Submitted:
09 January 2024
Posted:
10 January 2024
You are already at the latest version
Abstract
Keywords:
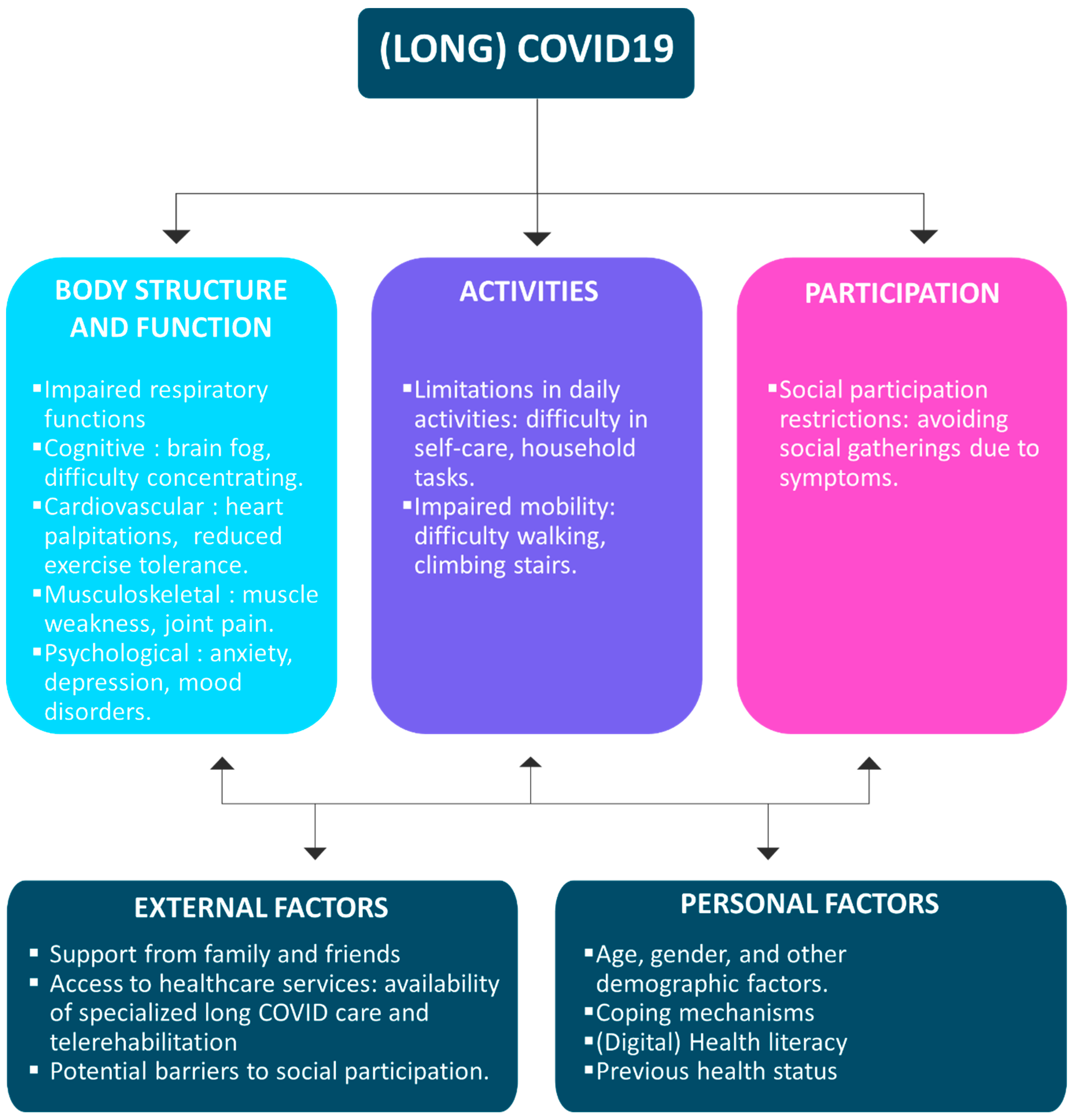
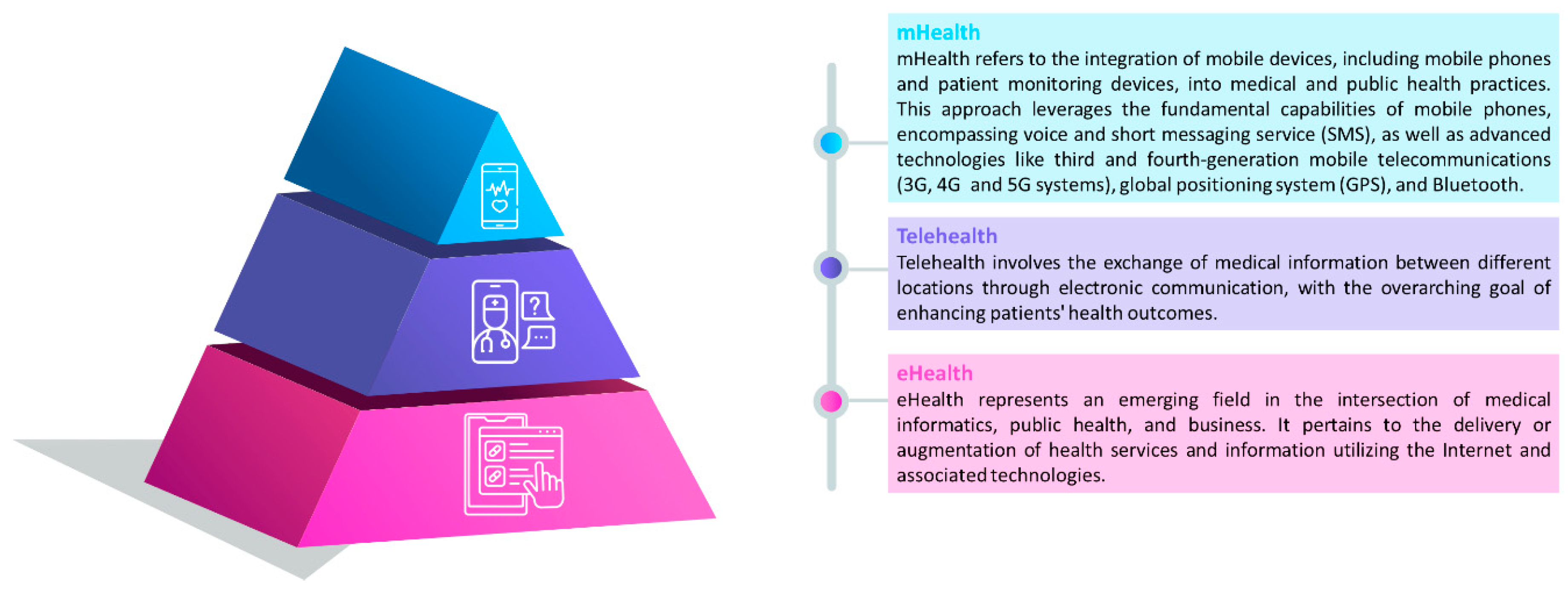
1. Introduction
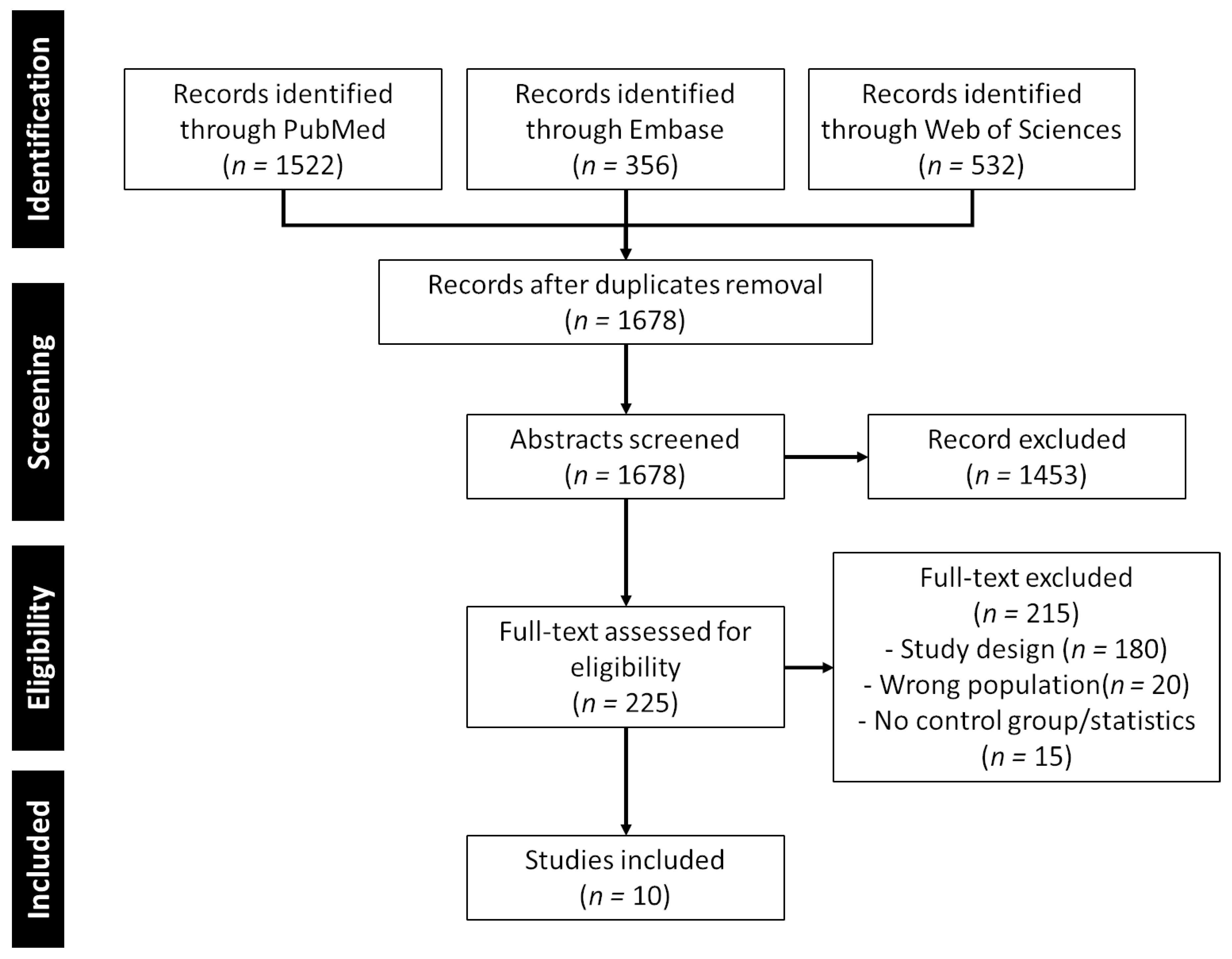
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Quality Assessment
2.4. Data Extraction
2.5. Ethical Approval
3. Results
3.1. Characteristics of the Included Studies and Patients
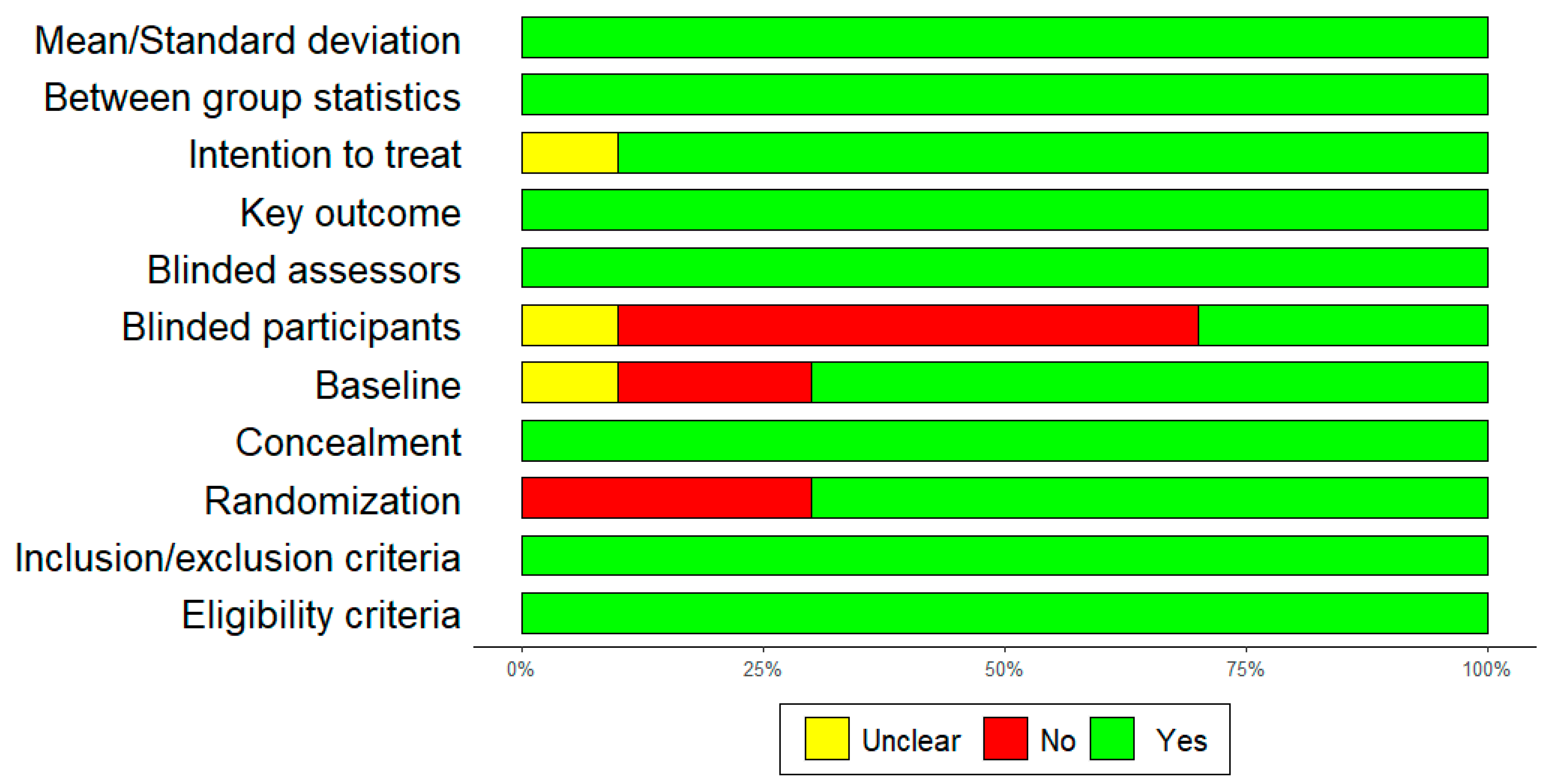
3.2. Qualitity Assessment
3.3. Evaluation Variables
3.4. Telerehabilitation Methods
3.5. Clinical Efficacy
3.5.1. Physical Function and Exercise Capacity
3.5.2. Mental Health and Quality of Life
3.5.3. Sleep Quality and Fatigue
3.5.4. Cognitive Function
| Study, country | Population | Intervention | Control | Outcomes | Results | Quality |
|---|---|---|---|---|---|---|
|
Samper-Pardo et al. 2023 Spain [30] |
100 Primary Health Care long COVID patients (18+) |
n = 52 ReCOVery APP and standard therapy |
n = 48 Treatment as usual methods established by their general practitioner |
Quality of life (SF-36), Sociodemographic variables, self-reported persistent symptoms, use of ReCOVery APP, cognitive domains (MoCA), physical functioning, Affective status (HADS); Sleep quality (ISI), social support (MOS-SS); Community social support (PCSQ), Physical Activity (IPAQ-SF), personal factors | Approximately 25% of participants actively utilized the app. Results from a linear regression model indicate that increased usage time predicts enhanced physical function (b = 0.001; p = 0.005) and community social support (b = 0.004; p = 0.021). Additionally, heightened self-efficacy and health literacy are associated with improved cognitive function (b = 0.346; p = 0.001) and a reduction in symptoms (b = 0.226; p = 0.002). | 8 |
|
Churchill et al., 2023 USA [24] |
44 participants discharged home following hospitalisation with COVID-19 (with and without intensive care unit (ICU) stay) <40 |
n = 27 Physical therapy and education sessions |
n = 14 Weekly check-in calls |
Demographics, Physical function testing, a health diar via fitbit Steps |
Step counts increased in favour of the intervention group (P <.001) culminating in an average daily step count of 7658 (P<.001) at the end of week 3. During the remaining 9 weeks, weekly step counts increased by an average of 67 (P<.001) steps per week, resulting in a final estimate of 8258 (P<.001) |
8 |
|
Hajibashi et al., 2023 Iran [29] |
52 Discharged COVID-19 patients (18–65) |
n = 26 pulmonary telerehabilitation and progressive muscle relaxation for 6 weeks |
n = 26 pulmonary telerehabilitation fir 6 weeks |
Functional capacity and secondary (dyspnoea, anxiety, depression, fatigue, sleep quality, and quality of life | The experimental group showed significantly higher sleep quality (P = 0.001) and significantly lower fatigue (P = 0.041) and anxiety (P = 0.001) than the comparison group. No between-group differences were observed in terms of other outcomes (P > 0.05) | 10 |
|
Campos et al., 2023 Brazil [31] |
