1. Introduction
Undernutrition (wasting, stunting and underweight) coupled with micronutrient deficiency and other health-related issues are immense public-health challenges that plague developing countries, in particular. Though other methods such as fortification and supplementation for addressing undernutrition exist, traditional natural food-based diet interventions seem to be the most sustainable option to confront this challenge. The EAT-Lancet Commission report builds upon the concept of Planetary health and puts forth the new term “Planetary health diet”. It highlights the critical role that diets play in linking human-health and environmental sustainability, and the need to integrate both into a common global agenda for food systems transformation to achieve the Sustainable Development Goals (SDGs) [30]. The “Planetary health diet” suggests increasing the intake of whole-grains, vegetables, fruits, legumes and pulses which are currently eaten way below the target globally [
1]. According to the World Health Organization (WHO) also, it is recommended to consume a healthy diet which includes 400 grams (5 portions) of fruits and vegetables every day [
2]. Among thousands of indigenous food crops existing on this planet, rice, wheat and maize are the three staple foods majorly consumed by humans and provide 60% of their calories [
3]. Diversifying the staple foods is thus an important step towards achieving maximum nutritional benefit, as staples form the larger portion of our diets. This poses the next question: Which other alternate staples could fit into our diets, to provide required energy and maximum nutrition availability?
Millets , pulses and groundnut are traditional crops grown in Asia and Africa and are rich sources of macro and micronutrients [
4,
5,
28,
29]. However, their share in the consumer food basket is limited. Scientific evidence prove that millets have the potential to reduce type 2 diabetes, manage lipid profile, and reduce anaemia [
6,
7,
8]. Millets contain sulphur-rich amino acids such as methionine and cysteine and are generally low in lysine and hence complement well, to provide a balanced diet, when consumed with protein-rich pulses such as pigeon pea and chickpea, that are deficient in sulphur-containing amino acids but rich in lysine [
5,
9]. Finger millet is a rich source of calcium, an important mineral for child growth and bone-health [
15]. Moreover, groundnut is also one of the most energy-dense food sources that provides 520 kcal energy per 100 gm
1.
Millets, also called nutri-cereals, have the potential to play a crucial role in combating food insecurity and malnutrition [
17]. A community feeding pilot-study conducted among school-going children in India, proved that millet-based food formulations are not only acceptable, but also help improve the growth of the children compared to regularly consumed rice-based diets [
9]. During the study, millets were introduced in the form of common south Indian food items, namely, idli, khichdi, upma and bisibella bath (traditional local rice-based recipe), in which rice was replaced by millets. Dhanashakti, a biofortified pearl millet high in iron and zinc was used for the recipe formulations. In addition to millets, legumes and vegetables were added to further elevate the nutrient profile of the menu, that helped in improving health status of the consumers. The Government of India supports the supplementary nutritional needs of children (below 6 years) as part of the Integrated Child Development Services (ICDS)
2 scheme under the component-Supplementary Nutrition Programme (ICDS-SNP). In addition, it also supports the supplementary nutritional needs of pregnant and lactating mothers. The ICDS-SNP scheme is primarily designed to bridge the gap between the Recommended Dietary Allowance (RDA) and the Average Daily Intake (ADI).
The pre-school children (3 to 6 years) go to Anganwadi Centers (AWCs - community feeding centers under ICDS) and receive food under the ICDS - SNP. The food is intended to provide 500 calories of energy and 12-15 g of protein per child per day. Since a child of this age group is not capable of consuming a meal of 500 calories in one sitting, the guidelines prescribe the provision of morning snack in the form of milk/banana/seasonal fruits/micronutrient fortified food, etc. and a hot, cooked mid-day meal. The ICDS-SNP school meal is critical for the children especially, in the tribal regions of India, as it provides for the major portion of their food and nutritional needs.
However, the major staple served at school, as part of the mid-day meal, is refined rice. The Government of India guidelines recommends to provide a hot meal of rice (75g), dal (soup prepared using 15g of red gram),vegetables (25g), egg (50g), and nutri snacks/channa dal (split and roasted chickpea). The mid-day meal recipe is thus designed to provide total energy of 548 kcal per day for children between 3 to 6 years at the AWCs
3.
Rice is majorly consumed by people in India as it is supplied at a subsidised rate through the Public Distribution System (PDS). Based on the evidence on the health benefits of consuming millets [
9,
16] and considering the need to tackle the increasing malnutrition and climate change issues, the Government of India has recommended introducing millets in school meals [
13,
31].
The poor health outcomes among the tribal population in India, particularly among women and children, is attributed to the lack of dietary diversity [
18]. Financial circumstances, shift to lucrative crops, dependency on a public distribution system (PDS) that failed to incorporate traditional food patterns etc., played a role in the loss of dietary diversity among tribals [
19]. Reports based on the fourth round of National Family Health Survey (NFHS 4, 2015-16) highlighted the alarmingly poor nutritional status among women and children in the tribal areas of Telangana State, India. The government of the Telangana State, in collaboration with ICRISAT and other local bodies, such as the Integrated Tribal Development Agency (ITDA), designed an initiative to address these prevalent nutrition issues among tribals in the state. The initiative is intended to improve the health outcomes among children under 6 years as well as anaemic women in the age group of 15-49 years. The Agribusiness and Innovation Platform (AIP) of ICRISAT collaborated with the Department of Tribal Welfare (TWD), and Department of Women Development and Child Welfare (WDCW) of Telangana, in conceptualising, formulating and producing nutritious millet-pulse-groundnut based food products with the objective of providing affordable, safe and nourishing foods to the tribals.
Giri Poshana [Giri (Tribal) Poshana (nutrition)], was thus conceived as a tribal nutrition project with the aim of providing nutrition support to children (3-6 years) and tribal women (pregnant women and lactating mothers) at the AWCs, involving ITDAs. Giri Poshana focused on two of the aspirational districts, Bhadadri Kothagudam and Jayashankar Bhupalpally (including Mulugu), in Telangana state of India
4. Considering the challenges of rapidly changing climate conditions and prevailing malnutrition, especially among the tribal population, the alternate climate-resilient staples, namely, millets with legumes and/pulses have the potential to provide sustainable solutions to combat the environmental stress of climate change alongside ensuring food and nutrition security [
16]. The current study was conducted with the aim of determining the impact of introducing the millet-pulse-groundnut based Ready-to-Cook (RTC) meals and Ready-to-Eat (RTE) snacks, as an addition to the regular ICDS-SNP mid-day school meal; on acceptability, growth (height, weight, and MUAC) and Hb levels among pre-school tribal children attending AWCs in the ITDA areas of Bhadrachalam and Eturunagaram, in the Telangana State of India.
2. Materials and Methods
2.1. Ethical Approval
ICRISAT’s Institutional Review Board (IRB) is the body responsible, for ensuring that all research involving “Humans” is carried out in an ethical manner. The said study received ethical approval from ICRISAT’s IRB. The details of the ethical clearance are: (a) Project identification code: IEC-ICRISAT/20210707/07 (b) Date of approval: 07/07/2021 (c) Name of the ethics committee: Institutional Review Board (IRB), International Crops Research Institute for the Semi-Arid Tropics (ICRISAT).
2.2. Methodology
Prior to the study, a sensory evaluation of the formulated millet-pulse-groundnut based food products was conducted among selected target beneficiaries to assess the acceptability and preferences. A representative sample of children (3-6 years) was selected in each interventional ITDA area. The selected sample was provided with food products and feedback was recorded through a specifically designed questionnaire using a five-point hedonic rating scale (1 = dislike very much, 2 = dislike slightly, 3 = neither like nor dislike, 4 = like slightly, 5 = like very much) (Table S3). Based on the stated responses and preferences, the products were re-formulated, formulation finalized and products distributed among the beneficiaries at the selected AWCs. The distribution and feeding were undertaken with the help of the AWC staff prior to the COVID-19 pandemic. With the onset of the COVID-19 pandemic, the restrictions on movements and closure of the AWCs necessitated change in the product formats (from RTC to RTE), as the food products needed to be distributed as take-home rations (THR) directly to the beneficiary households. The challenges posed by the pandemic and other natural disasters, such as, floods in the intervention areas, caused intermittent breakdown in the distribution of the food products, resulting in extension of duration of the project period from 12 to 18 months. However, the feeding intervention was only for 12 months. At the end of the intervention period (endline), anthropometry and Hb data were collected by trained enumerators to assess the changes in the nutritional status among the children, by comparing with measurements recorded before intervention (baseline).
