Introduction
Local anesthesia (LA) is the most commonly preferred technique, which is used to control occurrence of pain while performing dental procedures. It is utilized for prevention of pain preoperatively, intraoperatively and postoperatively [
1]. Many studies have reported that most of the patients delay their appointments or sometimes never come back for treatment due to their fear of pain towards dental procedures like extractions,root canal treatment etc. Thus, it is necessary to use a safe and effective method,such as usage of local anaesthesia, which reduces pain for patients while undergoing dental procedures. Several techniques for administering local anaesthesia were employed to achieve pain free treatment which include infiltration,nerve block, during extraction of teeth [
2]. Tooth extraction is considered to be one of the most common dental procedures that require administration of local anaesthesia, and the technique selected depends on location of the tooth to be extracted. Techniques such as mental nerve block, inferior alveolar nerve block,lingual nerve infiltration are some of the techniques that are used for extraction of mandibular teeth, of which Inferior alveolar nerve block is a more commonly used technique for anesthetizing mandibular incisors and bicuspids [
3]. However, Some studies have shown that Inferior alveolar nerve block has been associated with complications such as pain, nerve injury, trismus "and rarely paralysis of the facial nerve.
Another technique that has been used for anesthetizing mandibular incisors and bicuspids is the Mental Incisive Nerve Block (MINB) [
4,
5]. The Incisive nerve is a terminal branch of the inferior alveolar nerve, originating as a direct continuation of the inferior alveolar nerve at the mental foramen, the incisive nerve travels anteriorly in the incisive canal, providing sensory innervation to those teeth located anterior to the mental foramen [
6] .The areas which are anesthetized when Mental Nerve Block is administered are premolars, canine, and lateral and central incisors, along with their buccal soft tissues and bone. Mental nerve block can be administered when procedures such as extraction,root canal treatment etc., had to be performed on mandibular incisors and bicuspids.
The main aim of this study is to compare the onset and effectiveness of mental nerve block with lingual infiltration and inferior alveolar nerve block on patients visiting dental hospital for extraction of mandibular anterior teeth.(mandibular central incisor to first premolar)
Materials and Methods
The study was set in a clinical setting and Institutional Ethics Committee approval was obtained (ethical approval number - SDC/SIHEC/2020/DIASDATA/0619-0320) for conducting this randomized controlled double-blind cross study, where 25 subjects received two treatments at an interval of at least 1 week in a within a dental hospital. Informed consent was obtained from the subjects who were participating in this study. All local anaesthesia were given by the same operator. The volunteers and the investigator of anaesthetic outcome were blinded to the local anaesthetic technique used at each visit. Instructions regarding effects of administration of local anaesthesia were explained to patients. The previous medical history was recorded on a standard proforma.
Inclusion criteria:
Patients,18 years of age requiring extraction in 3rd and 4th quadrants anterior teeth central incisor to 1st premolar
Exclusion criteria:
Patients allergic to local anaesthetics, pregnancy, bleeding disorders and neurological conditions.
Procedure:
Inferior alveolar nerve block and lingual nerve block injection is given with 2mL lignocaine 2% with 1:2,00,000 epinephrine was administered for the right side.
Mental nerve block along with lingual infiltration of the corresponding tooth was given with 2mL lignocaine 2% with 1:2,00,000 epinephrine was administered on the left side.
Visual analogue scale (VAS) was used in this study, which consists of a scale with range of 0-10 pain severity on which 0 indicated absence of pain and 10 the worst pain possible. The patients were asked to give scores corresponding to his/her pain, after IANB, mental nerve block and lingual infiltration and these scores were recorded. The ‘‘faint, weak, or mild’’ pain corresponded to a score range between 0-3 and was kept as a cutoff for assessing successful anesthesia. If the patient reported a score between 0-3 on the VAS scale during the treatment, the anesthesia was marked as successful.