37 Adults with persistent symptoms of COVID-19 |
n = 15 Remote monitoring with health guidance |
n = 22 Face to face rehabilitation 8 weeks (2/week) |
Fatigue, dyspnea, and exercise capacity, Lung function, functional status, symptoms of anxiety and depression, attention, memory, handgrip strength, and knee extensor strength were secondary outcome measures | Both groups showed improved fatigue and exercise capacity. Exercise rehabilitation improved dyspnea, anxiety, attention, and short-term memory. | 8 |
|
Capin et al., 2022 USA [26] |
44 Participants discharged home following hospitalisation with COVID-19 (with and without intensive care unit (ICU) stay) |
n = 29 12 individual biobehaviourally informed, app-facilitated, multicomponent telerehabilitation sessions with a licenced physical therapist |
n = 15 Education on exercise and COVID-19 recovery trajectory, physical activity and vitals monitoring, and weekly check-ins with study staff. |
Primary outcome was feasibility, including safety and session adherence. Secondary outcomes included preliminary efficacy outcomes including tests of function and balance; patient-reported outcome measures; a cognitive assessment; and average daily step count. The 30 s chair stand test was the main secondary (efficacy) outcome | 8% (11/29) of the intervention group compared with 60% (9/15) of the control group experienced an AE (p=0.21), most of which were minor, over the course of the 12-week study. 27 of 29 participants (93%; 95% CI 77% to 99%) receiving the intervention attended ≥75% of sessions. Both groups demonstrated clinically meaningful improvement in secondary outcomes with no statistically significant differences between groups. | 8 |
|
Rodriguez-Blanco, 2021 Spain [25] |
36 COVID-19 patients with mild to moderate symptomatology in the acute stage |
n = 18 Muscle conditioning telerehabilitation |
n = 18 No physical activity |
Six-minute walking test, multidimensional dyspnoea-12, thirty seconds sit-to-stand test, and Borg Scale | Both groups were comparable at baseline. Statistically significant improvement between groups (p < 0.05) in favor of the experimental group was obtained. Ninety percent adherence was found in our program. | 6 |
|
Li et al., 2022 China [32] |
120 Formerly hospitalised COVID-19 survivors with remaining dyspnoea complaints |
n = 59 TERECO Unsupervised home-based 6-week exercise programme comprising breathing control and thoracic expansion, aerobic exercise and LMS exercise, delivered via smartphone, and remotely monitored with heart rate telemetry. |
n = 61 Short educational instructions |
6 min walking distance (6MWD), squat time in seconds; pulmonary function assessed by spirometry; HRQOL measured (SF-12) and mMRC-dyspnea. | Adjusted between-group difference in change in 6MWD was 65.45 m (p<0.001) at post-treatment and 68.62 m (p<0.001) at follow-up. Treatment effects for LMS were 20.12 s (p<0.001) post-treatment and 22.23 s (p<0.001) at follow-up. No group differences were found for lung function except post-treatment maximum voluntary ventilation. Increase in SF-12 physical component was greater in the TERECO group with treatment effects estimated as 3.79 (p=0.004) at post-treatment and 2.69 (p=0.045) at follow-up. | 7 |
