1. Introduction
Tooth eruption is a unique, genetically determined process [
1]. Variations and abnormalities in tooth eruption may occur both in syndromic and non-syndromic patients and may cause serious orthodontics disorders. Alterations of the eruption process in terms of timing, sequence and extent need to be noticed, monitored and adequately managed in order to minimize potential unwanted consequences [
2].
Various changes in the eruption process have been described, with a range of causes, either general (endocrine, carential, systemic, drug-induced) or genetic [
3]. Primary failure of eruption (PFE) is
defined as a non-syndromic condition involving total or partial non-eruption of posterior teeth, in the absence of mechanical obstruction [
4,
5]. It is a rare disease with a reported prevalence of 0.06% [
6]. PFE may
affect deciduous and/or permanent teeth [
2,
5]. Involved teeth are either completely retained or can erupt partially and then cease to erupt, remaining relatively submerged. As only lateral teeth are affected, posterior open bite is the characteristic clinical feature, with functional impairment as a consequence [
7,
8]. The disorder may occur in any or all of the posterior quadrants and it is rarely symmetric [
4,
7]. All teeth situated distal to the most mesial affected tooth are typically involved [
4,
7].
Clinical features and severity degrees may vary widely in non-syndromic PFE [
8]. A systematic review performed by Hanisch et al. (2018) on previous published studies (2006-2017) on PFE summarized that girls tend to be slightly more affected (1.38:1 ratio), in almost 70% of the reported cases both molars and premolars were involved, primary teeth were affected in only about ¼ of the situations while in most cases (75.7%) PFE was limited to permanent teeth and the condition was more frequently bilateral (64%) [
5].
Etiology of PFE is still subject to study. Associations between eruption failure and other dental anomalies of known genetic origin suggest that PFE may have a significant genetic component [
9]. Alterations of 2 genes have been associated to PFE so far. Mutations in parathyroid hormone receptor 1 (
PTH1R) have been identified in several familial cases of PFE [
2,
8,
10]. Decker et al. (2008) first reported that a variant in
PTH1R was associated with PFE. This gene is located on chromosome 3p21-p22.1, MIM # and contains 16 exons [
11]. According to Roth et al. (2014), mutations in
PTH1R are associated with lethal dwarfism, chondrodysplasia, and isolated dental disorders specific to eruption [
12]. More recently, reported mutations in lysine methyltransferase 2C
(KMT2C) gene have been suggested as another potential molecular etiology of familial non-syndromic PFE [
13]. However, not all patients with PFE carry mutations of known genes [
1,
14].
Diagnostic of certainty in PFE is a difficult task. Checking parents’ occlusion is the first step recommended by Yamaguchi et al. (2022), as in most cases there is a family history [
15]. This should be followed by exclusion of any local and systemic causes for a potential mechanical impairment of eruption. Ankyloses, cysts, interference of adjacent tooth, lateral pressure from the tongue, oral clefts are cited as local factors susceptible of causing eruption failure, while genetic syndromes, endocrine disorders and long-term chemotherapy are mentioned as systemic factors [
10,
15]. More than 40 genetic diseases or syndromes are associated with failure of eruption, e.g., cleidocranial dysplasia, osteopetrosis, Rutherford syndrome, GAPO syndrome, osteoglophonic dysplasia [
9,
15]. Infraocclusion, immobility, metallic sound on percussion, and radiographic obliteration of the periodontal ligament space are cited as indicators for mechanical failure of eruption (ankylosis) [
15]. In practice however it may actually be very difficult to accurately differentiate between PFE and ankylosis. Therefore, genetic tests looking for variations in the
PTH1R, whenever possible to perform, may help differential diagnosis [
10,
11].
Treatment of PFE can be very challenging, as the affected teeth do not react to orthodontic forces, regardless the type or clinical severity of the condition [
5,
16]. This suggests that the defect in the eruptive process is permanent and irreversible. The involved teeth are not only unresponsive to orthodontic mechanics, but tend to become ankylosed when orthodontic traction is applied [
4,
15,
17]. Orthodontic traction is therefore not to be attempted when diagnosis of PFE is confirmed [
4,
10,
15,
18]. Treatment of PFE requires an interdisciplinary approach [
8,
18]. Each case needs to be carefully evaluated and treatment planning must be done in accordance with the clinical situation and patient’s age [
5]. In mild cases, with a limited number of insufficiently erupted teeth, prosthodontic restoration may be enough for establishing a satisfactory occlusion. More severe situations may require surgical approached of variable complexity, from small-segment osteotomy, with or without bone grafting [
4,
19] to extraction of affected teeth followed by ridge augmentation and implants placing [
15]. In very severe cases, with a large number of affected teeth and a significantly deformed alveolar ridge, removable appliances may be considered in order to restore occlusion and appearance from early stages [
20].
