1. Introduction
Infective endocarditis (IE) is a potentially life-threatening syndrome with an in-hospital mortality rate ~20% despite optimal medical and surgical management [
1,
2,
3]. Echocardiography is an essential tool in the diagnosis of IE, but also in the identification of heart conditions that predispose to its development [
4,
5,
6,
7]. The designation of a predisposing heart condition is nonspecific for left-sided, native valve endocarditis (LS-NVE) and may include a myriad of congenital and acquired conditions such as congenital abnormalities, rheumatic heart disease, hypertrophic cardiomyopathy,
bicuspid aortic valve or mitral valve prolapse [
8,
9,
10,
11,
12,
13]
.
Considering the: (i) nonspecific classification of predisposing cardiac conditions associated with the development of LS-NVE; (ii) fact that 40% of patients with NVE do not have a structural abnormality or valve damage prior to with the development of IE [
14]; and (iii) evolution of technical advances in echocardiography over recent years, it seems appropriate to evaluate echocardiography as a potential tool in assessing the likelihood of the subsequent development of LS-NVE. Thus, the primary objective of the current investigation was to determine whether transthoracic echocardiogram (TTE) measurements were associated with the subsequent development of LS-NVE in patients with no predisposing cardiac conditions.
2. Methods
A case-control study design was conducted. Cases and controls were adult (≥18 years) patients from Mayo Clinic sites (Rochester, Florida, Arizona, and the Health Systems) from 2008 to 2020. To determine the cases, institutional databases of patients with an initial diagnosis of LS-NVE were queried. Medical charts were reviewed, and IE cases were identified according to the modified Duke criteria [
10], and categorized into either possible or definite LS-NVE. Only patients who had a TTE performed 6 months to 3 years before the development of IE were considered for study inclusion, and every individual was only included once. Controls were selected from a large retrospective cohort of adult patients with at least one TTE report over a similar period to that of the cases.. Patients with prosthetic valves, cardiovascular implantable electronic devices (CIEDs), intracardiac devices, previous IE, injection drug use, and predisposing heart conditions (congenital abnormalities, rheumatic heart disease, hypertrophic cardiomyopathy, bicuspid aortic valve and mitral valve prolapse) were excluded among cases and controls.
Case and controls were matched using age, sex, Charlson Comorbidity Index (CCI) and date of echocardiogram. Our matching algorithm attempted to sample all LS-NVE cases and 3 times as many controls as cases, matching them exactly on sex and CCI category, and closely on age (±3 years) and timing of echocardiography (±1 year).
Details characterizing the degree of valve abnormality and other echocardiographic measurements, were then collected for both matched cases and controls. Clinical characteristics, medical history, procedures, and comorbid conditions (at the time of the patients’ echocardiography) were also collected from the electronic health record. The CCI was calculated as described previously [
15]. This study was approved by the Mayo Clinic Institutional Review Board and included only patients with institutional research authorization.
2.1. Echocardiographic measurements
A registered cardiac sonographer conducted the echocardiographic examination following the American Society of Echocardiography guidelines [
16,
17,
18]. Data were extracted from the echocardiography reports for all patients. Mid-segmental linear measurements of the left ventricular (LV) internal systolic (LVISD) and diastolic dimensions (LVIDD), left ventricular posterior wall diastolic thickness (LVPWDT), and interventricular septum diastolic thickness (IVSDT) were performed in a parasternal long-axis view. LV ejection fraction (EF) was calculated using the modified Quinones equation or biplane method of disks (Simpson). For the hemodynamic measurements the velocity-time integral (VTI) and peak velocity of the left ventricular outflow tract (LVOT) were measured using pulsed wave Doppler in an apical long-axis or five-chamber view. LVOT diameter was measured using a parasternal long-axis view during systole. The LVOT cross-sectional area and VTI were multiplied to obtain the stroke volume [
19]. Cardiac output was derived from (stroke volume × heart rate) and then indexed according to the patient’s body surface area. Transmitral flow was acquired using pulsed-wave Doppler for E-wave and tissue doppler for e’-wave. Both measurements were obtained from the septal side of the mitral annulus during the same heartbeat using a four-chamber view. The E wave to e’ ratio was used to determine LV filling pressures. Native valvular regurgitation for the aortic and mitral valves was classified according to the American Society of Echocardiography guidelines into normal, trivial, mild, moderate, and severe [
20].
2.2. Analytic plan and statistical analysis
To test for unadjusted associations between the case-control group and each of the clinical and echocardiographic variables, we used unmatched methods (e.g., Wilcoxon rank-sum tests, Pearson χ² tests) to avoid deletion of matched sets with partially missing data. However, the comparisons were also repeated on the matched sets using matched methods (univariable conditional logistic regression models) and checked for agreement. Results of these bivariate analyses were not used in selecting variables to include in the prognostic model of LS-NVE.