The anthropometric and Hb data were further complemented with qualitative data collected through 13 FGDs and 26 key informant interviews with AWC teachers (Table S4) where the outcomes of the nutrition intervention were discussed. Standard protocols were followed during the conduct of the FGDs with the AWC teachers, pre-school children and mothers to understand their (i) awareness on millets; (ii) traditional food habits and consumption; (iii) changes in the consumption pattern; (iv)post-intervention shift in consumption of millet-pulse-groundnut based products; (v) any improvements observed in the school-attendance among children and (vi) portion sufficiency of the products distributed.
2.3. Administrative Structure of the Study Sites and Sample Sizes
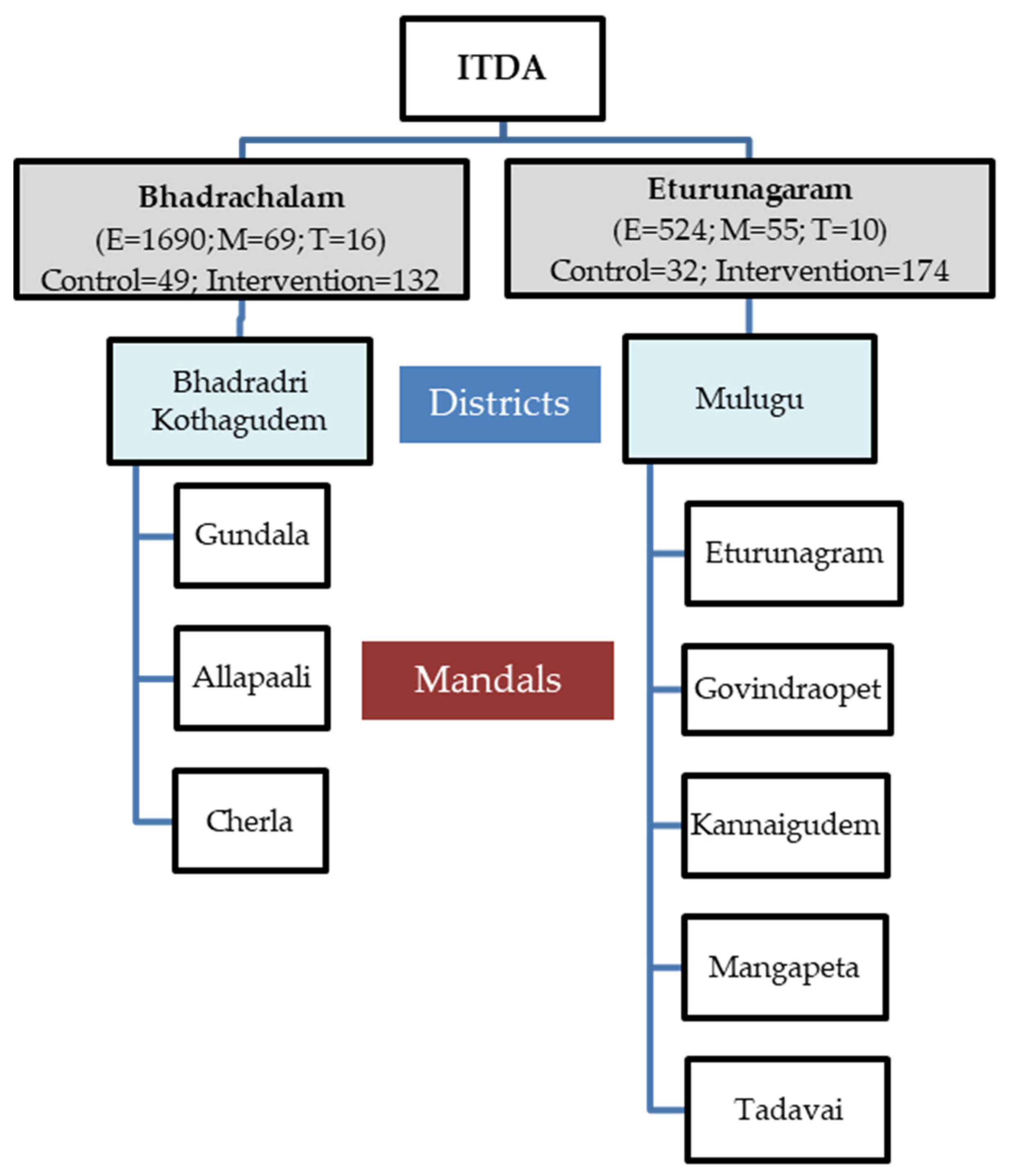
The Telangana State in India is divided into “Districts” which are again classified into “Sub-divisions.” The sub- divisions are further divided into “Mandals,” and the mandals consist of villages
5. Tribal dense areas namely Bhadrachalam and Eturunagaram ITDAs involving 273 AWCs were selected by the government body for the dietary intervention comprising of millet-pulse-groundnut based products (
Figure 1). The sample size of this study included 306 pre-schoolers who consumed the millet-pulse-groundnut based diet (Treatment group) and 81 pre-school children who had not received the intervention formed the Control group.
For the Bhadrachalam ITDA area, three mandals were chosen, namely Gundala, Allapally, and Cherla. Within each of these mandals, at least two FGDs were carried out. At Eturunagaram ITDA, five mandals were selected, including Govidraopet, Kannaigudem, Mangapet, Thadvai, and Eturunagaram. One FGD was conducted in each of these mandals, except for Mangapet, where two FGDs were conducted (
Figure 2 and
Figure 3).
Each FGD consisted of 10-12 mothers of pre-school children who were selected from the designated AWCs. The total number of mothers who participated in the FGDs conducted in Bhadrachalam and Eturunagaram ITDAs were 69 and 55, respectively. Additionally, AWC teachers from ITDA-Bhadrachalam (16) and ITDA-Eturunagaram (10) participated in individual interviews.
2.4. Products used in Giri Poshana and their nutrient profile
The food products used for the nutrition intervention were formulated using local climate resilient crops such as millets, pulses, groundnut etc, which provide energy, protein, fat and micronutrients. The intervention included RTC products such as Sorghum (jowar) Meal (sorghum, bengal gram, groundnut, spices and condiments), Multigrain Savoury Meal (sorghum, foxtail millet, green gram with spices and condiments), and Multigrain Sweet Meal (sorghum, wheat, almond, raisin, sugar and jaggery). These were given in the form of cooked meal (per serving per day was 50 g of uncooked meal equivalent to 150 g post-cooking).The RTE snacks comprised of energy bar (groundnut, jaggery, sesame, liquid glucose and sugar), energy bytes (sorghum, maize, rice, soya, oil, seasoning mix), and nutri-cookies (sorghum, finger millet, soya, vegetable fat, sugar, custard powder, cinnamon, and raising agent) provided in quantities of 35 g per serving per day as a combination of breakfast meal and evening snack for 6 days in a week, as per the standardized menu.
The nutrient profiling (
Table 1) was undertaken using approved Association of Agricultural Chemists (AOAC) International methods, for each of the respective parameters.
The products were designed to diversify and supplement the existing diets of the target population and were not fortified with additional micronutrients. The millets used in the food product formulations were malted to enhance the digestibility of carbohydrate/proteins and ensure reduction in anti-nutrients, thus leading to increased bioavailability of micronutrients [
17]. The AWC teachers were sensitized on, cooking methods for the RTC products, serving portions and the nutritional benefits of the products along with awareness on basic hygiene practices to be followed during food preparation, storage and serving.
2.5. Focus Group Discussions (FGDs)
The mothers of pre-school (3-6years) children and the teachers of AWCs were included in the FGDs. The respondents were interviewed individually to assess acceptance, preferences and challenges faced with respect to the three RTC and three RTE products, distributed to the beneficiaries during the intervention period.
These FGD sessions were conducted until the discussions or questions reached a saturation point, time varying between 60 to 90 minutes. A facilitator guided the group through the discussions in the local language, a note-taker documented the conversation without participating in the interactions and another team member recorded the conversation to create a transcript of the event.
The response on acceptability of the six products were recorded using a 6-point scale of 1 to 6; 6 being highly accepted and 1 being least accepted. The FGDs were designed to elicit responses about awareness on millets, the challenges faced while using them at home and their choices with respect to continued use of the products at AWCs or at homes. Some of the specific questions asked to the teachers during individual interviews, were related to challenges of implementation and changes observed among the children’s cognitive behaviour and overall performance.
2.6. Data Collection and Analysis
Anthropometry data that included indicators of height-for-age (stunting), weight-for-height (wasting), weight-for-age (underweight) and MUAC, were collected from both the treatment group (n=306) and the control group (n=81) of pre-school children at both baseline and endline. The instruments used were stadiometer (IS Indosurgicals Stadiometer-height), weighing scale (Seca 813 high capacity digital flat scale -weight) and MUAC tape (IS Indosurgicals Muac Tape - MUAC). The anthropometric indicators, were analysed using WHO developed online tool (WHO Anthro Survey Analyser). Paired t-test, to assess the mean anthropometric differences between treatment and control groups at baseline and endline, was performed using the Stata 14® software. Total Hb data were collected using a non-invasive haemoglobin measuring device- Masimo Rainbow SET® Pulse Co-Oximetry , from children, in both the intervention and control groups, at baseline and endline.