2. Case Report
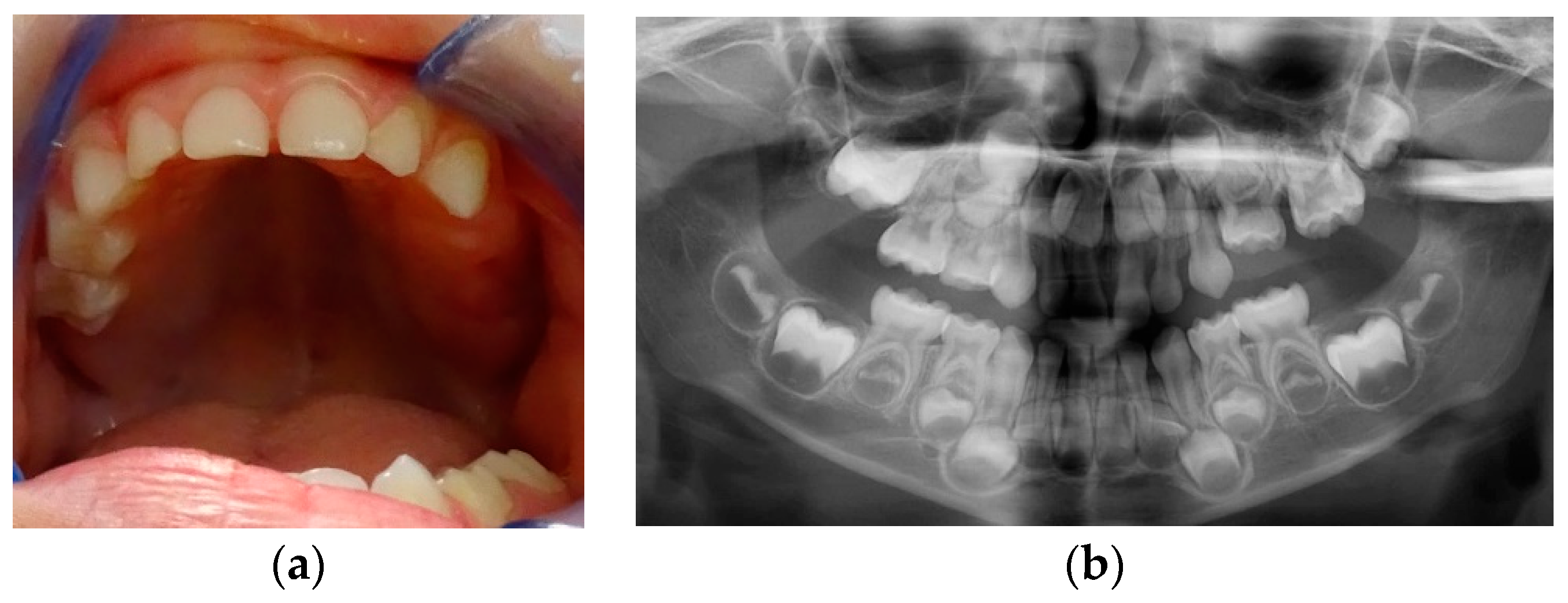
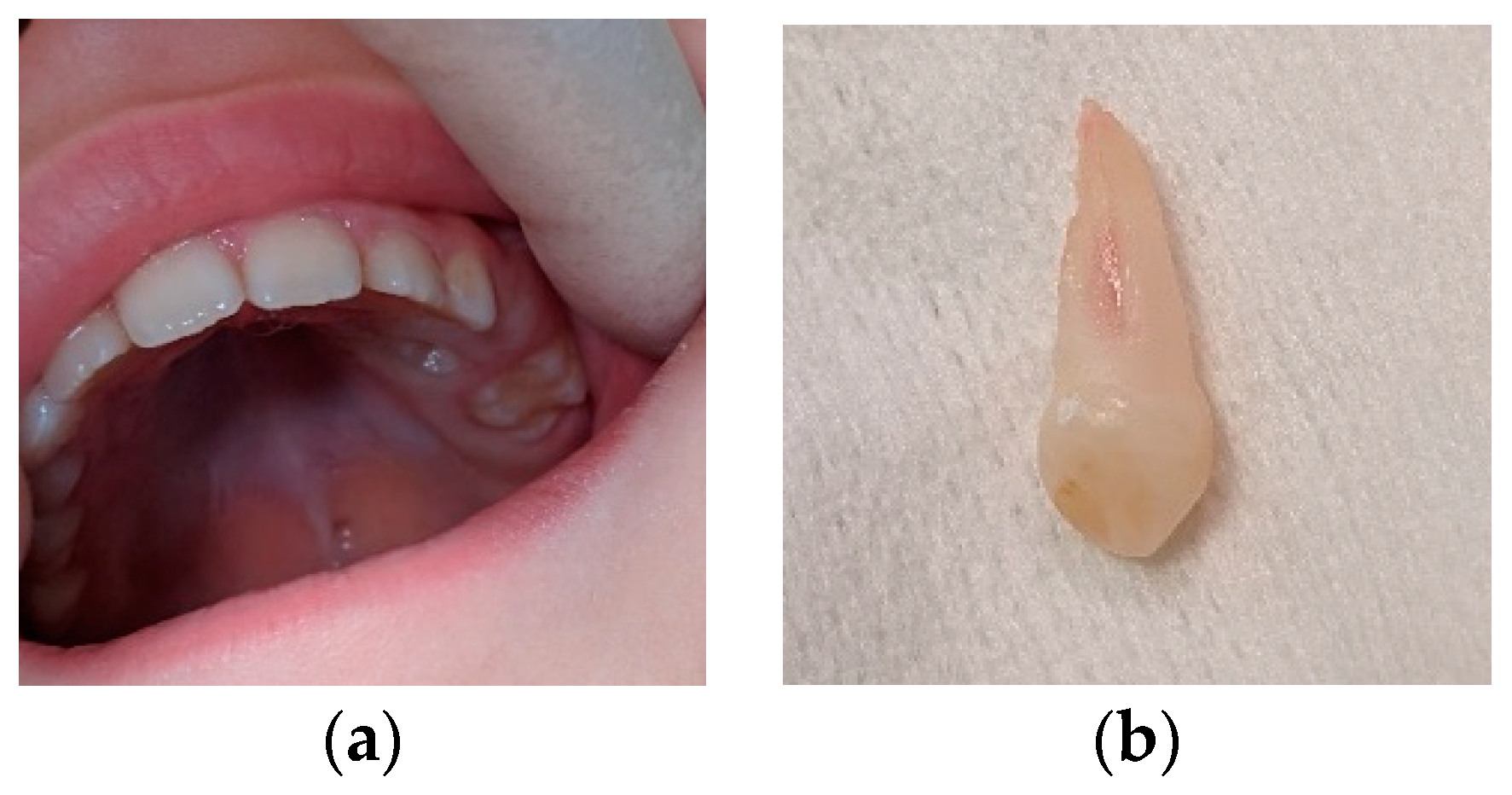
A 4-year-old girl presented for asymmetry of upper arch. The patient had no systemic disorder, her stature was normal for her age and there was no relevant family history of dental abnormalities. Clinical examination (
Figure 1a) revealed no erupted teeth distal to the left upper canine, a left lateral open bite and a slight shift of the upper midline to the left. Panoramic X-ray taken at this time showed delayed intra osseous development of lateral left upper teeth as compared to the right side (
Figure 1b) and no sign of mechanical obstruction. Agenesis of upper left premolars (24, 25) was suspected, but uncertain at that time.