For echocardiographic data, measurements on 46 variables were collected. Of them, 20 were missing in >15% of patients and were therefore removed from further evaluation. Due to the paucity of severity categories, the ordinal variables for mitral and aortic stenosis were removed. In contrast, those for mitral and aortic regurgitation were retained but were dichotomized as presence (mild, moderate, or severe) or absence (none or trivial) to preserve degrees of freedom (df). Next, the remaining 24 echocardiographic variables were reduced to the 12 most clinically relevant ones. Lastly, we examined data redundancy among the remaining variables and removed two more variables: LV mass index (due to overlapping information with the other variables) and LVEDD (due to collinearity with LVESD). Hence, the final model was fitted with 10 echocardiographic variables (13 df), including 5 anatomical-related measures – IVSDT, LVESD, LVWDT, and mitral and aortic regurgitation – and 5 hemodynamic-related measures – LVEF, LVOT velocity, LV cardiac index, E: e’ ratio, and AVSP velocity). Because significantly higher rates of chronic kidney disease and diabetes mellitus were found in the LS-NVE cases versus controls (despite matching on CCI), a post hoc analysis was conducted by repeating the original logistic regression with inclusion of these 2 additional covariates.
Continuous variables were modelled with 3-knot restricted cubic splines to assess the default assumption of nonlinearity. For those variables with little to no evidence of a nonlinear effect, the nonlinear terms were removed, and the variables were refitted as linear in the final model. To preserve the total sample size in the modelling despite missing data (the rate of missingness among echocardiographic variables ranged from 0% to 13.6%), multiple imputations were employed with 25 imputation sets based on predictive mean matching. Model estimates were depicted with partial effects plots to show how the predicted probabilities of IE changed over the range of observed values for each continuous variable. The relative contribution of variables to the model tested individually or as a group, was quantified with adjusted χ² statistics, whereby subtracting the degrees of freedom from the Wald partial χ² values, the contributions of variables can be compared on the same scale. The model was internally validated for discrimination and calibration using bootstrap resampling. Predictive discrimination was quantified by the C-statistic and other model indexes. At the same time, calibration was demonstrated with a smooth nonparametric calibration curve comparing predicted and observed probabilities of IE for both the original and bootstrapped models.
If not otherwise indicated, patient characteristics presented with median and interquartile ranges (IQR) for continuous variables and numbers and percentages for categorical or ordinal variables. A p value of <0.05 was considered statistically significant. Analyses were performed using the statistical programming language R, version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
3. Results
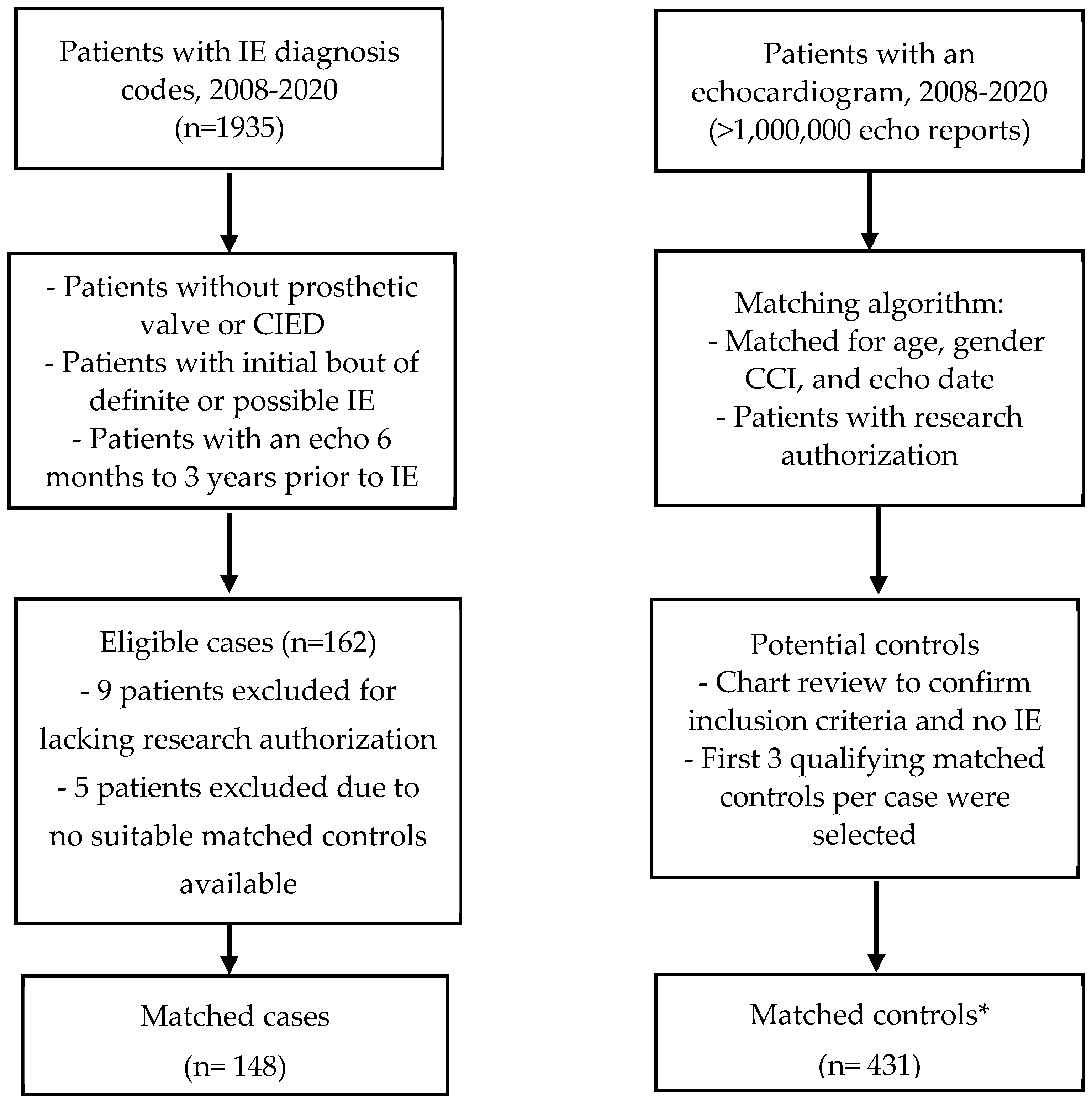
