1. Introduction
The operating environment of medical institutions has undergone rapid changes in recent decades, therefore more attention has been paid to improving the quality of health services and mitigating medical side effects. In particular, the aging of the population, the increase in costs related to the treatment of aging-related diseases, and the widespread use of expensive medical services have contributed to the imbalance in the financial situation of medical institutions. Consequently, health officials and facility managers increasingly focus on ongoing cost management, cost control, and evaluation of potential benefits related to physician quality performance indicators. Despite the establishment of many measurement indicators, the management of health institutions encountered various challenges and shortcomings [
1]. As medical facilities are forced to improve service efficiency and medical quality in patient care, health care providers at these facilities are expected to work longer hours. This long and demanding schedule often leads to fatigue, which reduces their work enthusiasm and overall job satisfaction [
2]. With continuous and long-term work, it is possible to increase the utilization rate of the equipment, but this can affect the physical and mental well-being of the personnel. severity of patients and # 039; illnesses and the short time from hospital arrival to discharge are major challenges for providing safe and effective medical services [
3]. Frequent contact between medical staff and patients, especially in smaller hospitals and clinics, inevitably increases medical risks. Addressing health issues and managing a variety of healthcare management issues can be a challenge for a nursing home. In addition, performance-based evaluation of clinical and medical services is difficult to improve medical quality [
4]. Therefore, the analysis of the quality of medical care services is very important in the preparation of metrics that improve the functioning of care institutions. However, due to limited and dispersed medical resources, it can be difficult for managers to comprehensively improve the quality of medical care [
5].
Measurement of medical facilities and # 039; the quality of service plays a central role in hospital management, and senior managers of medical institutions pay more and more attention to it. Since medical institutions provide diagnostic, treatment, and rehabilitation services, improving the service quality and efficiency of these institutions is essential. Thus, identifying appropriate measurement methods to evaluate the quality of medical services provided by medical facilities and determining effective medical strategies to provide quality medical services becomes a primary concern for medical facilities [
6]. Effective and safe measurements of the quality of medical services can improve the quality of medical services, reduce the costs of related medical institutions, optimize the processes of related medical services and achieve reasonable allocation of resources. This in turn leads to better medical management and functional performance [
7]. As the demand for medical services increases, so does the need for government oversight of health services, focusing on issues such as providing quality medical services and improving patient satisfaction among key managers of medical facilities [
8]. In the competitive and specialized field of private medical facilities, the quality of medical services is crucial for economic development and patient satisfaction. Measuring the quality of medical services provides managers of medical facilities with information about their medical outcomes, which highlights the need to improve the collection and analysis of problems [
9]. Considering that there are many indicators that can affect the delivery of services in nursing homes, monitoring and managing them all is unrealistic with limited medical resources. Improving the performance of medical services is related to the interests of different medical departments, which requires the participation of experts from different backgrounds in evaluating the performance measurement of medical care [
10]. Since measuring the effectiveness of medical care usually involves several indicators, it may not be enough to rely solely on the limited resources of medical institutions to fully improve the quality of medical care. Therefore, it is necessary to define a limited number of key performance indicators for medical facilities to measure and monitor service quality and ensure safe and efficient working conditions to achieve patient and staff satisfaction through appropriate and effective management [
10]. The literature on the evaluation and measurement of quality improvement processes in medical services has received increasing attention. Achieving quality medical service requires reliable management information, accurate problem identification, accurate analysis of relevant data, and the ability to measure and measure the quality of a redesigned medical service [
11].
The purpose of this study is to classify the service performance measurement of medical institutions into meaningful measures and to find out their relative importance. In addition, the purpose of the study is to analyze the relationships between the key indicators of nursing activity to find out the primary indicator influencing the performance of nursing activity. The main focus of this research is in medical facilities and #039; service performance. In addition, this study examines important indicators that can strengthen and improve the competitiveness of medical institutions and #039; quality of service, and quot; medical facilities; referring to hospitals and clinics during this study. Analysis of medical facilities and#039; Standards of services are based on the dimensions of Balanced Scorecard (BSC) and have been recognized as an effective tool in medical and health management and operations [
12,
13,
14]. Therefore, this study presents the integration of BSC in medical facilities to improve their performance. Despite the existing literature applying the BSC to medical institutions [
12,
13,
14], there is still a need for a deeper understanding of its systematic hierarchical structure in relation to the delivery of medical services in these institutions. To address this research gap, this study aims to establish an appropriate structure of BSC evaluation indicators determined by the Analytic Hierarchy Process (AHP) and expert surveys. This study recognizes possible relationships between different key indicators of relative importance. This study also aims to quantify the causality of service performance measurement in medical facilities in Taiwan using the Decision Making and Experimental Evaluation Laboratory (DEMATEL). This holistic approach aims to provide a nuanced understanding of the complex relationships and hierarchical structure of medical services performance indicators in the context of medical facilities in Taiwan.Parte superior do formulário
2. Materials and Methods
2.1. Developing Service Performance Measurements
Kaplan and Norton introduced the Balanced Scorecard (BSC) as an organizational performance management system in 1992 [
15,
16]. This innovative approach aimed to address the limitations of management and focus only on short-term financial results, as well as the poor design of performance measurement systems. Kaplan and Norton proposed a BSC performance measurement system that combines both financial and non-financial performance indicators and performance management systems [
15,
16].
Traditionally, an organization's performance has been measured primarily through return on investment (ROI) and financial statements, particularly the payback period. This narrow focus limited the performance management of factors important to organizational growth, adaptability, and competitiveness, such as new product development, process improvement, human resource development, information technology, and customer and market development. The BSC emerged as a dominant solution that prevents institutional managers from emphasizing only the long-term benefits of short-term financial performance indicators while neglecting future investment growth [
17].
The BSC consists of four dimensions: financial, customer, internal processes, and learning and growth [
9]. Although the financial dimension concerns traditional financial performance, the last three dimensions are covered by non-financial performance measurement indicators, especially the customer dimension, the internal process dimension, and the learning and growth dimension. The BSC evaluates and guides companies in certain functions and industries based on the organization or industry and specific factors. The relative weights of BSC performance indicators are widely used, including in medical institutions [
2,
4,
8]. Therefore, this study adopts the four dimensions of the BSC: finance, customer, internal process, and learning and growth.