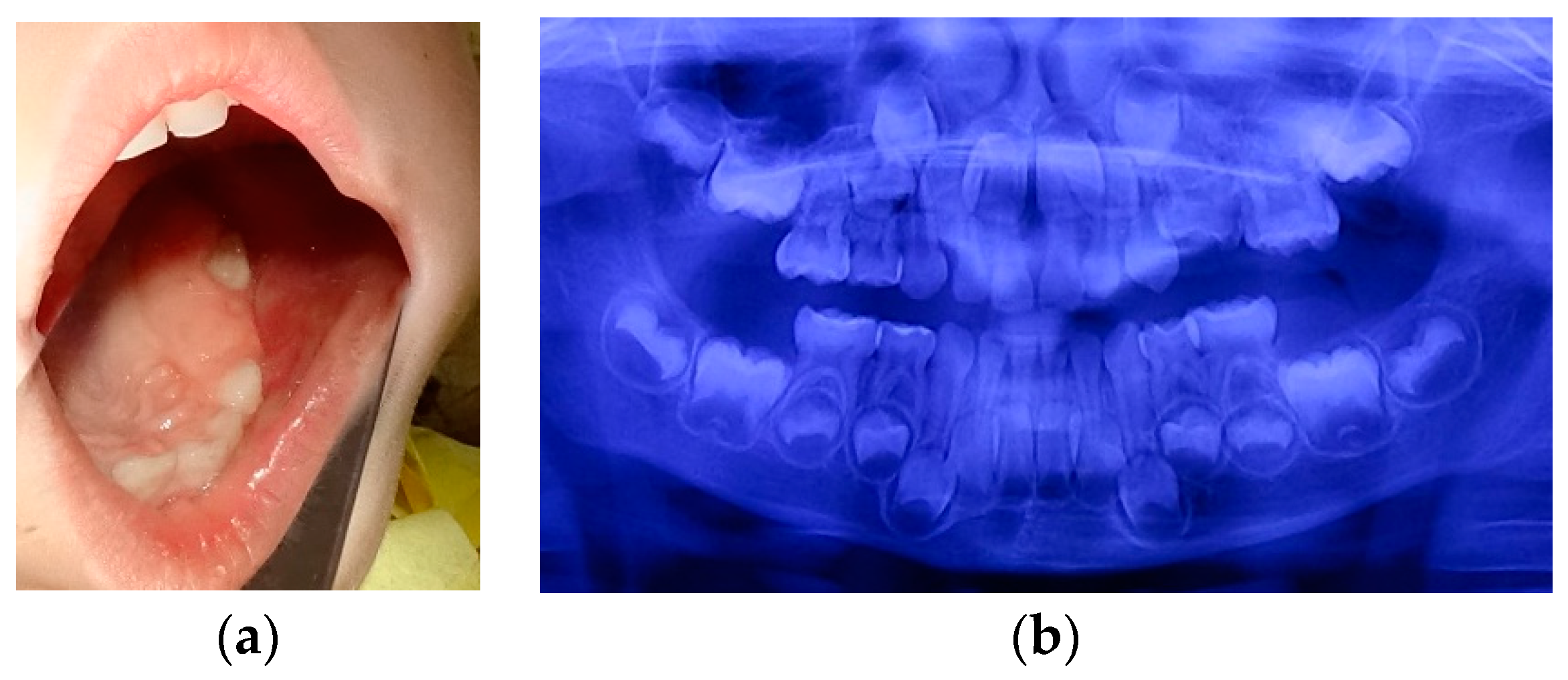
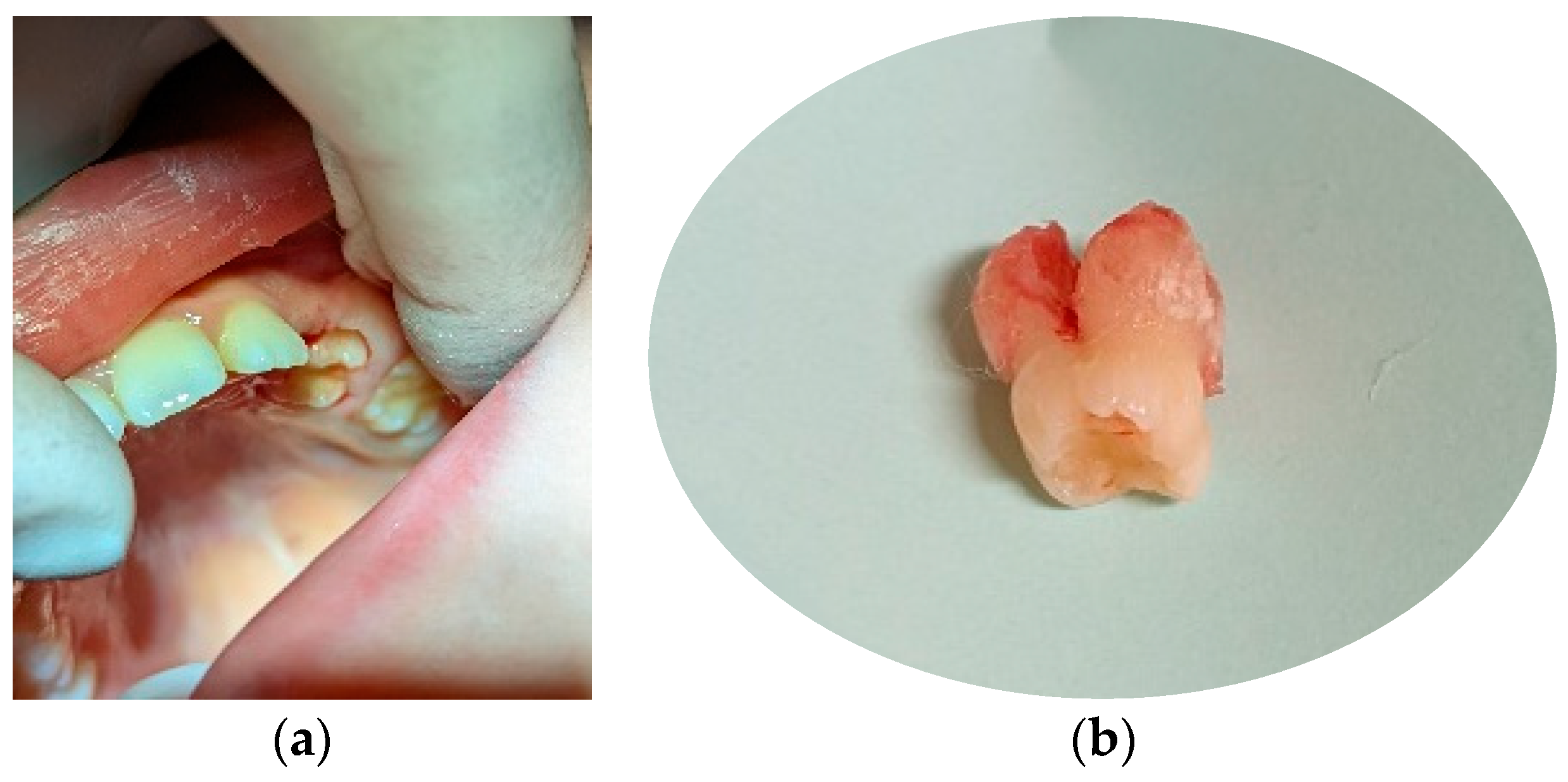
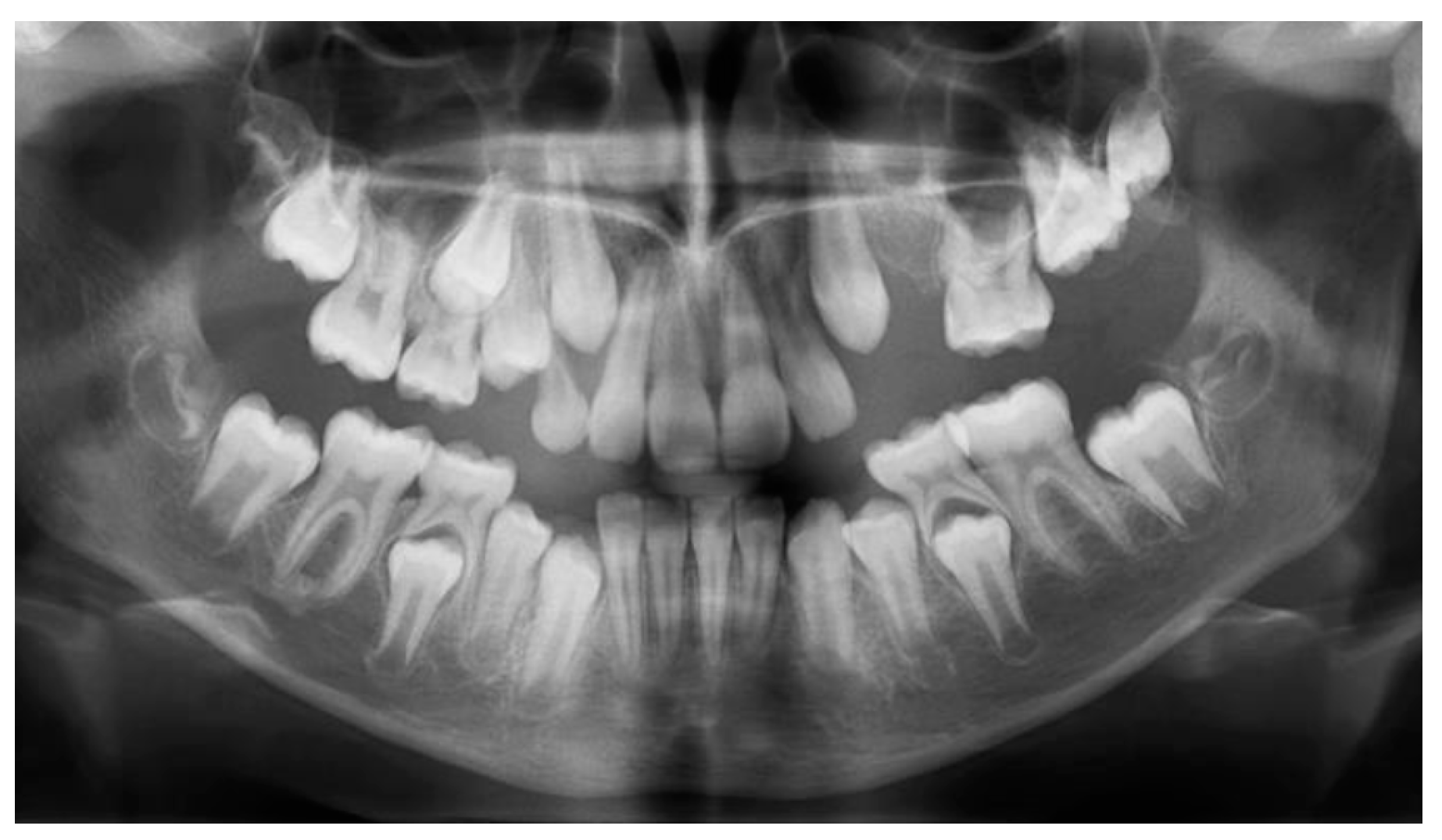
Eleven months later (age 5y 3m) a molar was erupting in the left upper arch. The erupting tooth was considered to be the second primary molar (65), although its shape and size as seen on the new panoramic X-ray substantially differed from those of 55, present on the arch. This new X-ray also suggested that 64 could be mechanically impacted by 63 (
Figure 2a,b).
