1. Introduction
With the increasing aging population, minimally invasive spine surgery has gained the greater attention. The classical anterior lumbosacral fusion surgery has been performed by relatively large incision with a wide surgical view due to the necessity of manipulating vascular and visceral structures [
1,
2]. However, the recent minimally invasive technology has allowed a tubular surgery with smaller incision through either prepsoas or transpsoas approach [
3,
4]. Woods and Hynes, et al successfully minimized the conventional ALIF using mini-retroperitoneal approach under lateral decubitus position, which was named as oblique lateral interbody fusion (OLIF) (Medtronics, Memphis TN, USA) [
3]. The advantage of anterior or anterolateral fusion includes superior anterior release, large bone graft area, better stability resistant to osteoporosis, and high fusion capacity [
3,
4,
5]. However, the application of this approach for L5/S1 level has been challenging due to the variation of major vascular tissues [
4,
5]. Woods and Hynes et al. successfully minimize this with standardized incision and approach protocols and the specially designed triple-arm retractor (OLIF51; Medtronics, Memphis TN, USA), in which the vascular tissues were safely retracted and secured [
3].
In turn, the use of OLIF51 approach is sometimes disturbed due to small vascular window. In those cases, the lateral corridor approach (LCA) can be performed, in which the approaching corridor is located between psoas muscle and ipsilateral common iliac vessels. The iliolumbar vein sometimes becomes the obstacle, which requires to be ligated.
In both OLIF51 and LCA approach, the understanding of precise vascular structure at L5/S1 level is indispensable. Specifically, the movement of vascular tissue surrounding the L5/S1 disc between supine and lateral decubitus position has to be taken into consideration, however, it has not been precisely measured to date. The objectives of this study were twofold. First, the precise vascular anatomy at L5/S1 level was studied when considering both OLIF51 and LCA surgical approaches, and secondly, the movement of vascular tissue between supine and lateral decubitus position was quantitatively measured using the intraoperative enhanced CT and MRI.