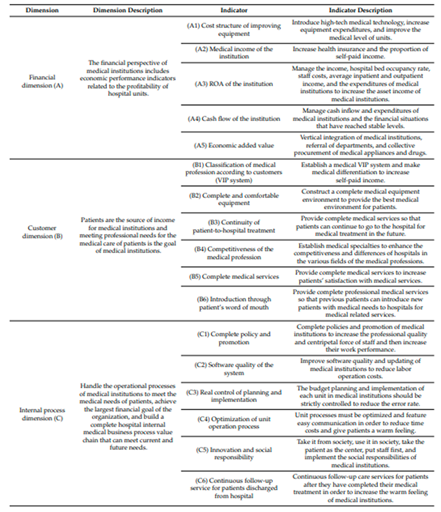
In this work, the collection of literature was based on the Balanced Scorecard as the basis for the management of medical institutions in the determination of operational and management indicators. At the same time, achieving the strategy and vision of nursing homes is considered the central basis of the study. It systematically examines the performance indicators of medical facility management by searching relevant literature, professional and scientific suggestions, and consulting with experts in the field. The evaluation dimensions and indicators to measure the service performance of medical facilities are summarized in
Table 1. To justify the content of BSC service indicators, references were collected from relevant experts or researchers who received unanimous approval from most national medical institutions. management of service indicators [
12,
13,
14,
18].
2.1.1. Economic Dimension
The financial dimension of medical facilities includes financial performance measures that are directly related to the profitability of each hospital unit. The following factors are formulated to measure this dimension:
Cost Structure of Improving Equipment: This factor involves understanding and optimizing the cost structure associated with enhancing medical equipment [
17,
19,
20].
Medical Incomes of Institutions: The financial health of medical institutions is assessed through their medical incomes, taking into account sources such as patient fees, insurance reimbursements, etc. [
20,
21].
Return on Assets (ROA) of the Institution: ROA is a key financial metric that gauges the institution's efficiency in generating profits relative to its assets [
8,
17,
20,
21].
Cash Flow of the Institution: Examining the cash flow is crucial for assessing the liquidity and financial stability of the medical institution [
8,
17,
21].
Economic Added Value: This indicator assesses the value generated by the medical institution beyond the cost of capital, providing insight into overall economic performance [
17,
22].
A good financial position allows medical institutions to invest in advanced medical instruments, which improves the quality of medical equipment. In addition, in larger medical facilities where different units have common needs for medical supplies, such as gloves, there is an opportunity for savings through pooled procurement. Such vertical integration takes advantage of the size of medical institutions to achieve economic added value, which contributes to the reduction of procurement costs [
13,
18].
2.1.2. Client Measurement
Patients become an important source of income for healthcare organizations, helping these organizations meet and Professional healthcare perspectives. When a pharmacy's expected goals are established, customers and the pharmaceutical market are separated. The following metrics were developed to measure the effectiveness of meeting patient needs:
Classification of Medical Profession According to Customers (VIP System): This indicator involves the implementation of a VIP system to categorize medical services based on customer preferences and needs [
8,
23].
Complete and Comfortable Equipment: Ensuring the availability of up-to-date and well-maintained equipment contributes to providing patients with comprehensive and comfortable facilities [
23].
Continuity in Patient-to-Hospital Treatments: The seamless continuity of care from the patient's entry to the hospital through their treatment is crucial for a positive patient experience [
8,
17].
Competitiveness of the Medical Profession: This indicator assesses the competitiveness of the medical profession, ensuring that the institution attracts and retains skilled medical professionals [
8,
20].
Complete Medical Services: Encompassing a comprehensive range of services, this indicator ensures that medical institutions fulfils all aspects of patient care, including diagnosis, treatment, and other healthcare needs [
4,
8,
20,
21].
Promotion through Patient Word of Mouth: Positive feedback and recommendations from patients contribute to the institution's reputation and attractiveness [
8,
17,
22].
A patient enters a hospital, a facility that provides care and related treatment. You can submit your application to the state health insurance agency for a fee. Through equipment renovations and maintenance, medical institutions can provide the best and most comfortable places for patients. In addition, we contribute to the provision of comprehensive health services by completing parts and equipment in health facilities. For example, in the case of a patient who has been in a car accident, a fracture may not be detected in a small clinic without X-ray equipment. Therefore, it is important that medical facilities provide all the facilities and amenities so that patients can receive comprehensive health services.
2.1.3. Internal Process Volume
Management processes in health management are aimed at satisfying the needs of patients and their requests for health services, but the main economic goals of the organization. At the same time, we are working to create a comprehensive value chain of hospital internal health business processes that can meet current and future needs. As a result, the following metrics were created:
Complete
the policy and
promotion: This indicator focuses on ensuring that internal policies and promotional strategies within medical institutions are comprehensive and effectively communicated [
21,
22,
23].
Quality of
the system: Assessing the effectiveness and reliability of system software is crucial to enhancing the efficiency and coherence of internal medical business processes [
19,
23].
The Internal Process Dimension encompasses critical elements to ensure the effectiveness of internal medical business processes within institutions. These key measurement indicators include:
- 3.
Real Control of Planning and Implementation: This involves establishing a system for real-time control of both planning and implementation processes, ensuring that activities align with organizational goals and objectives [
19,
23].
- 4.
Optimization of Unit Operational Processes: Efforts to streamline and optimize operational processes at the unit level contribute to overall efficiency and effectiveness [
19,
20].
- 5.
Innovation and social responsibility: Encouraging innovation and fostering a sense of social responsibility within internal processes are vital for adapting to changing demands and maintaining positive societal impact [
17,
20,
22].
- 6.
Regular follow-up of discharged patients: This indicator emphasizes the importance of providing ongoing support and services to patients even after they have been discharged from the hospital [
17,
22].
Without a healthy professional leader, defined policies, and criteria for staff promotion, policies, and promotions will be incomplete and staff quality will suffer. This leads to a decline in the quality of medical services and creates operational problems in medical facilities. Therefore, effective management of planning and implementation, optimization of operations, innovation, social responsibility, and continuous monitoring services are important aspects to ensure the success and sustainability of companies.Parte superior do formulário
2.1.4. The Degree of Learning and Growth
The learning and growth component focuses on the development and motivation of professionals within the organization. We aim to achieve long-term growth and improve healthcare by investing in our people, systems, and operations. Employee growth and the pharmaceutical industry is considered an important resource for the sustainable development of pharmaceutical products. The following metrics are designed to measure progress in this area:
Employee Growth (Education and Training): This indicator evaluates the improvement of the level of health knowledge of the staff through continuing professional health education [
17,
22,
23].
Organization and development of
internal staff: Signifying the presence of a comprehensive standard for employee promotion within the medical institution, this indicator ensures that employees can achieve smooth advancement through the organizational structure [
17,
20].
All fees, charges, and policies: Ensuring that the organization has well-defined and comprehensive policies related to salary and remuneration contributes to the motivation and satisfaction of internal staff [
17,
19].