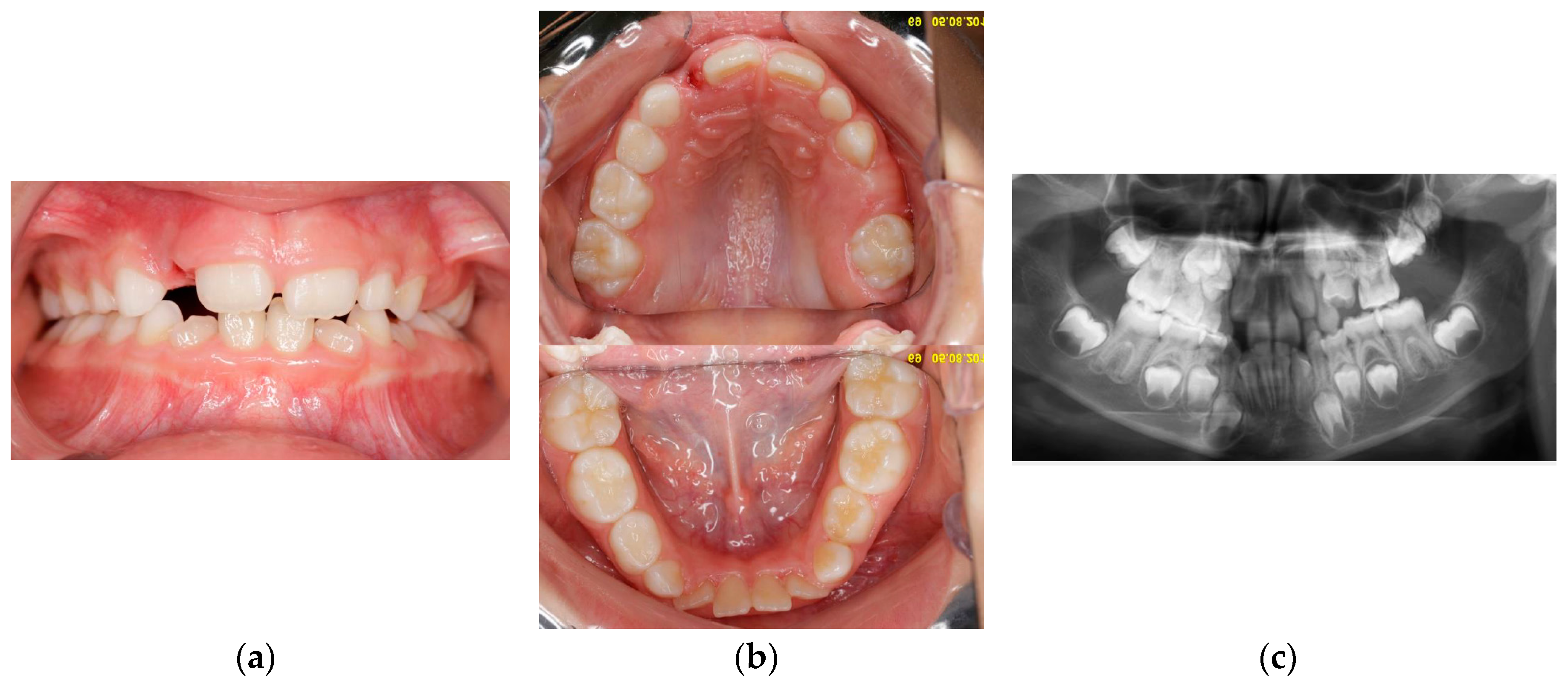
Four years later (age 7y 10m), 65 had fully erupted, with atypical crown shape and size (larger than usual, almost like a first permanent molar) (
Figure 3a,b); no premolar buds could be seen in the upper left quadrant; unerupted 26 had reached the coronal stage, while 27 had a delayed development as compared to 17 (
Figure 3c). 64 had become more re-intruded and seemed to be impacted by 63. PFE of upper left permanent molars was suspected. Some lower front crowding was also noticed.
