1. Introduction
The strabismic disease is a misalignment of the eyeballs covering a heterogeneous group of eye movement disorders characterized by permanent or temporary deviation [
1,
2,
3,
4]. Strabismus occurs in 4-6% of the population worldwide, with little geographic variation, in both children and adults, with the same frequency in both women and men [
3,
5]. Findings have shown that the strabismic disease occurs in 65% by the age of 3 and is one of the most common visual disorders in preschool children [
6]. Proper measurement of the type and magnitude of eye deviation is essential for proper diagnosis, observation, and treatment of strabismus [
7,
8].
Strabismus may be intermittent or constant. It could be defined by diction of deviating eye into esotropia (inturning deviation), exotropia (out-turning deviation) or, less commonly, hypertropia (upturning deviation), hypotropia (downturning deviation) and cyclotropia (rotatory deviation) [
9].
The undetected and untreated strabismic disease leads to varying degrees of reduced stereoscopic vision and the development of amblyopia in the eye where strabismus is consistently present. It can also lead to postural disorders and torticollis, accompanied by spinal pain, mainly in the cervical region, which can lead to further long-term orthopedic complications. The condition reduces the quality of life and impairs daily functioning [
10].
There are few treatment techniques depending on type and magnitude of deviation and age of the patient. Surgery with adjustable and nonadjustable suture could provide successful motor alignment outcomes in the majority of cases [
11]. Another method is prism correction which can be considered as initial management in patients with a wide range and variety of etiologies of ocular deviations, including larger and mixed strabismus [
12].
1.1. Traditional Methods Assessment
The basic manual methods for diagnosing the strabismic disease are the Hirschberg test, the Krimsky test, the cover-uncover test, and the prismatic cover-uncover test. The Hirschberg test assesses the parallel alignment of the eyeballs based on the location of reflections on the surface of the illuminated corneas. The Krimsky test is a modification of the Hirschberg test, adding prisms in the visual axis which allows quantitative measurement of the amount of deviation for both near and far [
13]. Both tests are considered the gold standard for testing eye alignment in uncooperative individuals, i.e. infants or people with mental disabilities [
14,
15]. The results of both Hirschberg and Krimsky tests performed depend on the subjective judgment of the examiner and are much less accurate than the other available strabismus angle tests, even when performed by experienced strabologists [
16,
17]. Currently, the gold standard for assessing eye deviation is the cover-uncover test and the prismatic cover-uncover test in which prism bars are additionally used. These tests should be performed for both near and far. These tests are time-consuming, and differences in measurements made by other researchers can be as high as 10DP [
18,
19].
Prism bars are commonly used in ophthalmology and orthoptic offices to determine the strength of the corrective prism values by performing a prismatic cover test (PCT). When assessing eye deviation to the distance, the patient fixes his or her gaze on an object at a distance of 6 meters, which requires a large space in the office [
20]. This test can be unreliable due to the fact that it requires the examiner to simultaneously cover the patient's eye, hold the prism bar, visually observe eye movements, and correct the patient's posture. Another complication of the PCT examination is the detection of the moment of stopping eye movement, which is particularly difficult when there are numerous reflections in the refractive glasses and prism bars. This is most often related to the unsuitable positioning of the examination chair in relation to the room lighting, over which the examiner has little influence. The manual occluder does not completely block the light entering the eye and part of the periphery of the field of view (FoV) may result in partial recovery of the binocular fusion. The strabismus examination involves the cooperation of the patient, remaining in a stable and fixed position for a long time, and, in the case of complex vertical and horizontal or oblique strabismus or uncooperative patients, requires the help of additional persons for head stabilization or handling of additional prism bars. The accuracy of the examination is significantly reduced for large deviation values due to the variable resolution of the prism bars. The interval between prism power values is 1PD in the 1-10DP range, then 2DP in the 10-20DP range, and as much as 5 DP at higher values. In the PCT test, the prism bars should be aligned perpendicular to the optical axis of the eye in all planes, which again requires the experience of the examiner and is not verified in any way. The bars have no indicators of correct alignment, and the greater the deviation, the greater the measurement error. The skill and experience of the examiner and such factors as the psychophysical condition of the examiner and the patient, time of day, or coexisting diseases such as developmental disability play a significant role [
20]. The difficulty of the tests performed and the role of the examiner's experience is evidenced by the development of a virtual reality strabismus angle assessment training application, the use of which significantly improves the examiner's accuracy and efficiency [
21].
An optical-mechanical synoptophore is also used to measure strabismic angles [
22]. This device consists of two rotating optical tubes, which are attached to the patient's eyes and display two complementary static images. As a result of the appropriate positioning of the tubes by the examiner or the patient himself, it is possible to combine the images into one image. At the same time, as the tubes progressively rotate, the images are alternately blanked out, forcing the patient's eyes to adjust. The optometrist evaluates the strabismic angle at far and near fixation distance, based on the visual assessment of the adjustment movements and the actual angles of rotation of the tubes (read from the scale or digital encoders). The synoptophores are complicated to use and require a great deal of experience for the examiner, and the results depend on the psychophysical condition and subjective vision of the patient. In addition, numerous reports have been made by doctors and optometrists that there are problems with the evaluation of the strabismic angles in distant vision, especially the overestimation of the angles in convergent strabismus, and the underestimation of the angles in divergent strabismus.
Advanced autorefractometers have implemented the strabismic angle measurement by measuring corneal reflectance on the pupil area (e.g. PlusOptix). In a simplified form, this measurement is carried out manually by optometrists using a point light source held at a distance from the patient's head, called the Hirshberg test [
23]. The location of the reflections allows only a preliminary diagnosis of the strabismus type and the deviation values.
1.2. Scientific Articles
Researchers around the world are working to develop new devices to diagnose the strabismic disease more accurately and quickly [
24,
25,
26,
27,
28,
29,
30,
31,
32]. Numerous scientific articles report methods for the estimation of strabismus angles based on the analysis of reflections on the pupil area, reflections from the cornea and deeper layers, and those based on the shape of the pupil in camera images.
However, in our opinion, these methods are unreliable because they do not take into account the real path of light from the observed object to the macula on the retina, often far from the ideal anatomy of the eye, even though the Kappa angle is estimated. Both methods can only provide a preliminary estimate of the diagnosis showing the presence and type of strabismus.
To the best of our knowledge, the state of the art does not know of any means or devices functionally and technically similar to the solution presented in this paper.