Competent Managers: This indicator focuses on the presence of skilled and competent managers within the organization, crucial for effective leadership and guidance [
20].
Introduction of New Technologies: Emphasizing the adoption and integration of cutting-edge technologies within the medical profession, this indicator ensures that the organization stays abreast of advancements in healthcare [
17,
22].
In this area, staff development involves improving the level of medical knowledge of staff through continuing professional medical education. The preparation and development of internal personnel indicates the existence of standard methods of personnel promotion, which favor the progress of the company. A comprehensive approach to compensation, benefits and policies contributes to employee motivation and satisfaction. In addition, the existence of competent managers and the introduction of new technologies are important to ensure the continuous improvement and growth of the medical community in the industry.
2.2. Integration of AHP and DEMATEL
The Analytical Hierarchy Process (AHP), conceptualized by Saaty at the University of Pittsburgh,
USA in 1971 [
23] serves as a foundational tool in this study. AHP provides a nonlinear framework adept at implementing deductive and inductive thinking modes, allowing simultaneous consideration of multiple factors without relying on syllogisms. The AHP evaluation scale consists of nine levels, ranging from equal importance to extreme importance, with corresponding values of 1, 3, 5, 7, and 9 for the nominal scales, and intermediary values of 2, 4, 6, and 8 for the remaining four levels [
24].
AHP, renowned for its simplicity and steadfastness, finds application in Group interaction, decision-making systems, and the resolution of intricate decision-making problems across diverse fields, including planning, resource assessment, performance measurement, resource allocation, strategy selection, and priority setting [
24,
25].
AHP's systematic approach involves decomposing problems into dimensions and factors, assuming the independence of all dimensions or sub-standards. However, AHP is limited in its capacity to analyze causality between these dimensions. To address this limitation, this study incorporates Decision Making and Laboratory Tests and Evaluation (DEMATEL). While AHP focuses on direct correlations and relative weights, DEMATEL examines causal relationships, providing a greater understanding of the complex interactions between standards.
The DEMATEL method, first developed at the Geneva Research Center of the Battelle Memorial Institute and improved by Gabus and Fontela, has proven useful for evaluating measurements in a variety of fields. It shows relationships between factors, visualizes them as groups of factors, and creates result matrices of influencing factors. DEMATEL can group groups into cause-and-effect groups based on their impact on a specific system. DEMATEL investigates how healthcare facility performance measurements influence each other in the context of healthcare facility performance measurement and improvement [
27].
The simplicity and efficacy of DEMATEL lie in the Ability to identify causal relationships between factors and demonstrate their influence.
As AHP falls short in explaining causality, DEMATEL becomes a valuable tool for researchers, enabling the classification of Therefore, this study strategically combined the AHP, which measures the main concepts of health service performance indicators of health centers, and the DEMATEL, which evaluates the causality between these indicators.Parte inferior do formulário
AHP, as a multifaceted decision-making tool, accommodates both Financial and non-financial measurement and measurement. Introducing several quantitative criteria to follow the weighting list, provides a reasonable basis for management decision-making [
24]. A systematic comparison and evaluation of the importance between attributes is performed using a pairwise comparison, which allows us to study something as an entity and examine the interactive relationships in its hierarchical components. In a tiered system model, elements are systematically ordered according to priority weights to clearly show their contribution to risk. This makes AHP a powerful tool for addressing quantitative and multi-criteria outcomes in decision-making processes.
The AHP process divides the decision problem into subproblems in a hierarchy, determines the weights of the elements in each hierarchy, sets the order of weights in the decision plan, and creates a hierarchy. This structure shows the importance of all elements in each hierarchy. To ensure consistent conclusions, the consistency of the results was checked by the degree of consistency measured by the similarity ratio (CR). Saaty [
23] recommends a CR of 0.1 or less to meet similar requirements.
Due to its success due to its simplicity, this method has been tested in many problem areas, from simple to complex, cosmetic decisions.
2.3. Participants and Data Collection
The collection of information for this investigation targeted senior management personnel within medical institutions, encompassing individuals in key roles such as deans (those in charge), deputy deans, and directors. The data collection method employed was a questionnaire survey. Due to the challenge of obtaining a comprehensive list of all senior operational managers across medical institutions, a sample questionnaire survey was conducted specifically among senior managers with practical management experience at local hospitals, clinics, and other health centers.
Given the adoption of AHP and DEMATEL methodologies, the necessity for During data collection, several expert opinions were relaxed [
25,
28]. Therefore, 52 management-level professionals or above with extensive experience in managing medical facilities were invited to participate in the study. Contact was made by e-mail and telephone, and questionnaires and return envelopes were sent to collect operative and operative experience from local hospitals and clinics. After the collection of the questionnaires, the selected experts were contacted again by e-mail and telephone to verify their answers [
23]. Invalid interviews were defined if they did not meet the consistency coefficient criterion of 0.1 or less, or if the interviewer did not complete the questionnaire.
In particular, one of the authors involved in the question as a medical director was involved in the management and administration of seven hospitals and two clinics in Taiwan, mostly in the southern and central regions. This approach was intended to ensure a general understanding of management and control indicators related to health management and #039. We examine the causal relationship between organizational performance and relevant health service indicators. Of the 52 questions collected, 43 were considered correct. Of the 52 questionnaires collected, 43 were confirmed as valid after passing the consistency check. Among the respondents to this official questionnaire, 27 (62.8%) were men and 16 (37.2%) were women. By industry, 19 people (44.2%) are in the public sector and 24 people (55.8%) are in the private sector. Looking at the job description, 21 people (47.6%) were managers, 7 people (16.3%) were assistant managers, and 15 people (34.9%) were general managers.
Regarding experiences and experience, the distribution was as follows: 4 individuals 10 to 14 years of managerial experience (9.3%), 6 people (14.0%) and 15 to 19 years of experience, 4 people (9.3%) and 20 to 24 years of experience, 16 people (37.2%) with 25 to 29 years of experience, people with more than 30 years of management experience. 13 people (30.2%). All 43 respondents successfully passed the consistency check, making the question suitable for AHP analysis. This diverse and knowledgeable group of participants contributes to the robustness and reliability of the study and results.