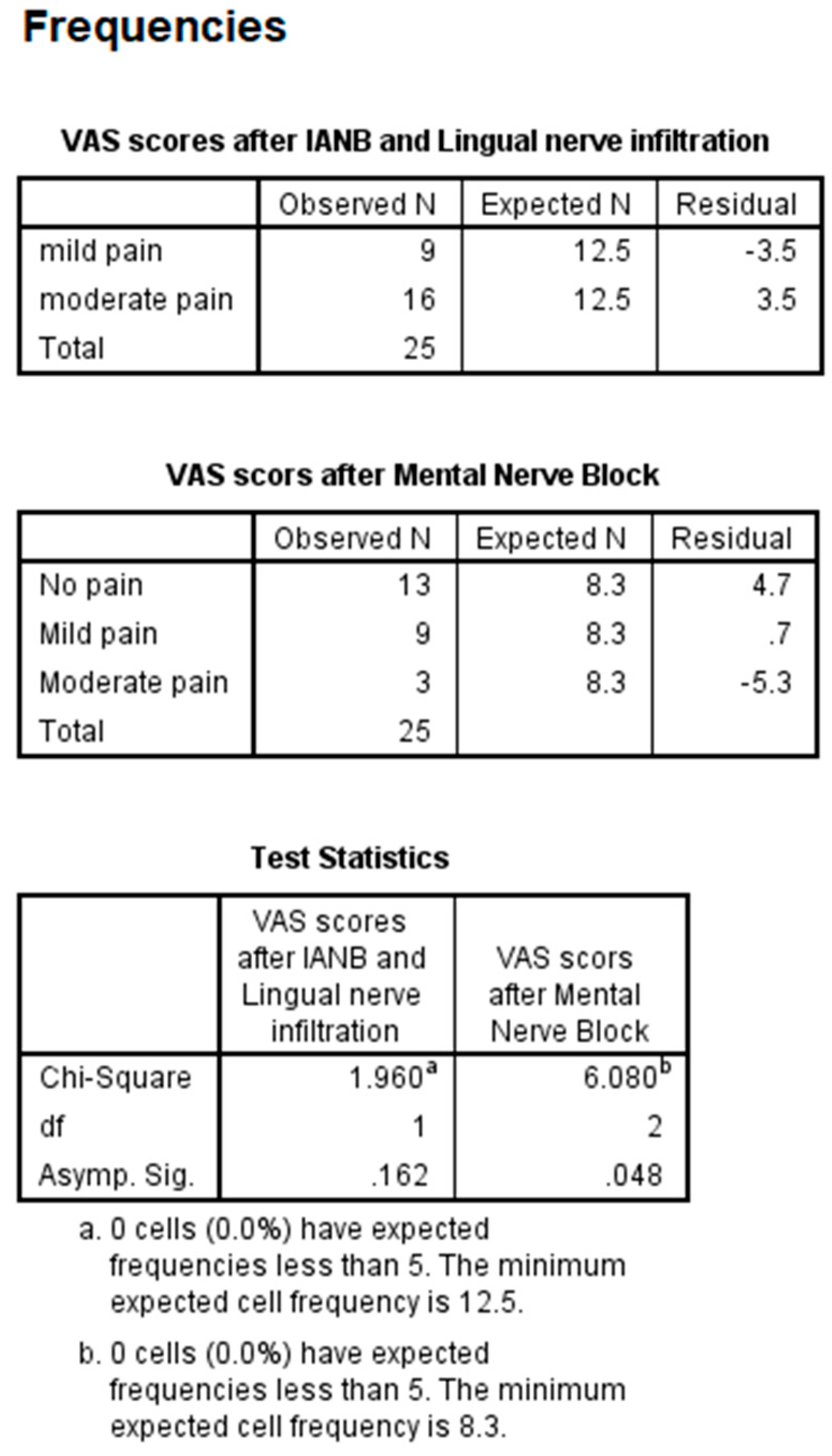
Statistical analysis was performed using IBM SPSS software (version 20). Visual analog scale values obtained from patients were compared between the 3 local anaesthesia techniques used before extraction. Chi square test was done between VAS scores recorded after administration of IANB Vs VAS scores recorded after administration of Mental nerve block and Lingual nerve infiltration. Results were considered significant if P<0.05.