2. Materials and Methods
2.1. Device Information
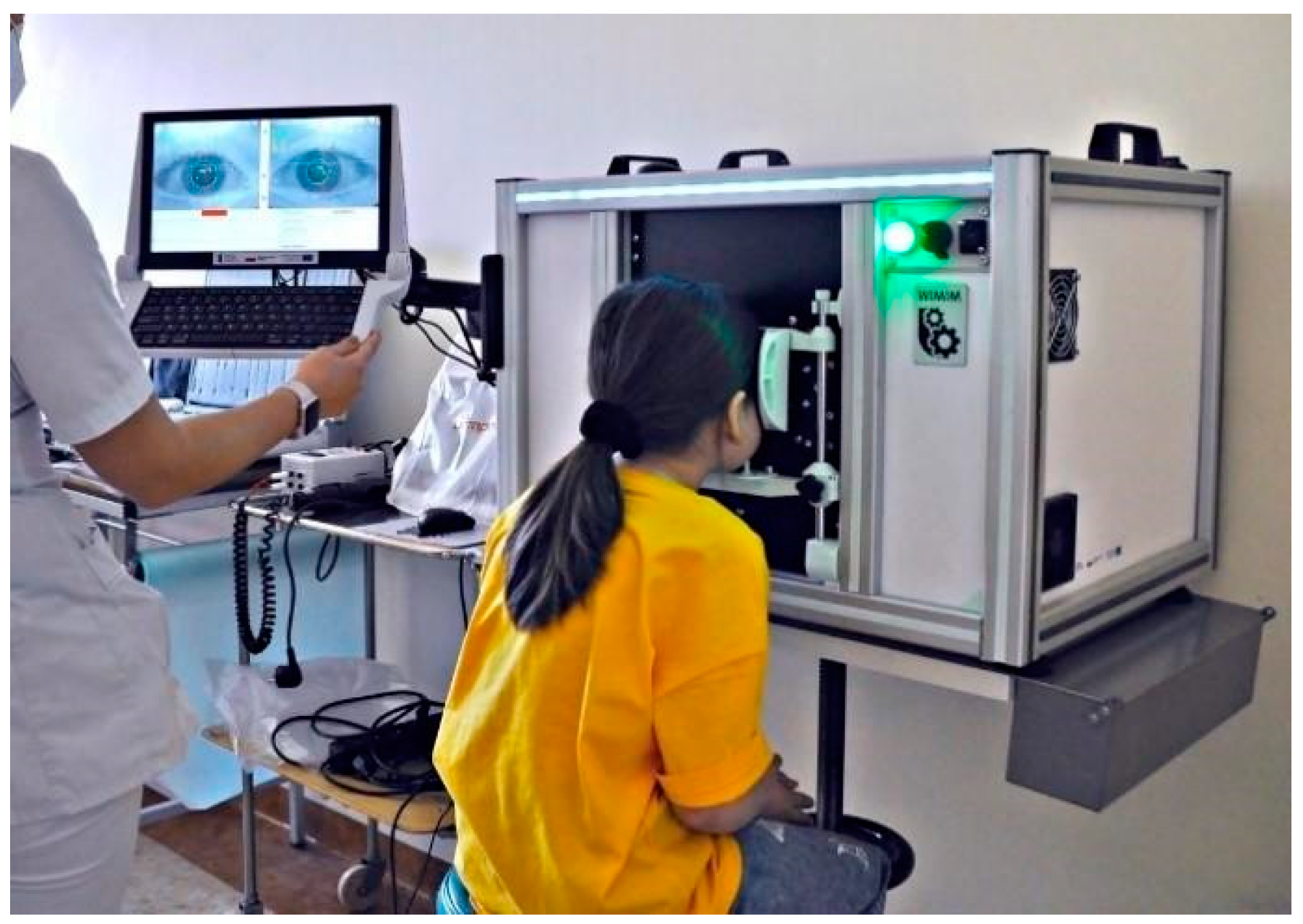
Our proposed device, called Strabiscan, was developed in a technology demonstrator form at the 2nd Department of Ophthalmology of the Pomeranian Medical University, Szczecin, Poland. The device performs fully automatic measurements of strabismus angles with a resolution of 0.1 DP of the vertical and horizontal deviation of the eyeballs at near and far fixation. The Strabiscan device uses an advanced mathematical model of FoV and a very accurate eye tracking system to determine strabismus angles, taking into account individual characteristics of a patient, i.e. pupil distance as well as distortions of the FoV, caused by correction lenses (
Figure 1 and
Figure 2). The device was developed as part of the mini-grant Innovation Incubator 4.0, funded by the European Union.
2.2. Construction of the Device
The device, like many other ophthalmic devices, is stationary and integrated into a single housing. When seated, the patient rests his head and chin on a suitably contoured and permanently fixed frame. In addition, the design of the frame minimizes the amount of scattered ambient light falling onto the retina, making it easier to break up the binocular fusion.
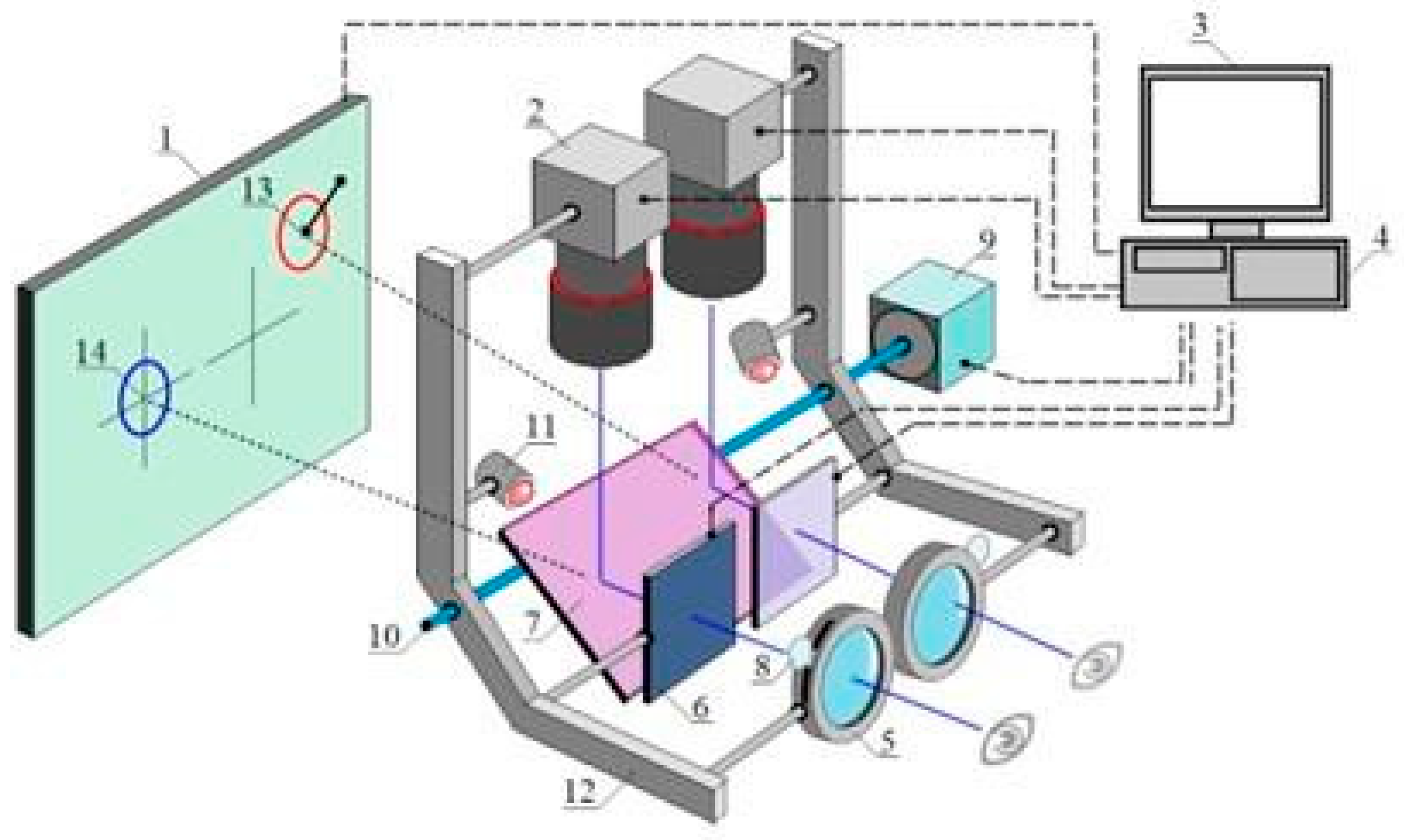
Figure 3.