2. Materials and Methods
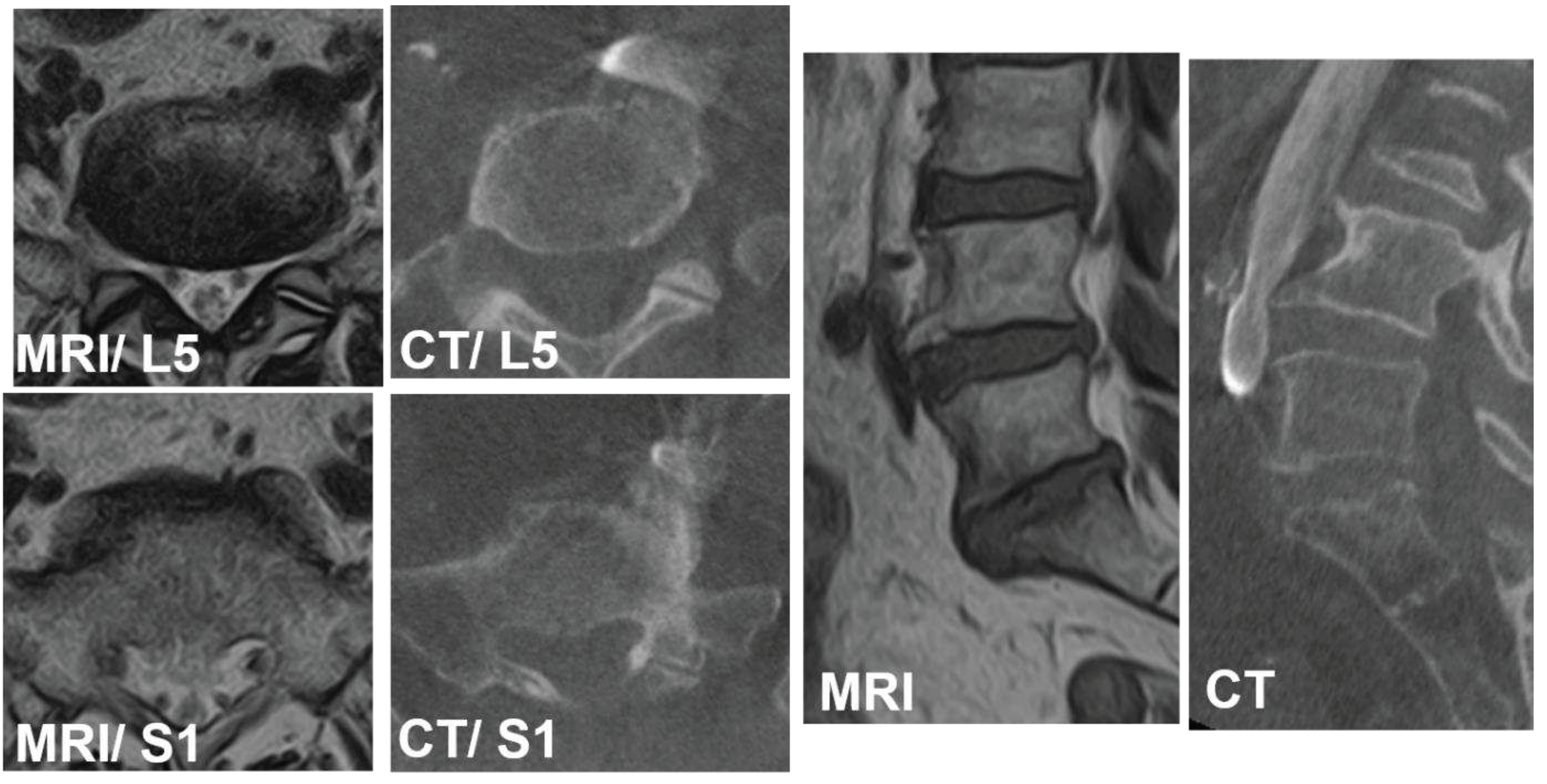
Over 220 patients underwent OLIF51 or LCA surgery from 2016 to 2023, forty-three patients were included in this study. There were 16 males and 27 females with the average age at surgery of 60.4 (37-80) years old. The average body height, weight, and body-mass index were 160 cm (146-187), 60.4 kg (41-86.9), and 23.5 (16.7-33.3). The disorders of patients included L5 isthmic spondylolisthesis, foraminal stenosis at L5/S1, degenerative disc disease, pseudarthrosis of transforaminal interbody fusion at L5/S1 and others. The infectious disease or any pathologies receiving previous retroperitoneal surgeries around lumbosacral area were excluded. All cases received preoperative lumbosacral MRI scans (Phillips Ingenia 3.0T, Canon Excelart Tiatan 1.5T) in a supine position. Before starting the OLIF51 surgery, intraoperative vein-enhanced CT (O-arm O2, Medtronics, MN) were taken in right decubitus position (
Figure 1). All surgeries were performed by single senior surgeon at the single institution.
Description of OLIF51 and LCA surgical procedures
In the OLIF51 surgery, 35mm oblique incision was made two-finger medial from anterior superior iliac spine. Following the dissection of abdominal muscles, the retroperitoneal space was enlarged and bilateral common iliac vessels were retracted. The placement of triple-arm retractor safely secured the anterior aspect of L5/S1 disc followed by discectomy and cartilaginous endplate removal. The 10-degree lordotic PEEK cage (MectaLIF, Medacta international, San Pietro, Switzerland) or 12 or 18-degree lordotic PEEK cage (Sovereign, Medtronics, Memphis TN) with demineralized bone matrix (DBM) soaked with aspirated bone marrow were placed