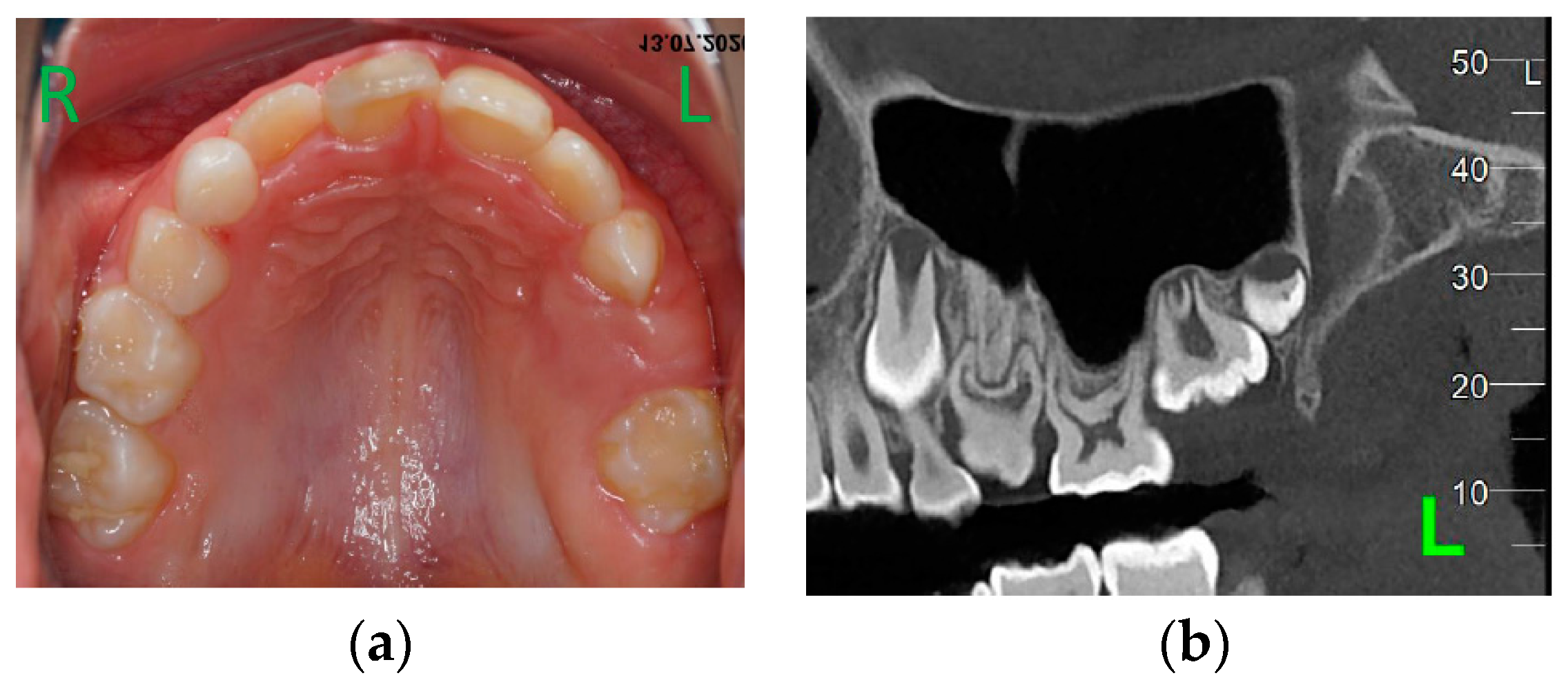
At age 9y 7m, 26 was still not on the arch (
Figure 4a). A CT examination was performed. Agenesis of 24, 25 became certain (
Figure 4b) and no areas of ankyloses in teeth with eruption failure were found. Decision was taken to remove 63 in order to favour eruption of mechanically impacted 64, but extraction was postponed at family’s request.
One year later, at age 10y 8m, 63 was extracted (
Figure 5), giving way for 64, while 65 had reached the occlusion plane.
Erupting 64 was subsequently removed (3 months later) under nitrous sedation (
Figure 6) in order to favour eruption of the upper left canine.
At 11y 8m, 23 was gaining its place on the arch (simultaneously with 13), 65 remained stable, while 26 and 27 seemed to continue their development very slowly within the alveolar bone (
Figure 7).
Genetic testing was proposed in order to identify potential underlying genetic factors for the diagnostic of PFE; after considering the pros (adding data for diagnostic) and cons (relatively high costs, not supported by the national health trust), the patient’s parents decided not to do genetic analysis for the time being.
Taking into account the presence of third molars’ buds in the upper right quadrant and in the mandible, a treatment plan was made that involved keeping 65, removal of 14, 34, 44 in order to favour a balanced occlusion and orthodontic correction of the midline, while waiting and observing the evolution of the upper left permanent molars. As previous case reports found orthodontic attempts to bring retained teeth on the arch unsuccessful, this was not considered as an option for 26, 27. Treatment plan was explained to the child and parents. Extraction of permanent teeth was regarded as a major drawback by the patient’s family, while displacement of the midline remained the main concern. Any further action was postponed and the case remained under observation.
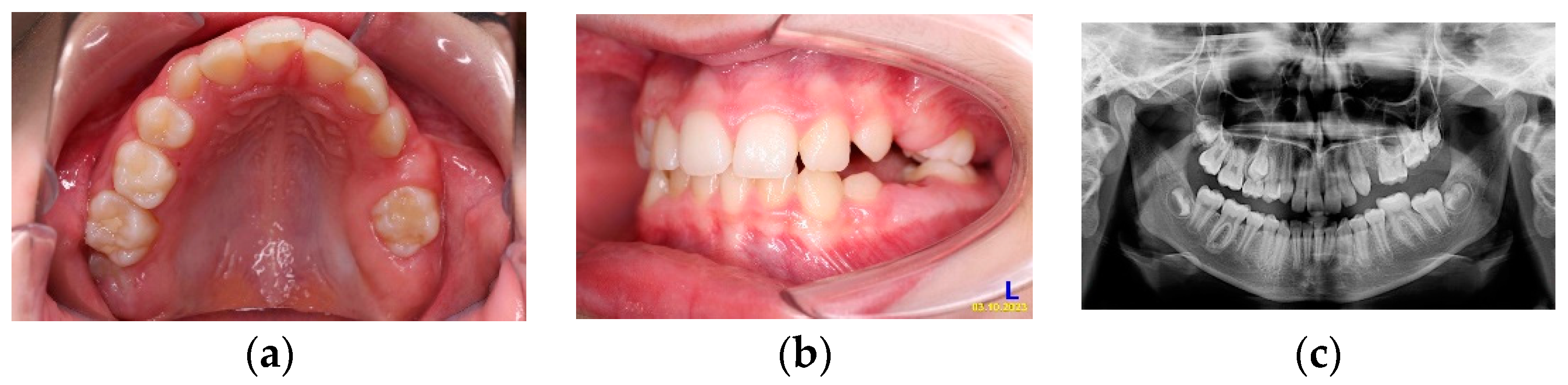
Fifteen months later, at age 12 y 11 m, while upper canines were erupting, clinical and radiological situation in the distal part of the upper left quadrant was not much different (
Figure 8a–c).