Schematic concept of the device. The numbers are labeled consecutively: 1) fixation points display screen, 2) NIR camera, 3) operator control panel, 4) PC, 5) adapter for trial lenses, 6) LCD shutters, 7) hot mirror, 8) trial lens, 9) drive system allowing the optics to be adjusted to the patient's pupil distance, 10) mechanism moving left and right optical module, 11) NIR LED illuminator, 12) movable fixing element for optical components, 13) fixation points for the non-fixing eye, 14) fixation points for the fixing eye.
Figure 3.
Schematic concept of the device. The numbers are labeled consecutively: 1) fixation points display screen, 2) NIR camera, 3) operator control panel, 4) PC, 5) adapter for trial lenses, 6) LCD shutters, 7) hot mirror, 8) trial lens, 9) drive system allowing the optics to be adjusted to the patient's pupil distance, 10) mechanism moving left and right optical module, 11) NIR LED illuminator, 12) movable fixing element for optical components, 13) fixation points for the non-fixing eye, 14) fixation points for the fixing eye.
The pupil distance can be set from 53 to 82 mm and is taken into account when setting the following fixation points positions on the test screen, increasing the reliability of the results in both children and adults. The test screen was installed behind the optomechanical modules and in front of the patient's eyes at a distance of 400 mm.
The physical size of the screen workspace allows a large part of the patient's FoV (70° horizontally and 40° vertically) to be covered during the examination. The patient looking straight through the hot mirror receives an image of the test screen in the visible band, while the image of the eye illuminated by the infrared LEDs is reflected by the mirror towards the cameras. A highly detailed image of the pupil is obtained, which enables an algorithm to detect adjusting movements of less than 0.2mm, difficult to observe during a traditional PCT examination.
2.3. Fundamentals of Measurement Techniques
The device performs an automated measurement simulating PCT. During the measurement, alternating and cyclic LCD shutter switching is performed and the fixation point is displayed for the left or right eye exclusively so that binocular vision is permanently switched off. In place of traditional prism bars that deflect the visual path, the device uses algorithms that simulate their operation and move the fixation point on the test screen surface. Patient cooperation is reduced to following and focusing the eye on the fixation point, which changes its position each cycle. The cameras capture and the computer analyses the intensity of the adjusting movements of the uncovered eyeballs. For the last position of the moving fixation point, the vertical and horizontal observation angles are determined. The device measures total strabismus angle, encompassing both latent and manifest components.
2.4. Measurements
For the purpose of evaluating the usefulness of the device, 30 patients aged 5–52 years with the manifest strabismic disease were tested with the Strabiscan device and with the prismatic cover-uncover test. The control group consisted of 30 healthy subjects (aged 5–25 years). The inclusion criteria for the study were: manifest horizontal strabismus and age 5–75 years. On the other hand, exclusion criteria were mental or physical impairment disallowing cooperation during the test, age <5 years, age >75 years, refractive defect > ±10D, other eye disease disabling fixation, systemic disease hindering the test, and low visual acuity (<0.1Sn).
The study received a positive opinion from the Bioethics Committee at the Pomeranian Medical University (KB-0012/199/2020). The study protocol followed the tenets of the Declaration of Helsinki. Each study participant gave written permission to participate in the study.
A detailed history was taken in all patients, and routine ophthalmic examinations were performed, including best-corrected visual acuity to the distance on Snellen charts (fixation points with numbers or pictures, depending on age). Each patient then underwent a prismatic cover-uncover test. The next test was the evaluation of the strabismus angle using the Strabiscan device. The final examinations were the evaluation of refractive error using an autorefractometer (Topcon KR-800, Tokyo, Japan, or Retinomax Righton) after cycloplegia with a drop of 1% cyclopentolate, and biomicroscopic evaluation of the anterior segment of the eye and evaluation of the fundus by indirect ophthalmoscopy using a Volk90D lens or with a Fison ophthalmoscope and a Volk20D lens.
PCT test was done by two examiners: EG and MD- ophthalmology residents after pediatric ophthalmology training. The interoperator differences never exceed 5DP. The procedure started with 5-minutes one eye occlusion. The test was done with the use of opaque occluder.
In the proposed device, the appropriate set of the trial lens was installed and the patient, after stabilizing his head, was asked to observe the fixation point on the screen. The device calculated the trial lens for the far distance test according to the results entered into the system from the previous refraction measurement, adding a correction to compensate for the distance between the screen and the patient's eyes (typically +2.5D for a distance of 0.4m). Since the head was placed on the device and until the first test started, the patient could observe the background image monocularly on the screen. In this way, breaking of binocular fusion was induced in the patient, crucial for relaxing the vision and obtaining a correct measurement result.
First, the device performed an automatic pupil-distance test, which involved the patient observing fixation points displayed sequentially exactly in front of the left eye and then in front of the right eye. During this time, the optical system adjusted its position so that the central point of the pupil was exactly halfway across the width of the images obtained from the cameras. Then, a strabismus angle test was performed at far fixation and then at near fixation distance, involving the patient's observation of fixation points moving automatically on the screen in the vertical and horizontal directions. During the alternating cover-uncover of the eyes, the system was analyzing the adjusting movements of both eyes. For the near test, this correction was not applied. Three to five measurements within one type of test were taken at a time, depending on the patient's ability to cooperate with the device. A single measurement usually takes between 10 and 30 seconds.