3. Results
3.1. AHP Results
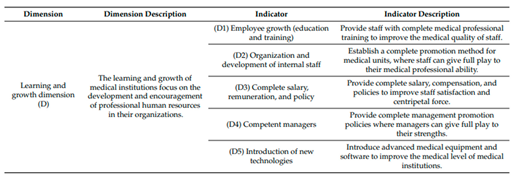
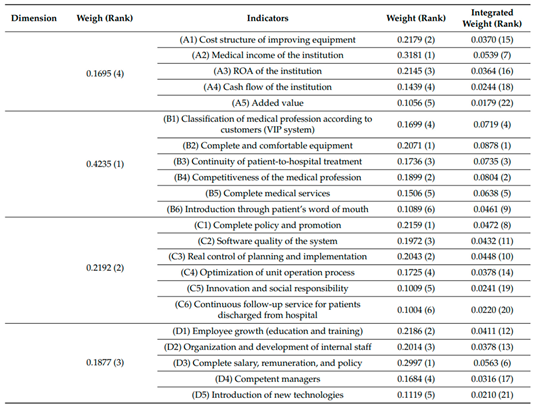
The weighted analysis and service performance measures for all aspects are shown in
Table 2. Looking at rating categories from the perspective of healthcare professionals, the customer category (0.4235) was the most important, and the internal component (0,2192) in the second. place. The education and growth sector (0.1877) ranks third in importance, while the financial sector (0.1695) ranks fourth. These weighted values provide information about the importance of each component in the context of measuring service performance.
From a financial point of view, the most important indicator of service performance is "healthy company income". in the customer's size, with the best equipment and comfort" It is the main indicator of service performance. At the internal process level, the most important service performance indicator is "Policy Completion and Promotion". It offers "remuneration, compensation and policies" in the area of learning and growth. It turns out to be the most important service performance indicator.
Many researchers have suggested that each company or industry depends on two to six factors that determine its organizational success [
24,
25]. In this regard, this study identified key service performance indicators that contribute to the success of pharmacy operations. Analyzing the results shown in
Table 2, in this study, there is little difference in all weight values between the 6th (0.0563) and the 7th (0.0539), while there is a significant difference in the 7th place. (0.0539) and 8 (0.0472). As a result, the first seven indicators of high performance of healthcare organizations were selected
: "complete and comfortable equipment," "competitiveness of the medical profession," "continuity of patient-to-hospital treatment," "classification of medical profession according to customers (VIP system)," "complete medical service," "complete salary, remuneration, and policies," and "medical incomes of institutions."
3.2. DEMATEL Results
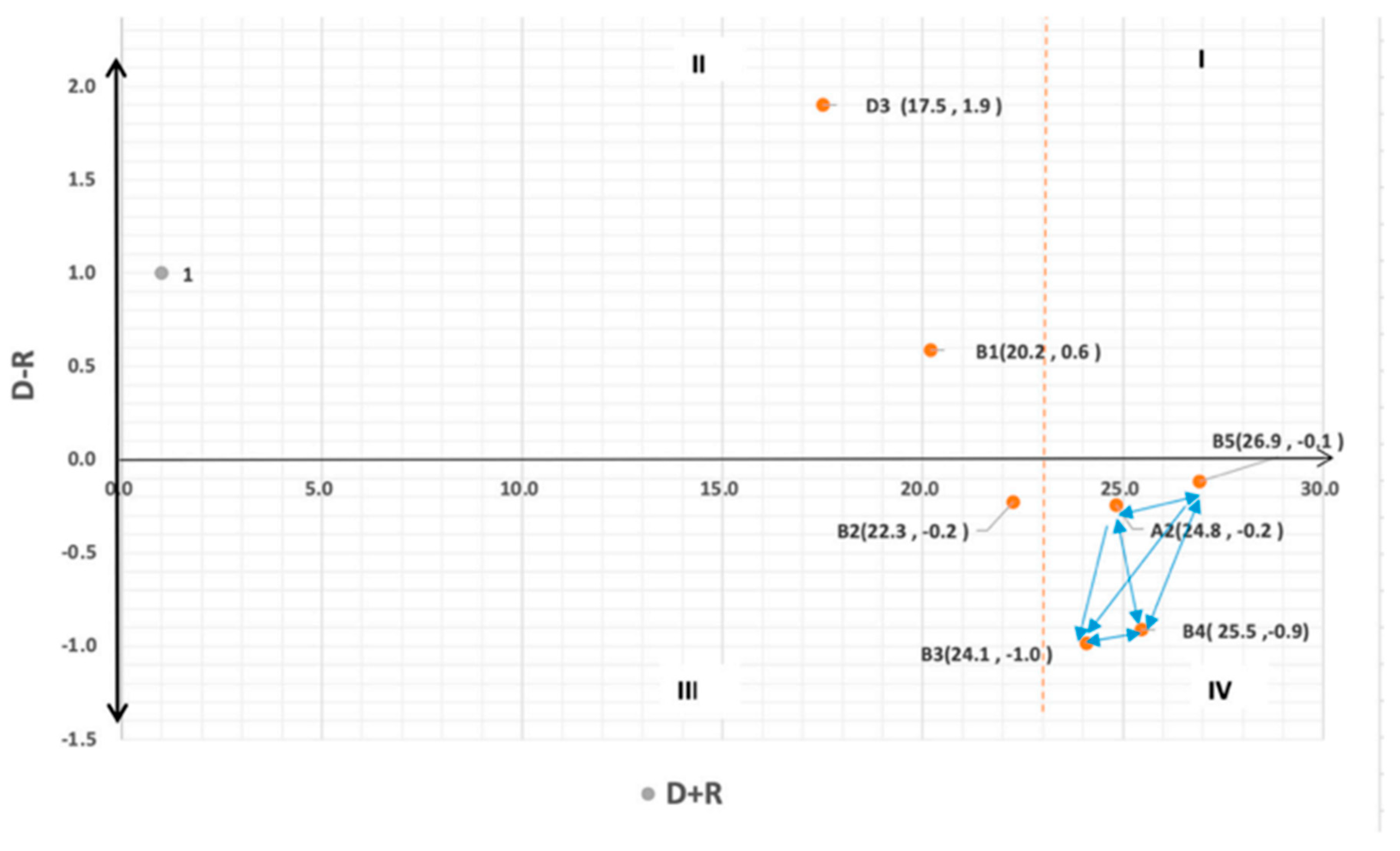
The association called D+R points out the importance of service standards in the management and operation of health facilities. Higher correlation degrees indicate greater significance of the service criteria, reflecting a higher willingness of medical institutions to enhance these criteria. In the context of the relation (D − R), a positive value designates the service criterion as a cause factor, signifying that medical institutions have substantial flexibility to adjust and improve the said criterion. The first section, which includes influential factors, identifies the main influences that require the attention of managers. The second part, which includes driving factors and characteristics, indicates the driving influence but low correlation (D + R) and high correlation (D - R). The third row, related to indicators and specific characteristics of factors, includes risk indicators with low correlation (D + R) and low correlation (D − R). The fourth quarter, contains the influence effectiveness indicators, the main indicators with a high correlation (D + R) and a low correlation (D - R).