in the disc space. The Sovereign cage allowed the use of integrated screws for enhancing the fixation. In the posterior part of surgery, the long cortical bone trajectory screws were inserted percutaneously in lateral decubitus position for short-segment fusion. In LCA surgery, 35mm oblique incision was made one-finger medial from anterior superior iliac spine. Following the dissection of abdominal muscles, the retroperitoneal space was enlarged and the interspace between psoas muscle common iliac vessels was approached to expose the L5/S1 disc. When the iliolumbar vein was detected, it was carefully ligated or retracted. The self-retained retractor was useful to secure the surgical view and disc preparation. All surgeries were conducted with use of surgical navigation and O-arm (Stealthstation 7, Medtronics, Memphis TN).
Evaluation of vascular anatomy in supine position on MRI
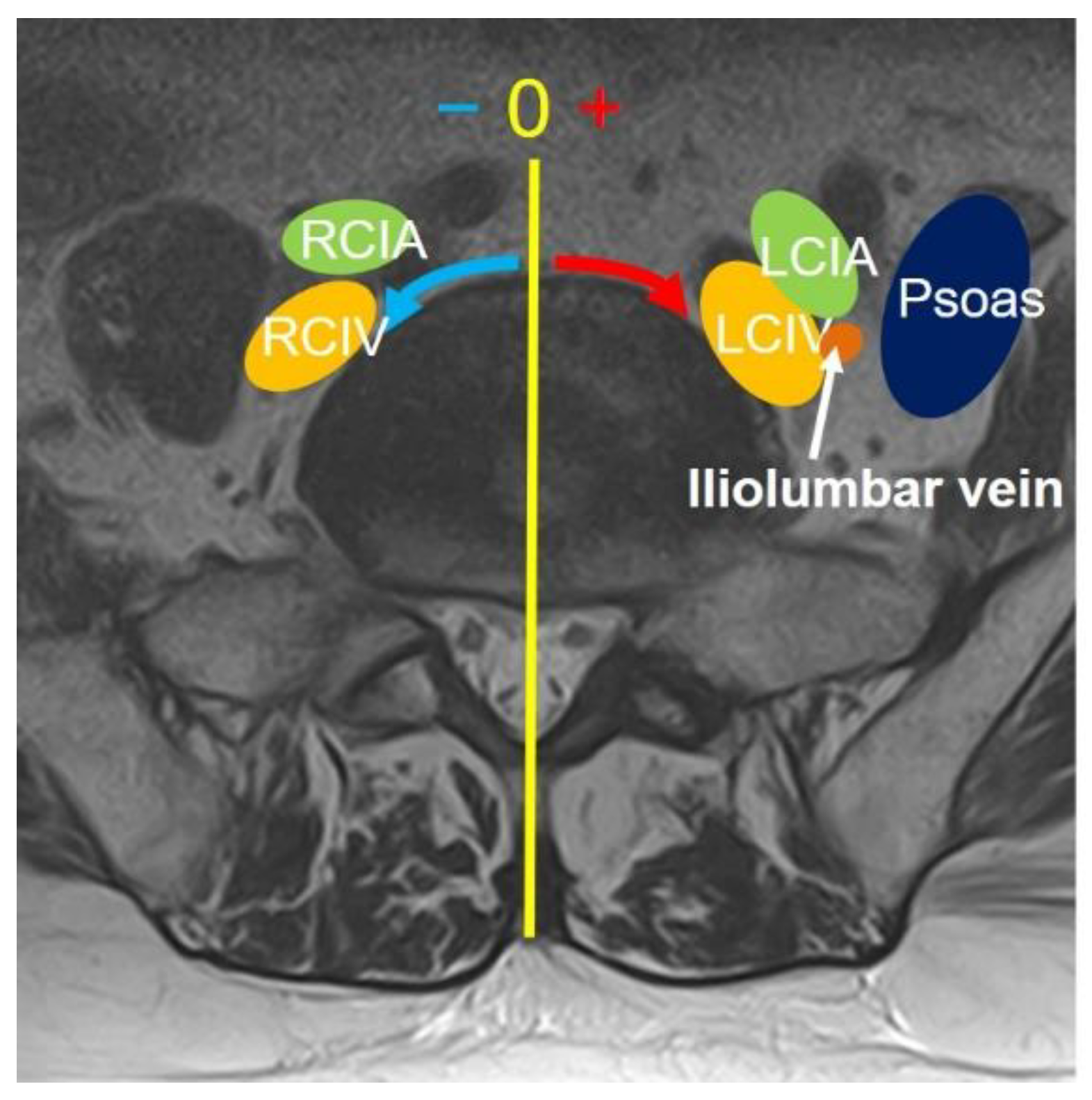
On MRI axial scan at either lower L5 endplate and S1 endplate level, the distance from sagittal mid-vertebral line to border of right and left common iliac vessels were measured as (L5-LCIV, L5-RCIV, L5-LCIA, L5-RCIA, S1-LCIV, S1-RCIV, S1-LCIA, S1-RCIA) (
Figure 2). The vascular window was measured between right and left iliac vessels, expressed as central corridor window (CCW). The lateral corridor window was expressed as the distance between the lateral border of left common iliac vein and medial border of psoas muscle (LCW) (
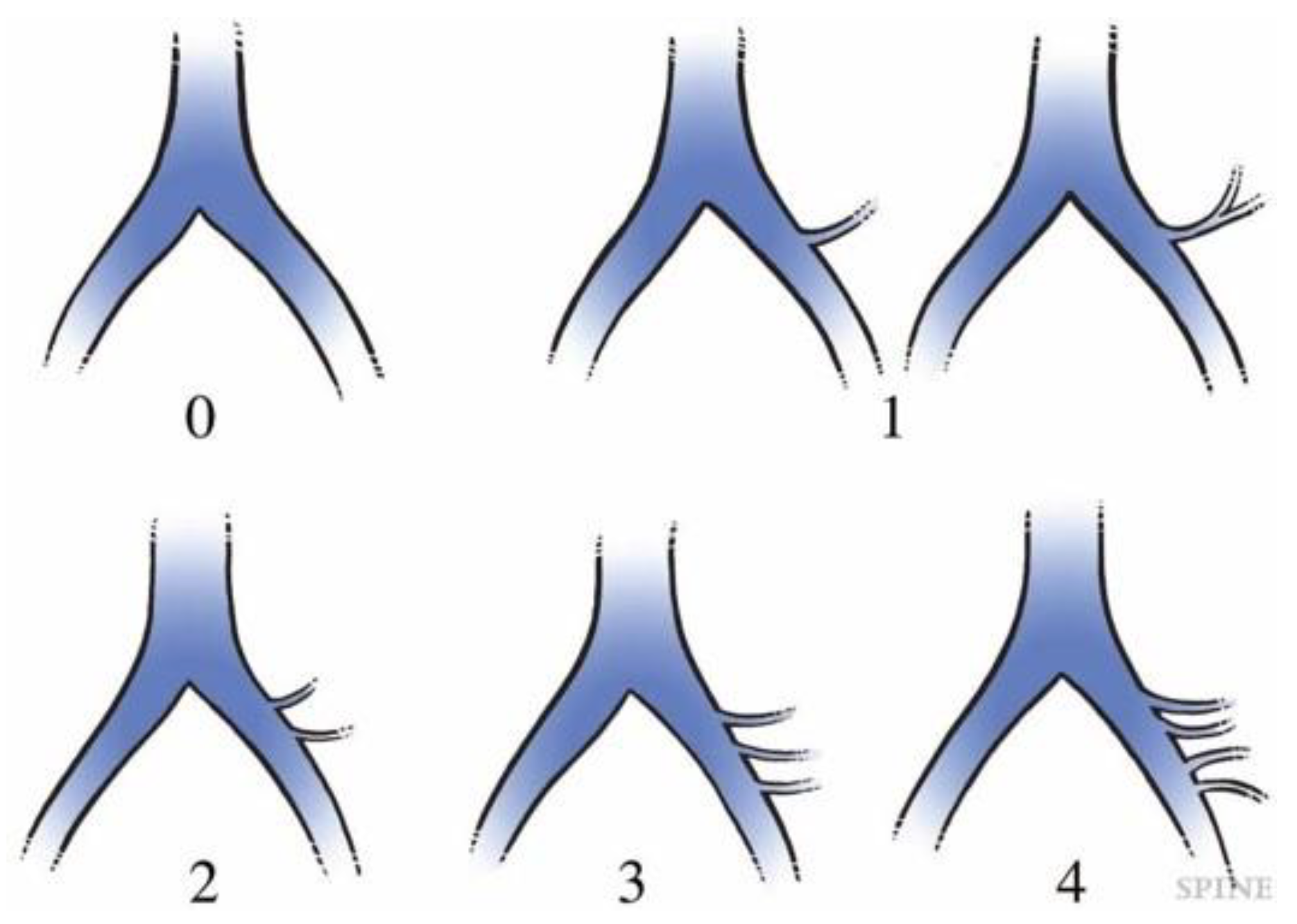
Figure 2). The iliolumbar vein anatomy was also evaluated in terms of visualization rate (%), axial position from sagittal mid-vertebral line (L5-ILV, S1-ILV). The type of iliolumbar vein was classified according to Nalbandian et al. (Nalbandian) (
Figure 3). Type 0 refers to no ILV, Type 1 is the single variant. Multiple ILVs are categorized into type 2, 3, and 4 according to the number of veins found. The vertical position of common iliac vein bifurcation was measured from the lower endplate of L5 (
Figure 4).