|
Gonzalez-Gerez et al., 2021 Spain [33] |
38 COVID-19 patients with mild to moderate symptomatology in the acute stage (18 – 75 years old) |
n = 19 Pulmonary rehabilitation |
n = 19 No physical activity |
Six-Minute Walk Test, Multidimensional Dyspnoea-12, Thirty-Second Sit-To-Stand Test, and Borg Scale. | Significant differences were found for all of the outcome measures in favor of the experimental group (P< 0.05). | 9 |
| Wei et al., 2020 China [27] | 26 COVID-19 patients (40 – 50 years old) |
n = 13 Self-help intervention containing four main components: breath relaxation training, mindfulness (body scan), “refuge” skills, and butterfly hug method. |
n = 13 Supportive care |
Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale | Depression and anxiety were significantly decreased in patients of the intervention group at the end of the first and second weeks when compared with the patients of the control group |
9 |
|
Liu et al., 2021 China [28] |
252 COVID-19 patients (45 – 45 years old) |
n = 126 Computerized cognitive behavioral therapy (cCBT). The system can systematically intervene in patients’cognition, emotions, and behavior through an offline mobile terminal. |
n = 126 Conventional treatment (periodic psychological assessments, general psychological support, and consultations discussing overall well-being and disease activity) |
Hamilton Depression Rating Scale, Hamilton Anxiety Rating Scale, Self-Rating Depression Scale, Self-Rating Anxiety Scale, Athens Insomnia Scale | The cCBT group displayed a significantly decreased scores after the intervention compared to the conventional group (all P<.001). A mixed-effects repeated measures model revealed significant improvement in symptoms of depression, anxiety and insomnia during the postintervention and follow-up periods in the cCBT group | 8 |
4. Discussion
4.1. Main Findings
4.2. Limitation of the Systematic Review
4.3. Future and Related Works
4.4. Implications for the Rehabilitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed 2020, 91, 157–160. [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239. [CrossRef]
- Burn, E.; Tebé, C.; Fernandez-Bertolin, S.; Aragon, M.; Recalde, M.; Roel, E.; Prats-Uribe, A.; Prieto-Alhambra, D.; Duarte-Salles, T. The Natural History of Symptomatic COVID-19 during the First Wave in Catalonia. Nat Commun 2021, 12, 777. [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an Acute to Chronic Disease? Potential Long-Term Health Consequences. Critical Reviews in Clinical Laboratory Sciences 2021, 58, 297–310. [CrossRef]
- Alwan, N.A. Surveillance Is Underestimating the Burden of the COVID-19 Pandemic. The Lancet 2020, 0. [CrossRef]
- Luo, Y.; Li, Q.; Jeong, H.; Cheatham, L. The Association between Social Determinants of Health and Psychological Distress during the COVID-19 Pandemic: A Secondary Analysis among Four Racial/Ethnic Groups. BMC Public Health 2022, 22, 2193. [CrossRef]