Overall, a total of 579 patients were included in the analysis: 148 LS-NVE cases (124 definite [83.8%] and 24 possible) and 431 matched controls (
Figure 1). The median age was 63.8 (IQR: 53.6 – 74.6) years, and 329 (56.8%) patients were males. The patients’ race was predominantly white in both cases (91.8%) and controls (92.2%). LS-NVE cases had a higher prevalence of diabetes mellitus (46.6% vs. 30.4%) and chronic kidney disease (46.6% vs. 28.1%) when compared with controls (p<0.001 for both comparisons). The median CCI score was 3 (IQR: 0-6) for cases and 2 (IQR: 0–6) for controls.
Figure 1.
Selection flow chart demonstrating cases and controls. Abbreviations: IE, infective endocarditis; Echo, transthoracic echocardiography; CIED, cardiac implanted electronic device; CCI, Charlson comorbidity index. * Of the 148 matched sets, 137 (92.6%) included three matched controls per case, 9 (6.1%) had two controls, and 2 (1.4%) had only one suitable control.
Figure 1.
Selection flow chart demonstrating cases and controls. Abbreviations: IE, infective endocarditis; Echo, transthoracic echocardiography; CIED, cardiac implanted electronic device; CCI, Charlson comorbidity index. * Of the 148 matched sets, 137 (92.6%) included three matched controls per case, 9 (6.1%) had two controls, and 2 (1.4%) had only one suitable control.
Table 1.
Demographics and Comorbid Conditions by IE Case Status.
Table 1.
Demographics and Comorbid Conditions by IE Case Status.
| Characteristic |
N |
Cases (N=148) |
Controls (N=431) |
p value |
| Year of echo |
579 |
2015.9 (2011.7-2018.3) |
2015.9 (2011.6-2018.4) |
0.8371 |
| Male Gender |
579 |
84 (56.8%) |
245 (56.8%) |
0.9852 |
| Age at Time of Echo |
579 |
63.7 (53.7-74.5) |
63.8 (53.6-74.6) |
0.9051 |
| Race: White |
572 |
135 (91.8%) |
392 (92.2%) |
0.8772 |
| Chronic Kidney Disease |
579 |
69 (46.6%) |
121 (28.1%) |
< 0.0012 |
| Hemodialysis |
579 |
14 (9.5%) |
1 (0.2%) |
< 0.0012 |
| Hypertrophic Cardiomyopathy |
579 |
2 (1.4%) |
3 (0.7%) |
0.4572 |
| Myocardial Infarction |
579 |
27 (18.2%) |
88 (20.4%) |
0.5672 |
| Hypertension |
579 |
88 (59.5%) |
238 (55.2%) |
0.3702 |
| Heart Failure |
579 |
51 (34.5%) |
139 (32.3%) |
0.6212 |
| Cerebral Stroke |
579 |
3 (2.0%) |
13 (3.0%) |
0.5262 |
| Diabetes Mellitus |
579 |
69 (46.6%) |
131 (30.4%) |
< 0.0012 |
| Charlson Index |
579 |
3 (0-6) |
2 (0-6) |
0.4211 |
| Charlson Index Levels |
579 |
|
|
0.8191 |
| 0 |
|
43 (29.1%) |
129 (29.9%) |
|
| 1 |
|
7 (4.7%) |
21 (4.9%) |
|
| 2 |
|
19 (12.8%) |
56 (13.0%) |
|
| 3 |
|
17 (11.5%) |
47 (10.9%) |
|
| 4-6 |
|
26 (17.6%) |
75 (17.4%) |
|
| 7-10 |
|
23 (15.5%) |
68 (15.8%) |
|
| >10 |
|
13 (8.8%) |
35 (8.1%) |
|
Echocardiographic variables that were routinely (i.e., in >80% of patients) measured in cases and controls are presented in
Table 2. In these unadjusted analyses, anatomical echocardiographic measurements were different in patients with LS-NVE than those without IE, as evidenced by higher IVSDT, LVWDT and LV mass index (p≤0.01 for all comparisons). LS-NVE cases also exhibited different hemodynamics compared with controls based on higher LVOT velocity, LV cardiac index, mitral E and A wave, E: e’ ratio, and AVSP velocity (p≤0.002 for all comparisons).