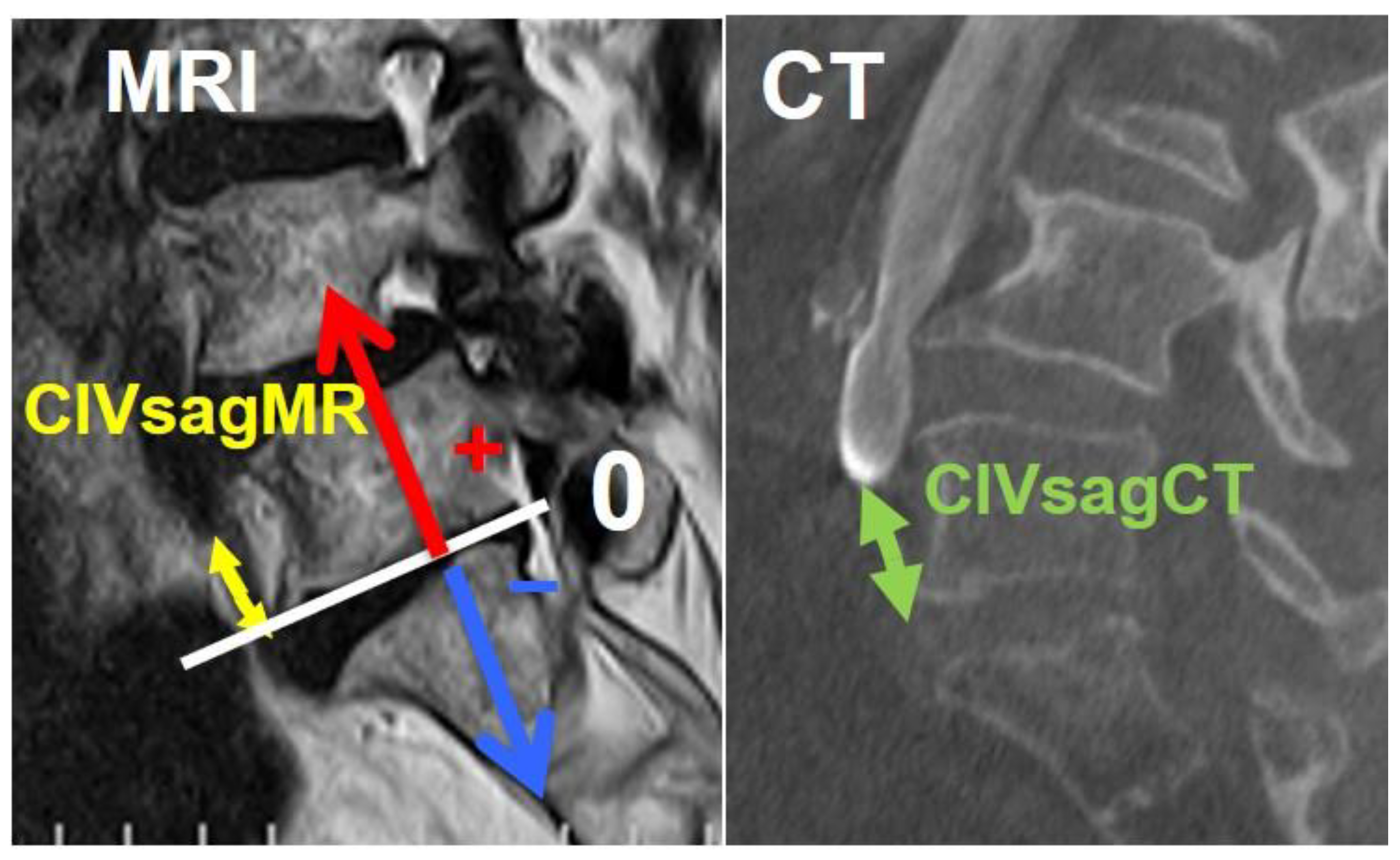
Intraoperative evaluation of vein anatomy in right decubitus position on enhanced CT
The intraoperative vein anatomy in right decubitus position was evaluated with vein-enhanced intraoperative CT (O-armO2, Medtronics) (
Figure 1C). Prior to the incision made for OLIF51 surgery, the contrast medium was injected from peripheral vein of left foot, and O-arm 3D scan was subsequently taken. The axial and sagittal position of vein structure surrounding L5/S1 disc was measured according to the parameters same as those in supine position on MRI (
Figure 2). The vein position on intraoperative CT was subsequently compared to that in supine position MRI, and the movement of vein structure was quantitatively analyzed (
Figure 2 and
Figure 4).