- Eadie, T.L. The ICF: A Proposed Framework for Comprehensive Rehabilitation of Individuals Who Use Alaryngeal Speech. Am J Speech Lang Pathol 2003, 12, 189–197. [CrossRef]
- Angeli, J.M.; Schwab, S.M.; Huijs, L.; Sheehan, A.; Harpster, K. ICF-Inspired Goal-Setting in Developmental Rehabilitation: An Innovative Framework for Pediatric Therapists. Physiother Theory Pract 2019, 1–10. [CrossRef]
- Hartasanchez, S.A.; Heen, A.F.; Kunneman, M.; García-Bautista, A.; Hargraves, I.G.; Prokop, L.J.; May, C.R.; Montori, V.M. Remote Shared Decision Making through Telemedicine: A Systematic Review of the Literature. Patient Educ Couns 2022, 105, 356–365. [CrossRef]
- Ward, K.; Vagholkar, S.; Sakur, F.; Khatri, N.N.; Lau, A.Y.S. Visit Types in Primary Care With Telehealth Use During the COVID-19 Pandemic: Systematic Review. JMIR Med Inform 2022, 10, e40469. [CrossRef]
- Nanda, M.; Sharma, R. A Review of Patient Satisfaction and Experience with Telemedicine: A Virtual Solution During and Beyond COVID-19 Pandemic. Telemed J E Health 2021, 27, 1325–1331. [CrossRef]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. JMIR Rehabil Assist Technol 2017, 4, e7. [CrossRef]
- Rahmati, M.; Udeh, R.; Yon, D.K.; Lee, S.W.; Dolja-Gore, X.; McEVoy, M.; Kenna, T.; Jacob, L.; López Sánchez, G.F.; Koyanagi, A.; et al. A Systematic Review and Meta-Analysis of Long-Term Sequelae of COVID-19 2-Year after SARS-CoV-2 Infection: A Call to Action for Neurological, Physical, and Psychological Sciences. J Med Virol 2023, 95, e28852. [CrossRef]
- Brigo, E.; Rintala, A.; Kossi, O.; Verwaest, F.; Vanhoof, O.; Feys, P.; Bonnechère, B. Using Telehealth to Guarantee the Continuity of Rehabilitation during the COVID-19 Pandemic: A Systematic Review. Int J Environ Res Public Health 2022, 19, 10325. [CrossRef]
- Huang, J.; Fan, Y.; Zhao, K.; Yang, C.; Zhao, Z.; Chen, Y.; Yang, J.; Wang, T.; Qu, Y. Do Patients with and Survivors of COVID-19 Benefit from Telerehabilitation? A Meta-Analysis of Randomized Controlled Trials. Front Public Health 2022, 10, 954754. [CrossRef]
- Vieira, A.G. da S.; Pinto, A.C.P.N.; Garcia, B.M.S.P.; Eid, R.A.C.; Mól, C.G.; Nawa, R.K. Telerehabilitation Improves Physical Function and Reduces Dyspnoea in People with COVID-19 and Post-COVID-19 Conditions: A Systematic Review. J Physiother 2022, 68, 90–98. [CrossRef]
- Seid, A.A.; Aychiluhm, S.B.; Mohammed, A.A. Effectiveness and Feasibility of Telerehabilitation in Patients with COVID-19: A Systematic Review and Meta-Analysis. BMJ Open 2022, 12, e063961. [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Int J Surg 2021, 88, 105906. [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A Comparison Study of Specificity and Sensitivity in Three Search Tools for Qualitative Systematic Reviews. BMC Health Serv Res 2014, 14. [CrossRef]
- de Morton, N.A. The PEDro Scale Is a Valid Measure of the Methodological Quality of Clinical Trials: A Demographic Study. Aust J Physiother 2009, 55, 129–133. [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys Ther 2003, 83, 713–721. [CrossRef]