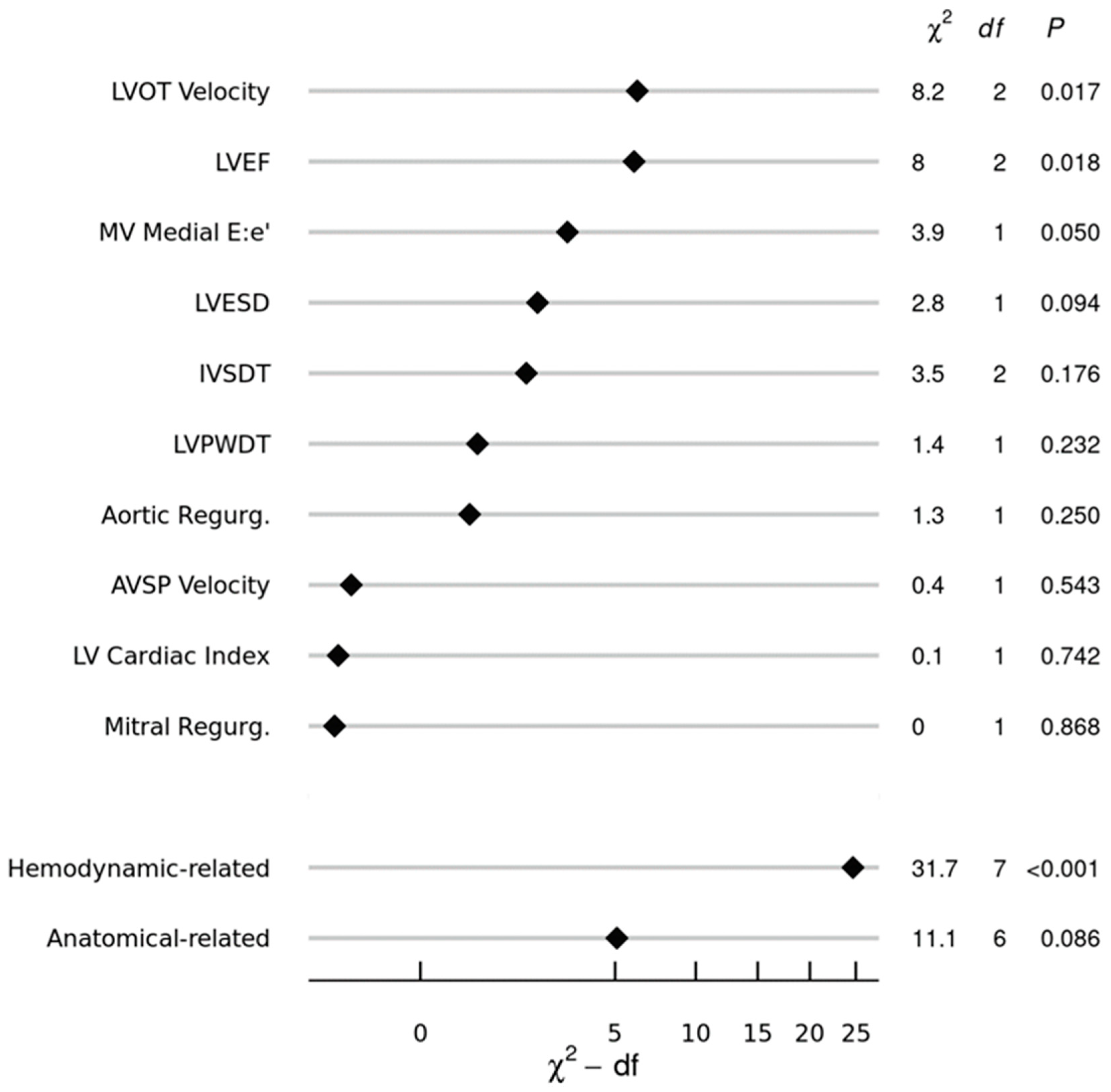
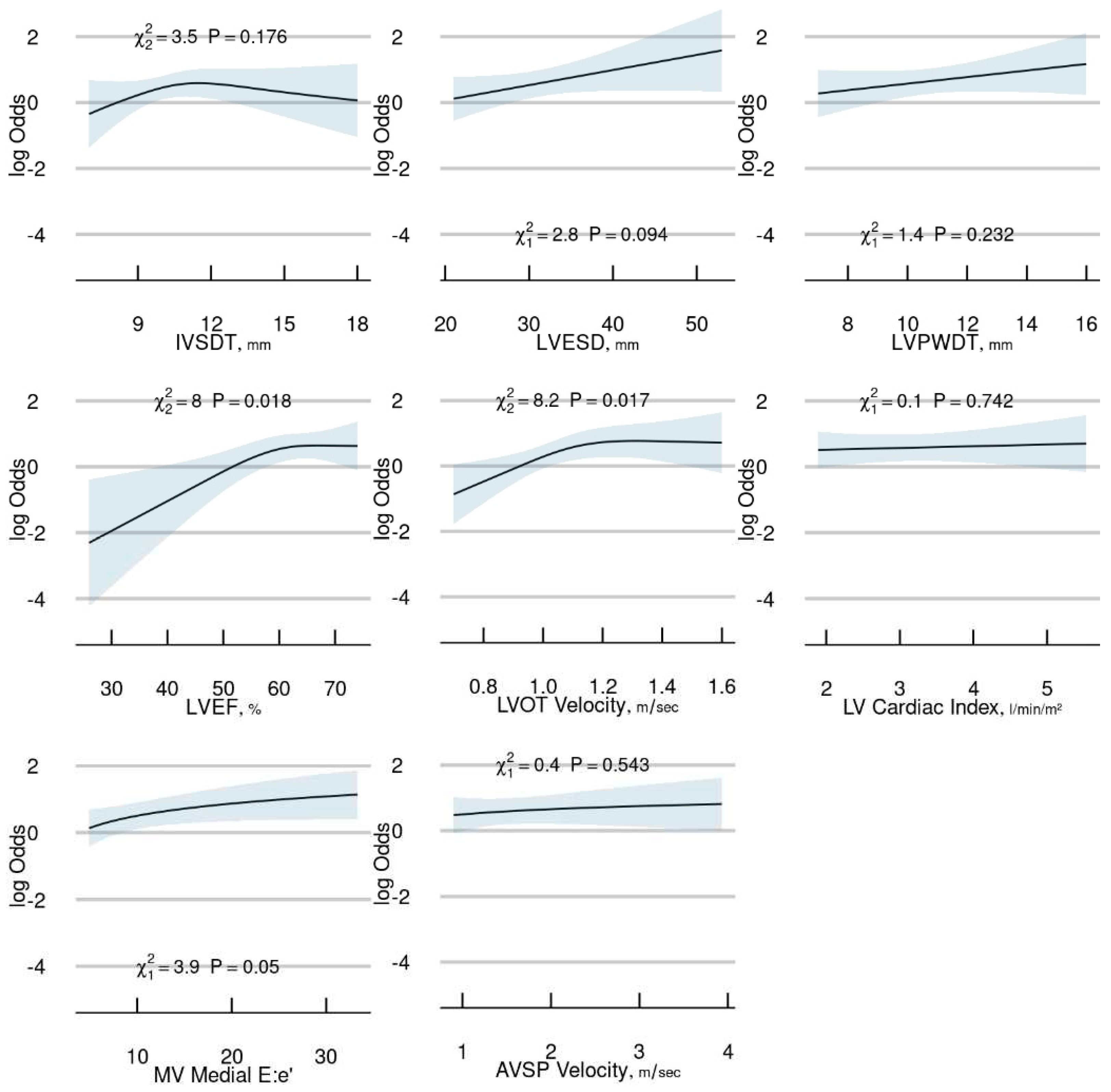
A multivariable conditional logistic regression model was developed to determine the association of anatomical and hemodynamic measurements with the risk of LS-NVE. The selection of variables to be included in the model was based on a priori knowledge and data reduction methods blinded to the case-control group, resulting in 10 variables selected for inclusion (
Table 3). Ranked by importance according to their adjusted χ² values from the model (
Figure 2), LVOT velocity (p=0.017), and LVEF (p=0.018) and E: e’ (p=0.050) were significantly associated with LS-NVE. When re-expressed in terms of grouped variables, the hemodynamic-related variables had a stronger contribution to the model (corrected χ²=31.7; p<0.001) than the anatomical landmark-related variables (corrected χ²=11.1; p=0.086). A partial effects plot for the continuous variables in the final model is presented in
Figure 3.