During the test, the patient was asked to stay in a possibly stable position. Any slight movement of the patient’s head could have been interpreted by the device as the adjusting movement of the eye and could prevent an automatic completion of the test. This condition was particularly important in pediatric patients. Between measurements, the patient was also asked to keep his head at the device, except when replacing trial lenses.
3. Results
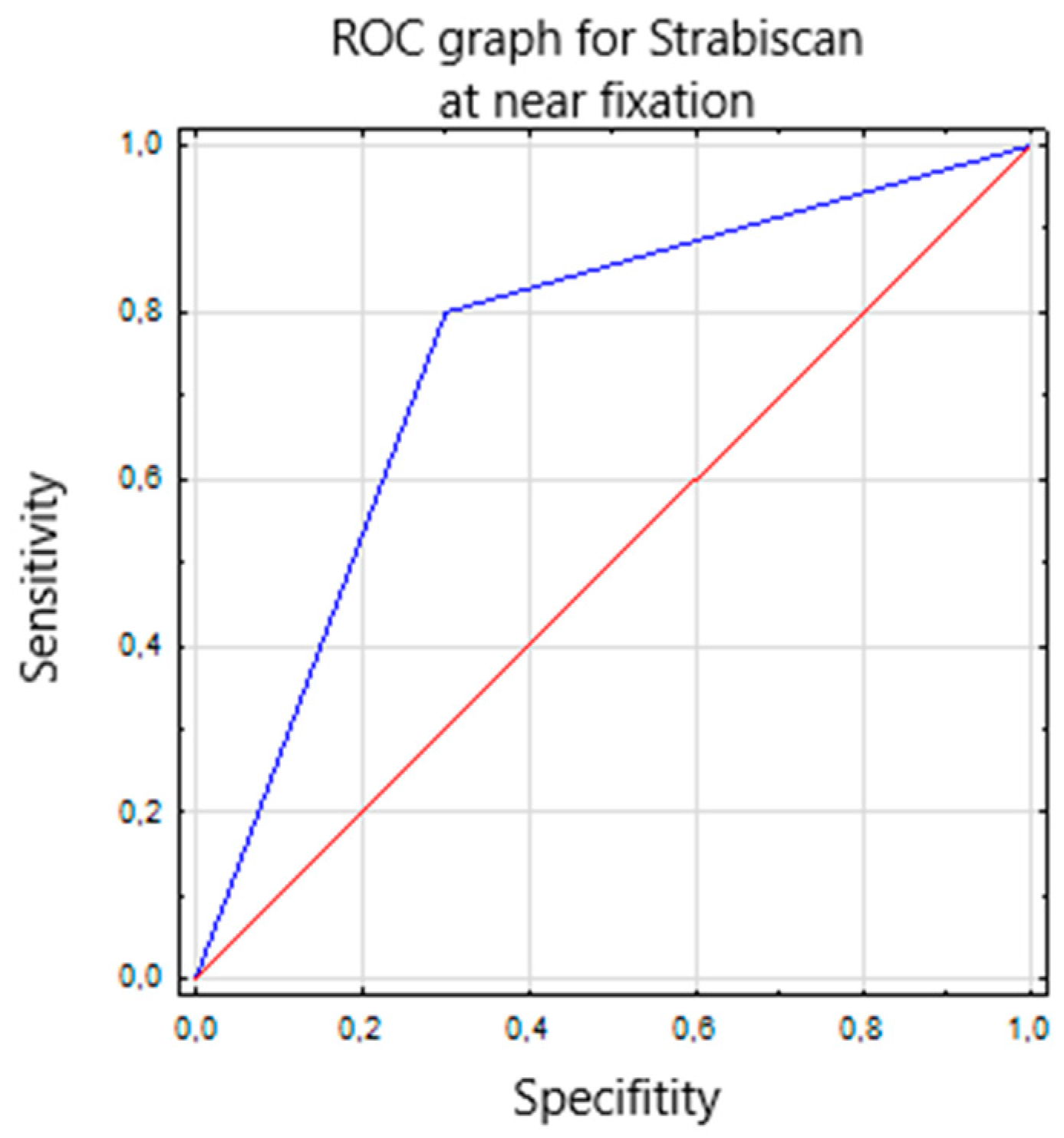
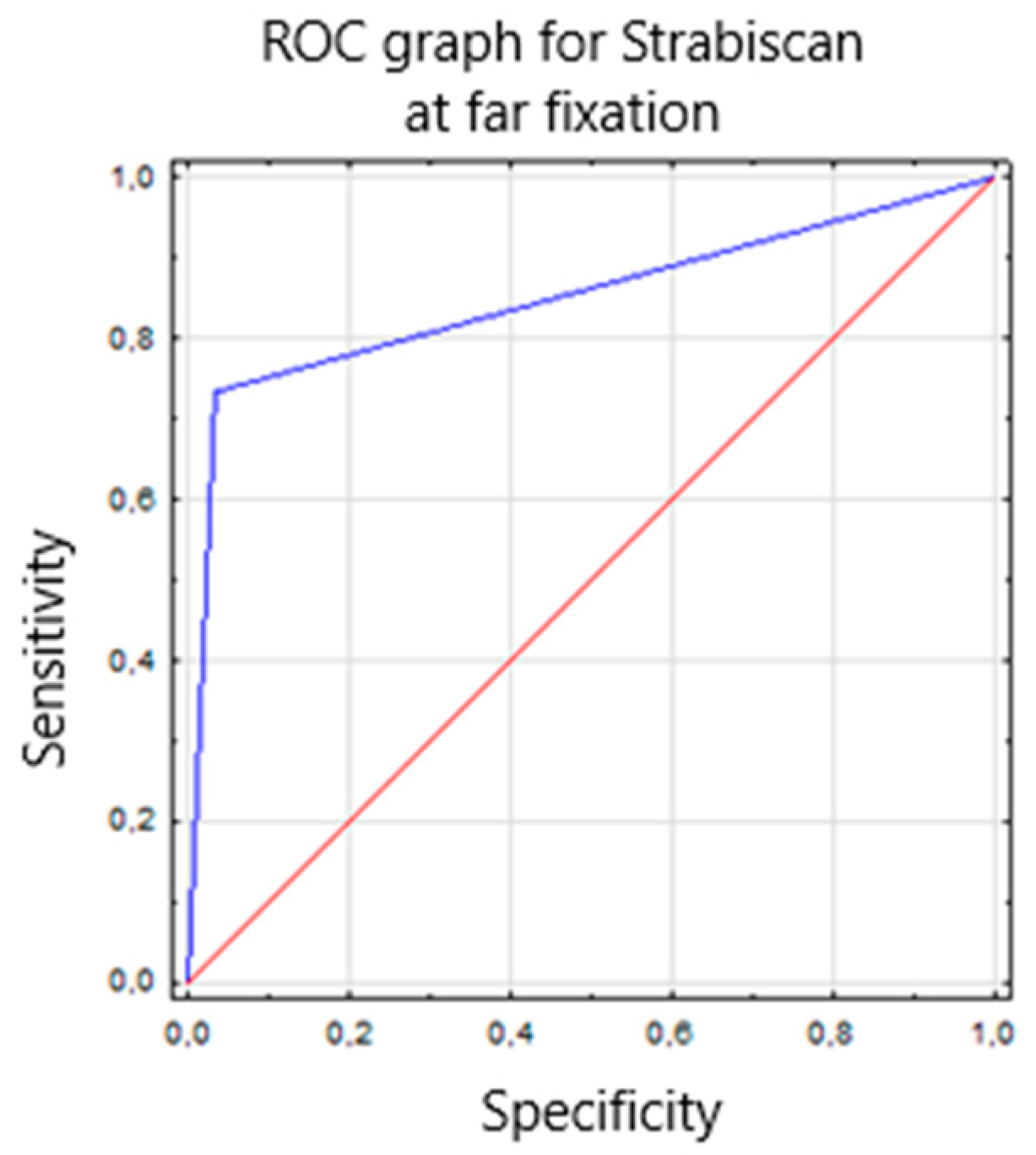
Characterization of the collected patient features was carried out using descriptive statistics such as mean, standard deviation (SD), minimum and maximum values, as well as counts and percentages. Compliance with the normal distribution of continuous variables was checked with the W Shapiro-Wilk test. Comparisons of test values, separately at near and far fixation, between devices, and comparison of test annoyance between them, were made using the Mann-Whitney U test. A Receiver Operating Characteristic (ROC) curve was calculated based on the near and far examination results from each device to compare the diagnostic capabilities of the devices. Parameters such as sensitivity, specificity, and area under the ROC curve – AUC (area under the curve) – were calculated. In addition, the concordance of results from the two devices was compared using Cochran's Q test. Results were considered statistically significant at p<0.05.