2.6.1. Data Preprocessing for Haemoglobin Data Analysis
Hb observations measured using a non-invasive device “Masimo Rainbow SET® Pulse Co-Oximetry”were first corrected in accordance with the reference “invasive” method using the following equation which was derived based on Taffé and Taffé et al. (2020) [
26,
27].
The reference method which is the `gold standard’ is not error-free but is almost free from measurement errors. What matters is the amount by which the two methods disagree (Bland & Altman, 1999) referred to as the bias. Total Hb levels were measured on 306 individuals in the treatment group while 81 individuals were monitored in the control group. However, 2 individuals from the treatment and 1 from the control group were excluded because the baseline and endline differences doubled after bias corrections with reference to the invasive method. Apart from this, 19 individuals in the treatment group did not have the baseline observations.
2.6.2. Repeated Measures Analysis of Variance (RM-ANOVA)
This is a classical repeated measures design in time where experimental units (individuals) receive a treatment and multiple measurements are made on the same individual for the response variable at different time points. Thus, the observations in the data set are no longer assumed to be independent as the residual errors are correlated among time points. The between-group factor here is Intervention (also referred to as the ‘Treatment’ – (Control Vs Treatment) and within-group factor is ‘Time’ (Pre Vs Post-intervention Hb measurements within each group). The mean change in the Hb levels when moving from pre- to post-intervention time in the control and treatment groups is directly measured by the Time*Treatment interaction term in the repeated measures ANOVA.
Statistical model:The ANOVA model for repeated Hb measures in time is
However, the residual (an estimate of the error) is a matrix.
In the residual matrix R, the diagonals and are the residual variances for the Pre- and Post-intervention time points respectively and the off-diagonals are the covariances between the two time-points, assumed to be the same across all individuals. The Time main effect was not included in the model as the overall effect of time across the two groups was not the focus.
3. Results
3.1. Pre-Intervention Assessment of Preferences
The study conducted prior to the commencement of the intervention indicated that the energy bar, energy bytes, multigrain sweet meal and nutri-cookies were on top of the beneficiaries’ preference list, especially among children (
Table 2)
. The reason for lower preferences for the sorghum meal and multigrain meal was mainly attributed to the spice levels and hence the spice levels were adjusted accordingly, as per the beneficiaries’ feedback.
3.2. Impact of Intervention on Growth Parameters
A paired t-test was performed to assess the differences in the mean of the anthropometric measures in the treatment and control groups before the intervention (baseline) and post- intervention (endline)
(Table 3). The treatment and control groups were similar and comparable in terms of their anthropometric measures prior to the intervention. The data analysis shows significant improvements (p<0.01) in the average anthropometric measures at endline as compared to baseline in both control and treatment groups. Importantly, the improvements in the anthropometric measures among the intervention group, (column (DT-DC) (
Table 3), were significantly higher, and can be attributed to the nutrition intervention. The intervention had the highest impact on improvement in height of the children in the treatment group (average height at baseline 91.3±8.72, at endline 104.1±7.51 (3.2 cm more compared to the control group) followed by higher average weight gain (average weight at baseline 11.9±2.26, at endline 15.5±2.34 (1.68 kg in the treatment group relative to the control group), MUAC (average MUAC at baseline 14.57±1.38, at endline 15.6±1.84 (0.33 cm in the treatment group relative to the control group). The results indicate the success of the intervention in terms of the positive impact, particularly on height and weight of the children in the treatment group.
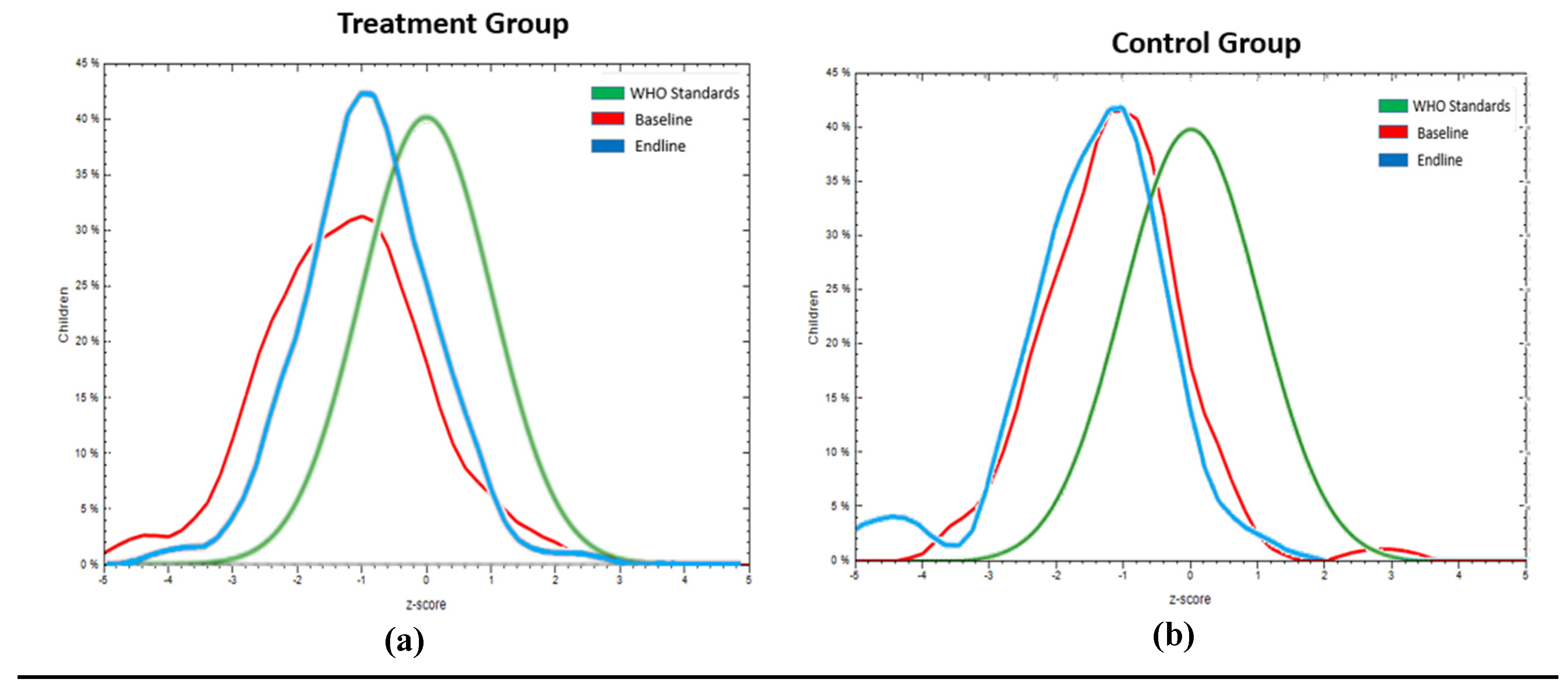
3.2.1. Impact on Wasting (Weight-for-Height)
In the treatment group (n=306), 7.2 % of the children were severely wasted (WHZ<-3), 20.8% were wasted (WHZ >-3 to <-2) at baseline. At endline 72.7% of the severely wasted children had moved to the wasted category. In the control group (n=81) 4.9% of the children were severely wasted, 14.8% were wasted at baseline. At endline there was 25% increase in severely wasted children. A considerable reduction was seen in the treatment group in severe wasting and wasting and a consequent increase in the normal category, in terms of linear growth. The percentage change (reduction or increase) in severe wasting, wasting and normal was -72.7%, -51.6% and +22.2%, respectively in the intervention group, while in the control group there was 25% and 50% increase in severe wasting and wasting, respectively and consequent reduction in normal category (-10.8%) (
Table 4).
Overall, the impact of the intervention on the treatment population moved [(mean WHZ moved from -1.2 ±1.3 to -0.9± 1 (
Figure 4 a)]. For the same period of the intervention, the control group (
Figure 4 b) showed a negative shift in mean WHZ from -1.2±1 to -1.4±1.1.