- Moseley, A.M.; Rahman, P.; Wells, G.A.; Zadro, J.R.; Sherrington, C.; Toupin-April, K.; Brosseau, L. Agreement between the Cochrane Risk of Bias Tool and Physiotherapy Evidence Database (PEDro) Scale: A Meta-Epidemiological Study of Randomized Controlled Trials of Physical Therapy Interventions. PLoS One 2019, 14, e0222770. [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLOS Medicine 2009, 6, e1000100. [CrossRef]
- Churchill, L.; Morrow, M.; Capin, J.J.; Jolley, S.E.; Hare, K.; MaWhinney, S.; Stevens-Lapsley, J.E.; Erlandson, K.M. Using Wearable Technology to Quantify Physical Activity Recovery: Secondary Report From the AFTER (App-Facilitated Tele-Rehabilitation) Program for COVID-19 Survivors Randomized Study. JMIR Rehabil Assist Technol 2023, 10, e43436. [CrossRef]
- Rodriguez-Blanco, C.; Gonzalez-Gerez, J.J.; Bernal-Utrera, C.; Anarte-Lazo, E.; Perez-Ale, M.; Saavedra-Hernandez, M. Short-Term Effects of a Conditioning Telerehabilitation Program in Confined Patients Affected by COVID-19 in the Acute Phase. A Pilot Randomized Controlled Trial. Medicina 2021, 57, 684. [CrossRef]
- Capin, J.J.; Jolley, S.E.; Morrow, M.; Connors, M.; Hare, K.; MaWhinney, S.; Nordon-Craft, A.; Rauzi, M.; Flynn, S.; Stevens-Lapsley, J.E.; et al. Safety, Feasibility and Initial Efficacy of an App-Facilitated Telerehabilitation (AFTER) Programme for COVID-19 Survivors: A Pilot Randomised Study. BMJ Open 2022, 12, e061285. [CrossRef]
- Wei, N.; Huang, B.; Lu, S.; Hu, J.; Zhou, X.; Hu, C.; Chen, J.; Huang, J.; Li, S.; Wang, Z.; et al. Efficacy of Internet-Based Integrated Intervention on Depression and Anxiety Symptoms in Patients with COVID-19. J Zhejiang Univ Sci B 2020, 21, 400–404. [CrossRef]
- Liu, Z.; Qiao, D.; Xu, Y.; Zhao, W.; Yang, Y.; Wen, D.; Li, X.; Nie, X.; Dong, Y.; Tang, S.; et al. The Efficacy of Computerized Cognitive Behavioral Therapy for Depressive and Anxiety Symptoms in Patients With COVID-19: Randomized Controlled Trial. Journal of Medical Internet Research 2021, 23, e26883. [CrossRef]
- Hajibashi, A.; Sarrafzadeh, J.; Amiri, A.; Salehi, R.; Vasaghi-Gharamaleki, B. Effect of Progressive Muscle Relaxation as an Add-on to Pulmonary Telerehabilitation in Discharged Patients with COVID-19: A Randomised Controlled Trial. Complement Ther Clin Pract 2023, 51, 101730. [CrossRef]
- Samper-Pardo, M.; León-Herrera, S.; Oliván-Blázquez, B.; Méndez-López, F.; Domínguez-García, M.; Sánchez-Recio, R. Effectiveness of a Telerehabilitation Intervention Using ReCOVery APP of Long COVID Patients: A Randomized, 3-Month Follow-up Clinical Trial. Sci Rep 2023, 13, 7943. [CrossRef]
- Campos, M.C.; Nery, T.; Speck, A.E.; Arpini, M.; Antunes, M.M.; De Bem Alves, A.C.; De Souza Santos, N.; Matos, M.P.P.; Schmidt, N.; Bicca, L.R.; et al. Rehabilitation Improves Persistent Symptoms of COVID-19: A Non-Randomized, Controlled, Open Study in Brazil. Am J Phys Med Rehabil 2023. [CrossRef]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. A Telerehabilitation Programme in Post-Discharge COVID-19 Patients (TERECO): A Randomised Controlled Trial. Thorax 2022, 77, 697–706. [CrossRef]
