intestinal loop is enough to induce a substantial change in the jejunal microbiota (12), and this can have dramatic consequences in patients with liver disease. Patients with an underlying liver disease should never be offered this type of surgery because of the risk of hepatic insufficiency (13) that on some occasion has led to the need of liver transplantation (14).
Surgeons and endocrinologists should be specially alerted when weight loss is too fast in the first postoperative year, or when there is a high number of bowel movements. These patients have to be tested for micronutrient or protein insufficiency before clinical manifestations and treated with supplementation of protein and vitamins.
Regarding the revisional technique, we initially introduced the Roux-en-Y configuration with the antiperistaltic alimentary limb to avoid touching the previous duodeno-ileostomy. When we demonstrated the feasibility of dividing the anastomosis and performing a new duodeno-enterostomy without affecting the pylorus function, the initial technique was abandoned. As a rule we first measure the biliary and the common limb, to know if the cause of malnutrition was an error of the first operation, and to assess how long can the proximalization be done. Then, 100 to 150 cm are usually added to the common limb, placing the new anastomosis at 300 to 350 cm from the ilio-cecal junction. When there is a severe underlying disease, as happened with the psychiatric patient and with those suffering from liver failure, the new anastomosis is placed in the first jejunal loop or even in the duodenum, restoring an almost normal anatomy.
In summary, SADI-S is an effective and safe operation when the selection of patients, the performance of the operation and the supplementation and follow up are correct. Older patients, patients with hypertension, lower BMI or bad controlled diabetes, as well as those with severe accompanying conditions or those with problems of adherence to supplementation and follow up should not undergo SADI-S 250. Limitations of this study are the single institution experience, the retrospective nature of the study, the short number of patients and the heterogeneity of the series.
Author Contributions
Conceptualization: ASP, MAR, EPA, BL; Methodology: ASP, MAR, EPA, BL; Software: ASP, BL, EPA; Validation: ASP, EPA, MAR, AJT; Investigation: ASP, NPF, CM, LLA; Writing - draft: ASP, BL, EPA, MAR; Writing – review and editing: ASP, BL, MAR, CM, LLA, AJT, NPF, EPA; Supervision: ASP, EPA, MAR, AJT
Institutional Review Board Statement
For this type of study formal consent is not required.
Conflicts of Interest
The authors declare that they have no conflicts of interest regarding this manuscript.
References
- Sánchez-Pernaute A, Rubio Herrera MA, Pérez-Aguirre E, García Pérez JC, Cabrerizo L, Díez Valladares L, Fernández C, Talavera P, Torres A. Proximal duodenal-ideal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg 2007, 17, 1614-1618. [CrossRef]
- Sánchez-Pernaute A, Rubio MA, Pérez Aguirre E, Barabash A, Cabrerizo L, Torres A. Single-anastomosis duodenoileal bypass with sleeve gastrectomy: metabolic improvement and weight loss in first 100 patients. Surg Obes Relat Dis 2013, 9, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Gagner, M. Hypoabsorption not malabsorption, hypoabsorptive surgery and not malabsorptive surgery. Obes Surg 2016, 26, 2783–2784. [Google Scholar] [CrossRef] [PubMed]
- Vilallonga R, Balibrea JM, Curell A, Gonzalez O, Caubet E, Ciudin A, Ortiz-Zúñiga AM, Fort JM. Technical options for malabsorption issues after single anastomosis duodenoileal bypass with sleeve gastrectomy. Obes Surg 2017, 27, 3344–3348. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Pernaute A, Rubio Herrera MA, Pérez Ferré N, Sáez Rodríguez C, Marcuello C, Pañella C, López Antoñanzas L, Torres A, Pérez-Aguirre E. Long-term results of single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Obes Surg 2022, 32, 682–689. [Google Scholar] [CrossRef] [PubMed]
- Wagner M, Mayer BFB, Bodenstedt S, Kowalewski K, Nickel F, Speidel S, Fischer L, Kenngott HG, Müller-Stich B. Comparison of conventional methods for bowel length measurement in laparoscopic surgery to a novel computer-assisted 3D measurement system. Obes Surg 2021, 31, 4692–4700. [Google Scholar] [CrossRef] [PubMed]
- Slagter N, van Wilsum M, de Heide LJM, Jutte EH, Kaiser MA, Damen SL, van Beek AP, Emous M. Laparoscopic small vowel length measurement in bariatric surgery using a hand-over-hand technique with marked graspers: an ex vivo experiment. Obes Surg 2022, 32, 1201–1208. [Google Scholar] [CrossRef]
- Karagül S, Kayaalp C. Repeated stretched or non-stretched small bowel length measurements in healthy individuals. Turk J Surg 2019, 35, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Cossu ML, Fais E, Meloni GB, Profili S, Masala A, Alagna S, Rovasio PP, Spartà C, Pilo L, Tilocca PL, Noya G. Impact of age on long-term complications after biliopancreatic diversion. Obes Surg 2004, 14, 1182–1186. [Google Scholar] [CrossRef]
- Carvalho J, Correia MA, Kanegusuku H, Longano P, Wolosker N, Ritti-Dias RM, Cucato GG. Association between the risk of malnutrition and functional capacity in patients with peripheral arterial disease: a cross-sectional study. PLoS ONE 2022, 17, e0273051. [CrossRef]
- Vespasiani-Gentilucci U, Vorini F, Carotti S, De Vincentis A, Galati G, Gallo P, Scopinaro N, Picardi A. Hepatic complications of bariatric surgery: the reverse side of the coin. Acta Gastroenterol Belg 2017, 80, 505–513. [Google Scholar]
- Prakash G, Drenick EJ, Wexler H, Delucia L, Finegold SM. Microbial flora in the bypassed jejunum of patients with biliopancreatic bypass for obesity. Am J Clin Nutr 1987, 46, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick V, Moon RC, Teixeira AF, Jawad MA. Cirrhosis following single anastomosis duodeno-ileal switch: a case report. Int J Surg Case Rep 2018, 45, 130–132. [Google Scholar] [CrossRef]
- Addeo P, Cesaretti M, Anty R, Iannelli A. Liver transplantation for bariatric surgery-related liver failure: a systematic review of a rare condition. Surg Obes Relat Dis 2019, 15, 1394–1401. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).