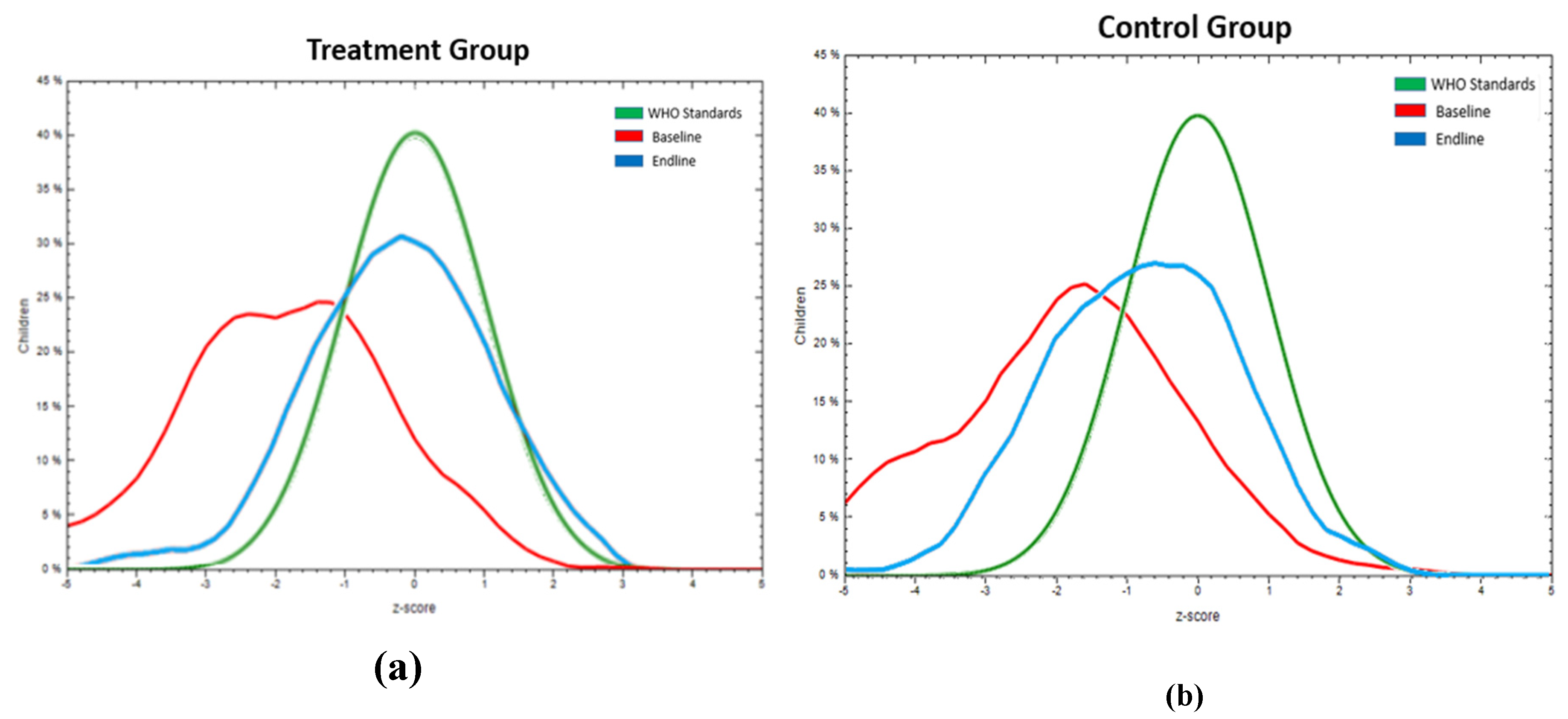
3.2.2. Impact on Stunting (Height- for- Age)
In the treatment group 20.8% of the children were severely stunted (HAZ<-3), 25.7% were stunted (HAZ >-3 to <-2) at baseline. At endline 87.5% of the severely stunted children had moved to the stunted category. In the control group 17.3% of the children were severely stunted, 24.7% were stunted at baseline. At endline, 64.3% of the severely stunted children, in the control group, had moved to the stunted category. There was a considerable reduction in severe stunting and stunting and a consequent increase in the normal category, in terms of linear growth in both the treatment and control groups . However, the positive rate of change observed in the control group was less than that in the intervention group. There was 73.8% increase in the number of children having normal growth in the intervention group compared to 29.8% increase in children having normal growth in the control group at endline, as compared to baseline. (
Table 4).
Overall, the impact of the intervention on the treatment population moved [(mean HAZ -1.8±1.6 to -0.3±1.3 for treatment (
Figure 5 a)]. For the same period , the control group (
Figure 5 b) showed a shift in HAZ from -2.0±1.7 to – 0.8±1.3.
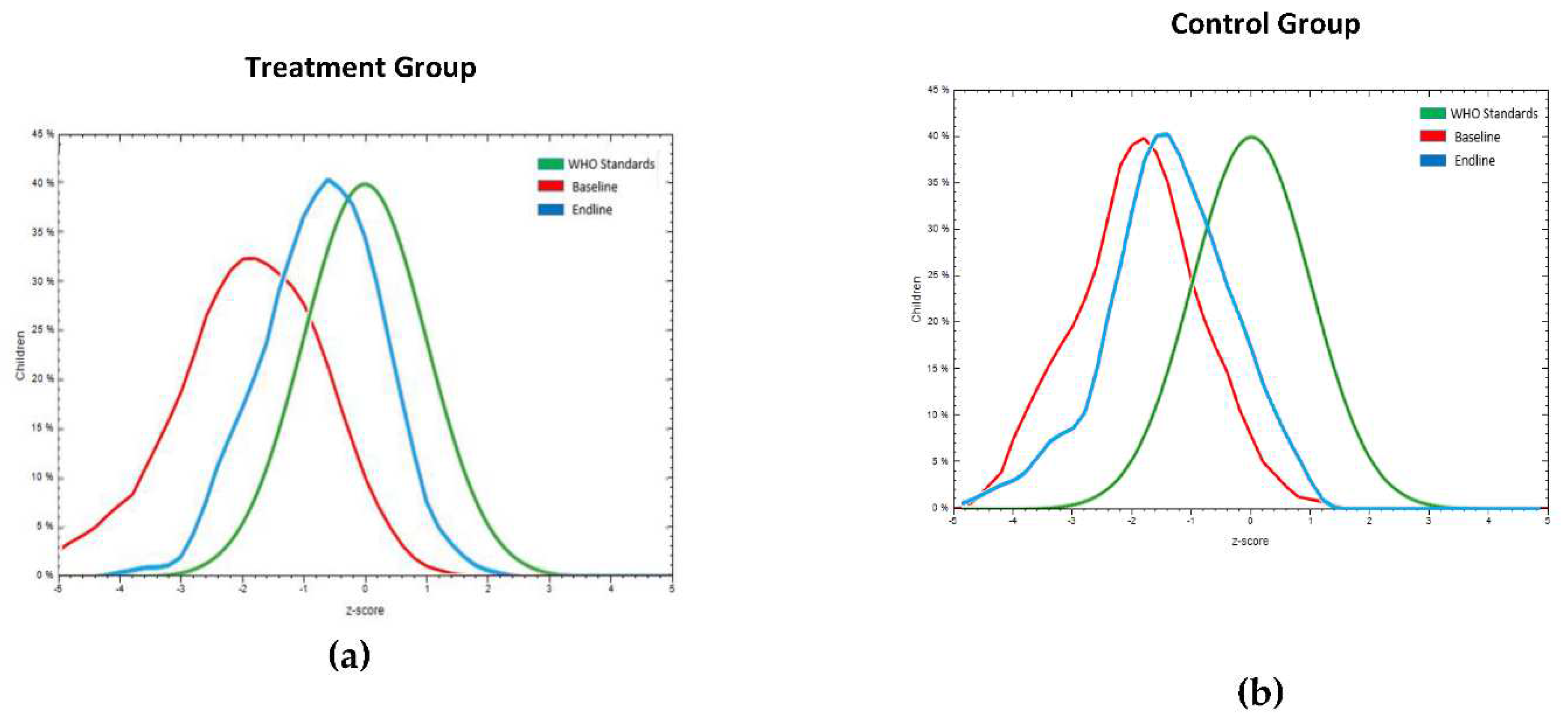
3.2.3. Impact on Underweight (Weight -for -Age)
In the treatment group 18.6% of the children were under severely thinness category (WAZ<-3), 27% were in thinness category (WAZ >-3 to <-2) at baseline. At endline 94.7% of the severely thinness category children had moved to thinness category. In the control group 8.6% of the children were in severely thinness category, 33.3% were in thinness category at baseline. At endline, 14.3% of the severely thinness children, in the control group, had moved to thinness category. There was considerable reduction in severe thinness and thinness categories which consequently increased the number of children in the normal category in both the groups. However, the positive rate of change observed in normal growth among children in the control group was less compared to children in the intervention group. There was 66.5% increase in children having normal growth in intervention group compared to 25.5% increase in children having normal growth in the control group at endline, compared to the baseline data (
Table 4). Overall, the impact of the intervention on the treatment population moved [(mean WAZ -1.9±1.2 to -0.7±1 for treatment (
Figure 6 a)]. For the same period, the control group (
Figure 6 b) showed a shift in WAZ from -1.9±1 to -1.4±1.