Results
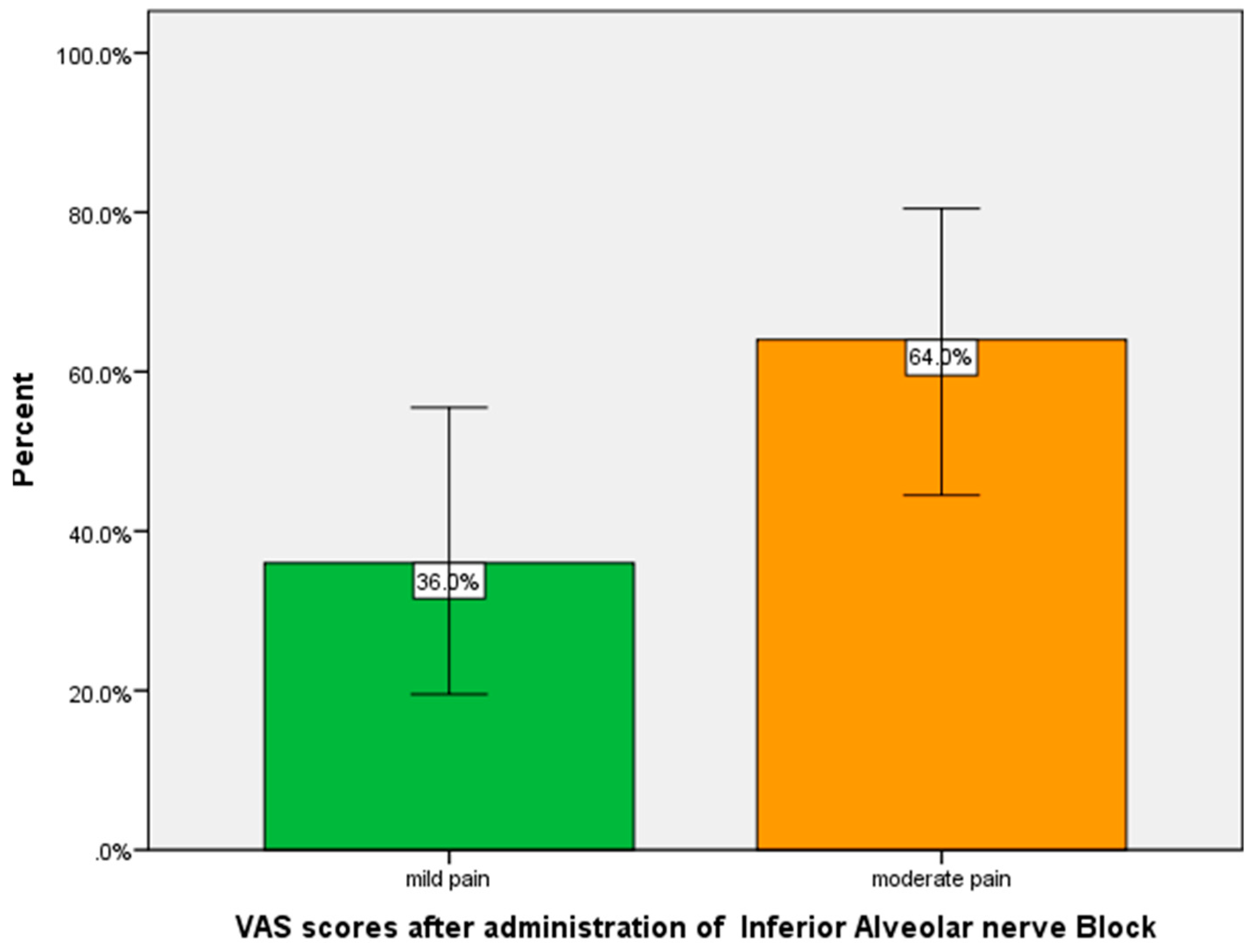
The VAS scores given by patients were analyzed and plotted in the form of graphs and tables. From the results we can see that patients gave scores between 3-4, stating that they had moderate pain during extraction after administration of IANB (54%) (
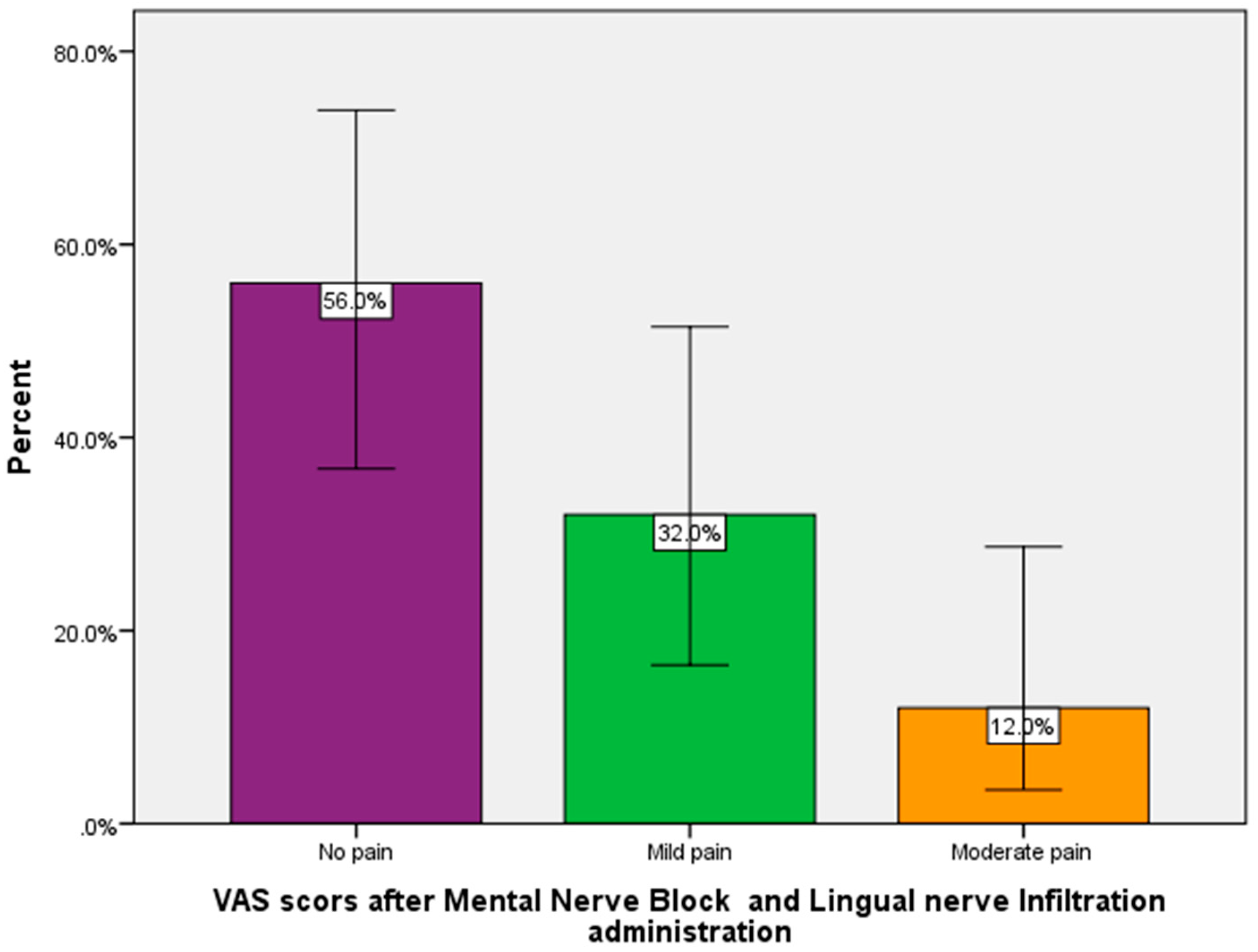
Figure 1) and VAS scores of 0-1 were given by patients, which is suggestive of no pain during extraction after administration of Mental nerve block and lingual nerve infiltration (62%) (
Figure 2). On performing a chi-square test between VAS scores recorded after IANB vs Lingual nerve infiltration and Mental nerve block, showed that the values were statistically insignificant (
Table 1)
Discussion
It is necessary to improve the quality of pain management and to evaluate new pain management techniques, to remove the negative attitude of patients towards dental procedures created due to fear of pain. From this study, it was found that Mental nerve block and lingual nerve infiltration showed immediate anesthetic effect when compared to IANB, onset time ranging between 30-60s (
Figure 2) whereas, IANB showed onset time about 4-5 minutes (
Figure 1) . This can be attributed to the fact that the onset of effectiveness of local anesthesia is quite fast (2–3 minutes) with mental nerve block when compared with the onset of effectiveness of an IANB (4-5 minutes) as with the inferior alveolar and lingual nerve block, the anesthetic effect starts from the third molar proceeding mesially and as the mental nerve is closer to the anterior tooth, the onset is quicker with this block.Similar findings were given in a study by Nist et al., [
6,
7] and Aggarwal et al. [
8], where they evaluated the combination of IANB and mental nerve block and reported that the combination was more successful in the first and second premolars and it enhanced anesthesia for the laterals and first molars. The present study evaluates IANB and lingual nerve block comparing it with mental nerve block and lingual infiltration of anterior tooth.