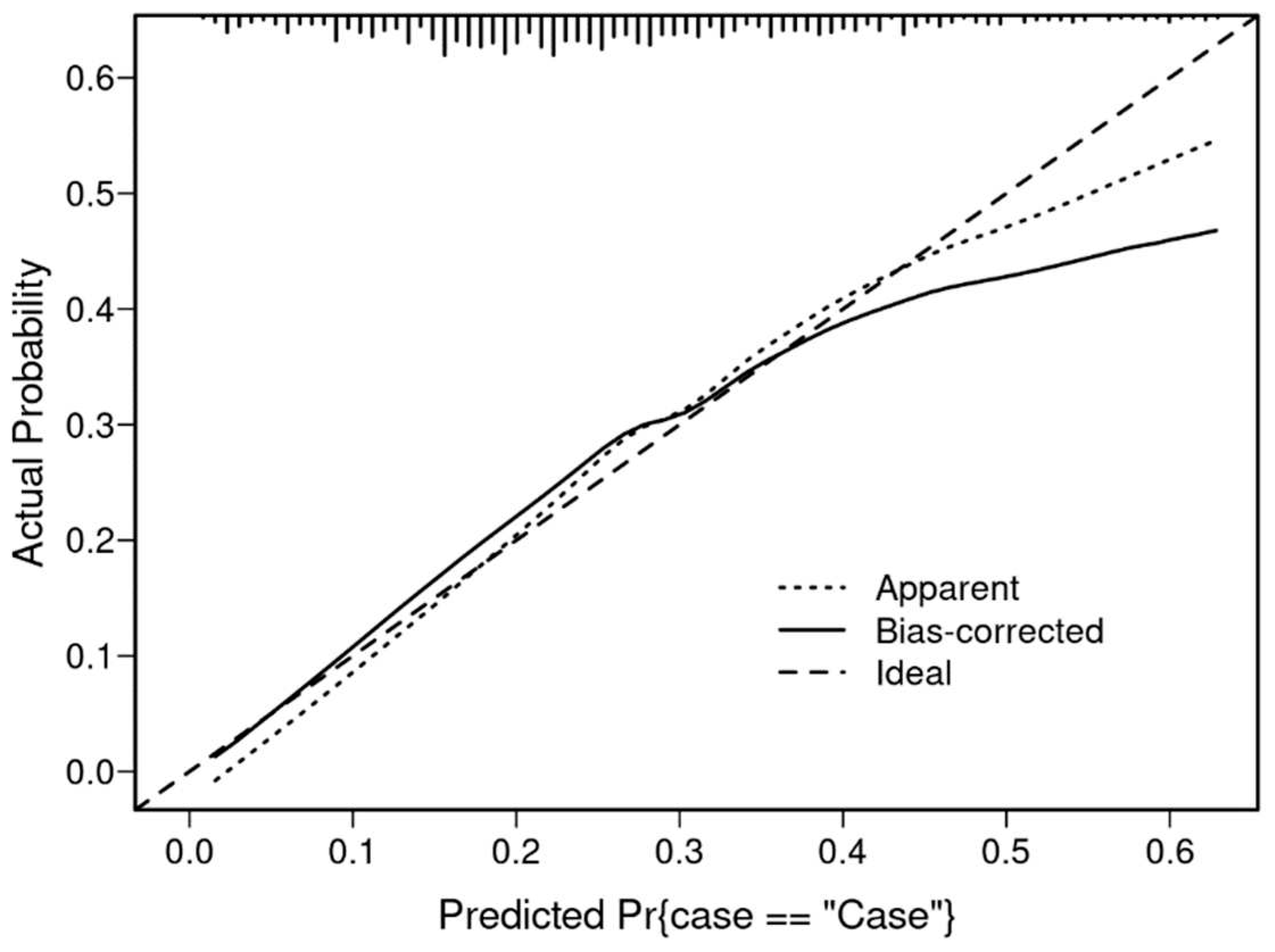
The bias-corrected C statistic of the model was 0.67, indicating modest discrimination in predicting LS-NVE for an individual patient. Using the bootstrap method to internally validate and calibrate the model, the estimated slope shrinkage factor of 0.79 suggested minor overfitting. The bias-corrected calibration curve presented in
Figure 4 demonstrates that the model is generally well calibrated across the risk range, except for higher risk profiles where the model tends to underestimate the probability of IE. Model-based predictions of LS-NVE (in the matched sample), as estimated by the mathematical formula in
Supplemental Figure S1, are illustrated for ten hypothetical patients in
Supplemental Table S1.
A secondary analysis in which terms for diabetes mellitus and chronic kidney disease were added to the original model yielded similar findings concerning echocardiographic variables, except for E: e’ which was no longer significant (
Supplemental Figures S2 and S3).
4. Discussion
This is the first study to evaluate multiple specific TTE measurements and determine whether they were associated the subsequent development of LS-NVE in patients with no known cardiac predisposing conditions. Our primary finding was that increased peak LVOT velocity and LVEF were hemodynamic echocardiographic measurements associated with the subsequent development of LS-NVE. It is conceivable that increased LV pressures and velocities could be operative in IE predisposition by causing substantial turbulence that could create a substrate for endocardial injury as highlighted in an experimental model highlighting a “damage-induced” pathway [
12]. Nevertheless, it is important to mention that there is limited clinical application for these results, future larger scale studies should be performed to assess the relevance of our findings.