3.3. Impact of intervention on Haemoglobin (Hb) levels
The pre-intervention and post-intervention measures were positively associated. Thus, post-intervention measurements can be predicted based on pre-intervention values, for instance, if the treatment (intervention) group is a better performer prior to intervention (pre), it tends to be the same after intervention (post) as seen in the following means table.
Study
Groups |
Time |
Estimate
(g/dl) |
Standard |
Mean differences (Pre & Post) |
| Error |
t-value |
p-value |
| Control |
Pre |
8.3696 |
0.2607 |
6.33 |
<.0001 |
| Control |
Post |
10.3506 |
0.2401 |
| Treatment |
Pre |
9.7030 |
0.1379 |
8.36 |
<.0001 |
| Treatment |
Post |
11.0794 |
0.1238 |
| |
|
|
|
The RM-ANOVA indicated a significant treatment x time interaction (p<0.0001). A significant (Treat x Time) interaction effect implies that the Hb levels in the groups are changing over time and are changing in different ways. The main effect of treatment was also significant which implies that the control and the treatment groups differ significantly across the time points.
The change in Hb levels within the intervention group shifted significantly from 9.70 ± 0.14 g/dl to 11.08 ± 0.13 g/dl. This shift indicates that the previously moderately anemic (Hb 7 to 9.9 g/dl) individuals in the treatment population, post-intervention transitioned to the normal Hb level category (Hb ≥11 g/dl). In comparison, the control population, post-intervention moved from moderately anaemic Hb levels from 8.36 ± 0.26 g/dl to 10.35 ± 0.24 g/dl to mildly anaemic levels (10 to 10.9 g/dl) [
24,
25]. This clearly shows the impact of consuming millet-pulse-groundnut based food products on addressing the prevalent problem of anaemia among tribal children.
3.6. FGD preference rating of the food products
A total of 124 mothers and 26 AWC teachers were actively engaged in the FGDs and individual interviews, respectively. Mothers who participated in the outcome assessment were able to recollect all the six types of nutritious millet-pulse-groundnut based food products provided at the AWCs during the intervention. Based on the responses from the mothers, on a 6-point Acceptance Rating (AR) scale (6 indicating high acceptance and 1 indicating low acceptance) (
Table 5), the energy bar was ranked as the most favoured product, (AR=4.7±1.2); followed closely by, nutri-cookies as the second (AR=3.7±1.3), energy bytes third (AR=3.6±1.2) and the multigrain sweet meal was the fourth choice (AR=3.5±1.8). The sorghum meal and multigrain meal had AR ratings of 2.0±1.1 and 1.4±1.3, respectively.
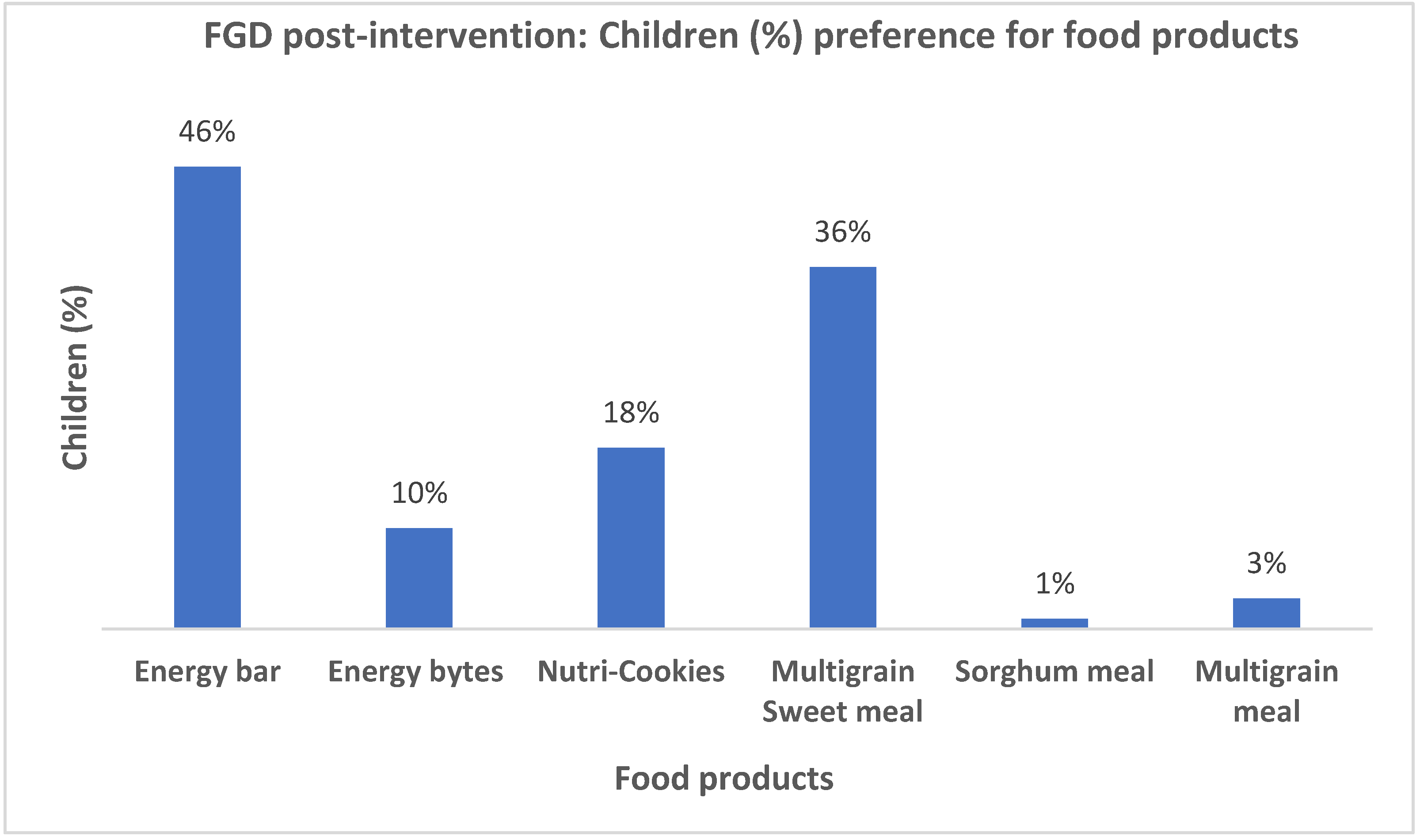
Mothers from both ITDAs mentioned that the energy bar received the highest preference rate, with 46% of them stating that their children favoured it (
Figure 7). Following closely, 36% of mothers rated the multi-grain sweet meal as the next preferred option for their children. Only 3% and 1% of the mothers indicated that their children showed a preference for the multigrain savoury meal and the sorghum meal, respectively.
4. Discussion
The results of the current study demonstrated the beneficial effects of dietary interventions based on millet- pulses-groundnut products. This study verified that consuming a diet, rich in millet and pulses helps combat undernutrition. This result aligns with past research conducted on millet consumption among adolescents in Karnataka state, India which had reported, that the groups who received millet-pulse food showed significantly greater anthropometric measurement readings than the adolescents who were not part of the nutrition intervention [
9]. A systematic review and meta-analysis study, involving publications on health impact of millet-based diets in comparison to consumption of only rice-based diets showed evidence on health benefits of consuming millets. Significant effect (p < 0.05) was indicated on mean height (8 publications) (+28.2%), weight (9 publications) (+26%), mid upper arm circumference (5 publications) (+39%) and chest circumference (5 publications) (+37%) in comparison to regular rice-based diets [
10].
In another study conducted among adolescent girls, millet-based foods had a significant impact on weight, BMI and also contributed to the improvement of Hb levels [
20]. Post-intervention data provided evidence that the mean weight improved from 26.77± 1.4 kg to 26.92±2.1 kg, mean BMI increased from 16.4±2.5kg/m
2 to 17.3±2.2 kg/m
2, and haemoglobin from 8.40±0.9 g/dl to 8.45±0.6 g/dl.
The positive effect on Hb levels in the current study findings are in line with other studies [
8,
21], showing that supplementation with iron-rich millet-based foods have a positive impact on haemoglobin levels and reduces the prevalence of anaemia.