- Gonzalez-Gerez, J.J.; Saavedra-Hernandez, M.; Anarte-Lazo, E.; Bernal-Utrera, C.; Perez-Ale, M.; Rodriguez-Blanco, C. Short-Term Effects of a Respiratory Telerehabilitation Program in Confined COVID-19 Patients in the Acute Phase: A Pilot Study. IJERPH 2021, 18, 7511. [CrossRef]
- Bonnechère, B.; Timmermans, A.; Michiels, S. Current Technology Developments Can Improve the Quality of Research and Level of Evidence for Rehabilitation Interventions: A Narrative Review. Sensors (Basel) 2023, 23, 875. [CrossRef]
- Hartman, M.; Mináriková, J.; Batalik, L.; Pepera, G.; Su, J.J.; Formiga, M.F.; Cahalin, L.; Dosbaba, F. Effects of Home-Based Training with Internet Telehealth Guidance in COPD Patients Entering Pulmonary Rehabilitation: A Systematic Review. Int J Chron Obstruct Pulmon Dis 2023, 18, 2305–2319. [CrossRef]
- Sapouna, V.; Kitixis, P.; Petrou, E.; Michailidou, T.; Dalamarinis, P.; Kortianou, E. Mobile Health Applications Designed for Self-Management of Chronic Pulmonary Diseases in Children and Adolescents: A Systematic Mapping Review. J Bras Pneumol 2023, 49, e20230201. [CrossRef]
- Garavand, A.; Khodaveisi, T.; Aslani, N.; Hosseiniravandi, M.; Shams, R.; Behmanesh, A. Telemedicine in Cancer Care during COVID-19 Pandemic: A Systematic Mapping Study. Health Technol (Berl) 2023, 1–14. [CrossRef]
- Fainardi, V.; Capoferri, G.; Tornesello, M.; Pisi, G.; Esposito, S. Telemedicine and Its Application in Cystic Fibrosis. J Pers Med 2023, 13, 1041. [CrossRef]
- Kepenek-Varol, B.; Zeren, M.; Dinçer, R.; Erkaya, S. Breathing and Relaxation Exercises Help Improving Fear of COVID-19, Anxiety, and Sleep Quality: A Randomized Controlled Trial. J Integr Complement Med 2022, 28, 579–586. [CrossRef]
- Baxter, C.A.; Carroll, J.-A.; Keogh, B.; Vandelanotte, C. Virtual Respiratory Therapy Delivered through a Smartphone App: A Mixed-Methods Randomised Usability Study. BMJ Open Respir Res 2022, 9, e001221. [CrossRef]
- Kohlbrenner, D.; Kuhn, M.; Stüssi-Helbling, M.; Nordmann, Y.; Spielmanns, M.; Clarenbach, C.F. Longitudinal Smartphone-Based Post-Hospitalisation Symptom Monitoring in SARS-CoV-2 Associated Respiratory Failure: A Multi-Centre Observational Study. Frontiers in Rehabilitation Sciences 2021, 2. [CrossRef]
- Del Corral, T.; Fabero-Garrido, R.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C.; Navarro-Santana, M.; López-de-Uralde-Villanueva, I. Home-Based Respiratory Muscle Training on Quality of Life and Exercise Tolerance in Long-Term Post-COVID-19: Randomized Controlled Trial. Ann Phys Rehabil Med 2023, 66, 101709. [CrossRef]
- Ahmadi Marzaleh, M.; Peyravi, M.; Azhdari, N.; Bahaadinbeigy, K.; Sharifian, R.; Samad-Soltani, T.; Sarpourian, F. Virtual Reality Applications for Rehabilitation of COVID-19 Patients: A Systematic Review. Health Sci Rep 2022, 5, e853. [CrossRef]