It has been estimated that more than 800,000 individuals are at a high risk of IE in the United States alone [
25]. Nevertheless, there is not a clear NVE diagnostic scheme for patients with ‘formally’ structural normal heart valve conditions. Thus, by implementing our analysis, which included an in-depth characterization of cardiac disease with the use of quantitative echocardiographic measurements, but also recognizing clinical parameters, may provide the most useful foundation for a future strategy in identifying patients who may have an increased risk of IE.
We did not detect an association between the degree of mitral and aortic regurgitation and subsequent development of IE in our multivariable model. Previous work has shown that valvular dysfunction is associated with IE, however, in contrast to our study, they included patients with predisposing cardiac conditions. Namely, the degree of mitral regurgitation, could be a risk factor associated with the development of IE in patients with mitral valve prolapse [
28]. Of note, the inclusion of stenotic lesions of the mitral and aortic valves in our multivariable model was not possible due to their limited prevalence in our study cohort.
Diabetes mellitus and chronic kidney disease were identified as predisposing comorbidities for the development of LS-NVE in the current investigation. Diabetes mellitus is well recognized as an independent risk factor associated with IE; these patients can have an impaired immune response, delayed healing, reduced tissue vascularization and endothelial dysfunction [
21]. Chronic kidney disease patients, particularly those with end-stage renal disease receiving hemodialysis, are at a significantly higher risk of developing IE when compared to the general population due to a higher prevalence of bacteremia related to vascular access and because of uremia-related impaired immune response [
22,
23]. In addition, both diabetes mellitus and chronic kidney disease have a higher rate of
S. aureus colonization than the general population, and hence, an increased risk of
S. aureus bacteremia, which consequently increases the risk of IE [
24].
5. Limitations
Our study is based on a retrospective case-control design and is subject to inherent limitations. First, given our relatively modest sample size, the large number of echocardiographic variables available posed statistical challenges with model development, therefore, we used data reduction based on clinical sensibility, lack of redundancy, and data completeness. Second, the retrospective nature of this study precluded the acquisition of complete echocardiographic measurements in all patients; however, a strength of our modeling approach is that only parameters that were routinely available (i.e., measured in ≥ 80% of the subjects) were included. Third, this study was conducted at a tertiary medical center which may have introduced selection and referral bias. Fourth, our population was composed of adult patients who were predominantly white and of northern European descent; thus, the generalizability of our results to other populations is uncertain. Finally, despite the association of peak LVOT velocity and LVEF measurements with the development of IE, the differences between the compared study groups were small and are not applicable in clinical practice given that they can be confounded by the inherent interobserver variability of TTE. However, it is crucial to recognize the potential value and opportunity this presents for conducting a larger-scale investigation to assess the importance of these findings. A larger sample size would enhance statistical power, allowing for more precise estimation of effect sizes and detection of smaller, yet clinically relevant, effects.
6. Conclusions
Specific hemodynamic echocardiographic measurements were independently associated with LS-NVE in patients with no known predisposing cardiac conditions in our preliminary investigation. These measurements underpin the importance of alterations in hemodynamic function in predisposing to NVE. While our results demonstrated an association of echocardiographic measures with the subsequent development of IE, further investigation is needed to validate these preliminary findings.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table S1: Model-Predicted Risk of LS-NVE for 10 Hypothetical Patients, Figure S1: Logistic Regression Equation for Risk of LS-NVE, Figure S2. Secondary model Relative Importance of Individual and Grouped Predictor Variables, Figure S3. Conditional versus Unconditional Logistic Regression.
Author Contributions
Conceptualization, J.A.Q.M and L.M.B.; methodology, J.A.Q.M, B.D.L and L.M.B; software, B.D.L.; validation, B.D.L; formal analysis, B.D.L; investigation, J.A.Q.M and L.M.B; data curation, J.A.Q.M and J.R.H; writing original draft preparation, J.A.Q.M, J.R.H, B.D.L and L.M.B; writing review and editing, J.A.Q.M, J.R.H, B.D.L, H.R.V, M.J.D, M.H.T, J.C.O, H.I.M, N.S.A, P.S, D.C.D, and L.M.B; supervision, H.R.V, M.J.D, M.H.T, J.C.O, H.I.M, N.S.A, P.S, D.C.D, and L.M.B; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data underlying this article cannot be shared publicly because the privacy of the individuals that participated in the study must be maintained and because the data underlying this article were provided by the Mayo Clinic under license and by permission. The data will be shared on reasonable request to the corresponding author with the permission of Mayo Clinic.
Acknowledgments
The authors are extremely grateful for the philanthropic support provided by a gift from Eva and Gene Lane (L.M.B.), which was paramount in our work to advance the science of cardiovascular infections and has been an ongoing focus of investigation at Mayo Clinic for over 60 years.
Conflicts of Interest
Larry M. Baddour, M.D. reports over the past 12 months UpToDate, royalty payments (authorship duties). None of the other authors had disclosures.