Figure 1- presents a cause-effect diagram of seven key service performance indicators and shows the complex causal relationships between these indicators. In particular, there are four service performance indicators on the right side of D, including industry medical income (A2), continuity of patient treatment to hospital (B3), industry competition medicine (B4), and comprehensive service of health (B5). + R design case-product. The calculated D+R values for these four dimensions were higher than the average value of 23.0, indicating a high correlation compared to other service performance indicators.
Moreover, The D - R values for the classification of medical institutions by the customer (B1) with the total price and the payment policy are greater than 0, indicating their condition as a factor criterion in the cause framework. However, for indicators such as the best and most accessible equipment (B2), the medical access of the company (A2), the continuity of care from the patient to the hospital (B3), the competence of the medical industry (B4) and complete. health service (B5), D - R Values indicate a function as an effective standard in causal relationships. Indicators such as the best and available equipment (B2), the access of the medical industry (A2), the continuity of patient care to the hospital (B3), the competitiveness of the medical industry (B4) and the complete medical service (B5). D-R values greater than 0. If they are low, they fall into the category of performance-related indicators, related to activities called "effectiveness" and "effectiveness". Problems in a causal framework.
4. Debate
4.1. Key Concepts for Measuring Service Performance Based on the results of the AHP, the study determined seven key performance indicators for healthcare organizations. The following information covers these points. 4.1.1. Complete and Simple Equipment (B2) Patients indicate the importance of functional equipment in healthcare institutions, including a physical table carried by service staff to guide and reassure patients when they argue. In this way, the patient will feel comfortable and at home. Pharmacies also require efficient and clean equipment [
29]. In addition, good equipment is important to manage and manage the pharmaceutical industry [
30]. The main feature and cornerstone of a high-quality health care system in medical facilities are basic medical facilities with lighting equipment and electrical equipment. Medical equipment in today's healthcare facilities must be constantly updated as technology rapidly advances and shortens the lifespan of the equipment. Medical devices are expensive and can cost tens of millions of dollars or more. Therefore, considering investment costs and equipment upgrades is an issue for hospital managers in terms of achieving sustainable operations. Currently, the development of clinical expertise in the pharmaceutical industry is largely dependent on the development of medical devices. The modernization of pharmacy equipment is an important indicator of medical innovation. Therefore, the production and management of medical equipment has become an important part of modern hospital management. Maintaining a good operational status of the medical device management system can improve the performance and operational value of medical institutions. Hospital social benefits, economic benefit and technical feedback are the goals of hospital management. Therefore, the development of medical technology cannot be separated into two things: talent and equipment. New medical equipment is the basis for improving medical technology, and the integration of talent is an important way to improve the capabilities of all health services of medical institutions.
4.1.2. Non-Medical Competence (B4)
Patients place significant emphasis on the ethical decision-making process involving medical professionals, particularly doctors, which encompasses essential qualities such as compassion, trust, and integrity. Establishing a strong physician-patient relationship is best achieved through maximum transparency in obtaining informed consent voluntarily from patients. This involves making patients familiar with and understanding the diagnoses, treatment plans, associated risks, and prognosis. It stands as a fundamental Service performance indicator for building hope in the medical profession.
For healthcare organizations, we should focus on developing clinical technology management skills to improve the healthcare system and management. In addition, medical schools and professional institutions can contribute to the development of medical education related to the improvement of professional skills related to medicine. Measuring the quality of healthcare from the patient's perspective takes into account both functional and technical aspects. In this context, technical quality is the professional services provided by the staff, the correct diagnostic tests and the correct treatment.
Patients often require a combination of medical resources and multispecialty care, so it is important to integrate a variety of health-related resources to improve patient outcomes. Quality of life and physical well-being. Addressing gaps in service quality compared to patient expectations is essential to delivering better health services and improving the health of communities. In the context of Taiwan and medical institutions, the main challenge is not in the national health insurance system but in the system that actually provides professional health services. Improving the medical experience improves the quality of care, strengthens patient control reduces healthcare costs, and improves the quality of service provided by healthcare professionals. Finally, patients increased with the number. Satisfaction with health care.
The pharmaceutical industry is highly specialized, and quality treatment is the main goal of the management and management of the pharmaceutical industry. Elevating medical expertise within these institutions is considered the most effective approach to fostering Quality of work and efficiency. Implementing cost-effective methods to deliver high-quality personalized healthcare services is critical to generating more profit for healthcare organizations.
The overarching goals of hospitals include treating a wide range of diseases and illnesses, ultimately saving patients. Patients, when choosing a medical institution, prioritize medical expertise, followed by other factors such as relevant services and environment. Patients should understand that a facility's medical expertise, values, and goals will be heavily influenced by the facility.
4.1.3. Continuity of Patient-to-Hospital Treatment (B3)
Addressing the challenges posed by a shortage of professional human resources, strategies aimed at reducing mortality rates and improving patient follow-up rates are positioned as mutually beneficial for both medical institutions and patient loyalty. This study proposes critical 12ravelli measurements to enhance patient retention, encompassing the establishment of a simple and standardized medical monitoring system to accurately assess patients’ real conditions. Ensuring a continuous supply of medications, minimizing patients’ indirect costs (such as transportation expenses associated with 12ravelling to and from medical institutions), and strengthening the connections between medical and health services, as well as internal community engagement (community medical treatments), are identified as key initiatives [
33]. These measures collectively contribute to improving the continuity of patient-to-hospital treatment and fostering a long-term relationship between patients and medical institutions. 4.1.3. Continuity of Patient-to-Hospital Treatment (B3) Addressing the challenges posed by a shortage of professional human resources, strategies aimed at reducing mortality rates and improving patient follow-up rates are positioned as mutually beneficial for both medical institutions and patient loyalty. This study proposes critical 12ravelli measurements to enhance patient retention, encompassing the establishment of a simple and standardized medical monitoring system to accurately assess patients’ real conditions. Ensuring a continuous supply of medications, minimizing patients’ indirect costs (such as transportation expenses associated with 12ravelling to and from medical institutions), and strengthening the connections between medical and health services, as well as internal community engagement (community medical treatments), are identified as key initiatives [
33]. These measures collectively contribute to improving the continuity of patient-to-hospital treatment and fostering a long-term relationship between patients and medical institutions. 4.1.3. Continuity of Patient-to-Hospital Treatment (B3) Addressing the challenges posed by a shortage of professional human resources, strategies aimed at reducing mortality rates and improving patient follow-up rates are positioned as mutually beneficial for both medical institutions and patient loyalty. This study proposes critical 12ravelli measurements to enhance patient retention, encompassing the establishment of a simple and standardized medical monitoring system to accurately assess patients’ real conditions. Ensuring a continuous supply of medications, minimizing patients’ indirect costs (such as transportation expenses associated with 12ravelling to and from medical institutions), and strengthening the connections between medical and health services, as well as internal community engagement (community medical treatments), are identified as key initiatives [
33]. These measures collectively contribute to improving the continuity of patient-to-hospital treatment and fostering a long-term relationship between patients and medical institutions. Parte superior do formulário
4.1.3. Patient Care to Hospital (B3)
Addressing the challenges posed by a shortage of professional human resources, strategies aimed at reducing mortality rates and improving patient follow-up rates are positioned as mutually beneficial for both medical institutions and patient loyalty. This study highlights important service areas to improve patient retention, including establishing simple and standardized medication tracking systems to accurately assess patients. Actual conditions. Ensure the continuous delivery of medicines, reducing patients and; Indirect costs (eg, bringing in health facilities), strengthening links between health services and health services, and involvement within the community (community health care) were prioritized [
33]. These processes help improve continuity of care between patients and hospitals and foster long-term relationships between patients and healthcare institutions.