Basic patient demographics are shown in
Table 1. The study group included 30 patients with manifest strabismus, while the second group included 30 healthy subjects without manifest strabismus. The measurements taken were compared to the traditionally used alternating cover-uncover test using a prism bar, and a 55% concordance of positive results and a 45% concordance of negative results for distance were obtained. At near fixation, the percentage of positive results was concordant at 38.3% and negative at 61.7%. The device correctly detected strabismus in all subjects, as well as detecting small angles of hidden strabismus <2PD that were not detected by PCT (in 11 patients). The described difference is related to the difficulty of capturing with the "naked" eye the small adjusting movements of the eyes during the PCT test, which are easily detected by the Strabiscan device. Due to the described difficulties in the PCT test, we suggest that the values read from the Strabiscan device might be characterized by higher measurement accuracy. In the control group, using the Strabiscan device, small-angle latent strabismus ≤3DP was diagnosed in 25/30 patients (83%) and >3DP in 4/30 patients (13%). In contrast, using the PCT test, latent strabismus ≤3DP was diagnosed in only 4/30 13% of patients, and latent strabismus with an angle of >3DP in 4/30 (13%) patients.
Strabismus at near fixation using the PCT test was diagnosed in 23 patients from the healthy group (76%) and in 28 patients with the strabismic disease (93%). Using Strabiscan, strabismus to the near was observed in 28 patients from the healthy group (93%) and in 30 patients with the strabismic disease (100%).
Table 2 shows detailed features on the diagnosis and treatment of strabismic disease in the study group.
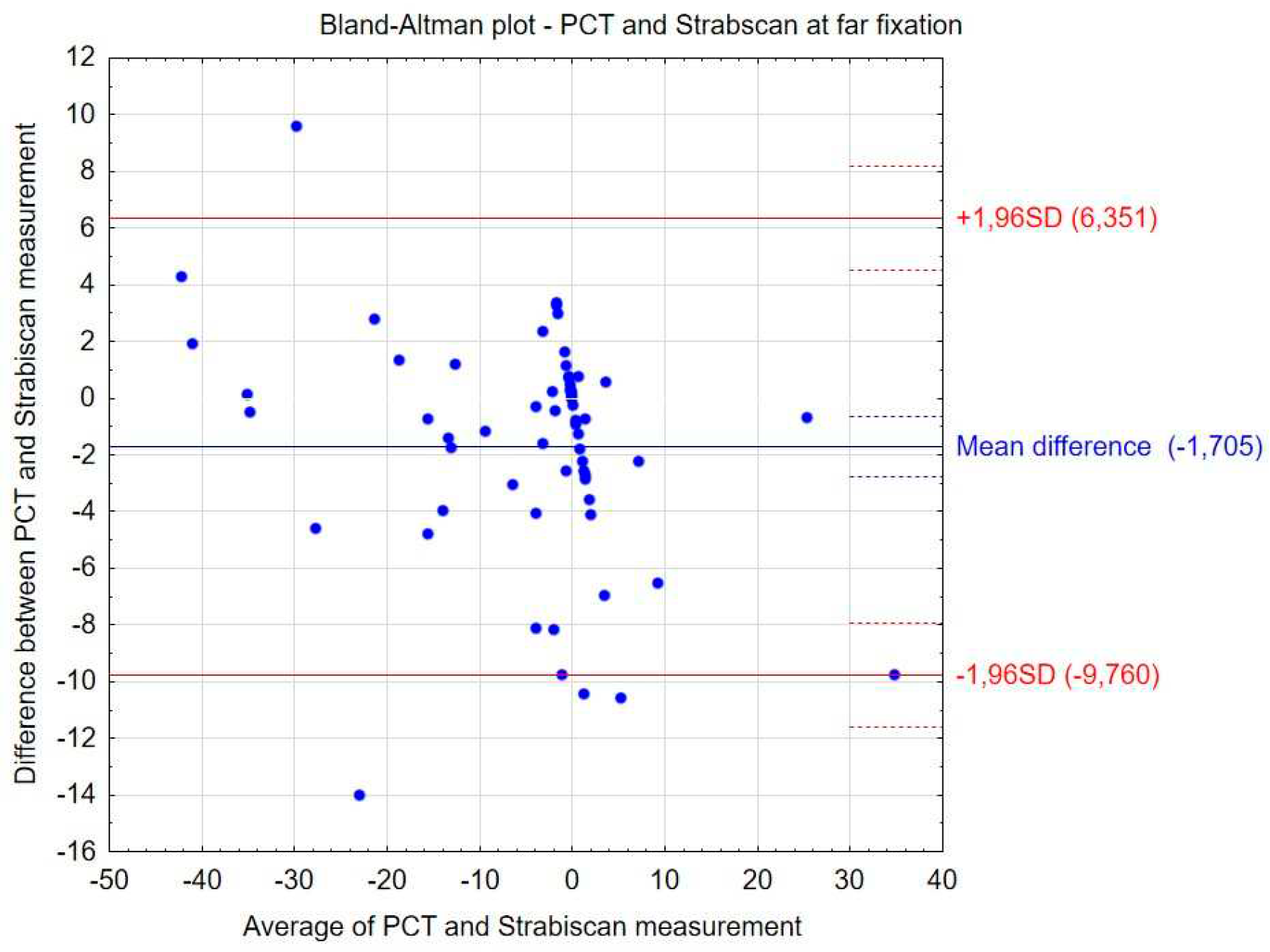
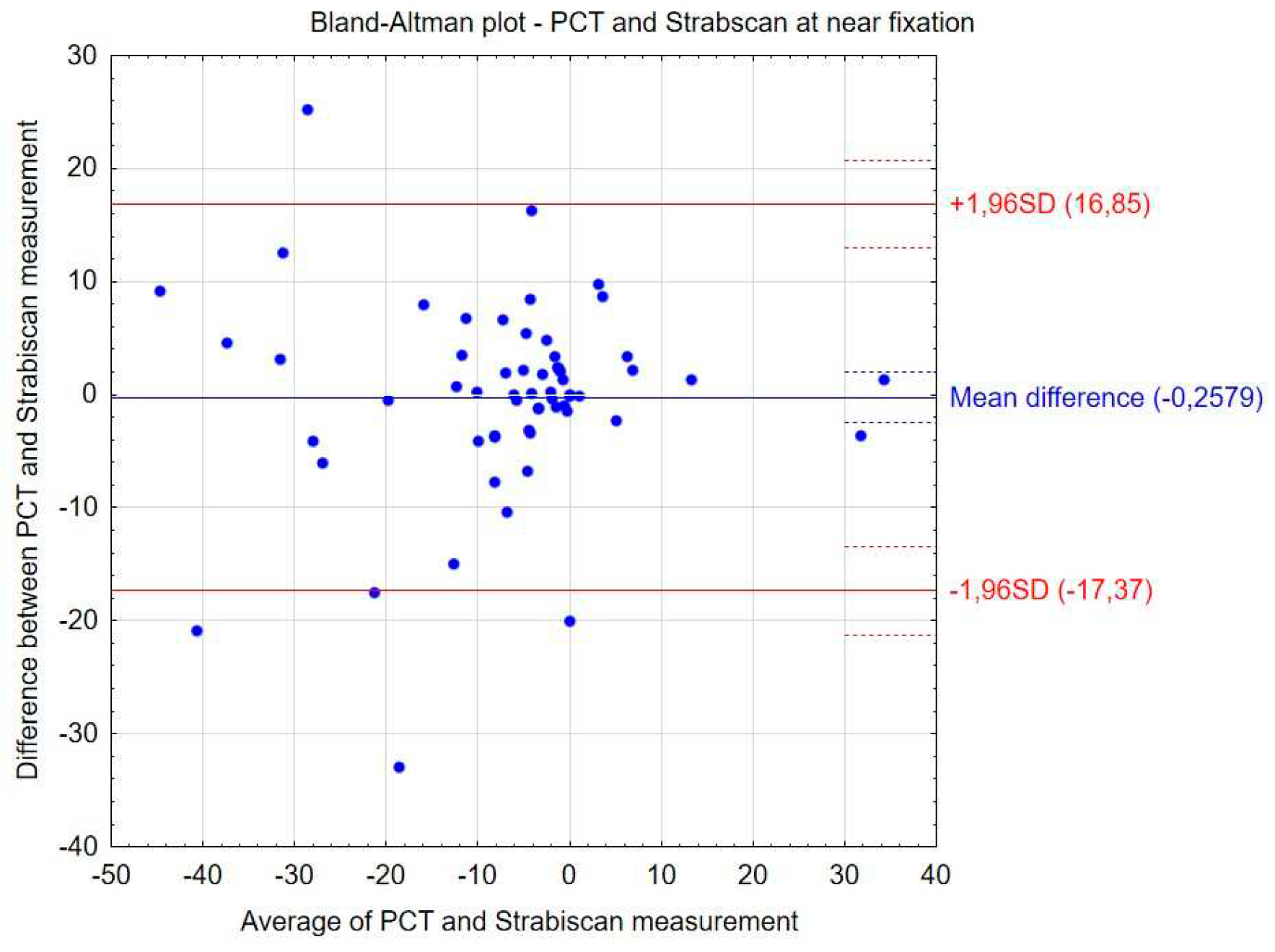
The comparative results of the PCT method and the Strabiscan device are shown in
Table 3. No statistically significant differences were noted in the measurements of strabismus angles performed by the different methods. Bland-Altman plots showing the agreement between compared procedures at far and near fixation (
Figure 4 and
Figure 5). Comparing the inconvenience of performing the tests for the patient, less inconvenience was noted in the test performed with the Strabiscan device than with the PCT method, but the difference was not statistically significant.
The sensitivity and specificity of strabismus detection with the Strabiscan device were analyzed. A Receiver Operating Characteristic (ROC) curve was calculated along with the Area Under Curve (AUC) (