This study was conducted based on the acceptance of the university ethics committee, and patient data and radiographs without personal information in this report are shown with the consent of the patients.
3. Results
Evaluation of vascular anatomy in supine position
The average positions of right and left CIV were -22.2 mm (SD:4.1mm) and 8.2 mm (4.0) at L5 lower endplate level, and -27.9 mm (2.9) and 16 mm (4.4) at S1 upper endplate level, respectively (
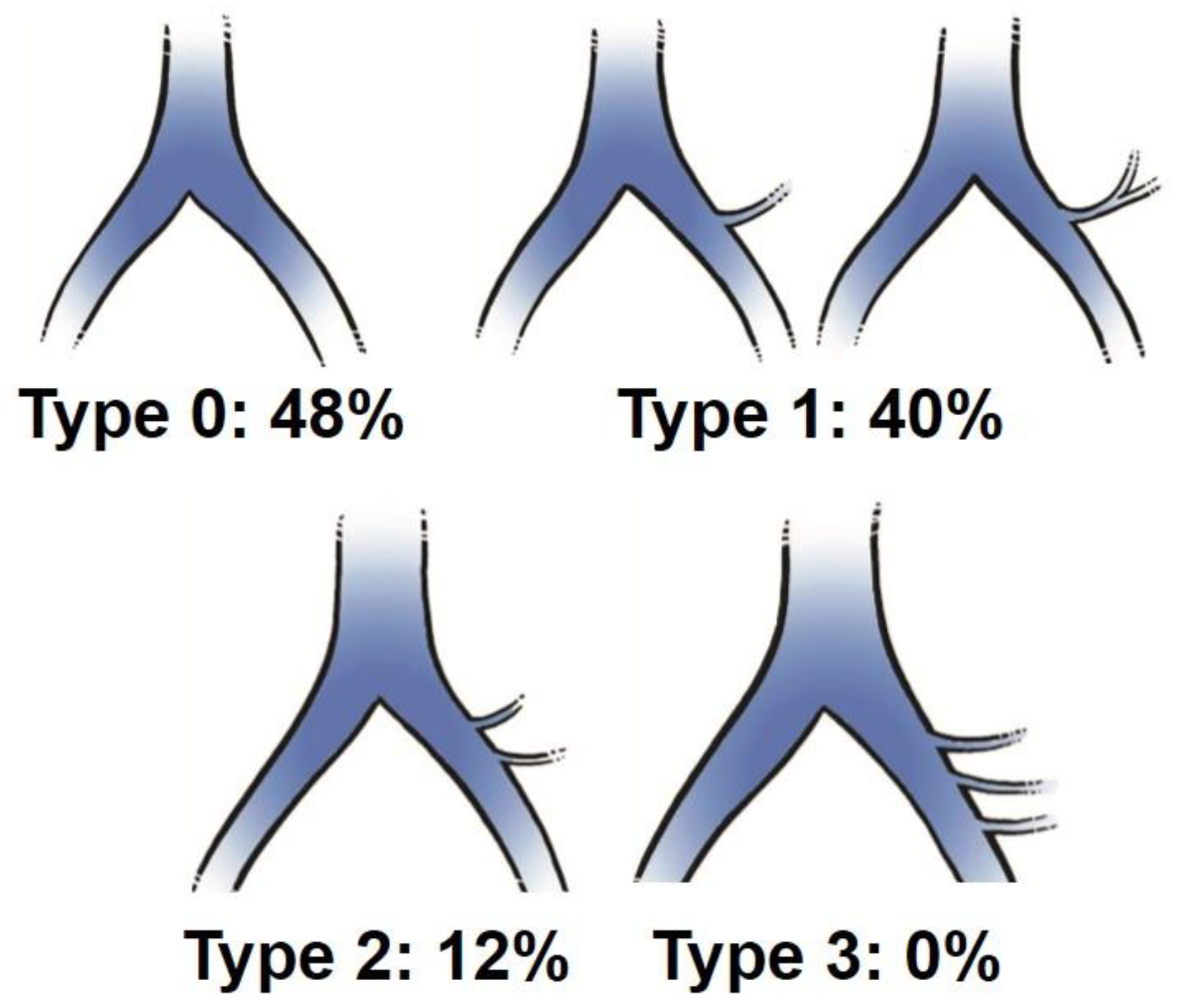
Table 1). The average positions of right and left CIA were -17.9 mm (4.5) and 17.8 mm (5.7) at L5 lower endplate level, and -21.3 mm (4.0) and 25.1 mm (5.3) at S1 upper endplate level, respectively. The average CCWs were 22.8 mm (7.3) at L5 lower endplate level, and 34.1 mm (7.3) at S1 upper endplate level. The average bifurcation position from L5 lower endplate was 25.3 mm (7.0mm SD). The average LCWs were 14.2 mm (4.8) at L5 lower endplate level, and 12.6 mm (3.6) at S1 upper endplate level. The visualization rate (%) of left iliolumbar vein (ILV) on preoperative MRI was 52% and the type was categorized into type 0 (48%), type 1 (40%), Type 2 (12%), and type 3 (0%) (
Figure 5). The average position of iliolumbar vein was 31.1 mm (5.7) at L5 lower endplate level, and 30.9 mm (8.1) at S1 upper endplate level (
Table 1).