Patient retention in a healthcare setting is a multifaceted challenge that depends on many interrelated factors. The healthcare system and the design of a medical facility are determined to evaluate patient retention rate standards. To increase patient retention rates, health departments should be able to identify and assess the causes of illness and stop treatment at the facility [
34]. A patient-cantered approach is essential for pharmacies to create a high-quality, patient-centered healthcare system. Like companies that have shifted to a customer-oriented structure, healthcare organizations must adapt their medical facilities and services to the health status of their patients. This patient-cantered program should cover the entire spectrum of medical care, including monitoring, prevention, diagnosis, treatment, and ongoing patient care. method the key to improving the patient-cantered professional health care system is to create three values for patients, health care workers, and medical institutions. Patient participation is essential to achieving good health outcomes and the co-creation of these products and services. Professional healthcare should involve collaboration between staff and patients.4.1.4. Classification of Medicines by Client (VIP System) (B1)
Patients, as customers of healthcare services, possess certain rights and responsibilities. Among these rights is the ability to upgrade their level of medical treatment based on their economic capacity, fulfilling their desire for enhanced comfort during medical service delivery. Factors driving patients to select high-quality medical institutions include personalized care from doctors, thorough consultations, involvement in treatment decisions, proven effectiveness over time (especially for chronic conditions), prompt responses from medical personnel during procedures, comprehensive medical equipment, and five-star medical facilities. However, this upgrade often entails bearing additional costs for medical services, which patients are willing to cover, often through insurance [
35].
The VIP system for professional health services includes topics such as medicine, health, rehabilitation and nursing. In the context of the globally competitive medical service industry, institutions are encouraged not only to meet the needs of domestic citizens but also to attract international patients seeking high-quality medical services. By improving operational efficiency in medical institutions, this approach not only enhances the economic value of domestic tourism and other service industries but also contributes to the growth of international medical tourism. The rising popularity of international medical tourism underscores the significance of catering to the diverse needs of both local and foreign patients while maintaining operational excellence in medical institutions.
4.1.5. Comprehensive Health Services (B5)
The evolving landscape medical
Center has engendered a competitive environment for healthcare facilities. With patients' expectations for high-quality medical services continually rising alongside increased educational levels and community economic development, medical institutions face the imperative of establishing comprehensive service systems. This imperative stems from the need to align with patients' demands for customer-oriented, high-quality medical services. Operating within the context of expensive hospital overheads, medical institutions must strategize for survival and growth, focusing on enhancing the quality of services. The goal is to augment revenue streams derived directly from patients, who serve as both the direct and indirect sources of income through health insurance reimbursements. The symbiotic relationship between patients and medical institutions underscores the vital role of providing comprehensive medical services to not only attract patients but also ensure their satisfaction, contributing to the overall success and development of medical institutions with high-quality medical services [
37]. Patients who receive medical services will form corresponding satisfaction with the quality of medical services according to their opinions on the quality of medical services. The research result of this study revealed that there was a relationship existing between the quality of medical services and patients’ loyalty. Therefore, the improvement of the overall professional competence of medical services in medical institutions played an important role in enhancing patients’ perception of medical services. The quality of medical services had a direct influence on patients’ loyalty. This finding is consistent with previous studies. Medical services of high quality can meet patients’ various demands so as to raise their willingness to go to the hospitals for treatments [
38]. Providing medical services of good quality to gain patients’ loyalty has become a key factor for medical institutions to survive and develop. When patients need hospitalization, they will choose the hospital they trust, and such trust comes from their loyalty to hospitals and satisfaction with medical services.
4.1.6. Complete Salary, Remuneration, and Policy (D3)
Salary and remuneration play important roles in improving employees’ welfare and enhancing employees’ performance and job satisfaction. However, there are still some employees that are not satisfied with their salary and remuneration. Nonetheless, salary and remuneration are very important in the human resources management of medical institutions. Furthermore, salary and remuneration are the tools for medical institutions or enterprises to bind themselves with their employees and the factors to drive employees to work hard and increase their satisfaction. In addition, salary and remuneration have a very important impact on organization operations. The use of human resources and the salary and remuneration policy of medical institutions with high efficiency allows medical institutions to achieve stable and growing performance and income. A successful salary and remuneration policy can automatically enhance employees’ work performance and create harmonious cooperation, which satisfies all parties [
39]. Therefore, the management of medical institutions must establish sound salary and remuneration policies and provide employees with allowances to stimulate employees’ working enthusiasm. Meanwhile, medical institutions should strengthen the communication between the management and employees through clear SOP, especially in terms of using the salary and remuneration policy as a tool to stimulate employees’ working enthusiasm.
4.1.7. Household Medical Income (A2)
The financial stability of medical institutions is crucial for their sustained operations and the provision of high-quality healthcare. Medical incomes, as a significant factor in the operation of institutions, directly influence the decisions made by medical institutions regarding the execution of relevant treatment departments and the practical treatment choices offered. The question of whether medical institutions should generate profits is framed within the broader goal of saving lives and enhancing patient health. To achieve this mission, medical institutions need continuous investment in updating medical equipment, improving the proficiency of medical professionals, and adopting new medical expertise. These endeavors require financial surplus, emphasizing the importance of medical incomes for the overall functioning and development of medical institutions.
4.2. Factors in Measuring Service Performance
DEMATEL results provide insight into the relationships between the seven key service performance indicators. The management and control of the health care industry is a great challenge in the context of dynamic changes in the health care environment and the competitive environment, especially under Taiwan and the international budget system for national health insurance. A successful leader must have a deep understanding of the basic concepts related to the administration and management of medical facilities and the application of related concepts to practice.