Figure 6 and
Figure 7).
4. Discussion
Currently, there is no ideal method for measuring the strabismic angle, although the prismatic cover test is the gold standard for the diagnosis of strabismic disease, it is known that the result depends on the examiner's experience and subjective judgment. Obtaining precise results, independent of the experience and skills of the examiner, could lead to better results of surgery on the extraocular muscles since measurements of the strabismus angle are the basis not only for the diagnosis of the type of strabismus, the degree of deviation of the eyeballs, the extent of this deviation, but also on the basis of these measurements the type and extent of surgery on the extraocular muscles are planned.
In our study, we used an innovative demonstration equipment called the Strabiscan. This device has no prism bars, but a precisely adjusted optical system that takes into account refractive correction and the resulting prismatic effect, as well as fully controlled LCD shutters and fixation points displayed in positions tailored to the individual anatomical features of the patient, and therefore does not have the disadvantages of traditionally used methods and allows standardization of the examination in each patient. Better stabilization of the head on the device in relation to the PCT increases the accuracy and repeatability of the measurement. A constant measurement resolution of 0.1DP is much greater in contrast to PCT where the stepped resolution of prism power is available. In addition, the result of the study is not affected by the psychophysical state of the examiner, and the patient is limited due to the shorter examination time. The amount of deviation is observed by software, not by the operator, so it cannot be affected by the individual operator's experience level and perceptiveness. Another advantage of the Strabiscan device is the constant obscuration time of 1.5 seconds, and the covered eye is almost fully isolated from ambient light, allowing for more effective fusion breaking than in a standard PCT test using a simple manual occluder. This effect is comparable to the use of one-eye occlusion prior to PCT testing.
Strabiscan does not have limitation like others devices based on eye movement which rely on the anatomical center of the pupil for positional assessment and do not contemplate the inclusion of the Kappa angle. The measurement with our device have enhance accuracy, because it rely on the catch the moment of stopping eye adjusting movements while eye is fixating.