Consumer acceptability has also been garnered for iron-rich snacks formulated using under-utilized millet grains [
21]. A “Multi-millet health mix” has been proven to have a positive effect in increasing the anthropometric indices of children [
22]. Our study further corroborates the acceptance of millet-pulse-groundnut based RTE and RTC products among the target beneficiaries leading to similar positive impact on anthropometric indices as well as haemoglobin levels.
Among the six recipes used for the intervention, four were generally liked by all the children (
Table 2). However, the multigrain savoury meal and sorghum meal were identified to have mixed responses among children, attributed mainly to the individual’s preference for salt, spices etc. Despite an initial sensory study to fine-tune the formulations, the said products elicited mixed responses, especially among children. This could be attributed to the changes in taste preferences in children of growing age. Further, mothers also informed that the meals were sometimes saltier. The possible reasons could be, not utilizing the pack containing the composite meal at one go or not shaking the packet well before using, resulting in salt deposits at the bottom of the packets. The AWC teachers also mentioned that sorghum meal and multigrain meal were the least popular products, among the cooks, because these two products took comparatively more time to cook. The most liked recipes were the sweet items especially energy bar and multigrain sweet meal, because of the taste- preference. Repeated demands for the products provide testimony to the fact that the sweet products were most preferred by the children. This highlights the necessity for ongoing product evaluation and modification in the formulations, when it comes to school meals, because acceptance among children may change for various reasons, such as change in childrens’ tastes or time taken for meal preparation by the community workers.
Mothers exhibited an improved understanding of the benefits that their children accrue from consumption of millets and pulses, which was clear from the FGDs (Table S1). The mothers stated that they had attempted to replicate some of the products provided at the AWCs, at their homes. Despite comprehending these incremental benefits of millets, mothers outlined and expressed concerns regarding the longer cooking time of millet meals compared to rice. This implies that there is scope for behavioural change communication interventions, complemented with sharing of nutritious recipes and their preparation protocols with the mothers, in their local languages. The government could allocate further funds towards research and development and pilot testing of easy cooking and inclusive millet-based recipes. Further, to facilitate behavioural change towards dietary diversity in rice-based meal consumption patterns and to provide ease of work for the AWC staff workers in terms of the number of preparations, interventions must be integrated to provide millets in mid-day meal (MDM) rather than as an additional meal with rice-based mid-day meal. The Uttar Pradesh Government has taken steps in this direction by deciding to incorporate millets in the form of 'Bajra khichdi' in the MDM provided to students [
31].
A similar discussion with AWC teachers revealed that the prevalent practices and preference for rice production were catalysed by water availability. Further, they also highlighted that millet production involved high risks and high production costs (labour cost for bird scaring, anti-bird net to prevent loss by birds and animals which is comparatively more in tribal-dense forest areas). The above statements indicate the need for further intensifying efforts by the government to encourage diversified farming systems in the country through appropriate incentives and better market linkages along with promoting current policies supporting millet production. The PDS could purchase more millets through Food Corporation of India (FCI) across the country and distribute it for consumption through the Fair Price Shops (FPSs) ration and school feeding programs, creating enhanced demand and markets for millets. Inclusion of millets in the PDS policy at an affordable price along with sensitization about the health benefits of millet consumption will result in sustained “demand pull” for millets.
Thus, apart from the nutritional benefits that are shown to be positively correlated with the intervention, the study also upholds significant implications for formulating appropriate polices to promote “demand driven” production of millets and related value-added products. Thus, the results from the current millet-pulse-groundnut based nutrition intervention study confirm that the improved growth and nourishment among the tribal children can be brought about by diversifying the diets to include millets, pulses and oilseeds. Apart from the statistical results, the conclusion is also empirically corroborated by the fact that AWC teachers reported a noticeable change in health and cognitive status among the children, during the intervention period (Table S2).
5. Conclusions
It is noteworthy that micronutrient demand is still unmet through natural diets even in the developed countries. Thus, concerted efforts to strengthen existing food systems in response to climate crisis and malnutrition is the need of the hour. In this regard, incorporating climate-resilient nutritious crops such as millets in the diet systems for creating resilient and sustainable agri-food systems is one of the solutions. Interventions such as the one described in the study are one of the solutions by which millets can gain importance in daily diets. The intervention was successful in improving the nutrition status of the children monitored, from being moderately acute malnourished to normal category. This study, thus, provides evidence to suggest that the interventions that are co-developed and co-designed with the relevant target population and stakeholders/community participation and undergo timely administration have high potential for achieving the desired impacts. Such interventions are likely to drive behavioural changes in consumption patterns. The International Year of Millets 2023 (IYM23) has provided us with the right opportunity to further scale-up such initiatives for future. IYM23 has attracted the global community by showcasing millets as potential solution for achieving climate-resilient and sustainable food systems and thus achieve nutritional security. The mission has paved way for global collaborative R&D support for the generation of strong evidence-base towards further understanding and promoting awareness on the health benefits of millets. Initiatives such as these, are suitable and efficient responses to combat the triple burden of malnutrition and also contribute to the growing evidence base of the nutritional benefits of millets.
Though this study was localized in its effects and was conducted in some of the tribal regions of Telangana, adaptation and scaling-up of such initiatives throughout India and in other developing countries and other parts of the world, where millets and pulses are common, and malnutrition is widespread would ensure significant progress towards building a food-secure society.
Author Contributions
Conceptualization, S.D.M. and Ar.S.; methodology, S.D.M, V.A, N.S; scientific methods for product validation R.B, P.D; data analysis, T.N, An.S, A.R, J.P; investigation, P.D, T.N, D.N, H.M, S.B, An.S; resources, S.D.M. and Ar.S; data curation, An.S, J.P, T.N, A.R; writing, review and editing S.D.M, V.A, An.S, T.N, R.B, A.R, D.B; project administration, T.N, P.D, D.N, H.M; detailed inputs in policy section, D.B.; funding acquisition, S.D.M, Ar.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Department of Tribal Welfare, Government of Telangana, bearing sanction letter number RC. No. G1/259415/2020-3.
Institutional Review Board Statement
The study was conducted with ethical approval, obtained from ICRISAT’s Institutional Review Board (IRB), which is the body responsible, for ensuring that all research involving humans is carried out in an ethical manner. Further details of the ethical approval are provided in section Materials and Methods, sub section Ethical Approval.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
Secretary & Commissioner-Tribal Welfare, Officials- Department of Tribal Welfare, Project Officers- ITDA, District Welfare Officers, Child Development Project Officers, ICDS Supervisors and Anganwadi Teachers. The team acknowledges Mr. Mohammed Irshad Ahmed, ICRISAT for generating GIS map of the study sites.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vaidyanathan, G. What Humanity Should Eat to Stay Healthy and Save the Planet. Nature 2021, 600, 22–25. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 9 November 2022).