At this point, decision was taken by parents to perform genetic testing. Sequence and Del/Dup (CNV) analysis using the Blueprint Genetics (BpG) PTH1R single gene test did not detect any known disease-causing or rare variants that could explain the patient’s phenotype as described to the laboratory at the time of interpretation.
The case remains under clinical surveillance.
4. Discussion
Proffit and Vig first introduced the term “primary failure of eruption” (PFE) to describe a condition in which a troubled eruption mechanism causes non-ankylosed teeth to be unable to erupt [
4].
Raghoebar et al. (1991) proposed two different terms for localized eruption failure:
primary retention (1) defines those situations where eruption is arrested before the crown has penetrated the oral mucosa, while
secondary retention (2) stands for those cases where the tooth has penetrated the oral mucosa but is not able to finalize the eruption process [
21,
22]. By this classification, our patient seems to be a primary retention case, with first and second upper left permanent molars unable to emerge. Frazier-Bowers et al. (2007) divided PFE into three different types. In Type I, all affected teeth show a similar or severe lack of eruption potential. In Type II, the teeth situated distally from the most mesial affected tooth show greater yet still inadequate eruption potential. Subjects displaying both Type I and II PFE are diagnosed with Type III [
7]. According to this classification, our patient fits into the Type I pattern.
All clinical features described in the presented patient suggest a diagnostic of PFE involving permanent upper left molars, co-existing with agenesis of both upper left premolars and unusual shape and dimensions of upper left primary molars, particularly the crown of 65 and roots of 64. No one in her family had a history of eruption failure. According to Hanish et al., almost 15% of patients with PFE had no family members affected by PFE [
5]. It is considered that the patient with PFE without family history may have had a spontaneous mutation in
PTH1R [
14]. This hypothesis was not confirmed in our patient, as genetic testing performed at almost 13 years of age found no mutations in
PTH1R gene. Although
KMT2C gene alteration has been suggested as another potential molecular etiology of familial non-syndromic PFE [
13], we estimated that, given the lack of family history of PFE in the presented case, it is unlikely that alteration of
KMT2C could be the cause; no further genetic testing was performed.
Except for the lack of genetic confirmation, all other factors indicate the diagnostic of PFE in our patient. Although mechanical impaction of 64 could not be ruled out and was clinically managed until the tooth erupted and could be removed, syndromic and local factors that might have caused eruption failure in the permanent molars were excluded, as recommended by Yamaguchi et al. (2022) [
10] and Frazier-Bowers et al. (2010) [
14].
The unusual crown shape and size of 65 are to be noted, alongside with the unusual root anatomy of the extracted, previously impacted 64. Abnormalities noticed in our patient (alteration of crown shape and size/root morphology, mechanical impaction, hypodontia) are found among those reported in other studies. Hanish et al. (2016) performed a systematic review on 17 articles reporting clinical data of 314 patients with PFE. In 39 cases, additional dental anomalies were described. These included alterations in the root morphology (
n = 11), impacted teeth (
n = 10), delayed eruption of further teeth (
n = 6), hypodontia (
n = 5), hyperdontia (
n = 3), transposition of teeth (
n = 2), peg-shaped teeth (
n = 1), and mechanical failure of eruption (
n = 1). In 70 cases, no further dental anomalies were reported, while no details regarding these data were available for 190 cases [
5].
Regular clinic and radiographic follow-up were performed during the next 9 years in order to monitor the eruption sequence and occlusion during growth. CBCT performed at age 9 ascertained the agenesis of premolars in the same quadrant where delayed evolution of both deciduous and permanent molars was seen
. Ahmad et al. [
9] reported that 13% of the patients with PFE had hypodontia, a percentage substantially higher than within regular population [
23].
Regarding the type of malocclusion associated to PFE, no consensus exists in the literature. Hanisch et al. (2018) report 5.9% of skeletal Classes I, 14.7% of Classes II and 79.4% of Classes III [
5]. Yamaguchi et al. (2011) and Awad et al. (2022) cited a predominance of skeletal Classes III [
1,
24]. Our patient associates a class II malocclusion.
In our case, the patient was a healthy 4-years girl presented with a shortened left upper arch initially due to the delayed eruption of the deciduous molars. She was closely monitored during the following 9 years and remains under clinical surveillance. It is important to mention that, to the authors’ knowledge, there are no reports on PFE cases described and monitored since such young age. A systematic review performed on 314 patients with PFE, aged between 8 and 58 years, showed that in only 24.3% of cases primary teeth were affected [
5]. The present case was initially diagnosed as a unilateral PFE during the primary dentition (age 4y). However, during follow-up, 65 had fully erupted by age 7y 10m, while 64 was mechanically impacted and managed to partially erupt after removal of the deciduous canine. We can therefore consider that in our case primary teeth were not affected by PFE, but rather by a delayed eruption.
Underlying genetics in PFE is still subject to study; not all patients with PFE carry mutations in known genes [
1,
14]. In the presented case 26 has not erupted by almost 13 years of age and 27 has delayed development (and an unusual shape). These findings, along with the absence of the premolars and the unusual shape and size of the deciduous molars as well as the patient’s gender made us consider that PFE is the most likely diagnostic, possibly falling into another, perhaps more rare, genetic category.
5. Conclusions
Even when detected early, PFE rises difficult problems with regard to diagnosis and treatment planning due to the impossibility to accurately predict the evolution. Tooth agenesis on the same arch worsens the prognosis and adds challenges to planning the treatment. Close long-term follow-up and timely adjustment of treatment plan in accordance to the evolution of the case are needed, while patient and family’s expectations need to be carefully considered in all stages.