The most debatable issue may be the accuracy of the measurements. The PCT test itself is the gold standard of testing, but there is no reference method for measuring strabismus angle to which new devices can be compared. As a new device, the Strabiscan does not have a specific measurement accuracy, but this will be the subject of future studies. In our opinion, the best indicator of the accuracy of the Strabiscan would be a study of a large group of patients conducted before and after surgery, planned on the basis of the results from the PCT. The final postoperative result should then be confronted with the difference in strabismus angle readings between the Strabiscan and the PCT, and recalculated whether, hypothetically, a surgery performed according to the strabismus angle readings measured by the Strabiscan would also cover the postoperative strabismus angle.
The Strabiscan device successfully attempted to eliminate psychological convergence and the associated distance compression in a virtual environment by displaying on the test screen a properly prepared and slightly blurred background image, showing a landscape with far-field objects. Technological difficulties may be encountered if the patient has a very large refractive error, i.e. > +/- 10 Diopters (D), or if the patient has nystagmus. Underestimation of the strabismus angle may be encountered in the case of visual field deficits.
A small technological risk is the imperfect pupil movement detection algorithm, which is based on very accurate detection of the pupil position in the image. The exact behavior of the algorithm in the case of very irregular pupils or pupils strongly obstructed by the eyelid during oblique gaze is not known. It should be emphasized that all of the analyzed publications show eye examinations under near ideal conditions, i.e., accurately visible entire pupil, no shadows, looking at a small angle, while the device we propose should work properly in contact with a variety of individual patients. It needs further research to answer these uncertainties.
Referring to PCT method, we stated the thesis that the standard PCT test, where the patient additionally wears his habitual correction lenses, results in an incorrect reading from the prism bar because when looking at an angle, the lens border acts as a prismatic element and causes an additional deflection of light rays. We conducted a laboratory experiment indicating that when looking at a fixation point at a certain large angle, the eyeball angle is noticeably different before and after wearing an additional correction lens. For example, the concave lenses cause the patient an apparent angular narrowing of the FoV, which in general is the result of keeping the lens at a distance of about 10 mm from the front of the cornea. The PCT method does not determine the corrections of the viewing angles of the fixation point according to the size of the refractive error. Large values of astigmatism or aberrations of the corrective lenses further complicate the problem. This thesis requires further analysis of the results of strabismic angle measurements in patients wearing corrective lenses. The most relevant may be the results of strabismus surgeries based on traditional diagnostic methods, especially whether there is a statistically significant correlation between the type of refractive error and the amount of surgical under correction of strabismus. The prototype device does not have capacity to discern latent and manifest components of strabismus independently. Main limitation of application the Strabiscan device is the requirement for at least 53mm interpupillary distance. Knowledge from epidemiology studies state that mean pupillary distance which is 53mm matches 4,8 years age [
33]. In addition, the use of the apparatus will depend on the child's level of cooperation and concentration, which the authors believe will be less challenging than the PCT.
At the moment, the lack of devices such as Strabiscan on the market constitutes a strabismus measurement niche in public and private centers, that treat strabismus, both with behavioral and surgical methods. The proposed device is distinguished by high reliability of the strabismus angle assessment, which may be easily used by ophthalmologists and orthoptists without specialized training courses which may encourage its widespread use in the health care system. In the current epidemiological situation related to COVID-19, an additional undoubted advantage of the device is the reduction of close contact with the patient and the possibility of using full personal protective equipment during examinations. Limitations of the current study include the small study group and the inclusion of only Caucasians. So far, results on only horizontal strabismus have been analyzed. It is not certain when the test can be performed on patients with severe mental disabilities.
5. Conclusions
In conclusion, the Strabiscan is a valuable and safe demonstration device that allows quick and objective evaluation of the strabismus angle and as the first in the world, is able to automatically diagnose the strabismus disease by performing a standard cover-uncover test obtaining comparable results to the test performed with the PCT test. Although the PCT is regarded as the gold standard it has a significant number of disadvantages and under some special conditions its indications may be biased within a certain measurement error range. Compared to the prismatic cover-uncover test, it has a higher sensitivity for detecting low-angle latent strabismus. The use of the Strabiscan device may allow accurate diagnosis of strabismus even in those ophthalmology offices that have not previously specialized in the detection and treatment of strabismus disease, as it does not require highly qualified personnel to operate it. As well as it can influence better final results of surgical treatment through accurate and reproducible measurements of strabismus angles.
References
- Robaei, D.; Rose, K.A.; Kifley, A.; Cosstick, M.; Ip, J.M.; Mitchell, P. Factors Associated with Childhood Strabismus. Findings from a Population-Based Study. Ophthalmology 2006, 113, 1146–1153. [Google Scholar] [CrossRef]
- Pundlik, S.; Tomasi, M.; Liu, R.; Houston, K.; Luo, G. Development and Preliminary Evaluation of a Smartphone App for Measuring Eye Alignment. Transl Vis Sci Technol 2019, 8. [Google Scholar] [CrossRef]
- von Bartheld, C.S.; Croes, S.A.; Johnson, L.A. Chapter 59 - Strabismus. In Ocular Disease; Levin, L.A., Albert, D.M., Eds.; W.B. Saunders: Edinburgh, 2010; pp. 454–460. ISBN 978-0-7020-2983-7. [Google Scholar]
- Michaelides, M.; Moore, A.T. The Genetics of Strabismus. J Med Genet 2004, 41, 641–646. [Google Scholar] [CrossRef]
- Jrbashyan, N.; Yeghiazaryan, N.; Sikder, A.; Nallasamy, S.; Reid, M.W.; Ohanesian, R.; Lee, T.C.; Espinoza, J. Pattern and Prevalence of Eye Disorders and Diseases in School-Aged Children: Findings from the Nationwide School Sight Sampling Survey in Armenia. BMJ Open Ophthalmol 2022, 7, 899. [Google Scholar] [CrossRef]
- Valente, T.L.A.; de Almeida, J.D.S.; Silva, A.C.; Teixeira, J.A.M.; Gattass, M. Automatic Diagnosis of Strabismus in Digital Videos through Cover Test. Comput Methods Programs Biomed 2017, 140, 295–305. [Google Scholar] [CrossRef]
- Yehezkel, O.; Belkin, M.; Wygnanski-Jaffe, T. Automated Diagnosis and Measurement of Strabismus in Children. Am J Ophthalmol 2020, 213, 226–234. [Google Scholar] [CrossRef]
- Schutte, S.; Polling, J.R.; van der Helm, F.C.T.; Simonsz, H.J. Human Error in Strabismus Surgery: Quantification with a Sensitivity Analysis. Graefe’s Archive for Clinical and Experimental Ophthalmology 2009, 247, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Rowe, F.J.; Noonan, C.P. Botulinum Toxin for the Treatment of Strabismus. Cochrane Database of Systematic Reviews 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.K.; Elflein, H.M.; Pokora, R.; Schlaud, M.; Baumgarten, F.; Urschitz, M.S. Health-Related Quality of Life and Mental Health in Children and Adolescents with Strabismus - Results of the Representative Population-Based Survey KiGGS. Health Qual Life Outcomes 2019, 17. [Google Scholar] [CrossRef] [PubMed]
- Heidary, G.; Aakalu, V.K.; Binenbaum, G.; Chang, M.Y.; Morrison, D.G.; VanderVeen, D.K.; Lambert, S.R.; Trivedi, R.H.; Galvin, J.A.; Pineles, S.L. Adjustable Sutures in the Treatment of Strabismus: A Report by the American Academy of Ophthalmology. Ophthalmology 2022, 129, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Anilkumar, S.E.; Narendran, K. Prisms in the Treatment of Diplopia with Strabismus of Various Etiologies. Indian Journal of Ophthalmology 2022, 70, 609–612. [Google Scholar] [CrossRef]
- Joo, K.S.; Koo, H.; Moon, N.J. Measurement of Strabismic Angle Using the Distance Krimsky Test. Korean J Ophthalmol 2013, 27, 276–281. [Google Scholar] [CrossRef]
- Rosenbaum, A.L.; Santiago, A. Pauline. Clinical Strabismus Management : Principles and Surgical Techniques. 1999, 569.