Intraoperative evaluation of vein anatomy in right decubitus position
From the measurement of vein position on intraoperative enhanced CT, axial and sagittal movement of vascular structure were summarized in
Table 2. From the position change of supine to right decubitus position, right and left CIV moved to 0.8 mm and 3.8 mm to right at L5 lower endplate level, respectively (
Table 2). At S1 upper endplate level, left CIV moved 6.9 mm to right, and right CIV moves 0.3 mm to left. Overall, left CIV moved to right much more than right CIV. The CCW at L5 lower endplate level became 3.6 mm smaller than that in supine position. The CCW at S1 upper endplate level became 2.5 mm smaller than that in supine position. The vein bifurcation level moved 6.3 mm caudally when compared to supine position.
Case presentation
Case 1: 75 years old, female with L4 degenerative spondylolisthesis and L5/S1 degenerative disc disease received L4-S1 OLIF followed by lateral position percutaneous screwing and fixation. The comparison between preoperative supine MRI images and intraoperative vein enhanced CT demonstrated left CIV movement of 6.7mm to right in right decubitus position at L5 lower endplate level, and 3.4mm to right at S1 upper endplate level. The vein bifurcation moved to caudal direction in 8.5mm under right decubitus position (
Figure 6).
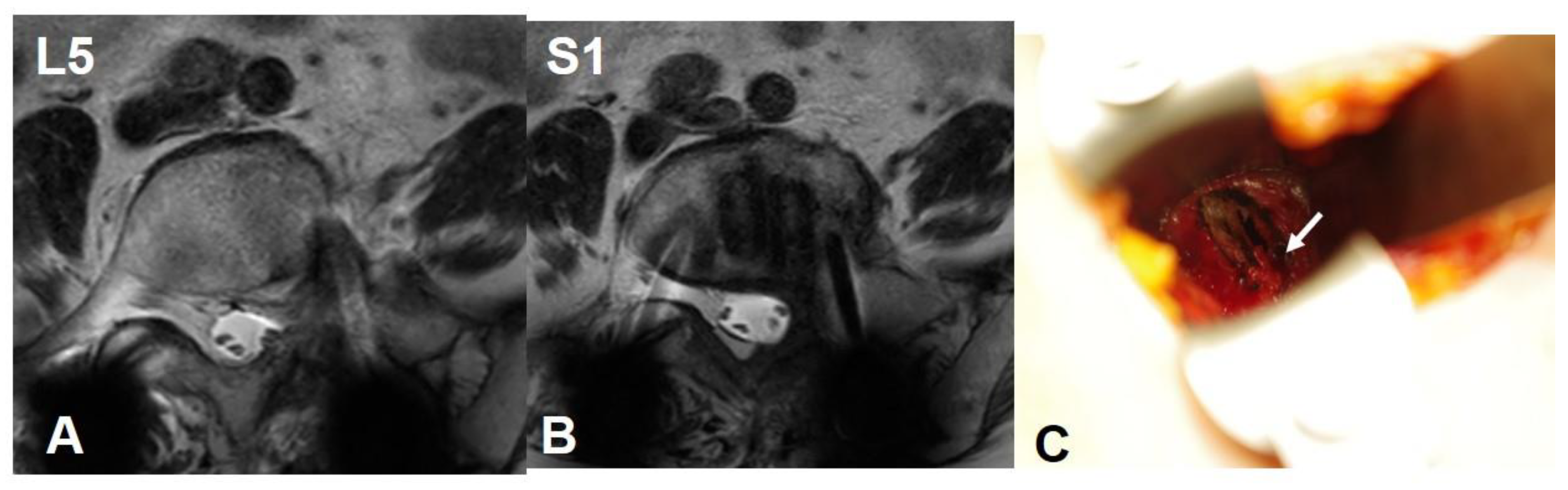
Case 2: 76 years old female, Pseudarthrosis of L5/S1 transforaminal interbody fusion.
The preoperative CCW was 7.4mm and 9.6mm at L5 and S1 level respectively. The lateral corridor approach was conducted instead of OLIF51 approach. The iliolumbar vein was ligated and interbody fusion was conducted successfully (
Figure 7).
The preoperative CCW was 7.4mm and 9.6mm at L5 and S1 level respectively. The lateral corridor approach was conducted instead of OLIF51 approach. The iliolumbar vein was ligated successfully.