In the competitive medical market of Taiwan, emphasis must be placed on certain medical service performance indicators to achieve effective improvements and enhance institutional competitiveness. The cause–effect diagram, where D + R represents the correlation degree, indicates the importance of selected service performance indicators in the operation and management of medical institutions. Higher correlation degrees signify greater significance, indicating institutions' higher willingness to improve these indicators.
Based on the relationship (D+R), the most important is that the service performance indicators such as the medical revenue of the department (A2), the continuity of patient care to the hospital (B3) and the competence in the medical field. field will be better than the first. (B4), full healthcare (B5). A positive correlation value (D - R) indicates these parameters as a reference standard, allowing for easy adjustments and improvements.
Among the seven indicators, two were identified as causal criteria: the classification of health posts by the consumer (B1) and the payment and payment policy. This allows pharmaceutical companies to adapt more easily. The partnership (D + R) indicates comprehensive health care (B5) as the most important indicator, but it is less expensive in terms of payment and payment policy.
Analyzing the direction of the arrow in the causal relationship design, health service (B5) was found to have a significant effect on pharmaceutical industry competition (B4), pharmaceutical industry revenue (A2) and patient continuity. -Hospital treatment (B3). As a sign and true relationship, the improvement of the comprehensive health service (B5) emerges as a priority for those responsible for health departments. Improvements in this area are expected to have a positive impact on the continuity of patient care for the hospital (B3), the competitiveness of the healthcare industry (B4), and the agency's healthcare costs (A2). Therefore, fixing and improving comprehensive healthcare services (B5) turns out to be the most important task for medical facility managers.
4.3. Limitations and Suggestions
A questionnaire was adopted in this study. The weight ranking and influence degree of the dimensions and service criteria were based on the opinions of the persons in charge of the operation and management of medical institutions. The present study took medical institutions in Taiwan as research objects. One limitation of this study is the restricted external validity as the sample frame is restricted to medical institutions in Taiwan. Making generalizations about the priority and causality of service performance indicators in other countries based on the present research findings may not be appropriate without further research. Future research can extend and replicate the current study in more countries. Furthermore, this study proposed 22 indicators to build the service performance measurements of medical institutions. We did not take the medical institution types into account in the current study. Medical institutions can be categorized into different types, e.g., public and private sectors; large, medium, and small hospitals. Future research can extend and replicate the current study to investigate the differences in the priority and causality of service performance indicators among different types of medical institutions.
5. Result
In summary, this study has made significant strides in understanding Service performance indicators of health facilities. By meticulously reviewing the literature, the study established four dimensions and identified 22 service performance indicators. Using AHP and DEMATEL methods, we created a questionnaire shipping medical center.
Customer Dimension Dominance: The AHP results underscore the paramount importance of the customer dimension in studying service performance indicators for medical institutions. Among the four dimensions, the customer dimension emerged as the most critical, aligning with the patient-oriented focus of medical institutions.
Critical Factors: Seven pivotal factors influencing medical service performance indicators were identified: "complete and comfortable equipment," "competitiveness of the medical profession," "continuity of patient-to-hospital treatment," "classification of medical profession according to customers (VIP system)," "complete medical service," "complete salary and remuneration policy," and "medical incomes of institutions."
Patient-Oriented Competitiveness: To foster competitiveness, medical institutions must maintain a patient-oriented approach, possess advanced medical equipment, deliver comprehensive medical services, and have competitive medical personnel. Additionally, a robust salary and remuneration policy is crucial for retaining qualified medical personnel, ensuring patients' comfort and loyalty.
Win-Win Outcome: The study advocates a patient-centric strategy, emphasizing that when patients feel at home and continue seeking treatment at medical institutions, overall income and the quality of medical services experience comprehensive enhancement, resulting in a win-win outcome.
Complete Medical Service as Critical Indicator: DEMATEL results and cause–effect diagrams revealed that complete medical service exerts the most significant influence on the competitiveness of the medical profession, medical incomes of institutions, and continuity of patient-to-hospital treatment. It is identified as the most critical service performance indicator demanding attention and improvement by medical institution managers.
6. Methodological Contribution: This study contributes to the literature by integrating AHP and DEMATEL methods and balanced scorecard theory to create a robust service performance measurement system that invests in healthcare facilities. While the study provides valuable insights, acknowledging its limitations, future research should aim to enhance generalizability and applicability by exploring diverse geographic regions and considering variations among different types of medical institutions.
Previous research on hospital supply chain performance has attempted to measure hospital supply chain performance either through performance indicators or by measuring the performance of specific functions. The purpose of this work is to measure the performance indicators of the hospital's internal supply chain to find their interdependencies, to understand the relationship between them and to identify key performance indicators for each aspect of the logistics process.
To assess, measure, and analyse internal treatment aspects, this study suggests a methodical analytical approach. The proposed method combines the group method of decision-making Experimental Evaluation Laboratory (DEMATEL) and rough set theory.
The results of the study indicate that the most critical aspects of hospital supply chain performance are continuity of care, timing of the clinical care process, and absence or delay of care.
De material causality can advise managers to first consider the timing of the clinical care process and related aspects of patient safety such as errors to improve the integrity of care to patient safety. free of charge, the productivity of clinical treatment should also be improved, etc. Improving these aspects also improves the other aspects to which they relate.
References
- Mainz J. Defining and classifying clinical indicators for quality improvement. Int. J. Qual. Health Care. 2003;15:523–530. [CrossRef]
- Weir E., d’Entremont N., Stalker S., Kurji K., Robinson V. Applying the balanced scorecard to local public health performance measurement: Deliberations and decisions. BMC Public Health. 2009;9:127. [CrossRef]
- Rogers A.E., Hwang W.T., Scott L.D., Aiken L.H., Dinges D.F. The working hours of hospital staff nurses and patient safety. Health Aff. 2004;23:202–212. [CrossRef]
- El-Jardali F., Saleh S., Ataya N., Jamal D. Design, implementation and scaling up of the balanced scorecard for hospitals in Lebanon: Policy coherence and application lessons for low and middle income countries. Health Policy. 2011;103:305–314. [CrossRef]
- Zhang L., Liu R., Jiang S., Luo G., Liu H.C. Identification of key performance indicators for hospital management using an extended hesitant linguistic DEMATEL approach. Healthcare. 2020;8:7. [CrossRef]
- Soysa I.B., Jayamaha N.P., Grigg N.P. Developing a strategic performance scoring system for healthcare nonprofit organisations. Benchmarking. 2018;25:3654–3678. [CrossRef]
- Christiansen T., Vrangbæk K. Hospital centralization and performance in Denmark—Ten years on. Health Policy. 2018;122:321–328. [CrossRef]
- Behrouzi F., Ma’aram A. Identification and ranking of specific balanced scorecard performance measures for hospitals: A case study of private hospitals in the Klang Valley area, Malaysia. Int. J. Health Plan. Manag. 2019;34:1364–1376. [CrossRef]
- Smith P., Mossialos E., Papanicholas I. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge University Press; New York, NY, USA: 2008.