- Yang, H.K.; Han, S.B.; Hwang, J.M.; Kim, Y.J.; Jeong, C.B.; Kim, K.G. Assessment of Binocular Alignment Using the Three-Dimensional Strabismus Photo Analyzer. British Journal of Ophthalmology 2012, 96, 78–82. [Google Scholar] [CrossRef]
- Choi, R.Y.; Kushner, B.J. The Accuracy of Experienced Strabismologists Using the Hirschberg and Krimsky Tests. Ophthalmology 1998, 105, 1301–1306. [Google Scholar] [CrossRef] [PubMed]
- Rainey, B.B.; Schroeder, T.L.; Goss, D.A.; Grosvenor, T.P. Reliability of and Comparisons among Three Variations of the Alternating Cover Test. Ophthalmic and Physiological Optics 1998, 18, 430–437. [Google Scholar] [CrossRef]
- Wright, K.W.; Spiegel, P.H.; Hengst, T.C. Pediatric Ophthalmology and Strabismus.; 2nd ed. 20.; Springer, 2013; Vol. 34; ISBN 978-1-4899-0511-6.
- De Jongh, E.; Leach, C.; Tjon-Fo-Sang, M.J.; Bjerre, A. Inter-Examiner Variability and Agreement of the Alternate Prism Cover Test (APCT) Measurements of Strabismus Performed by 4 Examiners. Strabismus 2014, 22, 158–166. [Google Scholar] [CrossRef]
- Yeh, P.H.; Liu, C.H.; Sun, M.H.; Chi, S.C.; Hwang, Y.S. To Measure the Amount of Ocular Deviation in Strabismus Patients with an Eye-Tracking Virtual Reality Headset. BMC Ophthalmol 2021, 21. [Google Scholar] [CrossRef]
- Moon, H.S.; Yoon, H.J.; Park, S.W.; Kim, C.Y.; Jeong, M.S.; Lim, S.M.; Ryu, J.H.; Heo, H. Usefulness of Virtual Reality-Based Training to Diagnose Strabismus. Sci Rep 2021, 11. [Google Scholar] [CrossRef] [PubMed]
- Pateras, E.S.; Pateras, E. Technique for Measuring Strabismus with Synoptophore-Review Eye Accommodation-Binocular Vision View Project Myopia-Corneal Topography View Project Technique for Measuring Strabismus with Synoptophore-Review. Asian Journal of Research and Reports in Ophthalmology 2020, 3, 6–12. [Google Scholar]
- Dallyson Sousa de Almeida, J.; Corrĉa Silva, A.; Cardoso de Paiva, A.; Antonio Meireles Teixeira, J. Computational Methodology for Automatic Detection of Strabismus in Digital Images through Hirschberg Test. Comput Biol Med 2012, 42, 135–146. [Google Scholar] [CrossRef]
- Chen, Z.H.; Fu, H.; Lo, W.L.; Chi, Z.; Xu, B. Eye-Tracking-Aided Digital System for Strabismus Diagnosis. Healthc Technol Lett 2018, 5, 1–6. [Google Scholar] [CrossRef]
- Weber, K.P.; Rappoport, D.; Dysli, M.; Schmückle Meier, T.; Marks, G.B.; Bockisch, C.J.; Landau, K.; MacDougall, H.G. Strabismus Measurements with Novel Video Goggles. Ophthalmology 2017, 124, 1849–1856. [Google Scholar] [CrossRef]
- Chopra, R.; Mulholland, P.J.; Tailor, V.K.; Anderson, R.S.; Keane, P.A. Use of a Binocular Optical Coherence Tomography System to Evaluate Strabismus in Primary Position. JAMA Ophthalmol 2018, 136, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.K.; Seo, J.M.; Hwang, J.M.; Kim, K.G. Automated Analysis of Binocular Alignment Using an Infrared Camera and Selective Wavelength Filter. Invest Ophthalmol Vis Sci 2013, 54, 2733–2737. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Tian, T.; Wygnanski-Jaffe, T.; Yehezkel, O.; Wang, S.; Moshkovitz, A.; Sun, X.; Liu, H.; Liu, R. Effectiveness and Repeatability of Eye-Tracking-Based Test in Strabismus Measurement of Children. Semin Ophthalmol 2022, 37, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Bindiganavale, M.; Buickians, D.; Lambert, S.R.; Bodnar, Z.M.; Moss, H.E. Development and Preliminary Validation of a Virtual Reality Approach for Measurement of Torsional Strabismus. Journal of Neuro-Ophthalmology 2022, 42, E248–E253. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Lynn, M.H.; Pundlik, S.; Almeida, C.; Luo, G.; Houston, K. A Smartphone Ocular Alignment Measurement App in School Screening for Strabismus. BMC Ophthalmol 2021, 21. [Google Scholar] [CrossRef]
- Oltrup, T.; Bende, M.; Henseling, C.; Bende, T.; Leitritz, M.A.; Ulrich Bartz-Schmidt, K. A New Digitised Screen Test for Strabismus Measurement. Z Med Phys 2022. [Google Scholar] [CrossRef]
- PING LIANG; FENG PAN; QIWEI GU Intelligent Type Digital Type Synoptophore 2010.
- Chen, A.H.; O’Leary, D.J. Changes in the Interpupillary Distance with Age and Its Effect on the near Fusion Free Position. Aust N Z J Ophthalmol 1997, 25 Suppl 1. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).