4. Discussion
The preoperative evaluation for vascular structures is indispensable for the safe and accurate minimally invasive anterior approach to the lumbosacral spine. The supine MRI or enhanced CT scan are often used for the evaluation; however, the vascular and visceral structures move downwards under OLIF51 or LCA approach in lateral decubitus position. Deukmedjian et al. evaluated the movement of abdominal structures on MRI during supine and right decubitus position [
7]. They found some movement of aorta, vena cava, and kidney in lateral position, the precise vascular anatomy with reference to the disc was not demonstrated at L5/S1 level. This report first to demonstrate the precise vascular anatomy both in OLIF51 and LCA approaches as well as its movement under the change between supine and lateral decubitus position.
There were some studies reporting the vascular window (CCW) which allowed for OLIF51 approach at the L5/S1 disc level [
8,
9] (
Table 3). Choi et al. measured CCW at mid-disc level on MRI, demonstrating 27 mm in average (8-46) [
8]. Nagamatsu et al. utilized combined MRI and CT images and reported 29.7 mm at L5 caudal endplate level, and 36.9 mm at S1 cephalad endplate level [
9]. The present study showed 22.9 mm and 34.1 mm at L5 caudal and S1 cephalad endplate level, respectively. Our data was smaller in both levels in spite of larger body height compared to Nagamatsu’s report.
There have been three previous reports demonstrating the length from midline to left CIV at L5/S1 level [
10,
11,
12] (
Table 3). Liu et al. utilized CT angiography and reported the length of 15.9 mm in average [
10]. Davis et al. reported a similar length of 14.75 mm in the cadaveric measurement [
11]. In turn, Molinares et al. reported smaller value of 10 mm in average measured on MRI [
12]. Our data showed relatively smaller values of 8.7 mm and 16.0 mm at L5 caudal and S1 cephalad endplate level, respectively.
The bifurcation level of common iliac vein was reported by Davis and Nagamatsu [
9,
11]. Davis et al. reported 23.8 mm from L5 caudal endplate level, and Nagamatsu et al. reported 23.7 mm. Our data showed 25.7 mm, which was almost equivalent to other reports. The LCW length was reported by Molinares et al., showing 10.8 mm in average [
12]. The present study demonstrated 14.3 mm in average, reflecting the smaller CCW and larger LCW in our series.
In the present study, we found the iliolumbar vein in 52% on preoperative MRI scan. Nalbandian et al. examined the detailed anatomy of ILV in 159 cases of anterior lumbar open surgeries, and only 1.3% was missing the LIV [
9]. As the LIV systems were hard to be visualized clearly on either MRI or enhanced CT [
6,
13], our detection rate of 52% on MRI was relatively reasonable. In our evaluation, type 1 and type 2 were detected in 40% and 12% respectively (
Figure 5). In Nalbandian’s report, 73% showed single branch of type 1, and 17% was double branches of type 2 [
6]. We speculate that 48% of our type 0 may have a possibility to show ILVs when we actually expose in the operation field.
Using intraoperative enhanced CT, we quantitated the movement of vascular tissues from supine to right decubitus position when compared to preoperative supine MRI. As shown on
Table 2, there have been discrepancies of CIV movement between right and left sides. The left CIV moved more to right side in 3.8 mm and 6.9 mm at L5 caudal and S1 cephalad endplate level, respectively. This led to 3.6 mm and 2.5 mm decrease of vascular window at L5 caudal and S1 cephalad endplate level, respectively. Choi et al. compared vascular window between supine and right decubitus positioned MRI, showing 5.2 mm decrease of window [
8]. We examined the intraoperative anatomy in actual operative position under general anesthesia setting. In our OLIF51 surgery, the hip and knee were extended for more caudal incision to fit the sacral slope, so the vascular tension may increase in our series. The vein bifurcation moved caudally in 6.3 mm from supine to right decubitus position in our study. This was beyond our imagination and it also contributed to the narrowing of vascular window for OLIF51 approach.
The quantitative data demonstrated in this study will be useful for minimally invasive OLIF51 and LCA. The present study showed that average vascular window for OLIF51 approach was 23-34 mm, and it for LCA was 12-14 mm. This meant that the average L5/S1 disc anatomy required OLIF51 approach instead of LCA, however, there was a wide variation of CCW from 0 to 63 mm in our study. Liu et al. described that vascular window below 10 mm was impractical for OLIF51 surgery [
10]. Choi et al. described that in patients with vascular window below 15 mm and absence of perivascular fat, the extreme caution should be taken in OLIF51 approach [
8]. We recommend the OLIF51 candidate for the vascular window over 15 mm basically, however, there are many other important factors which needed to be considered. First, OLIF51 surgery basically required the mobility of left CIV (LCIV), and the adhesion between CIV and disc is a major limiting factor. When there is much perivascular fat, the good mobility is anticipated. However, when perivascular tissue is scarce, or LCIV is directly attached to the osteophyte, the vascular mobility may be limited. Chung et al. classified the relationship of LCIV and L5/S1 disc into three categories; type I: LCIV located at the lateral one-third of disc or floating from the disc, type II: medial two-third, but LCIV surrounded by perivascular fat, type III: no perivascular fat [
14]. Their data demonstrated that 49.2% was type I, 27.7% in type II and 23.1% in type III. They experienced five out of seven vascular injury cases were occurred in type III and it should be avoided. According to my OLIF51 experience over 220 cases, even in type III cases, the LCIV mobility was mostly obtained during surgery. For the successful retraction, the step-by-step retraction of LCIV and extensive disc release should be proceeded before extending the window. Secondly, the careful surgical indication should be considered. Specifically, the patients who received previous lateral interbody or transforaminal interbody fusion at the cephalad segment sometimes showed adhesions around the approaching plane. As is obvious in previous malignancy surgery of retroperitoneal area, the patients who even underwent intraabdominal surgery sometimes showed adhesions in retroperitoneal area. Therefore, the precise examination of past history and alternative cages or approach should be always prepared.