References
- Murdoch, D.R., et al., Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med, 2009. 169(5): p. 463-73. [CrossRef]
- Chu, V.H., et al., Early predictors of in-hospital death in infective endocarditis. Circulation, 2004. 109(14): p. 1745-9. [CrossRef]
- Wallace, S.M., et al., Mortality from infective endocarditis: clinical predictors of outcome. Heart, 2002. 88(1): p. 53-60. [CrossRef]
- Habib, G., et al., 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J, 2015. 36(44): p. 3075-3128. [CrossRef]
- Joseph, J.P., et al., Prioritizing echocardiography in Staphylococcus aureus bacteraemia. J Antimicrob Chemother, 2013. 68(2): p. 444-9. [CrossRef]
- Sachdev, M., G.E. Peterson, and J.G. Jollis, Imaging techniques for diagnosis of infective endocarditis. Infect Dis Clin North Am, 2002. 16(2): p. 319-37, ix. [CrossRef]
- Van Hal, S.J., et al., The role of transthoracic echocardiography in excluding left sided infective endocarditis in Staphylococcus aureus bacteraemia. J Infect, 2005. 51(3): p. 218-21. [CrossRef]
- Büchi, A.E., et al., Infective Endocarditis: How Do We Currently Interpret the Duke Minor Criterion "Predisposing Heart Condition" in Native Valves? Cardiology and therapy, 2017. 6(1): p. 121-128. [CrossRef]
- Büchi, A., et al., The Duke minor criterion "predisposing heart condition" in native valve infective endocarditis - a systematic review. Swiss Med Wkly, 2018. 148: p. w14675. [CrossRef]
- Li, J.S., et al., Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis, 2000. 30(4): p. 633-8. [CrossRef]
- Zegri-Reiriz, I., et al., Infective Endocarditis in Patients With Bicuspid Aortic Valve or Mitral Valve Prolapse. J Am Coll Cardiol, 2018. 71(24): p. 2731-2740. [CrossRef]
- Liesenborghs, L., et al., Staphylococcus aureus endocarditis: distinct mechanisms of bacterial adhesion to damaged and inflamed heart valves. Eur Heart J, 2019. 40(39): p. 3248-3259. [CrossRef]
- Spirito, P., et al., Infective endocarditis in hypertrophic cardiomyopathy: prevalence, incidence, and indications for antibiotic prophylaxis. Circulation, 1999. 99(16): p. 2132-7. [CrossRef]
- Olmos, C., et al., Comparison of clinical features of left-sided infective endocarditis involving previously normal versus previously abnormal valves. Am J Cardiol, 2014. 114(2): p. 278-83. [CrossRef]
- Charlson, M.E., et al., A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis, 1987. 40(5): p. 373-83. [CrossRef]
- Lang, R.M., et al., Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr, 2015. 28(1): p. 1-39.e14. [CrossRef]
- Rudski, L.G., et al., Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr, 2010. 23(7): p. 685-713; quiz 786-8. [CrossRef]
- Mitchell, C., et al., Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr, 2019. 32(1): p. 1-64. [CrossRef]
- Germain, M.J., et al., Comparison of stroke volume measurements during hemodialysis using bioimpedance cardiography and echocardiography. Hemodial Int, 2018. 22(2): p. 201-208. [CrossRef]
- Zoghbi, W.A., et al., Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr, 2017. 30(4): p. 303-371. [CrossRef]
- Østergaard, L., et al., Duration and complications of diabetes mellitus and the associated risk of infective endocarditis. International Journal of Cardiology, 2019. 278: p. 280-284. [CrossRef]
- Powe, N.R., et al., Septicemia in dialysis patients: incidence, risk factors, and prognosis. Kidney Int, 1999. 55(3): p. 1081-90. [CrossRef]
- Leither, M.D., et al., Long-term Survival of Dialysis Patients With Bacterial Endocarditis Undergoing Valvular Replacement Surgery in the United States. Circulation, 2013. 128(4): p. 344-351. [CrossRef]
- Kluytmans, J., A. van Belkum, and H. Verbrugh, Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev, 1997. 10(3): p. 505-20. [CrossRef]
- Lockhart, P.B., et al., Drug cost implications for antibiotic prophylaxis for dental procedures. Oral Surg Oral Med Oral Pathol Oral Radiol, 2013. 115(3): p. 345-53. [CrossRef]
- Baddour, L.M., et al., Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications. Circulation, 2015. 132(15): p. 1435-1486. [CrossRef]
- Thornhill, M.H., et al., Quantifying infective endocarditis risk in patients with predisposing cardiac conditions. Eur Heart J, 2018. 39(7): p. 586-595. [CrossRef]
- Katan, O., et al., Incidence and Predictors of Infective Endocarditis in Mitral Valve Prolapse: A Population-Based Study. Mayo Clin Proc, 2016. 91(3): p. 336-42. [CrossRef]
- Ngiam, J.N., et al., Clinical and echocardiographic characteristics associated with the development of infective endocarditis in patients with significant mitral stenosis. Echocardiography, 2022. 39(1): p. 82-88. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).