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; Jonell, M.; Clark, M.; Gordon, L.J.; Fanzo, J.; Hawkes, C.; Zurayk, R.; Rivera, J.A.; De Vries, W.; Majele Sibanda, L.; Afshin, A.; Chaudhary, A.; Herrero, M.; Agustina, R.; Branca, F.; Lartey, A.; Fan, S.; Crona, B.; Fox, E.; Bignet, V.; Troell, M.; Lindahl, T.; Singh, S.; Cornell, S.E.; Srinath Reddy, K.; Narain, S.; Nishtar, S.; Murray, C.J.L. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Vetriventhan, M.; Azevedo, V.C.R.; Upadhyaya, H.D.; Nirmalakumari, A.; Kane-Potaka, J.; Anitha, S.; Ceasar, S.A.; Muthamilarasan, M.; Bhat, B.V.; Hariprasanna, K.; Bellundagi, A.; Cheruku, D.; Backiyalakshmi, C.; Santra, D.; Vanniarajan, C.; Tonapi, V.A. Genetic and Genomic Resources, and Breeding for Accelerating Improvement of Small Millets: Current Status and Future Interventions. Nucleus 2020, 63, 217–239. [Google Scholar] [CrossRef]
- Longvah, T.; An̲antan̲, I.; Bhaskarachary, K.; Venkaiah, K. Indian Food Composition Tables; National Institute of Nutrition, Indian Council of Medical Research: Hyderabad, Telangana State, India, 2017. [Google Scholar]
- Anitha, S.; Kane-Potaka, J.; Tsusaka, T.W.; Botha, R.; Rajendran, A.; Givens, D.I.; Parasannanavar, D.J.; Subramaniam, K.; Prasad, K.D.V.; Vetriventhan, M.; Bhandari, R.K. A Systematic Review and Meta-Analysis of the Potential of Millets for Managing and Reducing the Risk of Developing Diabetes Mellitus. Front. Nutr. 2021, 8, 687428. [Google Scholar] [CrossRef]
- Anitha, S.; Botha, R.; Kane-Potaka, J.; Givens, D.I.; Rajendran, A.; Tsusaka, T.W.; Bhandari, R.K. Can Millet Consumption Help Manage Hyperlipidemia and Obesity?: A Systematic Review and Meta-Analysis. Front. Nutr. 2021, 8, 700778. [Google Scholar] [CrossRef]
- Anitha, S.; Kane-Potaka, J.; Botha, R.; Givens, D.I.; Sulaiman, N.L.B.; Upadhyay, S.; Vetriventhan, M.; Tsusaka, T.W.; Parasannanavar, D.J.; Longvah, T.; Rajendran, A.; Subramaniam, K.; Bhandari, R.K. Millets Can Have a Major Impact on Improving Iron Status, Hemoglobin Level, and in Reducing Iron Deficiency Anemia–A Systematic Review and Meta-Analysis. Front. Nutr. 2021, 8, 725529. [Google Scholar] [CrossRef]
- Anitha, S.; Kane-Potaka, J.; Tsusaka, T.W.; Tripathi, D.; Upadhyay, S.; Kavishwar, A.; Jalagam, A.; Sharma, N.; Nedumaran, S. Acceptance and Impact of Millet-Based Mid-Day Meal on the Nutritional Status of Adolescent School Going Children in a Peri Urban Region of Karnataka State in India. Nutrients 2019, 11, 2077. [Google Scholar] [CrossRef]
- Anitha, S.; Givens, D.I.; Subramaniam, K.; Upadhyay, S.; Kane-Potaka, J.; Vogtschmidt, Y.D.; Botha, R.; Tsusaka, T.W.; Nedumaran, S.; Rajkumar, H.; Rajendran, A.; Parasannanavar, D.J.; Vetriventhan, M.; Bhandari, R.K. Can Feeding a Millet-Based Diet Improve the Growth of Children?—A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 225. [Google Scholar] [CrossRef]
- Wangari, C.; Mwema, C.; Siambi, M.; Silim, S.; Ubwe, R.; Malesi, K.; Anitha, S.; Kane-Potaka, J. Changing Perception through a Participatory Approach by Involving Adolescent School Children in Evaluating Smart Food Dishes in School Feeding Programs – Real-Time Experience from Central and Northern Tanzania. Ecol. Food Nutr. 2020, 59, 472–485. [Google Scholar] [CrossRef]
- Telangana, D. of W. D. and C. W. D. In Supplementary Nutrition Programme (SNP); Department of Women Development and Child Welfare; Available online: https://wdcw.tg.nic.in/Supplementary_Nutrition.html (accessed on 22 March 2023).
- Supplementary Nutrition Programme, PIB, GOI. February 21, 2014. 2014. Available online: https://pib.gov.in/newsite/printrelease.aspx?relid=104046 (accessed on 14 November 2022).
- Stata Statistical Software, StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Anitha, S.; Givens, D.; Botha, R.; Kane-Potaka, J.; Sulaiman, N.; Tsusaka, T.; Subramaniam, K.; Rajendran, A.; Parasannanavar, D.; Bhandari, R. Calcium from Finger Millet—A Systematic Review and Meta-Analysis on Calcium Retention, Bone Resorption, and In Vitro Bioavailability. Sustainability 2021, 13, 8677. [Google Scholar] [CrossRef]
- Kumar, A.; Tomer, V.; Kaur, A.; Kumar, V.; Gupta, K. Millets: A Solution to Agrarian and Nutritional Challenges. Agric. Food Secur. 2018, 7, 31. [Google Scholar] [CrossRef]
- Sabuz, A.A.; Rana, M.R.; Ahmed, T.; Molla, M.M.; Islam, N.; Khan, H.H.; Chowdhury, G.F.; Zhao, Q.; Shen, Q. Health-Promoting Potential of Millet: A Review. Separations 2023, 10, 80. [Google Scholar] [CrossRef]
- Diet and Nutritional Status of Tribal Population and Prevalence of Hypertension among Adults; Tribal-Second Repeat Survey; Report on Second Repeat Survey NNMB Technical Report No.25; National Institution of Nutrition-ICMR: Hyderabad, Telangana State, India, 2009. Available online: https://www.nin.res.in/downloads/NNMBTribalReport.pdf (accessed on 9 June 2023).
- Deol, T. No meat, more wheat: How tribal diets are changing in Madhya Pradesh. Available online: https://www.downtoearth.org.in/news/food/no-meat-more-wheat-how-tribal-diets-are-changing-in-madhya-pradesh-82878 (accessed on 9 June 2023).
- Department of Nutrition and Dietetics, Symbiosis Institute of Health Science, Symbiosis International University (Deemed) Pune, 411042 *, India; Devulapalli, D.; Gokhale, D. Impact of Millet-Based Interventions on Weight, Body Mass Index and Haemoglobin of School-Going Adolescent Girls. IJST 2022, 15, 983–988. [Google Scholar] [CrossRef]
- Suri, S.; Dutta, A.; Chandra Shahi, N.; Raghuvanshi, R.S.; Singh, A.; Chopra, C.S. Numerical Optimization of Process Parameters of Ready-to-Eat (RTE) Iron Rich Extruded Snacks for Anemic Population. LWT 2020, 134, 110164. [Google Scholar] [CrossRef]
- Durairaj, M.; Gurumurthy, G.; Nachimuthu, V.; Muniappan, K.; Balasubramanian, S. Dehulled Small Millets: The Promising Nutricereals for Improving the Nutrition of Children. Matern. Child. Nutr. 2019, 15. [Google Scholar] [CrossRef]
- Khader, V. Effect of Feeding Malted Foods on the Nutritional Status of Pregnant Women, Lactating Women and Preschool Children in Lepakshi Mandal of Ananthapur District, Andhra Pradesh, India. Int. J. Biotechnol. Mol. Biol. Res. 2012, 3, 35–46. [Google Scholar] [CrossRef]
- Aggarwal, A.; Aggarwal, A.; Goyal, S.; Aggarwal, S. Iron-Deficiency Anaemia among Adolescents: A Global Public Health Concern. Int. J. Adv. Community Med. 2020, 3, 35–40. [Google Scholar] [CrossRef]
- (WHO), W.H.O. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. WHO/NMH/NHD/MNM/11.1.
- Taffé, P. Assessing Bias, Precision, and Agreement in Method Comparison Studies. Stat Methods Med Res 2020, 29, 778–796. [Google Scholar] [CrossRef]
- Taffé, P.; Halfon, P.; Halfon, M. A New Statistical Methodology Overcame the Defects of the Bland–Altman Method. J. Clin. Epidemiol. 2020, 124, 1–7. [Google Scholar] [CrossRef]
- Langyan, S.; Yadava, P.; Khan, F.N.; Bhardwaj, R.; Tripathi, K.; Bhardwaj, V.; Bhardwaj, R.; Gautam, R.K.; Kumar, A. Nutritional and Food Composition Survey of Major Pulses Toward Healthy, Sustainable, and Biofortified Diets. Front. Sustain. Food Syst. 2022, 6, 878269. [Google Scholar] [CrossRef]
- Arya, S.S.; Salve, A.R.; Chauhan, S. Peanuts as Functional Food: A Review. J Food Sci Technol 2016, 53, 31–41. [Google Scholar] [CrossRef]
- Beal, T.; Ortenzi, F.; Fanzo, J. Estimated Micronutrient Shortfalls of the EAT–Lancet Planetary Health Diet. Lancet Planet. Health 2023, 7, e233–e237. [Google Scholar] [CrossRef]
- Hindusthan Times, India. Millets in ‘Bajra Khichdi’ Form to Be Included in Mid-Day Meals. August 19, 2023 edition. Available online: https://www.hindustantimes.com/cities/lucknow-news/up-government-to-include-millets-in-mid-day-meals-to-boost-farmers-income-and-encourage-millet-consumption-101692386445187.html.
| 1 |
Indian Food Composition Tables, 2017; National Institute of Nutrition, Indian Council of Medical Research |
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
Figure 1.
Flowchart of administrative divisions of study areas in Eturunagaram and Bhadrachalam ITDAs. E – Preschool children enrolled for the Giri Poshana programme in target ITDAs; M – Mothers of the pre-school children who participated in the FGDs; T – Anganwadi teachers interviewed; Control – children who did not receive millet feed and were followed up for the anthropometric measurements for the entire duration of the study; Intervention – children who received millet feed and were followed up for the anthropometric measurements for the entire duration of the study; E,M,T, Control and Intervention are the total number of individuals across three and five Mandals (M) in the two districts (D); Location: Anthropometry measurements, FGDs and key informant interviews were conducted at Anganwadi centres in the respective areas.