- Kirykowicz, K.; Jaworski, B.; Owen, J.; Kirschbaum, C.; Seedat, S.; van den Heuvel, L.L. Feasibility, Acceptability and Preliminary Efficacy of a Mental Health Self-Management App in Clinicians Working during the COVID-19 Pandemic: A Pilot Randomised Controlled Trial. Psychiatry Res 2023, 329, 115493. [CrossRef]
- Monteleone, G.; Terzulli, G.; Cefaloni, F.; Bonini, M.; Richeldi, L. The Impact of Telemedicine during Severe Acute Respiratory Syndrome Coronavirus 2 Pandemic and Future Perspectives: A Systematic Review. Respiration 2023, 102, 879–890. [CrossRef]
- Dixit, S.; Nandakumar, G. Promoting Healthy Lifestyles Using Information Technology during the COVID-19 Pandemic. Rev Cardiovasc Med 2021, 22, 115–125. [CrossRef]
- Shi, N.; Wong, A.K.C.; Wong, F.K.Y.; Sha, L. Mobile Health Application-Based Interventions to Improve Self-Management of Chemotherapy-Related Symptoms Among People with Breast Cancer Who Are Undergoing Chemotherapy: A Systematic Review. Oncologist 2023, 28, e175–e182. [CrossRef]
- Kashikar-Zuck, S.; Barnett, K.A.; Williams, S.E.; Pfeiffer, M.; Thomas, S.; Beasley, K.; Chamberlin, L.A.; Mundo, K.; Ittenbach, R.F.; Peugh, J.; et al. FIT Teens RCT for Juvenile Fibromyalgia: Protocol Adaptations in Response to the COVID 19 Pandemic. Contemp Clin Trials Commun 2022, 30, 101039. [CrossRef]
- Ali, O.I.; Abdelraouf, O.R.; El-Gendy, A.M.; Abdelgalil, A.A.; Abdelaal, A.K.; Dahlawi, H.A.; Selim, A.O. Efficacy of Telehealth Core Exercises during COVID-19 after Bariatric Surgery: A Randomized Controlled Trial. Eur J Phys Rehabil Med 2022, 58, 845–852. [CrossRef]
- Yang, Y.; Li, S.; Cai, Y.; Zhang, Q.; Ge, P.; Shang, S.; Han, H. Effectiveness of Telehealth-Based Exercise Interventions on Pain, Physical Function and Quality of Life in Patients with Knee Osteoarthritis: A Meta-Analysis. J Clin Nurs 2023, 32, 2505–2520. [CrossRef]
- Santiago, M.; Cardoso-Teixeira, P.; Pereira, S.; Firmino-Machado, J.; Moreira, S. A Hybrid-Telerehabilitation Versus a Conventional Program for Urinary Incontinence: A Randomized Trial during COVID-19 Pandemic. Int Urogynecol J 2023, 34, 717–727. [CrossRef]
- Bennell, K.L.; Marshall, C.J.; Dobson, F.; Kasza, J.; Lonsdale, C.; Hinman, R.S. Does a Web-Based Exercise Programming System Improve Home Exercise Adherence for People With Musculoskeletal Conditions?: A Randomized Controlled Trial. Am J Phys Med Rehabil 2019, 98, 850–858. [CrossRef]
- Lambert, T.E.; Harvey, L.A.; Avdalis, C.; Chen, L.W.; Jeyalingam, S.; Pratt, C.A.; Tatum, H.J.; Bowden, J.L.; Lucas, B.R. An App with Remote Support Achieves Better Adherence to Home Exercise Programs than Paper Handouts in People with Musculoskeletal Conditions: A Randomised Trial. J Physiother 2017, 63, 161–167. [CrossRef]
- Lawford, B.J.; Delany, C.; Bennell, K.L.; Hinman, R.S. “I Was Really Sceptical...But It Worked Really Well”: A Qualitative Study of Patient Perceptions of Telephone-Delivered Exercise Therapy by Physiotherapists for People with Knee Osteoarthritis. Osteoarthritis Cartilage 2018, 26, 741–750. [CrossRef]