There were several advantages and limitations in this study. Although several studies investigated the vascular anatomy of OLIF51 or LCA approach, they utilized the cadaver or laterally positioned MRI [
8,
9,
11]. The present study measured the vascular anatomy in actual operative setting of OLIF51 surgery in right decubitus position using intraoperative enhanced CT (O-arm). This minimized the error in which the patient was not positioned in true lateral position on MRI, or muscular tonus changed the vascular position without general anesthesia. There was a technical limitation in which the measurement of vascular position was performed between supine MRI and enhanced CT. In a usual OLIF51 surgery setting, the author firstly takes MRI scan for vascular and neural observation. If the vascular window is very small, we add the enhanced CT, so most cases only received MRI without additional radiation exposure. To accurately compare both modalities, we set the gantry parallel to the L5 caudal or S1 cephalad endplate, and measured the vascular position precisely.
5. Conclusion
The precise measurement of vascular anatomy indicated that OLIF51 approach was the standard minimally invasive anterior approach for L5/S1 disc level compared to LCA, however, there were many variations in quantitative anatomy as well as significant vascular movements between supine and right decubitus position. In the clinical setting of OLIF51 and LCA surgeries, the careful preoperative evaluation and intraoperative 3D imaging are recommended for the safe and accurate surgery.
Author Contributions
Conceptualization, Y.K., T.S.; methodology, Y.K., H.T, T.T., and A.I.; measurement, Y.K., H.T, T.T., and A.I.; data analysis, Y.K., H.T, T.T., and A.I.; writing, Y.K. and H.T.; Supervision, T.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kansai Medical University (protocol code 2022330, March 2022).
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available in the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hodgson, A.R.; Stock, F.E.; Fang, H.S.Y.; et al. Anterior spinal fusion the operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg 1960, 48, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, K.; Taneichi, H.; Abumi, K.; et al. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg 1997, 79, 69–83. [Google Scholar] [CrossRef]
- Woods, K.; Billy, J.B.; Hynes, R. Technical description of oblique lateral interbody fusion at L1–L5 (OLIF25) and at L5–S1 (OLIF51) and evaluation of complication and fusion rates. The Spine J 2017, 17, 545–553. [Google Scholar] [CrossRef]
- Graham, R.B.; Wong, A.P.; Liu, J.C. Minimally invasive lateral transpsoas approach to the lumbar spine: pitfalls and complication avoidance. Neurosurg Clin N Am 2014, 25, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Houten, J.K.; Alexandre, L.C.; Nasser, R.; Wollowick, A.L. Nerve injury during the transpsoas approach for lumbar fusion: report of 2 cases. J Neurosurg Spine 2011, 15, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, M.W.; Hoashi, J.S.; Errico, T.J. Variations in the iliolumbar vein during the anterior approach for spinal procedures. Spine 2013, 38, e445–e450. [Google Scholar] [CrossRef] [PubMed]
- Deukmedjian, A.R.; Le, T.V.; Dakwar, E. Movement of abdominal structures on magnetic resonance imaging during positioning changes related to lateral lumbar spine surgery: a morphometric study. J Neurosurg Spine J Neurosurg Spine, 16, 615–615. [Google Scholar] [CrossRef]
- Choi, J.; Rhee, I.; Ruparel, S. Assessment of great vessels for anterior access of L5/S1 using patient positioning. Asian Spine J 2020, 14, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Nagamatsu, M.; Ruparel, S.; Tanaka, M.; et al. Assessment of 3D lumbosacral vascular anatomy for OLIF51 by non-enhanced MRI and CT medical image fusion techniques. Diagnostics 2021, 11, 1744. [Google Scholar] [CrossRef]
- Liu, L.; Liang, Y.; Zhang, H.; et al. Imaging anatomical research on the operative windows of oblique lumbar interbody fusion. Plos one 2016, 29. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.T.; Hynes, R.; Fung, D.A. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 2014, 21, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Molinares, D.M.; Davis, T.T.; Fung, D.A. Retroperitoneal oblique corridor to the L2-s1 intervertebral discs: an MRI study. J Neurosurg Spine 2016, 24, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Kleeman, T.J.; Michael, A.U.; Clutterbuck, W.B. Laparoscopic anterior interbody fusion at L4-5: an anatomic evaluation and approach classification. Spine 2002, 27, 1390–5. [Google Scholar] [CrossRef] [PubMed]
- Chung, N.S.; Jeon, C.H.; Lee, H.D. Preoperative evaluation of left common iliac vein in oblique lateral interbody fusion at L5-S1. Eur Spine J. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).