Author Contributions
Conceptualization, A.V. and A.M.; methodology, A.V., A.M.; investigation, A.V.; resources, A.V., E.V.G.; data curation, X.X.; writing—original draft preparation, A.M., A.V.; writing—review and editing, E.V.G., F.C.; visualization, A.M.; supervision, A.V., F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
This paper did not require ethical approval.
Informed Consent Statement
Informed consent was obtained from the patient to publish this paper (available with corresponding author).
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Awad MG, Dalbah L, Srirengalakshmi M, Venugopal A, Vaid NR. Review and case report of the treatment in a young girl with primary failure of eruption. Clin Case Rep 2022, 10, e05632. [Google Scholar] [CrossRef] [PubMed]
- Grippaudo C, Cafiero C, D’Apolito I, Ricci B, Frazier-Bowers SA. Primary failure of eruption: Clinical and genetic findings in the mixed dentition. Angle Orthod 2018, 88, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Castaneda B, Choukroune C. Alterations of the permanent molars eruption. Revue Odonto Stomatologique 2016, 45, 180–206.
- Proffit WR, Vig KW. Primary failure of eruption: a possible cause of posterior open-bite. Am J Orthod 1981, 80, 173–190. [Google Scholar] [CrossRef] [PubMed]
- Hanisch M, Hanisch L, Kleinheinz J, Jung S. Primary failure of eruption (PFE): a systematic review. Head Face Med 2018, 14, 5. [CrossRef]
- Baccetti, T. Tooth anomalies associated with failure of eruption of first and second permanent molars. Am J Orthod Dentofac Orthop 2000, 118, 608–610. [Google Scholar] [CrossRef]
- Frazier-Bowers SA, Koehler KE, Ackerman JL, Proffit WR. Primary failure of eruption: further characterization of a rare eruption disorder. Am J Orthod Dentofac Orthop 2007, 131, 578. [CrossRef]
- Wagner D, Rey T, Maniere MC, Dubourg S, Bloch-Zupan A, Straub M – Primary failure of eruption: From molecular diagnosis to therapeutic management. Journal of Oral Biology and Craniofacial Research 2023, 13, 169–176. [CrossRef] [PubMed]
- Ahmad S, Bister D, Cobourne MT. The clinical features and aetiological basis of primary eruption failure. European Journal of Orthodontics 2006, 28, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Frazier-Bowers SA, Simmons D, Wright JT, Proffit WR, Ackerman JL. Primary eruption failure and PTH1R: the importance of a genetic diagnosis for orthodontic treatment planning. Am J Orthod Dentofacial Orthop 2010, 2, 160–161. [Google Scholar] [CrossRef]
- Decker E, Stellzig-Eisenhauer A, Fiebig BS, Rau C, Kress W, Saar K, Rüschendorf F, Hubner N, Grimm T, Weber BH. PTHR1 loss-of-function mutations in familial, nonsyndromic primary failure of tooth eruption. Am J Hum Genet 2008, 83, 781–6. [Google Scholar] [CrossRef] [PubMed]
- Roth, H. , Fritsche, L.G., Meier, C. et al. Expanding the spectrum of PTH1R mutations in patients with primary failure of tooth eruption. Clin Oral Invest 2014, 18, 377–384. [Google Scholar] [CrossRef]
- Assiry, A.A. , Albalawi, A.M., Zafar, M.S. et al. KMT2C, a histone methyltransferase, is mutated in a family segregating non-syndromic primary failure of tooth eruption. Sci Rep, 2019; 9, 16469. [Google Scholar] [CrossRef]
- Nagata M, Ono N, Ono W. Mesenchymal progenitor regulation of tooth eruption: a view from PTHrP. Journal of Dental Research. 2020, 99, 133-42. [CrossRef]
- Yamaguchi T, Hosomichi K, Shirota T, Miyamoto Y, Ono W, Ono N. Primary failure of tooth eruption: Etiology and management. Jpn Dent Sci Rev 2022, 58, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Łyczek J, Antoszewska J. Primary failure of tooth eruption – etiology, diagnosis and treatment. Dent Med Probl, 2013; 50, 349–354.
- Mouna B, Hassnae B, Bassima C – Idiopathic failure of eruption: Diagnosis and management dilemma. Advances in Oral and Maxillofacial Surgery 2022, 6, 100259. [CrossRef]
- Aruna U, Annamalai PR, Nayar S, Bhuminathan S. Primary failure of eruption- a case report with cone beam computerized tomographic imaging. J Clin Diagn Res 2014, 8, ZD14–6. [Google Scholar] [CrossRef]
- Brady, J. Familial primary failure of eruption of permanent teeth. Br J Orthod. 1990, 17, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Atobe, M. , Sekiya T., Tamura K., Hamada Y., Nakamura Y. Severe lateral open bite caused by multiple ankylosed teeth: a case report. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2009, 107, e14–e20. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar GM, Boering G, Vissink A. Clinical, radiographic and histological characteristics of secondary retention of permanent molars. J Dent 1991, 19, 164–170. [CrossRef]
- Raghoebar GM, Boering G, Vissink A, Stegenga B. Eruption disturbances of permanent molars: a review. J Oral Pathol Med 1991, 20, 159–166. [CrossRef]
- Mattheeuws N, Dermaut L, Martens G. Has hypodontia increased in Caucasians during the 20th century? A meta-analysis. Eur J Orthod 2004, 26, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi T, Tomoyasu Y, Shirota T, Takahashi M, Nakano H, Kurabayashi H. Craniofacial and dental characteristics of patients with primary failure of tooth eruption in Japanese. Hosp Dent 2011, 23, 11-15.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).