- Moffet, H.; Tousignant, M.; Nadeau, S.; Mérette, C.; Boissy, P.; Corriveau, H.; Marquis, F.; Cabana, F.; Belzile, É.L.; Ranger, P.; et al. Patient Satisfaction with In-Home Telerehabilitation After Total Knee Arthroplasty: Results from a Randomized Controlled Trial. Telemed J E Health 2017, 23, 80–87. [CrossRef]
- Wahezi, S.E.; Kohan, L.R.; Spektor, B.; Brancolini, S.; Emerick, T.; Fronterhouse, J.M.; Luedi, M.M.; Colon, M.A.; Kitei, P.M.; Anitescu, M.; et al. Telemedicine and Current Clinical Practice Trends in the COVID-19 Pandemic. Best Pract Res Clin Anaesthesiol 2021, 35, 307–319. [CrossRef]
- Van Hove, O.; Gillet, A.; Tack, J.; Reychler, G.; Guatteri, M.; Ballarin, A.; Thomas, J.; Espinoza, R.; Bonnier, F.; Norrenberg, M.; et al. Development of a Medium Care Unit Using an Inexperienced Respiratory Staff: Lessons Learned during the COVID-19 Pandemic. IJERPH 2022, 19, 7349. [CrossRef]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating Barriers to Adopting Telemedicine Worldwide: A Systematic Review. J Telemed Telecare 2018, 24, 4–12. [CrossRef]
- Marra, C.; Gordon, W.J.; Stern, A.D. Use of Connected Digital Products in Clinical Research Following the COVID-19 Pandemic: A Comprehensive Analysis of Clinical Trials. BMJ Open 2021, 11, e047341. [CrossRef]
- Carl, J.R.; Jones, D.J.; Lindhiem, O.J.; Doss, B.D.; Weingardt, K.R.; Timmons, A.C.; Comer, J.S. Regulating Digital Therapeutics for Mental Health: Opportunities, Challenges, and the Essential Role of Psychologists. Br J Clin Psychol 2021. [CrossRef]
- Rangachari, P.; Mushiana, S.S.; Herbert, K. A Narrative Review of Factors Historically Influencing Telehealth Use across Six Medical Specialties in the United States. Int J Environ Res Public Health 2021, 18, 4995. [CrossRef]
- Almathami, H.K.Y.; Win, K.T.; Vlahu-Gjorgievska, E. Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. J Med Internet Res 2020, 22, e16407. [CrossRef]
- Engelsma, T.; Jaspers, M.W.M.; Peute, L.W. Considerate mHealth Design for Older Adults with Alzheimer’s Disease and Related Dementias (ADRD): A Scoping Review on Usability Barriers and Design Suggestions. Int J Med Inform 2021, 152, 104494. [CrossRef]
- James, H.M.; Papoutsi, C.; Wherton, J.; Greenhalgh, T.; Shaw, S.E. Spread, Scale-up, and Sustainability of Video Consulting in Health Care: Systematic Review and Synthesis Guided by the NASSS Framework. J Med Internet Res 2021, 23, e23775. [CrossRef]

| Population | Patients with confirmed COVID-19. |
| Intervention | Patient education (information about COVID-19, causes, risk factors, healthy diet, treatment modalities and exercises), or physical exercises or activities (strengthening exercises, gait training, cycling, walking, gardening, etc.) through mHealth. |
| Comparison | Any other intervention (i.e., physical exercises or activities, patient education without mHealth) or no intervention |
| Outcome | Any type of outcome measure related to the International Classification of Functioning, Disability and Health (ICF) [8] |
| Study Design | Randomized Controlled studies |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