- Jiang S., Shi H., Lin W., Liu H.C. A large group linguistic Z-DEMATEL approach for identifying key performance indicators in hospital performance management. Appl. Soft Comput. 2019;86:105900. [CrossRef]
- Abujudeh H.H., Kaewlai R., Asfaw B.A., Thrall J.H. Quality initiatives: Key performance indicators for measuring and improving radiology department performance. Radiographics. 2010;30:571–580. [CrossRef]
- Vesty G., Brooks A. St George hospital: Flexible budgeting, volume variance, and balanced scorecard performance measurement. Issues Acc. Educ. 2017;32:103–116. [CrossRef]
- Aidemark L.G. The meaning of balanced scorecards in the health care organization. Financ. Account. Manag. 2001;17:23–40. [CrossRef]
- Northcott D., France N. The balanced scorecard in New Zealand health sector performance management: Dissemination to diffusion. Aust. Account. Rev. 2005;15:34–46. [CrossRef]
- Kaplan R.S., Norton D.P. The Balanced Scorecard—Measures that drive performance. Harv. Bus. Rev. 1992;70:71–79.
- Kaplan R.S., Norton D.P. The Balanced Scorecard: Translating Strategy into Action. Harvard Business School Press; Boston, MA, USA: 1996.
- Yaghoobi T., Haddadi F. Organizational performance measurement by a framework integrating BSC and AHP. Int. J. Prod. Perform. Manag. 2016;65:959–976. [CrossRef]
- Kober R., Northcott D. Testing cause-and-effect relationships within a balanced scorecard. Account. Financ. 2021;61:1815–1849. [CrossRef]
- Perez C.A., Montequin V.R., Fernandez F.O., Balsera J.V. Integrating analytic hierarchy process (AHP) and balanced scorecard (BSC) framework for sustainable business in a software factory in the financial sector. Sustainability. 2017;9:486. [CrossRef]
- Janeš A., Kadoić N., Begičević Ređep N. Differences in prioritization of the BSC’s strategic goals using AHP and ANP methods. J. Inf. Organ. Sci. 2018;42:193–217. [CrossRef]
- Noori B. Prioritizing strategic business units in the face of innovation performance: Combining fuzzy AHP and BSC. Int. J. Bus. Manag. 2015;3:36–56. [CrossRef]
- Lee A.H.I., Chen W.C., Chang C.J. A fuzzy AHP and BSC approach for evaluating performance of IT department in the manufacturing industry in Taiwan. Expert Syst. Appl. 2008;34:96–107. [CrossRef]
- Saaty R.W. The analytic hierarchy process: What and how it is used. Math. Model. 1987;9:161–176. [CrossRef]
- Ho W. Integrated analytic hierarchy process and its applications: A literature review. Eur. J. Oper. Res. 2008;186:211–228. [CrossRef]
- Ho W., Ma X. The state-of-the-art integrations and applications of the analytic hierarchy process. Eur. J. Oper. Res. 2018;267:399–414. [CrossRef]
- Gabus A., Fontela E. World Problems, an Invitation to Further Thought within the Framework of DEMATEL. Battelle Geneva Research Centre; Geneva, Switzerland: 1972.
- Si S.L., You X.Y., Liu H.C., Zhang P. DEMATEL technique: A systematic review of the state of the art literature on methodologies and applications. Math. Probl. Eng. 2018;1:3696457. [CrossRef]
- Glaize A., Duenas A., Di Martinelly C., Fagnot I. Healthcare decision-making applications using multicriteria decision analysis: A scoping review. J. Multi-Criteria Decis. Anal. 2019;26:62–83. [CrossRef]
- Derriennic J., Barais M., Le Goff D., Fernandez G., Le Borne F., Le Reste J. Patient, carer and healthcare professional experiences of complex care quality in multidisciplinary primary healthcare centres: Qualitative study with face-to-face, in-depth interviews and focus groups in five French multidisciplinary primary healthcare centres. BMJ Open. 2021;11:e050165.
- Miller W.R. Patient-centered outcomes in older adults with epilepsy. Seizure. 2014;23:592–597. [CrossRef]
- Walsh G., Hayes B., Freeney Y., McArdle S. Doctor, how can we help you? Qualitative interview study to identify key interventions to target burnout in hospital doctors. BMJ Open. 2019;9:e030209. [CrossRef]
- Sharifi T., Hosseini S.E., Mohammadpour S., Javan-Noughabi J., Ebrahimipour H., Hooshmand E. Quality assessment of services provided by health centers in Mashhad, Iran: SERVQUAL versus HEALTHQUAL scales. BMC Health Serv. Res. 2021;21:397. [CrossRef]
- Harries A.D., Zachariah R., Lawn S.D., Rosen S. Strategies to improve patient retention on antiretroviral therapy in Sub-Saharan Africa. Trop. Med. Int. Health. 2010;15:70–75. [CrossRef]
- Brown H.J., Andreason H., Melling A.K., Imel Z.E., Simon G.E. Problems with using patient retention in the evaluation of mental health providers: Differences in type of dropout. Psychiatr. Serv. 2015;66:879–882. [CrossRef]
- Bucatariu L., George B.P. Patient perception and choice factors related to international hospitals: A study in Ho Chi Minh City, Vietnam. J. Health Med. Inf. 2017;8:3. [CrossRef]
- Purwatiningrum F. Analysis of factors affecting BPJS patients choosing a class of care to VIP room. J. Qual. Public Health. 2019;3:112–121. [CrossRef]
- Putri A.D., Aulia D. Analysis quality of specialist doctor services and patient satisfaction at H. Abdul Manan Simatupang Hospital in Kisaran Regency. Int. Arch. Med. Sci. Public Health. 2020;1:62–72.
- Yu Y., Chen Z., Zhao Y., Wang Y., Zhang R., Zhou X. Medical service quality, psychological contract, and patient loyalty: An empirical study among patients in China. Medicine. 2020;99:E21079. [CrossRef]
- Permana I., Bharoto H. Remuneration to improve employee performance at waled regional hospital, Cirebon regency. Int. J. Res. Bus. Soc. Sci. 2021;10:163–169. [CrossRef]
- Bäuml M., Dette T., Pollmann M. Price and income effects of hospital reimbursements. J. Health Econ. 2022;81:102576. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).