Figure 1.
Flowchart of administrative divisions of study areas in Eturunagaram and Bhadrachalam ITDAs. E – Preschool children enrolled for the Giri Poshana programme in target ITDAs; M – Mothers of the pre-school children who participated in the FGDs; T – Anganwadi teachers interviewed; Control – children who did not receive millet feed and were followed up for the anthropometric measurements for the entire duration of the study; Intervention – children who received millet feed and were followed up for the anthropometric measurements for the entire duration of the study; E,M,T, Control and Intervention are the total number of individuals across three and five Mandals (M) in the two districts (D); Location: Anthropometry measurements, FGDs and key informant interviews were conducted at Anganwadi centres in the respective areas.
Figure 2.
ITDA-Eturunagaram showing mandals involved in the study.
Figure 2.
ITDA-Eturunagaram showing mandals involved in the study.
Figure 3.
ITDA-Bhadrachalam showing mandals involved in the study .
Figure 3.
ITDA-Bhadrachalam showing mandals involved in the study .
Figure 4.
Comparison of Z-scores for wasting or weight for height (WHZ) curve with WHO standard curve, at baseline and at endline (post intervention using millet—pulse-groundnut based formulations) of pre-school children in (a) treatment group (mean WHZ moved from -1.2 ±1.3 to -0.9± 1) (b) control group (mean WHZ from -1.2±1 to -1.4±1.1).
Figure 4.
Comparison of Z-scores for wasting or weight for height (WHZ) curve with WHO standard curve, at baseline and at endline (post intervention using millet—pulse-groundnut based formulations) of pre-school children in (a) treatment group (mean WHZ moved from -1.2 ±1.3 to -0.9± 1) (b) control group (mean WHZ from -1.2±1 to -1.4±1.1).
Figure 5.
Comparison of Z-scores for stunting or height for age (HAZ) curve with WHO standard curve, at baseline and at endline (post intervention using millet—pulse-groundnut based formulations) of pre-school children in (a) treatment group (mean HAZ moved from.-1.8±1.6 to -0.3±1.3); (b) control group (-2.0±1.7 to – 0.8±1.3).
Figure 5.
Comparison of Z-scores for stunting or height for age (HAZ) curve with WHO standard curve, at baseline and at endline (post intervention using millet—pulse-groundnut based formulations) of pre-school children in (a) treatment group (mean HAZ moved from.-1.8±1.6 to -0.3±1.3); (b) control group (-2.0±1.7 to – 0.8±1.3).
Figure 6.
Comparison of Z-scores for underweight or weight for age (WAZ) curve with WHO standard curve, at baseline and at endline (post intervention using millet—pulse-groundnut based formulations) of pre-school children in (a) treatment group (mean WAZ moved from -1.9±1.2 to -0.7±1); (b) control group (mean WAZ from -1.9±1 to -1.4±1).
Figure 6.
Comparison of Z-scores for underweight or weight for age (WAZ) curve with WHO standard curve, at baseline and at endline (post intervention using millet—pulse-groundnut based formulations) of pre-school children in (a) treatment group (mean WAZ moved from -1.9±1.2 to -0.7±1); (b) control group (mean WAZ from -1.9±1 to -1.4±1).
Figure 7.
Preference of food products by children from Bhadrachalam and Eturunagaram ITDAs.
Figure 7.
Preference of food products by children from Bhadrachalam and Eturunagaram ITDAs.
Table 1.
Nutrient profile of the products provided during the intervention.
Table 1.
Nutrient profile of the products provided during the intervention.
| Nutrition parameters tested (per 100g of the product) |
Ready-to-cook |
Ready-to-eat |
| Sorghum meal |
Multigrain meal |
Multigrain sweet meal |
Nutri-cookies |
Energy bar |
Energy bytes |
| Energy (Kcal) |
362.1 |
350.4 |
446.1 |
472.4 |
509.1 |
462.9 |
| Protein (g) |
12.3 |
14.6 |
4.8 |
5.8 |
16.0 |
9.0 |
| Fat (g) |
4.8 |
2.2 |
15.1 |
25.2 |
24.9 |
24.5 |
| Carbohydrate (g) |
65.4 |
66.0 |
75.0 |
55.7 |
54.5 |
51.5 |
| Calcium (mg) |
47.1 |
70.0 |
47.0 |
71.2 |
188.5 |
31.9 |
| Iron (mg) |
4.5 |
4.3 |
2.9 |
1.9 |
5.6 |
2.3 |
Table 2.
Results of acceptability study conducted using millet-pulse-groundnut based products (pre-intervention) among the pre-school children.
Table 2.
Results of acceptability study conducted using millet-pulse-groundnut based products (pre-intervention) among the pre-school children.
| Product name |
Children (%) accepting a product (Eturunagaram) |
Children (%) accepting a product (Bhadrachalam) |
| Sorghum meal |
95 |
80 |
| Multigrain meal |
80.7 |
93 |
| Multigrain sweet meal |
85.5 |
100 |
| Energy bar |
100 |
100 |
| Energy bytes |
96.8 |
100 |
| Nutri-cookies |
85.5 |
100 |
Table 3.
Differences in mean anthropometric measures.
Table 3.
Differences in mean anthropometric measures.
| Anthropometry |
Treatment |
Control |
|
| Baseline |
Std. dev |
Endline |
Std. dev |
p value |
Difference
(DT)#
|
Baseline |
Std. dev |
Endline |
Std.dev |
p value |
Difference
(DC)#
|
DT-DC |
| Height (in cm) |
91.3 |
8.72 |
104.1 |
7.51 |
0.000*** |
12.8 |
90.1 |
10.36 |
99.7 |
9.13 |
0.000*** |
9.6 |
3.2 |
| Weight (in kg) |
11.9 |
2.26 |
15.5 |
2.34 |
0.000*** |
3.58 |
11.7 |
2.27 |
13.6 |
2.53 |
0.000*** |
1.9 |
1.68 |
| MUAC( in cm) |
14.57 |
1.38 |
15.6 |
1.84 |
0.000*** |
0.99 |
15.1 |
1.02 |
15.7 |
2.08 |
0.007*** |
0.66 |
0.33 |
Table 4.
The change (% change and % difference at endline, in relation to baseline) of children in the categories of wasting, stunting, and underweight between intervention and control groups of pre-school children (3 to 6 years). .
Table 4.
The change (% change and % difference at endline, in relation to baseline) of children in the categories of wasting, stunting, and underweight between intervention and control groups of pre-school children (3 to 6 years). .
| Status of Treatment Group Vs Control Group |
Wasting (%) |
Stunting (%) |
Underweight (%) |
Severely wasted
(WHZ<-3) |
Wasted
(WHZ >-3 to <-2)
|
Normal |
Severely stunted
(HAZ<-3) |
Stunted
(HAZ >-3 to <-2) |
Normal
|
Severely Thinness
(WAZ<-3) |
Thinness
(WAZ >-3 to <-2) |
Normal |
A. Treatment
Group
|
|
| Baseline |
7.2 |
20.8 |
72.0 |
20.8 |
25.7 |
53.4 |
18.6 |
27.0 |
54.4 |
| Endline |
2.0 |
10.1 |
87.9 |
2.6 |
4.6 |
92.8 |
1.0 |
8.5 |
90.6 |
B. Control
Group
|
|
| Baseline |
4.9 |
14.8 |
80.2 |
17.3 |
24.7 |
58.0 |
8.6 |
33.3 |
58.0 |
| Endline |
6.2 |
22.2 |
71.6 |
6.2 |
18.5 |
75.3 |
7.4 |
19.8 |
72.8 |
| Difference (%) Treatment Vs Control |
% Difference in wasting |
% Difference in stunting |
% Difference in Underweight |
| Treatment |
-72.7 |
-51.6 |
22.2 |
-87.5 |
-82.3 |
+73.8 |
-94.7 |
-68.7 |
+66.5 |
| Control |
+25.0 |
+50.0 |
-10.8 |
-64.3 |
-25.0 |
+29.8 |
-14.3 |
-40.7 |
+25.5 |
Table 5.
Acceptance score of the products provided in both ITDAs.
Table 5.
Acceptance score of the products provided in both ITDAs.
| Food Products |
Mean of acceptance rating for the products* |
Ranking |
| Energy Bar |
4.7±1.2 |
1 |
| Nutri-Cookies |
3.7±1.3 |
2 |
| Energy Bytes |
3.6±1.2 |
3 |
| Multigrain Sweet meal |
3.5±1.8 |
4 |
| Sorghum meal |
2.0±1.1 |
5 |
| Multigrain meal |
1.4±1.3 |
6 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).