Similar findings were also observed in study by Nist et al., McLean et al. , Clark et al., where, IANB showed anesthetic success during extraction of lateral incisors, compared to 19.4% after IANB alone. The success of lateral incisor pulp anesthesia, reported in the literature following IANB injection only, ranges between 30% and 50% [
9,
10]. This increased from 40% when IANB injection was administered alone to 62% when additional labial infiltration was added to IANB (Clark et al. 2002). Another study reported complete central incisor pulp anesthesia when IANB was supplemented with buccal infiltration [
11]. Our success for lateral incisor pulp anesthesia was less than that reported in the study of Rood et al., and this is probably the result of buccal infiltration in the first molar region, not the incisor area. The onset of anesthesia was fastest in the 1st premolar region progressing towards the central incisor. With increased number of subjects, we can assess the results with accuracy (
Table 1).
Conclusion
Within the limits of the study we can conclude that mental nerve block along with lingual infiltration is an effective way to completely and quickly anesthetize the central incisor to the 1st premolar region. More specific study to compare each tooth could be undertaken to understand the full effectiveness of the technique.
Author Contributions
Manthra Prathoshni performed the conception of study, data collection, data analysing and interpreting statistics and contributed to manuscript writing, discussed the results and contributed to the final manuscript. Dr Rubin S John contributed to the conception of study, study design, analyzed the collected data, statistics and interpretation and also critically revised the manuscript, discussed the results and contributed to the final manuscript.
Funding
The present project is supported/ funded/sponsored by
Conflicts of Interest
Nil.
References
- McDonald RE, Avery DR, Dean JA, Jones JE. Local Anesthesia and Pain Control for the Child and Adolescent. McDonald and Avery Dentistry for the Child and Adolescent 2011:241–52. [CrossRef]
- Salem S, Namnakani A, Saad I. Cognizance of Undergraduate Students toward Periodontal Ligament Injection in Exodontia. Journal of Advances in Medicine and Medical Research 2018;25:1–9. [CrossRef]
- Malamed SF. Handbook of Local Anesthesia. Mosby Incorporated; 2004.
- Whitworth JM, Kanaa MD, Corbett IP, Meechan JG. Influence of injection speed on the effectiveness of incisive/mental nerve block: a randomized, controlled, double-blind study in adult volunteers. J Endod 2007;33:1149–54. [CrossRef]
- Batista da Silva C, Berto LA, Volpato MC, Ramacciato JC, Motta RHL, Ranali J, et al. Anesthetic efficacy of articaine and lidocaine for incisive/mental nerve block. J Endod 2010;36:438–41. [CrossRef]
- Meechan JG. The use of the mandibular infiltration anesthetic technique in adults. J Am Dent Assoc 2011;142 Suppl 3:19S – 24S. [CrossRef]
- Nist RA, Reader A, Beck M, Meyers WJ. An evaluation of the incisive nerve block and combination inferior alveolar and incisive nerve blocks in mandibular anesthesia. Journal of Endodontics 1992;18:455–9. [CrossRef]
- Aggarwal V, Singla M, Miglani S, Kohli S. Comparative Evaluation of Mental Incisal Nerve Block, Inferior Alveolar Nerve Block, and Their Combination on the Anesthetic Success Rate in Symptomatic Mandibular Premolars: A Randomized Double-blind Clinical Trial. Journal of Endodontics 2016;42:843–5. [CrossRef]
- McLean C, Reader A, Beck M, Meyers WJ. An evaluation of 4% prilocaine and 3% mepivacaine compared with 2% lidocaine (1:100,000 epinephrine) for inferior alveolar nerve block. Journal of Endodontics 1993;19:146–50. [CrossRef]
- Clark K, Reader A, Beck M, Meyers WJ. Anesthetic efficacy of an infiltration in mandibular anterior teeth following an inferior alveolar nerve block. Anesth Prog 2002;49:49–55.
- Rood JP. The analgesia and innervation of mandibular teeth. Br Dent J 1976;140:237–9.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).